Abstract
Background and Purpose
The common carotid artery (CCA) inter-adventitial diameter (IAD) is measured on ultrasound images as the distance between the media-adventitia interfaces of the near and far walls. It is associated with common carotid intima-media thickness (IMT) and left ventricular mass and might therefore also have an association with incident stroke.
Methods
We studied 6255 individuals free of coronary heart disease and stroke at baseline with mean age of 62.2 years (47.3% men), members of a multi-ethnic community based cohort of whites, blacks, Hispanics, and Chinese. Ischemic stroke events were centrally adjudicated. CCA IAD and IMT were measured. Cases with incident atrial fibrillation (n = 385) were excluded. Multivariable Cox proportional hazards models were generated with time to ischemic event as outcome, adjusting for risk factors.
Results
There were 115 first time ischemic strokes at 7.8 years of follow-up. CCA IAD was a significant predictor of ischemic stroke (Hazard ratio: 1.86; 95%CI 1.59, 2.17 per mm) and remained so after adjustment for risk factors and common carotid IMT with a hazard ratio of 1.52 per mm (95% CI: 1.22, 1.88). Common carotid IMT was not an independent predictor after adjustment (hazard ratio 0.14; 95% CI: 0.14, 1.19).
Conclusion
While common carotid IMT is not associated with stroke, inter-adventitial diameter of the common carotid artery is independently associated with first time incident ischemic stroke even after adjusting for IMT. Our hypothesis that this is in part due to the effects of exposure to blood pressure needs confirmation by other studies.
Introduction
Carotid artery diameter can increase when blood pressure elevations passively distend the artery or through an adaptive mechanism that causes artery dilation when arterial wall thickness increases1–3. Carotid artery inter-adventitial diameter (IAD) is measured on ultrasound images as the distance between the media adventitia interfaces of the artery near and far walls. IAD is associated with cardiovascular risk factors, left ventricular mass, and intima-media thickness (IMT) of the common carotid artery4.
Studies have shown an association between IAD and myocardial infarction5, 6. A recent study has indicated that IAD might also be associated with stroke7 in a patient group with a high overall cardiovascular risk burden.
We investigate the possible associations between inter-adventitial diameter and incident stroke in a longitudinally followed cohort free of cardiovascular disease and stroke at baseline. The Multi-Ethnic Study of Atherosclerosis (MESA) is a cohort of individuals aged 45 to 84 years and composed of four ethnicities: non-Hispanic Whites, Chinese, African-Americans, and Hispanics.
Methods
Population
MESA (Multi-Ethnic Study of Atherosclerosis) is a longitudinally followed cohort consisting of 6814 men and women aged 45–84 with no history of clinical cardiovascular disease enrolled between July 2000 and August 2002. The MESA cohort is multi-ethnic and includes Caucasian-white, Chinese, African-American, and Hispanic participants. Participants were excluded if they had physician diagnosis of heart attack, stroke, transient ischemic attack, heart failure, angina, atrial fibrillation or history of any cardiovascular procedure8. Participants with weight above 300 pounds (lbs), pregnancy, or any medical conditions that would prevent long-term participation were excluded. MESA protocols and all studies described herein have been approved by the Institutional Review Boards of all collaborating institutions and all participants gave informed consent. The participants studied underwent carotid artery imaging at the baseline visit (visit 1).
Follow-up was ascertained at intervals of 9–12 months by telephone interview to inquire about all interim hospital admissions, cardiovascular outpatient diagnoses and procedures, and deaths. Additional medical encounters through cohort clinic visits, participant call-ins, medical record abstractions or obituaries were recorded when possible. Copies of death certificates and medical records for all hospitalizations and selected outpatient cardiovascular diagnoses and procedures were obtained and reviewed.
Risk factors and anthropomorphic variables
Age, sex, race/ethnicity, and medical history were self-reported. Use of lipid-lowering and anti-hypertensive medications was recorded. Current smoking was defined as self-report of one or more cigarettes in the last 30 days. Resting blood pressures (BP) were measured in the seated position using a Dinamap model Pro 100 automated oscillometric sphygmomanometer (Critikon, Tampa, Florida).
Glucose and lipids were measured after a twelve-hour fast. Serum glucose was measured by rate reflectance spectrophotometry on the Vitros analyzer (Johnson & Johnson Clinical Diagnostics, Inc., Rochester, NY). The presence of diabetes mellitus was based on self-reported physician diagnosis, use of insulin and/or oral hypoglycemic agent, or a fasting glucose value ≥126 mg/dL9. Total cholesterol was measured using a cholesterol oxidase method (Roche Diagnostics), as was HDL after precipitation of non-HDL cholesterol with magnesium/dextran.
Carotid artery measures
For inter-adventitial diameter measurements, participants were examined supine with the head rotated 45° towards the left side. Imaging was done with the ultrasound transducer parallel to the long axis of the neck with the jugular vein lying immediately above the common carotid artery (or at 45 degrees from the vertical if the internal jugular vein is not visualized). Images of the right common carotid artery were centered 10 to 15 mm below (caudad to) the right common carotid artery bulb. End-diastolic images (smallest diameter of the artery) were captured4. Measurements were made with an edge-detector that identified the media-adventitia interfaces of the near and far walls. A diameter versus time curve was generated. An algorithm identified peak-systolic and end-diastolic fiduciary points. A reader reviewed these curves confirming valid end-diastolic values. The final IAD measurement was based on an average of seven end-diastolic diameter measurements. The reproducibility of the IAD was assessed by blinded readings of a separate series of images acquired on the same 89 participants on the same day giving a correlation coefficient of 0.93.
Intima-media thickness (IMT) measurements were made of the common carotid artery near and far wall over a distance of approximately 10 mm below the common carotid artery bulb. These tracings were then used to calculate maximum near and far wall IMT that was then averaged for the 4 locations.
Outcomes
All cardiovascular events were adjudicated and classified by two members of the mortality and morbidity review committee. Neurologists on the committee adjudicated the presence of strokes with all discordant cases requiring discussion to reach consensus.
Presence of incident atrial fibrillation during the follow-up period was determined by hospital review of hospital charts and the presence of ICD-9 diagnosis of atrial fibrillation or flutter (427.3; 427.31; 427.32) in 231 individuals and by self-report only in 154 for a total of 385 individuals. These individuals were excluded from the analysis. An additional 174 individuals did not have IAD measurements either because they did not have a carotid artery examination or the measurements were not obtainable. The final cohort included 6255 participants.
Incident stroke was defined as rapid onset of a documented focal neurologic deficit lasting 24 hours or until death, or if in less than 24 hours there was a clinically relevant lesion on brain imaging. Patients with focal neurologic deficits secondary to brain trauma, tumor, infection, or other non-vascular cause were excluded. Strokes were classified on the basis of neuroimaging or other tests. We studied ischemic stroke (n=115) censoring participants at the time of a stroke if they had experienced a hemorrhagic stroke (n = 22).
Statistical analyses
The mean (and standard deviation) values of continuous variables and the count (and percent) of categorical variables are shown. Cox proportional hazards models were fit with time to stroke as the outcome variable, adjusted initially for age, sex, race/ethnicity, then additionally for HDL cholesterol, total cholesterol, lipid-lowering medications, systolic blood pressure, anti-hypertensive medications use, diabetes status, current cigarette status, and common carotid IMT. Harrell’s C-statistics were obtained for the Cox proportional hazards models. The predictive value of common carotid artery inter-adventitial diameter was compared to the baseline model using the differences in Harrell’s C-statistic.
The relative hazard rates for quartiles of inter-adventitial diameter were estimated for descriptive purposes and Kaplan-Meier failure curves generated for quartiles of inter-adventitial diameter. We also generated Kaplan-Meir failure curves for quartiles of IMT.
P-values< 0.05 are assumed to be statistically significant. Statistical tests and associated p-values are two-sided and are performed using STATA 11.2 software (StataCorp, College Station, Texas).
Results
Average age of our population of 6255 individuals was 62.2 years and with an average follow-up of 7.8 years. Key demographics and risk factors are shown in Table 1. Men constituted 47.3% of the population. The prevalence of diabetes was 12.7% and that of current smoking 13.0%. Anti-hypertensive agents were being taken by 37.1% of the cohort whereas lipid lowering therapy was noted in 16.2%. Average inter-adventitial diameter of the common carotid artery was7.57 mm (± 0.92 mm). There were 115 adjudicated ischemic strokes.
Table 1.
Population demographics and risk factors for the population studied (n = 6255).
| Variable | Value* |
|---|---|
| Age (years) | 62.2 ± 10.2 |
| Sex(men) | 47.3% (2958) |
| Ethnicity | |
| White | 38.4% (2405) |
| Chinese | 12.1% (754) |
| Black | 27.3% (1705) |
| Hispanic | 22.2% (1391) |
| HDL cholesterol (mg/dl) | 50.9 ± 14.7 |
| Total cholesterol (mg/dl) | 194.1 ± 35.8 |
| Lipid lowering medication use (yes) | 16.2% (1016) |
| Systolic pressure (mmHg) | 126.5 ± 21.5 |
| Hypertension medication use (yes) | 37.1% (2320) |
| Diabetes (yes) | 12.7% (794) |
| Current Smoker (yes) | 13.0% (811) |
| Common carotid artery | |
| Inter-adventitial diameter (mm) | 7.57 ± 0.92 |
| Intima-media thickness (mm) | 0.87 ± 0.19 |
mean ± standard deviation for continuous variables and % values (numerical values) for categorical variables.
In Cox proportional hazards models, the hazard ratio for ischemic stroke was 1.86 (95% CI: 1.59, 2.17) for each mm increase in IAD. This was attenuated to 1.67 (95% CI: 1.38, 2.02) after adjustment for age, sex and race/ethnicity. Further adjustment for risk factors (Table 2) gave a hazard ratio of 1.52 (95% CI: 1.22, 1.88). Strong associations were seen between stroke and age, HDL cholesterol, total cholesterol, systolic blood pressure, and diabetes. Participants with Chinese ethnicity had a lower stroke incidence rate than whites. Common carotid IMT was not a significant predictor of ischemic stroke. The addition of carotid artery diameter did not significantly increase the C-statistic (0.0144; 95% CI −0.0017, 0.0305; p = 0.08) when added to the multivariable Cox proportional hazards model that included IMT (0.783; 95% CI 0.748, 0.819).
Table 2.
Results of multivariable Cox proportional Hazards model with time to ischemic stroke as outcome.
| Variable | Hazard ratio |
p-value | Hazard Ratio Lower 95% CI |
Hazard Ratio Upper 95% CI |
|---|---|---|---|---|
| Age (years) | 1.05 | < 0.001 | 1.03 | 1.08 |
| Sex(men) | 0.96 | 0.86 | 0.63 | 1.47 |
| Ethnicity | ||||
| White (referent) | ||||
| Chinese | 0.28 | 0.007 | 0.11 | 0.71 |
| Black | 0.82 | 0.41 | 0.51 | 1.31 |
| Hispanic | 0.96 | 0.86 | 0.60 | 1.54 |
| HDL Cholesterol (mg/dl) | 0.98 | 0.012 | 0.96 | 1.00 |
| Total Cholesterol (mg/dl) | 1.01 | 0.005 | 1.00 | 1.01 |
| Lipid lowering treatment | 1.23 | 0.37 | 0.78 | 1.94 |
| Systolic pressure (mmHg) | 1.02 | < 0.001 | 1.01 | 1.03 |
| Blood pressure lowering | ||||
| treatment | 1.28 | 0.23 | 0.86 | 1.93 |
| Diabetes | 1.78 | 0.011 | 1.14 | 2.77 |
| Smoker | 1.59 | 0.09 | 0.93 | 2.71 |
| Common carotid artery | ||||
| Inter-adventitial diameter (mm) | 1.52 | < 0.001 | 1.22 | 1.88 |
| Intima-media thickness (mm) | 0.41 | 0.10 | 0.14 | 1.19 |
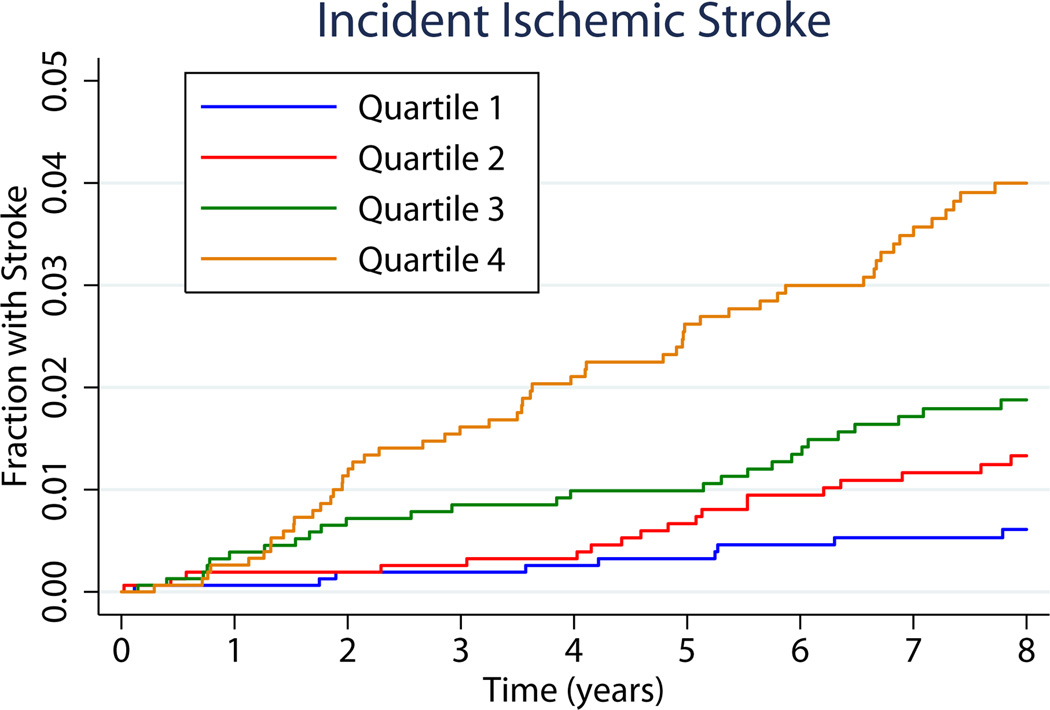
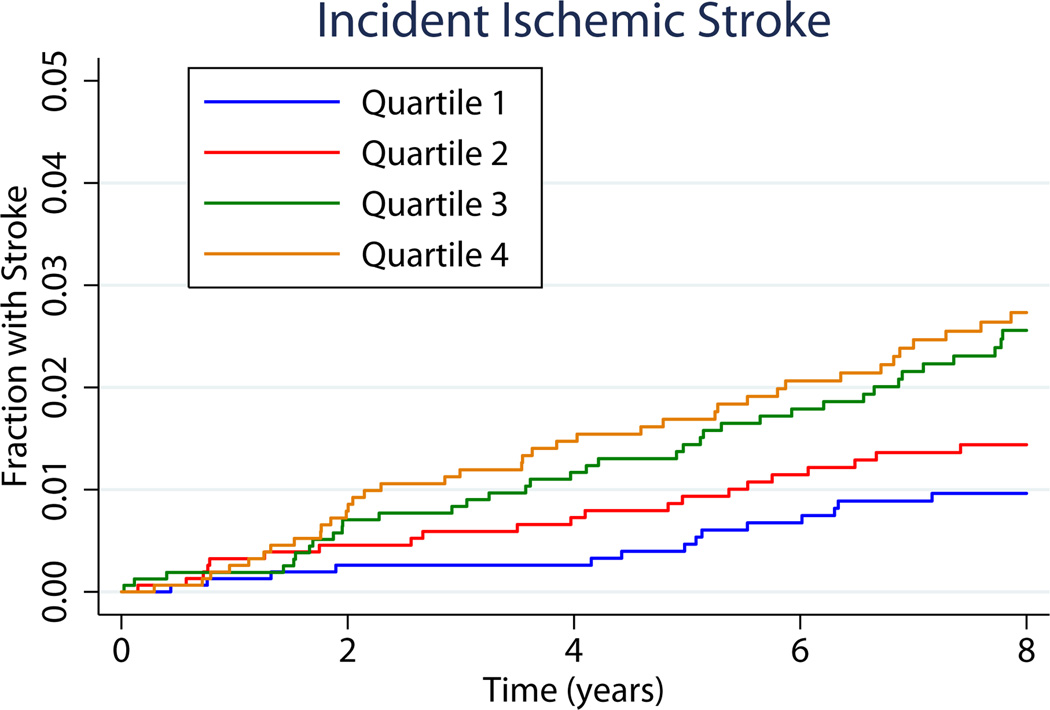
Kaplan-Meier failure curves for quartiles of IAD are shown in figure 1a. The cumulative risks of ischemic stroke at 8 years by quartiles were 0.63% (3.97 to 6.92 mm), 1.21% (6.93 to 7.48 mm), 1.80% (7.49 to 8.12 mm) and 3.75% (8.13 to 13.2 mm) for the respective quartiles of IAD. For illustrative purposes we also generated these curves for quartiles of IMT (Figure 1b). The association between IMT and stroke appears weaker than for IAD.
Figure 1.
a. Kaplan-Meier curves for incident ischemic stroke by quartiles of increasing common carotid artery inter-adventitial diameter (IAD) without adjustment for risk factors. Quartile ranges were 3.97 to 6.92 mm, 6.93 to 7.43 mm, 7.49 to 8.12 mm and greater than 8.13 mm. Level of significance was p < 0.0001 for Log-Rank of 52.1.
b. Kaplan-Meier curves for incident ischemic stroke by quartiles of increasing common carotid artery intima-media thickness (IMT) without adjustment for risk factors. Quartile ranges were 0.4 to 0.735 mm, 0.735 to 0.843 mm, 0.845 mm to 0.975 mm and greater than 0.975 mm. Level of significance was p = 0.0004 for Log-Rank of 18.0.
Discussion
We have found that the inter-adventitial diameter of the common carotid artery is a significant independent predictor of ischemic stroke after taking into consideration traditional (Framingham) cardiovascular risk factors. This association persisted after adjustment for common carotid artery IMT.
In this study, we have, replicated the findings of a prior report from the IMPROVE study showing an association between stroke and common carotid inter-adventitial diameter7. We have done so in a North American multi-ethnic cohort selected without cardiovascular disease at baseline whereas the prior report investigated the value of this measurement in a European population that was pre-selected to have a high burden of risk factors and subclinical cardiovascular disease7. Our findings are slightly discordant with those of Baldassarre et al since we do not find a positive association between common carotid IMT and incident stroke7. It is difficult to speculate on the reasons for this apparent discordance. One factor to take into consideration is the possibility that IMT is a better predictor of events in individuals with large burdens of subclinical cardiovascular disease than those with a lower burden. The other is that internal carotid artery IMT might be a better predictor of stroke than common carotid IMT. The IMPROVE trial pre-selected slightly more than 3000 individuals after screening 21,000 individuals7. MESA participants were selected by a random sampling of the population with the exclusion of individuals with baseline cardiovascular disease. Enrollees in IMPROVE had an average Framingham risks score of 22%7 whereas our cohort had an average of 11%. Another difference between our study and IMPROVE is the imaging protocol. IMPROVE performed a comprehensive, multi-angle sampling of the common carotid IMT and measured at two levels in the common carotid artery7. The measurement more closely resembling our IMT measurement is the one showing weaker association with stroke. In MESA, the IMT was measured on one projection and just below the beginning of the carotid bulb. As such, MESA measurements might be weighted towards medial hypertrophy of the wall whereas IMPROVE might be more representative of atherosclerotic changes. In addition, only 38% of our population was Caucasian white.
We did not find a significant association between IMT and incident stroke in our adjusted models whereas the unadjusted Kaplan-Meier survival curves did show a positive trend for IMT quantiles (Figure 1b). While the association between IMT and inter-adventitial diameter4 explains part of the loss of statistical power through confounding when they are included in the same model, this also suggests that inter-adventitial diameter is a stronger predictor of ischemic stroke than IMT. A similar lack of association between incident stroke has been suggested in the Tromso study, specifically in multi-variable adjusted models10. Our data confirm their observations although their event-rates and observation period were greater than ours10.
We used inter-adventitial diameter for two principal reasons. The first was the semi-automatic method of measurement4. An edge-detector was used to track the displacement of the near wall and the far wall intima-media interfaces. Performance of the edge detector was robust since the final diameter measurement was based on an average of seven cardiac cycles for the application of the edge detector to a 20-second long sequence of images. We also selected the inter-adventitial diameter based on observations linking increases in diameter to changes in IMT. The Glagov phenomenon holds that the artery lumen diameter will tend to be maintained in the presence of plaque build-up11. We have previously shown that this phenomenon also occurs in the common carotid artery12. In summary the outer diameter of the artery increases in response to increases in IMT but not the lumen diameter12. As such, IAD or adventitia-to adventitia diameter measurements might be more robust predictors of events than the lumen diameter.
Our previous work has shown a strong association between inter-adventitial diameter, cardiovascular risk, IMT, and left ventricular mass4. We therefore adjusted our multivariable model for all of these risk factors. We performed a sensitivity analysis to confirm that inter-adventitial diameter was an independent predictor of ischemic stroke after adjusting for left ventricular mass (data not shown). Inter-adventitial diameter remained significant with a hazard ratio of 1.58 (p = 0.001). We also performed additional analyses using all strokes as outcomes as well as included individuals with atrial fibrillation. Inter-adventitial diameter remained an independent predictor in all cases (data not shown).
We hypothesize that the association between stroke and inter-adventitial diameter is in part a reflection of the effects of chronic blood pressure elevations. We investigated this possibility by removing systolic blood pressure from the model and noted a significant increase in the inter-adventitial diameter hazard ratio to 1.7 suggesting that there is confounding or mediation between inter-adventitial diameter and systolic pressure.
Limitations of our study include the difference in IMT imaging protocol reported in IMPROVE. However, our protocol resembles the protocol adopted for the Framingham Heart Study13. We have a small number of exclusions that might have biased the analysis to a healthier subset of our cohort. However, we had complete data on 6255/6814 or 92% of our cohort. We also studied a population without prevalent cardiovascular disease at baseline therefore limiting our ability to determine if prevalent coronary heart disease or peripheral arterial disease might serve as risk factors for stroke. Our study might also be limited by the number of outcomes since the difference in C-statistic between the models without and with common carotid artery diameter was not statistically significant (p = 0.08).
We conclude that the inter-adventitial diameter of the common carotid artery is an independent predictor of ischemic stroke. The pathological source of this association is not clear but is likely in part mediated by the effects of blood pressure elevation. Further research is needed to confirm this hypothesis.
Acknowledgements
The authors would like to thank the investigators, the staff, and the participants of the Multi-Ethnic Study of Atherosclerosis (MESA) study for their valuable contributions. A full list of participating MESA investigators and institutions can be found at http://www.mesa-nhlbi.org.
Sources of Funding:
This research was supported by NIH contracts N01- HC-95159 through N01-HC-95165 and N01-HC-95169 as well as R01 HL069003 and R01 HL081352.
Footnotes
Conflict-of-Interest/Disclosure:
Daniel H. O’Leary owns stock and is an employee of Medpace, Inc., a clinical research organization.
References
- 1.Bots ML, Hofman A, Grobbee DE. Increased common carotid intima-media thickness. Adaptive response or a reflection of atherosclerosis? Findings from the Rotterdam Study. Stroke. 1997;28:2442–2447. doi: 10.1161/01.str.28.12.2442. [DOI] [PubMed] [Google Scholar]
- 2.Eigenbrodt ML, Bursac Z, Rose KM, Couper DJ, Tracy RE, Evans GW, et al. Common carotid arterial interadventitial distance (diameter) as an indicator of the damaging effects of age and atherosclerosis, a cross-sectional study of the Atherosclerosis Risk in Community Cohort Limited Access Data (ARICLAD), 1987–89. Cardiovascular Ultrasound. 2006;4:1. doi: 10.1186/1476-7120-4-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Glagov S, Zarins C, Giddens DP, Ku DN. Hemodynamics and atherosclerosis. Insights and perspectives gained from studies of human arteries. Archives of Pathology & Laboratory Medicine. 1988;112:1018–1031. [PubMed] [Google Scholar]
- 4.Polak JF, Wong Q, Johnson WC, Bluemke DA, Harrington A, O'Leary DH, et al. Associations of cardiovascular risk factors, carotid intima-media thickness and left ventricular mass with inter-adventitial diameters of the common carotid artery: The Multi-Ethnic Study of Atherosclerosis (MESA) Atherosclerosis. 2011;218:344–349. doi: 10.1016/j.atherosclerosis.2011.05.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Eigenbrodt ML, Sukhija R, Rose KM, Tracy RE, Couper DJ, Evans GW, et al. Common carotid artery wall thickness and external diameter as predictors of prevalent and incident cardiac events in a large population study. Cardiovascular Ultrasound. 2007;5:11. doi: 10.1186/1476-7120-5-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bots ML, Grobbee DE, Hofman A, Witteman JCM. Common carotid intima-media thickness and risk of acute myocardial infarction: the role of lumen diameter. Stroke. 2005;36:762–767. doi: 10.1161/01.STR.0000158924.71069.94. [DOI] [PubMed] [Google Scholar]
- 7.Baldassarre D, Hamsten A, Veglia F, de Faire U, Humphries SE, Smit AJ, et al. Measurements of carotid intima-media thickness and of interadventitia common carotid diameter improve prediction of cardiovascular events: results of the IMPROVE (Carotid Intima Media Thickness [IMT] and IMT-Progression as Predictors of Vascular Events in a High Risk European Population) study. Journal of the American College of Cardiology. 2012;60:1489–1499. doi: 10.1016/j.jacc.2012.06.034. [DOI] [PubMed] [Google Scholar]
- 8.Bild DE, Bluemke DA, Burke GL, Detrano R, Diez Roux AV, Folsom AR, et al. Multi-ethnic study of atherosclerosis: objectives and design. American Journal of Epidemiology. 2002;156:871–881. doi: 10.1093/aje/kwf113. [DOI] [PubMed] [Google Scholar]
- 9.Genuth S, Alberti KGMM, Bennett P, Buse J, Defronzo R, Kahn R, et al. Follow-up report on the diagnosis of diabetes mellitus. Diabetes Care. 2003;26:3160–3167. doi: 10.2337/diacare.26.11.3160. [DOI] [PubMed] [Google Scholar]
- 10.Mathiesen EB, Johnsen SH, Wilsgaard T, Bonaa KH, Lochen M-L, Njolstad I. Carotid plaque area and intima-media thickness in prediction of first-ever ischemic stroke: a 10-year follow-up of 6584 men and women: the Tromso study. Stroke. 2011;42:972–978. doi: 10.1161/STROKEAHA.110.589754. [DOI] [PubMed] [Google Scholar]
- 11.Glagov S, Weisenberg E, Zarins CK, Stankunavicius R, Kolettis GJ. Compensatory enlargement of human atherosclerotic coronary arteries. New England Journal of Medicine. 1987;316:1371–1375. doi: 10.1056/NEJM198705283162204. [DOI] [PubMed] [Google Scholar]
- 12.Polak JF, Kronmal RA, Tell GS, O'Leary DH, Savage PJ, Gardin JM, et al. Compensatory increase in common carotid artery diameter. Relation to blood pressure and artery intima-media thickness in older adults. Cardiovascular Health Study. Stroke. 1996;27:2012–2015. doi: 10.1161/01.str.27.11.2012. [DOI] [PubMed] [Google Scholar]
- 13.Polak JF, Pencina MJ, Meisner A, Pencina KM, Brown LS, Wolf PA, et al. Associations of carotid artery intima-media thickness (IMT) with risk factors and prevalent cardiovascular disease: comparison of mean common carotid artery IMT with maximum internal carotid artery IMT. Journal of Ultrasound in Medicine. 2010;29:1759–1768. doi: 10.7863/jum.2010.29.12.1759. [DOI] [PMC free article] [PubMed] [Google Scholar]