Abstract
Objective: To examine the effects of a 12-week therapeutic yoga program on gait speed, postural control, and mobility in community-dwelling older adults.
Design: Quasi-experimental study with a pretest/post-test design. Researchers evaluated changes over time (pretest to post-test) in all outcome measures. Paired t-tests were used to analyze normal and fast gait speed, Timed Up and Go test, and Timed Up and Go Dual Task. Wilcoxon signed-rank test was used to evaluate scores for the Mini-BESTest (MBT).
Setting: Yoga classes were performed at a local senior center. Blind examiners who were previously trained in the outcome measures performed all pretests and post-tests at the site.
Participants: Thirteen adults (12 women and 1 man, with a mean age±standard deviation of 72±6.9 years) completed the study. Research participants had minimal to no yoga experience.
Interventions: A 12-week, 60-minute, biweekly Kripalu yoga class designed specifically for community-dwelling older adults.
Outcome measures: Postural control (MBT), mobility (Timed Up and Go test), and gait speed (normal and fast) were assessed.
Results: All 13 participants attended at least 19 of the 24 classes (80% attendance). Statistically significant improvements were seen in the MBT (p=0.039), normal gait speed (p=0.015), fast gait speed (p=0.001), Timed Up and Go test (p=0.045), and Timed Up and Go Dual-Task (p=0.05).
Conclusions: Improvements in postural control and mobility as measured by the MBT and Timed Up and Go gait as measured by fast gait speed indicate that research participants benefitted from the therapeutic yoga intervention. The yoga program designed for this study included activities in standing, sitting, and lying on the floor and may be effective in improving mobility, postural control, and gait speed in community-dwelling older adults.
Introduction
Community-dwelling older adults are often defined as individuals over the age of 60 who reside independently in the community.1 One third of these individuals fall at least one time per year.2,3 In this population, falls represent the leading cause of death by injury,4 the most common cause of nonfatal injuries,5 and the most likely cause of fractures.6 Falls occur secondary to multiple risk factors:2,7 arthritis, symptoms of depression, orthostatis, impaired cognition, impaired balance and gait, decreased muscle strength, and polypharmacy.3,7–9 A study conducted by Rossat et al.3 found that the number of falls per patient increased with age, female sex, institutionalization, polypharmacy, the use of psychoactive drugs, increased time in the Timed Up and Go test (TUG), the use of a walking aid, muscle weakness, and increased fear of falling. Research suggests that reduction of one risk factor can reduce the overall risk of falling.7 Researchers have shown that reducing the number of prescription medications reduces falls,3,8 improving strength reduces falls,10–12 and improving measures of gait and balance reduces falls.13,14 In addition, group-based therapeutic exercise reduces falls in community-dwelling older adults7,11,15–17
Activities that incorporate complementary and alternative therapies are on the rise in the United States,18,19 with nearly 40% of adults and 12% of children in the United States using some form of complementary or alternative therapy.20,21 Complementary and alternative therapies are also recommended to the elderly to help maintain independence and mobility.22 In the U.S. population, 88% of older adults claim to use complementary and alternative therapies to treat conditions such as sleep disturbance, arthritis, back pain, heart disease, allergies, and diabetes.23 Complementary and alternative treatment of these conditions can reduce complications of chronic illnesses and increase quality of life. Yoga is one of the top 10 most commonly used alternative therapies.20 Yoga is accessible to the community-dwelling older adults and provides the benefits of group-based exercise.
The effects of yoga on cardiorespiratory function,24,25 anxiety and depression,26 stress,27 and low back pain28,29 have been examined. Zettergren et al.30 evaluated the effect of therapeutic yoga on postural control, mobility, rising from the floor, and gait speed in community-living older adults. Although researchers found improved postural control and gait speed, some limitations were noted, including small sample size and short intervention duration. Further investigation into the use of yoga as a general exercise and for possible use for prevention of falling is needed. Therefore, the purpose of this study was to assess the benefits of a therapeutic yoga program on one group of community-dwelling elderly individuals. The primary anticipated benefits are improved gait speed, postural control, and mobility.
Methods
Prospective participants were recruited from a local senior center by means of informational flyers and word of mouth. Participation eligibility was determined by prescreening measures that included an intake questionnaire, the Mini-Mental State Examination (MMSE), monofilament testing for bilateral feet, and an eye exam. Inclusion criteria for participation were (1) age 60 years or older, (2) ability to maintain upright standing with feet bare independently for 90 seconds without a device, (3) intact lower-extremity sensation, (4) visual acuity 20/20 (can be corrected), and (5) MMSE score of 24 or greater. Exclusion criteria for participation were (1) absence of any of the inclusion criteria, (2) history of neurologic pathology, (3) orthopedic surgery on either lower extremity within the last 3 years, (4) serious visual impairments (i.e., cataracts) or diagnosis of legally blind, and/or (5) preferred gait speed greater than 1.35 m/s for men or 1.29 m/s for women.31 Before participant recruitment, the Human Subjects Review Board at Quinnipiac University and the Quinnipiac University Institutional Review Board approved the study. Thirty-five participants (32 women and 3 men) were initially screened and deemed eligible to participate in the yoga program. Research participants were instructed to continue with any ongoing physical activities but were asked not to attend other yoga classes.
Procedures
The pretesting was completed the week before the start of yoga classes. Participants signed an informed consent form and were assured they could drop out without repercussions. Prospective participants were screened via a medical history questionnaire. The MMSE, monofilament testing, and an eye examination using a Snellen chart for visual acuity were performed. Once the aforementioned tests and measures were completed, researchers administered the Mini- BESTest (MBT) and measured participants' gait speed.
Two authors (physical therapist students) administered all tests. Both students demonstrated competence in administering the outcome measures before the pretesting sessions. One student performed the MBT on all participants, and the other performed the gait speed assessments for all participants. Tests were performed in random order.
The Yoga teachers (three authors) were blind to the results of all outcome measures. After 12 weeks of intervention, yoga participants who had completed the program were retested on all measures except the MMSE, monofilament testing, and visual acuity examination. Participants were also given note cards and asked to write down any comments or suggestions regarding the intervention.
Outcome measures
The MBT is a comprehensive balance assessment tool that identifies the six systems underlying postural control: biomechanical constraints, stability limits/verticality, anticipatory postural adjustments, postural responses, sensory orientation, and stability in gait.32 Research has shown that in addition to addressing the various systems underlying postural control, the MBT has a high ceiling effect, no floor effect, high reliability, and high content validity.32 The test takes approximately 10–15 minutes to administer. The MBT contains both unique assessment tools and components of the Berg Balance Scale, TUG, Ataxia Test Battery, Dynamic Gait Index, and the modified Clinical Test of Sensory Integration of Balance.33 The inclusion of these various components gives the MBT high consistency and reliability.32
Participants also underwent a gait speed assessment. Gait speed is an easily accessible and affordable measurement that is relevant to the safety and independence of older adults.31 Because walking is a complex functional activity that reflects functional and physiologic changes in the body, it can be used to predict falls and the potential need for rehabilitation in community-dwelling older adults.34 It is best to use walking speed with additional performance measures, such as the MBT, to predict future health status.35 At the pretest and post-test sessions, participants were timed while they walked a distance of 10 m on a level surface, with 2 m on each side of the marked 10-m distance to allow for acceleration and deceleration. Timing was completed using a stopwatch, which was started and stopped as the participants' mid-sagittal line crossed the tape at either end of the 10-m walkway. The reliability of gait speed measures, whether made by a stopwatch or electronic walkway, is well established.36 Participants were instructed to walk at a comfortable pace, stopping when they reached the opposite side of the marked path. After two trials at a self-selected speed, the process was repeated with participants instructed to walk as fast as they safely could. A value for gait speed was derived by dividing the length walked by the time. A mean of two trials was taken for both the self-selected speed and fast walking speed. The means of the trials were used in the data analysis to determine an average gait speed for each participant. Because gait speed varies with age and gender, the speeds the participants walked were compared with the normal values for their age group. The normal gait speeds used in clinical practice for women and men aged 70 to 79 are 1.13 m/sec and 1.26 m/sec, respectively.37
Yoga intervention
Yoga sessions were 60 minutes of Kripalu-style yoga. The sessions included pranayama (breathing exercises) and body awareness (5 minutes); warm-up activities (5 minutes); asana (physical postures) in the seated, standing, and supine positions (40 minutes); and meditation and shavasana (10 minutes). Yoga classes were designed by the primary investigator, a physical therapist and certified Kripalu yoga teacher. Classes were taught by three authors (physical therapy students and level 3 YogaFit instructors). Classes were specifically designed for the older adult with impaired mobility and postural control. Props and modifications were provided to participants when needed.
Each session began with seated centering and pranayama. The specific pranayama used were diaphragmatic breathing and the full yogic breath (three-part breath).38,39 After pranayama, a 5-minute warm-up was performed that included seated shoulder circles, wrist and neck rolls, standing heel and toe raises, hip circles, and heel walking. Standing yoga postures used in the program included tadasana (mountain pose), virabhadrasana I (warrior I), virabhadrasana II (warrior II), trikonasana (triangle pose), vrikshasana (tree pose [Fig. 1]), and utkata konasana (goddess pose). Additional postures included virabhadrasana III (warrior III) and ardha chandrasana (half-moon pose). These standing poses were chosen for their ability to increase strength in the quadriceps, tibialis anterior, and gastrocnemius to target potential gait and balance deficits. Participants were encouraged to engage the ankle dorsiflexors by lifting their toes during mountain pose. Vrikshasana (tree pose) requires the participants to attain and maintain unilateral standing. Participants were encouraged to attempt the pose without support but were allowed to use a chair if assistance was needed. Other poses included adho mukha svanasana (downward-facing dog pose [Fig. 2]) to increase upper-extremity weight bearing and promote stretching of the gastrocnemius/soleus groups and hamstrings, setu bandhasana (bridge pose) for overall lower-extremity strengthening, and badda konasana (bound angle pose) to increase hip range of motion. Each session ended with relaxation in shavasana (corpse pose).
FIG. 1.

Vrikshasana (tree pose).
FIG. 2.

Adho mukha svanasana (downward-facing dog).
Data analysis
Data were analyzed by using SPSS software, version 21 (IBM, Inc., Chicago, Illinois). Paired t-tests were used to assess the following outcome variables: TUG, TUG Dual Task (TUG-DT), and gait speed (self-selected and fast). A Wilcoxon signed-ranks test was used to determine p values for the MBT because the MBT generates nonparametric data. Paired t-tests were used to assess TUG and TUG-DT because in addition to assigning a rank to these tests, per the MBT, actual timed data (in seconds) were also collected. A p-value<0.05 was used to determine statistical significance.
Results
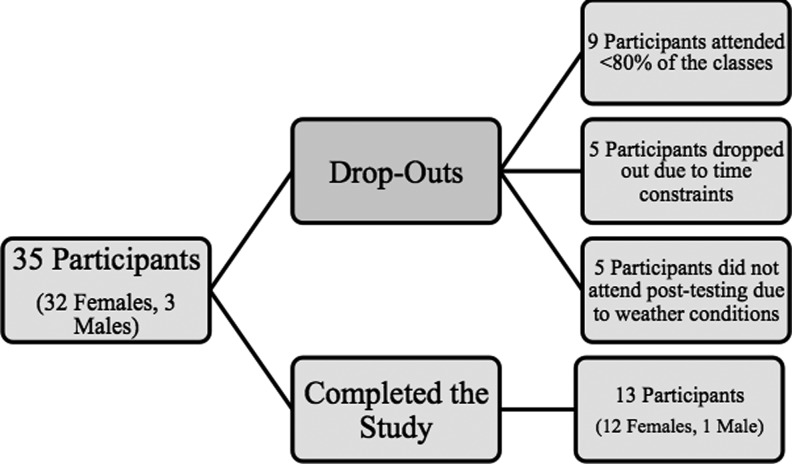
Thirty-five participants began the initial yoga program, and 13 participants (12 women and 1 man) completed the biweekly yoga program over the 12-week period. All yoga participants were required to attend 19 of the 24 yoga sessions (80%) to be eligible for post-testing. Of the 35 participants, 13 attended the required number of sessions. Of the 22 participants who did not complete the study, 9 did not attend the required number of yoga classes and were not included in the post-testing, 5 did not attend post-testing because of weather conditions, and 5 dropped out of the exercise program because of time constraints (Fig. 3). Of the 13 participants who were post-tested, 9 attended between 80%–90% of the classes, 3 attended 90%–99% of the classes, and 1 attended 100% of the classes. The average age of participants (±standard deviation) who completed the study was 72±6.9 years. On the basis of intake data and pretest results, there were no significant differences between participants who completed the study and those who dropped out of the study.
FIG. 3.
Participants selection.
In the yoga group, paired t-tests revealed statistically significant improvements in gait speed and mobility as measured by self-selected gait speed (p=0.015), fast gait speed (p=0.001), TUG test (p=0.045), and TUG-DT (p=0.050). The Wilcoxon signed-rank test revealed a statistically significant improvement in postural control and mobility as measured by the MBT (p=0.039) (Table 1).
Table 1.
Study Results
| Test | Data analysis test | Pretest average±SD | Post-test average±SD | Mean difference | p-Value |
|---|---|---|---|---|---|
| Mini-BESTest (points) | Wilcoxon signed-rank test | 22.8 | 24.31 | 1.46 | 0.039* |
| Normal gait speed (m/sec) | Paired t-test | 1.08±0.27 | 1.17±0.28 | −0.089 | 0.015* |
| Fast gait speed (m/sec)_ | Paired t-test | 1.33±0.28 | 1.55±0.35 | −0.22 | 0.001* |
| TUG (sec) | Paired t-test | 8.58±3.72 | 8.05±3.75 | 0.53 | 0.045* |
| TUG-DT (sec) | Paired t-test | 11.48±5.29 | 11.27±4.53 | 0.21 | 0.050 |
p<0.05.
SD, standard deviation; TUG, Timed Up and Go; TUG-DT, Timed Up and Go Dual Task.
The TUG and TUG-DT were components of the MBT analyzed individually. The average TUG scores of the 13 participants during pretesting and post-testing were 8.58 seconds and 8.05 seconds, respectively. The average improvement in TUG score was 0.53 seconds. The average TUG-DT scores of the 13 participants during pretesting and post-testing were 11.48 seconds and 11.27 seconds, respectively. The average improvement was 0.21 seconds (Table 1).
Gait was analyzed via paired t-tests. The results of the analysis revealed a statistically significant difference in normal and fast walking speed of yoga participants following the intervention. The 13 yoga participants who completed the study began the program with an average self-selected gait speed of 1.08±0.27 m/sec and ended with 1.17±0.45 m/sec, demonstrating a 089-m/sec improvement in self-selected gait speed. These participants also began the program with an average fast gait speed of 1.33±0.28 m/sec and ended with an average fast gait speed of 1.55±0.035 m/sec, demonstrating a 0.22-m/sec improvement in fast gait speed (Table 1).
Discussion
The results of the study support the use of a 12-week yoga program as an intervention to improve measures of postural control, mobility, and ambulation in community-dwelling older adults. Yoga participants reported positive experiences with the intervention program. Many of the poses practiced during the intervention program enhance dynamic control of stabilizing muscles of the hips as well as the core musculature.40 Weakness of the core musculature and imbalance of the hip-stabilizing musculature have been associated with lower-extremity instability and may contribute to impaired postural control.40 In addition, other muscles of the lower extremities that are fundamental for postural control and ambulation were activated in the poses practiced during the program.
The MBT identifies impairments in postural control by assessing dysfunctions in biomechanical constraints, stability limits, verticality, anticipatory postural adjustments, postural responses, sensory orientation, and stability in gait. Normal MBT scores for adults aged 70–79 years is 21±3.1. Although participant MBT scores improved (p=.039), the improvement did not satisfy criteria for minimal clinical difference. The minimal clinical difference for the MBT is 3.5 points. Participants had high baseline scores that may have contributed to the change in MBT score of only 1.46 points.
To date, there is no documented evidence on how yoga improves participant's scores on the MBT; however, inferences can be drawn from current knowledge of muscle activation during yoga poses.40,41 Mountain pose may improve participants' confidence in standing because it promotes even weight distribution through both feet. This pose may also improve pelvic stabilization and postural control because it requires coactivation of hip flexors and extensors.41 Warrior I emphasizes stepping and weight shifting and improves quadriceps and hamstring muscle length.41 Warrior II also emphasizes stepping and may stretch the adductor muscle group.42 It also strengthens the quadriceps and hamstring muscle group and the gluteus maximus muscle, which are important muscles activated during the gait cycle. Tree pose may improve gastrocnemius and hamstring muscle strength, as well as unilateral stance, and thus will improve postural control.41
Chui and Lusardi35 report average TUG scores for healthy older adults aged 70–79 years as 7.7±2.3 seconds. The minimal clinical difference for TUG scores has been reported as 1.0–2.39 seconds.35 The current participants demonstrated an average improvement of 0.212 seconds in the TUG. Although scores improved, the improvement was not great enough to achieve the minimal clinical difference; thus, the finding is statistically significant but not clinically significant. The small sample size may have prevented detection of clinical significance.36 In addition, only 37% of the originally screened participants completed the study. This high drop-out rate may also contribute to detection of clinical significance and overall generalizability.
No studies have examined the average scores or the minimal clinical difference of the TUG-DT. The participants did demonstrate a statistically significant improvement on the TUG-DT. Participating in a 12-week yoga program may improve TUG-DT scores because participants are asked to maintain postures (asana) while coordinating their breath.41 In poses such as warrior I and II, participants place one lower extremity forward and the other back, thus performing different activities with each extremity.41 These poses require not only core stability and overall muscle strength but also concentration and focus on the task at hand.
Gait speed is an important measure used to determine ambulatory status and an individual's potential for rehabilitation.34,36 The minimal clinical difference of fast gait speed in adults aged 70–79 years of age is 0.18 m/sec.36,42 Fast gait speed scores from the patient population analyzed in this study showed an improvement of 0.22 m/sec. This indicates a clinically significant difference, demonstrating an increase in fast gait speed that was greater than the published minimal clinical difference for this age group.42 Thus, the participants in this study demonstrated a clinically meaningful improvement in fast walking ability, which could lead to improved balance and functional mobility and reduce energy expenditure and risk for disability and falls.42
Yoga intervention may improve participants' self-selected and fast gait speeds. Tree pose encourages active engagement of the gastrocnemius muscle, and the heel and toe raises the participants performed directly strengthened the gastrocnemius-soleus muscle complex, as well as the anterior tibialis muscle.41 The gastrocnemius-soleus complex is important in the push-off phase of gait and is a crucial component in maintaining normal energy expenditure in ambulation.41 The anterior tibialis is important for foot clearance in gait, contributing to a reduced fall risk. Chair pose increases the strength of the quadriceps, which are crucial in promoting full knee extension between terminal stance and preswing, contributing to normal step length.41 Tree pose may improve gastrocnemius and hamstring muscle strength, as well as balance in unilateral stance, contributing to an increase in walking speed.41 Many of the previously described poses promote ankle stabilization muscle activation and intrinsic foot muscle activation, thus leading to improved postural stability and gait speed.
Conclusion
One of every four community-dwelling older adults have at least two falls per year.3 Group exercise programs decrease fall frequency, increase balance, and improve quality of life in this population.43,44 Yoga is an ideal group exercise program to improve postural control and mobility, reduce the risk of falling, and increase community participation in older adults. The participants in our yoga program expressed gratitude for the program. After the post-testing, participant number 6 stated, “I feel stronger in standing and in other things that I do everyday.” Participant number 29 noted, “I feel better and more in tune with my body and mind.”
Acknowledgments
The authors thank the Wallingford Senior Center for providing a location to perform the yoga treatment sessions and thank Denise Cameron, PT, PhD, for her assistance with data analysis.
Author Disclosure Statement
No competing financial interests exist.
References
- 1.Shumway-Cook A, Baldwin M, Polissar NL, Gruber W. Predicting the probability for falls in community-dwelling older adults. Phys Ther 1997;77:812–819 [DOI] [PubMed] [Google Scholar]
- 2.Brown C, Gottschalk M, Van Ness P, Fortinsky R, Tinetti M. Changes in physical therapy providers use of fall prevention strategies following a multi component behavior change intervention. Phys Ther 2005;85:394–403 [PubMed] [Google Scholar]
- 3.Rossat A, Fantino B, Nitenberg C, et al. Risk factors for falling in community-dwelling older adults: which of them are associated with the recurrence of falls? J Nutr Health Aging 2010;14:787–791 [DOI] [PubMed] [Google Scholar]
- 4.Murphy SL. Deaths: final data for 1998. National Vital Statistics Reports: National Center for Health Statistics; 2000;48. [PubMed] [Google Scholar]
- 5.Alexander BH, Rivara FP, Wolf ME. The cost and frequency of hospitalization for fall-related injuries in older adults. Am J Public Health 1992;82:1020–1023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bell AJ, Talbot-Stern JK, Hennessy A. Characteristics and outcomes of older patients presenting to the emergency department after a fall: a retrospective analysis. Med J Austral 2000;173:176–177 [DOI] [PubMed] [Google Scholar]
- 7.Tinetti M. Preventing falls in elderly persons. N Engl J Med 2003;348:42–50 [DOI] [PubMed] [Google Scholar]
- 8.Carter ND, Kannus P, Khan KM. Exercise in the prevention of falls in older people: a systematic literature review examining the rationale and the evidence. Sports Med. 2003;1:427–438 [DOI] [PubMed] [Google Scholar]
- 9.Ray W, Griffin MR. Prescribed medications and the risk of falling. Topics Geriatr Rehabil 1990;5:12–20 [Google Scholar]
- 10.Liu-Ambrose T, Khan KM, Eng JJ, Janssen PA, Lord SR, McKay HA. Resistance and agility training reduce fall risk in women aged 75–85 with low bone mass: a 6-month randomized, controlled trial. J Am Geriatr Soc 2004;52:657–665 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.LaStayo PC, Ewy GA, Pierotti DD, Johns RK, Lindstedt S. The positive effects of negative work: increased muscle strength and decreased fall risk in a frail elderly population. J Gerontol 2003;58A:419–424 [DOI] [PubMed] [Google Scholar]
- 12.Province M, Hadley E, Hornbrook M, et al. The effects of exercise on falls in elderly patients. A preplanned meta-analysis of the FICSIT trials. Frailty and injuries: cooperative studies of intervention techniques. JAMA 1995;273:1341–1347 [PubMed] [Google Scholar]
- 13.Shumway-Cook A, Gruber W, Baldwin M, Liao S. The effect of multidimensional exercise on balance, mobility, and falls risk in community dwelling older adults. Phys Ther 1997;77:46–57 [DOI] [PubMed] [Google Scholar]
- 14.Skelton DA, Beyer N. Exercise and injury prevention in older people. Scand J Med Sci Sports 2003;13:77–85 [DOI] [PubMed] [Google Scholar]
- 15.Barnett A, Smith B, Lord S, Williams M, Baumand A. Community-based group exercise improves balance and reduces falls in at-risk older people: a randomized controlled trial. Age Ageing 2003;32:407–414 [DOI] [PubMed] [Google Scholar]
- 16.Rubenstein LZ, Josephson KR, Trueblood PR, et al. Effects of a group exercise program on strength, mobility and falls among fall-prone elderly men. J Gerontol A Biol Sci Med Sci 2000:55:M317–M321 [DOI] [PubMed] [Google Scholar]
- 17.Buchner DM, Cress ME, de Lateur BJ, et al. The effect of strength and endurance training on gait, balance, fall risk, and health services use in community-living older adults. J Gerontol A Biol Sci Med Sci 1997;52:M218–M224 [DOI] [PubMed] [Google Scholar]
- 18.Saper RB, Eisenberg DM, Davis RB, Culpepper L, Phillips RS. Prevalence and patterns of adult yoga use in the united states: results of a national survey. Alternat Ther Health Med 2004;10:44–49 [PubMed] [Google Scholar]
- 19.Tindle HA, Davis RB, Phillips RS, Eisenberg DM. Trends in use of complementary and alternative medicine by US adults: 1997–2002. Altern Ther Health Med 2005;11:42–49 [PubMed] [Google Scholar]
- 20.National Center for Complementary and Alternative Medicine. The use of complementary and alternative medicine in the United States2007 Online document at: http://nccam.nih.gov/news/camstats/2007/camsurvey_fs1.htm#use Accessed March7, 2014
- 21.Barnes P, Bloom B, Nahin R. Complementary and alternative medicine use among adults and children: United States 2007. Natl Health Stat Report 2008;12:1–23 [PubMed] [Google Scholar]
- 22.Birkel D. Activities for the older adult: integration of the body and the mind. J Phys Educat Rec Dance. 1998;69:23–28 [Google Scholar]
- 23.Cuellar N, Rogers A, Hisghman B. Evidenced based research of complementary and alternative medicine (CAM) for sleep in community dwelling older adults. Geriatr Nurs 2007;28:46–52 [DOI] [PubMed] [Google Scholar]
- 24.McCaffrey R, Ruknui P, Hatthakit U, Kasetsomboon P. The effects of yoga on hypertensive persons in Thailand. Holist Nurs Prac 2005;19:173–180 [DOI] [PubMed] [Google Scholar]
- 25.Jayasinghe SR. Yoga in cardiac health (a review). Eur J Cardiovasc Prev Rehabil 2004;11:369–75 [DOI] [PubMed] [Google Scholar]
- 26.Brown RP, Gerberg PL. Sudarshan Kriya yogic breathing in the treatment of stress, anxiety, and depression: part I—neurophysiologic model. J Altern Complement Med 2005;11:383–384 [DOI] [PubMed] [Google Scholar]
- 27.McComb R, Tacon A, Randolph P, Caldera Y. A pilot study to examine the effects of a mindfulness-based stress-reduction and relaxation program on levels of stress hormones, physical functioning, and submaximal exercise responses. J Altern Complement Med 2004;10:819–827 [DOI] [PubMed] [Google Scholar]
- 28.Galantino JL, Bzdweka TM, Eissler-Russo JI, et al. The impact of modified hatha yoga on chronic low back pain: a pilot study. Altern Ther Health Med. 2004;10:56–59 [PubMed] [Google Scholar]
- 29.Williams KA, Pertronis J, Smith D, et al. Effect of Iyengar yoga therapy for chronic low back pain. Pain. 2005;115:107–117 [DOI] [PubMed] [Google Scholar]
- 30.Zettergren K, Lubeski J, Viverito J. Effects of a yoga program on postural control, mobility, and gait speed in community-living older adults: a pilot study. J Geriatr Phys Ther 2011;34:88–94 [DOI] [PubMed] [Google Scholar]
- 31.Bohannon RW. Population representative gait speed and its determinants. J Geriatr Phys Ther 2008;31:49–52 [DOI] [PubMed] [Google Scholar]
- 32.Horak FB, Wrisley DM, Frank J. The balance evaluation systems test (BESTest) to differentiate balance deficits. J Am Phys Ther 2009;89:484–498 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Franchignoni F, Horak F, Godi M, et al. Using psychometric techniques to improve the balance evaluation systems test: the mini-bestest. J Rehabil Med 2010;42:323–331 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Fritz S, Lusardi M. White paper: walking speed: the sixth vital sign. J Geriatr Phys Ther 2009;32:2–5 [PubMed] [Google Scholar]
- 35.Chui K, Lusardi M. Spatial and temporal parameters of self-selected and fast walking speeds in health community-living adults aged 72–98 year. J Geriatr Phys Ther 2010;33:173–83 [PubMed] [Google Scholar]
- 36.Lusardi M. Functional performance in community living older adults. J Geriatr Phys Ther 2003;26:14–22 [Google Scholar]
- 37.Bohannon A, Andrews AW. Normal walking speed: a descriptive meta-analysis. Physiotherapy 2011;97:182–189 [DOI] [PubMed] [Google Scholar]
- 38.Faulds R. Kripalu Yoga: A Guide to Practice On and Off the Mat. New York, New York: Bantam Books; 2006 [Google Scholar]
- 39.Keller D. Refining the Breath: The Yogic Practice of Pranayama. 3rd ed. Herndon, VA: DoYoga; 2003 [Google Scholar]
- 40.Ni M, Mooney K, Harriell K, Balachandran A, Signorile J. Core muscle function during specific yoga poses. Complement Therap Med 2014;22:235–243 [DOI] [PubMed] [Google Scholar]
- 41.Zettergren K, Simon L, Stawicki A. An electromyographic analysis of selected yoga asana: a comparison between inexperienced and experienced yogic practitioners. Presented at the APTA Combined Sections Meeting, San Diego, CA, January20–24, 2013 [Google Scholar]
- 42.Fulk GD, Ludwig M, Dunning K, et al. Estimating clinically important change in gait speed in people with stroke undergoing outpatient rehabilitation. J Neurol Phys Ther 2011;35:82–89 [DOI] [PubMed] [Google Scholar]
- 43.Lusardi M, Pellecchia G, Schulman M. Functional performance in community living older adults. J Geriatr Phys Ther 2003;26:14–22 [Google Scholar]
- 44.Martin JT, Wolf A, Moore J, Rolenz E, DiNinno A, Reneker JC. The effectiveness of physical therapist-administered group-based exercise on fall prevention: a systematic review of randomized controlled trials. J Geriatr Phys Ther 2013;36:182–193 [DOI] [PubMed] [Google Scholar]