Abstract
Purpose
The optimal outcome after radical prostatectomy (RP) for clinically localized prostate cancer is freedom from biochemical recurrence (BCR) along with recovery of continence and erectile function, a so-called trifecta. We evaluated our series of open radical prostatectomy patients to determine the likelihood of this outcome and to develop a nomogram predicting the trifecta.
Material and Methods
We reviewed records of patients undergoing open RP for clinical stage T1c–T3a prostate cancer at our center during 2000–2006. Men were excluded if they received preoperative hormonal therapy, chemotherapy, or radiation therapy; if their pre-treatment PSA was >50 ng/ml; or if they were impotent or incontinent before RP; 1577 men were included in the study. Freedom from BCR was defined as post-RP PSA <0.2 ng/ml. Continence was defined as not having to wear any protective pads. Potency was defined as erections adequate for intercourse on the majority of attempts, with or without a phosphodiesterase-5 inhibitor.
Results
Mean patient age was 58 years and mean pretreatment PSA was 6.4 ng/ml. A trifecta outcome (cancer-free status with recovery of continence and potency) was achieved in 62% of patients. In a nomogram developed to predict the likelihood of the trifecta, baseline PSA was the major predictive factor. The area under the receiver operating characteristic curve for the nomogram was 0.773, and calibration appeared excellent.
Conclusions
A trifecta (optimal) outcome can be achieved in the majority of men undergoing RP. The nomogram will permit patients to estimate preoperatively their likelihood of an optimal outcome after RP.
INTRODUCTION
Early detection programs for prostate cancer have resulted in a marked stage-shift; today, the majority of men diagnosed with prostate cancer has clinically localized cancer and are diagnosed at a younger age. Long-term outcomes from several open radical prostatectomy (RP) series suggest that at least 75% of men undergoing surgery remain free from cancer recurrence, and cancer-specific survival approaches 95% at 15 years.1,2 As a result, investigation of long-term outcomes after RP has increasingly focused on the recovery of continence and erectile function. While the individual likelihood of each of these three outcomes (cancer recurrence, continence, and potency) has been well documented, many patients desire to learn their likelihood of achieving an optimal outcome, meaning cancer-free and full functional recovery (“trifecta”).
The concept of combined reporting of cancer control and functional outcomes after RP was originated by Salomon et al, who suggested a point scale to assess outcomes.3 Each patient was attributed either 0 or 4 points according to the presence or absence of biochemical recurrence (BCR), 0 or 2 points according to the presence or absence of urinary incontinence, and 0 or 1 point according to the presence or absence of erectile dysfunction. The scores thus classify patients into eight distinct categories, from 0 to 7 points. Among their 205 patients, the mean score was 5.05 ± 1.78 and median score was 6. Approximately 20% of these patients had a score of 7, meaning freedom from BCR and complete continence and potency. This score-based approach, however, does not consider individual patient preferences (utilities) and assumes that BCR is twice as important as the recovery of continence and four times more important than the recovery of potency.
We have previously reported that a trifecta outcome occurred in 53% of 647 men undergoing RP.4 Our initial report was limited by not controlling for known risk factors of functional recovery (primarily patient age) or progression (serum PSA level, clinical stage, and biopsy features). In this current study we update our trifecta results and present a predictive model (nomogram) estimating the likelihood of an individual patient achieving this outcome.
METHODS
All men undergoing RP at Memorial Sloan-Kettering Cancer Center have their clinical information prospectively entered into a computerized database approved by the institutional review board. Following treatment, information on continence, potency, and serum PSA levels are captured. This study focuses on 2906 consecutive men with clinical stage T1c to T3a prostate cancer undergoing open RP at our center by two surgeons (PTS, JAE) from January 2000 through December 2006. All men were included, whether or not the surgeon intended to perform bilateral neurovascular bundle preservation. Patients were excluded if they received neoadjuvant hormonal therapy (n=158), preoperative radiation therapy (n=101), or neoadjuvant chemotherapy (n=20). Patients were also excluded if the pre-RP serum PSA was > 50 ng/ml (n=9) or if, prior to RP, the patient was incontinent (n=51). We define potency on a 5-point rigidity scale whether or not the patient uses a PDE-5 inhibitor (1- normal, full erections; 2- full, but diminished erections satisfactory for sexual activity on more than 50% of attempts; 3- partial erections satisfactory for sexual activity in less than 50% of attempts; 4- partial erections unsatisfactory for sexual activity; 5- no erectile function). Patients were considered potent if they responded “yes” to the question, “Are you able to reliably attain an erection rigid enough for intercourse with or without the use of a PDE-5 inhibitor (Viagra, Levitra, or Cialis) more than half the time?” corresponding to level 1 or 2 on our rigidity scale. Patients were excluded if they characterized themselves as having pre-operative erectile dysfunction (potency scale 3–5; an inability to achieve erections satisfactory for sexual intercourse at least 50% of the time; n=493). Finally, patients were excluded if information regarding pretreatment continence, pretreatment potency, post-RP BCR, post-RP continence, and/or post-RP potency was unavailable (n=497). Therefore, 1577 men were included in this study.
BCR was defined as a PSA ≥ 0.2 ng/ml after RP. Continence and potency were assessed by either patient-reported questionnaire or physician interview. Patients were considered continent if they answered “no” to the question, “Do you wear any protective material because you leak urine?” Patients were considered potent if they responded “yes” to the question, “Are you able to reliably attain an erection rigid enough for intercourse with or without the use of a PDE-5 inhibitor (Viagra, Levitra, or Cialis) more than half the time?” corresponding to level 1 or 2 on our rigidity scale. Thus, the same definition of potency was used both pre- and post-operatively.
Probabilities of achieving an individual outcome and trifecta were estimated using the cumulative incidence method. The probability of achieving trifecta was modeled using generalized estimating equations. A nomogram was constructed to graphically depict the prediction model for trifecta. The prediction model was subjected to 10-fold cross validation. These cross-validated predicted probabilities were assessed for discrimination and calibration when predicting trifecta. Discrimination was quantified as the area under the receiver operating characteristic curve. Calibration was assessed by plotting predicted vs. observed probabilities. For this plot, patients were grouped into deciles of their predicted probabilities. This study received institutional review board approval.
RESULTS
Patient characteristics of the 1577 men analyzed are summarized in Table 1. Mean age at RP was 58 years (range, 37 to 77 years) and mean pretreatment serum PSA was 6.4 ng/ml (range, 0.1 to 50 ng/ml). In the majority of patients (80%), RP included an attempt at bilateral neurovascular bundle (NVB) preservation; approximately 19% had partial or complete unilateral NVB resection and 1% had bilateral NVB resection. Importantly, all men, regardless of the surgeon’s perceived status of their NVB status, were included in all subsequent analyses, including potency. The positive surgical margin rate was 11%. Median follow-up was 23.5 months (range, 0 to 87 months).
Table 1.
Pre- and post-operative characteristics of 1577 men undergoing open radical prostatectomy.
| Number of patients | 1577 |
| Mean age, years (range) | 58 (37–77) |
| PSA (ng/ml) | |
| Mean | 6.4 |
| Median | 5.3 |
| Interquartile range | 4.1–7.3 |
| Biopsy Gleason grades (%) | |
| 2/3–3/3 | 56 |
| 3/4–3/5 | 22 |
| 4/3 | 8 |
| 4/4–5/5 | 6 |
| Missing | 9 |
| Clinical stage (%) | |
| T1c | 65 |
| T2a | 19 |
| T2b | 10 |
| T2c | 5 |
| T3a | 2 |
| RP Gleason score (%) | |
| ≤ 6 | 40 |
| 7 | 53 |
| 8–10 | 6 |
| Pathology (%) | |
| Organ confined | 71 |
| Extraprostatic extension | 28 |
| Seminal vesicle invasion | 6 |
| Node positive | 4 |
| Positive margin (%) | 11 |
PSA, prostate-specific antigen
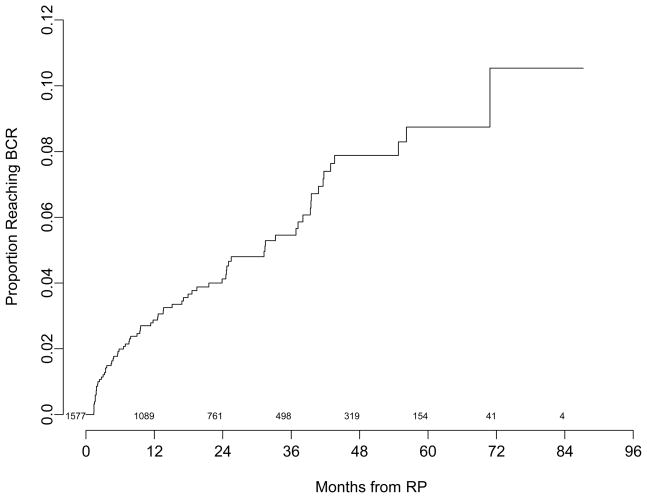
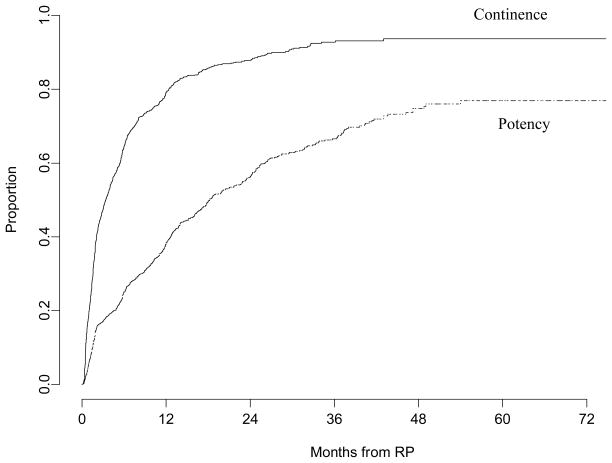
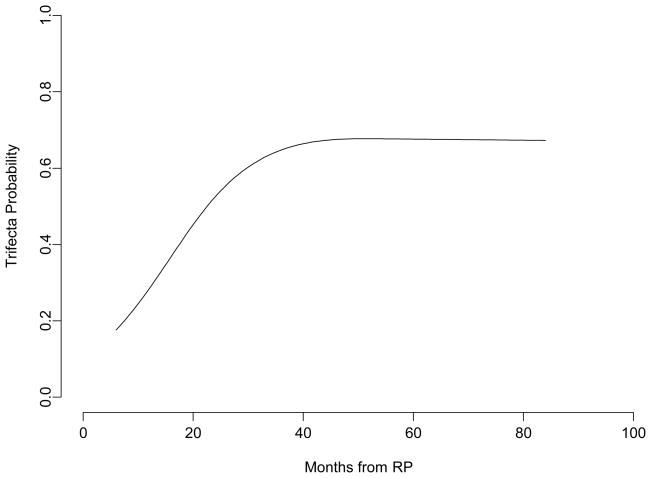
The probability that BCR occurred within 5 years is 9% (Fig. 1). The median time to recovery of urinary continence was 3.4 months, with 79% of men being continent at 12 months. The overall probability of recovering continence was 94% (Fig. 2). The probability of recovery of potency, regardless of age or status of the NVB’s, was 39%, 56%, and 67% at 12, 24, and 36 months, respectively (Fig. 2). The median time to recovery of potency was 18 months. Figure 3 illustrates the likelihood of achieving an optimal outcome in all three endpoints for a particular patient. This outcome is primarily determined by the recovery of potency. Sixty-two percent of patients in our study group were predicted to achieve a trifecta outcome at 48 months.
Figure 1.
The probability of biochemical recurrence (BCR) over time in 1577 men undergoing radical prostatectomy. The number at risk is shown above the x axis.
Figure 2.
The probability of recovery of continence (pad free) and potency (rigidity scale 1 or 2) after radical prostatectomy (RP)
Figure 3.
Trifecta probability for an individual patient after radical prostatectomy (RP). This is the probability of reaching and maintaining trifecta for a patient with average characteristics in our series: pre-RP PSA of 5.4, clinical stage T1c, normal pretreatment erectile function (rigidity scale 1), prostate biopsy Gleason grade 3+3, and pre-RP age of 58.2 years
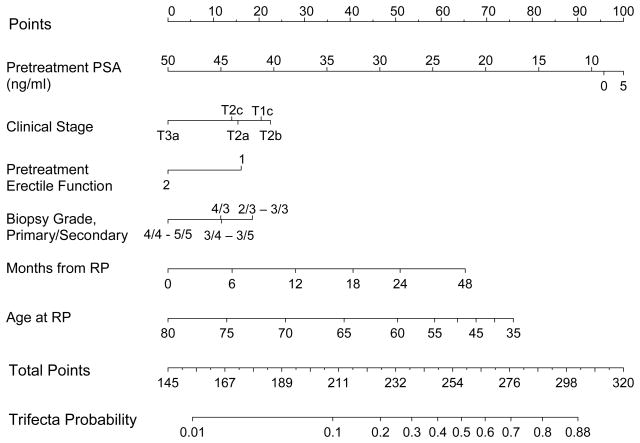
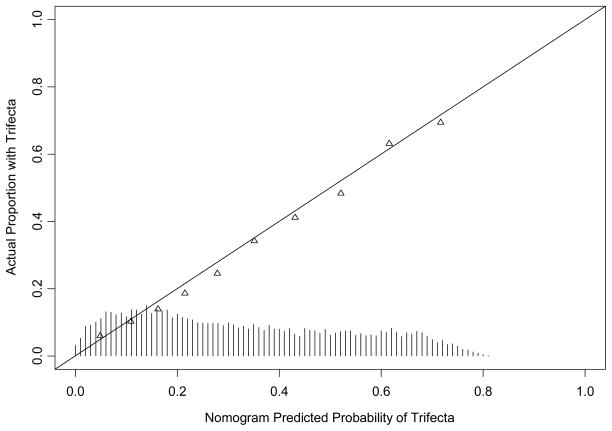
A nomogram was constructed to predict the likelihood that a man will achieve a trifecta outcome after RP based on preoperative clinical parameters (Fig. 4). Baseline PSA was the factor accorded the greatest predictive weight in the model. The accuracy of the nomogram, measured as area under the receiver operating characteristic curve, was 0.773. Calibration of the nomogram appeared to be excellent (Fig. 5).
Figure 4.
Nomogram predicting the likelihood of attaining a trifecta outcome after RP. The definitions of continence (the patient does not wear pads) and potency (rigidity scale 1 or 2) are the same prior to and after RP. Note that even a minor loss of erectile function (pre-RP rigidity scale 2 versus 1) is a risk factor for not achieving a trifecta outcome.
Note: This is to be used only prior to surgery, not during follow-up.
Figure 5.
Calibration plot for the trifecta nomogram. Histogram at the bottom illustrates the distribution of predicted probabilities.
DISCUSSION
The three long-term goals of RP are complete removal of the cancer, recovery of continence, and recovery of potency. These outcomes are not independent, meaning that improvement in one area may come at the expense of outcomes in the other two areas. Therefore, assessing an individual outcome after RP may not truly inform the patient as to what he might expect in terms of overall cancer control and quality of life. This has led to the concept of reporting the likelihood of achieving multiple outcomes after treatment.3,4 Our data suggest that in our patient population, approximately 60 to 70% of men undergoing RP can expect to be free of cancer recurrence and to recover continence and potency. This outcome is mainly determined by the recovery of potency after RP and may take 36 months or more to achieve. Such information is critical to the patient to better understand his risks and to have more realistic expectations regarding recovery.
Each of the three outcomes after RP depends upon patient-specific factors. Biochemical recurrence is influenced by pretreatment serum PSA level, clinical stage, and prostate biopsy features. The recovery of continence and potency after RP are known to be influenced by age, pre-treatment level of function, and surgical technique. Therefore, in developing models to predict these outcomes, all of these parameters must be considered and weighted according to their influence on the trifecta outcome. While surgical technique certainly plays a critical role in all outcomes after RP, the actual surgical technique to be used (such as the extent of NVB preservation) is not completely known before surgery. Thus, no model can perfectly predict an individual patient’s outcome. Considering these limitations, the nomogram we have developed provides a reasonable estimate of the patient’s likelihood of achieving a trifecta outcome.
Our study has several limitations. Our outcomes are based on only two surgeons, both of whom have performed more than 1,000 RP’s. Previous publications have demonstrated that surgical experience and surgical technique affect biochemical recurrence, continence, and potency after RP.5–7 Therefore, these results and the nomogram developed based on these results may not be applicable to other surgeons and await validation using other datasets. In addition, all of the procedures were performed using an open technique and thus these outcomes may not be applicable to patients treated with perineal, laparoscopic, or robotic-assisted laparoscopic RP. Our median follow-up is only 24 months so it is possible that our results may change as the series matures. We also note that our two quality-of-life outcomes are primarily determined by physician assessment rather than patient questionnaire. Nevertheless, we have previously demonstrated a high degree of correlation between physician-reported and patient-reported assessment of continence when the definition is pad-free.8 It is therefore unlikely that continence has been over- or under-reported in our patients. The same is true for potency. We have demonstrated a good correlation between the definition of potency used in this study and the patient-derived International Index of Erectile Function (IIEF), with our potency assessment (our rigidity scale defining pre- and post-operative erectile function as level 1 or 2) corresponding to a median IIEF score of ≥ 24 out of a maximum of 30.9 In addition, we have not included individual patient co-morbidities in our nomogram although factors such as a history of diabetes, hypertension and/or cigarette smoking may influence erectile function. Finally, although the three outcomes assessed in this study may not have equal importance to the individual patient, cancer recurrence, incontinence, and erectile dysfunction are all undesirable. Until a detailed assessment of patient preferences is available, our nomogram provides a reasonable tool to predict the likelihood of the optimal outcome.
CONCLUSIONS
While no surgeon universally achieves the trifecta outcome of freedom from BCR and complete recovery of continence and potency, our data suggest that a trifecta can be achieved in the majority of men undergoing RP. The nomogram we have developed allows men to assess their likelihood of achieving an optimal outcome after RP based on their unique pretreatment parameters.
Acknowledgments
Supported in part by funds from National Cancer Institute grant CA 92629-05 SPORE in prostate cancer
Definition of Abbreviations
- RP
Radical prostatectomy
- BCR
Biochemical recurrence
- NVB
Neurovascular bundle
- PSA
Prostate specific antigen
- IIEF
International Index of Erectile Function
Footnotes
This manuscript has not been submitted for publication or presented in all or in part at any meeting.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Bianco FJ, Jr, Scardino PT, Eastham JA. Radical prostatectomy: long-term cancer control and recovery of sexual and urinary function (“trifecta”) Urology. 2005;66:83. doi: 10.1016/j.urology.2005.06.116. [DOI] [PubMed] [Google Scholar]
- 2.Han M, Walsh P, Catalona W, Zahurak M, Piantadosi S, Roehl K, et al. Updated recurrence-free survival (RFS) prediction model following radical prostatectomy (RRP) J Urol, abstract. 2007;327 [Google Scholar]
- 3.Salomon L, Saint F, Anastasiadis AG, Sebe P, Chopin D, Abbou C. Combined reporting of cancer control and functional results of radical prostatectomy. Eur Urol. 2003;44:656. doi: 10.1016/j.eururo.2003.09.009. [DOI] [PubMed] [Google Scholar]
- 4.Saranchuk JW, Kattan MW, Elkin E, Touijer AK, Scardino PT, Eastham JA. Achieving optimal outcomes after radical prostatectomy. J Clin Oncol. 2005;23:4146. doi: 10.1200/JCO.2005.12.922. [DOI] [PubMed] [Google Scholar]
- 5.Begg CB, Riedel ER, Bach PB, Kattan MW, Schrag D, Warren JL, et al. Variations in morbidity after radical prostatectomy. N Engl J Med. 2002;346:1138. doi: 10.1056/NEJMsa011788. [DOI] [PubMed] [Google Scholar]
- 6.Eastham JA, Kattan MW, Riedel E, Begg CB, Wheeler TM, Gerigk C, et al. Variations among individual surgeons in the rate of positive surgical margins in radical prostatectomy specimens. J Urol. 2003;170:2292. doi: 10.1097/01.ju.0000091100.83725.51. [DOI] [PubMed] [Google Scholar]
- 7.Vickers AJ, Bianco FJ, Serio AM, Eastham JA, Schrag D, Klein EA, et al. The surgical learning curve for prostate cancer control after radical prostatectomy. J Natl Cancer Inst. 2007;99:1171. doi: 10.1093/jnci/djm060. [DOI] [PubMed] [Google Scholar]
- 8.Dash A, Otero J, Bianco FJ, Shabsigh A, Serio A, Vickers A, et al. The concordance between a systematically administered physician reported assessment of function and health-related quality of life instrument. J Urol, abstract. 2007:17. [Google Scholar]
- 9.Rabbani F, Cozzi P, Scardino P. Quantitative assessment of the response to Cavermap nerve stimulation at radical prostatectomy. J Urol. 2002;167:356. abstract 1414. [Google Scholar]