Abstract
Importance
Hypertension control for large populations remains a major challenge.
Objective
To describe a large-scale hypertension program in northern California and to compare rates of hypertension control of the program to statewide and national estimates.
Design, Setting, and Patients
The Kaiser Permanente Northern California (KPNC) Hypertension program included a multi-faceted approach to blood pressure control. Patients identified with hypertension within an integrated health care delivery system in northern California from 2001–2009 were included. The comparison group included insured patients in California between 2006–2009 who were included in the Healthcare Effectiveness Data and Information Set (HEDIS) commercial measurement by California health insurance plans participating in the National Committee for Quality Assurance (NQCA) quality measure reporting process. A secondary comparison group was the reported national mean NCQA HEDIS commercial rates of hypertension control from 2001–2009 from health plans that participated in the NQCA HEDIS quality measure reporting process.
Main Outcome Measure
Hypertension control as defined by NCQA HEDIS.
Results
The KPNC hypertension registry established in 2001 included 349,937 patients and grew to 652,763 by 2009. The NCQA HEDIS commercial measurement for hypertension control increased from 44% to 80% during the study period. In contrast, the national mean NCQA HEDIS commercial measurement increased modestly from 55.4% to 64.1%. California mean NCQA HEDIS commercial rates of hypertension were similar to those reported nationally from 2006–2009. (63.4% to 69.4%).
Conclusion and Relevance
Among adults diagnosed with hypertension, implementation of a large-scale hypertension program was associated with a significant increase in hypertension control compared with state and national control rates.
Keywords: Hypertension, Single pill combination Therapy, Angiotensin Enzyme Converting Inhibitor, Hydrochlorothiazide, Quality
INTRODUCTION
Hypertension affects 65 million adults in the US, 29% of Americans age ≥18 years,1 and is a major contributor to cardiovascular disease.2 Despite availability of effective therapies for >50 years,3 fewer than half of Americans with hypertension had controlled blood pressure In 2001–2002.1 Many hypertension control quality improvement strategies exist,4–10 but to date, no successful, large-scale program sustained over a long period of time has been described. In a review of 72 clinical trials,11 several interventions have been identified that improve blood pressure control in primary care settings, with the strongest evidence for an organized, comprehensive system of regular population review and intervention. Kaiser Permanente Northern California (KPNC) is a not-for-profit, integrated health care delivery system caring for >2.3 million adult members, with comprehensive inpatient and outpatient care provided through 21 hospitals, 45 medical facilities, and >7,000 physicians. In 2001, KPNC developed a system-level, multi-faceted hypertension quality improvement program. We describe the details of the development and implementation of this program and its associated results between 2001–2009.
METHODS
KPNC hypertension program
The study was exempted from review by the Kaiser Foundation Research Institute’s Institutional Review Board. The KPNC hypertension quality improvement program included five major components.
1. Health system-wide hypertension registry
In 2000, KPNC developed a large-scale program to improve blood pressure control. Patients with hypertension were identified quarterly using outpatient diagnostic codes, pharmacy data and hospitalization records from health plan databases, and diagnoses were verified through chart review audits of random samples of identified members. Patients were included if they met any of the following: (1) ≥2 hypertension diagnoses coded in primary care visits in the prior 2 years, (2) ≥1 primary care hypertension diagnosis and ≥1 hospitalization with a primary or secondary hypertension diagnosis in the prior 2 years, (3) ≥1 primary care hypertension diagnosis and ≥1 filled prescriptions for hypertension medication within the prior 6 months, or (4) ≥1 primary care hypertension diagnosis and ≥1 stroke-related hospitalization or a history of coronary disease, heart failure or diabetes mellitus. Per National Committee for Quality Assurance (NCQA) Healthcare Effectiveness Data and Information Set (HEDIS) specifications, patients were not included based on recorded blood pressure measurements alone.
2. Hypertension control rates
KPNC reported annual hypertension control rates to the NQCA in accordance with HEDIS specifications.12 The NCQA HEDIS definition was based on the blood pressure reading from the most recent visit with a reading during the measurement year (and after the diagnosis of hypertension was made). In KPNC, typical practice included blood pressure measurement by automated sphygmomanometers operated by trained medical assistants, with repeat measurements performed, as needed, by physicians using aneroid sphygmomanometers. A random sample of patient records was generated consisting of members aged 18–85 years (46–85 years before 2006) as of December 31 of the measurement year who were continuously enrolled, had ≥1 hypertension diagnosis confirmed in the medical record on or before June 30 of that year. The number of sampled patient charts (305–411 per year) was determined by NCQA HEDIS specifications.12 Individuals were excluded if they had end-stage renal disease, were pregnant, or admitted to a non-acute inpatient setting any time during the measurement year. The most recent outpatient, non-emergency department blood pressure measurement was used for the performance metric, excluding those taken during outpatient visits for the sole purpose of having diagnostic tests or surgical procedures performed (e.g., sigmoidoscopy), obtained the same day as a major diagnostic or surgical procedure (e.g., stress test, endoscopy), or patient self-reported values. Control was defined per NCQA HEDIS as both systolic blood pressure <140 mmHg and systolic blood pressure <90 mmHg (≤140/90 mmHg before 2006). If multiple readings were recorded for a single date, the lowest systolic and lowest diastolic blood pressure was used as the representative blood pressure but the systolic and diastolic results did not have to be from the same reading. If no blood pressure was recorded during the measurement year, the patient was classified as “not controlled.”
In 2001, internal hypertension control reports were developed for quality improvement use, and performance measurements were designed that were similar to those of the NCQA HEDIS metric described above. However, unlike the NCQA HEDIS measurement which included only a random sample of eligible individuals, the internal metric included all KPNC individuals eligible for inclusion in the NQCA HEDIS hypertension control metric: continuously enrolled members aged 18–85 years (46–85 years before 2006) as of December 31 of the measurement year with documented hypertension in the medical record on or before June 30 of the measurement year. Patients were excluded from the internal hypertension control metric using the same criteria as the NCQA HEDIS commercial metric. The number of individuals used to calculate the internal hypertension control metric varied from 234,852 in 2001 to 353,156 in 2009.
Hypertension control reports were generated every 1–3 months for each KPNC medical center and distributed to their directors. During the study period, a central hypertension management team identified successful practices and disseminated effective strategies to the medical centers.
3. Development of an evidence-based practice guideline
In 2001, an evidence-based, four-step hypertension control algorithm was developed to aid clinicians (Table 1). The guideline was updated every two years based on emerging randomized trial evidence and national guidelines. Clinicians were encouraged to follow the algorithm unless clinical discretion required otherwise. Dissemination of guidelines occurred through distribution of printed documents, email, clinical tools (e.g., pocket cards), videoconferences, lectures, partnering with pharmacy managers, and use of the electronic medical record to optimize medication selection.
Table 1.
Summary of evidence-based clinical practice guideline for initial therapy and treatment intensification for the Kaiser Permanente Northern California Hypertension Program, by year.
| Year | 2001 | 2003 | 2005 | 2007 | 2009 |
|---|---|---|---|---|---|
| Step 1 | TD or BB | TD | TD or TD + ACEI | TD or TD + ACEI | TD or TD + ACEI |
| Step 2 | TD + BB | TD + ACEI or TD + BB | TD + ACEI | TD + ACEI | TD + ACEI |
| Step 3 | TD + BB + ACEI | TD + BB + ACEI | TD + BB + ACEI | TD + BB + ACEI | TD + ACE + DCCB |
| Step 4 | TD + BB + ACEI + DCCB | TD + BB + ACEI + DCCB | TD + BB + ACEI + DCCB | TD + BB + ACEI + DCCB | TD + ACE + DCCB + BB or Spironolactone |
TD = thiazide diuretic; BB = beta-blocker; ACEI = angiotensin-converting enzyme Inhibitor; and DCCB=dihydropyridine calcium channel blocker
4. Medical assistant visits for follow-up measurements
In 2007, all medical centers developed a medical assistant follow-up visit typically scheduled two to four weeks after a medication adjustment. Typically, a medical assistant measured blood pressure and informed the primary care physician, who then directed treatment decisions and follow-up planning. Medical assistants were trained using standardized materials and blood pressure competency assessments. Patients were not charged a co-payment for these visits. This system accelerated treatment intensification without significantly increasing the need for repeat clinician visits while simultaneously improving patient convenience and affordability.
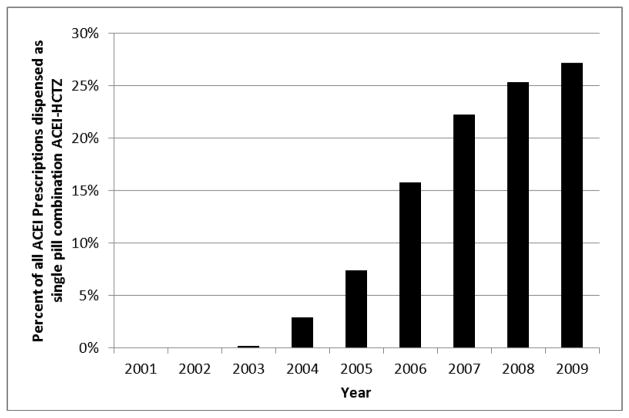
5. Promotion of single-pill combination (SPC) therapy
In 2005, SPC therapy with lisinopril-hydrochlorothiazide was incorporated into the regional guideline as being optional for initial treatment and recommended as a step two strategy (Table 1).
Patient characteristics
Information on demographic characteristics was available for patients in the hypertension registry (Table 2). Diabetes mellitus was ascertained from a regional diabetes registry (see Appendix for details).13
Table 2.
Patient characteristics of the Kaiser Permanente Northern California (KPNC) Hypertension Registry, 2001–2009.
| Year | 2001 | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 |
|---|---|---|---|---|---|---|---|---|---|
| KPNC total adult population, N | 2,278,043 | 2,345,910 | 2,325,616 | 2,339,898 | 2,384,895 | 2,421,141 | 2,423,368 | 2,416,095 | 2,371,761 |
| KPNC Hypertension Registry, N | 349,937 | 415,687 | 432,611 | 509,783 | 543,650 | 572,100 | 600,523 | 610,724 | 652,763 |
| % of total KPNC adult membership | 15.4% | 17.7% | 18.6% | 21.8% | 22.8% | 23.6% | 24.8% | 25.3% | 27.5% |
| Mean ± SD age, yr | 63.0 ± 13.6 | 63.0 ± 13.8 | 62.9 ± 13.8 | 63.0 ± 13.9 | 63.0 ± 13.9 | 62.9 ± 14.0 | 63.0 ± 14.1 | 63.3 ± 14.2 | 63.0 ± 14.4 |
| Age category, yr | |||||||||
| 18–44 | 10.4% | 10.6% | 10.7% | 10.7% | 10.7% | 10.9% | 10.9% | 10.5% | 11.0% |
| 45–65 | 44.7% | 44.8% | 45.0% | 45.5% | 45.9% | 46.3% | 46.0% | 45.6% | 45.7% |
| 66–85 | 44.8% | 44.6% | 44.3% | 43.8% | 43.4% | 42.8% | 43.1% | 44.0% | 43.3% |
| Women | 52.1% | 52.2% | 52.3% | 52.4% | 52.3% | 52.2% | 52.2% | 52.3% | 52.7% |
| Race/Ethnicity | |||||||||
| White | NA | NA | NA | NA | NA | NA | NA | 58.8% | 58.4% |
| Black or African American | NA | NA | NA | NA | NA | NA | NA | 10.6% | 10.8% |
| Hispanic or Latino | NA | NA | NA | NA | NA | NA | NA | 13.3% | 13.2% |
| Asian or Pacific Islander | NA | NA | NA | NA | NA | NA | NA | 16.1% | 16.5% |
| Multiracial | NA | NA | NA | NA | NA | NA | NA | 0.8% | 0.8% |
| American Indian or Alaskan Native | NA | NA | NA | NA | NA | NA | NA | 0.3% | 0.3% |
| Diabetes mellitus | 25.6% | 25.9% | 26.2% | 28.0% | 27.8% | 27.8% | 28.0% | 29.1% | 28.5% |
Hypertension control rates
Control rate was defined as meeting the NCQA HEDIS commercial hypertension control criteria, an externally reported standard that permits comparison of rates across reporting health plans.12 Using the same method, we also report on KPNC hypertension registry control rates during the study period. We also examined publicly available national and California state commercial NQCA HEDIS control rates.12 California data represented the mean control rate of commercial health insurance plans.
Statistical approach
Analyses were performed using SAS version 9.1 (Cary, NC). Data were reported as means with standard deviations or frequencies and proportions. Comparisons across study years were conducted using analysis of variance for continuous variables and chi-squared tests for categorical variables. Temporal trends for KPNC NCQA HEDIS hypertension control rates were assessed by the Cochran-Armitage test. For annual control rates measured on the KPNC hypertension registry, we accounted for the non-independence of proportions by treating as a time-series, fitting a log-linear regression of the proportion on time, allowing for autocorrelated errors. All p-values were two-sided.
RESULTS
Between 2001 and 2009, the KPNC hypertension registry increased from 349,937 (15.4% of adult membership) to 652,763 (27.5% of adult membership). Among hypertension registry members, mean age was 63 ± 14 years, and mean age remained stable throughout the study period with the majority of patients aged 45–85 years (Table 2). More than half of registry members were women and the proportion was similar across study years. Diabetes was common and increased from 25.6% in 2001 to 28.5% in 2009.
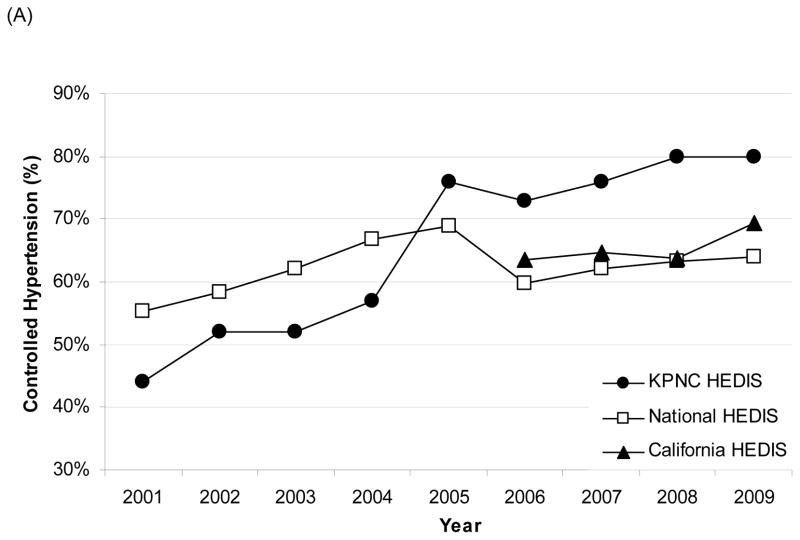
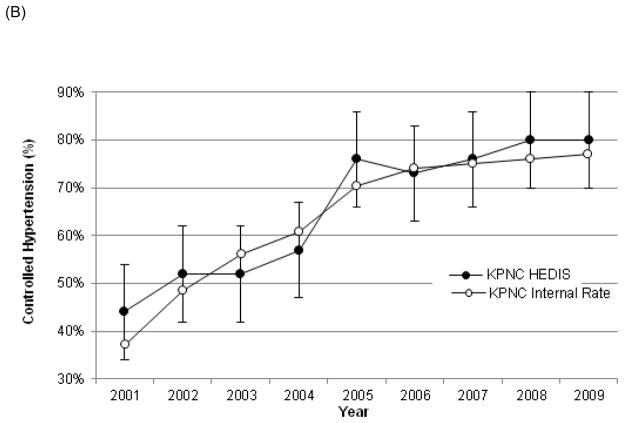
The NCQA HEDIS commercial hypertension control rate within KPNC increased after implementation of the hypertension program from 43.6% (95% confidence interval [CI] 39.4–48.6%) in 2001 to 80.4% (95% CI:75.6–84.4%) in 2009 (P<0.001 for trend) (Figure 1a). Control rates calculated using the NCQA HEDIS metric and internal hypertension registry control metric were similar (P<0.001 for trend) (Figure 1b). In contrast, the national mean NCQA HEDIS control rate increased from 55.4% to 64.1% between 2001 and 2009 (P=0.24 for trend). California-wide control rates were available since 2006 and were similar but slightly higher than the national average (63.4% versus 69.4% from 2006 to 2009 (P=0.37 for trend).
Figure 1.
(A) National Committee for Quality Assurance (NCQA) Healthcare Effectiveness Data and Information Set (HEDIS) hypertension control rates comparing Kaiser Permanente Northern California (KPNC), National, and California between 2001–2009; (B) KPNC NCQA HEDIS hypertension control rates versus KPNC internal hypertension registry control rates between 2001–2009. Confidence intervals for the KPNC NCQA HEDIS hypertension rates are indicated by the vertical bars on the graph. Confidence intervals for the KPNC internal hypertension registry control rates are not displayed as they are extremely small (<0.3%). See eTable 1 for complete details.
In addition, following the study period, the KPNC NCQA HEDIS hypertension control rate continued to improve from 83.7% in 2010 to 87.1% in 2011.
From 2001 to 2009, the rate of lisinopril-hydrochlorothiazide SPC prescriptions in KPNC increased from 13 to 23,144 prescriptions per month. During this period, the percentage of angiotensin-converting enzyme inhibitor prescriptions dispensed as a SPC (in combination with a thiazide diuretic) increased from < 1% to 27.2% (Figure 2).
Figure 2.
Percentage of ACEI prescriptions dispensed as single-pill combination ACEI-HCTZ combination tablets for Kaiser Permanente Northern California members between 2001–2009.
ACEI = Angiotensin Converting Enzyme Inhibitor; HCTZ = Hydrochlorothiazide
DISCUSSION
Control of hypertension remains elusive nationally despite widespread availability of effective therapies. Furthermore, limited data exist about the implementation and results of large, sustained hypertension programs. We describe a multi-factorial approach implemented in one of the largest, community-based hypertension programs nationally that was associated with a near doubling of hypertension control between 2001–2009. In contrast, only modest improvements in hypertension control were observed statewide and nationally.
Our study is observational in nature and several facets of the hypertension program may have contributed to the improved hypertension control within our population. Creation of a comprehensive hypertension registry facilitated customizable queries to access clinically important data-enabled prioritization of patient subgroups (e.g., poorly controlled hypertension) who were evaluated for appropriateness for treatment intensification. This is consistent with observations by Glynn et al. who reported that the most effective intervention to improve blood pressure control in primary care settings is an organized system of regular population review rather than primarily patient- or clinician-focused interventions.11
Regularly scheduled performance feedback delivered through quarterly and eventually monthly reports facilitated identification of high-performing medical centers where successful practices or innovations were identified and then disseminated program-wide. Although individual clinician feedback has long been used to promote change,14 we focused on clinic-level feedback to facilitate operational and system-level change.15
Health system-wide adoption, evaluation and distribution of an evidence-based practice guideline that had timely incorporation of new evidence facilitated the ability to introduce new treatment options and to re-emphasize existing evidence-based recommendations.4,15,16 For example, beta-blockers historically had an important role in hypertension management and were an important part of early KPNC practice guidelines. As new evidence became available, the role of beta-blockade in uncomplicated hypertension gradually diminished and KPNC practice guidelines were revised accordingly.
Systematic medical assistant follow-up visits were designed to optimize workflow for clinicians while leveraging the skills of ancillary staff. These visits allowed patients greater access to the medical team by eliminating co-payments, allowing greater scheduling flexibility, and involving shorter visit times, all of which reduced patient barriers.4,17
Use of lisinopril-hydrochlorothiazide SPC therapy was incorporated into KPNC practice guidelines in 2005, with subsequent rapid uptake system-wide. SPCs have important advantages including improved adherence,18,19 lower patient cost,19 and are associated with improved blood pressure control.15,20–22
It is not clear why in 2001 the KPNC NCQA HEDIS commercial control rate (43.6%) was lower than the national control rate (55.4%). Possible explanations include lower actual control rates or under-diagnosis of milder disease. Also, as patients without a recorded blood pressure during the measurement year are considered uncontrolled, it may be that the portion of patients without a recorded blood pressure decreased during the study period. The higher KPNC NCQA HEDIS control rates in 2005 relative to 2004 is likely due to variation in sampling, as NCQA HEDIS specifications stipulate a relatively small sample size (i.e., 305 to 411 patients) per measurement year with attendant lower precision and greater year-to-year variability. There was a smaller rise in the internal control rate in 2005 based on a much larger denominator (i.e., 234,852 to 353,156 patients)(Figure 1b). The decline in the mean national NCQA HEDIS control rate from 2005 to 2006 may be, in part, the result of the change in NCQA HEDIS reporting methodology for 2006. In 2006, NCQA changed the age of the HEDIS hypertension denominator from 46–85 to 18–85 years old, and changed the blood pressure control threshold from ≤140/90 to <140/90 mmHg. As the KPNC hypertension registry grew from 15.4% to 27.5% of the KPNC adult population during the study period, it is possible that the severity of hypertension within the registry decreased, although the prevalence was similar to that seen in NHANES (29.0%) in 2007–2008.1 Furthermore, during the same time period, the number of prescriptions per month for the most commonly used antihypertensive medications (i.e., thiazide diuretics, ACEI, angiotensin receptor blockers, beta-blockers, calcium channel blockers, and SPC ACEI-thiazide diuretics) increased in KPNC by 82%. Collectively, these data suggest that the apparent increase in hypertension reflects primarily improved detection and documentation of hypertension.
Comparison of demographic characteristics between subjects used to determine the KPNC NCQA HEDIS control rates and national or statewide NCQA HEDIS measures were not presented because demographic NCQA HEDIS data from other health plans were not publicly reported. Although survey data were available and reviewed from California (CHIS) and national (NHANES) sources, key methodological data acquisition differences precluded direct comparisons. KPNC data were collected for insured members using objective data documented in medical records. In contrast, NHANES and CHIS survey data were collected from volunteers with and without health insurance, which may influence the sociodemographic composition of respondents, and relied on self-report to identify the presence of diabetes (NHANES and CHIS) and diagnosed hypertension (CHIS) with attendant concerns about significant misclassification contributing to apparent variation in comorbidity prevalence. Census data from 2011 indicate that compared with the nation, California residents were slightly younger, more likely to be Hispanic and Asian, less likely to be white or black but had similar gender distribution.23 However, these differences are unlikely to explain the large differences between KPNC control rates compared with California and national rates, as both the state and national average NCQA HEDIS control rates were similar and the KPNC population is highly representative of the statewide population, except for slightly lower representation at the extremes of age and income.24,25
Comparisons of KPNC control rates to NHANES are also limited due to differences in the definition of controlled hypertension. KPNC rates were determined based on the standard NCQA HEDIS protocol using the most recent recorded outpatient blood pressure, which was the lowest recorded measurement on the day of examination, usually measured by a trained medical assistant using an automated sphygmomanometer. NHANES defined hypertension control based on blood pressure data measured by clinicians using mercury sphygmomanometers at a mobile examination center (using the mean of up to three blood pressure measurements during a single examination). Comparison of KPNC control rates to CHIS-derived California control rates is not possible as hypertension control was not a component of the CHIS survey.26 Finally, while patients with end-stage renal disease were excluded from the KPNC hypertension registry and control denominator in accordance with the NCQA HEDIS methodology, they comprised only 0.37% of the KPNC population so the impact on overall hypertension control measures would be minimal.
In this observational study of a multi-faceted intervention program, we cannot determine the degree to which individual components contributed to improved hypertension control or the role of other unidentified factors. Using the NCQA HEDIS commercial methodology facilitated comparisons against national and state estimates, but given this approach relies on data from only a small subset of the overall hypertensive population, variations in year-to-year control estimates could be due to fluctuations in random sampling. The NCQA HEDIS commercial control rate is used nationally to compare hypertension control across health care organizations, so we cannot directly compare control rates from our larger internal hypertension registry to those of other health care delivery systems. However, our internal hypertension registry control rates were very similar to our externally reported NCQA HEDIS commercial control rates, with the rates increasing similarly over time (Figure 1b). Our study extends reports from other large health care delivery systems have also observed significant improvement in hypertension control. For example, the Veterans Affairs health care system reported hypertension control rate improvement from 75% to 77% between 2006 and 2009.27–29
In sum, implementation of a large-scale hypertension program was associated with improvements in hypertension control rates between 2001 and 2009. Key elements of the program include establishment of a comprehensive hypertension registry, development and sharing of performance metrics, evidence-based guidelines, medical assistant visits for blood pressure measurement, and SPC pharmacotherapy.
Supplementary Material
Acknowledgments
Funding/Support: Hypertension control data and program implementation was under the clinical patient care domain of Kaiser Permanente Northern California. No funding was used for the acquisition of data, statistical analysis, or the preparation of the manuscript. This work was supported, in part, by funding from the National Heart Lung and Blood Institute (NHLBI) through the Cardiovascular Research Network (U19 HL91179-01, Dr. Go).
Role of the Sponsor: The funding organizations had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; or preparation, review, or approval of the manuscript.
APPENDIX
Annual hypertension control rates within different patient samples in KPNC between 2001–2009
eTable 1 below shows the yearly rate of hypertension control comparing data from an internal health plan-wide hypertension registry as compared with the NCQA HEDIS commercial sampling methodology.
KPNC Diabetes Registry Inclusion Criteria
The presence of diabetes mellitus was determined using a regional diabetes registry modeled after an approach described previously (see manuscript), which included members meeting any of the following criteria in the prior 24 months: ≥2 ambulatory diabetes-related diagnoses, ≥2 hospital discharge diagnoses, ≥2 emergency department diagnoses, or receiving anti-diabetic medications. Diabetes-related diagnoses were based on International Classification of Diseases, Ninth Edition (ICD-9) codes 250.x. Members were excluded from the diabetes registry if they had gestational diabetes, polycystic ovary syndrome, steroid-induced diabetes, were identified only based on isolated metformin use, were enrolled in a hospice program, or had end-stage renal disease.
Description of the Hypertension Control Program
The KPNC Hypertension Control Program consists of 5 key elements: a patient registry, an evidence based guideline, quality performance metrics with dissemination of successful practices, medical assistant blood pressure measurement, and single pill combination therapy.
Hypertension Patient Registry
A registry was created by identifying hypertensive individuals using outpatient diagnostic codes, pharmacy data and hospitalization records from health plan databases. This process was automated and initially the registry was updated quarterly. The accuracy of the registry inclusion criteria was validated through chart review audits of random samples of registry members. The inclusion criteria were selected to replicate the specifications utilized by NQCA HEDIS. Patients were included in the registry if they met one of the following criteria: (1) ≥2 hypertension diagnoses coded in primary care visits in the past 2 years, (2) ≥1 primary care hypertension diagnosis and ≥1 hospitalization with a primary or secondary hypertension diagnosis in the past 2 years, (3) ≥1 primary care hypertension diagnosis and ≥1 filled prescriptions for hypertension medication within the last 6 months, or (4) ≥1 primary care hypertension diagnosis plus ≥1 stroke-related hospitalizations or a history of coronary heart disease, heart failure or diabetes mellitus.
Quality Performance Metrics
Quality reports containing clinical information describing blood pressure control for all subjects in the hypertension registry was initially distributed quarterly. Hypertension control was defined similarly to the NCQA HEDIS specifications previously described in the manuscript. KPNC BP results were not readily available in an electronic format in 2001. From 2001 to 2005, before the implementation of an electronic health record in KPNC, clinic BP range measurements were recorded by clinicians in one of 6 systolic and one of 6 diastolic ranges according to JNC6 and JNC7 recommendations. Completed paper forms were forwarded to a central processing center where they were scanned, and data was collected. This BP range data was analyzed and utilized in quality improvement activities. From 2005 to 2008, KPNC transitioned from paper based health documentation to an EHR and during this period actual KPNC BP results became increasingly available. After full implementation of an EHR in 2008 actual BP results were collected for all medical centers in KPNC and used for quality improvement activities. In addition to BP results, the hypertension performance report also obtained relevant clinical information (demographics, medications, laboratory results, relevant co-morbidities, clinical encounter history, etc.). Access to the registry was granted to medical center managers who used the data to generate work plans for quality improvement processes. The original version of the registry was updated and generated every 3 months and then distributed to the medical center directors shortly after it was updated. Eventually the registry migrated to a dynamic database with information that was updated every 2 weeks and available by query at any time to authorized individuals.
A central management team reviewed the quality performance of the medical centers every 1 to 3 months. Medical centers with superior performance on the quality metrics were identified and extensively evaluated. The central management team reviewed data related to practice patterns including staffing support, medication prescription patterns, encounter rates, and other metrics. The central management team conducted site visits and interviews with medical directors of high performing programs. Successful practices were then disseminated to all medical center directors using training sessions twice yearly and with periodic email communications.
Evidence Based Hypertension Guideline
A hypertension guideline based on current clinical evidence was created and continually updated every 2 years. The guideline development team consisted of a central core team of primary care and specialty physicians as well as pharmacists and evidence based methodologists. The evidence review was performed by searching the literature for relevant publications (usually large randomized clinical trials, systematic evidence reviews, or published evidence based guidelines). After the review was complete, the recommendations were distributed to the stakeholder groups (for example departmental chiefs of Internal Medicine, Cardiology, Nephrology, and others) for comment then eventual endorsement. After completion, the guidelines were distributed to all clinicians. Vehicles for dissemination of guideline information included distribution of printed guideline documents, email updates, creation of physician tools (e.g., laminated pocket cards), regional televised videoconferences, local didactic teaching sessions, partnering with the pharmacy clinical operation managers, and use of the electronic health record to optimize medication drug selection. Protocols for nurse and pharmacist care managers were modified to reflect the guideline recommendations.
Medical assistant blood pressure measurement
In 2007, all KPNC medical centers developed an alternative type of follow-up visit whereby blood pressure was measured outside of traditional clinician office visits. Visits were usually scheduled two to four weeks after a blood pressure medication adjustment. Patients were not charged a co-payment for these visits. Typically, a medical assistant measured blood pressure and informed the primary care physician, who then directed treatment intensification and follow up care. Medical assistants were trained using standardized materials and blood pressure competency assessments.
Promotion of single-pill combination (SPC) therapy
In 2005, SPC therapy with lisinopril-hydrochlorothiazide was incorporated into the regional clinical practice guideline. This SPC therapy was recommended in the hypertension guideline as an option for initial antihypertensive pharmacological treatment and recommended when 2 antihypertensive medications were required. SPC therapy with lisinopril-hydrochlorothiazide was promoted by developing patient education materials as well as physician education such as email communications, printed materials, pocket card clinician tools, and highlighting SPC therapy in the practice improvement regional meetings.
Footnotes
Financial Disclosures: None
Author Contributions: Dr. Jaffe had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: Jaffe, Lee, Young, Go
Acquisition of data: Jaffe, Lee, Young
Analysis and interpretation of data: Jaffe, Lee, Young, Sidney, Go
Drafting of the manuscript: Jaffe, Lee
Critical revision of the manuscript for important intellectual content: Jaffe, Lee, Young, Sidney, Go
Statistical analysis: Lee, Sidney
Obtained funding: None.
Administrative, technical, or material support: Sidney
Study supervision: None
Additional Contributions: We thank Joan C. Lo, MD (Kaiser Northern California Permanente Division of Research, Oakland, California) for help with the initial design of this article; Laura J. Ransom, MS and Joyce Arango, MPH, DPH (Kaiser Permanente Northern California Department of Quality and Operation Support, Oakland, California) for regional project management and implementation support for the cardiovascular programs; Dawn Rezente, MBA, and Don Fordham, MPH (Kaiser Permanente Northern California Department of Quality and Operation Support, Oakland, California) for help with quality data acquisition and verification, Jocelyn Chan, Pharm D (Northern California Kaiser Foundation Health Plan, Oakland, California) for acquisition of pharmacy data; and Michael Sorel, MPH and Charles Quesenberry, PhD (Kaiser Permanente Northern California Division of Research, Oakland, California) for help with biostatistical support. These contributors were not compensated for their assistance.
References
- 1.Egan BM, Zhao Y, Axon RN. US trends in prevalence, awareness, treatment, and control of hypertension, 1988–2008. Jama. 2010 May 26;303(20):2043–2050. doi: 10.1001/jama.2010.650. [DOI] [PubMed] [Google Scholar]
- 2.Ezzati M, Lopez AD, Rodgers A, Vander Hoorn S, Murray CJ. Selected major risk factors and global and regional burden of disease. Lancet. 2002 Nov 2;360(9343):1347–1360. doi: 10.1016/S0140-6736(02)11403-6. [DOI] [PubMed] [Google Scholar]
- 3.The Seventh Report of the Joint National Committee on Prevention. Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 Report-Correction. Jama. 2003 Jul 9;290(2):197. doi: 10.1001/jama.289.19.2560. [DOI] [PubMed] [Google Scholar]
- 4.Handler J, Lackland DT. Translation of hypertension treatment guidelines into practice: a review of implementation. J Am Soc Hypertens. 2011 Jul-Aug;5(4):197–207. doi: 10.1016/j.jash.2011.03.002. [DOI] [PubMed] [Google Scholar]
- 5.Walsh JM, Sundaram V, McDonald K, Owens DK, Goldstein MK. Implementing effective hypertension quality improvement strategies: barriers and potential solutions. J Clin Hypertens (Greenwich) 2008 Apr;10(4):311–316. doi: 10.1111/j.1751-7176.2008.07425.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Green BB, Cook AJ, Ralston JD, et al. Effectiveness of home blood pressure monitoring, Web communication, and pharmacist care on hypertension control: a randomized controlled trial. Jama. 2008 Jun 25;299(24):2857–2867. doi: 10.1001/jama.299.24.2857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Luders S, Schrader J, Schmieder RE, Smolka W, Wegscheider K, Bestehorn K. Improvement of hypertension management by structured physician education and feedback system: cluster randomized trial. Eur J Cardiovasc Prev Rehabil. 2010 Jun;17(3):271–279. doi: 10.1097/HJR.0b013e328330be62. [DOI] [PubMed] [Google Scholar]
- 8.Choma NN, Huang RL, Dittus RS, Burnham KE, Roumie CL. Quality improvement initiatives improve hypertension care among veterans. Circ Cardiovasc Qual Outcomes. 2009 Jul;2(4):392–398. doi: 10.1161/CIRCOUTCOMES.109.862714. [DOI] [PubMed] [Google Scholar]
- 9.Casey PE, Compton-Phillips A, Shapiro S, Nguyen P. Controlling high blood pressure. Perm J. 2006 Summer;10(2):13–16. doi: 10.7812/tpp/05-144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Aucott JN, Pelecanos E, Dombrowski R, Fuehrer SM, Laich J, Aron DC. Implementation of local guidelines for cost-effective management of hypertension. A trial of the firm system. J Gen Intern Med. 1996 Mar;11(3):139–146. doi: 10.1007/BF02600265. [DOI] [PubMed] [Google Scholar]
- 11.Glynn LG, Murphy AW, Smith SM, Schroeder K, Fahey T. Interventions used to improve control of blood pressure in patients with hypertension. Cochrane Database Syst Rev. 2010;(3):CD005182. doi: 10.1002/14651858.CD005182.pub4. [DOI] [PubMed]
- 12.Ad N, Suri RM, Gammie JS, Sheng S, O’Brien SM, Henry L. Surgical ablation of atrial fibrillation trends and outcomes in North America. J Thorac Cardiovasc Surg. 2012 Nov;144(5):1051–1060. doi: 10.1016/j.jtcvs.2012.07.065. [DOI] [PubMed] [Google Scholar]
- 13.Selby JV, Ray GT, Zhang D, Colby CJ. Excess costs of medical care for patients with diabetes in a managed care population. Diabetes Care. 1997;20(9):1396–1402. doi: 10.2337/diacare.20.9.1396. [DOI] [PubMed] [Google Scholar]
- 14.Teleki SS, Shaw R, Damberg CL, McGlynn EA. Providing Performance Feedback to Individual Physicians: Current Practice and Emerging Lessons--Final Report (WR-381- CHCF) RAND Corporation; 2006. [Google Scholar]
- 15.Grol R, Grimshaw J. From best evidence to best practice: effective implementation of change in patients’ care. Lancet. 2003 Oct 11;362(9391):1225–1230. doi: 10.1016/S0140-6736(03)14546-1. [DOI] [PubMed] [Google Scholar]
- 16.Carter BL, Rogers M, Daly J, Zheng S, James PA. The potency of team-based care interventions for hypertension: a meta-analysis. Arch Intern Med. 2009 Oct 26;169(19):1748–1755. doi: 10.1001/archinternmed.2009.316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Siegel D. Barriers to and strategies for effective blood pressure control. Vasc Health Risk Manag. 2005;1(1):9–14. doi: 10.2147/vhrm.1.1.9.58940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gradman AH, Basile JN, Carter BL, et al. Combination therapy in hypertension. J Am Soc Hypertens. 2010 Mar-Apr;4(2):90–98. doi: 10.1016/j.jash.2010.03.001. [DOI] [PubMed] [Google Scholar]
- 19.Sherrill B, Halpern M, Khan S, Zhang J, Panjabi S. Single-pill vs free-equivalent combination therapies for hypertension: a meta-analysis of health care costs and adherence. J Clin Hypertens (Greenwich) 2011 Dec;13(12):898–909. doi: 10.1111/j.1751-7176.2011.00550.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Epstein M, Bakris G. Newer approaches to antihypertensive therapy. Use of fixed-dose combination therapy. Arch Intern Med. 1996 Sep 23;156(17):1969–1978. [PubMed] [Google Scholar]
- 21.Neutel JM. Prescribing patterns in hypertension: the emerging role of fixed-dose combinations for attaining BP goals in hypertensive patients. Curr Med Res Opin. 2008 Aug;24(8):2389–2401. doi: 10.1185/03007990802262457. [DOI] [PubMed] [Google Scholar]
- 22.Weir MR, Bakris GL. Combination therapy with Renin-Angiotensin-aldosterone receptor blockers for hypertension: how far have we come? J Clin Hypertens (Greenwich) 2008 Feb;10(2):146–152. doi: 10.1111/j.1751-7176.2008.07439.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.United States Census Bureau. [Accessed March 11, 2013]; http://quickfacts.census.gov/qfd/
- 24.Krieger N. Overcoming the absence of socioeconomic data in medical records: validation and application of a census-based methodology. Am J Public Health. 1992 May;82(5):703–710. doi: 10.2105/ajph.82.5.703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gordon NP. Similarity of the Adult Kaiser Permanente Membership in Northern California to the Insured and General Population in Northern California: Statistics from the 2009 California Health Interview Survey. Oakland: Kaiser Permanente Northern California; Jan 24, 2012. [Google Scholar]
- 26.California Health Interview Survey. [Accessed March 11, 2013]; http://healthpolicy.ucla.edu/chis/design/Pages/questionnaires.aspx.
- 27.2009 VHA Facility Quality and Safety Report. Department of Veterans Affairs, Veterans Health Administration, Office of Quality and Safety; Oct, 2009. http://www.va.gov/health/docs/HospitalReportCard2009.pdf. [Google Scholar]
- 28.Report to the Appropriations Committee of the US House of Representatives in response to House Appropriations Report No. 110-186, accompanying Public Law 110-161, The Consolidated Appropriations Act. Department of Veterans Affairs, Veterans Health Administration; 2008. http://www.va.gov/health/docs/Hospital_Quality_Report.pdf. [Google Scholar]
- 29.2010 VHA Facility Quality and Safety Report. Department of Veterans Affairs, Veterans Health Administration; 2010. http://www.va.gov/health/docs/HospitalReportCard2010.pdf. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.