Abstract
Background
Age-related macular degeneration (AMD) is the most common cause of uncorrectable severe vision loss in people aged 55 years and older in the developed world. Choroidal neovascularization (CNV) secondary to neovascular AMD accounts for most AMD-related severe vision loss. Anti-vascular endothelial growth factor (anti-VEGF) agents, injected intravitreally, aim to block the growth of abnormal blood vessels in the eye to prevent vision loss and, in some instances, improve vision.
Objectives
To investigate: (1) the ocular and systemic effects of, and quality of life associated with, intravitreally injected anti-VEGF agents (pegaptanib, ranibizumab, and bevacizumab) for the treatment of neovascular AMD compared with no anti-VEGF treatment; and (2) the relative effects of one anti-VEGF agent compared with another when administered in comparable dosages and regimens.
Search methods
We searched Cochrane Central Register of Controlled Trials (CENTRAL) (which contains the Cochrane Eyes and Vision Group Trials Register) (2014, Issue 3), Ovid MEDLINE, Ovid MEDLINE In-Process and Other Non-Indexed Citations, Ovid MEDLINE Daily, Ovid OLDMEDLINE (January 1946 to March 2014), EMBASE (January 1980 to March 2014), Latin American and Caribbean Health Sciences Literature Database (LILACS) (January 1982 to March 2014), the metaRegister of Controlled Trials (mRCT) (www.controlledtrials.com), ClinicalTrials.gov (www.clinicaltrials.gov) and the World Health Organization (WHO) International Clinical Trials Registry Platform (ICTRP) (www.who.int/ictrp/search/en). We used no date or language restrictions in the electronic searches for trials. We last searched the electronic databases on 27 March 2014.
Selection criteria
We included randomized controlled trials (RCTs) that evaluated pegaptanib, ranibizumab, or bevacizumab versus each other or a control treatment (e.g., sham treatment or photodynamic therapy). All trials followed participants for at least one year.
Data collection and analysis
Two review authors independently screened records, extracted data, and assessed risks of bias. We contacted trial authors for additional data. We analyzed outcomes as risk ratios (RRs) or mean differences (MDs). We used the standard methodological procedures expected by The Cochrane Collaboration.
Main results
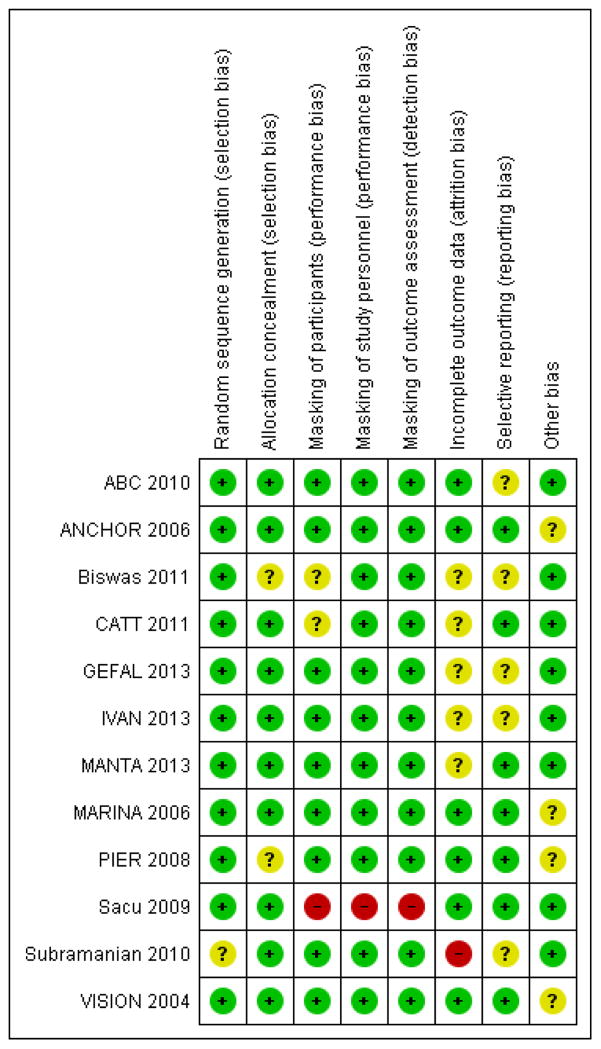
We included 12 RCTs including a total of 5496 participants with neovascular AMD (the number of participants per trial ranged from 28 to 1208). One trial compared pegaptanib, three trials ranibizumab, and two trials bevacizumab versus controls; six trials compared bevacizumab with ranibizumab. Four trials were conducted by pharmaceutical companies; none of the eight studies which evaluated bevacizumab were funded by pharmaceutical companies. The trials were conducted at various centers across five continents (North and South America, Europe, Asia and Australia). The overall quality of the evidence was very good, with most trials having an overall low risk of bias.
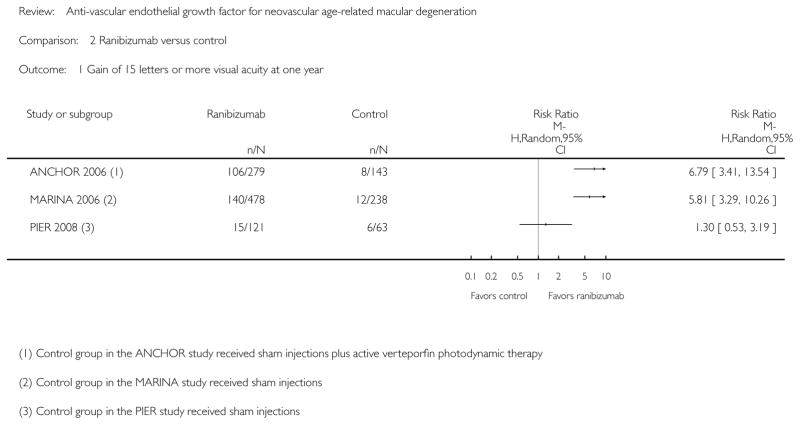
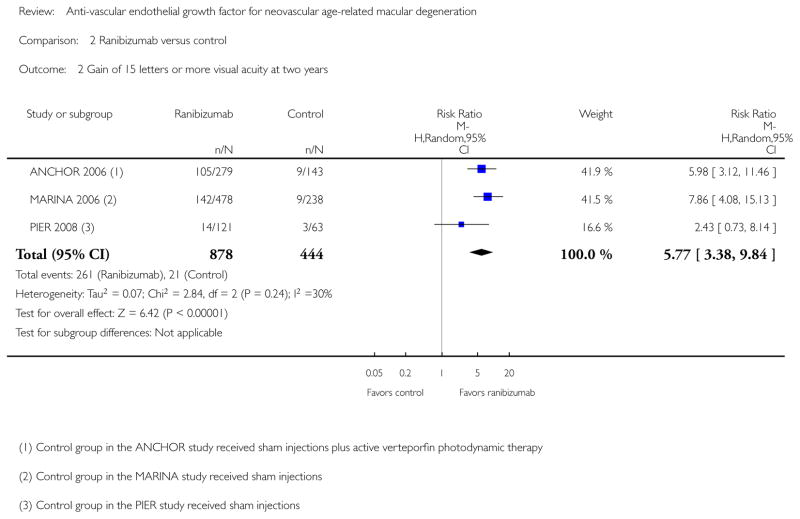
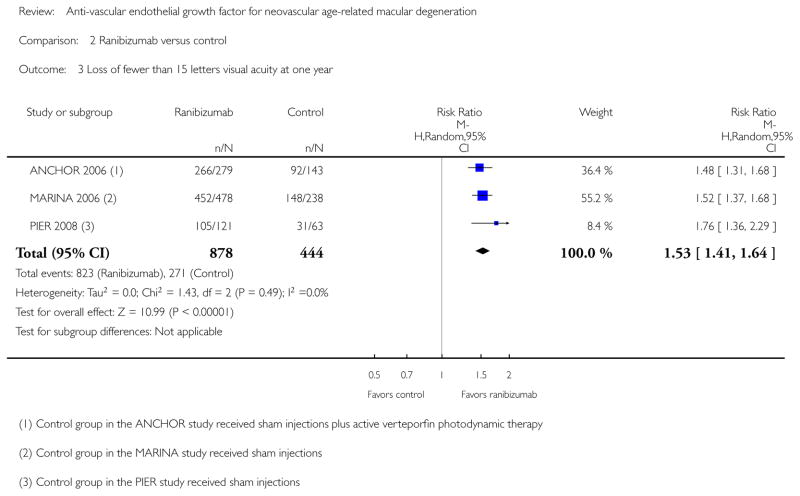
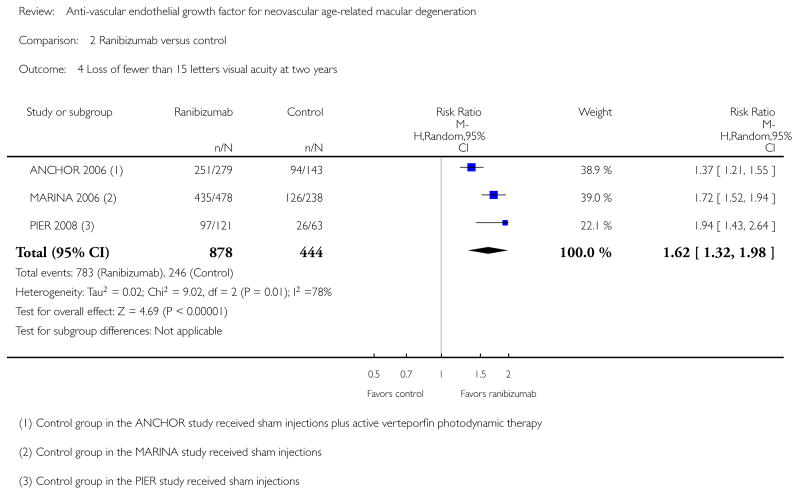
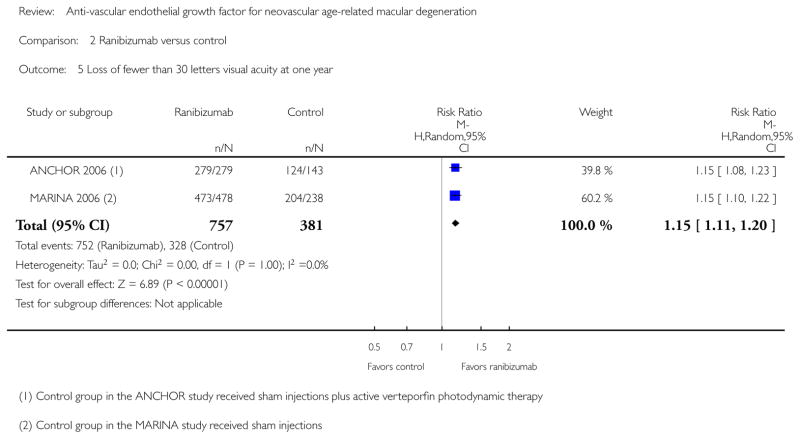
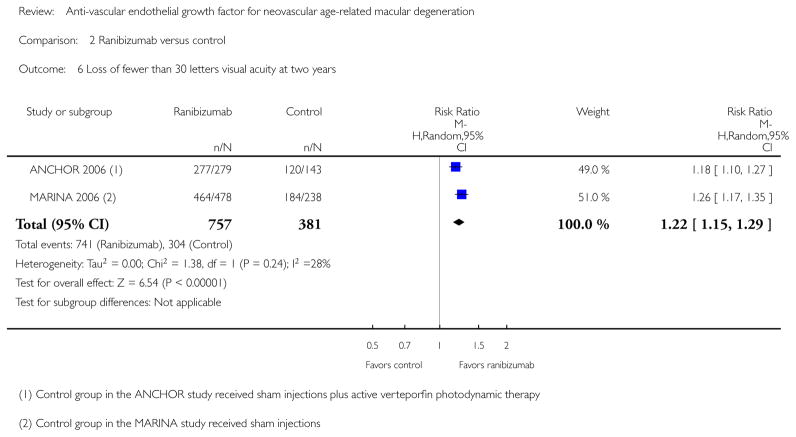
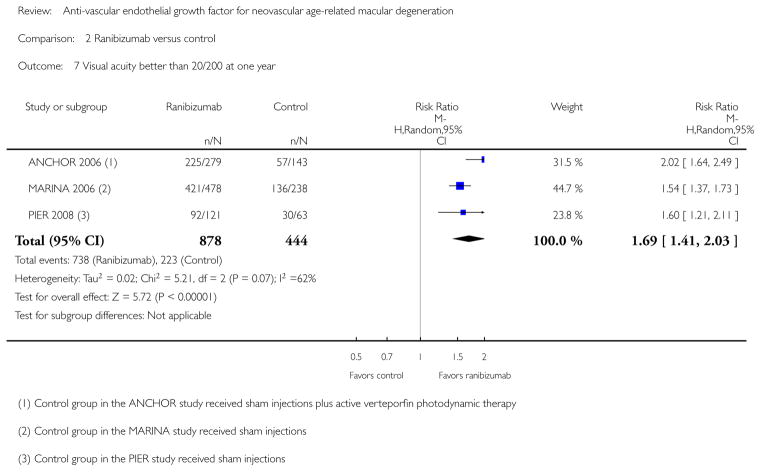
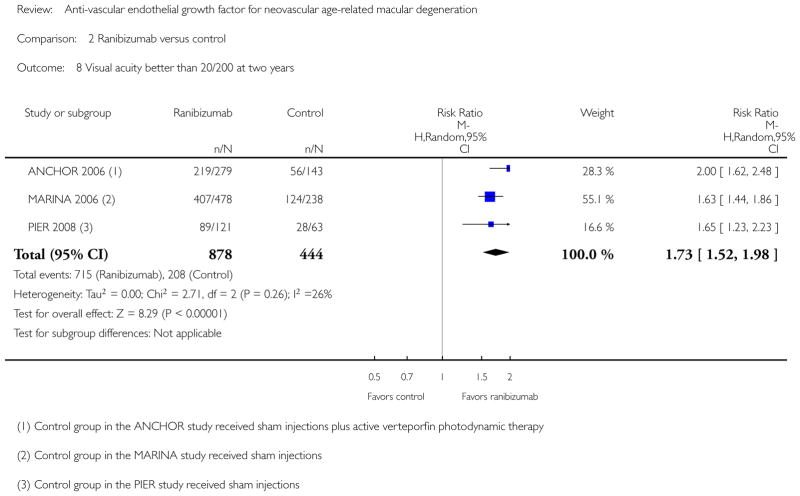
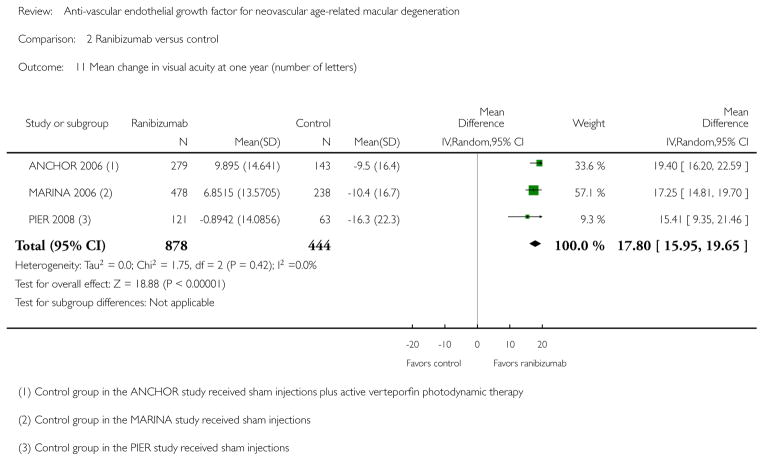
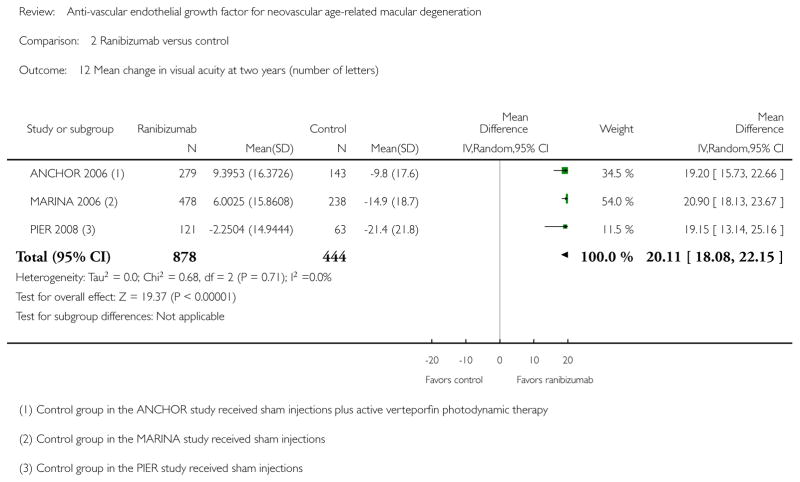
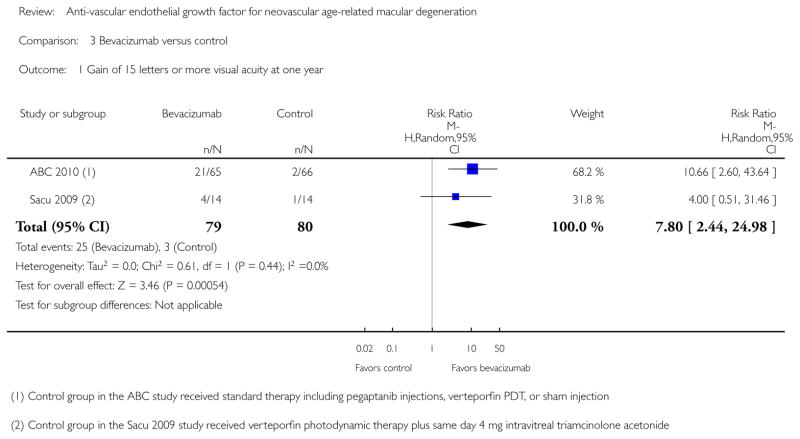
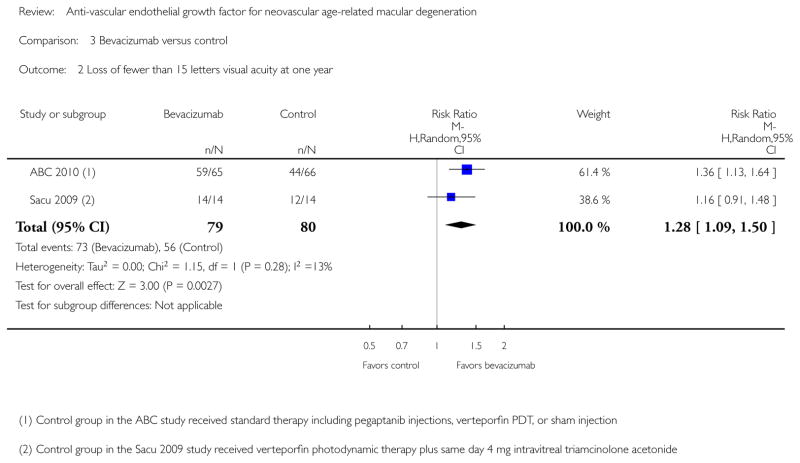
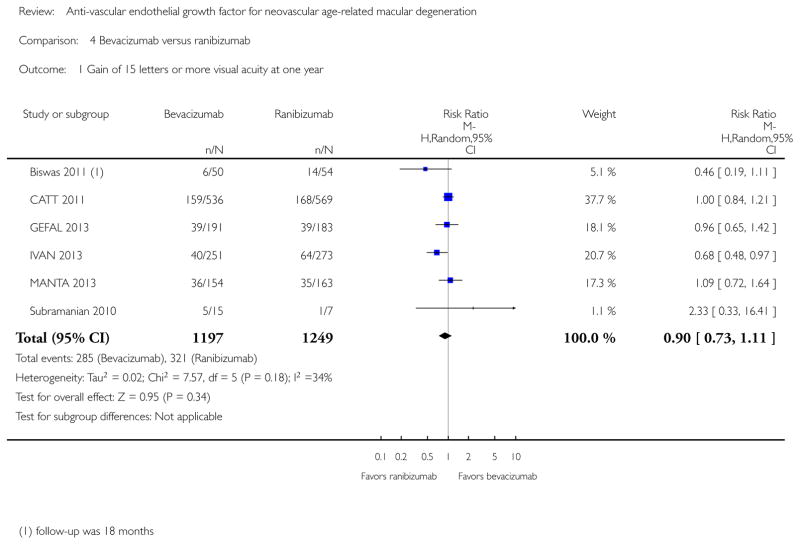
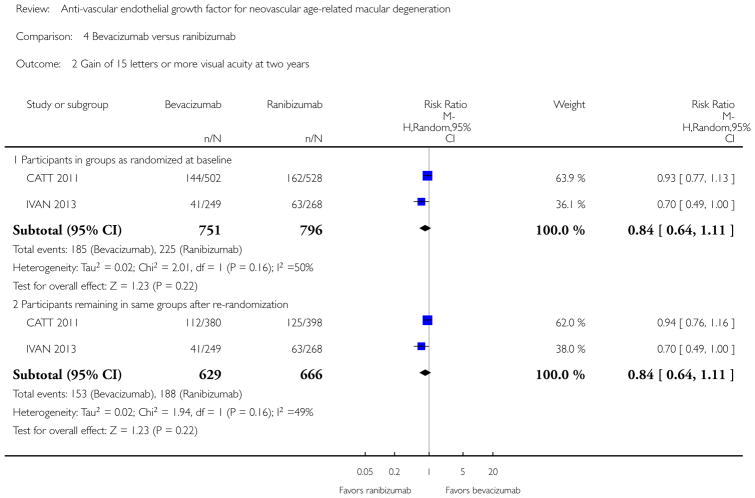
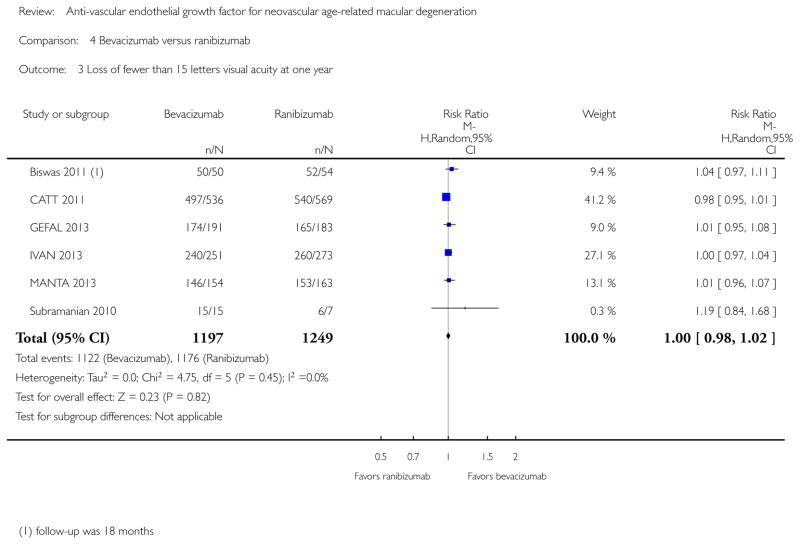
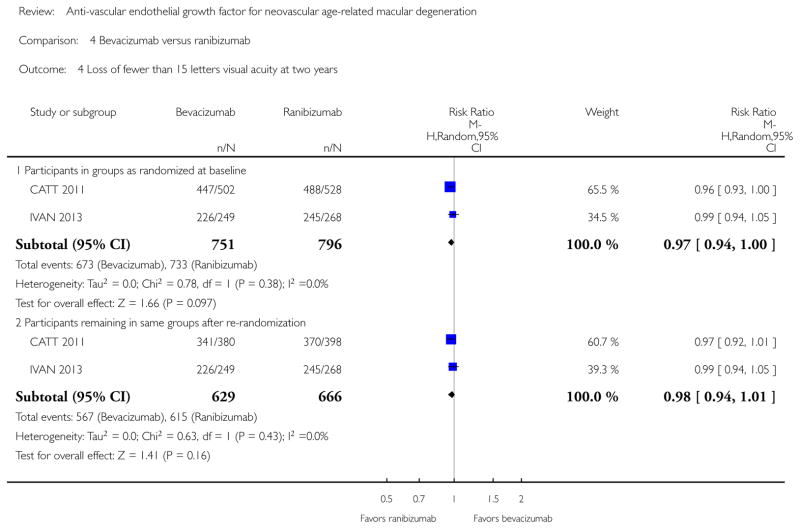
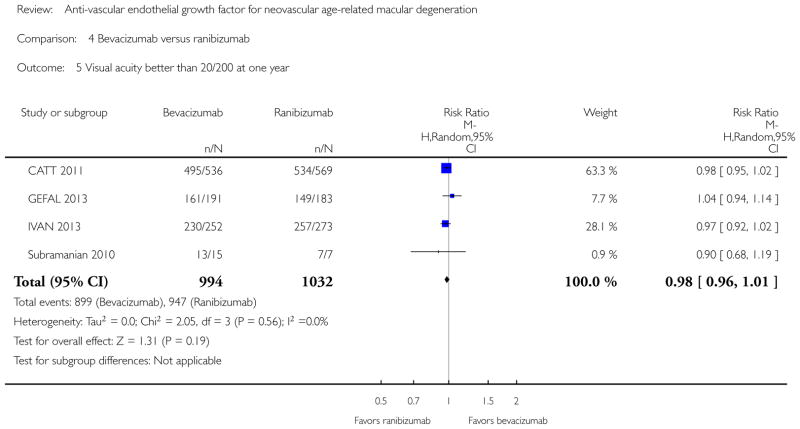
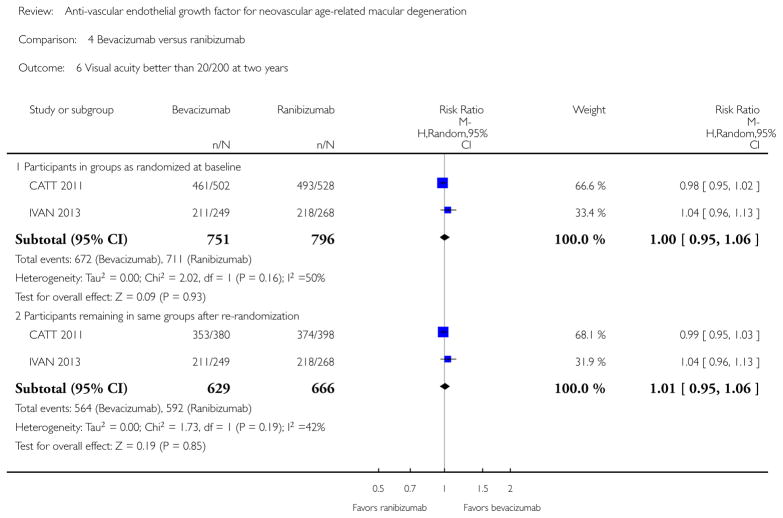
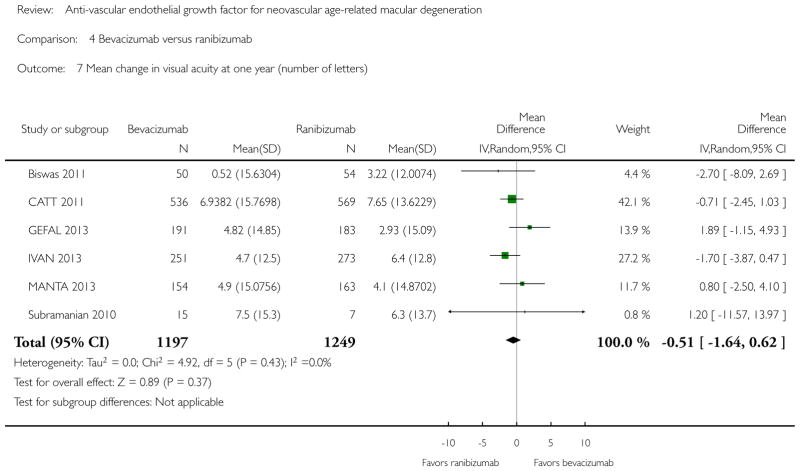
When compared with control treatments, participants who received any of the three anti-VEGF agents were more likely to have gained 15 letters or more of visual acuity, lost fewer than 15 letters of visual acuity, and had vision 20/200 or better after one year of follow up. Visual acuity outcomes after bevacizumab and ranibizumab were similar when the same regimens were compared in the same RCTs, despite the substantially lower cost for bevacizumab compared with ranibizumab. No trial directly compared pegaptanib with other anti-VEGF agents; however, when compared with controls, ranibizumab or bevacizumab yielded larger improvements in visual acuity outcomes than pegaptanib.
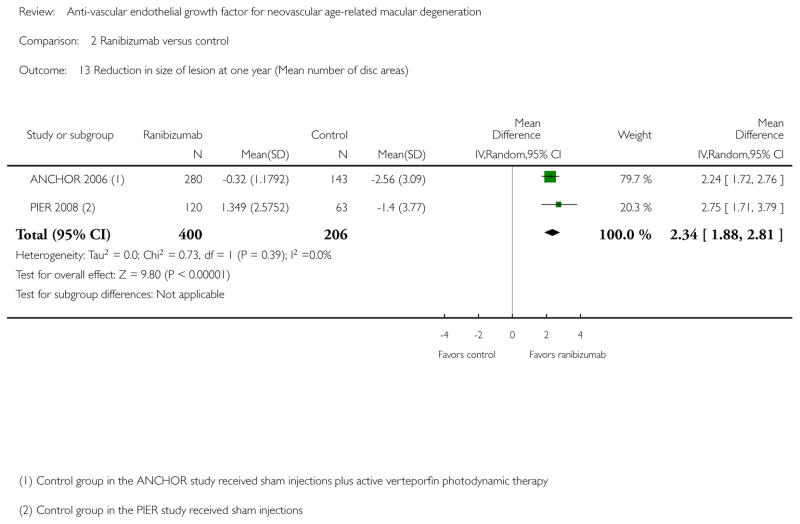
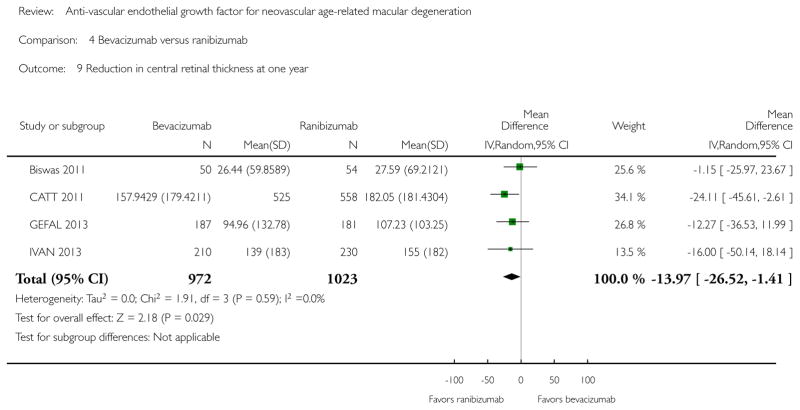
Participants treated with anti-VEGFs showed improvements in morphologic outcomes (e.g., size of CNV or central retinal thickness) compared with participants not treated with anti-VEGF agents. There was less reduction in central retinal thickness among bevacizumab-treated participants than among ranibizumab-treated participants after one year (MD −13.97 μm; 95% confidence interval (CI) −26.52 to −1.41); however, this difference is within the range of measurement error and we did not interpret it as being clinically meaningful.
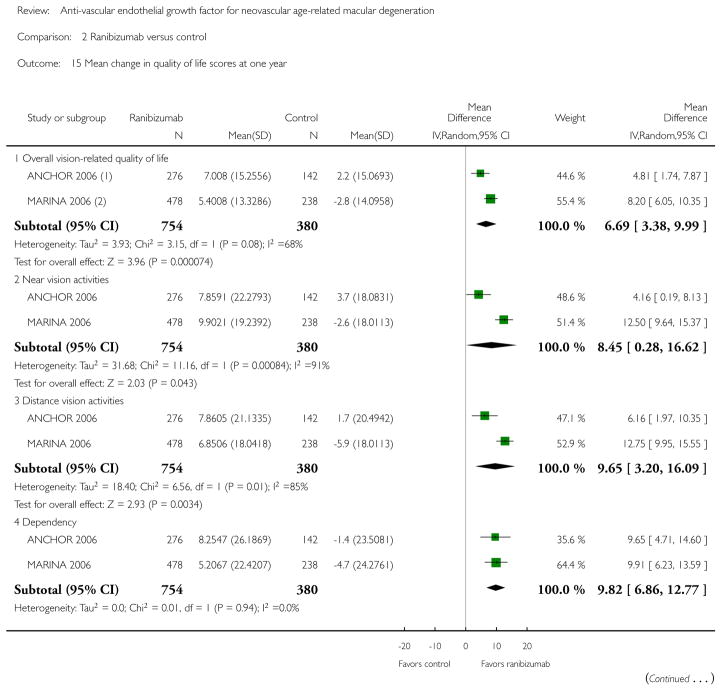
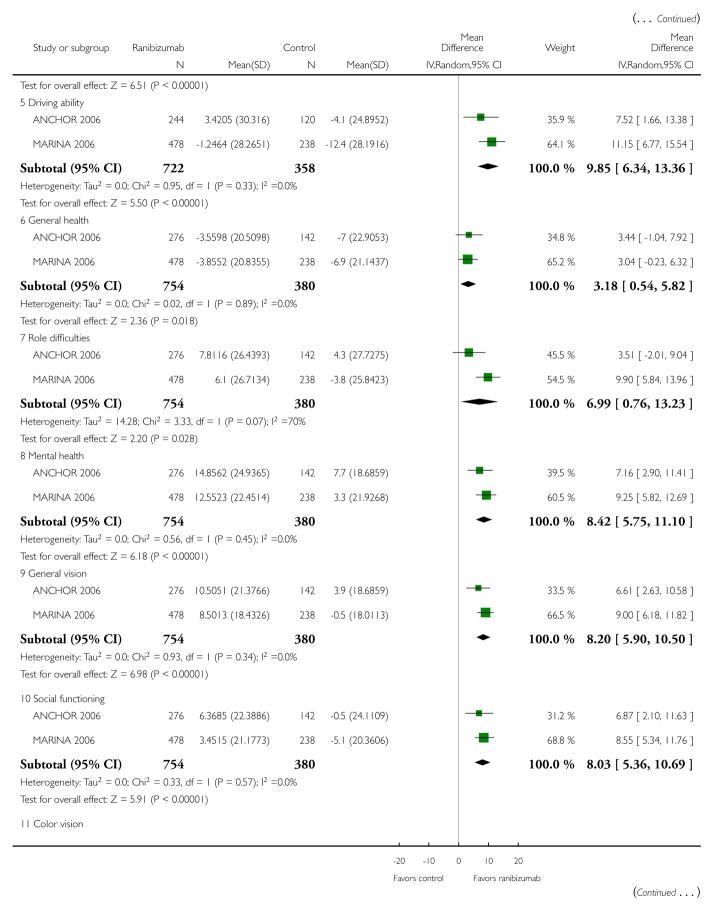
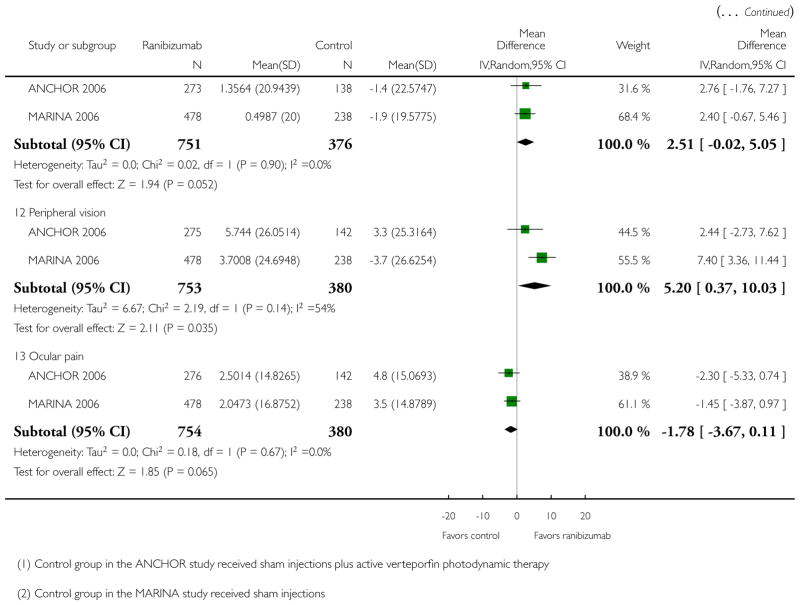
Ocular inflammation and increased intraocular pressure after intravitreal injection were the most frequently reported serious ocular adverse events. Endophthalmitis was reported in fewer than 1% of anti-VEGF treated participants; no cases were reported in control groups. The occurrence of serious systemic adverse events was comparable across anti-VEGF-treated groups and control groups; however, the numbers of events and trial participants may have been insufficient to detect a meaningful difference between groups. Data for visual function, quality of life, and economic outcomes were sparsely measured and reported.
Authors’ conclusions
The results of this review indicate the effectiveness of anti-VEGF agents (pegaptanib, ranibizumab, and bevacizumab) in terms of maintaining visual acuity; ranibizumab and bevacizumab were also shown to improve visual acuity. The information available on the adverse effects of each medication do not suggest a higher incidence of potentially vision-threatening complications with intravitreal injection compared with control interventions; however, clinical trial sample sizes may not have been sufficient to detect rare safety outcomes. Research evaluating variable dosing regimens with anti-VEGF agents, effects of long-term use, combination therapies (e.g., anti-VEGF treatment plus photodynamic therapy), and other methods of delivering the agents should be incorporated into future Cochrane reviews.
INDEX TERMS Medical Subject Headings (MeSH): Angiogenesis Inhibitors [*therapeutic use]; Antibodies, Monoclonal [therapeutic use]; Antibodies, Monoclonal, Humanized, Aptamers, Nucleotide [therapeutic use]; Choroidal Neovascularization; Macular Degeneration [*drug therapy]; Porphyrins [therapeutic use]; Randomized Controlled Trials as Topic; Vascular Endothelial Growth Factor A [*antagonists & inhibitors]
MeSH check words: Aged, Humans, Middle Aged
PLAIN LANGUAGE SUMMARY
Anti-vascular endothelial growth factor for neovascular age-related macular degeneration
Background
Age-related macular degeneration (AMD) is a common cause of severe vision loss in people 55 years and older. Neovascular AMD, which involves abnormal growth of blood vessels in the back of the eye, accounts for most AMD-related severe vision loss. Injections into the eye of medications, such as pegaptanib, ranibizumab, and bevacizumab, that block this abnormal growth of blood vessels in the back of the eye are the main way to treat this condition. These types of medications are known as anti-vascular endothelial growth factors (anti-VEGFs).
Review question
We aimed to investigate: (1) the effects of anti-VEGF agents injected into the eye for the treatment of neovascular AMD when compared with no anti-VEGF treatment; and (2) the relative effects of one anti-VEGF agent compared with another when administered in comparable dosages and regimens.
Study details
We found 12 randomized controlled trials (RCTs), which included a total of 5496 participants with neovascular AMD (the number of participants per trial ranged from 28 to 1208). One trial compared pegaptanib, three trials ranibizumab, and two trials bevacizumab versus no anti-VEGF treatment; six trials compared bevacizumab with ranibizumab. Four trials were conducted by drug companies; none of the eight studies which evaluated bevacizumab were funded by drug companies. The trials were conducted at various centers on five continents (North and South America, Europe, Asia and Australia). All trials treated and followed-up participants for at least one year. The evidence is current to 27 March 2014.
Key results
Participants treated with any of the three anti-VEGF agents more often experienced improved vision, less often lost vision, and were less likely to be legally blind than participants treated with control interventions after one year of treatment. Participants treated with anti-VEGF agents also showed improvements in structural areas of the eye that doctors use to monitor disease progression and treatment response compared with participants not treated with anti-VEGF agents.
Compared with control treatments, treatment with ranibizumab or bevacizumab yielded larger improvements than pegaptanib. No trial compared pegaptanib directly with other anti-VEGF agents. When bevacizumab and ranibizumab were compared with each other, there were no major differences with respect to vision-related outcomes; there was, however, a large difference in cost between the two agents.
Inflammation and increased pressure in the eye were the most common vision-related adverse events with anti-VEGF agents. Endophthalmitis (inflammation in the inner part of the eye, which can lead to blindness) was reported in fewer than 1% of anti-VEGF-treated participants; no cases were reported in control groups. The occurrence of serious adverse health effects, such as high blood pressure and internal bleeding, was comparable across anti-VEGF-treated groups and control groups; however, the number of events was small relative to the number of people in the studies making it difficult to detect any meaningful differences between groups. Few data were available for visual function (e.g., reading speed and critical print size), quality of life, and economic outcomes.
Quality of the evidence
The overall quality of the evidence was very good, with most trials having an overall low risk of bias (i.e., good methodological quality).
SUMMARY OF FINDINGS FOR THE MAIN COMPARISON [Explanation]
| Bevacizumab compared with ranibizumab for neovascular age-related macular degeneration | ||||||
|---|---|---|---|---|---|---|
| Participant or population: people with neovascular age-related macular degeneration Settings: clinical centers Intervention: intravitreal injections of bevacizumab Comparison: intravitreal injections of ranibizumab | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No. of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Ranibizumab | Bevacizumab | |||||
| Gain of 15 letters or more visual acuity at one year | 257 per 1000 | 231 per 1000 (188 to 285) | RR 0.90 (0.73 to 1.11) | 2446 (6) | ⊕⊕⊕⊕ high |
|
| Loss of fewer than 15 letters visual acuity at one year | 942 per 1000 | 942 per 1000 (923 to 960) | RR 1.00 (0.98 to 1.02) | 2446 (6) | ⊕⊕⊕⊕ high |
|
| Mean change in visual acuity at one year (number of letters) | The mean change across ranibizumab groups ranged from gains of 3 to 8 letters | The mean change in visual acuity in the bevacizumab groups was on average 0.51 fewer letters gained (95% CI 1.64 fewer letters to 0.62 more letters) | MD −0.51 (−1.64 to 0.62) | 2446 (6) | ⊕⊕⊕⊕ high |
|
| Reduction in central retinal thickness at one year | The mean reduction in central retinal thickness across ranibizumab groups ranged from 30 to 182 μm | The mean reduction in central retinal thickness in the bevacizumab groups was on average 13.97 μm less (95% CI 26.52 less to 1.41 less) | MD −13.97 (−26.52 to −1. 41) | 1995 (4) | ⊕⊕⊕⊕ high |
Two additional trials reported no difference between groups for this outcome; however, these data were not reported in formats that could be included in meta-analysis |
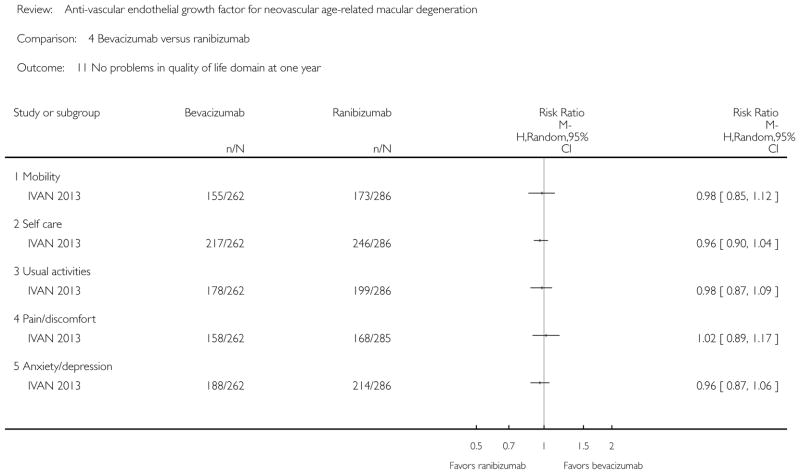
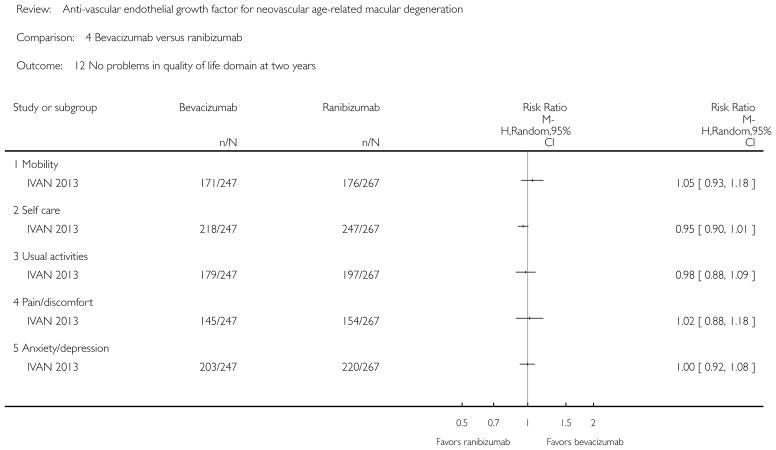
| No problems in quality of life domains at one year | Range of 591 per 1000 to 861 per 1000 across five quality of life domains | Range of 608 per 1000 to 828 per 1000 across five quality of life domains | Range of RRs 0.96 (0.90 to 1.04) to 1.02 (0.89 to 1.17) | 548 (1) | ⊕⊕⊕○ moderate1 |
Quality of life domains included: mobility, self care, usual, activities, pain/discomfort, anxiety/depression |
| Serious systemic adverse events at one year | 139 per 1000 with at least one serious systemic adverse event | 177 per 1000 (148 to 212) | RR 1.27 (1.06 to 1.52) | 2597 (4) | ⊕⊕⊕○ moderate1 |
|
| Serious ocular adverse events at one year | <5 per 1000 | <5 per 1000 | Range of RRs 0.51 (0.05 to 5.62) to 7.05 (0.36 to 136.28) | Range 1670 to 2280 (2 to 3) | ⊕⊕⊕○ moderate1 |
Studies reported different ocular adverse events |
The basis for the assumed risk is estimated by the proportion with the event in the ranibizumab group. The corresponding risk (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI).
CI: confidence interval; RR: risk ratio; MD: mean difference
| The Grading of Recommendations Assessment, Development and Evaluation (GRADE) Working Group grades of evidence: High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. |
Quality of life and adverse event outcomes downgraded to moderate quality as not all eligible trials reported these outcomes and numbers of some adverse events were small (<1%)
BACKGROUND
Description of the condition
Introduction
Age-related macular degeneration (AMD) is a progressive, degenerative disease of the retina that occurs with increasing frequency with age. There are two major types of AMD, commonly referred to as non-neovascular (‘dry’) and neovascular (‘wet’) AMD. The non-neovascular type is characterized by drusen (yellow spots under the retina), pigmentary changes (re-distribution of melanin within the retinal pigment epithelium (RPE) under the retina and migration of melanin into the retina), and geographic atrophy (loss of the RPE and choriocapillaris).
This review concerns neovascular AMD and its treatment. The hallmark of neovascular AMD is choroidal neovascularization (CNV). Breaks in the RPE and Bruch’s membrane allow naturally occurring vessels in the choroid to grow aberrantly into the subretinal space. These choroidal neovascular vessels typically leak and bleed, causing exudative or hemorrhagic retinal detachments. Without treatment, the process usually evolves into a fibrous scar, which replaces the outer layers of the retina, the RPE, and the choriocapillaris. The scarred retina has greatly diminished visual capacity.
Epidemiology
AMD is a leading cause of irreversible vision loss in the elderly in developed countries (Bourne 2014; Bunce 2006; Congdon 2004; Ghafour 1983; Hyman 1987; Leibowitz 1980; Tielsch 1994). While the non-neovascular type is much more common, the neovascular form of AMD is responsible for most cases of severe vision loss. The incidence of progression from non-neovascular AMD to neovascular AMD is increased by the presence of numerous, large and confluent drusen in the macula as well as by the presence of pigment in the macula. Neovascular AMD occurs in only 10% of people with AMD, yet 80% of those with severe visual loss (worse than 20/200 Snellen acuity) have the neovascular form (Leibowitz 1980). Once neovascular disease develops in one eye, the risk of developing neovascular disease in the other eye in the same person is approximately 40% by 5 years (AREDS 2001; SST 20).
The overall prevalence of AMD, in a meta-analysis of studies from Australia, Europe, and the United States, has been estimated at 1.47%(95% confidence interval (CI) 1.38%to 1.55%) (Friedman 2004); however, AMD increases in prevalence with age, with a low incidence among individuals aged less than 50 years. Thus, the burden of disease is greatest in regions where life expectancy is highest. Among those aged 80 years or older, the prevalence of neovascular AMD is estimated to be 5.79% (95% CI 4.72 to 7.01%) in the UK (Owen 2003) and 8.18% (95% CI 7.07% to 9.29%) in the United States (Friedman 2004).
There is no consistent evidence that modifiable factors such as lipid levels, blood pressure, light exposure, or alcohol intake put people at greater risk of developing AMD. One notable exception is smoking (Klein 2008; Mitchell 2002; Smith 1996). Elevated baseline levels of inflammatory biomarkers such as C-reactive protein have been found to be associated with the development of early and late AMD in a large population-based cohort (Boekhoorn 2007). Furthermore, several studies have shown gene-environment interactions of complement factor H with smoking and C-reactive protein (Deangelis 2007; Haddad 2006; Schaumberg 2007; Seddon 2006). High doses of vitamins C and E, beta-carotene, and zinc provide a modest protective effect against the progression to advanced AMD in individuals with extensive drusen or in initially unaffected fellow eyes with neovascular AMD (AREDS 2001; AREDS2 2013).
As the population continues to age, a higher prevalence of this disease is expected in the future, at least in certain populations. A population-based survey estimated AMD, as a contributing cause of blindness, increased worldwide from 4.4% (95% CI 4.0 to 5.1) in 1990 to 6.6% (95% CI 5.9 to 7.9) in 2010 (Bourne 2014).
Presentation and diagnosis
Neovascular AMD may affect one eye or both eyes at the same time or sequentially. The symptoms of neovascular AMD are metamorphopsia (distortions while looking at objects), scotomata (black or gray spots), and blurry vision. Depending upon the location of CNV and the vision in the fellow eye, individuals with AMD may be unaware of the change in visual acuity or may note difficulty with performing normal activities that require good central vision, such as reading and writing, watching television, driving and recognizing faces. When AMD affects only one eye, visual loss may go undetected until monocular testing at a routine eye examination or chance occlusion of the better eye. Frequently, people are unaware that their disturbed binocular vision is caused by changes in only one eye.
A diagnosis of neovascular AMD is made clinically and with the help of imaging such as optical coherence tomography (OCT) and fluorescein angiography, which may be necessary to detect subtle exudation in some individuals who have experienced a recent change in visual acuity. At the onset of symptoms, fundus examination often reveals subretinal exudation of fluid, lipid, or blood. OCT, a non-invasive imaging modality, shows cross-sectional images of the retina, RPE, and choroid. Some studies have defined the characteristic appearance of the different stages of the disease process on OCT (Ting 2002; Van Kerckhoven 2001). The most characteristic findings on OCT corresponding to a CNV lesion include areas of hyporeflectivity under the retina that, in turn, correspond to subretinal fluid, cystic hyporeflective changes consistent with macular edema, and attenuation of the photoreceptor/chorio-capillaris layer. CNV has several characteristic patterns on fluorescein angiography. Classic CNV is defined as an area of early hyperfluorescence with increasing fluorescein leakage on late frames of the angiogram (MPSG 1991). Occult CNV occurs in two different patterns: fibrovascular pigment epithelial detachment and late leakage from an undetermined source. Classic CNV typically has well-demarcated borders, whereas occult CNV usually has poorly demarcated borders.
Another test, indocyanine green (ICG) angiography, may aid in evaluating individuals with neovascular AMD, as it images the choroidal circulation better than fluorescein angiography and may show ‘hot’ spots under the RPE that are amenable to treatment. ICG angiography is particularly useful in the diagnosis of polypoidal choroidal vasculopathy, a form of AMD most common in Asian populations.
Description of the intervention
Until the advent of anti-VEGF agents, treatments most frequently used for neovascular AMD included thermal laser photocoagulation and verteporfin photodynamic therapy (PDT). A Cochrane systematic review concluded that laser photocoagulation effectively slowed the progression of neovascularization in non-subfoveal lesions compared with observation alone (Virgili 2007). A Cochrane review of verteporfin PDT concluded that PDT was effective in preventing clinically significant vision loss (Wormald 2007). However, neither laser photocoagulation or PDT offered any significant chance for vision improvement.
Over the past two decades, researchers have developed new drugs for the treatment of neovascular AMD. These drugs target a protein in the body known as vascular endothelial growth factor (VEGF) that stimulates the growth of the abnormal blood vessels in neovascular AMD in a process called angiogenesis; the drugs block VEGF leading to regression of the abnormal blood vessels. Antiangiogenic therapy is the most commonly used treatment for neovascular AMD, particularly subfoveal neovascular lesions.
An example of an anti-VEGF antagonist is pegaptanib (Macugen®, a trademark of Eyetech/Pfizer, Inc.). Pegaptanib is a chemically synthesized 28-base ribonucleic acid molecule. It is an aptamer (foldable single-strand nucleic acid) and has a capability to change its three-dimensional structure to fit a target protein, in this case VEGF. By binding to VEGF, pegaptanib blocks and inactivates VEGF, thus, halting the process of neovascularization. Pegaptanib was approved for the treatment of neovascular AMD by the Food and Drug Administration (FDA) in the United States in December 2004.
Ranibizumab, previously known as rhuFab-VEGF (Lucentis®, a trademark of Genentech, Inc.), is another example of an anti-VEGF medication developed for ocular administration. It is a humanized antibody fragment capable of binding to the VEGF protein to prevent it from binding to its receptor, thus inhibiting angiogenic activity. Ranibizumab was the first treatment for neovascular AMD that offered a realistic hope for vision improvement; it was approved by the FDA in 2007.
Bevacizumab is another anti-VEGF agent that is used to treat CNV secondary to neovascular AMD. Bevacizumab (Avastin®, a trademark of Genentech, Inc.) is a humanized monoclonal antibody against VEGF. It is the larger parent molecule from which ranibizumab was derived. Bevacizumab is currently approved for the treatment of conditions such as colorectal cancer, but it is widely used by ophthalmologists as an off-label drug for neovascular AMD.
Aflibercept, previously known as VEGFTrap (Eylea®, a trademark of Regeneron Pharmaceuticals, Inc.), is another anti-VEGF agent; the molecule serves as a VEGF decoy to inhibit the growth of new blood vessels. Aflibercept was approved for the treatment of neovascular AMD by the FDA in 2011. Because its mechanism of action is slightly different than those of the drugs listed above (pegaptanib, ranibizumab, and bevacizumab) and it was introduced after the protocol for this review was written, we have not evaluated aflibercept in this review.
How the intervention might work
Angiogenesis is a complex process whereby interactions between stimulatory and inhibitory factors result in new blood vessel formation. These factors have been identified in CNV formation in animal models and human tissue (Aiello 1994; Kvanta 1996; Lopez 1996). Antiangiogenic therapies work either by blocking stimulatory factors or by promoting inhibitory factors, thus disrupting the formation of new vessels. Agents that block the activity of VEGF (anti-VEGFs), a polypeptide with mitogenic effects on endothelial blood vessels, form one type of antiangiogenic therapy. VEGF antagonists have been shown to inhibit CNV in animal models.
In the past, the primary goal of both laser photocoagulation and PDT was to prevent or delay further loss of visual acuity in the treated eye. With the development of agents to counteract VEGF, together known as anti-VEGF agents, the primary goal of the intravitreal injection of these agents is to retain or improve visual acuity. Currently, anti-VEGF agents are administered most commonly via monthly intravitreal injections or as needed after three consecutive monthly injections.
Why it is important to do this review
The previous version of this Cochrane review documented the effectiveness of anti-VEGF agents in halting the loss of visual acuity in a substantial fraction of treated eyes (Vedula 2008). Further, intravitreal injections with ranibizumab led to improvements in vision not previously observed with other AMD treatments. Since this Cochrane review was first published in 2008, numerous studies have been conducted to evaluate the safety and effectiveness of various anti-VEGF agents, treatment modalities, and combination therapies for the treatment of neovascular AMD (Table 1). This review is restricted to: (1) primary RCTs of anti-VEGF agents versus no anti-VEGF treatment; and (2) head-to-head (comparative effectiveness) RCTs of one anti-VEGF agent versus another. Studies of dosage, different treatment strategies, and the combination of anti-VEGF agents with other treatments are outside the scope of this review. The emphasis of this updated review is the stabilization of or improvement in visual acuity with treatment.
Table 1.
Table of Study Acronyms
| Acronym | Details |
|---|---|
| Included studies | |
| ABC | Avastin® (Bevacizumab) in Choroidal Neovascularization Trial |
| ANCHOR | Anti-VEGF Antibody for the Treatment of Predominantly Classic Choroidal Neovascularization in Age-related Macular Degeneration |
| CATT | Comparison of Age-related macular degeneration Treatment Trials |
| GEFAL | French Evaluation Group Avastin® Versus Lucentis® |
| IVAN | A randomized controlled trial of alternative treatments to Inhibit VEGF in Age-related choroidal Neovascularisation |
| MANTA | A Randomized Observer and Subject Masked Trial Comparing the Visual Outcome After Treatment With Ranibizumab or Bevacizumab in Patients With Neovascular Age-related Macular Degeneration Multicenter Anti VEGF Trial in Austria |
| MARINA | Minimally Classic/Occult Trial of the Anti-VEGF Antibody Ranibizumab in the Treatment of Neovascular Age-Related Macular Degeneration |
| PIER | A Phase IIIb, Multicenter, Randomized, Double-Masked, Sham Injection-Controlled Study of the Efficacy and Safety of Ranibizumab in Subjects with Subfoveal Choroidal Neovascularization with or without Classic CNV Secondary to Age-Related Macular Degeneration |
| VISION | VEGF Inhibition Study in Ocular Neovascularization |
| Ongoing studies | |
| BRAMD | Comparison of Bevacizumab (Avastin®) and Ranibizumab (Lucentis®) in Exudative Age-related Macular Degeneration |
| LUCAS | Lucentis® Compared to Avastin® Study |
| MAAM | Avastin® and Macugen® Versus Avastin® Versus Macugen® |
| RATE | Ranibizumab and the Risk of Arterial Thromboembolic Events |
| VIBERA | Prevention of Vision Loss in Patients With Age-Related Macular Degeneration by Intravitreal Injection of Bevacizumab and Ranibizumab |
| Other studies evaluating anti-VEGF therapies for AMD* | |
| ADVANCE | Safety and Efficacy of Oral PTK787 in Patients With Subfoveal Choroidal Neovascularization Secondary to Age-Related Macular Degeneration (NCT00138632) |
| ARMAST | Photodynamic Therapy Combined With Bevacizumab vs Bevacizumab Alone for Neovascular Age-Related Macular Degeneration (NCT00696592) |
| ATLAS | Repeated Eye Injections of Aflibercept for Treatment of Wet Age Related Macular Degeneration (NCT01773954) |
| BEAT-AMD | Systemic Avastin Therapy in Age-Related Macular Degeneration (NCT00531024) |
| BeMOC | Randomised controlled trial of bevacizumab in choroidal neovascularisation secondary to age related macular degeneration (ISRCTN12980412) |
| CARBON | Safety & Efficacy Study Evaluating the Combination of Bevasiranib & Lucentis Therapy in Wet AMD (NCT00557791) |
| CLOVER | Combination Lucentis and Ocular Photodynamic Therapy With Visudyne, With Evaluation-based Retreatment (NCT00680498) |
| COBALT | Safety & Efficacy Study Evaluating the Combination of Bevasiranib & Lucentis Therapy in Wet AMD (NCT00499590) |
| DENALI | Efficacy/Safety of Verteporfin Photodynamic Therapy and Ranibizumab Compared With Ranibizumab in Patients With Subfoveal Choroidal Neovascularization (NCT00436553) |
| EVEREST | Efficacy and Safety of Verteporfin Added to Ranibizumab in the Treatment of Symptomatic Macular Polypoidal Choroidal Vasculopathy (NCT00674323) |
| EXCITE | Efficacy and Safety of Ranibizumab in Patients With Subfoveal Choroidal Neovascularization Secondary to Age-related Macular Degeneration (NCT00275821) |
| EXTEND-I/II/III | Efficacy and Safety of Ranibizumab in Patients With Subfoveal Choroidal Neovascularization Secondary to Age-related Macular Degeneration (NCT00826371; NCT00470678) |
| FOCUS | RhuFab V2 Ocular Treatment Combining the Use of Visudyne® to Evaluate Safety (NCT00056823) |
| GMAN | Greater Manchester Avastin® for choroidal Neovascularisation trial (ISRCTN34221234) |
| HARBOR | A Study of Ranibizumab Administered Monthly or on an As-needed Basis in Patients With Subfoveal Neovascular Age-related Macular Degeneration (NCT00891735) |
| HORIZON | An Open-Label Extension Trial of Ranibizumab for Choroidal Neovascularization Secondary to Age-Related Macular Degeneration (cohort of participants who completed the MARINA, ANCHOR, or FOCUS trials) |
| LAST | A Pilot Study to evaLuate the Role of High-dose rAnbizumab (2.0mg) in the Management of AMD in Patients With perSistent/recurrenT Macular Fluid Less Than 30 Days Following Treatment With Intravitreal Anti-VEGF Therapy (NCT01115556) |
| LOW-VISION | Intravitreal Bevacizumab for Low Vision in Neovascular Age-related Macular Degeneration (NCT01327222) |
| LUV | Lucentis Utilizing Visudyne Combination Therapy in the Treatment of Age-Related Macular Degeneration (NCT00423189) |
| MERLOT | Macular EpiRetinal Brachytherapy Versus Lucentis® Only Treatment (NCT01006538) |
| MONET | Phase II Open Label Multicenter Study For Age Related Macular Degeneration Comparing PF-04523655 Versus Lucentis In The Treatment Of Subjects With CNV (NCT00713518) |
| MONT BLANC | Verteporfin Photodynamic Therapy Administered in Conjunction With Ranibizumab in Patients With Subfoveal Choroidal Neovascularization Secondary to Age-related Macular Degeneration (NCT00433017) |
| NEXUS | Efficacy and Safety Study of iSONEP With and Without Lucentis/Avastin to Treat Age-related Macular Degeneration (NCT01414153) |
| PERSPECTIVES | An Open Label Trial to Investigate Macugen for the Preservation of Visual Function in Subjects With Neovascular AMD (NCT00327470) |
| PrONTO | Prospective Optical coherence tomography imaging of patients with Neovascular AMD Treated with intra-Ocular ranibizumab (NCT00344227) |
| RADICAL | Reduced Fluence Visudyne-Anti-VEGF-Dexamethasone In Combination for AMD Lesions (NCT00492284) |
| SAILOR | Safety Assessment of Intravitreal Lucentis® for Age-Related Macular Degeneration (NCT00251459) |
| SALUTE | Comparison of Safety, Effectiveness and Quality of Life Outcomes Between Labeled Versus “Treat and Extend” Regimen in Turkish Patients With Choroidal Neovascularisation Due to AMD (NCT01148511) |
| SUMMIT | Unclear (clinical trial program including the DENALI, EVEREST, and MONT BLANC trials) |
| SUSTAIN | Study of Ranibizumab in Patients with Subfoveal Choroidal Neovascularization Secondary to Age-Related Macular Degeneration (NCT00331864) |
| VERITAS | A Safety and Efficacy Study Comparing the Combination Treatments of Verteporfin Therapy Plus One of Two Different Doses of Intravitreal Triamcinolone Acetonide and the Verteporfin Therapy Plus Intravitreal Pegaptanib (NCT00242580) |
| VIEW-1/2 | Vascular Endothelial Growth Factor (VEGF) Trap-Eye: Investigation of Efficacy and Safety in Wet Age-Related Macular Degeneration (NCT00509795; NCT00637377) |
| WALTZ | Wet Age-Related Macular Degeneration AL-39324 Treatment Examination (NCT00992563) |
List of studies that may or may not be listed as excluded studies. Clinical trial identifiers are shown in parentheses.
OBJECTIVES
To investigate: (1) the ocular and systemic effects of, and quality of life associated with, intravitreally injected anti-VEGF agents (pegaptanib, ranibizumab, and bevacizumab) for the treatment of neovascular AMD compared with no anti-VEGF treatment; and (2) the relative effects of one anti-VEGF agent compared with another when administered in comparable dosages and regimens.
METHODS
Criteria for considering studies for this review
Types of studies
We included RCTs only.
Types of participants
We included trials in which the participants had neovascular AMD as defined by study investigators.
Types of interventions
We included studies in which anti-VEGF treatment was compared with another treatment, sham treatment, or no treatment. We did not include studies in which different doses of one anti-VEGF treatment were compared with each other, with no control or comparator group. We did not include studies of aflibercept (VEGF Trap-Eye/EYLEA® solution) or studies that used anti-VEGF agents in combination with other treatments.
Types of outcome measures
Primary outcomes
The primary outcome for this review was best-corrected visual acuity (BCVA) at one year of follow up. As all the included RCTs randomized only one eye per participant (i.e., the study eye), we defined the primary outcome for the comparison of treatments as the proportion of participants who gained 15 letters or more (3 lines) of BCVA in the study eye when BCVA was measured on a visual acuity chart with a LogMAR scale.
Secondary outcomes
-
Visual acuity outcomes
Proportion of participants who gained 15 letters or more of BCVA in the study eye at two years of follow up
Proportion of participants who lost fewer than 15 letters of visual acuity
Proportion of participants who lost fewer than 30 letters of visual acuity
Proportion of participants in whom blindness was prevented in the study eye, defined as those eyes with visual acuity better than 20/200
Proportion of participants maintaining visual acuity, defined as gain of 0 letters or more (i.e., no loss of BCVA from baseline)
Mean change in visual acuity
In addition to visual acuity outcomes, the following secondary outcomes were considered
Contrast sensitivity, reading speed, or any other validated measure of visual function as measured in the included studies
Assessment of morphological characteristics by fluorescein angiography or OCT, including mean change in size of CNV, mean change in size of total lesion, and mean change in central retinal thickness (CRT)
Quality-of-life measures, as assessed with any validated measurement scale
Economic data, such as comparative cost analyses
Ocular or systemic adverse outcomes
Follow up
We included trials in which participants were followed for at least one year. We also included outcomes at two years of follow up when data were available.
Search methods for identification of studies
Electronic searches
We searched CENTRAL (which contains the Cochrane Eyes and Vision Group Trials Register) (2014, Issue 3), Ovid MEDLINE, Ovid MEDLINE In-Process and Other Non-Indexed Citations, Ovid MEDLINE Daily, Ovid OLDMEDLINE (January 1946 to March 2014), EMBASE (January 1980 to March 2014), Latin American and Caribbean Health Sciences Literature Database (LILACS) (January 1982 to March 2014), the metaRegister of Controlled Trials (mRCT) (www.controlled-trials.com), ClinicalTrials.gov (www.clinicaltrials.gov) and the World Health Organization (WHO) International Clinical Trials Registry Platform (ICTRP) (www.who.int/ictrp/search/en). We did not use any date or language restrictions in the electronic searches for trials. We last searched the electronic databases on 27 March 2014.
See: Appendices for details of search strategies for CENTRAL (Appendix 1), MEDLINE (Appendix 2), EMBASE (Appendix 3), LILACS (Appendix 4), mRCT (Appendix 5), ClinicalTrials.gov (Appendix 6) and the ICTRP (Appendix 7).
Searching other resources
We reviewed the reference lists of included trial reports and related systematic reviews to identify additional potentially relevant trials. We contacted pharmaceutical companies conducting studies on anti-VEGF drugs for information about any ongoing or completed clinical trials not published. One author (SSV) handsearched abstracts from the annual meetings of the Association for Research in Vision & Ophthalmology (ARVO) for the years 2006 and 2007 for ongoing trials (http://files.abstractsonline.com/SUPT/163/1807/PresentationTitle.htm; http://files.abstractsonline.com/SUPT/163/1601/Presentation_Title_PDF_wlinks.htm accessed November 24, 2007). After 2007, the Cochrane Eyes and Vision Group began handsearching conference abstracts reporting clinical trials and the identified trial records are listed in CENTRAL. Another author (KL) handsearched abstracts from the 2006 annual meeting of the European VitreoRetinal Society (http://www.evrs.eu/2006-evrs-congress-cannes/ accessed November 27, 2012). For future updates of this review, we will consider handsearching abstracts for the following conferences when they have not been searched by the Cochrane Eyes and Vision Group: ARVO; Macula Society; Retina Society; subspecialty meetings from the American Academy of Ophthalmology meeting; American Society of Retinal Surgeons; and European VitreoRetinal Society.
Data collection and analysis
Selection of studies
Two review authors independently evaluated the titles and abstracts resulting from the electronic searches. We classified each record as ‘definitely relevant’, ‘possibly relevant’, or ‘definitely not relevant’; a third review author resolved discrepancies. We obtained full-text reports for all records assessed as ‘definitely relevant’ or ‘possibly relevant’. Two review authors independently assessed the full-text reports and classified each study as ‘include’, ‘exclude’, ‘awaiting classification’, or ‘ongoing’; a third review author resolved discrepancies. For trials identified by handsearching conference abstracts, a second author verified eligibility based on the stated criteria. We contacted authors to clarify any details necessary to make a complete assessment of the relevance of the study. We documented studies excluded after review of the full-text report and noted the reasons for exclusion.
Data extraction and management
Two review authors independently extracted study characteristics, including details of study methods, participants, interventions, outcomes, and funding resources, using data collection forms developed specifically for this purpose. We contacted the trial authors for data on primary and secondary outcomes in the individual trials when the information was not clearly available from published reports. We extracted data on visual acuity, adverse events, and other outcomes for the two trials forming part of the VISION 2004 study from documents available on the FDA website. We also extracted data from figures published in the trial reports and communicated with the authors to verify extracted data. One author entered data into Review Manager (RevMan 2012), and a second author verified the data entry.
Assessment of risk of bias in included studies
Two review authors assessed potential sources of bias in trials according to methods set out in Chapter 8 of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). The following parameters were considered: random sequence generation and method of allocation concealment (selection bias), masking of participants and researchers (performance bias), masking of outcome assessors (detection bias), rates of losses to follow up and non-compliance as well as failure to include analysis of all participants after randomization (attrition bias), reporting bias, and other potential sources of bias. We judged each potential source of bias as low risk, unclear risk, or high risk. We contacted authors of trials for additional information when descriptions of study methods needed to assess bias domains were unclear or not reported.
Measures of treatment effect
Data analysis was guided by Chapter 9 of the Cochrane Handbook for Systematic Reviews of Interventions (Deeks 2011). The primary outcome and some secondary outcomes for this review related to BCVA in the study eye. We analyzed visual acuity, measured on LogMAR charts, as both dichotomous and continuous outcomes. We calculated the risk ratios (RRs) with 95% confidence intervals (CIs) for dichotomous outcomes. Dichotomous visual acuity outcomes included: proportion of participants who gained 15 letters or more (same as a gain of 3 lines or more) of visual acuity; proportion of participants who lost fewer than 15 letters (same as fewer than 3 lines) of visual acuity; proportion of participants who lost fewer than 30 letters (same as fewer than 6 lines) of visual acuity; proportion of participants not blind (defined as visual acuity better than 20/200); and proportion of participants maintaining visual acuity (same as gain of 0 letters or more). We calculated the mean difference (MD) in mean change of visual acuity from baseline as a continuous visual acuity outcome.
Secondary outcomes relating to visual function and morphology of CNV also included both dichotomous and continuous outcomes. We calculated RRs with 95% CIs for dichotomous outcomes and MDs with 95% CIs for continuous outcomes. Contrast sensitivity outcomes, measured by Pelli-Robson charts, were reported both dichotomously (proportion of participants with a gain of 15 letters or more of contrast sensitivity) and continuously (mean number of letters of contrast sensitivity). We calculated MDs with 95% CIs for near visual acuity and reading speed outcomes when sufficient data were available.
Continuous morphological outcomes included mean change in size of CNV, mean change in size of lesion, and mean change in CRT. We included one dichotomous morphological outcome, which was the resolution of subretinal or intraretinal fluid based on OCT evaluation.
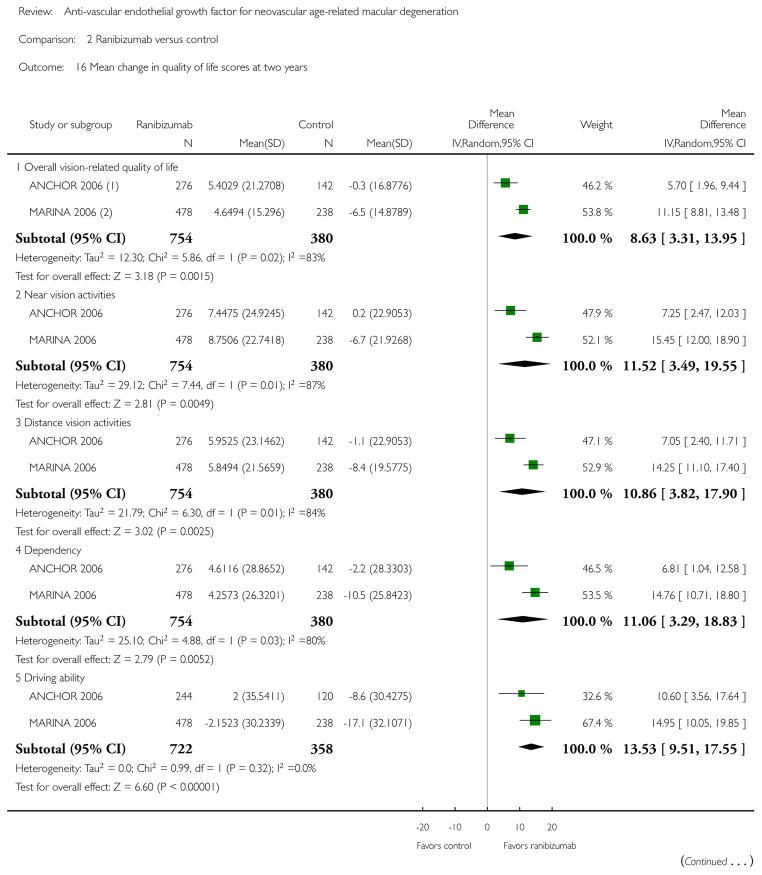
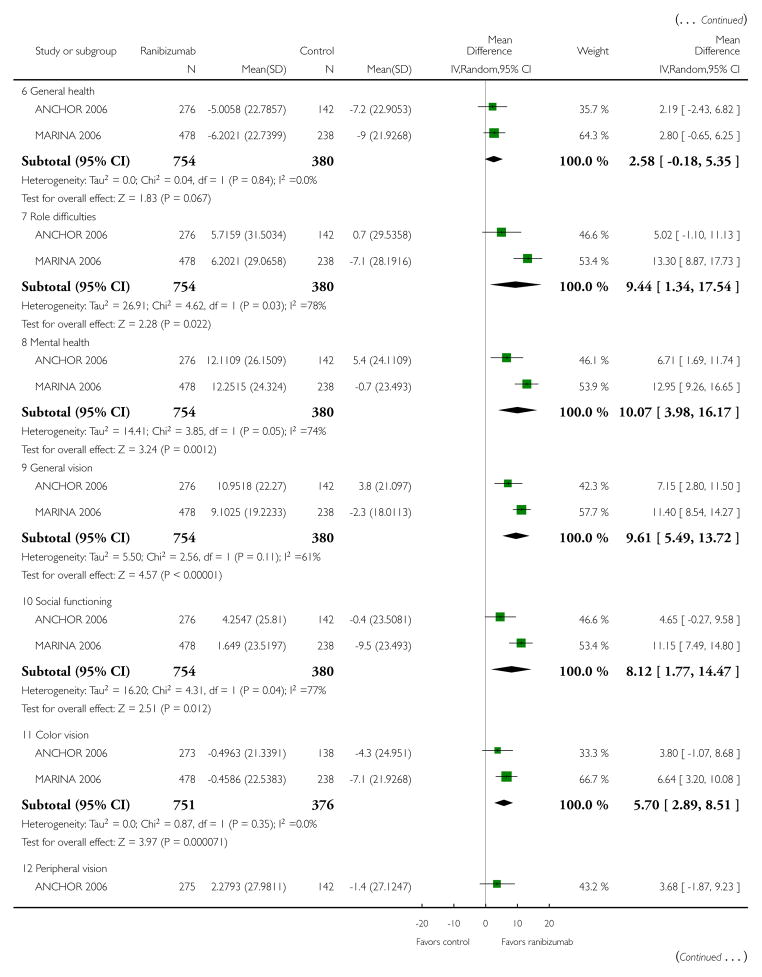
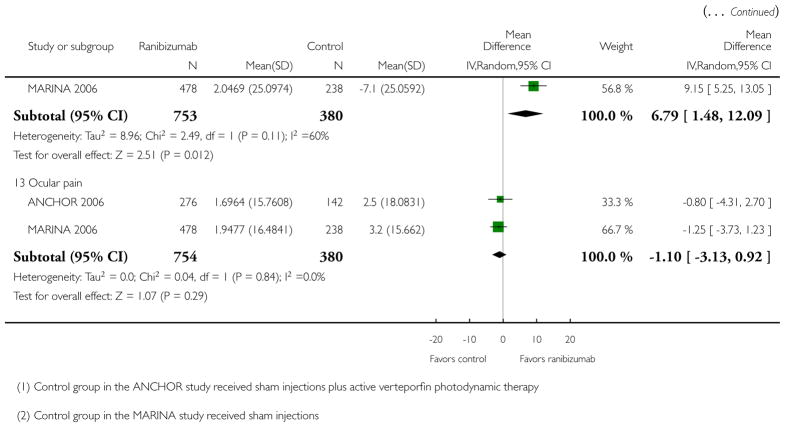
We analyzed quality-of-life scores as continuous outcomes. Because the trials that reported quality-of-life outcomes included in meta-analyses used the same scale, we did not need to calculate standardized mean differences.
We reported adverse events as RRs with 95% CIs when sufficient data were available. Otherwise we reported the numbers of participants experiencing adverse events in narrative and tabular form.
Unit of analysis issues
The unit of analysis was the individual (one study eye per participant).
Dealing with missing data
We used multiple sources to identify relevant data for this review, such as journal publications, conference abstracts, FDA documents, and clinical trial registries. When data were unclear (e.g., data were extracted from graphs or derived from percentages), we contacted study investigators for verification. When data were missing, we contacted study investigators for additional information. If no response was received within two weeks, we attempted to contact them again. Whenever no response was received by six weeks after the first attempt, we used the data as available.
For outcome data, we used the data as reported in the trial reports or as supplied by the primary investigators. We noted the number of participants with missing data and the statistical methods used in the individual studies to analyze data (e.g., available case analysis, last-observation-carried-forward, etc.). We did not impute missing outcome data for our analyses.
Assessment of heterogeneity
We assessed statistical heterogeneity based on the Chi2 test, I2 statistic and the overlap of CIs in the forest plots. We considered a Chi2 P value of < 0.10 to represent significant statistical heterogeneity and an I2 statistic of 60% or more to represent substantial statistical heterogeneity. We assessed clinical and methodological heterogeneity among studies by comparing the study populations, interventions, and methods of each study.
Assessment of reporting biases
We assessed selective outcome reporting for each study by comparing the outcomes specified in a protocol, research plan, or clinical trial registry with the results reported. When protocols, research plans, or clinical trial registry records were not available, we assessed selective outcome reporting based on the outcomes specified in the methods section of the study report and the data that were collected as described in the study design. In further updates of this review, whenever 10 or more studies are included in a meta-analysis, we will use a funnel plot to judge publication bias.
Data synthesis
Statistical analyses were performed using RevMan 2012. We did not combine studies in meta-analysis when we identified clinical or methodological heterogeneity (e.g., different anti-VEGF agents or outcome time points); instead we either analyzed data by type of anti-VEGF agent and time point or, when data were not sufficient for meta-analysis, we reported a narrative summary. We used a random-effects model for all analyses. When the I2 statistic was 60% or greater, suggesting substantial statistical heterogeneity, we assessed the direction of treatment effects across studies and the overlap of the CIs to determine whether meta-analysis was appropriate. We did not adjust estimates of treatment effects to account for comparisons of different doses of an anti-VEGF agent to a single control group, as observed in several studies.
Subgroup analysis and investigation of heterogeneity
In the previously published version of this review we conducted subgroup analyses of the primary outcome, as specified in the protocol, by stratifying the data according to the angiographic subtype of CNV using the definitions adopted in the included trials (Vedula 2008). Because we changed the primary outcome to a gain of 15 letters or more of visual acuity for this version of the review, we did not conduct these subgroup analyses as data were insufficient. If data by angiographic subtype of CNV are available for inclusion in future updates to this review, we will include these subgroup analyses.
Sensitivity analysis
In an earlier published version of this review we conducted sensitivity analyses to examine potential bias caused by missing data from participants excluded after randomization or lost to follow up in analyses for the primary outcome. We did this by analyzing the primary outcome assuming that: 1) participants lost to follow up had lost 15 letters or more of visual acuity (worst-case analysis); and 2) participants did not lose 15 letters or more of visual acuity at one year follow up (best-case analysis) (Vedula 2008). Because these analyses did not alter the conclusions of the review, we did not conduct these sensitivity analyses for this version of the review and do not plan to conduct them in future updates.
We planned to conduct sensitivity analyses to assess the impact of studies graded as having a high risk of bias on any parameter, unpublished data only, or industry funding. After assessing the data collected, we determined these analyses were not needed because studies within each meta-analysis did not differ based on these factors.
RESULTS
Description of studies
Results of the search
The electronic searches for the first published version of this review (conducted in August 2005, October 2006, June 2007 and February 2008) resulted in the identification of a total of 1407 titles and abstracts (Vedula 2008). We selected 36 records for full-text review, and identified five trials described in 10 reports for inclusion in the review (ANCHOR 2006; EOP 1003; EOP 1004; FOCUS 2006; MARINA 2006). We excluded 16 studies (24 reports) and listed two additional studies identified through the handsearching of abstracts as awaiting classification. Acronyms used to refer to the studies in this review are listed in Table 1.
Two concurrent, randomized trials that used individual participant data meta-analyses under the acronym VISION were identified (Gragoudas 2004), an international trial (EOP 1003) and a North American trial (EOP 1004). In the first published version of this review, we assessed the data from these two trials separately and analyzed them according to the original protocol of the review. We obtained the data for the primary and secondary outcomes for the two trials from the information available on the FDA website and by contacting the authors. For this update we considered the two trials as one study, VISION 2004, and collected new data from published articles as available. The characteristics of the two individual trials are summarized in Appendix 8 and Appendix 9. For this update, we also refined the eligibility criteria to exclude studies in which anti-VEGF treatment was given in combination with other AMD treatments and to include trials in which two anti-VEGF agents had been compared (i.e., head-to-head trials). Combination therapies for AMD will be covered in a separate Cochrane review. Thus, we did not include the FOCUS 2006 trial, which compared ranibizumab with PDT versus PDT alone and was included in the first version of this review, in this update of the review.
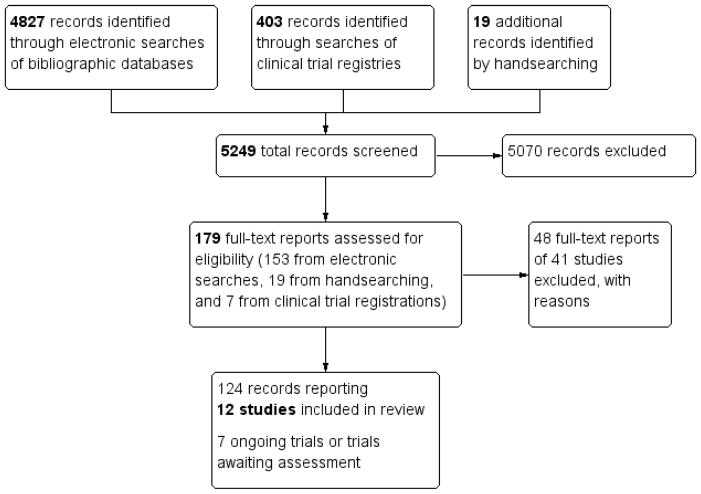
We conducted updated electronic searches in September 2008, April 2011, February 2013, and March 2014. Because we modified the eligibility criteria and new authors joined the review team, we combined all search results and assessed the records as a new review. In all, there were 4827 unique records from electronic searches of bibliographic databases, 403 clinical trial registrations, and 19 additional records identified by the handsearching of conference abstracts (Figure 1). From the bibliographic databases, we identified 153 records for full-text review. Of these 153 records, we included 12 RCTs (reported in 108 records) and excluded 39 studies (reported in 45 records). We excluded two additional studies from three records identified by handsearching. We list the reasons for exclusion of each of the 41 studies in the ‘Characteristics of excluded studies’ table. We included the remaining 16 records identified by handsearching as additional reports of the included studies. We identified seven additional studies from the search of clinical trial registries, one of which is awaiting classification due to insufficient information to determine eligibility and six are ongoing (or completed with results not yet published). Descriptions of studies awaiting classification and those that are ongoing are available in the Characteristics of studies awaiting classification section and the Characteristics of ongoing studies section, respectively.
Figure 1.
Study flow diagram. Results of searches as of 27 March 2014.
Table 9.
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Bashshur 2007 | Follow up less than one year: 6 months; RCT of 32 participants treated with bevacizumab or verteporfin PDT for neovascular AMD |
| BEAT-AMD 2009 | Follow up less than one year: 6 months; RCT of 16 participants treated with systemic bevacizumab or placebo for neovascular AMD |
| Bolz 2008 | Dosing study: 0.3 mg or 0.5 mg intravitreal ranibizumab; method of allocation not clear |
| Cohen 2008 | Not a RCT: cost-effectiveness assessment |
| Costagliola 2010 | Combination therapy: intravitreal bevacizumab alone versus intravitreal bevacizumab plus low-fluence PDT |
| Earnshaw 2007 | Not a RCT: cost-effectiveness assessment |
| Erdokur 2009 | Not a RCT: retrospective cohort study of 88 participants who received either PDT monotherapy, intravitreal bevacizumab monotherapy, or combination PDT plus intravitreal bevacizumab therapy |
| EXTEND-I 2008 | Dosing study: 0.3 mg or 0.5 mg intravitreal ranibizumab |
| Eyetech Study 2003 | Not a RCT: phase II uncontrolled study of 21 participants treated with intravitreal anti-VEGF therapy with or without PDT |
| Falkenstein 2007 | Not a RCT: cohort study of 38 participants receiving primary versus secondary bevacizumab |
| Fletcher 2008 | Not a RCT: cost-effectiveness assessment |
| FOCUS 2006 | Combination therapy: intravitreal ranibizumab alone versus intravitreal ranibizumab plus verteporfin PDT |
| Hahn 2007 | Follow up less than one year: 3 months; RCT of 30 participants treated with standard light fluence PDT plus intravitreal triamcinolone, reduced light fluence PDT plus intravitreal triamcinolone, or intravitreal bevacizumab |
| Hatta 2010 | Not a RCT: 242 participants selected treatment with PDT alone, PDT with sub-tenon injection of triamcinolone acetonide, or PDT with intravitreal bevacizumab |
| Heier 2006 | Follow up less than one year: 3 months; RCT of 64 participants treated with intravitreal ranibizumab or usual care; after 3 months, participants could select their treatment method |
| Hernandez-Pastor 2008 | Not a RCT: cost-effectiveness assessment |
| Hernandez-Pastor 2010 | Not a RCT: cost-effectiveness assessment |
| Javitt 2008 | Not a RCT: cost-effectiveness assessment |
| Lai 2009 | Dosing study: 1.25 mg (n = 24) or 2.5 mg (n = 26) intravitreal bevacizumab; follow up less than one year: 6 months |
| Lazic 2007 | Follow up less than one year: 3 months; RCT of 165 participants treated with PDT, intravitreal bevacizumab, or combination PDT with intravitreal bevacizumab |
| Li 2012 | Dosing study: 6 week (n = 91) or 12 week (n = 94) injection schedule following first three injections of intravitreal bevacizumab |
| Li 2013 | Not a RCT: historical cohort of 28 participants treated with intravitreal bevacizumab from 2008 to 2009 compared with 32 participants treated with intravitreal ranibizumab from 2010 to 2012 |
| Matthe 2011 | Not a RCT: historical cohort of 88 participants treated with intravitreal ranibizumab followed by pegaptanib injections or intravitreal ranibizumab injections only |
| MIRA-1 2005 | Did not include participants with neovascular AMD: RCT of 43 participants with non-exudative AMD; compared rheopheresis versus placebo |
| Modarres 2009 | Dosing study: 1.25 mg (n = 47) or 2.5 mg (n = 39) intravitreal bevacizumab |
| Neubauer 2007 | Not a RCT: statistical modeling using ANCHOR 2006 and MARINA 2006 cost data |
| Nguyen 2006 | Follow up less than one year: 99 days; RCT of 25 participants treated with VEGF Trap® (aflibercept) or placebo |
| Nowak 2012 | Not a RCT: case series of 426 consecutive participants treated with verteporfin PDT, intravitreal bevacizumab, or transpupillary thermotherapy based on angiographic subtypes |
| Parodi 2012 | Follow up less than one year: 6 months; RCT comparing intravitreal bevacizumab versus observation in participants with advanced-stage neovascular AMD |
| PERSPECTIVES 2012 | Not a RCT: cohort of participants receiving pegaptanib sodium for 102 weeks |
| Raftery 2007 | Not a RCT: cost-effectiveness assessment |
| SAILOR 2009 | Dosing study: 0.3 mg (n = 1169) or 0.5 mg (n = 1209) intravitreal ranibizumab |
| Schmid-Kubista 2011 | Follow up less than one year: 6 months; RCT comparing sequential administration of intravitreal bevacizumab and pegaptanib versus treatment with intravitreal bevacizumab or pegaptanib alone |
| SUMMIT 2007 | Combination therapy: three RCTs comparing intravitreal ranibizumab alone versus intravitreal ranibizumab plus PDT; DENALI (trial in the United States and Canada), EVEREST (trial in Asia), and MONT BLANC (trial in Europe) |
| Suñer 2009 | Not a RCT: validation of NEI Visual Function Questionnaire using ANCHOR 2006 and MARINA 2006 data |
| Tano 2008 | Dosing study: 0.3 mg (n = 47) or 1.0 mg (n = 48) pegaptanib sodium |
| Vallance 2010 | Combination therapy: RCT of intravitreal ranibizumab + sham PDT versus intravitreal ranibizumab + standard-fluence verteporfin PDT |
| VERITAS 2006 | Combination therapy: RCT of verteporfin PDT plus one of two doses of intravitreal triamcinolone (1 mg or 4 mg) versus verteporfin PDT plus intravitreal pegaptanib |
| VIEW 2014 | Aflibercept study: two RCTs of intravitreal aflibercept versus intravitreal ranibizumab with two-year follow up; excluded from this review as aflibercept for treatment of AMD was not eligible for this review |
| Wolowacz 2007 | Not a RCT: cost-effectiveness assessment |
| Zehetner 2013 | Follow up less than one year: 1 month; RCT to evaluate plasma VEGF levels of 30 participants randomized to bevacizumab, ranibizumab or pegaptanib |
Study acronyms: see Table 1
AMD: age-related macular degeneration
NEI: National Eye Institute, National Institutes of Health, USA
PDT: photodynamic therapy
RCT: randomized controlled trial
VEGF: vascular endothelial growth factor
Table 10.
Characteristics of studies awaiting assessment [ordered by study ID]
| NCT00087763 | |
| Methods |
Study design: phase 2 RCT Planned enrollment: 135 participants Length of follow-up: 54 weeks |
| Participants |
Inclusion criteria: age 50 or older; subfoveal CNV secondary to AMD; total lesion size ≤ 12 disk areas and ≥ 50% active CNV; foveal thickness ≤ 300 μm; BCVA of 20/40 to 20/320 in study eye and ≥20/800 in non-study eye Exclusion criteria: subfoveal atrophy, scarring, blood over fovea, or fibrosis; > 25% of lesion size with scarring or atrophy; history of subfoveal thermal laser therapy or PDT |
| Interventions |
Intervention 1: intravitreal pegaptanib (0.3 mg or 1.0 mg) Intervention 2: sham control |
| Outcomes | Not reported |
| Notes |
Study name: A Phase II Prospective, Randomized, Double-Masked, Sham-Controlled, Dose-Ranging, Multi-Center Trial to Assess the Effect of Pegaptanib Sodium on Foveal Thickening in Patients With Exudative Subfoveal Age- Related Macular Degeneration (AMD) (EOP1009) Study objective: “The purpose of this study is to determine if Macugen™ reduces foveal thickness and improves vision in patients with wet AMD.” Study dates: start date of March 2004; primary completion date of May 2006 Sponsors/Collaborators: Eyetech Pharmaceuticals, Pfizer |
AMD: age-related macular degeneration
BCVA: best-corrected visual acuity
CNV: choroidal neovascularization
PDT: photodynamic therapy
RCT: randomized controlled trial
Table 11.
Characteristics of ongoing studies [ordered by study ID]
| NCT00531336 | |
| Trial name or title | Avastin and Macugen Versus Avastin Versus Macugen (MAAM) |
| Methods |
Study design: phase 2 RCT Planned enrollment: 60 participants Length of follow-up: 54 weeks |
| Participants |
Inclusion criteria: age 50 years or older; predominantly occult CNV; lesion size < 5400 μm; distance acuity > 0.1 Exclusion criteria: previous treatment for CNV; intraocular surgery within 4 weeks; vision threatening diseases other than CNV; general disorders that may affect the healing process; unwillingness to consent |
| Interventions |
Intervention 1: 1.25 mg intravitreal bevacizumab administered once, followed by 0.3 mg intravitreal pegaptanib administered every 6 weeks Intervention 2: 1.25 mg intravitreal bevacizumab administered every 6 weeks Intervention 3: 0.3 mg intravitreal pegaptanib administered every 6 weeks |
| Outcomes |
Primary outcome, as defined: retinal thickness at 54 weeks Secondary outcomes, as defined: distance acuity at 54 weeks; number of adverse events at 54 weeks |
| Starting date | July 2006; primary completion date of December 2008 |
| Contact information | Ilse Krebs, MD Ludwig Boltzmann Institute for Biomicroscopic Lasersurgery Vienna, Austria, A1030 |
| Notes | “In this pilot study, the safety (number of adverse events) and efficacy (distance acuity testing retinal thickness measurement) of Avastin and Macugen applied as monotherapy will be compared to a combined treatment of Avastin followed by Macugen used for retreatment.” Sponsors/Collaborators: The Ludwig Boltzmann Institute of Retinology and Biomicroscopic Laser Surgery |
| NCT00559715 | |
| Trial name or title | Prevention of Vision Loss in Patients With Age-Related Macular Degeneration (AMD) by Intravitreal Injection of Bevacizumab and Ranibizumab (VIBERA) |
| Methods |
Study design: phase 3 RCT Planned enrollment: 366 participants Length of follow-up: 2 years |
| Participants |
Inclusion criteria: age 50 years or older; visual impairment due to active primary or recurrent CNV associated with AMD; classical or predominantly classic lesion with largest diameter of the subretinal neovascular membrane smaller than greatest distance between major temporal vascular arcades, minimally classic lesion, or occult lesion with no classic CNV; BCVA of 20/40 to 20/320 Exclusion criteria: subretinal hemorrhage involving ≥ 50% of the lesion area or ≥ 1 optic disk areas; subfoveal fibrosis or atrophy; CNV of other pathogenesis; previous treatment for CNV or treatment with any antiangiogenic drugs; previous intravitreal drug delivery, laser photocoagulation, vitreoretinal surgery, submacular surgery, or other surgical intervention for AMD in the study eye; retinal pigment epithelial tear; active inflammation, vitreous hemorrhage, infectious conjunctivitis, keratitis, scleritis, or endophthalmitis; history of rhegmatogenous retinal detachment, macular hole, idiopathic or autoimmune-associated uveitis, or corneal transplant; aphakia or lack of posterior capsule in the study eye; > −8 diopters of myopia; any intraocular condition that requires surgery or could lead to vision loss within 2 years; intraocular surgery in study eye within 2 months; uncontrolled glaucoma or history of glaucoma filtering surgery; impaired visualization of the retina precluding adequate diagnosis; premenopausal women not using adequate contraception or nursing; active systemic infection or other disease, dysfunction, or finding to contraindicate participation; hypersensitivity to study drugs or allergy to agents used for ocular testing; involvement in another clinical study within 4 weeks; unwillingness or inability to comply with study |
| Interventions |
Intervention 1: 1.25 mg intravitreal bevacizumab administered monthly or on demand Intervention 2: 0.5 mg intravitreal ranibizumab administered monthly or on demand |
| Outcomes |
Primary outcome, as defined: proportion of participants losing fewer than 15 letters at 1 year Secondary outcomes, as defined: proportion of participants losing fewer than 15 letters at 2 years; mean change in BCVA at 1 and 2 years; proportion of participants with at least 3 months treatment-free in 2 years; number of doses of study drugs at 2 years; rate of drop-out at 2 years; number of non-responders at 2 years; retinal lesions at 2 years; adverse events at 2 years; quality of life at 2 years |
| Starting date | August 2008; primary completion date of August 2009 |
| Contact information | Bernd Muehlbauer, Professor MD Department of Pharmacology at Klinikum Bremen Mitte Bremen, Germany, 28177 |
| Notes | “The study is designed to demonstrate the therapeutic non-inferiority of the recombinant humanized monoclonal VEGF antibody bevacizumab administered by intravitreal injection in the treatment of AMD in comparison to the related fragment ranibizumab.” Sponsors/Collaborators: Klinikum Bremen-Mitte, gGmbH; Kompetenzzentrum für Klinische Studien, Bremen |
| NCT01127360 | |
| Trial name or title | Lucentis Compared to Avastin Study (LUCAS) |
| Methods |
Study design: phase 4 RCT Planned enrollment: 420 participants Length of follow-up: 2 years |
| Participants |
Inclusion criteria: age 50 years or older; unilateral or bilateral neovascular AMD (one study eye eligible in bilateral cases); untreated CNV including retinal angiomatous proliferation, with edema involving the fovea as assessed by fluorescein angiography and OCT; BCVA of 20/25 to 20/320 Exclusion criteria: subretinal hemorrhage and/or fibrosis involving ≥ 50% of the lesion area; CNV of other pathogenesis; previous treatment for CNV; history of anti-VEGF treatment in non-study eye within 4 weeks; intraocular surgery or laser treatment within 3 months; infection in either eye; active uveitis or intraocular inflammation; retinal disease that may lead to vision loss in the study eye; impaired visualization of the retina precluding adequate diagnosis; IOP ≥25 mmHg or uncontrolled glaucoma; cataract requiring surgery within 2 years; history of treatment with systemic anti-VEGF drugs; premenopausal women not using adequate contraception or nursing; mentally or physically unable to participate; serious disease with probability of death during the study; involvement in another clinical study or use of investigational drugs |
| Interventions |
Intervention 1: 25 mg/mL intravitreal bevacizumab administered following the “inject and extend” principle Intervention 2: 10 mg/mL intravitreal ranibizumab administered following the “inject and extend” principle |
| Outcomes |
Primary outcome, as defined: mean change in visual acuity at 1 and 2 years, as measured on an ETDRS chart (non-inferiority limit of 5 letters) Secondary outcomes, as defined: number of treatments at 1 and 2 years; proportions of participants losing fewer than 15 letters at 1 and 2 years, as measured on an ETDRS chart; macular morphology at 2 years, as measured by fluorescein angiography and OCT; adverse events at 2 years; number of non-responders at 2 years |
| Starting date | March 2009; primary completion date of July 2013 |
| Contact information | Karina Berg, MD Department of Ophthalmology, Oslo University Hospital Oslo, Norway, 0407 |
| Notes | “The goal of the study is to demonstrate if the two agents are equivalent regarding both efficacy and safety.” Sponsors/Collaborators: Ullevaal University Hospital |
| NCT01319188 | |
| Trial name or title | Ranibizumab and the Risk of Arterial Thromboembolic Events (RATE) |
| Methods |
Study design: phase 4 RCT Planned enrollment: 380 participants Length of follow-up: 2 years |
| Participants |
Inclusion criteria: age 50 years or older; untreated AMD with lesion size < 12 disk areas for minimally classic or occult lesions and < 5400 μm for predominantly classic lesions; BCVA of 20/40 to 20/320 on ETDRS scale Exclusion criteria: permanent structural damage to foveal center; history of cardiovascular events or cerebrovascular events within 6 months; stenting or surgery within 6 months; III-IV New York Heart Association functional class of heart failure; acute illnesses within 3 months; mental or brain disorders; blood disorders; malignant tumors; pregnancy; family history of hypercholesterolemia; involvement in another clinical study or use of investigational drugs within 3 months |
| Interventions |
Intervention 1: 0.50 mg intravitreal ranibizumab administered every 4 weeks for 6 months, then every 3 months Intervention 2: 0.50 mg intravitreal ranibizumab plus PDT Intervention 3: sham injection |
| Outcomes |
Primary outcome, as defined: arterial thromboembolic events rate at 6, 12, and 24 months (includes all-cause mortality, non-fatal stroke, non-fatal myocardial infarction, and vascular death) Secondary outcomes, as defined: serum concentration of ranibizumab, VEGF, fibrinogen, C-reactive protein, and D-dimer at 6, 12, and 24 months; mean change in visual acuity at 6, 12, and 24 months; coronary and/or cerebral stenting, and/or coronary artery bypass graft rate at 6, 12, and 24 months; total cholesterol and systolic blood pressure at 6, 12, and 24 months; New York Heart Association functional class of heart failure at 6, 12, and 24 months; diabetes mellitus morbidity at 6, 12, and 24 months |
| Starting date | June 2010; primary completion date of August 2012 |
| Contact information | Alexander Kharlamov Ural Institute of Cardiology, Ural State Medical Academy Yekaterinburg, Russian Federation, 620144 |
| Notes | “The main objective of study is to reveal contraindications for ranibizumab prescription in patients with history of coronary artery disease and cerebrovascular events.” Sponsors/Collaborators: Ural Institute of Cardiology, Ural State Medical Academy |
| NCT02036723 | |
| Trial name or title | Safety and Efficacy Study of BCD-021 Compared to Lucentis in Patients With Neovascular Wet Age-related Macular Degeneration (GALATIR) |
| Methods |
Study design: phase 3 RCT Planned enrollment: 108 participants Length of follow-up: 12 months |
| Participants |
Inclusion criteria: age 50 years or older; neovascular AMD in the study eye (one study eye per participant); untreated CNV including retinal angiomatous proliferation, with edema involving the fovea as assessed by fluorescein angiography and OCT; BCVA of 20/32 to 20/320; size of lesion < 12 disc areas; if occult neovessels, proof of recent development of lesion Exclusion criteria: subretinal hemorrhage involving ≥50% of the lesion area, fibrosis or retrofoveal retinal atrophy, or retinal pigment epithelial tear reaching the macula in the study eye; CNV of other pathogenesis; previous treatment for CNV; history or current use of anti-VEGF treatment; other treatment in study eye within 3 months; history of vitrectomy, photocoagulation, corneal graft or medical devices in study eye; infection, active uveitis or intraocular inflammation; retinal disease that may lead to vision loss in the study eye; impaired visualization of the retina precluding adequate diagnosis; IOP ≥25 mmHg or uncontrolled glaucoma; aphakia; myopia > −8 diopter; allergy to treatments or testing agents; uncontrolled arterial hypertension; immunodeficiency, syphilis, HIV, hepatitis B, or history of hepatitis C virus; history of malignant neoplasm; history of treatment with systemic bevacizumab; premenopausal women not using adequate contraception, pregnant, or nursing; mentally unable to participate; drug addiction or alcoholism; involvement in another clinical study currently or within 3 months |
| Interventions |
Intervention 1: 1.25 mg intravitreal BCD-021 (bevacizumab biosimilar manufactured by CJSC BIOCAD, Russia) administered on day 1, then every 28 days for 12 months Intervention 2: 0.50 mg intravitreal ranibizumab administered on day 1, then every 28 days for 12 months |
| Outcomes |
Primary outcome, as defined: proportion of participants losing fewer than 15 letters on EDTRS chart at 12 months Secondary outcomes, as defined: frequency of ocular and systemic adverse events (AE) and serious adverse events (SAE) related to AMD therapy at 12 months; frequency of AE and SAE with toxicity level of 3–4 related to AMD therapy at 12 months; number of cases of early withdrawal from the study caused by AE or SAE at 12 months; number of participants who have binding and neutralizing antibodies to BCD-021/Lucentis in serum at screening and 12 months; mean titer of binding and neutralizing antibodies to BCD- 021/Lucentis in serum at screening and 12 months; mean number of injections and time before re-injection at 12 months; lesion size at 6 months and 12 months; lesion leakage at 6 months and 12 months; change in fluid and foveal thickness on OCT at 12 months; retinal sensitivity measured by microperimetry at screening, 6 months and 12 months; timing of visual improvement after initiation of therapy up to 12 months |
| Starting date | March 2014; primary completion date of March 2016 |
| Contact information | Roman Ivanov, PhD Vice President, Research & Development Biocad, Russia |
| Notes | “The purpose of the study is to demonstrate the non-inferiority of efficacy and safety of BCD-021 compared to Lucentis.” Sponsors/Collaborators: Biocad, Russia |
| NTR1704 | |
| Trial name or title | Comparison of Bevacizumab (Avastin) and Ranibizumab (Lucentis) in Exudative Age-related Macular Degeneration (BRAMD) |
| Methods |
Study design: RCT Planned enrollment: 306 participants Length of follow-up: 12 months |
| Participants |
Inclusion criteria: age 60 years or older; primary or recurrent sub-, juxta- or extrafoveal CNV secondary to AMD; CNV including retinal angiomatous proliferation, that may benefit from treatment; BCVA of 78 to 20 letters; size of lesion < 12 disc areas Exclusion criteria: subretinal hemorrhage involving ≥ 70% of the lesion area; subfoveal fibrosis or atrophy in the study eye; CNV of other pathogenesis; history of ocular anti-VEGF treatment within 2 months, triamcinolone within 6 months, or laser treatment within 1 month; active intraocular inflammation, retinal pigment epithelial tear involving the macula, or vitreous hemorrhage obscuring view of the posterior pole in the study eye; IOP > 25 mmHg; cataract extraction within 3 months; myopia > −8 diopter; hypersensitivity or allergy to testing agents; mentally or physically unable to participate; serious disease with probability of death during the study |
| Interventions |
Intervention 1: 1.25 mg intravitreal bevacizumab administered monthly for 12 months Intervention 2: 0.5 mg intravitreal ranibizumab administered monthly for 12 months |
| Outcomes |
Primary outcome, as defined: change in BCVA in the study eye from baseline to 12 months, assessed with ETDRS-like charts at an initial distance of four meters Secondary outcomes, as defined: proportion of participants losing fewer than 15 letters at 12 months (responders); proportion of participants with a loss or gain of BVCA less than 15 letters at 12 months (stabilizers); proportion of participants losing 15 letters or more of BCVA at 12 months (losers); proportion of participants gaining 15 letters or more of BCVA at 12 months (gainers); incidence of fluorescein leakage at 4 and 12 months; change in total area of CNV, total area of leakage from CNV, and total lesion area at 12 months, as determined by the reading center; absolute and percent change in retinal thickness, as measured by OCT at 4 and 12 months; proportion of dropouts before the final 12-month assessment; proportion of non-responders at the 4-month assessment; occurrence of (serious) adverse events during 12 months; costs of the two treatments |
| Starting date | March 2009; primary completion date of July 2013 |
| Contact information | Prof. dr. R.O. Schlingemann Department of Ophthalmology, Academisch Medisch Centrum Amsterdam, The Netherlands, 1105 AZ |
| Notes | “The primary objective is to demonstrate the non-inferiority of bevacizumab to ranibizumab in the treatment of patients with subfoveal CNV secondary to AMD as determined by the change in best-corrected visual acuity in the study eye from baseline to month 12.” Sponsors/Collaborators: Academic Medical Center (AMC), Department of Ophthalmology; The Netherlands Organization for Health Research and Development |
AMD: age-related macular degeneration
BCVA: best-corrected visual acuity
CNV: choroidal neovascularization
ETDRS: Early Treatment Diabetic Retinopathy Study
IOP: intraocular pressure
OCT: optical coherence tomography
PDT: photodynamic therapy
RCT: randomized controlled trial
VEGF: vascular endothelial growth factor
Included studies
Types of participants
This review included a total of 5496 participants from 12 RCTs; the number of participants per trial ranged from 28 to 1208. In all 12 trials, one eye per participant was randomized. The countries in which the trials were conducted spanned the globe: two studies were international (ANCHOR 2006; VISION 2004), four were conducted in the United States only (CATT 2011; MARINA 2006; PIER 2008; Subramanian 2010), two each in Austria (MANTA 2013; Sacu 2009) and the United Kingdom (ABC 2010; IVAN 2013), and one each in France (GEFAL 2013) and India (Biswas 2011). The 12 trials were similar in that they all enrolled both men and women 50 years of age or older who had subfoveal CNV secondary to AMD. Among the included trials, there were variations in the types of eligible neovascular lesions (e.g., predominantly classic CNV, minimally classic CNV, or occult CNV), lesion sizes, and baseline visual acuities of participants. Although the majority of participants in most trials were women, all but one of the enrollees in one trial were men (Subramanian 2010).
All trials predefined visual acuity eligibility criteria for the study eye of each participant. The most common criterion was a BCVA of 20/40 to 20/320 (Snellen equivalent) in the study eye, which was specified in six studies (ABC 2010; ANCHOR 2006; MANTA 2013; MARINA 2006; PIER 2008; VISION 2004). BCVA eligibility ranges included participants with somewhat better visual acuity in the CATT 2011 (20/25 to 20/320), GEFAL 2013 (20/32 to 20/320), and IVAN 2013 (20/320 or better) trials, but potentially worse visual acuity in the Sacu 2009 (20/40 to 20/800) and Subramanian 2010 (20/400 or better) studies. In Biswas 2011, participants with a BCVA between 35 and 70 Early Treatment Diabetic Retinopathy Study (ETDRS) letters were eligible; however, the test distance was not reported.
Five trials included only participants with no previous treatment for CNV or AMD (Biswas 2011; CATT 2011; IVAN 2013; MANTA 2013; Sacu 2009). The remaining seven trials allowed participants to have received previous therapy for AMD, with certain restrictions as to the type (e.g., verteporfin PDT, intravitreal injections, or surgery), location, and time interval since last treatment. Five trials enrolled participants with either primary or recurrent CNV in the study eye (ANCHOR 2006;MARINA 2006; PIER 2008; Subramanian 2010; VISION 2004) and one enrolled participants with primary CNV only (ABC 2010).
Of the six studies that reported the type of neovascular lesion, the ANCHOR 2006 study had the highest proportion of participants with predominantly classic CNV (410/423, 97%). The other five studies had fewer participants with predominantly classic CNV. In the ABC 2010 study, 25% of 131 participants had predominantly classic CNV; the remaining 75% had either minimally classic or occult CNV. In the VISION 2004 study, 26% of 1208 participants had predominantly classic CNV, 36% had minimally classic CNV, and 38% had occult CNV. The PIER 2008 study had similar proportions as the VISION 2004 study, with 19% of 184 participants having predominantly classic CNV, 38% having minimally classic CNV, and 43% having occult CNV at baseline. Forty-four percent of 120 participants had occult CNV in Biswas 2011. The MARINA 2006 study was limited to participants with only minimally classic or occult CNV and, thus, had the greatest proportion of participants with occult CNV (451/716, 63%).
Two studies that did not report neovascular lesion type described the subfoveal component of the CNV lesion in the study population. In the CATT 2011 study (1208 participants), 58% had CNV in the foveal center, 27% had fluid in the foveal center, 8% had hemorrhage in the foveal center, and 6%had other foveal center involvement. The distribution was similar in the IVAN 2013 study (628 participants) in which 54% participants had CNV in the foveal center, 29% had hemorrhage in the foveal center, and 13% had other foveal center involvement. The two smallest studies (Sacu 2009; Subramanian 2010), with 28 participants in each, and the GEFAL 2013 (501 participants) and MANTA 2013 (321 participants) studies did not describe the type of neovascularization or subfoveal component of the CNV lesion in the study population.
Five trials specified size of the lesion as an inclusion criterion. Four trials (ABC 2010; GEFAL 2013; MARINA 2006; PIER 2008) included participants with lesions of 12 disc areas (DA) or smaller (1 DA = 2.54 mm2, i.e., standard DA) and one study (Sacu 2009) set 4 DAs as the maximum lesion size.
Additional details about each trial included in this review are summarized in the Characteristics of included studies table.
Table 8.
Characteristics of included studies [ordered by study ID]
| ABC 2010 | ||
| Methods |
Number randomized (total and per group): 131 participants randomly assigned to study treatment; 65 to bevacizumab and 66 to ’standard treatment’. Standard treatment included intravitreal pegaptanib injections (n = 38), PDT with verteporfin (n = 16), or sham injection (n = 12) Exclusions after randomization: none Number analyzed (total and per group): 131 total participants; 65 bevacizumab and 66 standard treatment Unit of analysis: individuals (one study eye per participant) Losses to follow up: bevacizumab group: 1 participant died; standard treatment group: 3 participants withdrew from the trial and chose to have alternative treatment and 1 participant withdrew due to pain of treatment Compliance: limited information given: “more than 90% of patients in each group (overall 96%) were receiving treatment at the last treatment visit (48 weeks) and were followed up to week 54” Intention to treat analysis: yes, using last observation carried forward for 1 participant in bevacizumab group and 4 in standard treatment group Reported power calculation: yes, sample of 130 participants for power of 82% Study design comment: standard treatment group was not homogeneous; the ’standard treatment’ was decided for each participant before randomization based on eligibility for NHS coverage of treatments |
|
| Participants |
Country: UK (London, England) Age: mean in bevacizumab group was 79 years and in standard treatment group was 81 years Gender (percent): 80/131 (61%) women and 51/131 (39%) men Inclusion criteria: age 50 years or older; primary subfoveal CNV lesion in study eye secondary to AMD; occult CNV lesions required evidence of “disease progression”, based on deteriorating VA, sub- or intraretinal blood, or increase in lesion size; evidence of central macular thickening assessed using OCT; lesion in study eye with total size < 12 optic disc areas for minimally classic or occult lesions; area of fibrosis < 25% of the total lesion area; area of subretinal blood less than 50% of total lesion area; no more than 5400 microns in greater linear dimension for predominantly classic lesions; BCVA of 20/40 to 20/320 on ETDRS chart; no permanent structural damage to central fovea Exclusion criteria: surgery or other treatment in study eye; participation in any other clinical trial of antiangiogenic agents or (within previous month) of investigational drugs; primarily hemorrhagic lesion; coexisting ocular disease; premenopausal women not using adequate contraception; current treatment for active systemic infection; history of cardiac events (myocardial infarction, unstable angina) or cerebrovascular event in preceding 6 months; history of allergy to fluorescein; inability to obtain fundus photographs or fluorescein angiograms of sufficient quality to be analyzed and graded; inability to comply with study or follow up procedures Equivalence of baseline characteristics: yes Diagnoses in participants: 3/4 (75% of bevacizumab group and 76% of standard treatment group) had “minimally classic-occult” CNV; remainder of participants had predominantly classic CNV |
|
| Interventions |
Intervention 1: Bevacizumab: three initial injections every 6 weeks (1.25 mg in 0.05 mL per injection). “After the first three injections, investigators masked to treatment allocation used standardized criteria to decide whether to give further injections... Patients could therefore receive between three and nine injections over a total of 54 weeks.”
Intervention 2: Standard treatment group: one of three treatment options decided for each participant before randomization based on eligibility for NHS coverage of treatments
Length of follow up: Planned: 54 weeks Actual: 96% followed to week 54 |
|
| Outcomes |
Primary outcome, as defined: proportion of participants gaining 15 letters or more of BCVA at 1 year (54 weeks), as measured on an ETDRS chart Secondary outcomes, as defined: proportions of participants gaining 10 letters or more of BCVA at 6 months and 1 year (54 weeks) and proportions of participants gaining 5 letters or more of BCVA at 6 months and 1 year (54 weeks) as measured on an ETDRS chart; proportion with stable vision (defined as loss of < 15 letters); mean change in VA at 12 months; mean change in macular thickness from baseline to 6- and 12-month examinations; contrast sensitivity (Pelli-Robson charts), unspecified outcome definition and time; reading ability (maximum reading speed, critical print size and reading acuity) using Minnesota Reading cards, unspecified outcome definition and time Adverse events Intervals at which outcomes assessed: 1 week (safety visit), 6, 12, 18, 24, 30, 36, 42, 48 weeks (treatment or assessment for treatment), 1 year (54 weeks) |
|
| Notes |
Full study name: Avastin® (Bevacizumab) in Choroidal Neovascularization Trial Type of study: published Funding sources: special trustees of Moorfields Eye Hospital; Department of Health through an award by the National Institute for Health Research to Moorfields Eye Hospital NHS Foundation Trust and UCL Institute of Ophthalmology for a Specialist Biomedical Research Centre for Ophthalmology; additional support from the National Eye Research Centre, Bristol Declarations of interest: “The authors who work at Moorfields Eye Hospital have no financial gain from this endeavour, and no patents or patent applications with regard to bevacizumab are owned by the authors or Moorfields Pharmaceuticals.”; “The pharmaceutical division at Moorfields (Moorfields Pharmaceuticals) is involved in the repackaging of bevacizumab for intraocular use for sale to other institutions.”; various authors reported being on advisory boards for Novartis, Pfizer, GSK, MSD, and/or Allergan; receiving research grants for investigator sponsored trials, money, travel grants, and/or lecture fees from Novartis; and/or being a shareholder of a software company that has business links with Novartis and Pfizer Study period: August 2006 to November 2008 (enrollment Aug 2006 to November 2007) Reported subgroup analyses: by type of lesion (minimally classic/occult; predominantly classic) Contacting study investigators: trial authors contacted; no additional information provided for this review |
|
| Risk of bias | ||
| Bias | Authors’ judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | “Patients were allocated to treatment groups by minimisation-a dynamic process.” |
| Allocation concealment (selection bias) | Low risk | “The trial manager telephoned the clinical trials unit to obtain a treatment allocation. ” |
| Masking of participants (performance bias) | Low risk | “To maintain masking, patients randomized to bevacizumab received sham treatments if they did not require intravitreal treatment at that visit.” Participants also received placebo PDT therapy if in the bevacizumab group; “care was taken to ensure that the intravenous infusion pump and line were covered as the active verteporfin solution is green while the placebo infusion is a clear solution.” |
| Masking of study personnel (performance bias) | Low risk | Treating physicians were not masked; however, “investigators masked to treatment allocation used standardised criteria to decide whether to give further injections” in the bevacizumab group |
| Masking of outcome assessment (detection bias) | Low risk | “We assured outcome assessors were masked to treatment allocation by the use of a standard operating procedure that kept the outcome assessors out of contact with treating physicians and unable to obtain access to the treatment allocation.” |
| Incomplete outcome data (attrition bias) All outcomes |
Low risk | Four participants in the standard treatment group and one participant in the bevacizumab group were without 54-week VA outcome data. Intent-to-treat analysis was followed using last observation carried forward for missing data |
| Selective reporting (reporting bias) | Unclear risk | Study outcomes were published in a design and methods paper. We identified published results for these outcomes with the exception of outcomes related to reading ability (maximum reading speed, critical print size and reading acuity) |
| Other bias | Low risk | The standard therapy group did not receive the same intervention (PDT, pegaptanib injection, or sham injection) |
| ANCHOR 2006 | ||
| Methods |
Number randomized (total and per group): 423 participants randomly assigned to study treatment; 140 to 0.3 mg ranibizumab, 140 to 0.5 mg ranibizumab, and 143 to verteporfin PDT Exclusions after randomization: 3 participants in the 0.3 mg ranibizumab group did not receive treatment after randomization, one because of participant’s decision and two based on physician’s decision Number analyzed (total and per group): 422 total participants; 140 in 0.3 mg ranibizumab group, 139 in 0.5 mg ranibizumab group, and 143 in verteporfin PDT group Unit of analysis: individuals (one study eye per participant) Losses to follow up: 10 in 0.3 mg ranibizumab group, 5 in 0.5 mg ranibizumab group, and 10 in verteporfin PDT group; reasons included death, adverse events, loss to follow up, participant’s decision, physician’s decision and participant non-compliance Compliance: limited information given: “more than 90% of patients in each group (91. 5% overall) were receiving treatment at 12 months” Intention to treat analysis: yes, using last observation carried forward for missing data Reported power calculation: yes, sample of 426 participants for power of 96% Study design comment: none |
|
| Participants |
Country: USA, France, Germany, Hungary, Czech Republic, and Australia (83 study centers) Age: mean (range) was 77 years (54 to 97) in 0.3 ranibizumab group, 76 years (54 to 93) in 0.5 mg ranibizumab group, and 78 years (53 to 95) in verteporfin PDT group Gender (percent): 211/423 (50%) women and 212/423 (50%) men Inclusion criteria: age 50 years or older; subfoveal CNV lesion secondary to AMD determined independently based on fluorescein angiography and fundus photography to be predominantly classic in composition and suitable for treatment with verteporfin PDT; ≤ 5400 microns in greater linear dimension; BCVA of 20/40 to 20/320 Snellen using equivalent ETDRS charts; no permanent structural damage to central fovea; participants with juxta- or extrafoveal photocoagulation in the study eye more than 1 month prior to day 0 and prior verteporfin PDT in the non-study eye more than 7 days before study day 0 were included Exclusion criteria: surgery or other treatment in study eye; treatment with verteporfin PDT in the non-study eye less than 7 days preceding study day 0; participation in any other clinical trial of antiangiogenic agents or (within previous month) of investigational drugs; subretinal hemorrhage in study eye 50% or more of lesion area; subfoveal fibrosis or atrophy in study eye; coexisting ocular disease; premenopausal women not using adequate contraception; current treatment for active systemic infection; history of other disease, metabolic dysfunction, or physical examination or laboratory finding giving reasonable suspicion of a condition that contraindicates use of an investigational drug or that might affect interpretation of the results of the study or place the participant at a high risk for complications; history of allergy to fluorescein; inability to obtain fundus photographs or fluorescein angiograms of sufficient quality to be analyzed and graded; inability to comply with study or follow-up procedures Equivalence of baseline characteristics: a slightly higher percentage of participants in 0.3 mg ranibizumab group were aged 75–84 years (60% compared with 45.7% in 0.5 mg group and 51.7% in verteporfin PDT group) Diagnoses in participants: 410/423 (97%) had predominantly classic CNV; 12/423 (3%) had minimally classic CNV; and 1/423 (0.2%) had occult with no classic CNV |
|
| Interventions |
Intervention 1: 0.3 mg ranibizumab plus sham verteporfin PDT (intravenous infusion of saline followed by laser irradiation of macula) Intervention 2: 0.5 mg ranibizumab plus sham verteporfin PDT Intervention 3: sham intravitreal injection plus active verteporfin therapy (laser irradiation of macula following intravenous administration of verteporfin) Ranibizumab was injected into the study eye at monthly intervals (ranging from 23 to 37 days) for a total of 12 injections in the first year beginning on day 0. Either verteporfin or sham verteporfin PDT was administered on day 0 and then if needed on the basis of investigators’ evaluation of angiography at months 3, 6, 9, or 12. Length of follow up: Planned: 2 years Actual: 2 years |
|
| Outcomes |
Primary outcome, as defined: proportion of participants losing fewer than 15 letters from baseline visual acuity in the study eye at 12 months Secondary outcomes reported: proportion of participants gaining 15 letters or more from baseline; proportion of participants with a Snellen equivalent of 20/40 or better; proportion of participants with a Snellen equivalent of 20/200 or worse; mean change from baseline (letters over time); mean change from baseline to month 12 in the size of the classic CNV component and total area of leakage from CNV Exploratory efficacy endpoints: loss of 30 letters or more of visual acuity, mean changes in area of CNV and area of the entire lesion Safety assessments: IOP measurement before and 50 to 70 minutes after each study treatment, ocular and non-ocular adverse events, changes and abnormalities in clinical laboratory parameters and vital signs, and immunoreactivity to ranibizumab Quality-of-life indicators Intervals at which outcomes were assessed: “at regularly scheduled study visits,” 12 and 24 months, angiography evaluation was performed at months 3, 6, 9, 12 |
|
| Notes |
Full study name: Anti-VEGF Antibody for the Treatment of Predominantly Classic Choroidal Neovascularization in Age-related Macular Degeneration Type of study: published Funding sources: Genentech, USA and Novartis Pharma, Switzerland Declarations of interest: various authors reported having received consulting fees from Genentech, Eyetech, Novartis, Allergan, Alcon, Thea, Alimera, Oxigene, Genzyme, iScience, ISTA, Regeneron, Theragenics, VisionCare, and/or Jerini; lecture fees from Genentech, Eyetech, Novartis, Allergan, Pfizer, Alcon, Thea, and/or Jerini; grant support from Alcon, Acuity Pharmaceuticals, Allergan, Alimera, Eyetech, Pfizer Novartis, Genentech, Eli Lilly, Oxigene, and the Diabetic Retinopathy Clinical Research network; and/or having an equity interest in Pfizer or being full-time employees of Genentech, holding an equity interest in the company, and having received stock options Study period: May 2003 to September 2006 Reported subgroup analyses: multiple subgroup analyses reported and specified as retrospective analyses (see Kaiser 2007 under ANCHOR 2006) Contacting study investigators: trial authors contacted and contributed information for this review |
|
| Risk of bias | ||
| Bias | Authors’ judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | A dynamic randomization method was used, stratified by study center and visual acuity scores on day 0 (< 45 letters vs >= 45 letters) “Dynamic randomization, a generalization of the hierarchical method proposed by Signorini, et al. (1993)” (email communication with Genentech, dated 24 October 2007) |
| Allocation concealment (selection bias) | Low risk | “A centralized IVRS was used to conduct the randomization. Participants, study site personnel, and Sponsors’ personnel were masked to the treatment assignment throughout the study, except for the injecting physician, designated unmasked site personnel, and Sponsors’ drug accountability monitors.” (email communication with Genentech, dated 24 October 2007) |
| Masking of participants (performance bias) | Low risk | “To maintain masking, patients who had received saline as well as those who had received verteporfin were instructed to follow exposure-to-light-precautions after PDT administration according to the verteporfin package insert.” “An empty, needle-less syringe was used for sham injections, with pressure applied to the anesthetized and prepared eye at the site of a typical intravitreal injection. Pre- and post-injection procedures (described previously) were identical for ranibizumab and sham injections.” |
| Masking of study personnel (performance bias) | Low risk | “The ”injecting“ ophthalmologist administering the study treatments was unmasked. All other study site personnel (except those assisting with study treatment administration), patients, and central reading center personnel were masked to treatment assignment.” |
| Masking of outcome assessment (detection bias) | Low risk | “Double masking of treatment assignment necessitated at least two investigators per study site: an unmasked ”injecting“ ophthalmologist to administer the study treatments and a masked ”evaluating“ ophthalmologist to perform study assessments.” |
| Incomplete outcome data (attrition bias) All outcomes |
Low risk | “Efficacy analyses were performed on an intent-to-treat basis (including all randomized patients and according to the treatment group to which they were assigned) using a last-observation-carried-forward method to impute missing data (primary analysis) and using observed data (exploratory sensitivity analysis).” |
| Selective reporting (reporting bias) | Low risk | We did not have access to the protocol. However, primary and secondary outcomes reported to the FDA were reported in the publication with no changes |
| Other bias | Unclear risk | Sponsored by Genentech and Novartis Pharma. |
| Biswas 2011 | ||
| Methods |
Number randomized (total and per group): 120 participants randomly assigned to study treatment; 60 in bevacizumab group and 60 in ranibizumab group Exclusions after randomization: none Number analyzed (total and per group): 104 total participants; 50 in bevacizumab group and 54 in ranibizumab group Unit of analysis: individuals (one study eye per participant) Losses to follow up: 16 participants: reasons for losses to follow up not reported (ten in bevacizumab group, six in ranibizumab group) Compliance: 104/120 participants completed the study Intention to treat analysis: no, 16 participants enrolled and randomized were not included in analysis Reported power calculation: yes, “aimed to enroll a total of 120 patients... this number was arrived at by the investigators after considering the sample size of the available literature” Study design comment: randomization logistics were complicated (see ’Risk of bias’ table below) |
|
| Participants |
Country: two study centers in Kolkata, India Age: not reported for 120 enrolled participants (mean 64.4 years in analyzed bevacizumab group; mean 63.5 years in analyzed ranibizumab group) Gender (percent): not reported for 120 enrolled participants (28/50 (56%) men and 22/50 (44%) women in analyzed bevacizumab group; 22/54 (41%) men and 32/54 (59%) women for analyzed ranibizumab group) Inclusion criteria: age 50 years or older; presence of subfoveal or juxtafoveal CNV of any type; active leakage pattern; baseline BCVA between 35 to 70 ETDRS letters; baseline central macular thickness greater than or equal to 250 μm, measured by OCT Exclusion criteria: previous treatment for CNV in either eye; macular scarring; any coexisting ocular disease or pathology; monocular participants; history of ocular surgery within six months of enrollment; history of cerebrovascular accident and myocardial infarction Equivalence of baseline characteristics: gender imbalance between analyzed groups Diagnoses in participants: all with subfoveal or juxtafoveal CNV; 22/50 participants with occult CNV in bevacizumab group and 24/54 participants with occult CNV in ranibizumab group |
|
| Interventions |
Intervention 1: 1.25 mg intravitreal bevacizumab every month for first three months; re-treatment afterwards based on OCT or VA changes Intervention 2: 0.5 mg intravitreal ranibizumab every month for first three months; re- treatment afterwards based on OCT or VA changes Length of follow up: Planned: 18 months Actual: 18 months |
|
| Outcomes |
Primary outcomes, as defined: “changes in BCVA and CMT from baseline (month 0) to month 18” Secondary outcomes, as reported: blood pressure measurements; reports of unusual extremity pain Adverse events Intervals at which outcome assessed: monthly through 18 months |
|
| Notes |
Type of study: published Funding sources: reported “nil” Declarations of interest: “none declared” Study period: April 2007 to April 2009 Reported subgroup analyses: yes, for participants with predominantly classic CNV Contacting study investigators: trial authors contacted; no additional information provided for this review |
|
| Risk of bias | ||
| Bias | Authors’ judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | “Using random numbers tables, 60 numbers were randomly picked up from 1 to 120 and assigned to group A while the remaining sixty numbers were assigned to group B.” |
| Allocation concealment (selection bias) | Unclear risk | “...randomization of the 120 numbers into two groups was done before initiation of enrolment itself. Upon initiation of enrollment, the patients were numbered sequentially based on the serial order of enrolment in the study. Depending on the enrolment number, the patients were automatically assigned to either group A or B based on the prior randomization of number 1–120 into two equal groups using random number tables.” |
| Masking of participants (performance bias) | Unclear risk | Masking of participants not reported. |
| Masking of study personnel (performance bias) | Low risk | “The injections were given...by the investigators, who were blinded to the type of injection.” |
| Masking of outcome assessment (detection bias) | Low risk | “All assessors were masked to the group of patient they were following up.” |
| Incomplete outcome data (attrition bias) All outcomes |
Unclear risk | Sixteen (13%) participants lost to follow up were excluded from the analyses; 10 in the bevacizumab group and 6 in the ranibizumab group |
| Selective reporting (reporting bias) | Unclear risk | No protocol or clinical trial registration was identified for this study. Outcomes were reported for stated outcomes in the methods section of the published report; however, only P values were reported for between-group comparisons and no standard deviation or variance measures were reported for continuous outcomes |
| Other bias | Low risk | None observed. |
| CATT 2011 | ||
| Methods |
Number randomized (total and per group): 1208 participants randomly assigned to study treatment; number of participants randomized per group not reported Exclusions after randomization: one study center (23 participants) was excluded due to protocol violations Number analyzed (total and per group): 1105 total participants; 265 in bevacizumab monthly group, 284 in ranibizumab monthly group, 271 in bevacizumab as needed group, and 285 in ranibizumab as needed group Unit of analysis: individuals (one study eye per participant) Losses to follow up: 80 total participants: 21 in bevacizumab monthly group (4 died and 17 with missing data), 17 in ranibizumab monthly group (4 died and 13 with missing data), 29 in bevacizumab as needed group (11 died and 18 with missing data), 13 in ranibizumab as needed group (5 died and 8 with missing data) Compliance: limited information given: mean of 11.9 treatments given for bevacizumab monthly group and mean of 11.7 treatments given for ranibizumab monthly group Intention to treat analysis: no, 103 participants enrolled and randomized were not included in the analyses Reported power calculation: yes, sample of 277 participants per group for power of 90% Study design comment: non-inferiority design, four arms, six pairwise comparisons planned; at one year, participants in the monthly dose treatment groups were re-randomized to either continue with monthly injections or switch to as needed injections of the same treatment drug |
|
| Participants |
Country: USA Age: mean was 80 years in bevacizumab monthly group, 79 years in ranibizumab monthly group, 79 years in bevacizumab as needed group, and 78 years in ranibizumab as needed group Gender (percent): 732/1185 (61.8%) women and 453/1185 (38.2%) men Inclusion criteria: age 50 years or older; one study eye per participant with untreated active CNV due to AMD (based on presence of leakage as seen by fluorescein angiography and of fluid as seen by OCT); VA of 20/25 to 20/320 on electronic visual-acuity testing Exclusion criteria: fibrosis or atrophy in center of fovea in the study eye; CNV in either eye due to other causes; retinal pigment epithelial tear involving the macula; any concurrent intraocular condition in the study eye (e.g., cataract or diabetic retinopathy) that, in the opinion of the investigator, could either require medical or surgical intervention or contribute to VA loss during the 3 year follow-up period; active or recent (within 4 weeks) intraocular inflammation; current vitreous hemorrhage in the study eye; history of rhegmatogenous retinal detachment or macular hole; active infectious conjunctivitis, keratitis, scleritis, or endophthalmitis; spherical equivalent > 8 diopters; intraocular surgery (including cataract surgery) in the study eye within 2 months; uncontrolled glaucoma; participants unable to be photographed to document CNV due to known allergy to fluorescein dye, lack of venous access or cataract obscuring the CNV; pre-menopausal women not using adequate contraception; pregnancy or lactation; history of other disease, metabolic dysfunction, physical examination finding, or clinical laboratory finding giving reasonable suspicion of a disease or condition that contraindicates the use an investigational drug or that might affect interpretation of the results of the study or render the subject at high risk for treatment complications; current treatment for active systemic infection; uncontrolled concomitant diseases such as cardiovascular disease, nervous system, pulmonary, renal, hepatic, endocrine, or gastrointestinal disorders; history of recurrent significant infections or bacterial infections; inability to comply with study or follow-up procedures Equivalence of baseline characteristics: a slightly higher percentage of participants in bevacizumab monthly group had history of transient ischemic attack (8.7% compared with 4% in ranibizumab monthly group, 4% in ranibizumab as needed group, and 6. 3% in bevacizumab as needed group) Diagnoses in participants: 688/1185 (58%) had active neovascular AMD with CNV in foveal center; 315/1185 (27%) had fluid in foveal center; 93/1185 (8%) had hemorrhage in foveal center; 71/1185 (6%) had other foveal center involvement; and 18/1185 (1. 5%) had no CNV or not possible to grade |
|
| Interventions |
Intervention 1: 1.25 mg intravitreal bevacizumab on a fixed schedule of every 4 weeks for 1 year, at 1 year, re-randomization to bevacizumab every 4 weeks or as needed Intervention 2: 0.5 mg intravitreal ranibizumab on a fixed schedule of every 4 weeks for 1 year, at 1 year, re-randomization to ranibizumab every 4 weeks or as needed Intervention 3: 1.25 mg intravitreal bevacizumab as needed for 2 years Intervention 4: 0.5 mg intravitreal ranibizumab as needed for 2 years Length of follow up: Planned: 12 months for primary analysis; 24 months for secondary analyses, with modifications to two intervention arms as described above Actual: 12 months for primary analysis; 24 months for secondary analyses |
|
| Outcomes |
Primary outcome, as defined: change in visual acuity from baseline at 12 months with a non-inferiority margin of 5 letters Secondary outcomes: proportion of eyes with 15-letter change, number of injections, OCT measured change in foveal thickness, change in lesion size on OCT and also on fluorescein angiography, incidence of ocular and systemic adverse events, and annual drug cost Intervals at which outcomes were assessed: weeks 4, 12, 24, 36, 52 during first year for visual acuity; weeks 4, 8, 12, 24, 52 for changes on OCT |
|
| Notes |
Full study name: Comparison of Age-related macular degeneration Treatment Trials Type of study: published Funding: National Eye Institute, National Institutes of Health, US Declarations of interest: one investigator reported receiving consulting fees from GlaxoSmithKline and another consulting fees from Neurotech and SurModics Study period: accrual February 2008 through December 2009; follow up through December 2011 Reported subgroup analyses: none Contacting study investigators: trial authors not contacted as data were available in published reports |
|
| Risk of bias | ||
| Bias | Authors’ judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | “Patients were randomly assigned to 1 of 4 study groups. Randomization schedules were stratified according to clinical center with the use of a permuted-block method with randomly chosen block sizes.” |
| Allocation concealment (selection bias) | Low risk | Web-based data entry system was used to allocate participants to treatment groups |
| Masking of participants (performance bias) | Unclear risk | Initially, participants were masked to which drug they received, but not to the treatment schedule. The study investigators noted that “insurance and billing documents specified ranibizumab but not study- supplied bevacizumab. Therefore, patients may have learned or deduced their assigned drug from these financial documents.” |
| Masking of study personnel (performance bias) | Low risk | Physicians were masked to drug but not to injection schedule. Physicians were uninvolved in visual acuity testing and in secondary outcome assessments |
| Masking of outcome assessment (detection bias) | Low risk | Electronic Visual Acuity system (computerized testing) was used for primary outcome. Retinal center personnel were masked. Adverse event reporting was unmasked, but medical monitor who evaluated serious adverse events was masked |
| Incomplete outcome data (attrition bias) All outcomes |
Unclear risk | 103/1208 (8.5%) participants randomized were not included in the one-year analysis. At two years, outcomes were not available for all participants by their originally assigned treatment groups |
| Selective reporting (reporting bias) | Low risk | Primary and secondary outcomes, specified a priori, for 1 year follow up were reported |
| Other bias | Low risk | None observed. |
| GEFAL 2013 | ||
| Methods |
Number randomized (total and per group): 501 participants randomly assigned to study treatment; 255 in bevacizumab group and 246 in ranibizumab group Exclusions after randomization: 16 participants excluded because they received no injection (9 in bevacizumab group and 7 in ranibizumab group) Number analyzed (total and per group): 485 participants (246 in bevacizumab group and 239 in ranibizumab group) for safety analysis at one year; 404 participants (207 in bevacizumab group and 197 in ranibizumab group) for analysis on visual acuity at one year; most data analyzed for 374 participants (191 in bevacizumab group and 183 in ranibizumab group) with available baseline BCVA data, at least 10 months follow up, and did not have major deviations from the study protocol Unit of analysis: individuals (one study eye per participant) Losses to follow up: 81 total participants: 39 in bevacizumab group and 42 in ranibizumab group; additional 30 participants (16 in bevacizumab group and 14 in ranibizumab group) excluded from most analyses due to protocol violations Compliance: 374/501 participants completed the study without major protocol violations Intention to treat analysis: no, not all participants enrolled and randomized were included in the analyses Reported power calculation: yes, sample of 200 participants per group for power of 90% to detect 15 letters changes in BCVA Study design comment: non-inferiority design |
|
| Participants |
Country: France (38 study centers) Age: mean age for 374 participants without major protocol violations was 79 years Gender (percent): 248/374 (66%) women and 126/374 (34%) men Inclusion criteria: age 50 years or older; active subfoveal neovascular AMD (one study eye eligible in bilateral cases); lesion size < 12 disk areas; recent development of lesion in cases of occult neovessels; BCVA of 20/32 to 20/320 on ETDRS scale Exclusion criteria: subretinal hemorrhage reaching foveal center and > 50% of the lesion area; fibrosis or atrophy in center of fovea in the study eye; CNV of other pathogenesis; retinal pigment epithelial tear reaching the macula; previous or current treatment with intravitreal anti-VEGF therapy; history of treatment 3 months prior or intraocular surgery 2 months prior to first study injection; history of photocoagulation or intravitreal medical device in the study eye; ocular or periocular infection; intraocular inflammation; diabetic retinopathy; history of autoimmune or idiopathic uveitis; IOP ≥ 25 mmHg with topical hypotensive therapy; aphakia or lack of lens capsule in the study eye; known illness or condition requiring intraocular surgery within 12 months; known hypersensitivity to study drugs or allergy to agents used for ocular testing; uncontrolled arterial hypertension; history of treatment with systemic bevacizumab; premenopausal women not using adequate contraception; involvement in another clinical study; not part of French national health insurance program Equivalence of baseline characteristics: yes Diagnoses in participants: 354/374 (95%) had intraretinal and/or subretinal fluid on OCT |
|
| Interventions |
Intervention 1: 1.25 mg intravitreal bevacizumab every month for first three months; re-treatment afterwards based on OCT or VA changes Intervention 2: 0.50 mg intravitreal ranibizumab every month for first three months; re-treatment afterwards based on OCT or VA changes Length of follow up: Planned: 1 year Actual: 1 year |
|
| Outcomes |
Primary outcome, as defined: mean change in BCVA at 1 year (at least 10 months after inclusion), as measured on an ETDRS chart Secondary outcomes, as defined in published reports: visual acuity outcomes at 1 year: BCVA, change in BCVA, proportion with gain of ≥15 letters, proportion with loss of ≥15 letters, proportion with gain of ≥5 letters, proportion with loss of ≥5 letters; change in CNV area between the baseline and final evaluations; presence of intraretinal and/or subretinal fluid; presence of pigment epithelial detachment; central subfield macular thickness; change in central subfield macular thickness; dye leakage on angiogram; number of injections; model of OCT equipment; adverse events Secondary outcomes, as defined in trial registry: efficacy of treatments at 1 year; proportions of ocular and systemic adverse events at 1 year; average number of injections and time before re-injection during 1 year; drug profiles in blood and aqueous humor of a subset of 20 participants at 3 months; medico-economic impact of treatments at 1 year Intervals at which outcomes were assessed: monthly through 12 months |
|
| Notes |
Full study name: Groupe d’Etude Français Avastin versus Lucentis dans la DMLA néovasculaire Type of study: published Funding sources: French Ministry of Health (Programme Hospitalier de Recherche Clinique National 2008); the French Health Insurance System co-financed the study and funded study drugs Declarations of interest: four authors declared disclosures as principal investigators for trials sponsored by Novartis, Bausch & Lomb, Théa, and Alcon; serving on advisory boards for Alcon, Allergan, Bayer, Bausch & Lomb, Novartis, and Théa; receiving lecture fees from Alcon, Allergan, Bayer, Bausch & Lomb, Heidelberg Engineering, the Krys group, Novartis, Théa, and Zeiss; receiving consulting fees from Novartis, Bayer, and Allergan; or receiving honoraria from Novartis, Bayer, and Allergan; the other four authors declared no conflicts of interests Study period: random enrollment 24 June 2009 to 9 November 2011 Reported subgroup analyses: none Contacting study investigators: trial authors contacted and contributed information for this review |
|
| Risk of bias | ||
| Bias | Authors’ judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | “The randomization was stratified by center and visual acuity (threshold: 20/100). Local hospital pharmacies were responsible for randomizing patients in each center using pre-established lists.”’ |
| Allocation concealment (selection bias) | Low risk | Hospital pharmacy used to conceal treatment assignments prior to participant enrollment and randomization (email communication with Dr Kodjikian, dated 7 August 2014) |
| Masking of participants (performance bias) | Low risk | “Identical syringes were masked and delivered by local hospital pharmacies after aseptic preparation in authorized, centralized drug-preparation units, using vials of Avastin 100 mg/ml and Lucentis 10 mg/ml.” “The main strength of the GEFAL trial is that the study remained effectively double-masked, unlike CATT in which some participants received billing information and IVAN in which the masking differed between centers (some treating teams were aware of treatment allocation).” |
| Masking of study personnel (performance bias) | Low risk | “Identical syringes were masked and delivered by local hospital pharmacies after aseptic preparation in authorized, centralized drug-preparation units, using vials of Avastin 100 mg/ml and Lucentis 10 mg/ml.” “The main strength of the GEFAL trial is that the study remained effectively double-masked, unlike CATT in which some participants received billing information and IVAN in which the masking differed between centers (some treating teams were aware of treatment allocation).” |
| Masking of outcome assessment (detection bias) | Low risk | Only the pharmacists who prepared the syringes knew about the randomization assignments; ophthalmologists, study coordinators, and all outcome assessors were masked like participants (email communication with Dr Kodjikian, dated 7 August 2014) |
| Incomplete outcome data (attrition bias) All outcomes |
Unclear risk | 16/501 (3%) participants randomized were not included in any analysis; most analyses reported did not include 127/501 (25%) of participants |
| Selective reporting (reporting bias) | Unclear risk | Differences in outcomes between the trial registration and published one-year results papers included:
|
| Other bias | Low risk | None observed. |
| IVAN 2013 | ||
| Methods |
Number randomized (total and per group): Drug randomization: 628 total participants; 305 to bevacizumab group and 323 to ranibizumab group Regimen randomization: 294/305 in bevacizumab group and 312/323 in ranibizumab group completed first three injections and were randomized to continue or discontinue treatment: 149 continued bevacizumab; 145 discontinued bevacizumab; 157 continued ranibizumab; and 155 discontinued ranibizumab Exclusions after randomization: 18 participants did not receive treatment and were excluded after randomization to drug treatment (9 in bevacizumab group and 9 in ranibizumab group) Number analyzed (total and per group): at one year follow up: 561 total participants at one year; 136 in continued bevacizumab group; 138 in discontinued bevacizumab group; 141 in continued ranibizumab group; and 146 in discontinued ranibizumab group at two years follow up: 525 total participants at one year; 127 in continued bevacizumab group; 127 in discontinued bevacizumab group; 134 in continued ranibizumab group; and 137 in discontinued ranibizumab group Unit of analysis: individuals (one study eye per participant) Losses to follow up: at one year follow up: 49 total participants: 4 participants receiving treatment withdrew prior to completing third injection (2 in bevacizumab group and 2 in ranibizumab group); 45 participants randomized to regimen groups exited trial before one year (13 in continued bevacizumab group; 7 in discontinued bevacizumab group; 16 in continued ranibizumab group; and 9 in discontinued ranibizumab group) at two years follow up: 85 total participants: 5 participants receiving treatment withdrew prior to completing third injection (3 in bevacizumab group and 2 in ranibizumab group); 80 participants randomized to regimen groups exited trial before two years (21 in continued bevacizumab group; 18 in discontinued bevacizumab group; 23 in continued ranibizumab group; and 18 in discontinued ranibizumab group) Compliance: the wrong study drug was administered twice during the first year; at one year follow up: adherence was 6576/6699 (98%) scheduled injections received at two years follow up: adherence was 12761/14640 (87%) scheduled injections received Intention to treat analysis: no, 67 participants enrolled and randomized were not included in the analyses at one year and 103 at two years Reported power calculation: yes, sample of 600 participants per group for power of 90% to detect non-inferiority Study design comment: non-inferiority design; 2 × 2 factorial design - randomization in two stages: first randomized to drug treatment (bevacizumab or ranibizumab), then to treatment regimen (continue monthly injections or discontinue monthly injections and switch to as needed injections given in three month cycles); results reported only as bevacizumab versus ranibizumab and continuous versus discontinuous |
|
| Participants |
Country: UK (23 study centers) Age: mean age for 610 participants receiving treatment was 78 years Gender (percent): 366/610 (60%) women and 244/610 (40%) men Inclusion criteria: age 50 years or older; previously untreated neovascular AMD in study eye with any component of the neovascular lesion (CNV, blood, serous pigment epithelial detachment, elevated blocked fluorescence) involving the center of the fovea, confirmed by fluorescein angiography; best-corrected VA of 25 letters or greater on the ETDRS chart (measured at 1 m) Exclusion criteria: neovascular lesion of 50% or more fibrosis or blood; more than 12 disc diameters; argon laser treatment in study eye within 6 months; presence of thick blood involving the center of the fovea; presence of other active ocular disease causing concurrent vision loss; myopia 8 or more diopters; previous treatment with PDT or a VEGF inhibitor in study eye; women pregnant, lactating, or of child-bearing potential; men with a spouse or partner of child-bearing potential Equivalence of baseline characteristics: yes Diagnoses in participants: 301/610 (58%) had neovascular AMD with CNV in foveal center; 308/610 (54%) had fluid in foveal center; 90/610 (16%) had hemorrhage in foveal center; 75/610 (13%) had other foveal center involvement; and 15/610 (3%) had no CNV or not possible to grade |
|
| Interventions |
Intervention 1: 1.25 mg intravitreal bevacizumab monthly for two years Intervention 2: 0.5 mg intravitreal ranibizumab monthly for two years Intervention 3: after first 3 monthly 1.25 mg intravitreal bevacizumab injections, monthly treatment was discontinued and treatment was given as needed in cycles of 3 monthly doses Intervention 4: after first 3 monthly 0.5 mg intravitreal ranibizumab injections, monthly treatment was discontinued and treatment was given as needed in cycles of 3 monthly doses Length of follow up: Planned: 2 years Actual: 2 years |
|
| Outcomes |
Primary outcome, as defined: best-corrected distance visual acuity measured as ETDRS letters at two years Secondary outcomes, as defined in protocol: at 1 year and 2 years follow up - frequencies of adverse effects of treatment; generic and vision-specific health-related quality of life; treatment satisfaction; cumulative resource use/cost and cost-effectiveness; clinical measures of vision (contrast sensitivity measured with Pelli-Robson charts, near visual acuity measured by Bailey-Love near reading cards, and reading speed measured with Belfast reading charts); lesion morphology (fluorescein angiography and OCT); distance visual acuity at one year; survival free from treatment failure Exploratory analysis: association between serum markers and cardiovascular serious adverse events Intervals at which outcomes were assessed: monthly through 24 months; various data were collected at every visit depending on assessment schedule and regimen group |
|
| Notes |
Full study name: alternative treatments to Inhibit VEGF in Age-related choroidal Neo- vascularisation Type of study: published Funding sources: National Institute for Health Research Health Technology Assessment program, UK Declarations of interest: various authors reported being principal investigators of trials sponsored by Novartis; attending and being remunerated for attendance at advisory boards for Novartis, Bayer, Neovista, Oraya, Allergan, and/or Bausch and Lomb; being employed by institution that has received payments from Novartis, Bayer, Neovista, Oraya, Alcon, and/or Pfizer; receiving honoraria from Novartis for lecture and/or teaching fees from Janssen-Cilag Study period: random enrollment 27 March 2008 to 15 October 2010 Reported subgroup analyses: none Contacting study investigators: trial authors not contacted as data were available in published reports |
|
| Risk of bias | ||
| Bias | Authors’ judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | “Randomized allocations were computer generated by a third party in blocks and stratified by center.” “Randomisation was stratified by centre and was blocked to ensure roughly equal numbers of participants per group within a centre.” |
| Allocation concealment (selection bias) | Low risk | “Research teams at sites recruited participants, and accessed a password-protected website to randomize participants. Allocations were concealed until participants’ eligibility and identities were confirmed.” “Allocations were computer generated and concealed with an internet-based system (Sealed Envelope, London, UK). Staff in participating centres accessed the website and, on entering information to confirm a participant’s identity and eligibility, were provided with the unique study number.” |
| Masking of participants (performance bias) | Low risk | From study protocol: “Participants, clinicians and trial personnel will be masked to the VEGF inhibitor to which a participant is assigned.” “We have chosen not to mask participants, clinicians and trial personnel to whether patients are allocated to continue or stop treatment at 3 months.” |
| Masking of study personnel (performance bias) | Low risk | “We intended that drug allocation should be concealed by having separate masked assessment and unmasked treating teams. This system was achieved by 14 sites. At the other 9 sites, staffing levels could not support this system and an unmasked staff member prepared ranibizumab in a syringe identical to those containing bevacizumab and did not perform assessments.” From study protocol: “We have chosen not to mask participants, clinicians and trial personnel to whether patients are allocated to continue or stop treatment at 3 months.” |
| Masking of outcome assessment (detection bias) | Low risk | “We intended that drug allocation should be concealed by having separate masked assessment and unmasked treating teams. This system was achieved by 14 sites. At the other 9 sites, staffing levels could not support this system and an unmasked staff member prepared ranibizumab in a syringe identical to those containing bevacizumab and did not perform assessments.” “Lesion morphology was assessed by independent graders masked to drug and treatment regimen.” From study protocol: “We have chosen not to mask participants, clinicians and trial personnel to whether patients are allocated to continue or stop treatment at 3 months.” |
| Incomplete outcome data (attrition bias) All outcomes |
Unclear risk | 67/628 (11%) participants randomized were not included in the one-year analysis; 111/628 (18%) participants randomized were not included in the two-year analysis |
| Selective reporting (reporting bias) | Unclear risk | Differences between the protocol and published one-year and two-year results papers included: 1) two secondary outcomes in the protocol were not listed in paper: treatment satisfaction and survival free from treatment failure; and 2) exploratory (serum) analysis in protocol upgraded to a secondary outcome in paper |
| Other bias | Low risk | None observed. |
| MANTA 2013 | ||
| Methods |
Number randomized (total and per group): 321 participants randomly assigned to study treatment; number per group not reported Exclusions after randomization: 4 participants (3 due to receiving the wrong drug and 1 because the participant received prior treatment and was not eligible) Number analyzed (total and per group): 317 total participants; 154 in bevacizumab group and 163 in ranibizumab group Unit of analysis: individuals (one study eye per participant) Losses to follow up: 69 participants: reasons for losses to follow up not reported (33 in bevacizumab group, 36 in ranibizumab group) Compliance: 248/317 participants completed the study Intention to treat analysis: no, 4 participants enrolled and randomized were not in- cluded in analysis; data imputed using last-observation-carried-forward method for 69 participants lost to follow up Reported power calculation: yes, sample of 320 participants for power of 95% Study design comment: non-inferiority design |
|
| Participants |
Country: 10 clinical centers in Austria Age: mean 76.7 years in bevacizumab group and 77.6 years in ranibizumab group Gender (percent): 115/317 (36.3%) men and 202/317 (63.7%) women Inclusion criteria: age 50 years or older; active primary or recurrent subfoveal lesion with CNV, measured by fluorescein angiography or OCT; BCVA in study eye between 20/40 to 20/320, measured by ETDRS charts Exclusion criteria: previous treatment for CNV or AMD; prior treatment with any intravitreal drug or verteporfin PDT in study eye; prior treatment with systemic bevacizumab; prior treatment with any intravitreal drug or verteporfin PDT in non-study eye within 3 months; laser photocoagulation in study eye within 1 month; participation in another clinical trial within 1 month; subfoveal fibrosis or atrophy > 50% in study eye; CNV in either eye due other causes than AMD; RPE tear involving macula of study eye; history of uncontrolled glaucoma or concurrent intraocular condition in study eye; pregnancy; allergy to fluorescein; inability to comply with study procedures Equivalence of baseline characteristics: yes Diagnoses in participants: active primary or recurrent subfoveal CNV |
|
| Interventions |
Intervention 1: 1.25 mg intravitreal bevacizumab every month for first three months; re-treatment afterwards based on OCT or VA changes Intervention 2: 0.5 mg intravitreal ranibizumab every month for first three months; re-treatment afterwards based on OCT or VA changes Length of follow up: Planned: 12 months Actual: 12 months |
|
| Outcomes |
Primary outcomes, as defined: “mean change in BCVA between baseline and 1 year” Secondary outcomes, as reported: Kaplan-Meier proportions of the gain of 15 letters of vision, gain of 5 letters of vision, loss of 5 letters of vision, loss of 15 letters of vision; lesion size, assessed by fluorescein angiography; number of retreatments; and retinal thickness, assessed by OCT Adverse events Intervals at which outcome assessed: monthly through 12 months |
|
| Notes |
Full study name: A Randomized Observer and Subject Masked Trial Comparing the Visual Outcome After Treatment With Ranibizumab or Bevacizumab in Patients With Neovascular Age-related Macular Degeneration Multicenter Anti VEGF Trial in Austria Type of study: published Funding sources: Austrian ophthalmologic society; the Ludwig Boltzmann Institute of Retinology and Biomicroscopic Lasersurgery; the participating study center sites Declarations of interest: authors reported no competing interests Study period: not reported Reported subgroup analyses: none Contacting study investigators: trial authors contacted; no additional information provided for this review |
|
| Risk of bias | ||
| Bias | Authors’ judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | “Randomisation was stratified according to the clinical centre using a permuted block method with a fixed block size of 20.” |
| Allocation concealment (selection bias) | Low risk | “Eligible patients were randomized in a 1: 1 ratio to one of two groups by members of the Department of Clinical Pharmacology, Medical University of Vienna, which was otherwise not involved in the study.” |
| Masking of participants (performance bias) | Low risk | “All other personnel and the patients were masked to treatment assignment.” |
| Masking of study personnel (performance bias) | Low risk | “The evaluating physician was masked to treatment assignment, whereas the injecting physician was not involved in the collection of data.” |
| Masking of outcome assessment (detection bias) | Low risk | “The evaluating physician was masked to treatment assignment, whereas the injecting physician was not involved in the collection of data.” |
| Incomplete outcome data (attrition bias) All outcomes |
Unclear risk | There were 4/321 (1. 2%) participants excluded from the study. At 12 months, 69 participants did not have outcome data; last-observation-carried-forward method was used to impute missing data for these 69 participants |
| Selective reporting (reporting bias) | Low risk | All primary and secondary outcomes were reported. |
| Other bias | Low risk | None observed. |
| MARINA 2006 | ||
| Methods |
Number randomized (total and per group): 716 participants randomly assigned to study treatment; 238 to 0.3 mg ranibizumab group, 240 to 0.5 mg ranibizumab group, and 238 to sham injection group Exclusions after randomization: none Number analyzed (total and per group): all 716 participants; 238 to 0.3 mg ranibizumab group, 240 to 0.5 mg ranibizumab group, and 238 to sham injection group Unit of analysis: individuals (one study eye per participant) Losses to follow up: 52 participants did not complete 12 months: 12 in the 0.3 mg ranibizumab group, 14 in the 0.5 mg ranibizumab group, and 26 in the sham injection group. Reasons included death, adverse events, loss to follow up, participant’s decision, physician’s decision, participant non-compliance, and need for other therapeutic inter- vention Compliance: “more than 90% of patients in each treatment group remained in the study at 12 months, and approximately 80 to 90% remained at 24 months” Intention to treat analysis: yes, using last observation carried forward for missing data Reported power calculation: yes, sample of 720 participants for power of 95% Study design comment: following primary analyses of the study at one year and with recommendation of the data monitoring committee, the study protocol was amended to offer treatment with 0.5 mg ranibizumab to participants still being followed in the sham control group. The study protocol was amended four months into the study to allow photodynamic therapy for active minimally classic or occult with no classic lesions that were no larger than 4 disc areas in size and accompanied by a 20-letter or greater loss from baseline visual acuity confirmed at consecutive study visits. When photodynamic therapy was used, the scheduled study treatment was postponed until the next scheduled monthly study visit |
|
| Participants |
Country: USA Age: range 52 to 95 years; mean was 77 years in each of the three treatment groups Gender (percent): 464/716 (65%) women and 252/716 (35%) men Inclusion criteria: age 50 years or older; active primary or recurrent subfoveal lesions with CNV secondary to AMD defined as: (1) exhibiting at least a 10% increase in lesion size determined by comparing a fluorescein angiogram performed within 1 month preceding study day 0 with a fluorescein angiogram performed within 6 months preceding study day 0, (2) resulting in a visual acuity loss of greater than 1 Snellen line any time within the prior 6 months, or (3) subretinal hemorrhage associated with CNV within 1 month preceding study day 0; total area of CNV encompassed within the lesion at least 50% of the total lesion area; total lesion area of 12 disc areas or less in size; best-corrected visual acuity of 20/40 to 20/320 (Snellen equivalent on ETDRS chart). Participants with lesions with an occult CNV component were included, but for participants with concomitant classic CNV, the area of classic CNV must have been less than 50% of the total lesion size Exclusion criteria: prior treatment with verteporfin, external-beam radiation therapy, or transpupillary thermotherapy in the study eye; previous participation in a clinical trial involving antiangiogenic drugs; treatment with verteporfin in the non-study eye less than 7 days preceding study day 0; previous intravitreal drug delivery or subfoveal focal laser photocoagulation in the study eye; laser photocoagulation in the study eye within 1 month preceding study day 0; history of vitrectomy surgery, submacular surgery, or other surgical intervention for AMD in study eye; participation in any studies of investigational drugs within 1 month preceding study day 0; subretinal hemorrhage in study eye involving center of the fovea if the size of hemorrhage is either 50 % or more of the total lesion area or 1 or more disc areas in size; subfoveal fibrosis or atrophy in study eye; CNV in either eye due to other causes; retinal pigment epithelia tear involving the macula in the study eye Equivalence of baseline characteristics: yes Diagnoses in participants: 1/716 (0.1%) had predominantly classic CNV; 264/716 (37%) had minimally classic CNV; and 451/716 (63%) had occult with no classic CNV |
|
| Interventions |
Intervention 1: 0.3 mg ranibizumab intravitreal injection monthly for 2 years Intervention 2: 0.5 mg ranibizumab intravitreal injection monthly for 2 years Intervention 3: sham injection monthly for 2 years In all intervention groups, verteporfin photodynamic therapy for the study eye was allowed if the choroidal neovascularization converted to a predominantly classic pattern. Length of follow up: Planned: 2 years Actual: 2 years |
|
| Outcomes |
Primary outcomes, as defined: proportion of participants who lost fewer than 15 letters from baseline visual acuity in study eye at 12 months Secondary outcomes, as defined: proportion of participants who gained 15 letters or more from baseline, proportion of participants with a Snellen equivalent of 20/200 or worse, and mean change from baseline (letters over time); mean change from baseline to month 12 in the size of the classic CNV component and total area of leakage from CNV Exploratory efficacy end points: proportion of participants with visual acuity 20/40 or better, and 20/20 at 12 and 24 months (Snellen equivalent), total area of and change from baseline CNV lesion, area of leakage Adverse events, including ocular and non-ocular adverse events and proportion of participants developing immunoreactivity to ranibizumab, intraocular inflammation, and IOP Safety assessments: IOP measurement 60 minutes after each injection, incidence and severity of ocular and non-ocular adverse events, changes and abnormalities in clinical laboratory parameters and vital signs, and immunoreactivity to ranibizumab Intervals at which outcomes assessed: 12 and 24 months |
|
| Notes |
Full study name: Minimally Classic/Occult Trial of the Anti-VEGF Antibody Ranibizumab in the Treatment of Neovascular Age-Related Macular Degeneration Type of study: published Funding sources: Genentech, USA and Novartis Pharma, Switzerland Declarations of interest: various authors reported having received consulting fees from Genentech, Eyetech, Novartis Ophthalmics, Novartis, QLT, Alcon Laboratories, Pfizer, Regeneron, Theragenics, VisionCare, Protein Design Labs, Allergan, BioAxone, Tanox, Genaera, Jerini, Oxigene, Quark, Genzyme, iScience, ISTA, and Athenagen; lecture fees from Genentech, Eyetech, Pfizer, Jerini, Allergan, and Novartis Ophthalmics; grant support from Genentech, Novartis, Eyetech, Pfizer, Theragenics, and Genaera and Alcon Laboratories; and/or equity interest in Pfizer and/or being employees of Genentech and owning Genentech stock Study period: enrollment March 2003 to December 2003 Reported subgroup analyses: by baseline lesion (4 or fewer optic-disk areas; more than 4), type of lesion (minimally classic; occult with no classic), and baseline VA (less than 55 letters; 55 or more letters) Contacting study investigators: trial authors contacted and contributed information for this review |
|
| Risk of bias | ||
| Bias | Authors’ judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | “Eligible patients were randomly assigned in a 1:1:1 ratio, using a dynamic randomization algorithm, to receive ranibizumab (LUCENTIS®, Genentech, Inc., South San Francisco, CA) 0.3 or 0.5 mg or a sham injection monthly (30±7 days) for 2 years (24 injections). Randomization was stratified by baseline visual acuity score (<55 letters [approximately worse than 20/80] vs. ≥55 letters) at day 0, by choroidal neovascularization subtype (minimally classic or occult with no classic), and by study center. ” |
| Allocation concealment (selection bias) | Low risk | “A centralized interactive voice response system (IVRS) was used to handle the randomization” (email communication with Genentech, dated 24 October 2007) |
| Masking of participants (performance bias) | Low risk | “All other study site personnel (except those assisting with injections), patients, and central reading center personnel were masked to treatment assignment.” |
| Masking of study personnel (performance bias) | Low risk | “Masking of treatment assignment required at least two investigators per study site: an evaluating physician (masked to treatment assignment), and an injecting physician (unmasked regarding ranibizumab or sham treatment but masked to ranibizumab dose).” |
| Masking of outcome assessment (detection bias) | Low risk | “All other study site personnel (except those assisting with injections), patients, and central reading center personnel were masked to treatment assignment.” |
| Incomplete outcome data (attrition bias) All outcomes |
Low risk | “Efficacy analyses were performed on an intent-to-treat basis (all randomized patients) using a last observation carried forward method to handle missing data.” |
| Selective reporting (reporting bias) | Low risk | We did not have access to the protocol. We matched all outcomes reported in publications with those reported to the FDA |
| Other bias | Unclear risk | Sponsored by Genentech and Novartis Pharma. The study authors disclosed financial interests and/or were paid consultants, employees, and/or shareholders of the funding companies |
| PIER 2008 | ||
| Methods |
Number randomized (total and per group): 184 participants randomly assigned to study treatment; 60 to 0.3 mg ranibizumab, 61 to 0.5 mg ranibizumab, and 63 to sham injection Exclusions after randomization: one participant in the 0.3 mg ranibizumab group withdrew from the study prior to receiving first treatment and was excluded Number analyzed (total and per group): 183 participants; 59 in the 0.3 mg ranibizumab, 61 in the 0.5 mg ranibizumab, and 63 in the sham injection group Unit of analysis: individuals (one study eye per participant) Losses to follow up: 13 participants did not complete 12 months: 1 in the 0.3 mg ranibizumab group, 2 in the 0.5 mg ranibizumab group, and 8 in the sham injection group. Reasons included participant’s decision, participant non-compliance, and need for other therapeutic intervention Compliance: “...treatment compliance was good in the ranibizumab groups, with 85% or more of subjects receiving each scheduled injection. In the sham group, 27% of subjects permanently discontinued treatment before month 12, most often because the subject’s condition mandated another therapeutic intervention.” Intention to treat analysis (Y/N): yes, using last observation carried forward for missing data Reported power calculation: yes, sample of 180 participants for power of 90% Study design comment: following reports of other clinical trials, the study protocol was amended (February 2006) to offer treatment with 0.5 mg ranibizumab to participants in the sham control group who had completed 12 months of follow up and were still being followed. The study protocol was amended again (August 2006) to switch participants in the 0.3 mg ranibizumab group to receive 0.5 mg ranibizumab, to change assessments for all participants from quarterly to monthly after month 12, and to allow treatment with ranibizumab in the fellow eyes |
|
| Participants |
Country: USA (43 study centers) Age: range 54 to 94 years; mean was 79 years in each ranibizumab treatment group and 78 years in the sham injection group Gender (percent): 110/184 (60%) women and 74/184 (40%) men Inclusion criteria: age 50 years or older; primary or recurrent subfoveal CNV secondary to AMD, with total CNV area (classic plus occult CNV) 50% or more of the total lesion area and total lesion size 12 or fewer disc areas; best-corrected visual acuity of 20/40 to 20/320 (Snellen equivalent on ETDRS chart). participants with minimally classic or occult with no classic CNV were included if they had 10% or more increase in lesion size between one and six months prior to day 0, one or fewer Snellen line (or equivalent) VA loss within the prior six months, or CNV-associated subretinal hemorrhage within one month before day zero Exclusion criteria: prior treatment with verteporfin photodynamic therapy, external-beam radiation therapy, transpupillary thermotherapy, or subfoveal laser photocoagulation (or juxtafoveal or extrafoveal laser photocoagulation within one month before day zero); subretinal hemorrhage in the study eye involving the center of the fovea, if the size of the hemorrhage is either 50% or more of the total lesion area or one or more disk areas in size; previous inclusion in antiangiogenic drug trial; prior treatment with photodynamic therapy in non-study eye within seven days before day zero Equivalence of baseline characteristics: yes Diagnoses in participants: 35/184 (19%) had predominantly classic CNV; 69/184 (38%) had minimally classic CNV; 79/184 (43%) had occult with no classic CNV; and 1/184 (< 1%) could not be classified |
|
| Interventions |
Intervention 1: 0.3 mg ranibizumab intravitreal injection every month for first three doses (day 0, months one and two), followed by doses every three months (months 5, 8, 11, 14, 17, 20, and 23) Intervention 2: 0.5 mg ranibizumab intravitreal injection every month for first three doses (day 0, months one and two), followed by doses every three months (months 5, 8, 11, 14, 17, 20, and 23) Intervention 3: sham injection every month for first three doses (day 0, months one and two), followed by doses every three months (months 5, 8, 11, 14, 17, 20, and 23) Length of follow up: Planned: 2 years Actual: 2 years |
|
| Outcomes |
Primary outcomes, as defined: mean change from baseline to 12 months in visual acuity score Secondary outcomes, as defined: proportion of participants losing 15 letters or fewer from baseline; proportion of participants gaining 15 letters or greater from baseline; proportion of participants with a Snellen equivalent of 20/200 or worse; mean change from baseline in the near activities, distance activities, and vision-specific dependency NEI VFQ-25 subscales; and mean change from baseline in total area of CNV and total area of leakage from CNV (based on central reading center assessment) Exploratory efficacy end points: proportion of participants who had lost 30 letters or fewer from baseline VA at 12 months; mean change in visual acuity score from baseline to three months; mean change in visual acuity score from three months to 12 months Adverse events Safety assessments: incidence and severity of ocular and non-ocular adverse events, changes in vital signs, incidence of positive serum antibodies to ranibizumab, IOP measurement 60 minutes after each injection Intervals at which outcomes assessed: injection visits at day 0 and months 1, 2, 3, 8, 11, 14, 17, 20, and 23; clinic visits at months 3, 12, and 24 |
|
| Notes |
Full study name: A Phase IIIb, Multicenter, Randomized, Double-Masked, Sham Injection-Controlled Study of the Efficacy and Safety of Ranibizumab in Subjects with Subfoveal Choroidal Neovascularization with or without Classic CNV Secondary to Age-Related Macular Degeneration Type of study: published Funding sources: Genentech, USA and Novartis Pharma, Switzerland Declarations of interest: various authors reported receiving consulting fees from Genentech, Novartis, OSI/Eyetech, Eyetech/Pfizer, Novartis, and Alcon; lecture fees from Genentech, Novartis, OSI/Eyetech, Eyetech/Pfizer; and grant support from Genentech, Novartis, Alcon, Allergan, Acuity, OSI/Eyetech, and Eyetech/Pfizer; holding Pfizer stock; and/or being an employee and/or stockholder of Genentech Study period: enrollment 7 September 2004 to 16 March 2005 Reported subgroup analyses: none Contacting study investigators: trial authors contacted and contributed information for this review |
|
| Risk of bias | ||
| Bias | Authors’ judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | “Using a dynamic randomization algorithm, subjects were randomly assigned 1: 1:1 to receive 0.3 mg ranibizumab, 0.5 mg ranibizumab, or sham injections. Randomization was stratified by VA score at day zero (≤54 letters [approximately worse than 20/80] vs ≥55 letters [approximately 20/80 or better], CNV type (minimally classic vs occult with no classic vs predominantly classic CNV), and study center.” |
| Allocation concealment (selection bias) | Unclear risk | Method of allocation concealment not reported. Study investigators were contacted, but could not provide additional information (email communication with Dr Regillo, dated 16 May 2012) |
| Masking of participants (performance bias) | Low risk | “All other study site personnel (other than those assisting with study treatment administration), central reading center personnel, and the subjects were masked to treatment assignment.” “For the sham-injected control group, an empty syringe without a needle was used, with pressure applied to the anesthetized and antiseptically prepared eye at the site of a typical intravitreal injection. Pre- and post-injection procedures were identical for all group.” “No subjects were unmasked to their original treatment assignment as a result of these protocol amendments.” |
| Masking of study personnel (performance bias) | Low risk | “To achieve double-masking of treatment assignment, at least two investigators participate at each study site: an ’injecting’ ophthalmologist unmasked to treatment assignment (ranibizumab vs sham) but masked to ranibizumab dose, and a masked ’evaluating’ ophthalmologist for efficacy and safety assessments.” |
| Masking of outcome assessment (detection bias) | Low risk | “To achieve double-masking of treatment assignment, at least two investigators participate at each study site: an ’injecting’ ophthalmologist unmasked to treatment assignment (ranibizumab vs sham) but masked to ranibizumab dose, and a masked ’evaluating’ ophthalmologist for efficacy and safety assessments. All other study site personnel (other than those assisting with study treatment administration), central reading center personnel, and the subjects were masked to treatment assignment.” |
| Incomplete outcome data (attrition bias) All outcomes |
Low risk | “Efficacy analyses used the intent-to-treat approach and included all subjects as randomized. Missing values were imputed using the last-observation-carried-forward method.” |
| Selective reporting (reporting bias) | Low risk | Results were reported for primary and secondary outcomes specified in the Methods section |
| Other bias | Unclear risk | Sponsored by Genentech and Novartis Pharma. The study authors disclosed financial interests and/or were paid consultants, employees, and/or shareholders of the funding companies |
| Sacu 2009 | ||
| Methods |
Number randomized (total and per group): 28 participants randomly assigned to study treatment; 14 in bevacizumab group and 14 in PDT + IVTA group Exclusions after randomization: none Number analyzed (total and per group): 28 total participants; 14 in bevacizumab group and 14 in PDT + IVTA group Unit of analysis: individuals (one study eye per participant) Losses to follow up: one participant in PDT + IVTA group did not complete 6 or 12 month visits Compliance: not reported; no participant was excluded up to 12 months Intention to treat analysis: yes, although the paper does not state how data were imputed for the participant missing the 6 and 12 month follow-up visits in the PDT + IVTA group Reported power calculation: yes, sample of 14 participants per group for power of 80% Study design comment: bevacizumab group had more follow-up visits than the PDT + IVTA group |
|
| Participants |
Country: Vienna, Austria Age: mean 78 years (range 58 to 88) Gender (percent): 19/28 women (68%) and 9/28 men (32%) Inclusion criteria: participants with neovascular AMD of any lesion type; lesion smaller than four disc areas; no prior treatment for neovascular AMD; VA of 20/40 to 20/800 Exclusion criteria: participants with a history of thromboembolic events within the past 3 months and predictable need for ocular surgery Equivalence of baseline characteristics: yes Diagnoses in participants: neovascular AMD |
|
| Interventions |
Intervention 1: 1 mg intravitreal bevacizumab; after 3 initial injections at monthly intervals re-treatment was based on OCT findings only (evidence of persistent or recurrent intra- or subretinal fluid); participants seen at monthly intervals Intervention 2: standard verteporfin PDT plus same day 4 mg intravitreal triamcinolone acetonide; re-treatment at 3 months if there was evidence of leakage by fluorescein angiography Length of follow up: Planned: 12 months Actual: 12 months |
|
| Outcomes |
Primary outcome, as defined: change in mean visual acuity Secondary outcomes, as reported: change in mean 1 mm central retinal thickness; BCVA; StratusOCT; fluorescein angiography; indocyanine green angiography; microperimetry Adverse events Intervals at which outcomes assessed: baseline, months 1, 3, 6, and 12 |
|
| Notes |
Type of study: published Funding sources: not reported Declarations of interest: one investigator reported being “an owner of the patent on the use of green porphyrins in neovasculature of the eye under the guidelines of the Wellman Laboratories of Photomedicine, Harvard Medical School, Boston, MA, USA” Study period: not reported Reported subgroup analyses: none Contacting study investigators: trial authors contacted and contributed information for this review |
|
| Risk of bias | ||
| Bias | Authors’ judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | “In our study we used computer generated randomized scheme and the allocation concealment methods was used (central coordinating center)” (email communication with Dr Stefan Sacu, dated 19 May 2012) |
| Allocation concealment (selection bias) | Low risk | “In our study we used computer generated randomized scheme and the allocation concealment methods was used (central coordinating center)” (email communication with Dr Stefan Sacu, dated 19 May 2012) |
| Masking of participants (performance bias) | High risk | “Open label”; participants could not be masked to treatment groups |
| Masking of study personnel (performance bias) | High risk | “Open label”; physicians were not masked to treatment groups |
| Masking of outcome assessment (detection bias) | High risk | “Patients in the PDT + IVTA groups had characteristic post-treatment hypofluorescence within the area of the PDT treatment spot...” |
| Incomplete outcome data (attrition bias) All outcomes |
Low risk | Intent-to-treat analysis was followed. |
| Selective reporting (reporting bias) | Low risk | Primary and secondary outcomes were reported. |
| Other bias | Low risk | None observed. |
| Subramanian 2010 | ||
| Methods |
Number randomized (total and per group): 28 participants randomly assigned to study treatment; 20 in bevacizumab group and 8 in ranibizumab group Exclusions after randomization: none Number analyzed (total and per group): 22 total participants; 15 in bevacizumab group and 7 in ranibizumab group Unit of analysis: individuals (one study eye per participant) Losses to follow up: six participants: three participants voluntarily dropped out (two in bevacizumab group, one in ranibizumab group); one participant relocated (in bevacizumab group); and two participants died (both in bevacizumab group) Compliance: 22/28 participants completed the study Intention to treat analysis: no, six participants enrolled and randomized were not included in analysis Reported power calculation: yes, 79% power for sample size of 135 participants using 2:1 randomization ratio Study design comment: although the target sample size was 135, only 28 participants were evaluated |
|
| Participants |
Country: Boston, MA, USA Age: not reported for 28 enrolled participants (mean 78 years for analyzed bevacizumab group; mean 80 years for analyzed ranibizumab group) Gender (percent): not reported for 28 enrolled participants (all men for analyzed bevacizumab group; 6 men and 1 woman for analyzed ranibizumab group) Inclusion criteria: age 50 years or older; presence of symptomatic CNV, confirmed by intravenous fluorescein angiogram and optical coherence tomography as affecting the foveal centre; ability to provide informed consent; willing to commit to regular clinic appointments and follow-up; original protocol specified baseline VA between 20/40 and 20/200, later amended to include all baseline VAs equal to or better than 20/400 Exclusion criteria: previous treatment for wet AMD within the past year; presence of subretinal hemorrhage greater than 50% of the size of the lesion on fluorescein angiography, presence of advanced glaucoma; any coexisting macular disease causing decreased vision; history of malignant or uncontrolled hypertension; intraocular inflammation; history of thromboembolic phenomena; inability to provide informed consent; participation in another concurrent ophthalmic clinical trial Equivalence of baseline characteristics: yes Diagnoses in participants: AMD |
|
| Interventions |
Intervention 1: 0.05 ml intravitreal bevacizumab every month for first three months; re-treatment afterwards based on OCT or VA changes Intervention 2: 0.05 ml intravitreal ranibizumab every month for first three months; re-treatment afterwards based on OCT or VA changes Length of follow up: Planned: 12 months Actual: 12 months |
|
| Outcomes |
Primary outcomes, as defined: visual acuity Secondary outcomes, as reported: central foveal thickness by OCT, total number of injections; blood pressure measurements Adverse events Intervals at which outcome assessed: one week after injections to assess adverse events; and monthly through 12 months |
|
| Notes |
Type of study: published Funding sources: Veterans Affairs Boston Healthcare System, USA Declarations of interest: “The authors declare no conflict of interest” Study period: April 2007 to February 2009 Reported subgroup analyses: none Contacting study investigators: trial authors contacted and contributed information for this review |
|
| Risk of bias | ||
| Bias | Authors’ judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | “Patients were enrolled by a 2:1 randomization to either the bevacizumab (2) or the ranibizumab (1) arm of the study.” Study investigators were contacted, but could not provide additional information as to how the sequence was generated (email communication with Dr Subramanian, dated 16 May 2012) |
| Allocation concealment (selection bias) | Low risk | “The Research Pharmacist at the [Veterans Affairs] Hospital Pharmacy was responsible for randomization” and “all subjects were assigned a study number.” |
| Masking of participants (performance bias) | Low risk | Reported as “double-blind”; identical syringes were used to administer agents, and study personnel in contact with participants were all masked |
| Masking of study personnel (performance bias) | Low risk | “To obtain blinding of treatment assignments, the Research Pharmacist at the [Veterans Affairs] Hospital Pharmacy was responsible for randomization, tracking and ensuring the correct study drug was administered to each patient at each visit, and dispensing the same volume of each drug in identical 1 ml syringes.” |
| Masking of outcome assessment (detection bias) | Low risk | “As the only investigator with knowledge of subject assignments, the Research Pharmacist was, in turn, masked to all visual and anatomic outcomes to treatment. All other investigators, as well as other physicians, residents, and office personnel who may have inadvertently come in contact with study subjects, were masked to treatment assignments.” |
| Incomplete outcome data (attrition bias) All outcomes |
High risk | Six of 28 (21%) participants enrolled were not included in the analysis: three voluntarily dropped out; one relocated; and two died |
| Selective reporting (reporting bias) | Unclear risk | Primary outcomes were reported; however, the clinical trials register record for this trial but not the published reports specified quality of life as an outcome |
| Other bias | Low risk | None observed. |
| VISION 2004 | ||
| Methods |
Included trials: two concurrent RCTs (EOP 1003; EOP 1004) Number randomized (total and per group): 1208 participants randomly assigned to study treatment; 297 in 0.3 mg pegaptanib group, 305 in 1.0 mg pegaptanib group, 302 in 3.0 mg pegaptanib group, and 304 in sham injection group Exclusions after randomization: 22 total participants; 18 participants did not receive at least one injection and four participants were not included in the efficacy analyses because “sufficiently standardized assessment of visual acuity was not completed at baseline” Number analyzed (total and per group): 1186 participants at one year; 294 in 0.3 mg pegaptanib group, 300 in 1.0 mg pegaptanib group, 296 in 3.0 mg pegaptanib group, and 296 in sham injection group Unit of analysis: individuals (one study eye per participant) Losses to follow up: 101 at one year; 23 in 0.3 mg pegaptanib group, 25 in 1.0 mg pegaptanib group, 32 in 3.0 mg pegaptanib group, and 21 in sham injection group Compliance: approximately 90% of participants completed the study Intention to treat analysis: no, 22 participants enrolled and randomized were not included in analysis Reported power calculation: yes, sample of 244 participants in each group for power of 95%; at least 270 participants were recruited for each group assuming 10% would have missing data Study design comment: at 54 weeks, participants were re-randomized; those in the pegaptanib groups were randomized to either discontinue treatment or continue with same dose and those in the sham group were randomized to one of five groups: discontinue sham injections, continue with sham injections, or receive injections with 0.3, 1.0, or 3. 0 mg pegaptanib |
|
| Participants |
Country: USA, Canada, Austria, Belgium, Czech Republic, Denmark, France, Germany, Hungary, Israel, Italy, the Netherlands, Poland, Portugal, Spain, Switzerland, UK, Brazil, Chile, Colombia, and Australia (117 study centers) Age: mean age in EOP 1003 was 77 years and in EOP 1004 was 75 years Gender (percent): 696/1190 (58%) women and 494/1190 (42%) men [based on those receiving at least one study treatment] Inclusion criteria: age 50 years or older; subfoveal CNV lesion secondary to AMD; BCVA of 20/40 to 20/320 in the study eye and 20/800 or better in the fellow eye; all angiographic subtypes of total lesion size up to and including 12 disc areas Exclusion criteria: subretinal hemorrhage in study eye 50% or more of lesion area; less than 50% of lesion with active CNV; more than one previous PDT treatment; PDT treatment less than 8 weeks or more than 13 weeks prior to baseline visit; IOP more than 23 mmHg; without clear ocular media; inadequate pupillary dilation for stereoscopic fundus photography; atrophy greater than 25% of total lesion area or subfoveal scarring in the study eye; history of previous subfoveal thermal laser therapy or previous or concomitant therapy with any investigational therapy to treat AMD; need for cataract surgery within two years; other potential causes of CNV such as myopia; having ocular histoplasmosis syndrome, angioid streaks, choroidal rupture, or multifocal choroiditis; any intraocular surgery within three months or extrafoveal/juxtafoveal laser within two weeks of study entry; previous posterior vitrectomy or scleral buckling surgery; presence of retinal pigment epithelial tears or rips; participants with diabetic retinopathy, severe cardiac disease, myocardial infarction within six months, ventricular tachyarrhythmia requiring ongoing treatment, unstable angina, peripheral vascular disease, stroke within 12 months, acute ocular or periocular infection, previous therapeutic radiation to the eye, head, or neck; treatment with any investigational agent within 60 days; allergies to fluorescein dye or to components of the pegaptanib formulation Equivalence of baseline characteristics: yes Diagnoses in participants: 306/1190 (26%) had predominantly classic CNV; 426/1190 (36%) had minimally classic CNV; and 458/1190 (38%) had occult with no classic CNV |
|
| Interventions |
Intervention 1: 0.3 mg pegaptanib intravitreal injection every six weeks; at 54 weeks re-randomization to continue or discontinue treatment Intervention 2: 1.0 mg pegaptanib intravitreal injection every six weeks; at 54 weeks re-randomization to continue or discontinue treatment Intervention 3: 3.0 mg pegaptanib intravitreal injection every six weeks; at 54 weeks re-randomization to continue or discontinue treatment Intervention 4: sham injection every six weeks; at 54 weeks re-randomization to continue sham injections, discontinue sham injections, or treatment with one of three pegaptanib doses (0.3, 1.0, or 3.0 mg) Length of follow up: Planned: 54 weeks after first randomization; 48 weeks after re-randomization Actual: 54 weeks after first randomization; 48 weeks after re-randomization; up to four years for safety outcomes |
|
| Outcomes |
Primary outcome, as defined: proportion of participants losing fewer than 15 letters of VA between baseline and 54 weeks Secondary outcomes, as defined: proportion of participants maintaining or gaining ≤0, 5, 10, or 15 letters, or losing 30 letters or more; mean changes in VA at six-week intervals from baseline to week 54; proportion with VA 20/200 or worse at week 54; changes in size of lesion, size of CNV, and size of leakage at weeks 30 and 54 as measured by color fundus photography and fluorescein angiography Adverse events Intervals at which outcomes assessed: 6-week intervals from baseline to week 54; 6- week intervals from week 54 to week 102; color fundus photography and fluorescein angiography done at baseline, and weeks 30, 54, 78, and 102 |
|
| Notes |
Full study name: VEGF Inhibition Study in Ocular Neovascularization Type of study: published Funding sources: Eyetech Pharmaceuticals, Inc., New York and Pfizer Inc., New York, USA Declarations of interest: various authors reported having served as a paid consultant for Eyetech Pharmaceuticals and Neovista; receiving royalty income from Coherent, the manufacturer of a laser used in photodynamic therapy; and/or being employees of and shareholders in Eyetech Pharmaceuticals Study period: not reported Reported subgroup analyses: none Contacting study investigators: trial authors contacted and contributed information for this review |
|
| Risk of bias | ||
| Bias | Authors’ judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | “Patients were allocated in each trial to one of four treatment arms (sham or 0.3 mg, 1 mg, or 3 mg pegaptanib) by a dynamic procedure using a stochastic treatment allocation algorithm based on the variance method to minimize imbalances simultaneously for study center, angiographic lesion subtype and previous treatment with PDT” |
| Allocation concealment (selection bias) | Low risk | “The study coordinator randomized the patient by going on-line to IDDI (an independent statistics/CRO) and answering eligibility and stratification questions. In response they were instructed which code on the treatment pack to use. Only when it was openend [sic] immediately prior to use would the injecting physician know whether it was active (but not which dose) or sham” (email communication with Eyetech, dated 11 July 2005) |
| Masking of participants (performance bias) | Low risk | “To maintain masking of the patients, the patients receiving sham injections and those receiving the study medication were treated identically, with the exception of scleral penetration. All patients (including those receiving sham injection) underwent an ocular antisepsis procedure and received injected subconjunctival anesthetic. The patients receiving sham injections had an identical syringe - but without a needle - pressed against the eye wall to mimic the active doses that were injected through the pars plana into the vitreous cavity. The injection technique precluded the patient from seeing the syringe.” |
| Masking of study personnel (performance bias) | Low risk | “To maintain masking of the investigators, the study ophthalmologist responsible for patient care and for the assessments did not administer the injection.” |
| Masking of outcome assessment (detection bias) | Low risk | “In all cases, a separate, certified visual-acuity examiner masked to the treatment assignment and to previous measurements of visual acuity assessed distance visual acuity. ” |
| Incomplete outcome data (attrition bias) All outcomes |
Low risk | “For all efficacy analyses, patients were evaluated in the treatment group to which they were randomly assigned. Several analyses of the primary efficacy endpoint that accounted for missing data were also conducted.” At 54 weeks, 18 participants were excluded because they had not received at least one study treatment; four participants were excluded “because a sufficiently standardized assessment of visual acuity was not completed at baseline”; and missing data for about 10% of the study population were imputed using the last observation carried forward method |
| Selective reporting (reporting bias) | Low risk | Primary and secondary outcomes for week 54 (first year) were reported; visual acuity outcomes defined for the first year were not reported in the second year outcomes |
| Other bias | Unclear risk | Sponsored by Eyetech Pharmaceuticals and Pfizer. The study chair and some others involved in the trials were paid consultants, employees, and/or shareholders of Eyetech Pharmaceuticals |
Study acronyms: see Table 1
AMD: age-related macular degeneration
BCVA: best-corrected visual acuity
CMT: central macular thickness
CNV: choroidal neovascularization
CRO: clinical research organization
ETDRS: Early Treatment Diabetic Retinopathy Study
FDA: Food and Drug Administration
IOP: intraocular pressure
IVRS: interactive voice response system
IVTA: intravitreal triamcinolone acetonide
NHS: UK National Health Service
OCT: optical coherence tomography
PDT: photodynamic therapy
RCT: randomized controlled trial
RPE: retinal pigment epithelium
VA: visual acuity
VEGF: vascular endothelial growth factor
Types of interventions
Comparisons of interventions evaluated in the trials included in this review are listed in Table 2 and are summarized here. Among the 12 trials, there were four comparisons of interventions: one study evaluated three doses of pegaptanib versus sham injection (VISION 2004), three studies compared two doses of ranibizumab with sham injections or PDT (ANCHOR 2006;MARINA 2006; PIER 2008), two studies compared bevacizumab with other treatments for AMD (ABC 2010; Sacu 2009), and six studies were head-to-head trials of bevacizumab versus ranibizumab (Biswas 2011; CATT 2011; GEFAL 2013; IVAN 2013; MANTA 2013; Subramanian 2010).
Table 2.
Treatment groups in included trials
| Study Treatment period | Intervention 1 | Intervention 2 | Intervention 3 | Intervention 4 |
|---|---|---|---|---|
| Pegaptanib versus control | ||||
|
VISION 2004 2 years; re-randomized at end of first year |
0.3 mg pegaptanib every 6 weeks | 1.0 mg pegaptanib every 6 weeks | 3.0 mg pegaptanib every 6 weeks | Sham every 6 weeks |
| Ranibizumab versus control | ||||
|
ANCHOR 2006 2 years |
0.3 mg ranibizumab monthly plus sham verteporfin PDT | 0.5 mg ranibizumab monthly plus sham verteporfin PDT | Sham intravitreal injection plus verteporfin PDT | - |
|
MARINA 2006 2 years |
0.3 mg ranibizumab monthly | 0.5 mg ranibizumab monthly | Sham intravitreal injection monthly | - |
|
PIER 2008 2 years |
0.3 mg ranibizumab monthly for 3 months, then every 3 months | 0.5 mg ranibizumab monthly for 3 months, then every 3 months | Sham intravitreal injection monthly for 3 months, then every 3 months | - |
| Bevacizumab versus control | ||||
|
ABC 2010 1 year |
1.25 mg bevacizumab given first three injections every 6 weeks, then as needed | Standard therapy (0.3 mg pegaptanib every six weeks, verteporfin PDT, or sham injection) | - | - |
|
Sacu 2009 1 year |
1.0 mg bevacizumab monthly for 3 months, then as needed | Verteporfin PDT plus same day 4 mg triamcinolone acetonide | - | - |
| Bevacizumab versus ranibizumab | ||||
|
CATT 2011 2 years; re-randomized at end of first year |
1.25 mg bevacizumab monthly for 1 year; at 1 year, re-randomization to ranibizumab monthly or variable dosing | 0.5 mg ranibizumab monthly for 1 year; at 1 year, re-randomization to ranibizumab monthly or variable dosing | 1.25 mg bevacizumab as needed after first injection for 2 years | 0.5 mg ranibizumab as needed after first injection for 2 years |
|
IVAN 2013 2 years; ongoing |
1.25 mg bevacizumab monthly for 2 years | 0.5 mg ranibizumab monthly for 2 years | 1.25 mg bevacizumab monthly for 3 months, then as needed in 3 month cycles | 0.5 mg ranibizumab monthly for 3 months, then as needed in 3 month cycles |
|
Biswas 2011 18 months |
1.25 mg bevacizumab monthly for 3 months, then as needed | 0.5 mg ranibizumab monthly for 3 months, then as needed | - | - |
|
GEFAL 2013 1 year |
1.25 mg bevacizumab; maximum of one injection per month | 0.5 mg ranibizumab; maximum of one injection per month | - | - |
|
MANTA 2013 1 year |
1.25 mg bevacizumab monthly for 3 months, then as needed | 0.5 mg ranibizumab monthly for 3 months, then as needed | - | - |
|
Subramanian 2010 1 year |
0.05 ml bevacizumab monthly for 3 months, then as needed | 0.05 ml ranibizumab monthly for 3 months, then as needed | - | - |
PDT: photodynamic therapy
The VISION 2004 investigators compared sham injections with intravitreal injection of pegaptanib at dosages of 0.3 mg, 1.0 mg, or 3.0 mg given every 6 weeks over a 48-week period.
Two different doses of ranibizumab (0.3 mg and 0.5 mg) were evaluated in three trials (ANCHOR 2006; MARINA 2006; PIER 2008). The control groups and the dosing schedule for ranibizumab differed among the three trials. Monthly intravitreal injection of ranibizumab (for 12 months) was compared with sham intravitreal injections in MARINA 2006. For participants assigned to receive sham intravitreal injections in MARINA 2006, verteporfin PDT was allowed whenever the CNV lesion in their eyes became predominantly classic CNV. Monthly injection of ranibizumab combined with sham PDT (for 24 months) was compared with verteporfin PDT and sham intravitreal ranibizumab injections in ANCHOR 2006. A regimen of monthly injection of ranibizumab for three months followed by an injection every three months was compared with sham intravitreal injections in PIER 2008.
Bevacizumab was evaluated in eight trials. In the ABC 2010 trial, a 1.25 mg dose of bevacizumab was compared with standard therapy. Standard therapy was determined by clinical evaluation and included 0.3 mg pegaptanib, verteporfin PDT, or sham injection. In the small Sacu 2009 trial, a 1 mg dose of bevacizumab was compared with verteporfin PDT combined with intravitreal triamcinolone. In six trials, bevacizumab was compared for non-inferiority with ranibizumab. In both CATT 2011 and IVAN 2013, in addition to the primary comparison of the two agents, monthly injections of the anti-VEGF agents were compared with an ‘as needed’ regimen following three initial injections of the assigned agent. The latter treatment regimen, using a 0.5 mg dose of ranibizumab and a 1.25 mg dose of bevacizumab, was used to compare the two anti-VEGF agents in the Biswas 2011, GEFAL 2013, MANTA 2013, and Subramanian 2010 trials.
Types of outcome measures
Visual acuity
BCVA was the basis of the primary outcome for all the included studies. The primary outcome for this review, the proportion of participants who gained 15 letters or more of BCVA at one year of follow up, was the primary outcome for one study (ABC 2010) and a secondary outcome for the remaining 11 studies. The proportion of participants losing fewer than 15 letters at one year was the primary outcome for the three earliest studies (ANCHOR 2006; MARINA 2006; VISION 2004) and a secondary outcome for the remaining nine studies. The primary outcome was mean change in visual acuity at one year for six studies (CATT 2011;GEFAL 2013; MANTA 2013; PIER 2008; Sacu 2009; Subramanian 2010), and the mean change in visual acuity at 18 months for one study (Biswas 2011). The remaining five studies reported mean change in visual acuity as a secondary outcome. The primary outcome for one study (IVAN 2013) was best-corrected distance visual acuity at two years of follow up; BCVA (as opposed to mean change from baseline) was not an outcome considered in this review.
Other visual acuity outcomes relevant to this review were also reported by some of the included studies. Loss of fewer than 30 letters of visual acuity was reported in five studies (ABC 2010; ANCHOR 2006; MARINA 2006; Subramanian 2010; VISION 2004); BCVA better than 20/200 was reported for eight studies (ANCHOR 2006; CATT 2011; GEFAL 2013; IVAN 2013; MARINA 2006; PIER 2008; Subramanian 2010;VISION 2004); and maintenance of visual acuity (defined as a gain of 0 letters or more) was reported in four studies (ANCHOR 2006; Sacu 2009; Subramanian 2010; VISION 2004). Investigators of included studies reported a number of other visual acuity outcomes that we did not consider in this review.
In all studies, visual acuity was measured using the ETDRS chart, which has a LogMAR scale. Each line on the ETDRS chart consists of 5 letters; thus, a change of 15 letters approximates a 3-line change in visual acuity. The outcome for visual acuity of 20/200 or better was reported as the Snellen equivalent.
Visual function
Visual function outcomes were assessed in five studies. In the ABC 2010 trial, contrast sensitivity and reading ability were specified as secondary outcomes. In the IVAN 2013 trial, contrast sensitivity, near visual acuity, and reading index outcomes were specified as secondary outcomes. We identified one conference abstract in which contrast sensitivity outcomes were reported for the ANCHOR 2006, MARINA 2006, and PIER 2008 trials.
Visual function outcomes were not reported by six studies (Biswas 2011; CATT 2011; MANTA 2013; Sacu 2009; Subramanian 2010; VISION 2004).
Morphological outcomes
All studies included at least one measure relating to the morphological characteristics of neovascular lesions in study eyes. In many cases, sufficient data were not available in publications or conference abstracts to analyze these outcomes informatively. Whenever possible we used data provided by primary investigators or asked primary investigators to confirm data extracted from graphs. We have not reported data derived from graphs in study reports unless confirmation of the data was received from study investigators.
All studies used fluorescein angiography. Fundus photography also was used in five studies (ANCHOR 2006; GEFAL 2013; MARINA 2006; PIER 2008; VISION 2004) and ICG angiography was used in two studies (GEFAL 2013; Sacu 2009). Mean change in the size of CNV was evaluated by fluorescein angiography in six studies (ABC 2010; ANCHOR 2006; GEFAL 2013; MARINA 2006; PIER 2008; VISION 2004) and mean change in the size of neovascular lesions was evaluated by fluorescein angiography in seven studies (ABC 2010; ANCHOR 2006; CATT 2011; IVAN 2013;MARINA 2006; PIER 2008; VISION 2004). OCT for the assessment of subretinal characteristics of eyes with neovascular AMD was not used in the earliest study included in the review (VISION 2004). The next three studies conducted chronologically (ANCHOR 2006; MARINA 2006; PIER 2008) used OCT to assess a subset of study participants. In the eight studies most recently conducted (ABC 2010; Biswas 2011; CATT 2011; GEFAL 2013; IVAN 2013; MANTA 2013; Sacu 2009; Subramanian 2010), OCT was used in all study participants and at least one OCT measure was specified as a primary or secondary outcome. Mean change in CRT was assessed in the 11 studies that used OCT. We considered central macular thickness, central foveal thickness, and center point thickness to be interchangeable terms for CRT.
Other morphological outcomes, such as area of CNV leakage and subretinal fluid, were reported by individual studies, but we did not include these outcomes in this review.
Quality-of-life outcomes
Vision-specific quality of life was evaluated in four studies (ANCHOR 2006; MARINA 2006; PIER 2008; VISION 2004) using the 25-item National Eye Institute-Visual Functioning Questionnaire (NEI-VFQ). The NEI-VFQ, administered by an interviewer, relies on patient-reported responses to specific visual function questions in order to calculate overall and subscale scores, which can range from 0 to 100, with higher values representing better visual function.
One study (IVAN 2013) evaluated general quality of life using the EuroQoL health-related quality of life assessment (EQ-5D). For the EQ-5D, participant responses to specific health questions are converted to scales of 1 to 3, where 1 represents no health problems, 2 represents moderate health problems, and 3 represents extreme health problems. The scores for each of the five subscale domains (mobility, self-care, usual activities, pain/discomfort and anxiety/depression) are then summarized into a single index score ranging from −0.59 to 1.00, with 1.00 representing no health problems. Both the NEI-VFQ and EQ-5D are validated tools by which to assess quality-of-life outcomes.
Quality-of-life outcomes were been reported by seven studies (ABC 2010; Biswas 2011; CATT 2011; GEFAL 2013; MANTA 2013; Sacu 2009; Subramanian 2010).
Economic outcomes
Two studies included economic-related outcomes as prespecified secondary outcomes. In the CATT 2011 study, the annual costs associated with each treatment group were evaluated. In the IVAN 2013 study, cumulative resource use and costs for each treatment group were evaluated.
Adverse events
Ocular and non-ocular adverse events up to one year of follow up were reported by studies (ABC 2010; GEFAL 2013; MANTA 2013; Sacu 2009; Subramanian 2010), up to 18 months of follow up by one study (Biswas 2011), up to two years of follow up by five studies (ANCHOR 2006; CATT 2011; IVAN 2013; MARINA 2006; PIER 2008), and up to four years of follow up by one study (VISION 2004).
Excluded studies
We excluded 41 studies after full-text assessment: 18 studies were not RCTs; 9 studies followed participants for less than one year; 7 studies were dose-response studies in which no control or comparator arm was part of the study; 5 studies compared combination therapies in which treatment groups received the same anti-VEGF therapy; 1 study did not include participants with neovascular AMD; and 1 study evaluated intravitreal aflibercept for the treatment of AMD, which is covered in a separate Cochrane review.
Risk of bias in included studies
Assessments of risks of bias for each included study are given at the end of each respective ‘Characteristics of included studies’ table. When unpublished information was needed to assess the risk of bias for any given parameter, we contacted primary investigators for additional information. We have documented these instances together with the investigators’ responses in the ‘Characteristics of included studies’ tables. Figure 2 summarizes the ‘Risk of bias’ assessments for all 12 studies.
Figure 2.
Risk of bias summary: review authors’ judgements about each risk of bias item for each included study.
Allocation
Overall the included studies were at low risk of selection bias. Reports from 11 of the 12 studies described methods of random sequence generation that we judged to confer a low risk of bias; the method used in the Subramanian 2010 trial was not described in sufficient detail for us to assess its risk of bias. The most common method used for random sequence generation was dynamic randomization, used in five studies (ABC 2010; ANCHOR 2006;MARINA 2006; PIER 2008;VISION 2004). Three studies used permuted block randomization designs (CATT 2011; IVAN 2013; MANTA 2013), two studies used random number tables or lists (Biswas 2011; GEFAL 2013), and one study only reported using a computer-randomized schema (Sacu 2009).
Investigators of 10 of the 12 trials reported adequate allocation concealment. In Biswas 2011, it was unclear whether the randomization sequence, determined by random number tables generated prior to study enrollment, was concealed or made available to the study investigators. Reports from the PIER 2008 study did not describe how assignments were allocated; we were unable to make an assessment using available information. In seven studies a third party or central coordinating center was employed (ABC 2010; ANCHOR 2006;GEFAL 2013;MANTA 2013;MARINA 2006; Sacu 2009; Subramanian 2010) and in three studies (CATT 2011; IVAN 2013; VISION 2004) a computer-based portal was used for allocation concealment.
Communication with investigators from the Biswas 2011, Subramanian 2010, and PIER 2008 studies did not yield additional information about the methods used to assess these risks of bias (email communications).
Masking (performance bias and detection bias)
Most of the included studies we judged to be at low risk of performance bias and detection bias. Only one study (Sacu 2009) was an open-label study in which no form of masking was employed. Participants in the CATT 2011 study initially were masked to the drug (not to the dosing schedule), but may have become aware of the treatment assignments due to billing records. The authors of Biswas 2011 did not report whether study participants were masked. In both the Biswas 2011 and CATT 2011 studies, personnel and outcome assessors were masked. In the remaining nine studies, study participants, personnel (other than personnel directly administering treatment), and outcome assessors were masked; thus, we assessed these studies as being at low risk of performance bias and detection bias. The most common method used to mask participants in studies in which intravitreal injections were compared to no injections was the use of sham injections when participants were not assigned or did not require an injection. In the head-to-head studies of ranibizumab versus bevacizumab, participants were masked as to which treatment group they were assigned. To minimize detection bias, study investigators who were involved with assessing outcomes were separate from the treating physicians and masked to treatment groups, with the exception of the Sacu 2009 study in which no masking was done.
Incomplete outcome data
In all 12 trials, few participants missed the follow-up examination specified as the primary time for assessing the study’s primary outcome or were not treated in accord with the randomized treatment assignment. In nine trials, the rates of loss to follow up at the primary follow-up visits were less than 15%; the GEFAL 2013, MANTA 2013, and Subramanian 2010 studies had 19%, 23%, and 21% missing data, respectively. Losses to follow up were evenly balanced across treatment groups among the included studies.
Seven trials included in this review analyzed the data using methods designed to overcome, in part, loss of information due to missed follow-up examinations. Six of these seven trials used the last-observation-carried-forward method to impute missing data (ABC 2010; ANCHOR 2006; MANTA 2013; MARINA 2006; PIER 2008; VISION 2004) and the seventh trial (Sacu 2009) did not report the method for imputing data for one participant with missing data. The remaining five trials reported the available-case data in which only participants with data were included in the analyses: 91.5% in CATT 2011, 81% in GEFAL 2013, 89% in IVAN 2013, 87% in Biswas 2011, and 79% in Subramanian 2010. The investigators of all trials reported that they had analyzed data for participants by the treatment arms to which they had been assigned. However, analyses using single imputation methods or available-case data assume that participants are lost to follow up at random and may introduce bias if this assumption is not true.
Selective reporting
With the exception of the Biswas 2011 study, we identified protocols or clinical trial registrations for 11 of the included studies. We judged seven of these 11 trials to be free of reporting bias based on the consistency between study outcomes defined in the protocols and clinical trial registrations and those reported in the study results papers. Although quality-of-life outcomes were specified, we identified no report of quality-of-life findings from the Subramanian 2010 trial. We also found no reports of reading ability outcomes, which were specified as secondary outcomes in the ABC 2010 trial. Results for three outcomes specified in the IVAN 2013 trial protocol were not reported in published articles of the one-year and two-year results: treatment satisfaction, survival free from treatment failure, and exploratory (serum) analysis. Differences in outcomes between the trial registration and the published one-year results paper of the GEFAL 2013 study included differences in details of outcome specification (e.g., efficacy of treatments versus proportion of participants with a gain of 15 letters or more of visual acuity), outcomes specified in the trial registration not reported in the paper, and a newly added outcome in the paper that was not listed in the trial registration.
Other potential sources of bias
Various other aspects of trial design, reporting, trial sponsorship, and financial interests of investigators were considered as other potential sources of bias.
ANCHOR 2006, MARINA 2006, PIER 2008, and VISION 2004 were sponsored by pharmaceutical companies marketing the study drugs under investigation; data from these trials were submitted to the FDA to obtain approval of ranibizumab and pegaptanib. In addition, the pharmaceutical company sponsors had important roles in the trial design, analysis, and reporting. Some investigators from other trials reported that they received financial support from pharmaceutical companies; however, because the companies did not have direct sponsorship of the trials we did not judge these trials to be at risk of bias for this domain (CATT 2011; GEFAL 2013; IVAN 2013). We observed no other potential sources of bias in the remaining five studies.
Effects of interventions
See: Summary of findings for the main comparison Summary of findings: bevacizumab versus ranibizumab; Summary of findings 2 Summary of findings: pegaptanib versus control; Summary of findings 3 Summary of findings: ranibizumab versus control; Summary of findings 4 Summary of findings: bevacizumab versus control
We conducted meta-analyses of results by drug, combining different doses and regimens of the same drug evaluated in the individual trials, as evident from Table 2. In the forest plots reported in this review, it should be noted that, for all visual acuity outcomes, effect estimates to the right of the vertical line of the forest plots (i.e., risk ratios > 1 and mean differences > 0) favor the test treatment.
Pegaptanib versus sham
One study, comprising two individual RCTs, compared three doses of intravitreal pegaptanib (0.3 mg, 1.0 mg, and 3.0 mg) with a sham injection control group (VISION 2004). The study was conducted at 117 international centers and enrolled 1208 adult participants (50 years of age or older) with subfoveal CNV lesions secondary to AMD. Findings from the two trials were combined in study reports. There were 904 participants in the pegaptanib groups and 304 in the sham injection group. At one year of follow up, 1186 (98%) participants were included in the primary analyses and 1053 (87%) remained in the study and were re-randomized according to their original treatment assignment. Participants in the pegaptanib groups were re-randomized to continue current treatment or discontinue treatment and participants in the sham group were re-randomized to continue with sham injections, discontinue sham injections, or receive one of the three study doses of pegaptanib. Study follow up continued for one year after the re-randomization and participants were analyzed in three cohorts: those who continued with their original assignments, those who discontinued treatment, and those who received sham injections during the first year then pegaptanib during the second year. In total, 1053 (87%) participants were included in the two-year analysis; however, we did not analyze the two-year data since results were reported for changes from year 1 to year 2 rather than from baseline to year 2.
The VISION 2004 study, sponsored by Eyetech Pharmaceuticals and Pfizer, was assessed as having a low risk of bias inmost domains. The study had high retention rate (90% of participants followed for one year and 85% for two years).
(1) Visual acuity
(a) Gain of 15 letters or more of visual acuity
More participants in the combined pegaptanib groups than in the sham group had a gain of 15 letters or more of visual acuity at year 1. Since gaining vision is a positive outcome, an RR greater than 1 favors treatment with pegaptanib. The RR for the combined pegaptanib versus sham groups was 2.83 (95% CI 1.23 to 6.52); that is, eyes treated with pegaptanib were 2.83 times more likely to gain 15 letters or more of vision than eyes treated with sham injections (Analysis 1.1; Figure 3).
Figure 3.
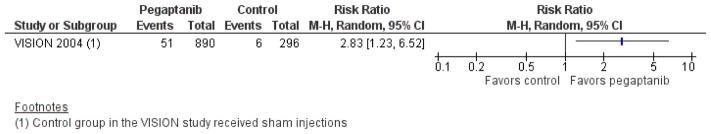
Forest plot of comparison: 1 Pegaptanib versus control, outcome: 1.1 Gain of 15 letters or more visual acuity at one year.
(b) Loss of fewer than 15 letters of visual acuity
At one year, the RR for loss of fewer than 15 letters of visual acuity when comparing the combined pegaptanib groups with the sham group favored treatment with pegaptanib and was 1.24 (95% CI 1.11 to 1.39) (Analysis 1.2).
(c) Loss of fewer than 30 letters of visual acuity
At one year, the RR for the combined pegaptanib groups versus the sham group was 1.15 (95% CI 1.08 to 1.23), indicating that eyes treated with pegaptanib were 15% (95% CI 8% to 23%) less likely to have lost 30 letters or more of vision compared with eyes treated with sham therapy (Analysis 1.3).
(d) Prevention of blindness (visual acuity better than 20/200)
Pegaptanib resulted in fewer blind participants across the three treatment groups at one year of follow up. The pooled RR for having visual acuity better than 20/200 was 1.33 (95% CI 1.15 to 1.52) compared with sham therapy (Analysis 1.4).
(e) Maintenance of visual acuity
A greater number of participants treated with pegaptanib maintained visual acuity at one year. The pooled RR for pegaptanib versus sham therapy was 1.49 (95% CI 1.19 to 1.88) (Analysis 1.5).
(f) Mean change in visual acuity
The study investigators provided us with the data required to analyze the mean change in visual acuity at one year of follow up. Visual acuity was measured using the ETDRS chart placed at 2 m from the participant. The mean change from baseline in number of letters read on the ETDRS chart was measured. The final mean visual acuity in the three active treatment groups was consistently greater than in the sham group.
The MD in mean change in visual acuity from baseline between the combined pegaptanib groups versus the sham group was 6.72 letters (95% CI 4.43 to 9.01), meaning that eyes treated with pegaptanib lost on average 6.72 letters fewer than eyes in the sham-treated group (Analysis 1.6). On the logMAR scale, 0.10 log-MAR units correspond to 1 line (5 letters) on the visual acuity chart. Thus, the MD between the pegaptanib and sham groups was equivalent to 0.13 logMAR units; that is, the mean change in visual acuity was less in the pegaptanib groups than in the sham group by 0.13 logMAR units.
(2) Visual function
Visual function outcomes were not reported in VISION 2004.
(3) Morphological outcomes
Mean change in size of CNV
Insufficient information was available to analyze the mean change in size of CNV; however, study investigators provided data allowing us to evaluate mean CNV size at one year of follow up. Given that baseline CNV sizes were comparable among all study participants, the difference in the mean size of CNV between study groups at one year may be used to estimate the treatment effect. Total CNV sizes were measured as numbers of standard DA. Pegaptanib treatment, across all doses studied, resulted in a lower final mean CNV size compared to the sham group at one year of follow up (MD 0.92 DAs; 95% CI 0.42 to 1.42) (Analysis 1.7). We considered a difference in size of CNV of one DA or more as a clinically meaningful difference.
Mean change in size of lesion
Insufficient information was available to analyze the mean change in size of total subfoveal lesion; however, study investigators provided data allowing us to analyze the mean size of lesion at one year of follow up. Mean size of lesion is described in terms of standard DA. Pegaptanib treatment resulted in a lower mean size of lesion at one year of follow up compared to sham treatment (MD 0.86 DAs; 95% CI 0.35 to 1.37) (Analysis 1.8).
Mean change in CRT
OCT was not used in the VISION 2004 study; CRT outcomes were not measured.
(4) Quality-of-life outcomes
Vision-related quality of life was measured in one of the two trials from the VISION 2004 study using the NEI-VFQ questionnaire (EOP 1004). Since it was validated only for United States English, this questionnaire was administered only to participants from the United States and Canada, 578 (48%) of 1208 total study participants, at baseline and at weeks 30 and 54 of follow up. At one year, data were available for 569 (98%) of the 578 study participants who completed the questionnaire at baseline. Treatment with pegaptanib was associated with better scores on the NEI-VFQ questionnaire, specifically for distance vision and role limitation domains. However, standard deviations for scores were not reported.
(5) Economic outcomes
We did not find any report of economic outcomes comparing pegaptanib with sham treatment from the VISION 2004 study.
(6) Adverse events
Ocular and systemic adverse events were reported in the VISION 2004 study. Participants in the pegaptanib groups experienced an ocular adverse event nearly four times more often (RR 3.84; 95% CI 0.91 to 16.20) and were 1.25 times more likely to have a serious systemic adverse event (RR 1.25; 95% CI 0.93 to 1.70) than participants in the control group. Results for the most frequent adverse events are shown in Table 3. Although uncommon, 12 eyes treated with pegaptanib injections for one year developed endophthalmitis, compared to no cases in control eyes. Because of the small number of events, risk estimates for individual adverse events are imprecise.
Table 3.
Adverse events up to one year: pegaptanib vs. control
| Ocular adverse event* | 0.3 mg pegaptanib n = 295 |
1.0 mg pegaptanib n = 301 |
3.0 mg pegaptanib n = 296 |
All doses pegaptanib n = 892 |
Control n = 298 |
RR [95% CI] All doses vs. control |
|---|---|---|---|---|---|---|
| Any eye disorder | 9 (3%) | 4 (1%) | 10 (3%) | 23 (3%) | 2 (< 1%) | 3.84 [0.91, 16. 20] |
| Endophthalmitis | 6 (2%) | 3 (1%) | 3 (1%) | 12 (1%) | 0 | 8.37 [0.50, 140. 95] |
| Retinal detachment | 1 (< 1%) | 2 (< 1%) | 2 (< 1%) | 5 (< 1%) | 0 | 3.68 [0.20, 66. 41] |
| Traumatic cataract | 1 (< 1%) | 2 (< 1%) | 2 (< 1%) | 5 (< 1%) | 0 | 3.68 [0.20, 66. 41] |
| Retinal hemorrhage | 1 (< 1%) | 0 | 1 (< 1%) | 2 (< 1%) | 0 | 1.67 [0.08, 34. 77] |
| Vitreous hemorrhage | 0 | 0 | 1 (< 1%) | 1 (< 1%) | 0 | 1.00 [0.04, 24. 59] |
| Uveitis | 0 | 0 | 1 (< 1%) | 1 (< 1%) | 0 | 1.00 [0.04, 24. 59] |
| Elevated intraocular pressure | 1 (< 1%) | 0 | 0 | 1 (< 1%) | 0 | 1.00 [0.04, 24. 59] |
| Papilledema | 0 | 0 | 0 | 0 | 1 (< 1%) | 0.11 [0.00, 2.73] |
| Non-ocular adverse event* | 0.3 mg pegaptanib n = 295 |
1.0 mg pegaptanib n = 301 |
3.0 mg pegaptanib n = 296 |
All doses pegaptanib n = 892 |
Control n = 298 |
RR [95% CI] All doses vs. control |
|---|---|---|---|---|---|---|
| At least 1 serious adverse event | 55 (19%) | 50 (17%) | 64 (22%) | 169 (19%) | 45 (15%) | 1.25 [0.93, 1.70] |
| Cardiac disorders | 11 (4%) | 4 (1%) | 10 (3%) | 25 (3%) | 14 (5%) | 0.60 [0.31, 1.13] |
| Neoplasms (benign, malignant, unspecified) | 11 (4%) | 7 (2%) | 8 (3%) | 26 (3%) | 12 (4%) | 0.72 [0.37, 1.42] |
| Injury and procedural complications, such as fractures (also includes traumatic cataracts) | 10 (3%) | 9 (3%) | 8 (3%) | 27 (3%) | 3 (1%) | 3.01 [0.92, 9.84] |
| Nervous system disorders | 10 (3%) | 5 (2%) | 10 (3%) | 25 (3%) | 7 (2%) | 1.19 [0.52, 2.73] |
| Infections and infestations | 2 (<1%) | 7 (2%) | 11 (4%) | 20 (2%) | 5 (2%) | 1.34 [0.51, 3.53] |
| Gastrointestinal disorders | 3 (1%) | 6 (2%) | 5 (2%) | 14 (2%) | 4 (1%) | 1.17 [0.39, 3.52] |
| Respiratory, thoracic, mediastinal disorders | 2 (< 1%) | 5 (2%) | 5 (2%) | 12 (1%) | 4 (1%) | 1.00 [0.33, 3.08] |
| Musculoskeletal and connective tissue | 1 (< 1%) | 5 (2%) | 3 (1%) | 9 (1%) | 2 (<1%) | 1.50 [0.33, 6.92] |
| Renal and urinary disorders | 2 (< 1%) | 3 (1%) | 2 (<1%) | 7 (<1%) | 3 (1%) | 0.78 [0.20, 3.00] |
| Vascular disorders | 3 (1%) | 2 (< 1%) | 2 (< 1%) | 7 (< 1%) | 3 (1%) | 0.78 [0.20, 3.00] |
CI: confidence interval
RR: risk ratio
Most frequent serious adverse events experienced by 1190 participants in the VISION 2004 study
Ranibizumab versus control
Three studies comprising a total of 1323 participants compared two doses of intravitreal ranibizumab (0.3 mg or 0.5 mg) with sham or control treatment. In the ANCHOR 2006 study, 280 participants received ranibizumab and 143 participants received verteporfin PDT therapy. Injections were administered monthly and verteporfin PDT therapy was administered on day 0 and as needed at visits at months 3, 6, 9, and 12. In the MARINA 2006 study, 478 participants received ranibizumab and 238 participants received sham injections. All injections were administered on a monthly basis. In the PIER 2008 study, 121 participants received ranibizumab and 63 participants received sham injections. Injections were administered monthly for the first three months, then every three months. During the second year of the PIER 2008 study, participants in the 0.3 mg ranibizumab and sham-treated groups crossed over to receive 0.5 mg ranibizumab.
Overall, we rated the risk of bias as low among the three studies. Participant masking in all studies was achieved by the use of sham injections and by sham PDT therapy in the ANCHOR 2006 study. Although the clinicians administering treatment were not masked, those assessing outcomes were masked to treatment groups. At one year of follow up, two participants, one participant in the ANCHOR 2006 study and one in the PIER 2008 study, were excluded from the analyses. The remaining study participants were analyzed and missing data were imputed using the last-observation-carried-forward method. All three studies were funded by pharmaceutical companies (Genentech, USA, and Novartis Pharma, Switzerland).
(1) Visual acuity
(a) Gain of 15 letters or more of visual acuity
At one year of follow up, we observed substantial statistical heterogeneity in the effect of ranibizumab compared with sham therapy for a gain of 15 letters or more of visual acuity; the I2 statistic was 80% and the Chi2 test for heterogeneity was statistically significant (P value < 0.01) (Analysis 2.1; Figure 4). Therefore, we did not combine study results in meta-analysis. The RR for a gain of 15 letters or more of visual acuity comparing the combined ranibizumab groups with sham control was 6.79 (95% CI 3.41 to 13.54) in ANCHOR 2006, 5.81 (95% CI 3.29 to 10.26) in MARINA 2006, and 1.30 (95% CI 0.53 to 3.19) in PIER 2008. Although the direction of treatment effect in all three trials included in this analysis favored ranibizumab, the magnitude of effect observed in PIER 2008 was smaller and not statistically significant compared with that observed in MARINA 2006 and ANCHOR 2006. This difference may have been attributable to differences among the studies with respect to dosing schedules (monthly injections in ANCHOR 2006 and MARINA 2006 versus injections monthly for the first three months, then every three months in PIER 2008).
Figure 4.
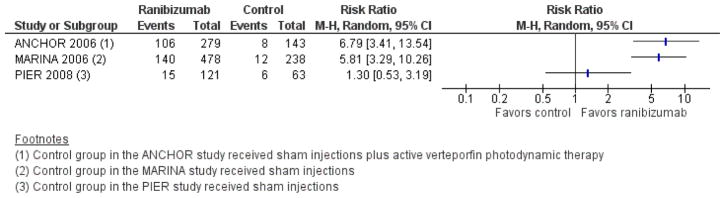
Forest plot of comparison: 2 Ranibizumab versus control, outcome: 2.1 Gain of 15 letters or more visual acuity at one year.
At two years of follow up, there was less statistical heterogeneity for this outcome, as indicated by the I2 statistic (30%) and the Chi2 test for heterogeneity (Analysis 2.2), although the PIER 2008 findings still deviated somewhat from those of the other two trials. The proportion of participants who were treated with ranibizumab and gained 15 letters or more at two years was 5.77 times the proportion of participants treated with control interventions who gained 15 letters or more (RR 5.77; 95% CI 3.38 to 9.84) (Analysis 2.2).
(b) Loss of fewer than 15 letters of visual acuity
A greater proportion of participants treated with ranibizumab lost fewer than 15 letters of visual acuity at one year of follow up compared with those treated with sham or control therapy. Participants were 1.53 times more likely to not lose 15 letters or more of visual acuity when treated with ranibizumab compared with sham or control therapy (RR 1.53; 95% CI 1.41 to 1.64) (Analysis 2.3). We observed no statistical heterogeneity among the three trials (I2 = 0) and the CIs of the individual trials overlapped one another. At two-year follow-up, the beneficial effect of ranibizumab persisted at a similar magnitude and was statistically significant when compared with sham or control therapy. Nearly twice as many participants treated with ranibizumab lost fewer than 15 letters of visual acuity at two years of follow up than those in control groups (RR 1.62; 95% CI 1.32 to 1.98) (Analysis 2.4). We observed substantial statistical heterogeneity in the analysis comparing ranibizumab with control (I2 = 78%; P value for Chi2 test of heterogeneity = 0.01); however, the CIs among the individual studies overlapped and the effect estimates were in the same direction. This difference may have been attributable to the control group in the ANCHOR 2006 study receiving an active treatment (verteporfin PDT therapy) compared with sham injections in MARINA 2006 and PIER 2008.
(c) Loss of fewer than 30 letters of visual acuity
Data for this outcome were available from only two of the three trials that compared ranibizumab with control interventions (ANCHOR 2006;MARINA 2006). At one-year follow up, fewer than 1%of participants treated with ranibizumab lost 30 letters or more of visual acuity (5/757) compared with 14% in the control groups (53/381). Comparing both ranibizumab groups combined with controls, we observed a 15% benefit of ranibizumab with respect to the loss of fewer than 30 letters of visual acuity (RR 1.15; 95% CI 1.11 to 1.20) (Analysis 2.5). The meta-analysis for this outcome revealed no statistical heterogeneity (I2 = 0%) and the point estimates and CIs of the two studies analyzed overlapped. The treatment effect persisted through two years, with fewer participants treated with ranibizumab losing 30 letters or more (16/757, 2%) than participants in the control groups (77/381, 20%). Comparing both ranibizumab groups combined versus controls, we observed a 22% benefit of ranibizumab with respect to the loss of fewer than 30 letters of visual acuity after two years (RR 1.22; 95% CI 1.15 to 1.29) (Analysis 2.6).
(d) Prevention of blindness (visual acuity better than 20/200)
Ranibizumab resulted in fewer cases of blindness at both one and two years of follow up compared with control interventions. In a meta-analysis comparing the combined ranibizumab groups with the control intervention groups, a greater proportion of participants in the ranibizumab groups had visual acuity better than 20/200 than participants in the control group at one year (RR 1.69; 95% CI 1.41 to 2.03) (Analysis 2.7) and two years (RR 1.73; 95% CI 1.52 to 1.98) (Analysis 2.8). Although the point estimates and CIs of the individual studies overlapped one another, some degree of statistical heterogeneity was observed for this outcome (I2 = 62% at one year and 26% at two years).
(e) Maintenance of visual acuity
Data on the maintenance of visual acuity were available for only one of the three trials comparing ranibizumab with a control intervention (ANCHOR 2006). At both one and two years of follow up, a greater proportion of participants treated with ranibizumab maintained visual acuity (i.e., visual acuity at follow up was the same as or better than at baseline), compared with participants in the control group. At one year, the RR for the maintenance of visual acuity comparing ranibizumab with control was 2.53 (95% CI 1.95 to 3.27) (Analysis 2.9). At two years, the corresponding effect estimate was 2.71 (95% CI 2.08 to 3.54) (Analysis 2.10).
(f) Mean change in visual acuity
On average, at both one and two years of follow up, participants treated with ranibizumab read more letters on ETDRS charts placed at 4 m than participants in the control groups. Participants treated with ranibizumab were able to read 18 letters more at the one-year follow up (MD 17.80, 95% CI 15.95 to 19.65) (Analysis 2.11) and 20 letters more at the two-year follow up (MD 20.11, 95% CI 18.08 to 22.15) (Analysis 2.12) than participants in the control groups.
(2) Visual function
Visual function outcomes were not specified as outcomes of interest by any of the three trials; however, we identified one conference abstract that discussed contrast sensitivity outcomes in participants from these trials (see Korobelnik 2006 under ANCHOR 2006). No between-group comparisons were reported for contrast sensitivity as measured using Pelli-Robson charts, but the abstract author reported that participants in the ranibizumab groups had statistically significant increases of 2 to 4 letters (i.e., approximately one contrast level) after one year. Participants in the control groups lost an average of 3 letters (i.e., one contrast level) at one year. The MD comparing ranibizumab with control would be 6 letters (i.e., two contrast levels on the Pelli-Robson chart), based on data extracted from the abstract.
(3) Morphological outcomes
Mean change in size of CNV
We were unable to identify and extract any data on mean change in size of the CNV from any of the three included trials comparing ranibizumab with control interventions.
Mean change in size of lesion
Data on the mean change in size of the total subfoveal lesion were available from two of the three included trials comparing ranibizumab with control interventions (ANCHOR 2006; PIER 2008). The mean reduction in the size of the lesion was greater by 2.34 DAs (95% CI 1.88 to 2.81) among participants treated with ranibizumab compared with participants treated with control interventions after one year (Analysis 2.13). At two years, this effect persisted in the ANCHOR 2006 study (MD 2.44, 95% CI 1.87 to 3.00), but was muted in the PIER 2008 study (MD 0.59, 95% CI −0.55 to 1.73) (Analysis 2.14). Due to substantial statistical heterogeneity (I2 = 88%) and differences in control groups in the two trials during the second year of follow up, we did not combine these studies in a meta-analysis.
Mean change in CRT
We were unable to find data on CRT in reports from any of the three included trials comparing ranibizumab with control interventions.
(4) Quality-of-life outcomes
Vision-related quality of life was measured in all three trials using an interviewer-administered NEI-VFQ questionnaire at baseline, and after one and two years of follow up. Two trials provided sufficient data to include in meta-analysis (ANCHOR 2006; MARINA 2006). The investigators of both studies considered a 10-point change in scores as clinically meaningful.
At one year, overall vision-related quality of life improved more often among participants in ranibizumab groups compared with participants in control groups (MD 6.69; 95% CI 3.38 to 9.99). The MD was greater in the MARINA 2006 study (MD 8.20; 95% CI 6.05 to 10.35) than in the ANCHOR 2006 study (MD 4.81; 95% CI 1.74 to 7.87). This difference between the two trials may be because participants in the control group of the ANCHOR 2006 study received an active treatment, verteporfin PDT therapy. Subscale domains of the NEI-VFQ questionnaire in which participants in ranibizumab groups showed greater improvement at one-year of follow up than participants in control groups included near-vision activities, distance-vision activities, vision-related dependency, driving ability, general health, role difficulties, mental health, general vision, social functioning, color vision, and peripheral vision (Analysis 2.15). The I2 statistic for subscale analyses ranged from 0 to 91%, which may have been due to differences in control groups. No combined MDs differed by more than 10 points between ranibizumab and control groups.
At two years, overall vision-related quality of life improved more often among participants in ranibizumab groups compared with participants in control groups (MD 8.63; 95% CI 3.31 to 13.95). Similar to one-year results, the MD was greater in the MARINA 2006 study (MD 11.15; 95% CI 8.81 to 13.48) than in the ANCHOR 2006 study (MD 5.70; 95% CI 1.96 to 9.44). Subscale domains of the NEI-VFQ questionnaire in which participants in ranibizumab groups showed greater improvement at two years of follow up compared with participants in control groups were consistent with those identified at one-year (Analysis 2.16). The I2 statistic for subscale analyses ranged from 0 to 87%, reflecting greater comparative differences between the treatment and sham control groups in the MARINA 2006 study than between the treatment and active control groups in the ANCHOR 2006 study. For five subscales, MDs differed by more than 10 points between the ranibizumab and control groups: near vision activities, distance vision activities, vision-related dependency, driving ability, and mental health (Analysis 2.16).
We did not extract the limited data available from the third trial (PIER 2008) because the data in the full-text articles were presented only as graphs and the information contained in the conference abstracts was insufficient for inclusion in our analysis. Correspondence with the trial investigators did not yield additional information for data analysis.
(5) Economic outcomes
We did not identify data on economic outcomes comparing ranibizumab with controls directly from the ANCHOR 2006, MARINA 2006, and PIER 2008 studies. Estimates of the cost of treatment with ranibizumab were reported to be USD 27,004 for the first year and USD 26,417 for the second year, based on data from the MARINA 2006 study; data were not reported for the control group (Brown 2008).
(6) Adverse events
Ocular and systemic adverse events were reported in the ANCHOR 2006 and PIER 2008 studies at one-year follow up (Table 4) and in all three studies at two-year follow up (Table 5). At both the one- and two-year follow ups, there were small numbers of participants who experienced ocular adverse events, such as endophthalmitis, uveitis, retinal detachment, and retinal or vitreous hemorrhage, and non-ocular adverse events, such as myocardial infarction, stroke or cerebral infarction, ischemic cardiomyopathy, and death (< 1% of total participants). Because of the small number of events, risk estimates for these adverse events are imprecise.
Table 4.
Adverse events up to one year: ranibizumab vs. control
| Ocular adverse event* | 0.3 mg ranibizumab n = 196 |
0.5 mg ranibizumab n = 201 |
All doses ranibizumab n = 397 |
Control n = 206 |
RR [95% CI] All doses vs. control |
|---|---|---|---|---|---|
| Endophthalmitis | 0 | 2 (< 1%) | 2 (< 1%) | 0 | 2.60 [0.13, 53.92] |
| Retinal detachment | 1 (< 1%) | 0 | 1 (< 1%) | 1 (< 1%) | 0.52 [0.03, 8.25] |
| Traumatic cataract | 18 (9%) | 22 (11%) | 40 (10%) | 14 (7%) | 1.48 [0.83, 2.66] |
| Retinal hemorrhage | 2 (1%) | 0 | 2 (< 1%) | 2 (< 1%) | 0.52 [0.07, 3.66] |
| Vitreous hemorrhage | 1 (< 1%) | 0 | 1 (< 1%) | 0 | 1.56 [0.06, 38.13] |
| Uveitis | 0 | 1 (< 1%) | 1 (< 1%) | 0 | 1.56 [0.06, 38.13] |
| Elevated intraocular pressure (30 mmHg or more increase) | 13 (7%) | 17 (8%) | 30 (8%) | 7 (3%) | 2.22 [0.99, 4.98] |
| Ocular inflammation (trace to 4+) | 21 (11%) | 26 (13%) | 47 (12%) | 9 (4%) | 2.71 [1.36, 5.42] |
| Non-ocular adverse event* | 0.3 mg ranibizumab n = 196 |
0.5 mg ranibizumab n = 201 |
All doses ranibizumab n = 397 |
Control n = 206 |
RR [95% CI] All doses vs. control |
|---|---|---|---|---|---|
| Death | 3 (2%) | 2 (<1%) | 5 (1%) | 2 (< 1%) | 1.30 [0.25, 6.63] |
| Myocardial infarction | 1 (< 1%) | 3 (1%) | 4 (1%) | 1 (< 1%) | 2.08 [0.23, 18.45] |
| Stroke or cerebral infarction | 1 (< 1%) | 1 (< 1%) | 2 (< 1%) | 1 (< 1%) | 1.04 [0.09, 11.38] |
| Ischemic cardiomyopathy | 0 | 0 | 0 | 1 (< 1%) | 0.17 [0.01, 4.24] |
| Treatment-emergent hypertension | 7 (4%) | 15 (7%) | 22 (6%) | 17 (8%) | 0.67 [0.36, 1.24] |
| Non-ocular hemorrhage | 9 (5%) | 13 (6%) | 22 (6%) | 6 (3%) | 1.90 [0.78, 4.62] |
CI: confidence interval
RR: risk ratio
Adverse events experienced by 420 participants in the ANCHOR 2006 study and 183 participants in the PIER 2008 study. Adverse events at one-year follow up not reported in MARINA 2006.
Table 5.
Adverse events up to two years: ranibizumab vs. control
| Ocular adverse event* | 0.3 mg ranibizumab n = 434 |
0.5 mg ranibizumab n = 440 |
All doses ranibizumab n = 874 |
Control n = 441 |
RR [95% CI] All doses vs. control |
|---|---|---|---|---|---|
| Endophthalmitis | 2 (< 1%) | 6 (1%) | 8 (< 1%) | 0 | 8.59 [0.50, 148.44] |
| Retinal detachment | 2 (< 1%) | 0 | 2 (< 1%) | 2 (< 1%) | 0.50 [0.07, 3.57] |
| Traumatic cataract | 65 (15%) | 76 (17%) | 141 (16%) | 57 (13%) | 1.25 [0.94, 1.66] |
| Retinal hemorrhage | 1 (< 1%) | 0 | 1 (< 1%) | 1 (< 1%) | 0.50 [0.03, 8.05] |
| Vitreous hemorrhage | 3 (< 1%) | 1 (< 1%) | 4 (< 1%) | 2 (< 1%) | 1.01 [0.19, 5.49] |
| Uveitis | 3 (< 1%) | 4 (< 1%) | 7 (<1%) | 0 | 7.58 [0.43, 132.36] |
| Elevated intraocular pressure (30 mmHg or more increase)** | 45 (15%) | 61 (20%) | 106 (18%) | 11 (4%) | 4.81 [2.63, 8.81] |
| Ocular inflammation (1+ to 4+) | 32 (7%) | 30 (7%) | 62 (7%) | 8 (2%) | 3.91 [1.89, 8.09] |
| Non-ocular adverse event* | 0.3 mg ranibizumab n = 434 |
0.5 mg ranibizumab n = 440 |
All doses ranibizumab n = 874 |
Control n = 441 |
RR [95% CI] All doses vs. control |
|---|---|---|---|---|---|
| Death | 12 (3%) | 9 (2%) | 21 (2%) | 13 (3%) | 0.82 [0.41, 1.61] |
| Myocardial infarction | 7 (2%) | 8 (2%) | 15 (2%) | 7 (2%) | 1.08 [0.44, 2.63] |
| Stroke or cerebral infarction | 6 (1%) | 6 (1%) | 12 (1%) | 5 (1%) | 1.21 [0.43, 3.42] |
| Ischemic cardiomyopathy | 0 | 0 | 0 | 1 (< 1%) | 0.17 [0.01, 4.12] |
| Treatment-emergent hypertension | 60 (14%) | 69 (16%) | 129 (15%) | 68 (15%) | 0.96 [0.73, 1.25] |
| Nonocular hemorrhage | 38 (9%) | 40 (9%) | 78 (9%) | 24 (5%) | 1.64 [1.05, 2.55] |
CI: confidence interval
RR: risk ratio
Adverse events experienced by 420 participants in the ANCHOR 2006 study; 713 participants in the MARINA 2006 study; and 182 participants in the PIER 2008 study.
Adverse events for elevated intraocular pressure not reported in the ANCHOR 2006 study at two-year follow up (n = 297 in 0.3 mg ranibizumab group, n = 300 in 0.5 mg ranibizumab group, and n = 298 in 0.3 mg control group).
With respect to ocular adverse events, eyes treated with ranibizumab more often developed cataracts compared with eyes in the control groups at both the one year (RR 1.48; 95% CI 0.83 to 2.66) and two year follow ups (RR 1.25; 95% CI 0.94 to 1.66). Elevated intraocular pressure (IOP), defined as a 30 mmHg or more increase, occurred more often in eyes in the ranibizumab groups than eyes in the control groups at both one-year (RR 2.22; 95% CI 0.99 to 4.98) and two-year follow up (RR 4.81; 95% CI 2.63 to 8.81). Ocular inflammation, graded from trace (1+) to 4+, also occurred more often in eyes in the ranibizumab groups than in eyes in the control groups at both the one year (RR 2.71; 95% CI 1.36 to 5.42) and two year follow ups (RR 3.91; 95% CI 1.89 to 8.09). Two eyes during the first year of ranibizumab injections and six more during the second year developed endophthalmitis, compared to no cases in the control eyes.
With respect to non-ocular adverse events, participants in the ranibizumab groups less often experienced treatment-emergent hypertension than participants in the control groups at one-year follow up (RR 0.67; 95% CI 0.36 to 1.24); however, at two-year follow up the risk was the same between the ranibizumab and control groups (RR 0.96; 95% CI 0.73 to 1.25). Non-ocular hemorrhage occurred more often in participants in the ranibizumab groups than in participants in the control groups at both one-year (RR 1.90; 95% CI 0.78 to 4.62) and two-year follow up (RR 1.64; 95% CI 1.05 to 2.55).
Bevacizumab versus control
Two studies of 159 total participants compared intravitreal bevacizumab injections with control treatment. In the ABC 2010 study, 131 participants received either 1.25 mg intravitreal bevacizumab (65 participants) or standard therapy consisting of pegaptanib injections (38 participants), verteporfin PDT (16 participants), or sham injections (12 participants). In Sacu 2009, 28 participants received either 1.0 mg intravitreal bevacizumab (14 participants) or verteporfin PDT with 4 mg intravitreal triamcinolone acetonide (14 participants). In both studies intravitreal bevacizumab was administered as needed following the first three scheduled injections. We assessed both studies as having a low risk of bias overall.
(1) Visual acuity
(a) Gain of 15 letters or more of visual acuity
At one year of follow up, the overall RR for a gain in 15 letters or more of visual acuity for bevacizumab versus control treatment was 7.80 (95% CI 2.44 to 24.98) (Analysis 3.1; Figure 5); that is, nearly eight times as many people treated with bevacizumab gained 15 letters or more of visual acuity after one year of treatment compared with control.
Figure 5.
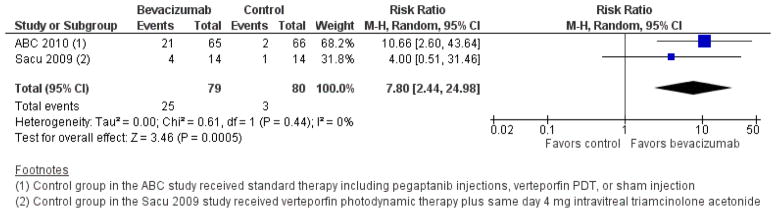
Forest plot of comparison: 3 Bevacizumab versus control, outcome: 3.1 Gain of 15 letters or more visual acuity at one year.
(b) Loss of fewer than 15 letters of visual acuity
More participants treated with bevacizumab lost fewer than 15 letters of visual acuity at one year of follow up compared with participants in the control group. The overall RR for bevacizumab versus control treatment was 1.28 (95% CI 1.09 to 1.50) (Analysis 3.2).
(c) Loss of fewer than 30 letters of visual acuity
In the ABC 2010 study, 64/65 participants in the bevacizumab group did not lose 30 letters or more visual acuity at one year of follow-up compared with 63/66 participants in the control group (RR 1.03; 95% CI 0.97 to 1.10). The authors of Sacu 2009 did not report results for this outcome.
(d) Prevention of blindness (visual acuity better than 20/200)
Blindness was not reported in Sacu 2009. The authors of the ABC 2010 trial noted that more participants in the bevacizumab group than in the control group had visual acuities of 20/200 or better at one year.
(e) Maintenance of visual acuity
Maintenance of visual acuity was not reported in the ABC 2010 study. In Sacu 2009, a greater proportion of participants in the bevacizumab group (11/14) maintained visual acuity at one year compared with participants in the control group (5/14) (RR 2.20; 95% CI 1.03 to 4.68).
(f) Mean change in visual acuity
Insufficient data were available to analyze the difference in mean changes in visual acuity between treatment groups. In the ABC 2010 trial, the mean change from baseline in visual acuity was 7.0 letters in the bevacizumab group and −9.4 letters in the control group at one year of follow up. This equates to a MD of 16.4 letters (more than 3 lines of visual acuity); however, we were unable to compute the standard error (SE) using information available. The authors of Sacu 2009 reported a statistically significant difference between groups at one year, when participants in the bevacizumab group had gained 8 letters on average and participants in the control group had lost 3 letters on average.
(2) Visual function
Visual function outcomes were not reported in Sacu 2009. Outcomes for contrast sensitivity, measured with Pelli-Robson charts, were reported from the ABC 2010 trial. Although the published protocol for the ABC 2010 trial lists reading ability (including a maximum reading speed, critical print size, and reading acuity), measured with Minnesota Reading charts, as a secondary outcome for the study, we did not identify reports with results for this outcome.
At one year, no statistical difference was observed between bevacizumab and control groups in terms of a gain of 15 letters or more (i.e., five levels of contrast) of contrast sensitivity (RR 2.03; 95% CI 0.39 to 10.71); however, a greater proportion of participants in the bevacizumab group (23/65) compared with the control group (10/66) gained 6 letters or more (i.e., two levels of contrast) of contrast sensitivity (RR 2.34; 95% CI 1.21 to 4.51). Also, participants in the control group more often lost 6 letters or more (two contrast levels) of contrast sensitivity compared to participants in the bevacizumab group (RR 0.22; 95% CI 0.07 to 0.72).
(3) Morphological outcomes
Mean change in size of CNV
The median change in the size of CNV was reported in the ABC 2010 study. At 54 weeks, the size of CNV regressed by 0.88 mm2 (interquartile range (IQR), reduction of 4.08 mm2 to increase of 0.40 mm2) in the bevacizumab-treated group compared with 0.27 mm2 (IQR, reduction of 2.58 mm2 to increase of 1.24 mm2) in the control group. The authors of Sacu 2009 did not report results for this outcome.
Mean change in size of lesion
The median change in the size of the subfoveal lesion was reported only for the ABC 2010 study. At 54 weeks, the size of the total subfoveal lesion regressed by 0.03 mm2 (IQR, reduction of 1.88 mm2 to increase of 2.63 mm2) in the bevacizumab-treated group and increased by 2.33 mm2 (IQR, reduction of 0.06 mm2 to increase of 6.44 mm2) in the control group. The authors of Sacu 2009 did not report results for this outcome.
Mean change in CRT
In the ABC 2010 study, the mean change in CRT at 54 weeks was −91 μm in the bevacizumab group and −55 μm in the control group (P value = 0.08). In Sacu 2009, the mean change in CRT at 12 months was −113 μm in the bevacizumab group and −72 μm in the control group (P value = 0.8; analysis of variance, ANOVA). No measures of variability were reported for these outcomes, precluding meta-analysis.
(4) Quality-of-life outcomes
Quality-of-life outcomes were not assessed by the investigators of the ABC 2010 or Sacu 2009 trials.
(5) Economic outcomes
Economic outcomes were not assessed by the investigators of the ABC 2010 or Sacu 2009 trials.
(6) Adverse events
Serious ocular and non-ocular adverse events occurring among 65 bevacizumab-treated participants and 66 control participants were reported in the ABC 2010 study. Serious ocular events affecting at least one study participant included uveitis (two bevacizumab participants; one control participant), rhegmatogenous retinal detachment (no bevacizumab participants; one control participant), vitreous hemorrhage (one bevacizumab participant; no control participants), and ocular inflammation (eight bevacizumab participants; four control participants). No instances of presumed endophthalmitis, retinal tear, or lens damage were reported in either group. Three participants experienced a non-ocular adverse event: myocardial infarction (bevacizumab group), death due to vascular cause (bevacizumab group), and non-ocular hemorrhage reported as serious (control group).
The authors of Sacu 2009 reported no occurrences of severe ocular or systemic events during the study period.
Bevacizumab versus ranibizumab
Six non-inferiority trials directly compared intravitreal bevacizumab with intravitreal ranibizumab. There were 2806 total participants in the six studies. In the largest study, 1208 participants were randomized in a 2 × 2 factorial design (two drugs administered in two dosing schedules) to receive 1.25 mg intravitreal bevacizumab or 0.5 mg intravitreal ranibizumab on a monthly or as-needed basis (CATT 2011). Participants in the as-needed dosing groups received the first three injections monthly; they then received an injection whenever treatment was needed based on monthly examinations. After one year of treatment, participants in the groups treated monthly were re-randomized to continue treatment on a monthly basis or to change to treatment as needed. Participants in the as-needed dosing groups remained on their original assignments and all participants were followed for another year. The IVAN 2013 study, with 628 participants, had four treatment groups similar to those in the CATT study: 1.25 mg intravitreal bevacizumab monthly, 0.5 mg intravitreal ranibizumab monthly, 1.25 mg intravitreal bevacizumab as needed, and 0.5 mg intravitreal ranibizumab as needed. Participants in the as-needed dosing groups received the first three injections monthly; they then received three consecutive monthly treatments whenever treatment was needed. The treatment period was two years. In the four smaller studies, participants were randomized to receive 1.25 mg intravitreal bevacizumab or 0.5 mg intravitreal ranibizumab on an as-needed basis for one year (GEFAL 2013; MANTA 2013; Subramanian 2010) or 18 months (Biswas 2011). We included the 18-month data with the 12-month data.
For the data analyses in this section, we combined groups of the same drug type regardless of dosing regimen. Thus the bevacizumab and ranibizumab groups include both monthly and as needed dosing schedules. Risk of bias in most domains was low among the studies and none of these studies was funded by pharmaceutical companies. At one-year follow up, data for the primary outcome were reported for 2446 (87%) of 2806 participants.
(1) Visual acuity
(a) Gain of 15 letters or more of visual acuity
Overall, the proportion of participants who gained 15 letters or more of visual acuity at one year did not differ statistically significantly between bevacizumab- and ranibizumab-treated groups (RR 0.90; 95% CI 0.73 to 1.11) (Analysis 4.1; Figure 6). Individual results for five of the six trials crossed unity and the I2 statistic was 34%.
Figure 6.
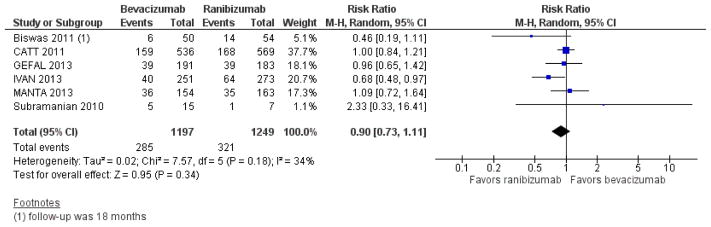
Forest plot of comparison: 4 Bevacizumab versus ranibizumab, outcome: 4.1 Gain of 15 letters or more visual acuity at one year.
At two years, data were available for 1030 (85%) of 1208 participants in the CATT 2011 trial and 517 (82%) of 628 participants in the IVAN 2013 trial. Results were consistent with one-year outcomes in terms of the effect estimate and CIs when comparing the proportion of participants who gained 15 letters or more of visual acuity between ranibizumab- and bevacizumab-treated groups (RR 0.84; 95% CI 0.64 to 1.11) (Analysis 4.2). When analyzing only the 778 participants who remained in their originally randomized groups in the CATT 2011 trial (i.e., excluding participants who were switched to a different treatment regimen after one year), summary results were unchanged (RR 0.84; 95% CI 0.64 to 1.11). The I2 statistics for these analyses were at or about 50% indicating a difference in treatment effect between the CATT 2011 and IVAN 2013 trials.
(b) Loss of fewer than 15 letters of visual acuity
At one year of follow up, the overall RR for the loss of fewer than 15 letters of visual acuity was 1.00 (95% CI 0.98 to 1.02) when comparing participants treated with bevacizumab and those treated with ranibizumab (Analysis 4.3). The CIs for all six individual studies also crossed the line of unity. These results suggest that there was no clinical or statistical difference between the two drugs in terms of the loss of fewer than 15 letters of visual acuity after one year of treatment.
At two years of follow up, the relative treatment effect between the two drugs was almost identical to the relative effect at one year when analyzing participants based on their original randomization (RR 0.97; 95% CI 0.94 to 1.00) or participants who remained in their originally randomized groups (RR 0.98; 95% CI 0.94 to 1.01) (Analysis 4.4).
(c) Loss of fewer than 30 letters of visual acuity
No participant in the Subramanian 2010 study lost 30 letters or more of visual acuity during the one-year study period. This outcome was not reported by the other five trials.
(d) Prevention of blindness (visual acuity better than 20/200)
Four trials reported the proportion of participants with visual acuity better than 20/200 as an outcome (CATT 2011;GEFAL 2013; IVAN 2013; Subramanian 2010) and two did not (Biswas 2011; MANTA 2013).
At one year of follow up, the proportion of participants with visual acuity better than 20/200 was neither clinically nor statistically significantly different when comparing participants treated with bevacizumab and participants treated with ranibizumab (RR 0.98; 95% CI 0.96 to 1.01) (Analysis 4.5). There was no statistical heterogeneity among studies (I2 = 0%) and the CIs for these four individual studies all crossed the line of unity.
At two years, results were consistent with one-year outcomes in that no significant difference in the proportion of participants with visual acuity better than 20/200 was observed between bevacizumab- and ranibizumab-treated groups (RR 1.00; 95% CI 0.95 to 1.06) (Analysis 4.6). When analyzing only the 778 participants in the CATT 2011 trial who remained in their originally randomized groups, results were similar (RR 1.01; 95% CI 0.95 to 1.06). There was moderate statistical heterogeneity between the CATT 2011 and IVAN 2013 trials for these analyses (I2 > 40%), which could be an artifact of the precision of the individual study effect estimates.
(e) Maintenance of visual acuity
Maintenance of visual acuity was not reported in the CATT 2011, GEFAL 2013, IVAN 2013, or MANTA 2013 trials. In Subramanian 2010, 10/15 (67%) participants maintained baseline visual acuity after one year of treatment with bevacizumab and 6/7 (86%) participants maintained baseline visual acuity after one year of treatment with ranibizumab (RR 0.78; 95% CI 0.49 to 1.24).
The investigators of Biswas 2011 reported different cut-points for the change in visual acuity at 18 months follow up. In the bevacizumab group, 16 (32%) participants gained more than 5 letters, 30 (60%) participants did not change more than 5 letters, and 4 (8%) participants lost more than 5 letters of visual acuity. In the ranibizumab group, 18 (33%) participants gained more than 5 letters, 30 (56%) participants did not change more than 5 letters, and 6 (11%) participants lost more than 5 letters of visual acuity.
(f) Mean change in visual acuity
At one year, the mean difference in mean change in visual acuity between bevacizumab and ranibizumab groups was less than 1 ETDRS letter (MD −0.51, 95% CI −1.64 to 0.62) (Analysis 4.7). The CIs for all six individual studies crossed the line of no difference and the I2 statistic was 0%.
Data for the mean change from baseline in visual acuity at two years were reported in the IVAN 2013 trial and for only the 778 participants who remained in their originally randomized groups in the CATT 2011 trial. The mean difference between bevacizumab and ranibizumab groups was less than 2 ETDRS letters (MD −1.15, 95% CI −2.82 to 0.51) (Analysis 4.8).
(2) Visual function
Only one of the six trials comparing bevacizumab with ranibizumab reported visual function outcomes (IVAN 2013).
At one year, participants in the ranibizumab and bevacizumab groups were comparable in regard to mean letters of contrast sensitivity (adjusted MD 0.20; 95% CI −0.47 to 0.87) and reading index (MD −5.53; 95% CI −14.59 to 3.54). Participants in the ranibizumab groups had slightly better (8%) near LogMAR visual acuity compared with participants in the bevacizumab group (adjusted geometric mean ratio 0.92; 95% CI 0.84 to 1.00; P value = 0.058).
At two years of follow up, results for visual function outcomes were similar to those at one year. Participants in the ranibizumab and bevacizumab groups were comparable in regard to mean letters of contrast sensitivity (adjusted MD 0.21; 95% CI −0.62 to 1.04) and reading index (MD −1.34; 95% CI −8.29 to 5.61). Participants in the ranibizumab groups had slightly better (6%) near LogMAR visual acuity compared with participants in the bevacizumab group (adjusted geometric mean ratio 0.94; 95% CI 0.85 to 1.04).
(3) Morphological outcomes
Mean change in size of CNV
One study reported mean change in size of CNV from baseline (GEFAL 2013). At one year, there was no difference observed between bevacizumab (156 participants) and ranibizumab (144 participants) groups (MD 0.00 DAs; 95% CI −0.32 to 0.32).
Mean change in size of lesion
In two of the six studies, the outcome of change in size of total lesion was reported. We considered a difference of one or more DAs as a clinically meaningful difference.
In the CATT 2011 study, the mean change in size of lesion was similar in both the bevacizumab (479 participants) and ranibizumab (509 participants) groups at one year (MD 0.20 optic DAs; 95% CI −0.09 to 0.49). Among the 778 participants who remained in their originally randomized groups through two years, participants in the bevacizumab groups (341 participants) showed larger increases in lesion size compared with those in the ranibizumab groups (360 participants) (MD 1.37 mm2; 95% CI 0.39 to 2.36). In the IVAN 2013 study, the median change in lesion size after one year of treatment was similar in both the bevacizumab (median −1.79 DAs; IQR −5.18 to 0.00) and ranibizumab (median −1.92 DAs; IQR −4.81 to −0.01) groups. After two years, the median change in size of lesion was −1.86 DAs (IQR −5.51 to 0.16) in the bevacizumab group and −0.96 DAs (IQR −4.29 to 0.39) in the ranibizumab group.
Mean change in size of lesion was not reported in Biswas 2011, GEFAL 2013, MANTA 2013, or Subramanian 2010. The authors of MANTA 2013 reported that “no significant difference was observed in terms of lesion size between the two groups (P = 0.55)”.
Mean change in CRT
Five of the six trials reported mean change in CRT at one year. Participants treated with bevacizumab showed less reduction in CRT compared with participants treated with ranibizumab in four trials (MD −13.97 μm; 95% CI −26.52 to −1.41) (Analysis 4.9). This difference is not considered to be clinically meaningful as it falls within the typical range of measurement error. The authors of Subramanian 2010 reported a mean change of −50 μm in the bevacizumab group and −91 μm in the ranibizumab group at one year. Mean change in CRT was not reported as an outcome in the MANTA 2013 study reports; however, the investigators reported that “differences were not significant between the groups (P = 0.81)”.
At two years, the trend was similar among the study participants who remained in their originally randomized groups in the CATT 2011 and IVAN 2013 trials. Participants in the bevacizumab groups showed less reduction in CRT compared with participants in the ranibizumab groups (MD −12.40 μm; 95% CI −33.83 to − 9.04) (Analysis 4.10).
(4) Quality-of-life outcomes
One study (IVAN 2013) evaluated quality of life using the EQ-5D.
At one-year of follow up, the median (IQR) EQ-5D summary score was the same for both the bevacizumab- and ranibizumab-treated groups (median 0.85; IQR 0.73 to 1.00). The number of participants who reported “no health problems” for each of the five subscale domains was similar between groups (Analysis 4.11).
At two-year follow up, the median (IQR) EQ-5D summary score was the same as at the one year follow up (median 0.85; IQR 0.73 to 1.00) in both the bevacizumab- and ranibizumab-treated groups. The number of participants who reported “no health problems” for each of the five subscale domains was similar in the two groups (Analysis 4.12).
Quality-of-life outcomes have not been reported from the remaining five studies (Biswas 2011; CATT 2011; GEFAL 2013; MANTA 2013; Subramanian 2010).
(5) Economic outcomes
Three studies included economic-related outcomes as prespecified secondary outcomes. In the CATT 2011 study, the annual costs associated with each treatment group were evaluated in USD. In the IVAN 2013 study, cumulative resource use and costs for each treatment group were evaluated in GBP. In the GEFAL 2013 study, medicoeconomic outcomes were prespecified as secondary outcomes of interest; however, no results for economic outcomes were published with the one-year results.
The average annual cost of treatment per participant was USD 490 in the bevacizumab groups (USD 595 when treated monthly and USD 385 when treated as needed) compared with USD 18,590 (USD 23,400 when treated monthly and USD 13,800 when treated as needed) in the ranibizumab groups in the first year of the CATT 2011 study. For the 778 participants who remained in their originally randomized groups, the average cost of two years of treatment was USD 860 per participant in the bevacizumab groups (USD 1170 when treated monthly and USD 705 when treated as needed) and USD 31,805 per participant in the ranibizumab groups (USD 44,800 when treated monthly and USD 25,200 when treated as needed).
In the IVAN 2013 study, the average total cost of treatment per participant for the first year was GBP 1580 in the bevacizumab groups (GBP 1654 when treated monthly and GBP 1509 when treated as needed) compared with GBP 8035 in the ranibizumab groups (GBP 9656 when treated monthly and GBP 6398 when treated as needed). These values corresponded to approximately USD 2500 and USD 12,700 for the bevacizumab and ranibizumab groups, respectively (based on an average exchange rate of 1.58 for years 2010 to 2011). The mean difference was GBP 8001 (SE 113) when comparing monthly treatment with ranibizumab versus bevacizumab, and GBP 4889 (SE 184) when comparing as-needed treatment with ranibizumab versus bevacizumab. Economic outcomes at two years of follow up have not been reported for the IVAN 2013 study.
(6) Adverse events
Although all six trials reported information related to adverse events, there was variation in the types of adverse events reported among studies.
At one year, no serious ocular events were reported in three trials (Biswas 2011;MANTA 2013; Subramanian 2010). Minor adverse events reported in these three trials included subconjunctival hemorrhage, increased IOP, transient post-injection pain, and mild ocular inflammation; the numbers of participants who experienced these adverse events were not reported. There were no cases of endophthalmitis or retinal detachment in these three trials. In the CATT 2011, GEFAL 2013, and IVAN 2013 studies, less than 1% of participants had endophthalmitis, retinal detachment, retinal pigment epithelial tear, traumatic cataract, or uveitis (Table 6). Because of the small number of events, risk estimates for these adverse events are imprecise.
Table 6.
Adverse events up to one year: bevacizumab vs. ranibizumab
| Serious ocular adverse event | Studies reporting adverse event* | Bevacizumab | Ranibizumab | RR [95% CI] Bevacizumab vs. ranibizumab |
||
|---|---|---|---|---|---|---|
| Number with event | Total participants | Number with event | Total participants | |||
| Endophthalmitis | CATT 2011; GEFAL 2013 | 4 (< 1%) | 832 | 3 (< 1%) | 838 | 1.34 [0.30, 5.98] |
| Retinal detachment | CATT 2011; GEFAL 2013 | 3 (< 1%) | 832 | 0 | 838 | 7.05 [0.36, 136. 28] |
| Retinal pigment epithelial tear | CATT 2011; IVAN 2013 | 3 (< 1%) | 882 | 3 (< 1%) | 913 | 1.04 [0.21, 5.11] |
| Traumatic cataract | CATT 2011; GEFAL 2013; IVAN 2013 | 1 (< 1%) | 1128 | 2 (< 1%) | 1152 | 0.51 [0.05, 5.62] |
| Severe uveitis | CATT 2011; IVAN 2013 | 4 (< 1%) | 882 | 1 (< 1%) | 913 | 4.14 [0.46, 36. 97] |
| Non-ocular adverse event | Studies reporting adverse event** | Bevacizumab | Ranibizumab | RR [95% CI] Bevacizumab vs. ranibizumab |
||
|---|---|---|---|---|---|---|
| Number with event | Total participants | Number with event | Total participants | |||
| At least 1 serious adverse event | CATT 2011; GEFAL 2013; IVAN 2013; MANTA 2013 | 227 (18%) | 1282 | 183 (14%) | 1315 | 1.27 [1.06, 1.52] |
| Death | CATT 2011; GEFAL 2013; IVAN 2013; MANTA 2013 | 25 (2%) | 1282 | 20 (2%) | 1315 | 1.28 [0.72, 2.30] |
| Myocardial infarction | CATT 2011; GEFAL 2013; IVAN 2013; MANTA 2013 | 8 (< 1%) | 1282 | 10 (< 1%) | 1315 | 0.82 [0.32, 2.07] |
| Stroke or cerebral infarction | CATT 2011; GEFAL 2013; IVAN 2013; MANTA 2013 | 5 (< 1%) | 1282 | 8 (< 1%) | 1315 | 0.64 [0.21, 1.95] |
| Transient ischemic attack | CATT 2011; GEFAL 2013; IVAN 2013 | 4 (< 1%) | 1128 | 4 (< 1%) | 1152 | 1.02 [0.26, 4.07] |
| Venous thrombotic event | CATT 2011; GEFAL 2013; IVAN 2013 | 8 (< 1%) | 1128 | 2 (< 1%) | 1152 | 4.09 [0.87, 19. 20] |
| Cardiac disorders | CATT 2011; GEFAL 2013; IVAN 2013; MANTA 2013 | 37 (3%) | 1282 | 36 (3%) | 1315 | 1.05 [0.67, 1.66] |
| Gastrointestinal disorders | CATT 2011; GEFAL 2013; IVAN 2013; MANTA 2013 | 24 (2%) | 1282 | 11 (< 1%) | 1315 | 2.24 [1.10, 4.55] |
| Infections | CATT 2011; GEFAL 2013; IVAN 2013; MANTA 2013 | 42 (3%) | 1282 | 27 (2%) | 1315 | 1.60 [0.99, 2.57] |
| Injury and procedural complications | CATT 2011; GEFAL 2013; IVAN 2013; MANTA 2013 | 30 (2%) | 1282 | 21 (2%) | 1315 | 1.47 [0.84, 2.55] |
| Neoplasms (benign, malignant, unspecified) | CATT 2011; GEFAL 2013; IVAN 2013; MANTA 2013 | 20 (2%) | 1282 | 21 (2%) | 1315 | 0.98 [0.53, 1.79] |
| Nervous system disorders | CATT 2011; GEFAL 2013; IVAN 2013; MANTA 2013 | 25 (2%) | 1282 | 24 (2%) | 1315 | 1.07 [0.61, 1.86] |
| Surgical or medical procedure | CATT 2011; GEFAL 2013; IVAN 2013; MANTA 2013 | 26 (2%) | 1282 | 13 (1%) | 1315 | 2.05 [1.06, 3.97] |
CI: confidence interval
RR: risk ratio
CATT 2011 (n = 586 in bevacizumab group; n = 599 in ranibizumab group); GEFAL 2013 (n = 246 in bevacizumab group; n = 239 in ranibizumab group); IVAN 2013 (n = 296 in bevacizumab group; n = 314 in ranibizumab group)
CATT 2011 (n = 586 in bevacizumab group; n = 599 in ranibizumab group); GEFAL 2013 (n = 246 in bevacizumab group; n = 239 in ranibizumab group); IVAN 2013 (n = 296 in bevacizumab group; n = 314 in ranibizumab group); MANTA 2013 (n = 154 in bevacizumab group; n = 163 in ranibizumab group)
At one year, no serious systemic adverse events were reported in Subramanian 2010. Systemic adverse events were not assessed in Biswas 2011. In the remaining four trials (CATT 2011; GEFAL 2013; IVAN 2013; MANTA 2013), 18%of participants in the bevacizumab groups versus 14% of participants in the ranibizumab groups experienced at least one serious adverse event (RR 1.27; 95% CI 1.06 to 1.52). Mortality from any cause was approximately 2% in both the bevacizumab and ranibizumab groups in the first year of follow up (RR 1.28; 95% CI 0.72 to 2.30). Less than 1%of participants had a myocardial infarction, stroke or cerebral infarction, transient ischemic attack, or venous thrombotic event (Table 6). Rates were comparable between bevacizumab and ranibizumab groups with respect to cardiac disorders (RR 1.05; 95% CI 0.67 to 1.66), neoplasms (RR 0.98; 95% CI 0.53 to 1.79), and nervous system disorders (RR 1.07; 95% CI 0.61 to 1.86). There were more gastrointestinal disorders (RR 2.24; 95% CI 1.10 to 4.55), infections (RR 1.60; 95% CI 0.99 to 2.57), injuries and procedural complications (RR 1.47; 95% CI 0.84 to 2.55), and surgical or medical procedures (RR 2.05; 95% CI 1.06 to 3.97) reported in the bevacizumab groups compared with ranibizumab groups at one year.
At two years, data for ocular and systemic adverse events were available for the CATT 2011 and IVAN 2013 trials. Less than 1% of participants had endophthalmitis, retinal detachment, retinal pigment epithelial tear, traumatic cataract, or uveitis (Table 7). Because of the small number of events, risk estimates for these adverse events are imprecise. In the bevacizumab groups, 36% of participants had at least one serious adverse event compared with 30% in the ranibizumab groups (RR 1.20; 95% CI 1.05 to 1.37). Mortality from any cause was 6% and 5% in the bevacizumab and ranibizumab groups, respectively (RR 1.12; 95% CI 0.76 to 1.65). There were 2% or fewer participants with myocardial infarction, stroke or cerebral infarction, venous thrombotic event, or transient ischemic attack (Table 7). As with one-year outcomes, more gastrointestinal disorders (RR 2.74, 95% CI 1.49 to 5.02), infections (RR 1.37, 95% CI 0.96 to 1.95), and injuries and procedural complications (RR 1.33, 95% CI 0.86 to 2.05) were reported in the bevacizumab groups compared with ranibizumab groups. More cardiac disorders were also reported in the bevacizumab groups compared with ranibizumab groups at two years (RR 1.25; 95% CI 0.92 to 1.71). Rates were comparable between bevacizumab and ranibizumab groups with respect to neoplasms (RR 0.98; 95% CI 0.63 to 1.53), nervous system disorders (RR 1.06; 95% CI 0.70 to 1.60), and surgical or medical procedures (RR 0.91; 95% CI 0.44 to 1.84).
Table 7.
Adverse events up to two years: bevacizumab vs. ranibizumab
| Ocular adverse event (CATT trial)* | Bevacizumab n = 586 |
Ranibizumab n = 599 |
RR [95% CI] Bevacizumab vs. ranibizumab |
|---|---|---|---|
| Endophthalmitis | 7 (1%) | 4 (< 1%) | 1.79 [0.53, 6.08] |
| Ocular adverse event (IVAN trial)** | Bevacizumab n = 296 |
Ranibizumab n = 314 |
RR [95% CI] Bevacizumab vs. ranibizumab |
|---|---|---|---|
| Traumatic cataract | 1 (< 1%) | 1 (< 1%) | 1.06 [0.07, 16.88] |
| Severe uveitis | 1 (< 1%) | 0 | 3.18 [0.13, 77.80] |
| Retinal detachment | 0 | 1 (< 1%) | 0.35 [0.01, 8.64] |
| Retinal pigment epithelial tear | 1 (< 1%) | 3 (< 1%) | 0.35 [0.04, 3.38] |
| Non-ocular adverse event† | Bevacizumab n = 882 |
Ranibizumab n = 913 |
RR [95% CI] Bevacizumab vs. ranibizumab |
|---|---|---|---|
| At least 1 serious adverse event | 314 (36%) | 271 (30%) | 1.20 [1.05, 1.37] |
| Death | 51 (6%) | 47 (5%) | 1.12 [0.76, 1.65] |
| Myocardial infarction | 11 (1%) | 13 (1%) | 0.88 [0.39, 1.94] |
| Stroke or cerebral infarction | 11 (1%) | 14 (2%) | 0.81 [0.37, 1.78] |
| Venous thrombotic event | 14 (2%) | 6 (< 1%) | 2.42 [0.93, 6.26] |
| Transient ischemic attack** | 1 (< 1%) | 1 (< 1%) | 1.04 [0.06, 16.52] |
| Cardiac disorders | 81 (9%) | 67 (7%) | 1.25 [0.92, 1.71] |
| Gastrointestinal disorders | 37 (4%) | 14 (2%) | 2.74 [1.49, 5.02] |
| Infections | 66 (7%) | 50 (5%) | 1.37 [0.96, 1.95] |
| Injury and procedural complications | 45 (5%) | 35 (4%) | 1.33 [0.86, 2.05] |
| Neoplasms (benign, malignant, unspecified) | 36 (4%) | 38 (4%) | 0.98 [0.63, 1.53] |
| Nervous system disorders | 44 (5%) | 43 (5%) | 1.06 [0.70, 1.60] |
| Surgical or medical procedure** | 14 (5%) | 16 (5%) | 0.91 [0.44, 1.84] |
CI: confidence interval
RR: risk ratio
Adverse events for endophthalmitis not reported in the IVAN 2013 study; data for CATT 2011 study only
ADDITIONAL SUMMARY OF FINDINGS [Explanation]
| Pegaptanib compared with control for neovascular age-related macular degeneration | ||||||
|---|---|---|---|---|---|---|
| Participant or population: people with neovascular age-related macular degeneration Settings: clinical centers Intervention: intravitreal injections of pegaptanib Comparison: sham injections | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No. of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control | Pegaptanib | |||||
| Gain of 15 letters or more visual acuity at one year | 20 per 1000 | 57 per 1000 (25 to 132) | RR 2.83 (1.23 to 6.52) | 1186 (1) | ⊕⊕⊕⊕ high |
|
| Loss of fewer than 15 letters visual acuity at one year | 554 per 1000 | 687 per 1000 (615 to 770) | RR 1.24 (1.11 to 1.39) | 1186 (1) | ⊕⊕⊕⊕ high |
|
| Mean change in visual acuity at one year (number of letters) | The mean change in the control group was a loss of 15 letters | The mean change in visual acuity in the pegaptanib groups was on average 6.72 more letters gained (95% CI 4.43 letters to 9.01 letters) | MD 6.72 (4.43 to 9.01) | 1186 (1) | ⊕⊕⊕⊕ high |
|
| Reduction in central retinal thickness at one year | - | - | - | - | - | Outcome not assessed by this trial. |
| No problems in quality of life domains at one year | - | - | - | - | - | Treatment with pegaptanib was associated with better scores on the NEI-VFQ questionnaire, specifically for distance vision and role limitation domains; however, standard deviations for scores were not reported |
| Serious systemic adverse events at one year | 151 per 1000 with at least one serious systemic adverse event | 189 per 1000 (140 to 257) | RR 1.25 (0.93 to 1.70) | 1190 (1) | ⊕⊕⊕○ moderate1 |
|
| Serious ocular adverse events at one year | 7 per 1000 with any eye disorder | 26 per 1000 (6 to 109) | RR 3.84 (0.91 to 16.20) | 1190 (1) | ⊕⊕⊕○ moderate1 |
|
The basis for the assumed risk is estimated by the proportion with the event in the control group. The corresponding risk (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI).
CI: confidence interval; RR: risk ratio; MD: mean difference
| The Grading of Recommendations Assessment, Development and Evaluation (GRADE) Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. |
Adverse events downgraded to moderate quality as the numbers of events were small (<1%) for many specific adverse events
| Ranibizumab compared with control for neovascular age-related macular degeneration | ||||||
|---|---|---|---|---|---|---|
| Participant or population: people with neovascular age-related macular degeneration Settings: clinical centers Intervention: intravitreal injections of ranibizumab Comparison: sham injections with or without verteporfin photodynamic therapy | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No. of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control | Ranibizumab | |||||
| Gain of 15 letters or more visual acuity at one year | 59 per 1000 | 230 per 1000 (93 to 566) | see comment | 1322 (3) | ⊕⊕⊕○ moderate1 |
Meta-analysis not performed due to high I2 (80%). |
| Loss of fewer than 15 letters visual acuity at one year | 610 per 1000 | 934 per 1000 (861 to 1000) | RR 1.53 (1.41 to 1.64) | 1322 (3) | ⊕⊕⊕⊕ high |
|
| Mean change in visual acuity at one year (number of letters) | The mean change across control groups ranged from a loss of 10 to 16 letters | The mean change in visual acuity in the ranibizumab groups was on average 17.80 more letters gained (95% CI 15.95 letters to 19.65 letters) | MD 17.80 (15.95 to 19. 65) | 1322 (3) | ⊕⊕⊕⊕ high |
|
| Reduction in central retinal thickness at one year | - | - | - | - | - | We were unable to find data on central retinal thickness in reports from any of the three included trials comparing ranibizumab with control interventions |
| Mean change in vision-related quality of life | The mean change across control groups in vision-related quality of life scores ranged from −3 to 2 points | The mean change across control groups in vision-related quality of life scores ranged from 5 to 7 points | MD 6.69 (3.38 to 9.99) | 1134 (2) | ⊕⊕⊕○ moderate2 |
Using the NEI-VFQ questionnaire with a 10-point difference considered as being clinically meaningful |
| Serious systemic adverse events at one year | Range of 5 to 83 per 1000 for various systemic adverse events | Range of 0 to 55 per 1000 for various systemic adverse events | Range of RRs 0.17 (0.01 to 4.24) to 2.08 (0.23 to 18.45) | 603 (2) | ⊕⊕⊕○ moderate3 |
|
| Serious ocular adverse events at one year | Range of 0 to 68 per 1000 for various ocular adverse events | Range of 3 to 118 per 1000 for various ocular adverse events | Range of RRs 0.52 (0.03 to 8.25) to 2.71 (1.36 to 5.42) | 603 (2) | ⊕⊕⊕○ moderate3 |
|
The basis for the assumed risk is estimated by the proportion with the event in the control group. The corresponding risk (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI).
CI: confidence interval; RR: risk ratio; MD: mean difference
| The Grading of Recommendations Assessment, Development and Evaluation (GRADE) Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. |
Gain of vision outcome downgraded due to high statistical heterogeneity
Quality of life outcomes downgraded due to not all studies reporting this outcome and non-clinically significant results.
Adverse events downgraded to moderate quality as not all eligible trials reported all types of adverse events and numbers were small (<1%) for many specific adverse events
| Bevacizumab compared with control for neovascular age-related macular degeneration | ||||||
|---|---|---|---|---|---|---|
| Participant or population: people with neovascular age-related macular degeneration Settings: clinical centers Intervention: intravitreal injections of bevacizumab Comparison: standard therapy (intravitreal injections of pegaptanib, verteporfin photodynamic therapy with or without triamcinolone acetonide, or sham injections) | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No. of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control | Bevacizumab | |||||
| Gain of 15 letters or more visual acuity at one year | 38 per 1000 | 293 per 1000 (92 to 937) | RR 7.80 (2.44 to 24.98) | 159 (2) | ⊕⊕⊕○ moderate1 |
|
| Loss of fewer than 15 letters visual acuity at one year | 700 per 1000 | 896 per 1000 (763 to 1000) | RR 1.28 (1.09 to 1.50) | 159 (2) | ⊕⊕⊕○ moderate1 |
|
| Mean change in visual acuity at one year (number of letters) | - | - | - | - | - | The mean change from baseline in visual acuity was 7.0 letters in the bevacizumab group and −9.4 letters in the control group in one study. The second study reported participants in the bevacizumab group gained 8 letters on average and participants in the control group lost 3 letters on average |
| Reduction in central retinal thickness at one year | - | - | - | - | - | The mean change was −91 μm in the bevacizumab group and −55 μm in the control group in one study and −113 μm in the bevacizumab group and −72 μm in the control group in the other study |
| Mean change in vision-related quality of life | - | - | - | - | - | Outcome not assessed by these trials. |
| Serious systemic adverse events at one year | 15 per 1000 experienced any systemic adverse event | 31 per 1000 (3 to 331) | RR 2.03 (0.19 to 21.85) | 131 (1) | ⊕⊕○○ low2 |
|
| Serious ocular adverse events at one year | 91 per 1000 experienced any ocular adverse event | 169 per 1000 (66 to 431) | RR 1.86 (0.73 to 4.74) | 131 (1) | ⊕⊕○○ low2 |
|
The basis for the assumed risk is estimated by the proportion with the event in the control group. The corresponding risk (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI).
CI: confidence interval; RR: risk ratio; MD: mean difference
| The Grading of Recommendations Assessment, Development and Evaluation (GRADE) Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. |
Vision outcomes downgraded to moderate quality due to small sample sizes
Adverse events downgraded to low quality as sample sizes were small and numbers of events were small (<1%) for many specific adverse events
DISCUSSION
Summary of main results
All twelve trials included in this systematic review were of good methodological quality and demonstrated the beneficial effect of anti-VEGF therapy on visual acuity in the management of neovascular AMD. Participants treated with any one of the anti-VEGF agents featured in these trials, pegaptanib (one trial), ranibizumab (three trials), or bevacizumab (two trials), more often maintained visual acuity at one year and less often lost visual acuity, compared with participants who received no anti-VEGF agent. Stability of visual acuity at one year was more often achieved in an anti-VEGF treatment group than in a control group not treated with anti-VEGFs. The safety profile of anti-VEGFs was acceptable based on the information reported in the included studies.
Functional outcomes (e.g., visual acuity) correlated with quality-of-life outcomes, when reported, and anatomic outcomes (e.g., lesion size and retinal thickening) across trials. Participants treated with pegaptanib showed a decrease in size of the choroidal neovascular complex with less leakage observed on fluorescein angiograms compared with participants treated with sham injections. In bevacizumab-treated participants, there was a reduction in CRT on OCT compared with participants in the control groups.
Improvement in vision-specific quality of life was reported more often in the anti-VEGF-treated groups compared to the control groups. Improved scores on the NEI-VFQ scale were reported with both pegaptanib and ranibizumab compared to controls. Cost utility analysis, based on data from one trial and with standardized utilities of degree of visual loss, which compared ranibizumab with pegaptanib found ranibizumab to be associated with a better quality of life when compared with pegaptanib (Brown 2008). Data on visual function (e.g., contrast sensitivity) costs were sparse in these trials.
We found no trial in which pegaptanib had been compared with another anti-VEGF agent head-to-head. Six head-to-head trials compared bevacizumab versus ranibizumab. At one and two years of follow up, differences between bevacizumab and ranibizumab for visual acuity outcomes were comparable clinically and statistically, although CIs for some outcomes reported by individual studies indicate some uncertainty in the true effects. In terms of visual function, one trial showed better near LogMAR visual acuity among participants in the ranibizumab groups than among participants in the bevacizumab groups at one-year follow up; this effect had diminished at two-years follow up. At one and two years of follow up, there were no clinically meaningful differences in the reduction of CRT between bevacizumab-treated participants and ranibizumab-treated participants. Participant responses to quality-of-life questionnaires were comparable between the two treatment groups. A small number of ocular adverse events were reported for both bevacizumab or ranibizumab (fewer than 1%) across all trials. However, endophthalmitis rates were higher with injection of anti-VEGF agents than with intravitreal surgery unless estimates were based on number of injections given rather than number of eyes treated. It is important that individuals with AMD and their ophthalmologists be aware of this small, but serious risk. At both one and two-year follow ups, fewer participants in the ranibizumab groups experienced any serious systemic adverse event compared with participants in the bevacizumab groups.
Overall completeness and applicability of evidence
The aim of this review was to investigate both the effects and quality of life associated with intravitreally injected anti-VEGF agents for the treatment of neovascular AMD when compared to either sham treatment or a different anti-VEGF treatment administered at comparable dosages and regimens. Only RCTs were included in this review, each with a minimum follow up of one year. The primary outcome for this review was the proportion of participants who gained 15 letters or more of BCVA by the one-year follow- up examination. Secondary outcomes included other visual acuity outcomes at one and two years of follow up, visual function outcomes, morphological characteristics assessed by fluorescein angiography or OCT, ocular and systemic adverse outcomes, cost outcomes, and quality-of-life measures. Multiple sources were used to identify relevant data for this review, not only journal publications, but also conference abstracts, FDA documents, and clinical trial registries. When data were unclear or missing, study investigators were contacted for clarification or information.
This review ultimately included representative and applicable outcomes data on 5496 participants from 12 trials conducted in various countries that included both men and women aged 50 years or older with subfoveal CNV secondary to AMD. Approximately half of the trials reported the type of neovascular lesion, with all lesion types (predominantly classic CNV, minimally classic CNV, and occult CNV only) represented among these trials. All studies included at least one measure related to the morphological characteristics of study eyes, with fluorescein angiography used in all studies and OCT used in all but the earliest of these 12 RCTs.
The initial RCTs of anti-VEGF agents incorporated in this review, both individually and collectively, established a new paradigm for the management of neovascular AMD, particularly for lesions under or near the central fovea, and validated the administration of intravitreal anti-VEGF therapy in affected individuals with clinical profiles similar to those of the participants enrolled in these trials. Reported outcomes related to visual acuity gains, the stability of visual acuity at one year, the decreased risk of significant visual acuity loss, and the low rates of ocular and systemic adverse events are mirrored in real-life clinical encounters when anti-VEGF agents are used to manage neovascular AMD in the retina specialist’s office (Carneiro 2012; Gillies 2014; Holz 2013; Rasmussen 2014). As observed in the clinical trials incorporated into this review, morphologic changes in the CNV lesion complex, with regard to decreased size on fluorescein angiography, decreased leakage on fluorescein angiography, and decreased CRT on OCT, are also observed to occur in-office in individuals receiving anti-VEGF therapy for neovascular AMD (Carneiro 2012).
With completion of head-to-head trials of bevacizumab versus ranibizumab, and the finding of little or no difference in outcomes between the two drugs, a major challenge for the ophthalmologist and individual with AMD has been the choice of anti-VEGF agent. Issues considered have been costs, availability, and quality control of the preparation of bevacizumab for intravitreal injection. Issues as yet unresolved are the optimal frequency with which anti-VEGF agents should be injected in most affected eyes, the length of calendar time over which anti-VEGF agents must be injected to maintain the benefits seen with two-year outcomes, and the long-term ocular and systemic effects of these treatments.
Quality of the evidence
In addition to the inclusion of only RCTs in this review, two review authors assessed potential sources of bias in these trials according to methods established by The Cochrane Collaboration. Parameters considered included selection bias, performance bias, detection bias, attrition bias, and reporting bias; each potential source of bias was graded as low risk, unclear risk, or high risk. Overall, the included studies were found to be at low risk for all categories of bias. In all 12 trials, few participants missed the primary outcome visit or were not treated per-protocol assignment. In nine trials, the rates of loss to follow up at the primary follow-up visits were less than 15%. Athough not the best method to account for missing data, six trials used the last-observation-carried-forward method to impute missing data. Protocols or clinical trial registrations were identified for 11 of the 12 included studies. Seven of these 11 trials were judged to be free of reporting bias based on the consistency between study outcomes defined in the protocols and clinical trial registers and those reported in study publications to date.
Various other aspects of trial design, reporting, and financial support were considered as potential sources of bias. Four of 12 trials, one study of pegaptanib and three studies comparing ranibizumab with controls, were sponsored by pharmaceutical companies that marketed the study drugs under investigation. In addition, the pharmaceutical company sponsors had important roles in the design, analysis, and reporting of these trials and some of the investigators reported that they had financial relationships with the company that manufactured the study drug.
Potential biases in the review process
For this review, we conducted broad electronic searches for studies and imposed no date or language restrictions in the searches in order to minimize potential biases in the study selection process. We followed standard Cochrane review methodology.
Agreements and disagreements with other studies or reviews
Whether assessed by systematic, comprehensive reviews, like this one, or by more traditional, clinical reviews, treatments for neovascular AMD with anti-VEGF compounds appear to be efficacious and safe (Ip 2008; Mitchell 2011; Schmucker 2010; Schmucker 2012). Beneficial effects with pegaptanib, ranibizumab, and bevacizumab are evident in terms of the proportion of participants with stabilization or small losses of BCVA. Ranibizumab and bevacizumab additionally resulted in a greater proportion of participants with improved BCVA after one and two years of injections. In independent studies and comprehensive reviews, visual acuity effects have been consistent with morphologic changes in the size and composition of the CNV lesion complex as well as with the observed change in CRT on OCT following treatment with these agents. In general, considerations of costs were limited in the trials included in this systematic review; additional analyses indicating a favorable cost utility ratio for anti-VEGF agents versus control or no treatment were cited in research using RCT and observational data (Cohen 2008; Earnshaw 2007; Fletcher 2008;Hernandez-Pastor 2008; Javitt 2008;Wolowacz 2007). Economic analyses have documented the lower cost of bevacizumab compared with ranibizumab to achieve the same benefits (Raftery 2007; Stein 2014). A separate Cochrane review specifically evaluating the systemic safety of bevacizumab versus ranibizumab also concluded no significant differences between intravitreal injection of the two drugs after two years of follow up with respect to deaths or overall serious systemic adverse events (Moja 2014).
AUTHORS’ CONCLUSIONS
Implications for practice
The results of this review indicate effectiveness of anti-VEGF agents (pegaptanib, ranibizumab, and bevacizumab) in terms of the stability or improvement in visual acuity after one and two years of treatment. Ranibizumab and bevacizumab have resulted in improved visual acuity in a sizable fraction of treated eyes. The beneficial effects of these anti-VEGF agents with respect to visual acuity are consistent with their effects on changes in lesion size evaluated on fluorescein angiograms and by OCT. The available information on adverse effects with each medication does not suggest a higher incidence of potentially vision-threatening complications with intravitreal injection compared with control interventions; however, clinical trial data may not be sufficiently powered to detect rare safety outcomes. We found no trials that had compared pegaptanib directly with either ranibizumab or bevacizumab.
At the time of this review, bevacizumab remains an off-label therapy for neovascular AMD. The manufacturer (Genentech) that produces both bevacizumab and ranibizumab has not submitted bevacizumab for approval as a treatment for AMD. As bevacizumab is a significantly less expensive treatment option, it perhaps would compete with the company’s more costly and FDA-approved ophthalmic anti-VEGF agent, ranibizumab. Thus, trials comparing functional, anatomic, vision-specific quality of life, and cost utility outcomes between bevacizumab and ranibizumab ultimately may have no effect on the treatment of individuals with neovascular AMD if off-label therapy with bevacizumab is proscribed. The US Centers for Medicare and Medicaid (CMS) and other national health agencies currently cover bevacizumab for ophthalmic use in hospital outpatient settings; however, other national health agencies do not include off-label use bevacizumab in their coverage (CMS 2014; Cohen 2014).
Implications for research
As the use of anti-VEGF agents for the treatment of AMD becomes part of standard clinical practice, certain issues regarding their use remain. Several factors encourage evaluation of the efficacy of alternative and less-frequent dosing regimens with anti-VEGF compounds. Some of these include concerns about ocular and systemic toxicity, the convenience to individuals with AMD and their physicians of fewer intravitreal injections, and the costs of treatment. Research evaluating the long-term use of anti-VEGF agents should consider both the effects of the drugs on vision and the long-term effects of multiple injections over time. It is unclear how best to evaluate these effects as RCTs to identify rare events during long follow-up periods are difficult to conduct and finance. Data for up to seven years of follow up have been reported for some RCTs included in this review (Rofagha 2013); however, these follow-up data are observational, were not part of the trial protocols, and include only a subset of originally enrolled participants. The CATT 2011 trial has received funding from the US National Eye Institute to continue follow up of participants enrolled in that trial in order to document long-term positive and negative effects of anti-VEGF treatment.
The use of anti-VEGF agents in combination with other neovascular AMD treatments, such at PDT or intravitreal steroids, is an important and active area of research since the acceptance of anti-VEGF therapy may make it unethical to conduct trials without providing this treatment to all participants with neovascular AMD. The goal of combination treatments would be to improve vision and quality of life even further than what is achievable with anti-VEGF agents alone, and perhaps reduce the number of intravitreal injections needed. Research also is needed to evaluate methods of delivering the agents other than intravitreally. Possibilities already under development are implants and refillable reservoirs (de Juan 2013).
Acknowledgments
We are grateful to the editorial team of the Cochrane Eyes and Vision Group (CEVG) for comments and evaluation of this review. Iris Gordon and Karen Blackhall, Trials Search Co-ordinators for CEVG, designed and conducted the electronic searches. Usha Reddy, MD, and Harold Woodcome Jr, MD, contributed to the protocol for this review. We thank Gianni Virgili, Richard Wormald, Jennifer Evans, Anupa Shah, Tasanee Smith and Marie Diener-West for their comments on the review or review update.
We are grateful to Dr Brown (ANCHOR 2006), Dr Deppenschmidt at Genentech (ANCHOR 2006; MARINA 2006; PIER 2008), Dr Feinsod at Eyetech Pharmaceuticals (VISION 2004), Dr Regillo (PIER 2008), Dr Rosenfeld (MARINA 2006; PIER 2008; SAILOR 2009), Dr Sacu (Sacu 2009), and Dr Subramanian (Subramanian 2010) for their kind assistance with providing additional information on trial methodology and results for the purposes of this review.
SOURCES OF SUPPORT
Internal sources
Southern New England Retina Associates, Providence RI, USA.
Brown University, USA.
Johns Hopkins Medical Institutions, Johns Hopkins University, USA.
External sources
Cochrane Eyes and Vision Group US Project supported by Grant 1 U01 EY020522, National Eye Institute, National Institutes of Health, USA.
SDS and BSH received support during the preparation of this review from an unrestricted grant to the Wilmer Eye Institute from Research to Prevent Blindness, New York, New York, USA.
National Institute for Health Research (NIHR), UK.
Richard Wormald, Co-ordinating Editor for the Cochrane Eyes and Vision Group (CEVG) acknowledges financial support for his CEVG research sessions from the Department of Health through the award made by the National Institute for Health Research to Moorfields Eye Hospital NHS Foundation Trust and UCL Institute of Ophthalmology for a Specialist Biomedical Research Centre for Ophthalmology.
The NIHR also funds the CEVG Editorial Base in London.
The views expressed in this publication are those of the authors and not necessarily those of the NIHR, NHS, or the Department of Health.
APPENDICES
Appendix 1. CENTRAL search strategy
-
#1
MeSH descriptor Macular Degeneration
-
#2
MeSH descriptor Retinal Degeneration
-
#3
MeSH descriptor Neovascularization, pathologic
-
#4
((macul* OR retina* OR choroid*:TI) AND (degener* OR neovasc*:TI))
-
#5
((macul* OR retina* OR choroid*:AB) AND (degener* OR neovasc*:AB))
-
#6
maculopath*
-
#7
(#1 OR #2 OR #3 OR #4 OR #5 OR #6)
-
#8
MeSH descriptor Angiogenesis Inhibitors
-
#9
MeSH descriptor Angiogenesis Inducing
-
#10
MeSH descriptor Endothelial Growth Factors
-
#11
macugen or pegapanib or lucentis or rhufab or rhu fab or ranibizumab or bevacizumab
-
#12
angiogen* or antiangiogen* or neovasculari* or vasculari*
-
#13
anti-vegf* or anti next vegf
-
#14
endothelial near growth near factor*
-
#15
(#8 OR #9 OR #10 OR #11 OR #12 OR #13 OR #14)
-
#16
(#7 AND #15)
Appendix 2. MEDLINE search strategy
randomized controlled trial.pt.
(randomized or randomised).ab,ti.
placebo.ab,ti.
dt.fs.
randomly.ab,ti.
trial.ab,ti.
groups.ab,ti.
or/1–7
exp animals/
exp humans/
9 not (9 and 10)
8 not 11
exp macular degeneration/
exp retinal degeneration/
exp retinal neovascularization/
exp choroidal neovascularization/
exp macula lutea/
maculopath$.tw.
((macul$ or retina$ or choroid$) adj3 degener$).tw.
((macul$ or retina$ or choroid$) adj3 neovasc$).tw.
(macula$ adj2 lutea).tw.
(AMD or ARMD or CNV).tw.
or/13–22
exp angiogenesis inhibitors/
angiogenesis inducing agents/
endothelial growth factors/
exp vascular endothelial growth factors/
(anti adj2 VEGF$).tw.
(endothelial adj2 growth adj2 factor$).tw.
(anti adj1 angiogen$).tw.
(macugen$ or pegaptanib$ or lucentis$ or rhufab$ or ranibizumab$ or bevacizumab$ or avastin$).tw.
VEGF TRAP$.tw.
or/24–32
23 and 33
12 and 34
The search filter for trials at the beginning of the MEDLINE strategy is from the published paper by Glanville (Glanville 2006).
Appendix 3. EMBASE search strategy
exp randomized controlled trial/
exp randomization/
exp double blind procedure/
exp single blind procedure/
random$.tw.
or/1–5
(animal or animal experiment).sh.
human.sh.
7 and 8
7 not 9
6 not 10
exp clinical trial/
(clin$ adj3 trial$).tw.
((singl$ or doubl$ or trebl$ or tripl$) adj3 (blind$ or mask$)).tw.
exp placebo/
placebo$.tw.
random$.tw.
exp experimental design/
exp crossover procedure/
exp control group/
exp latin square design/
or/12–21
22 not 10
23 not 11
exp comparative study/
exp evaluation/
exp prospective study/
(control$ or prospectiv$ or volunteer$).tw.
or/25–28
29 not 10
30 not (11 or 23)
11 or 24 or 31
exp retina macula degeneration/
exp retinal degeneration/
exp subretinal neovascularization/
maculopath$.tw.
((macul$ or retina$ or choroid$) adj3 degener$).tw.
((macul$ or retina$ or choroid$) adj3 neovasc$).tw.
(macula$ adj2 lutea).tw.
(AMD or ARMD or CNV).tw.
or/33–40
angiogenesis/
exp angiogenesis inhibitors/
angiogenic factor/
endothelial cell growth factor/
monoclonal antibody/
vasculotropin/
(anti adj2 VEGF$).tw.
(endothelial adj2 growth adj2 factor$).tw.
(anti adj1 angiogen$).tw.
(macugen$ or pegaptanib$ or lucentis$ or rhufab$ or ranibizumab$ or bevacizumab$ or avastin$).tw.
VEGF TRAP$.tw.
or/42–52
41 and 53
32 and 54
Appendix 4. LILACS search strategy
macugen or pegaptanib or lucentis or rhufab or ranibizumab or bevacizumab or avastin and macula$ degenerat$ or AMD or ARMD
Appendix 5. metaRegister of Controlled Trials search strategy
(macular degeneration or AMD or ARMD) and (macugen or pegaptanib or lucentis or rhufab or ranibizumab or bevacizumab or avastin)
Appendix 6. ClinicalTrials.gov search strategy
(Macular Degeneration OR AMD OR ARMD) AND (Macugen OR Pegaptanib OR Lucentis OR rhufab OR ranibizumab OR bevacizumab OR avastin)
Appendix 7. ICTRP search strategy
Macular Degeneration OR AMD OR ARMD = Condition AND Macugen OR Pegaptanib OR Lucentis OR rhufab OR ranibizumab OR bevacizumab OR avastin = Intervention
Appendix 8. EOP 1003 study data
| Methods | Method of randomization: stochastic treatment allocation algorithm based on the variance method Method of allocation concealment: centralized randomization where the study coordinator was instructed the code of the medication for the patient after determining her eligibility. The medication packet was not opened until just before administering the injection Masking: Participants: yes Care providers: examiner: yes; injector: no Outcome assessors: yes Number randomized: 144 to 0.3 mg pegaptanib, 146 to 1 mg pegaptanib, 143 to 3 mg pegaptanib, and 145 to placebo groups Exclusions after randomization: none Number analyzed: 144 in 0.3 mg pegaptanib, 146 in 1 mg pegaptanib, 143 in 3 mg pegaptanib, and 145 in placebo groups for the primary outcome alone Losses to follow up: 11 in placebo group, 12 in 0.3 mg pegaptanib group, 17 in 1 mg pegaptanib group, 20 in 3 mg pegaptanib group discontinued therapy during the trial Intention to treat analysis: reported an intention to treat analysis only for the primary outcome Unit of analysis: individuals Reported power calculations: yes |
| Participants | Country: USA, Canada Age: Mean age was 78, 76.5, 77.1, and 76.7 years in 0.3 mg pegaptanib, 1 mg pegaptanib, 3 mg pegaptanib, and placebo groups, respectively Gender: 56%, 53%, 69%, and 57% in 0.3 mg pegaptanib, 1 mg pegaptanib, 3 mg pegaptanib, and placebo groups respectively, were females Inclusion criteria: age greater than or equal to 50 years; subfoveal choroidal neovascularization (CNV) secondary to age-related macular degeneration; best corrected visual acuity of 20/40 to 20/320 in the treated eye and greater than 20/800 in the fellow eye; CNV lesion may be predominantly classic, minimally classic, occult with no classic; size of lesion < 12 disc areas (including blood, scar/atrophy, neovascularization); no greater than 50% of lesion could be due to subretinal hemorrhage and 50% of lesion had to be due to CNV; for occult lesions, lesions had to be subretinal and no greater than 50% of total lesion area, or presence of lipid or loss of 15 letters or more of visual acuity during previous 12 weeks; patients were eligible even if they received 1 photodynamic treatment if it was at least 8 to 12 weeks prior to enrollment; intraocular pressure < 23 mmHg; adequate pupil dilation; clear media Exclusion criteria: atrophy exceeding 20% of total lesion or subfoveal scarring; previous thermal laser; therapy with another investigational drug; likelihood of requiring cataract removal within 2 years; other potential causes of CNV including high myopia, ocular histoplasmosis, angioid streaks, choroidal rupture, multifocal choroiditis, any intraocular surgery within 3 months or extrafoveal/juxtafoveal laser within 2 weeks of study entry or posterior vitrectomy or scleral buckle or presence of intraretinal tears or rips; concomitant presence of diabetic retinopathy, severe cardiac disease, myocardial infarction within 6 months, ventricular tachycardia requiring treatment, unstable angina, evidence of peripheral vascular disease, stroke within 12 months, acute or chronic periocular infection, previous therapeutic radiation to eye/head/neck; any treatment with any investigational agent within past 30 days; serious allergies to fluorescein dye or indocyanine green or components of pegaptanib Equivalence of baseline characteristics: The treatment groups were similar with respect to age, gender, race, smoking status, angiographic subtypes, prior treatment status with photodynamic therapy, and Early Treatment Diabetic Retinopathy Study visual acuity scores |
| Interventions | Treatment: Intravitreal injection of pegaptanib at dosages of either 0.3 mg, 1.0 mg, or 3.0 mg given every 6 weeks over period of 48 weeks Control: sham injection with patients treated identically with the exception of scleral penetration with the needle Length of follow-up: 54 weeks |
| Outcomes | Primary outcome: proportion of patients losing fewer than 15 letters of visual acuity between baseline and week 54 Other outcomes reported: Gain of 3 or more lines visual acuity, maintenance of visual acuity or gain of 0 lines of visual acuity, mean visual acuity, legal blindness, loss of 30 letters or more of visual acuity, size of lesion, and total CNV size Reported quality of life indicators: yes Intervals at which outcome assessed: every 6 weeks before treatment with main assessment analyzed after 54 weeks |
| Notes | Funding: Eyetech Pharmaceuticals and Pfizer NCT00321997 |
Appendix 9. EOP 1004 study data
| Methods | Method of randomization: stochastic treatment allocation algorithm based on the variance method Method of allocation concealment: centralized randomization where the study coordinator was instructed the code of the medication for the patient after determining her eligibility. The medication packet was not opened until just before administering the injection Masking: Participants: yes Care providers: examiner: yes; injector: no Outcome assessors: yes Number randomized: 151 to 0.3 mg pegaptanib, 155 to 1 mg pegaptanib, 153 to 3 mg pegaptanib, and 153 to placebo groups Exclusions after randomization: none Number analyzed: 151 in 0.3 mg pegaptanib, 155 in 1 mg pegaptanib, 153 in 3 mg pegaptanib, and 153 in placebo groups for the primary outcome alone Losses to follow up: 12 in placebo group, 11 in 0.3 mg pegaptanib group, 13 in 1 mg pegaptanib group, 17 in 3 mg pegaptanib group discontinued therapy during the trial Intention to treat analysis: yes except don’t know why 18 patients were excluded after randomization Unit of analysis: individuals Reported power calculations: yes |
| Participants | Country: US, Canada, Europe, Israel, Australia, South America Age: Mean age was 74.9, 74.5, 75.4, and 74.9 years in 0.3 mg pegaptanib, 1 mg pegaptanib, 3 mg pegaptanib, and placebo groups, respectively Gender: 54%, 56%, 61%, and 63% in 0.3 mg pegaptanib, 1 mg pegaptanib, 3 mg pegaptanib, and placebo groups, respectively, were females Inclusion criteria: age greater than or equal to 50 years; subfoveal choroidal neovascularization (CNV) secondary to age-related macular degeneration; best corrected visual acuity of 20/40 to 20/320 in the treated eye and greater than 20/800 in the fellow eye; CNV lesion may be predominantly classic, minimally classic, occult with no classic; size of lesion < 12 disc areas (including blood, scar/atrophy, neovascularization); no greater than 50% of lesion could be due to subretinal hemorrhage and 50% of lesion had to be due to CNV; for occult lesions, lesions had to be subretinal and no greater than 50% of total lesion area, or presence of lipid or loss of 15 letters or more of visual acuity during previous 12 weeks; patients were eligible even if they received 1 photodynamic treatment if it was at least 8 to 12 weeks prior to enrollment; intraocular pressure < 23 mmHg; adequate pupil dilation; clear media Exclusion criteria: atrophy exceeding 20% of total lesion or subfoveal scarring; previous thermal laser; therapy with another investigational drug; likelihood of requiring cataract removal within 2 years; other potential causes of CNV including high myopia, ocular histoplasmosis, angioid streaks, choroidal rupture, multifocal choroiditis, any intraocular surgery within 3 months or extrafoveal/juxtafoveal laser within 2 weeks of study entry or posterior vitrectomy or scleral buckle or presence of intraretinal tears or rips; concomitant presence of diabetic retinopathy, severe cardiac disease, myocardial infarction within 6 months, ventricular tachycardia requiring treatment, unstable angina, evidence of peripheral vascular disease, stroke within 12 months, acute or chronic periocular infection, previous therapeutic radiation to eye/head/neck; any treatment with any investigational agent within last 30 days; serious allergies to fluorescein dye or indocyanine green or components of pegaptanib Equivalence of baseline characteristics: the treatment groups were similar with respect to age, gender, race, smoking status, angiographic subtypes, prior treatment status with photodynamic therapy, and Early Treatment Diabetic Retinopathy Study visual acuity scores |
| Interventions | Treatment: Intravitreal injection of pegaptanib at dosages of either 0.3 mg, 1.0 mg, or 3.0 mg given every 6 weeks over period of 48 weeks Control: sham injection with participants treated identically with the exception of scleral penetration with the needle Length of follow up: 54 weeks |
| Outcomes | Primary outcome: proportion of patients losing fewer than 15 letters of visual acuity between baseline and week 54 Other outcomes reported: gain of 3 or more lines visual acuity, maintenance of visual acuity or gain of 0 lines of visual acuity, mean visual acuity, legal blindness, loss of 30 letters or more of visual acuity, size of lesion, and total CNV size Reported quality of life indicators: yes Intervals at which outcome assessed: every 6 weeks before treatment with main assessment analyzed after 54 weeks |
| Notes | Funding: Eyetech Pharmaceuticals and Pfizer NCT00021736 |
DATA AND ANALYSES
Comparison 1. Pegaptanib versus control
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Gain of 15 letters or more visual acuity at one year | 1 | Risk Ratio (M-H, Random, 95% CI) | Totals not selected | |
| 2 Loss of fewer than 15 letters visual acuity at one year | 1 | Risk Ratio (M-H, Random, 95% CI) | Totals not selected | |
| 3 Loss of fewer than 30 letters visual acuity at one year | 1 | Risk Ratio (M-H, Random, 95% CI) | Totals not selected | |
| 4 Visual acuity better than 20/200 at one year | 1 | Risk Ratio (M-H, Random, 95% CI) | Totals not selected | |
| 5 Maintenance of visual acuity at one year | 1 | Risk Ratio (M-H, Random, 95% CI) | Totals not selected | |
| 6 Mean change in visual acuity at one year (number of letters) | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 7 Reduction in size of CNV at one year (Mean number of disc areas) | 1 | Mean Difference (Random, 95% CI) | Totals not selected | |
| 8 Reduction in size of lesion at one year (Mean number of disc areas) | 1 | Mean Difference (Random, 95% CI) | Totals not selected |
Comparison 2. Ranibizumab versus control
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Gain of 15 letters or more visual acuity at one year | 3 | Risk Ratio (M-H, Random, 95% CI) | Totals not selected | |
| 2 Gain of 15 letters or more visual acuity at two years | 3 | 1322 | Risk Ratio (M-H, Random, 95% CI) | 5.77 [3.38, 9.84] |
| 3 Loss of fewer than 15 letters visual acuity at one year | 3 | 1322 | Risk Ratio (M-H, Random, 95% CI) | 1.53 [1.41, 1.64] |
| 4 Loss of fewer than 15 letters visual acuity at two years | 3 | 1322 | Risk Ratio (M-H, Random, 95% CI) | 1.62 [1.32, 1.98] |
| 5 Loss of fewer than 30 letters visual acuity at one year | 2 | 1138 | Risk Ratio (M-H, Random, 95% CI) | 1.15 [1.11, 1.20] |
| 6 Loss of fewer than 30 letters visual acuity at two years | 2 | 1138 | Risk Ratio (M-H, Random, 95% CI) | 1.22 [1.15, 1.29] |
| 7 Visual acuity better than 20/200 at one year | 3 | 1322 | Risk Ratio (M-H, Random, 95% CI) | 1.69 [1.41, 2.03] |
| 8 Visual acuity better than 20/200 at two years | 3 | 1322 | Risk Ratio (M-H, Random, 95% CI) | 1.73 [1.52, 1.98] |
| 9 Maintenance of visual acuity at one year | 1 | Risk Ratio (M-H, Random, 95% CI) | Totals not selected | |
| 10 Maintenance of visual acuity at two years | 1 | Risk Ratio (M-H, Random, 95% CI) | Totals not selected | |
| 11 Mean change in visual acuity at one year (number of letters) | 3 | 1322 | Mean Difference (IV, Random, 95% CI) | 17.80 [15.95, 19.65] |
| 12 Mean change in visual acuity at two years (number of letters) | 3 | 1322 | Mean Difference (IV, Random, 95% CI) | 20.11 [18.08, 22.15] |
| 13 Reduction in size of lesion at one year (Mean number of disc areas) | 2 | 606 | Mean Difference (IV, Random, 95% CI) | 2.34 [1.88, 2.81] |
| 14 Reduction in size of lesion at two years (Mean number of disc areas) | 2 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 15 Mean change in quality of life scores at one year | 2 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 15.1 Overall vision-related quality of life | 2 | 1134 | Mean Difference (IV, Random, 95% CI) | 6.69 [3.38, 9.99] |
| 15.2 Near vision activities | 2 | 1134 | Mean Difference (IV, Random, 95% CI) | 8.45 [0.28, 16.62] |
| 15.3 Distance vision activities | 2 | 1134 | Mean Difference (IV, Random, 95% CI) | 9.65 [3.20, 16.09] |
| 15.4 Dependency | 2 | 1134 | Mean Difference (IV, Random, 95% CI) | 9.82 [6.86, 12.77] |
| 15.5 Driving ability | 2 | 1080 | Mean Difference (IV, Random, 95% CI) | 9.85 [6.34, 13.36] |
| 15.6 General health | 2 | 1134 | Mean Difference (IV, Random, 95% CI) | 3.18 [0.54, 5.82] |
| 15.7 Role difficulties | 2 | 1134 | Mean Difference (IV, Random, 95% CI) | 6.99 [0.76, 13.23] |
| 15.8 Mental health | 2 | 1134 | Mean Difference (IV, Random, 95% CI) | 8.42 [5.75, 11.10] |
| 15.9 General vision | 2 | 1134 | Mean Difference (IV, Random, 95% CI) | 8.20 [5.90, 10.50] |
| 15.10 Social functioning | 2 | 1134 | Mean Difference (IV, Random, 95% CI) | 8.03 [5.36, 10.69] |
| 15.11 Color vision | 2 | 1127 | Mean Difference (IV, Random, 95% CI) | 2.51 [−0.02, 5.05] |
| 15.12 Peripheral vision | 2 | 1133 | Mean Difference (IV, Random, 95% CI) | 5.20 [0.37, 10.03] |
| 15.13 Ocular pain | 2 | 1134 | Mean Difference (IV, Random, 95% CI) | −1.78 [−3.67, 0.11] |
| 16 Mean change in quality of life scores at two years | 2 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 16.1 Overall vision-related quality of life | 2 | 1134 | Mean Difference (IV, Random, 95% CI) | 8.63 [3.31, 13.95] |
| 16.2 Near vision activities | 2 | 1134 | Mean Difference (IV, Random, 95% CI) | 11.52 [3.49, 19.55] |
| 16.3 Distance vision activities | 2 | 1134 | Mean Difference (IV, Random, 95% CI) | 10.86 [3.82, 17.90] |
| 16.4 Dependency | 2 | 1134 | Mean Difference (IV, Random, 95% CI) | 11.06 [3.29, 18.83] |
| 16.5 Driving ability | 2 | 1080 | Mean Difference (IV, Random, 95% CI) | 13.53 [9.51, 17.55] |
| 16.6 General health | 2 | 1134 | Mean Difference (IV, Random, 95% CI) | 2.58 [−0.18, 5.35] |
| 16.7 Role difficulties | 2 | 1134 | Mean Difference (IV, Random, 95% CI) | 9.44 [1.34, 17.54] |
| 16.8 Mental health | 2 | 1134 | Mean Difference (IV, Random, 95% CI) | 10.07 [3.98, 16.17] |
| 16.9 General vision | 2 | 1134 | Mean Difference (IV, Random, 95% CI) | 9.61 [5.49, 13.72] |
| 16.10 Social functioning | 2 | 1134 | Mean Difference (IV, Random, 95% CI) | 8.12 [1.77, 14.47] |
| 16.11 Color vision | 2 | 1127 | Mean Difference (IV, Random, 95% CI) | 5.70 [2.89, 8.51] |
| 16.12 Peripheral vision | 2 | 1133 | Mean Difference (IV, Random, 95% CI) | 6.79 [1.48, 12.09] |
| 16.13 Ocular pain | 2 | 1134 | Mean Difference (IV, Random, 95% CI) | −1.10 [−3.13, 0.92] |
Comparison 3. Bevacizumab versus control
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Gain of 15 letters or more visual acuity at one year | 2 | 159 | Risk Ratio (M-H, Random, 95% CI) | 7.80 [2.44, 24.98] |
| 2 Loss of fewer than 15 letters visual acuity at one year | 2 | 159 | Risk Ratio (M-H, Random, 95% CI) | 1.28 [1.09, 1.50] |
Comparison 4. Bevacizumab versus ranibizumab
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Gain of 15 letters or more visual acuity at one year | 6 | 2446 | Risk Ratio (M-H, Random, 95% CI) | 0.90 [0.73, 1.11] |
| 2 Gain of 15 letters or more visual acuity at two years | 2 | Risk Ratio (M-H, Random, 95% CI) | Subtotals only | |
| 2.1 Participants in groups as randomized at baseline | 2 | 1547 | Risk Ratio (M-H, Random, 95% CI) | 0.84 [0.64, 1.11] |
| 2.2 Participants remaining in same groups after re-randomization | 2 | 1295 | Risk Ratio (M-H, Random, 95% CI) | 0.84 [0.64, 1.11] |
| 3 Loss of fewer than 15 letters visual acuity at one year | 6 | 2446 | Risk Ratio (M-H, Random, 95% CI) | 1.00 [0.98, 1.02] |
| 4 Loss of fewer than 15 letters visual acuity at two years | 2 | Risk Ratio (M-H, Random, 95% CI) | Subtotals only | |
| 4.1 Participants in groups as randomized at baseline | 2 | 1547 | Risk Ratio (M-H, Random, 95% CI) | 0.97 [0.94, 1.00] |
| 4.2 Participants remaining in same groups after re-randomization | 2 | 1295 | Risk Ratio (M-H, Random, 95% CI) | 0.98 [0.94, 1.01] |
| 5 Visual acuity better than 20/200 at one year | 4 | 2026 | Risk Ratio (M-H, Random, 95% CI) | 0.98 [0.96, 1.01] |
| 6 Visual acuity better than 20/200 at two years | 2 | Risk Ratio (M-H, Random, 95% CI) | Subtotals only | |
| 6.1 Participants in groups as randomized at baseline | 2 | 1547 | Risk Ratio (M-H, Random, 95% CI) | 1.00 [0.95, 1.06] |
| 6.2 Participants remaining in same groups after re-randomization | 2 | 1295 | Risk Ratio (M-H, Random, 95% CI) | 1.01 [0.95, 1.06] |
| 7 Mean change in visual acuity at one year (number of letters) | 6 | 2446 | Mean Difference (IV, Random, 95% CI) | −0.51 [−1.64, 0.62] |
| 8 Mean change in visual acuity at two years (number of letters) | 2 | 1295 | Mean Difference (IV, Random, 95% CI) | −1.15 [−2.82, 0.51] |
| 9 Reduction in central retinal thickness at one year | 4 | 1995 | Mean Difference (IV, Random, 95% CI) | −13.97 [−26.52, −1. |
| 10 Reduction in central retinal thickness at two years | 2 | 1199 | Mean Difference (IV, Random, 95% CI) | −12.40 [−33.83, 9. |
| 11 No problems in quality of life domain at one year | 1 | Risk Ratio (M-H, Random, 95% CI) | Totals not selected | |
| 11.1 Mobility | 1 | Risk Ratio (M-H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 11.2 Self care | 1 | Risk Ratio (M-H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 11.3 Usual activities | 1 | Risk Ratio (M-H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 11.4 Pain/discomfort | 1 | Risk Ratio (M-H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 11.5 Anxiety/depression | 1 | Risk Ratio (M-H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 12 No problems in quality of life domain at two years | 1 | Risk Ratio (M-H, Random, 95% CI) | Totals not selected | |
| 12.1 Mobility | 1 | Risk Ratio (M-H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 12.2 Self care | 1 | Risk Ratio (M-H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 12.3 Usual activities | 1 | Risk Ratio (M-H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 12.4 Pain/discomfort | 1 | Risk Ratio (M-H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 12.5 Anxiety/depression | 1 | Risk Ratio (M-H, Random, 95% CI) | 0.0 [0.0, 0.0] |
Analysis 1.1.
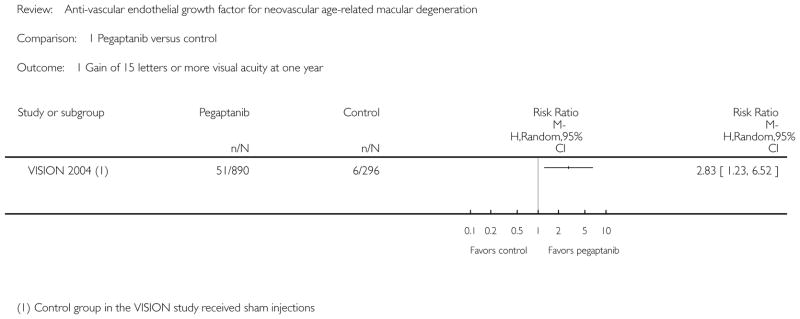
Comparison 1 Pegaptanib versus control, Outcome 1 Gain of 15 letters or more visual acuity at one year.
Analysis 1.2.
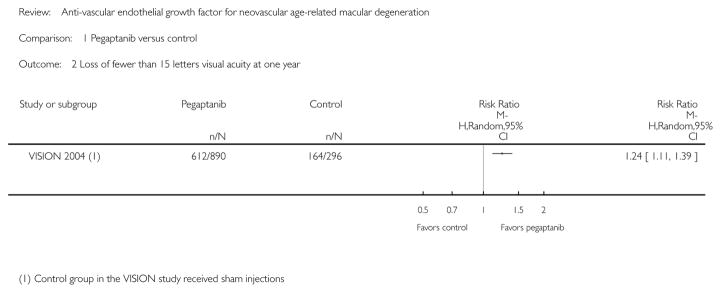
Comparison 1 Pegaptanib versus control, Outcome 2 Loss of fewer than 15 letters visual acuity at one year.
Analysis 1.3.
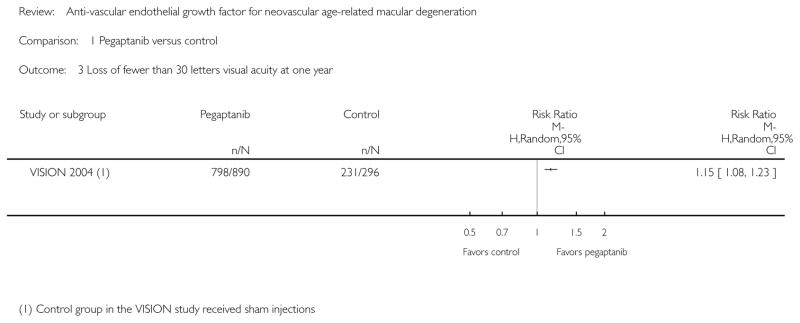
Comparison 1 Pegaptanib versus control, Outcome 3 Loss of fewer than 30 letters visual acuity at one year.
Analysis 1.4.
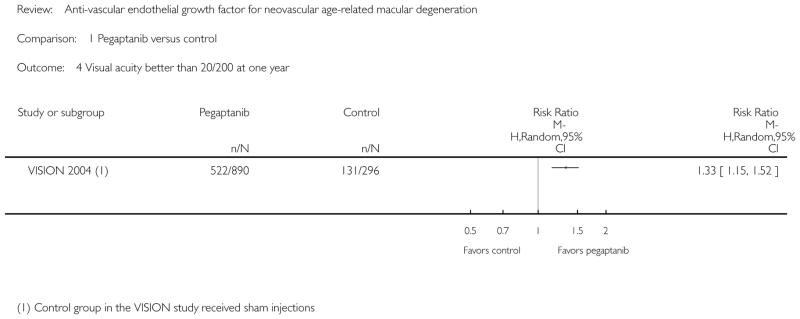
Comparison 1 Pegaptanib versus control, Outcome 4 Visual acuity better than 20/200 at one year.
Analysis 1.5.
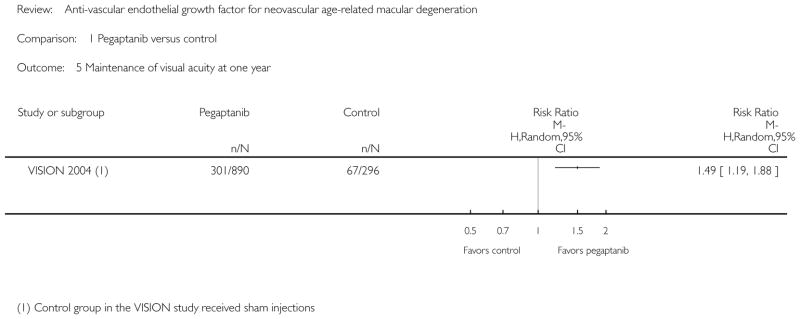
Comparison 1 Pegaptanib versus control, Outcome 5 Maintenance of visual acuity at one year.
Analysis 1.6.
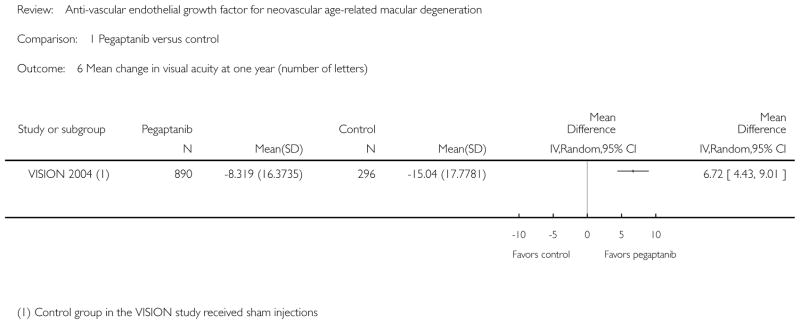
Comparison 1 Pegaptanib versus control, Outcome 6 Mean change in visual acuity at one year (number of letters).
Analysis 1.7.
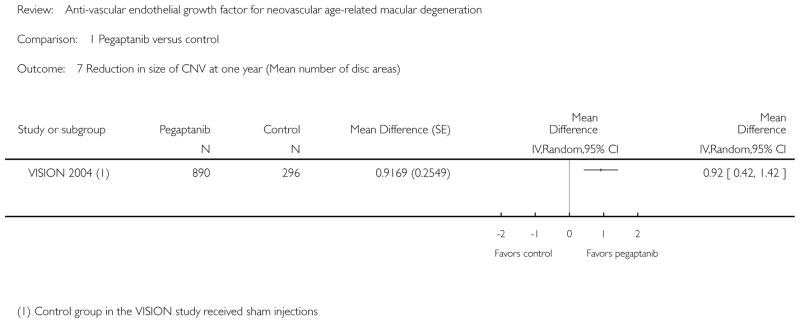
Comparison 1 Pegaptanib versus control, Outcome 7 Reduction in size of CNV at one year (Mean number of disc areas).
Analysis 1.8.
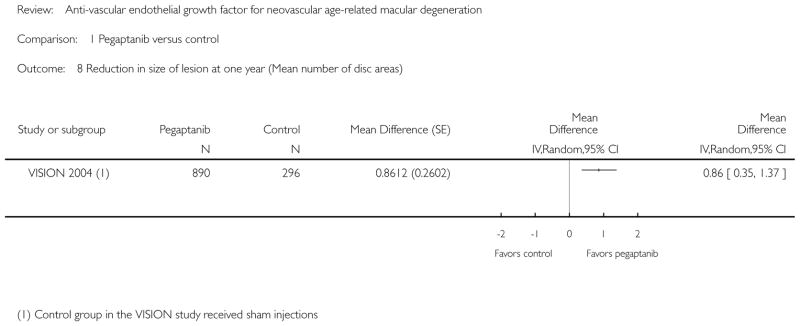
Comparison 1 Pegaptanib versus control, Outcome 8 Reduction in size of lesion at one year (Mean number of disc areas).
Analysis 2.1.
Comparison 2 Ranibizumab versus control, Outcome 1 Gain of 15 letters or more visual acuity at one year.
Analysis 2.2.
Comparison 2 Ranibizumab versus control, Outcome 2 Gain of 15 letters or more visual acuity at two years.
Analysis 2.3.
Comparison 2 Ranibizumab versus control, Outcome 3 Loss of fewer than 15 letters visual acuity at one year.
Analysis 2.4.
Comparison 2 Ranibizumab versus control, Outcome 4 Loss of fewer than 15 letters visual acuity at two years.
Analysis 2.5.
Comparison 2 Ranibizumab versus control, Outcome 5 Loss of fewer than 30 letters visual acuity at one year.
Analysis 2.6.
Comparison 2 Ranibizumab versus control, Outcome 6 Loss of fewer than 30 letters visual acuity at two years.
Analysis 2.7.
Comparison 2 Ranibizumab versus control, Outcome 7 Visual acuity better than 20/200 at one year.
Analysis 2.8.
Comparison 2 Ranibizumab versus control, Outcome 8 Visual acuity better than 20/200 at two years.
Analysis 2.9.
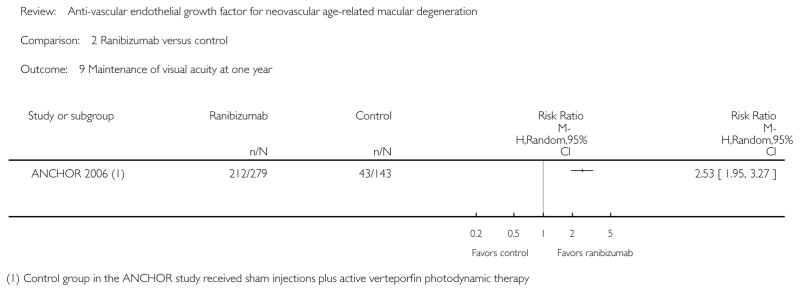
Comparison 2 Ranibizumab versus control, Outcome 9 Maintenance of visual acuity at one year.
Analysis 2.10.
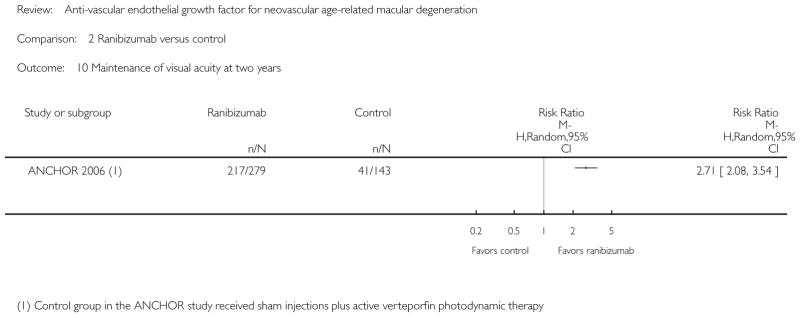
Comparison 2 Ranibizumab versus control, Outcome 10 Maintenance of visual acuity at two years.
Analysis 2.11.
Comparison 2 Ranibizumab versus control, Outcome 11 Mean change in visual acuity at one year (number of letters).
Analysis 2.12.
Comparison 2 Ranibizumab versus control, Outcome 12 Mean change in visual acuity at two years (number of letters).
Analysis 2.13.
Comparison 2 Ranibizumab versus control, Outcome 13 Reduction in size of lesion at one year (Mean number of disc areas).
Analysis 2.14.
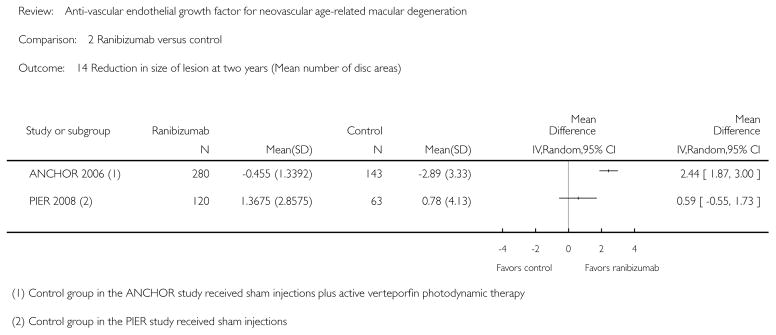
Comparison 2 Ranibizumab versus control, Outcome 14 Reduction in size of lesion at two years (Mean number of disc areas).
Analysis 2.15.
Comparison 2 Ranibizumab versus control, Outcome 15 Mean change in quality of life scores at one year.
Analysis 2.16.
Comparison 2 Ranibizumab versus control, Outcome 16 Mean change in quality of life scores at two years.
Analysis 3.1.
Comparison 3 Bevacizumab versus control, Outcome 1 Gain of 15 letters or more visual acuity at one year.
Analysis 3.2.
Comparison 3 Bevacizumab versus control, Outcome 2 Loss of fewer than 15 letters visual acuity at one year.
Analysis 4.1.
Comparison 4 Bevacizumab versus ranibizumab, Outcome 1 Gain of 15 letters or more visual acuity at one year.
Analysis 4.2.
Comparison 4 Bevacizumab versus ranibizumab, Outcome 2 Gain of 15 letters or more visual acuity at two years.
Analysis 4.3.
Comparison 4 Bevacizumab versus ranibizumab, Outcome 3 Loss of fewer than 15 letters visual acuity at one year.
Analysis 4.4.
Comparison 4 Bevacizumab versus ranibizumab, Outcome 4 Loss of fewer than 15 letters visual acuity at two years.
Analysis 4.5.
Comparison 4 Bevacizumab versus ranibizumab, Outcome 5 Visual acuity better than 20/200 at one year.
Analysis 4.6.
Comparison 4 Bevacizumab versus ranibizumab, Outcome 6 Visual acuity better than 20/200 at two years.
Analysis 4.7.
Comparison 4 Bevacizumab versus ranibizumab, Outcome 7 Mean change in visual acuity at one year (number of letters).
Analysis 4.8.
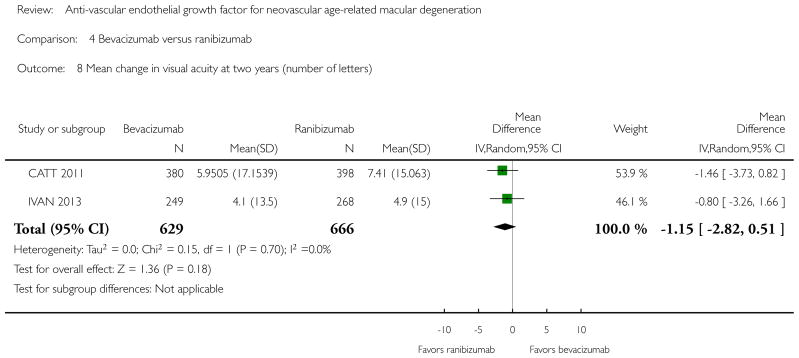
Comparison 4 Bevacizumab versus ranibizumab, Outcome 8 Mean change in visual acuity at two years (number of letters).
Analysis 4.9.
Comparison 4 Bevacizumab versus ranibizumab, Outcome 9 Reduction in central retinal thickness at one year.
Analysis 4.10.
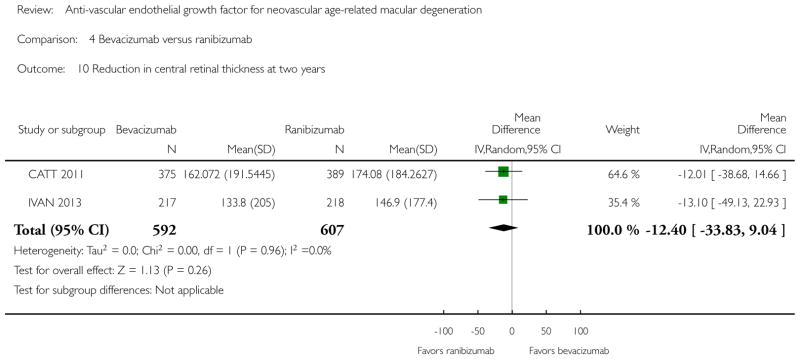
Comparison 4 Bevacizumab versus ranibizumab, Outcome 10 Reduction in central retinal thickness at two years.
Analysis 4.11.
Comparison 4 Bevacizumab versus ranibizumab, Outcome 11 No problems in quality of life domain at one year.
Analysis 4.12.
Comparison 4 Bevacizumab versus ranibizumab, Outcome 12 No problems in quality of life domain at two years.
DIFFERENCES BETWEEN PROTOCOL AND REVIEW
The inclusion criteria were modified between the 2008 publication and this update to the review. In the 2008 publication, all trials that investigated anti-VEGF agents, alone or in conjunction with other treatments, were eligible for inclusion in the review. For this update of the review, we did not include studies in which anti-VEGF treatment was given in combination with other AMD treatments. These combination therapies for AMD will be covered in a separate Cochrane review. Thus, the FOCUS 2006 trial, which was included in the 2008 publication, was not included in this update of the review.
The primary outcome for this update was changed from ‘loss of 15 letters or more of visual acuity at one year to ‘gain of 15 letters or more of visual acuity at one year’. The primary outcome was changed from the protocol and 2008 publication to reflect advancements in the treatment of AMD, which now provide the potential to improve vision. We swapped the number of events with non-events for negative outcomes in order to maintain the same direction of the treatment effect across outcomes.
CONTRIBUTIONS OF AUTHORS
Contributions to the first published version of this review (2008)
Conceiving the review: MK
Designing the review: MK, SSV
Coordinating the review: MK, SSV
Data collection for the review
Designing search strategies: CEVG Trials Search Co-ordinator, MK, SSV
Undertaking manual searches: MK, SSV
Screening search results: MK, SSV
Organising retrieval of papers: MK, SSV
Screening retrieved papers against inclusion criteria: MK, SSV
Appraising quality of papers: MK, SSV
Abstracting data from papers: MK, SSV
Writing to authors of papers for additional information: MK, SSV
Providing additional data about papers: MK
Obtaining and screening data on unpublished studies: MK, SSV
Data management for the review: MK, SSV
Entering data into RevMan: MK, SSV
Analysis of data: MK, SSV
Interpretation of data
Providing a methodological perspective: SSV, MK
Providing a clinical perspective: MK, SSV
Providing a policy perspective: MK
Writing the review: MK, SSV
Securing funding for the review: MK, CEVG US Project
Performing previous work that was the foundation of current study: MK
Guarantor for the review: MK
Contributions to updating the review (2014)
Data collection for the review
Screening search results: KL, BSH, SSV, MK
Organising retrieval of papers: KL
Screening retrieved papers against inclusion criteria: KL, BSH, SSV, MK
Appraising quality of papers: KL, BSH, SSV, MK
Abstracting data from papers: KL, BSH, SSV, MK
Writing to authors of papers for additional information: KL
Providing additional data about papers: MK, BSH
Data management for the review: KL, BSH, SSV, MK
Entering data into RevMan: KL
Analysis of data: KL, BSH, SSV, MK
Interpretation of data
Providing a methodological perspective: KL, BSH, SSV, MK
Providing a clinical perspective: SDS, MK, BSH, SSV
Providing a policy perspective: SDS, MK, BSH
Writing the review: SDS, KL, SSV, MK, BSH
Footnotes
Indicates the major publication for the study
DECLARATIONS OF INTEREST
None known.
References to studies included in this review
- ABC 2010 {published and unpublished data}.Keane PA, Heussen FM, Ouyang Y, Mokwa N, Walsh AC, Tufail A, et al. Assessment of differential pharmacodynamic effects using optical coherence tomography in neovascular age-related macular degeneration. Investigative Ophthalmology and Visual Science. 2012;53(3):1152–61. doi: 10.1167/iovs.11-8130. [DOI] [PMC free article] [PubMed] [Google Scholar]; Patel PJ, Chen FK, Cruz L, Rubin GS, Tufail A. Contrast sensitivity outcomes in the ABC Trial: a randomized trial of bevacizumab for neovascular age-related macular degeneration. Investigative Ophthalmology and Visual Science. 2011;52(6):3089–93. doi: 10.1167/iovs.10-6208. [DOI] [PubMed] [Google Scholar]; Patel PJ, Henderson L, Sivaprasad S, Bunce C, Wormald R, Tufail A. The ABC trial - a randomized double-masked phase III study of the efficacy and safety of Avastin® (Bevacizumab) intravitreal injections compared to standard therapy in subjects with choroidal neovascularization secondary to age-related macular degeneration (AMD) Investigative Ophthalmology and Visual Science. 2007;48 doi: 10.1186/1745-6215-9-56. ARVO E-abstract 4536. [DOI] [PMC free article] [PubMed] [Google Scholar]; Patel PJ, Tufail A, Bunce C, da Cruz L, Dowler J, Egan C, et al. A randomised, double-masked phase III/IV study of the efficacy and safety of Avastin® (Bevacizumab) intravitreal injections compared to standard therapy in subjects with choroidal neovascularisation secondary to age-related macular degeneration: clinical trial design. Trials. 2008;9:56. doi: 10.1186/1745-6215-9-56. [DOI] [PMC free article] [PubMed] [Google Scholar]; * Tufail A, Patel PJ, Egan C, Hykin P, da Cruz L, Gregor Z, et al. Bevacizumab for neovascular age related macular degeneration (ABC Trial): multicentre randomised double masked study. BMJ. 2010;340:c2459. doi: 10.1136/bmj.c2459. [DOI] [PubMed] [Google Scholar]
- ANCHOR 2006 {published and unpublished data}.Alexander SG, Blodi BA, Webster MKW, Elledge JA, Hiner CJ, Armstrong J, et al. Ranibizumab (Lucentis®) in subjects With predominantly classic CNV: reading center evaluation of angiographic eligibility characteristics and baseline fluorescein angiographic data. Investigative Ophthalmology and Visual Science. 2006;47 ARVO E-abstract 2207. [Google Scholar]; Barbazetto I, Saroj N, Shapiro H, Wong P, Freund KB. Dosing regimen and the frequency of macular hemorrhages in neovascular age-related macular degeneration treated with ranibizumab. Retina. 2010;30(9):1376–85. doi: 10.1097/IAE.0b013e3181dcfb0b. [DOI] [PubMed] [Google Scholar]; Barbazetto IA, Saroj N, Shapiro H, Wong P, Ho AC, Freund KB. Incidence of new choroidal neovascularization in fellow eyes of patients treated in the MARINA and ANCHOR trials. American Journal of Ophthalmology. 2010;149(6):939–46. doi: 10.1016/j.ajo.2010.01.007. [DOI] [PubMed] [Google Scholar]; Bressler NM, Boyer DS, Williams DF, Butler S, Francom SF, Brown B, et al. Cerebrovascular accidents in patients treated for choroidal neovascularization with ranibizumab in randomized controlled trials. Retina. 2012;32(9):1821–8. doi: 10.1097/IAE.0b013e31825db6ba. [DOI] [PubMed] [Google Scholar]; Bressler NM, Chang TS, Fine JT, Dolan CM, Ward J Anti-VEGF Antibody for the Treatment of Predominantly Classic Choroidal Neovascularization in Age-Related Macular Degeneration (ANCHOR) Research Group. Improved vision-related function after ranibizumab vs photodynamic therapy: a randomized clinical trial. Archives of Ophthalmology. 2009;127(1):13–21. doi: 10.1001/archophthalmol.2008.562. [DOI] [PubMed] [Google Scholar]; Bressler NM, Chang TS, Suñer IJ, Fine JT, Dolan CM, Ward J, et al. Vision-related function after ranibizumab treatment by better- or worse-seeing eye: clinical trial results from MARINA and ANCHOR. Ophthalmology. 2010;117(4):747–56. doi: 10.1016/j.ophtha.2009.09.002. [DOI] [PubMed] [Google Scholar]; Bressler NM, Chang TS, Varma R, Suner I, Lee P, Dolan CM, et al. Driving ability reported by neovascular age-related macular degeneration patients after treatment with ranibizumab. Ophthalmology. 2013;120(1):160–8. doi: 10.1016/j.ophtha.2012.07.027. [DOI] [PubMed] [Google Scholar]; Bressler NM, Dolan CM, Fine J, Marceau C, Chang TS. Vision-specific quality of life at 12 months in predominantly classic neovascular AMD in ANCHOR: a phase III trial of ranibizumab and verteporfin PDT. European VitreoRetinal Society; Symposium II: Anti-Angiogenesis (Part 2); 2006. [accessed 13 March 2013]. Available at www.evrs.eu/2006-evrs-congress-cannes. [Google Scholar]; * Brown DM, Kaiser PK, Michels M, Soubrane G, Heier JS, Kim R, et al. Ranibizumab versus verteporfin for neovascular age-related macular degeneration. New England Journal of Medicine. 2006;355(14):1432–44. doi: 10.1056/NEJMoa062655. [DOI] [PubMed] [Google Scholar]; Brown DM, Michels M, Kaiser PK, Heier JS, Sy JP, Ianchulev T, et al. Ranibizumab versus verteporfin photodynamic therapy for neovascular age-related macular degeneration: two-year results of the ANCHOR study. Ophthalmology. 2009;116(1):57–65. doi: 10.1016/j.ophtha.2008.10.018. [DOI] [PubMed] [Google Scholar]; Brown DM, Shapiro H, Schneider S. Subgroup analysis of first-year results of ANCHOR: a phase III, double-masked, randomized comparison of ranibizumab and verteporfin photodynamic therapy for predominantly classic choroidal neovascularization related to age-related macular degeneration. Investigative Ophthalmology and Visual Science. 2006;47 ARVO E-abstract 2963. [Google Scholar]; Chang TS, Fine JT, Bressler N. Self-reported vision-specific quality of life at 1 year in patients with neovascular age-related macular degeneration in 2 phase III randomized clinical trials of ranibizumab (Lucentis®) Investigative Ophthalmology and Visual Science. 2006;47 ARVO E-abstract 5252. [Google Scholar]; Ciulla TA, Shapiro H, Schneider S. Ranibizumab (Lucentis®) for neovascular age-related macular degeneration (AMD): 1-year visual acuity (VA) results for fellow eyes with neovascular AMD in MARINA and ANCHOR. Investigative Ophthalmology and Visual Science. 2007;48 ARVO E-Abstract 4573. [Google Scholar]; Cunningham ET, Feiner L, Chung C, Tuomi L, Ehrlich JS. Incidence of retinal pigment epithelial tears after intravitreal ranibizumab injection for neovascular age-related macular degeneration. Ophthalmology. 2011;118(12):2447–52. doi: 10.1016/j.ophtha.2011.05.026. [DOI] [PubMed] [Google Scholar]; Heier JS, Chung C, Schneider S. Time course of visual acuity changes with ranibizumab (Lucentis®) in the 2-tear ANCHOR study of patients with neovascular age-related macular degeneration (AMD) Investigative Ophthalmology and Visual Science. 2007;48 ARVO E-Abstract 2872. [Google Scholar]; Kaiser PK, Brown DM, Zhang K, Hudson HL, Holz FG, Shapiro H, et al. Ranibizumab for predominantly classic neovascular age-related macular degeneration: subgroup analysis of first-year ANCHOR results. American Journal of Ophthalmology. 2007;144(6):850–7. doi: 10.1016/j.ajo.2007.08.012. [DOI] [PubMed] [Google Scholar]; Korobelnik JF. Consistency of effect of ranibizumab at 2 doses on contrast sensitivity in 3 phase III and IIIB studies of patients with CNV secondary to AMD. European VitreoRetinal Society; Symposium I: Anti-Angiogenesis (Part 1); 2006. [accessed 13 March 2013]. Available at www.evrs.eu/2006-evrs-congress-cannes. [Google Scholar]; Lanzetta P. Ranibizumab and patient-reported outcomes: VFQ-25 data from the ANCHOR and PIER trials in patients with neovascular AMD. Investigative Ophthalmology and Visual Science. 2008;49 ARVO E-abstract 5571. [Google Scholar]; Lanzetta P MARINA and ANCHOR Study Groups. Combined safety of intravitreal ranibizumab in two phase III studies of CNV secondary to ARMD. European VitreoRetinal Society; Symposium I: Anti-Angiogenesis (Part 1); 2006. [accessed 13 March 2013]. Available at www.evrs.eu/2006-evrs-congress-cannes. [Google Scholar]; Loewenstein A, MARINA and ANCHOR Study Groups. Combined efficacy of intravitreal ranibizumab in two phase III studies of choroidal neovascularization secondary to age-related macular degeneration. European VitreoRetinal Society; Symposium I: Anti-Angiogenesis (Part 1); 2006. [accessed 13 March 2013]. Available at www.evrs.eu/2006-evrs-congress-cannes. [Google Scholar]; McDonald HR, Schneider S, Sy JP. One-year results of ANCHOR: a phase III, multicenter, randomized, double-masked comparison of ranibizumab and verteporfin photodynamic therapy in treatment of predominantly classic choroidal neovascularization secondary to age-related macular degeneration. The Macula Society; 2006. p. 114. [Google Scholar]; Rofagha S, Bhisitkul RB, Boyer DS, Sadda SR, Zhang K. Seven-year outcomes in ranibizumab-treated patients in ANCHOR, MARINA, and HORIZON: A multicenter cohort study (SEVEN-UP) Ophthalmology. 2013;120(11):2292–9. doi: 10.1016/j.ophtha.2013.03.046. [DOI] [PubMed] [Google Scholar]; Rosenfeld PJ, Shapiro H, Shams N, Schneider S, Depperschmidt EE MARINA and ANCHOR Study Groups. Baseline and treatment characteristics of patients losing vision at year 1 of the MARINA and ANCHOR trials. Investigative Ophthalmology and Visual Science. 2007;48 ARVO E-abstract 4576. [Google Scholar]; Rosenfeld PJ, Shapiro H, Tuomi L, Webster M, Elledge J, Blodi B. Characteristics of patients losing vision after 2 years of monthly dosing in the phase III ranibizumab clinical trials. Ophthalmology. 2011;118(3):523–30. doi: 10.1016/j.ophtha.2010.07.011. [DOI] [PubMed] [Google Scholar]; Rosenfeld PJ, Shapiro H, Tuomi L, Webster M, Elledge J, Blodi B. Lesion characteristics in ranibizumab (Lucentis®) treated patients with a visual acuity (VA) gain or loss in the MARINA and ANCHOR trials for wet age-related macular degeneration (AMD) Investigative Ophthalmology and Visual Science. 2008;49 ARVO E-abstract 329. [Google Scholar]; Sadda SR, Shapiro H, Schneider S. Anatomic outcomes at 2 years in the ANCHOR study comparing ranibizumab (Lucentis®) and verteporfin photodynamic therapy (PDT) in predominantly classic neovascular age-related macular degeneration (AMD) Investigative Ophthalmology and Visual Science. 2007;48 ARVO E-abstract 4561. [Google Scholar]; Sadda SR, Stoller G, Boyer DS, Blodi BA, Shapiro H, Ianchulev T. Anatomical benefit from ranibizumab treatment of predominantly classic neovascular age-related macular degeneration in the 2-year anchor study. Retina. 2010;30(9):1390–9. doi: 10.1097/IAE.0b013e3181e44599. [DOI] [PubMed] [Google Scholar]; Schwartz SG, Bressler N, Fine JT, Dolan CM, Yu EM, Ward JF, et al. Patient-reported visual function over 24 months in predominantly classic neovascular AMD: results from ANCHOR, a phase III trial of ranibizumab and verteporfin PDT. Investigative Ophthalmology and Visual Science. 2007;48 ARVO E-abstract 1822. [Google Scholar]; Sutter FK, Kurz-Levin MM. Towards an optimized treatment scheme of ranibizumab in patients with subfoveal choroidal neovascularization secondary to age-related macular degeneration: subanalysis of clinical trial data and clinical routine use. Investigative Ophthalmology and Visual Science. 2008;49 ARVO E-abstract 2884. [Google Scholar]; Webster MK, Blodi BA, Elledge JA, Danis RP. Angiographic results of the ANCHOR study of ranibizumab in neovascular age-related macular degeneration: reading center evaluation of angiographic data. Investigative Ophthalmology and Visual Science. 2007;48:ARVO E-Abstract 4583. [Google Scholar]; Weinberg DV, Shapiro H, Ehrlich JS. Ranibizumab treatment outcomes in phakic versus pseudophakic eyes: An individual patient data analysis of 2 phase 3 trials. Ophthalmology. 2013;120(6):1278–82. doi: 10.1016/j.ophtha.2012.11.042. [DOI] [PubMed] [Google Scholar]; Win PH, Bressler NM, Chang TS, Fine JT, Dolan CM, Ward J. Self-reported perception of driving function after ranibizumab therapy in patients with neovascular age-related macular degeneration (AMD) Investigative Ophthalmology and Visual Science. 2008;49 ARVO E-abstract 5578. [Google Scholar]; Wolf S. Visual acuity gain with ranibizumab therapy: two-year data from the MARINA, ANCHOR, and PIER trials in patients with neovascular AMD. Investigative Ophthalmology and Visual Science. 2008;49 ARVO E-abstract 2883. [Google Scholar]; Wolf S, Holz FG, Korobelnik JF, Lanzetta P, Mitchell P, Prünte C, et al. Outcomes following three-line vision loss during treatment of neovascular age-related macular degeneration: subgroup analyses from MARINA and ANCHOR. British Journal of Ophthalmology. 2011;95(12):1713–8. doi: 10.1136/bjophthalmol-2011-300471. [DOI] [PubMed] [Google Scholar]; Yang YC. Two year contrast sensitivity results from the ANCHOR study comparing intravitreal ranibizumab 0.3 mg and 0.5 mg with verteporfin PDT for predominantly classic CNV lesions secondary to age-related macular degeneration. Investigative Ophthalmology and Visual Science. 2007;48 ARVO E-Abstract 4545. [Google Scholar]
- Biswas 2011 {published data only}.Biswas P, Sengupta S, Choudhary R, Home S, Paul A, Sinha S. Comparative role of intravitreal ranibizumab versus bevacizumab in choroidal neovascular membrane in age-related macular degeneration. Indian Journal of Ophthalmology. 2011;59(3):191–6. doi: 10.4103/0301-4738.81023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CATT 2011 {published and unpublished data}. [accessed 20 December 2011];Comparison of Age-related macular degeneration Treatment Trials. www.med.upenn.edu/cpob/studies/documents/CATTEligibilityCriteria.pdf.; * CATT Research Group. Martin DF, Maguire MG, Ying GS, Grunwald JE, Fine SL, Jaffe GJ. Ranibizumab and bevacizumab for neovascular age-related macular degeneration. New England Journal of Medicine. 2011;364(20):1897–908. doi: 10.1056/NEJMoa1102673. [DOI] [PMC free article] [PubMed] [Google Scholar]; Daniel E, Toth CA, Grunwald JE, Jaffe GJ, Martin DF, Fine SL, et al. Risk of scar in the Comparison of Age-related Macular Degeneration Treatments Trials. Ophthalmology. 2014;121(3):656–66. doi: 10.1016/j.ophtha.2013.10.019. [DOI] [PMC free article] [PubMed] [Google Scholar]; Grunwald JE, Daniel E, Huang J, Ying GS, Maguire MG, Toth CA, et al. Risk of geographic atrophy in the Comparison of Age-Related Macular Degeneration Treatments Trials. Ophthalmology. 2014;121(1):150–61. doi: 10.1016/j.ophtha.2013.08.015. [DOI] [PMC free article] [PubMed] [Google Scholar]; Grunwald JE, Daniel E, Ying GS, Pistilli M, Maguire MG, Alexander J, et al. Photographic assessment of baseline fundus morphologic features in the Comparison of Age-Related Macular Degeneration Treatments Trials. Ophthalmology. 2012;119(8):1634–41. doi: 10.1016/j.ophtha.2012.02.013. [DOI] [PMC free article] [PubMed] [Google Scholar]; Hagstrom SA, Ying GS, Pauer GJ, Sturgill-Short GM, Huang J, Callanan DG, et al. Pharmacogenetics for genes associated with age-related macular degeneration in the Comparison of AMD Treatments Trials (CATT) Ophthalmology. 2013;120(3):593–9. doi: 10.1016/j.ophtha.2012.11.037. [DOI] [PMC free article] [PubMed] [Google Scholar]; Jaffe GJ, Martin DF, Toth CA, Daniel E, Maguire MG, Ying GS, et al. Macular morphology and visual acuity in the comparison of age-related macular degeneration treatments trials. Ophthalmology. 2013;120(9):1860–70. doi: 10.1016/j.ophtha.2013.01.073. [DOI] [PMC free article] [PubMed] [Google Scholar]; Maguire MG. Comparing treatments for age-related macular degeneration: safety, effectiveness and cost. LDI Issue Brief. 2012;17(8):1–4. [PubMed] [Google Scholar]; Maguire MG, Daniel E, Shah AR, Grunwald JE, Hagstrom SA, Avery RL, et al. Incidence of choroidal neovascularization in the fellow eye in the comparison of age-related macular degeneration treatments trials. Ophthalmology. 2013;120(10):2035–41. doi: 10.1016/j.ophtha.2013.03.017. [DOI] [PMC free article] [PubMed] [Google Scholar]; Martin DF, Maguire MG, Fine SL, Ying GS, Jaffe GJ, Grunwald JE, et al. Ranibizumab and bevacizumab for treatment of neovascular age-related macular degeneration: Two-year results. Ophthalmology. 2012;119(7):1388–98. doi: 10.1016/j.ophtha.2012.03.053. [DOI] [PMC free article] [PubMed] [Google Scholar]; Ying GS, Huang J, Maguire MG, Jaffe GJ, Grunwald JE, Toth C, et al. Baseline predictors for one-year visual outcomes with ranibizumab or bevacizumab for neovascular age-related macular degeneration. Ophthalmology. 2013;120(1):122–9. doi: 10.1016/j.ophtha.2012.07.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- GEFAL 2013 {published and unpublished data}.Kodjikian L, Souied EH, Mimoun G, Mauget-Faysse M, Behar-Cohen F, Decullier E, et al. Ranibizumab versus bevacizumab for neovascular age-related macular degeneration: Results from the GEFAL noninferiority randomized trial. Ophthalmology. 2013;120(11):2300–9. doi: 10.1016/j.ophtha.2013.06.020. [DOI] [PubMed] [Google Scholar]
- IVAN 2013 {published and unpublished data}. [accessed 4 April 2014];A randomised controlled trial of alternative treatments to Inhibit VEGF in Age-related choroidal Neovascularisation. www.ivan-trial.co.uk/Default.aspx. Erratum: Ranibizumab versus bevacizumab to treat neovascular age-related macular degeneration: one-year findings from the IVAN randomized trial (Ophthalmology (2012) 119 (1399–1411)). Ophthalmology 2012;119(8): 1508.; * Chakravarthy U, Harding SP, Rogers CA, Downes SM, Lotery AJ, Culliford LA on behalf of the IVAN study investigators. Alternative treatments to inhibit VEGF in age-related choroidal neovascularisation: 2-year findings of the IVAN randomised controlled trial. Lancet. 2013;382(9900):1258–67. doi: 10.1016/S0140-6736(13)61501-9. [DOI] [PubMed] [Google Scholar]; Chakravarthy U, Harding SP, Rogers CA, Downes SM, Lotery AJ, Wordsworth S, et al. Ranibizumab versus bevacizumab to treat neovascular age-related macular degeneration: one-year findings from the IVAN randomized trial. Ophthalmology. 2012;119(7):1399–411. doi: 10.1016/j.ophtha.2012.04.015. [DOI] [PubMed] [Google Scholar]; Lotery AJ, Gibson J, Cree AJ, Downes SM, Harding SP, Rogers CA, et al. Pharmacogenetic associations with vascular endothelial growth factor inhibition in participants with neovascular age-related macular degeneration in the IVAN study. Ophthalmology. 2013;120(12):2637–43. doi: 10.1016/j.ophtha.2013.07.046. [DOI] [PubMed] [Google Scholar]
- MANTA 2013 {published and unpublished data}.Krebs I, Schmetterer L, Boltz A, Told R, Vécsei-Marlovits V, Egger S, et al. A randomised double-masked trial comparing the visual outcome after treatment with ranibizumab or bevacizumab in patients with neovascular age-related macular degeneration. British Journal of Ophthalmology. 2013;97(3):266–71. doi: 10.1136/bjophthalmol-2012-302391. [DOI] [PubMed] [Google Scholar]
- MARINA 2006 {published and unpublished data}.Barbazetto I, Saroj N, Shapiro H, Wong P, Freund KB. Dosing regimen and the frequency of macular hemorrhages in neovascular age-related macular degeneration treated with ranibizumab. Retina. 2010;30(9):1376–85. doi: 10.1097/IAE.0b013e3181dcfb0b. [DOI] [PubMed] [Google Scholar]; Barbazetto IA, Saroj N, Shapiro H, Wong P, Ho AC, Freund KB. Incidence of new choroidal neovascularization in fellow eyes of patients treated in the MARINA and ANCHOR trials. American Journal of Ophthalmology. 2010;149(6):939–46. doi: 10.1016/j.ajo.2010.01.007. [DOI] [PubMed] [Google Scholar]; Boyer DS, Antoszyk AN, Awh CC, Bhisitkul RB, Shapiro H, Acharya NR MARINA Study Group. Subgroup analysis of the MARINA study of ranibizumab in neovascular age-related macular degeneration. Ophthalmology. 2007;114(2):246–52. doi: 10.1016/j.ophtha.2006.10.045. [DOI] [PubMed] [Google Scholar]; Bressler NM, Boyer DS, Williams DF, Butler S, Francom SF, Brown B, et al. Cerebrovascular accidents in patients treated for choroidal neovascularization with ranibizumab in randomized controlled trials. Retina. 2012;32(9):1821–8. doi: 10.1097/IAE.0b013e31825db6ba. [DOI] [PubMed] [Google Scholar]; Bressler NM, Chang TS, Suñer IJ, Fine JT, Dolan CM, Ward J, et al. Vision-related function after ranibizumab treatment by better- or worse-seeing eye: clinical trial results from MARINA and ANCHOR. Ophthalmology. 2010;117(4):747–56. doi: 10.1016/j.ophtha.2009.09.002. [DOI] [PubMed] [Google Scholar]; Bressler NM, Chang TS, Varma R, Suner I, Lee P, Dolan CM, et al. Driving ability reported by neovascular age-related macular degeneration patients after treatment with ranibizumab. Ophthalmology. 2013;120(1):160–8. doi: 10.1016/j.ophtha.2012.07.027. [DOI] [PubMed] [Google Scholar]; Chang TS, Bressler NM, Fine JT, Dolan CM, Ward J. Self-reported perception of driving function following ranibizumab treatment in patients with neovascular AMD. Investigative Ophthalmology and Visual Science. 2007;48 ARVO E-Abstract 1830. [Google Scholar]; Chang TS, Bressler NM, Fine JT, Dolan CM, Ward J, Klesert TR, et al. Improved vision-related function after ranibizumab treatment of neovascular age-related macular degeneration: results of a randomized clinical trial. Archives of Ophthalmology. 2007;125(11):1460–9. doi: 10.1001/archopht.125.11.1460. [DOI] [PubMed] [Google Scholar]; Chang TS, Fine JT, Alexander S, Bressler N. Ranibizumab (Lucentis®) self-reported vision specific quality of life through 12 months in age-related macular degeneration patients with minimally classic or occult-with-no-classic choroidal neovascularization in a phase III randomized clinical trial. The Macula Society. 2006:106. [Google Scholar]; Chang TS, Fine JT, Bressler N. Self-reported vision-specific quality of life at 1 year in patients with neovascular age-related macular degeneration in 2 phase III randomized clinical trials of ranibizumab (Lucentis®) Investigative Ophthalmology and Visual Science. 2006;47 ARVO E-abstract 5252. [Google Scholar]; Chang TS, Fine JT, Dolan CM, Marceau C, Bressler NM. Ranibizumab (Lucentis®) vision-specific quality of life through 24 months in neovascular AMD subjects in MARINA: a phase III clinical trial. European VitreoRetinal Society; Symposium II: Anti-Angiogenesis (Part 2); 2006. [accessed 13 March 2013]. Available at www.evrs.eu/2006-evrs-congress-cannes. [Google Scholar]; Ciulla TA, Shapiro H, Schneider S. Ranibizumab (Lucentis®) for neovascular age-related macular degeneration (AMD): 1-year visual acuity (VA) results for fellow eyes with neovascular AMD in MARINA and ANCHOR. Investigative Ophthalmology and Visual Science. 2007;48 ARVO E-abstract 4573. [Google Scholar]; Cunningham ET, Feiner L, Chung C, Tuomi L, Ehrlich JS. Incidence of retinal pigment epithelial tears after intravitreal ranibizumab injection for neovascular age-related macular degeneration. Ophthalmology. 2011;118(12):2447–52. doi: 10.1016/j.ophtha.2011.05.026. [DOI] [PubMed] [Google Scholar]; Heier JS, Shapiro H, Singh AA. Randomized, controlled phase III study of ranibizumab (Lucentis®) for minimally classic or occult neovascular age-related macular degeneration: two-year efficacy results of the MARINA study. Investigative Ophthalmology and Visual Science. 2006;47 ARVO E-abstract 2959. [Google Scholar]; Ho A, Shapiro H, Acharya N. Ranibizumab for neovascular age-related macular degeneration: one-year subanalysis of the MARINA study. The Macula Society. 2006:108. [Google Scholar]; Holekamp NM, Acharya N, Shapiro H. Two-year FA/OCT results of MARINA study of ranibizumab (Lucentis®) in neovascular AMD. American Academy of Ophthalmology. 2006:194. [Google Scholar]; Hurley SF, Matthews JP, Guymer RH. Cost-effectiveness of ranibizumab for neovascular age-related macular degeneration. Cost Effectiveness and Resource Allocation. 2008;6:12. doi: 10.1186/1478-7547-6-12. [DOI] [PMC free article] [PubMed] [Google Scholar]; Kaiser PK, Blodi BA, Shapiro H, Acharya NR MARINA Study Group. Angiographic and optical coherence tomographic results of the MARINA study of ranibizumab in neovascular age-related macular degeneration. Ophthalmology. 2007;114(10):1868–75. doi: 10.1016/j.ophtha.2007.04.030. [DOI] [PubMed] [Google Scholar]; Kokame GT. Anatomic outcomes from the MARINA study of ranibizumab (Lucentis®) for minimally classic or occult neovascular age-related macular degeneration. The Macula Society. 2006:110. [Google Scholar]; Korobelnik JF. Consistency of effect of ranibizumab at 2 doses on contrast sensitivity in 3 phase III and IIIB studies of patients with CNV secondary to AMD. European VitreoRetinal Society; Symposium I: Anti-Angiogenesis (Part 1); 2006. [accessed 13 March 2013]. Available at www.evrs.eu/2006-evrs-congress-cannes. [Google Scholar]; Lanzetta P MARINA and ANCHOR Study Groups. Combined safety of intravitreal ranibizumab in two phase III studies of CNV secondary to ARMD. European VitreoRetinal Society; Symposium I: Anti-Angiogenesis (Part 1); 2006. [accessed 13 March 2013]. Available at www.evrs.eu/2006-evrs-congress-cannes. [Google Scholar]; Loewenstein A MARINA and ANCHOR Study Groups. Combined efficacy of intravitreal ranibizumab in two phase III studies of choroidal neovascularization secondary to age-related macular degeneration. European VitreoRetinal Society; Symposium I: Anti-Angiogenesis (Part 1); 2006. [accessed 13 March 2013]. Available at www.evrs.eu/2006-evrs-congress-cannes. [Google Scholar]; Miller JW, Shapiro H, Acharya N. Randomized, controlled phase III study of ranibizumab (Lucentis®) for minimally classic or occult neovascular age-related macular degeneration: two-year safety results of the MARINA study. Investigative Ophthalmology and Visual Science. 2006;47 ARVO E-abstract 3539. [Google Scholar]; Reichel E, Shapiro H, Acharya N. Subgroup analyses of two-year results of MARINA study of ranibizumab in neovascular AMD. American Academy of Ophthalmology. 2006:194. [Google Scholar]; Rofagha S, Bhisitkul RB, Boyer DS, Sadda SR, Zhang K. Seven-year outcomes in ranibizumab-treated patients in ANCHOR, MARINA, and HORIZON: A multicenter cohort study (SEVEN-UP) Ophthalmology. 2013;120(11):2292–9. doi: 10.1016/j.ophtha.2013.03.046. [DOI] [PubMed] [Google Scholar]; * Rosenfeld PJ, Brown DM, Heier JS, Boyer DS, Kaiser PK, Chung CY, et al. Ranibizumab for neovascular age-related macular degeneration. New England Journal of Medicine. 2006;355(14):1419–31. doi: 10.1056/NEJMoa054481. [DOI] [PubMed] [Google Scholar]; Rosenfeld PJ, Shapiro H, Shams N, Schneider S, Depperschmidt EE MARINA and ANCHOR Study Groups. Baseline and treatment characteristics of patients losing vision at year 1 of the MARINA and ANCHOR trials. Investigative Ophthalmology and Visual Science. 2007;48 ARVO E-abstract 4576. [Google Scholar]; Rosenfeld PJ, Shapiro H, Tuomi L, Webster M, Elledge J, Blodi B. Characteristics of patients losing vision after 2 years of monthly dosing in the phase III ranibizumab clinical trials. Ophthalmology. 2011;118(3):523–30. doi: 10.1016/j.ophtha.2010.07.011. [DOI] [PubMed] [Google Scholar]; Rosenfeld PJ, Shapiro H, Tuomi L, Webster M, Elledge J, Blodi B. Lesion characteristics in ranibizumab (Lucentis®) treated patients with a visual acuity (VA) gain or loss in the MARINA and ANCHOR trials for wet age-related macular degeneration (AMD) Investigative Ophthalmology and Visual Science. 2008;49 ARVO E-abstract 329. [Google Scholar]; Schmidt-Erfurth U, Williams GA MARINA Study Group. Two-year efficacy and safety results from the MARINA study. European VitreoRetinal Society; Symposium I: Anti-Angiogenesis (Part 1); 2006. [accessed 13 March 2013]. Available at www.evrs.eu/2006-evrs-congress-cannes. [Google Scholar]; Suner IJ, Bressler NM, Chang TS, Fine JT, Dolan CM, Ward J. Vision-related function after ranibizumab treatment by better- or worse-seeing eye: 24 month results from MARINA. Investigative Ophthalmology and Visual Science. 2007;48 doi: 10.1016/j.ophtha.2009.09.002. ARVO E-Abstract 1808. [DOI] [PubMed] [Google Scholar]; Sutter FK, Kurz-Levin MM. Towards an optimized treatment scheme of ranibizumab in patients with subfoveal choroidal neovascularization secondary to age-related macular degeneration: subanalysis of clinical trial data and clinical routine use. Investigative Ophthalmology and Visual Science. 2008;49 ARVO E-abstract 2884. [Google Scholar]; Webster MK, Blodi BA, Glaeser Alexander S, Elledge KA, Hiner C, Hurtenbach CH, et al. Ranibizumab (Lucentis®) in subjects with minimally classic or occult CNV (MARINA): reading center evaluation of angiographic eligibility characteristics and baseline fluorescein angiographic data. Investigative Ophthalmology and Visual Science. 2006;47 ARVO E-abstract 2206. [Google Scholar]; Weinberg DV, Shapiro H, Ehrlich JS. Ranibizumab treatment outcomes in phakic versus pseudophakic eyes: An individual patient data analysis of 2 phase 3 trials. Ophthalmology. 2013;120(6):1278–82. doi: 10.1016/j.ophtha.2012.11.042. [DOI] [PubMed] [Google Scholar]; Wolf S. Visual acuity gain with ranibizumab therapy: two-year data from the MARINA, ANCHOR, and PIER trials in patients with neovascular AMD. Investigative Ophthalmology and Visual Science. 2008;49 ARVO E-abstract 2883. [Google Scholar]; Wolf S, Holz FG, Korobelnik JF, Lanzetta P, Mitchell P, Prünte C, et al. Outcomes following three-line vision loss during treatment of neovascular age-related macular degeneration: subgroup analyses from MARINA and ANCHOR. British Journal of Ophthalmology. 2011;95(12):1713–8. doi: 10.1136/bjophthalmol-2011-300471. [DOI] [PubMed] [Google Scholar]; Yu EB, Bressler NM, Fine JT, Ward JF, Dolan CM, Klesert T, et al. Relationship between patient-reported visual function and visual acuity in subjects with neovascular AMD. Investigative Ophthalmology and Visual Science. 2007;48 ARVO E-abstract 1174. [Google Scholar]
- PIER 2008 {published and unpublished data}.Abraham P, Yue H, Shams N. PIER: Year 1 results of a phase IIIb study of ranibizumab efficacy and safety in choroidal neovascularization due to age-related macular degeneration. European VitreoRetinal Society; Symposium I: Anti-Angiogenesis (Part 1); 2006. [accessed 13 March 2013]. Available at www.evrs.eu/2006-evrs-congress-cannes. [Google Scholar]; Abraham P, Yue H, Wilson L. Randomized, double-masked, sham-controlled trial of ranibizumab for neovascular age-related macular degeneration: PIER study year 2. American Journal of Ophthalmology. 2010;150(3):315–24. doi: 10.1016/j.ajo.2010.04.011. [DOI] [PubMed] [Google Scholar]; Barbazetto I, Saroj N, Shapiro H, Wong P, Freund KB. Dosing regimen and the frequency of macular hemorrhages in neovascular age-related macular degeneration treated with ranibizumab. Retina. 2010;30(9):1376–85. doi: 10.1097/IAE.0b013e3181dcfb0b. [DOI] [PubMed] [Google Scholar]; Benz MS, Brown DM, Shapiro H, Tuomi L. Ranibizumab for neovascular age-related macular degeneration (AMD): optical coherence tomography (OCT) vs. visual acuity (VA) changes in PIER study. Investigative Ophthalmology and Visual Science. 2008;49 doi: 10.1167/iovs.08-1689. ARVO E-abstract 347. [DOI] [PMC free article] [PubMed] [Google Scholar]; Bressler NM, Boyer DS, Williams DF, Butler S, Francom SF, Brown B, et al. Cerebrovascular accidents in patients treated for choroidal neovascularization with ranibizumab in randomized controlled trials. Retina. 2012;32(9):1821–8. doi: 10.1097/IAE.0b013e31825db6ba. [DOI] [PubMed] [Google Scholar]; Brown DM, Chung CY, Tuomi L. Ranibizumab (Lucentis®) for neovascular age-related macular degeneration (AMD): optical coherence tomography (OCT) vs. visual acuity (VA) changes in PIER study. The Macula Society. 2008:78. [Google Scholar]; Brown DM, Tuomi L, Shapiro H PIER Study Group. Anatomical measures as predictors of visual outcomes in ranibizumab-treated eyes with neovascular age-related macular degeneration. Retina. 2013;33(1):23–34. doi: 10.1097/IAE.0b013e318263cedf. [DOI] [PubMed] [Google Scholar]; Brown DM, Yue H, Shams N. Ranibizumab (Lucentis®) in neovascular age-related macular degeneration (AMD): subgroup analysis of year 1 PIER efficacy data. Investigative Ophthalmology and Visual Science. 2007;48 ARVO E-Abstract 4540. [Google Scholar]; Cunningham ET, Feiner L, Chung C, Tuomi L, Ehrlich JS. Incidence of retinal pigment epithelial tears after intravitreal ranibizumab injection for neovascular age-related macular degeneration. Ophthalmology. 2011;118(12):2447–52. doi: 10.1016/j.ophtha.2011.05.026. [DOI] [PubMed] [Google Scholar]; Ho AC, Shapiro H, Wilson L. Ranibizumab (Lucentis®) for neovascular age-related macular degeneration (AMD): two-year angiographic results of PIER study. The Macula Society. 2008:164. [Google Scholar]; Ho AC, Yue H, Wilson L. Ranibizumab in wet age-related macular degeneration (AMD): crossover/rollover patient results in PIER study. Investigative Ophthalmology and Visual Science. 2008;49 ARVO E-abstract 368. [Google Scholar]; Kaiser PK, Yue H, Shams N. Subgroups analyses of one-year results of the PIER study of ranibizumab in neovascular AMD. American Academy of Ophthalmology. 2006:195. [Google Scholar]; Lanzetta P. Ranibizumab and patient-reported outcomes: VFQ-25 data from the ANCHOR and PIER trials in patients with neovascular AMD. Investigative Ophthalmology and Visual Science. 2008;49 ARVO E-abstract 5571. [Google Scholar]; Michels M, Shapiro H, Wilson L. Ranibizumab (Lucentis®) for neovascular age-related macular degeneration (AMD): 2-year angiographic results of PIER study. Investigative Ophthalmology and Visual Science. 2008;49 ARVO E-abstract 2882. [Google Scholar]; Mieler WF. PIER: Year 1 FA/OCT results in a study of ranibizumab (Lucentis™) for CNV due to ARMD. European VitreoRetinal Society 2006. [accessed 13 March 2013];Symposium I: Anti-Angiogenesis (Part 1) Available at www.evrs.eu/2006-evrs-congress-cannes.; Regillo CD, Bressler NM, Fine JT, Dolan CM, Marceau C, Chang TS. Vision-specific quality of life at 12 months in subjects with or without classic CNV due to AMD: phase III clinical trial of ranibizumab (Lucentis™) [accessed 13 March 2013];European VitreoRetinal Society 2006. Poster Session. Available at www.evrs.eu/2006-evrs-congress-cannes/poster-session-amdanti-angiogenesis.; * Regillo CD, Brown DM, Abraham P, Yue H, Ianchulev T, Schneider S, et al. Randomized, double-masked, sham-controlled trial of ranibizumab for neovascular age-related macular degeneration: PIER Study year 1. American Journal of Ophthalmology. 2008;145(2):239–48. doi: 10.1016/j.ajo.2007.10.004. [DOI] [PubMed] [Google Scholar]; Regillo CD, Chung CY, Wilson L PIER Study Group. Ranibizumab in neovascular age-related macular degeneration (AMD): crossover/rollover treatment effects in PIER study. The Macula Society. 2008:166. [Google Scholar]; Wolf S. Visual acuity gain with ranibizumab therapy: two-year data from the MARINA, ANCHOR, and PIER trials in patients with neovascular AMD. Investigative Ophthalmology and Visual Science. 2008;49 ARVO E-abstract 2883. [Google Scholar]
- Sacu 2009 {published and unpublished data}.Michels SM, Weigert G, Geitzenauer W, Sacu S, Alina V, Schmidt-Erfurth U. Intravitreal bevacizumab (Avastin®) therapy versus verteporfin therapy and intravitreal triamcinolone for neovascular age-related macular degeneration. Investigative Ophthalmology and Visual Science. 2007;48 ARVO E-abstract 1820. [Google Scholar]; Prager F, Michels S, Sacu S, Weigert G, Dunavölgyi R, Geitzenauer W, et al. Intravitreal bevacizumab (Avastin®) monotherapy versus photodynamic therapy plus intravitreal triamcinolone for neovascular age-related macular degeneration: 12 months results of a prospective, randomized, controlled clinical trial. Investigative Ophthalmology and Visual Science. 2008;49 doi: 10.1136/bjo.2007.125823. ARVO E-abstract 1168. [DOI] [PubMed] [Google Scholar]; * Sacu S, Michels S, Prager F, Weigert G, Dunavoelgyi R, Geitzenauer W, et al. Randomised clinical trial of intravitreal Avastin® vs photodynamic therapy and intravitreal triamcinolone: long-term results. Eye. 2009;23(12):2223–7. doi: 10.1038/eye.2008.423. [DOI] [PubMed] [Google Scholar]; Weigert G, Michels S, Sacu S, Varga A, Prager F, Geitzenauer W, et al. Intravitreal bevacizumab (Avastin®) therapy versus photodynamic therapy plus intravitreal triamcinolone for neovascular age-related macular degeneration: 6-month results of a prospective, randomised, controlled clinical study. British Journal of Ophthalmology. 2008;92(3):356–60. doi: 10.1136/bjo.2007.125823. [DOI] [PubMed] [Google Scholar]
- Subramanian 2010 {published and unpublished data}.Donahue SP, Recchia F, Sternberg P., Jr Bevacizumab vs ranibizumab for age-related macular degeneration: early results of a prospective double-masked, randomized clinical trial. American Journal of Ophthalmology. 2010;150(2):287. doi: 10.1016/j.ajo.2010.04.006. [DOI] [PubMed] [Google Scholar]; Messori A, Fadda V, Trippoli S. Randomized study of bevacizumab vs ranibizumab for age-related macular degeneration: inappropriate conclusions. American Journal of Ophthalmology. 2010;149(5):867. doi: 10.1016/j.ajo.2009.12.039. [DOI] [PubMed] [Google Scholar]; * Subramanian ML, Abedi G, Ness S, Ahmed E, Fenberg M, Daly MK, et al. Bevacizumab vs ranibizumab for age-related macular degeneration: 1-year outcomes of a prospective, double-masked randomised clinical trial. Eye. 2010;24(11):1708–15. doi: 10.1038/eye.2010.147. [DOI] [PubMed] [Google Scholar]; Subramanian ML, Ness S, Abedi G, Ahmed E, Daly M, Feinberg E, et al. Bevacizumab vs ranibizumab for age-related macular degeneration: early results of a prospective double-masked, randomized clinical trial. American Journal of Ophthalmology. 2009;148(6):875–82. doi: 10.1016/j.ajo.2009.07.009. [DOI] [PubMed] [Google Scholar]; Subramanian ML, Ness S, Abedi G, Ahmed E, Daly M, Feinberg E, et al. Reply. American Journal of Ophthalmology. 2010;149(5):867. [Google Scholar]
- VISION 2004 {published and unpublished data}.Chakravarthy U. Efficacy and safety of pegaptanib in age-related macular degeneration: three-year results of the V.I.S.I.O.N. trials. The Macula Society. 2006:116. [Google Scholar]; D’Amico DF. Macugen® in neovascular age-related macular degeneration: exploratory subgroup analyses. American Academy of Ophthalmology. 2005:261. [Google Scholar]; D’Amico DJ. VEGF Inhibition Study in Ocular Neovascularization (VISION): second year efficacy data. Investigative Ophthalmology and Visual Science. 2005;46 ARVO E-abstract 2309. [Google Scholar]; D’Amico DJ, Bird AC. VEGF Inhibition Study in Ocular Neovascularization-1 (VISION-1): safety evaluation from the pivotal Macugen® (pegaptanib sodium) clinical trials. Investigative Ophthalmology and Visual Science. 2004;45 ARVO E-abstract 2363. [Google Scholar]; Eyetech Pharmaceuticals, Inc, Pfizer. Inc. [accessed 20 December 2011];Pegaptanib sodium injection in the treatment of neovascular age-related macular degeneration. www.fda.gov/ohrms/dockets/ac/04/briefing/2004-4053b1.htm.; FDA. [accessed 20 December 2011];Macugen® (pegaptanib sodium injection) for the treatment of neovascular age-related macular degeneration. www.fda.gov/ohrms/dockets/ac/04/briefing/2004-4053b1.htm.; Gragoudas ES. VEGF Inhibition Study in Ocular Neovascularization-1 (VISION-1): efficacy results from phase II/III Macugen® (pegaptanib sodium) clinical trials. Investigative Ophthalmology and Visual Science. 2004;45 ARVO E-abstract 2364. [Google Scholar]; * Gragoudas ES, Adamis AP, Cunningham ET, Jr, Feinsod M, Guyer DR. Pegaptanib for neovascular age-related macular degeneration. New England Journal of Medicine. 2004;351(27):2805–16. doi: 10.1056/NEJMoa042760. [DOI] [PubMed] [Google Scholar]; Jackson TL, Danis RP, Goldbaum M, Slakter JS, Shusterman EM, Oeshaughnessy DJ, et al. Retinal vascular abnormalities in neovascular age-related macular degeneration. Retina. 2014;34(3):568–75. doi: 10.1097/IAE.0b013e3182a487be. [DOI] [PubMed] [Google Scholar]; Kuppermann BD. The V.I.S.I.O.N Study: results with two years of Macugen® and outcomes of earlier treatment in early disease. American Academy of Ophthalmology. 2005:178. [Google Scholar]; Larsen M, Sander B, Villumsen JE, Haamann PH, la Cour M, Lund-Andersen H, et al. Treatment of neovascular age-related macular degeneration with intravitreal vascular endothelial growth factor inhibitor--secondary publication. Ugeskrift for Laeger. 2005;167(35):3301–5. [PubMed] [Google Scholar]; Leys A, Zlateva G, Shah SN, Patel M. Quality of life in patients with age-related macular degeneration: results from the VISION study. Eye. 2008;22(6):792–8. doi: 10.1038/sj.eye.6702900. [DOI] [PubMed] [Google Scholar]; Macugen AMD Study Group. Apte RS, Modi M, Masonson H, Patel M, Whitfield L, et al. Pegaptanib 1-year systemic safety results from a safety-pharmacokinetic trial in patients with neovascular age-related macular degeneration. Ophthalmology. 2007;114(9):1702–12. doi: 10.1016/j.ophtha.2007.02.021. [DOI] [PubMed] [Google Scholar]; Marcus DM. Four-year safety of pegaptanib sodium in neovascular age-related macular degeneration (AMD): results of the V.I.S.I.O.N. trial. Investigative Ophthalmology and Visual Science. 2008;49 ARVO E-abstract 5069. [Google Scholar]; Mieler W. Safety evaluation of second year treatment of age-related macular degeneration with pegaptanib sodium (Macugen®): VEGF Inhibition Study in Ocular Neovascularization (VISION) Investigative Ophthalmology and Visual Science. 2005;46 ARVO E-abstract 1380. [Google Scholar]; Mills E, Heels-Ansdell D, Kelly S, Guyatt G. A randomized trial of Pegaptanib sodium for age-related macular degeneration used an innovative design to explore disease-modifying effects. Journal of Clinical Epidemiology. 2007;60(5):456–60. doi: 10.1016/j.jclinepi.2006.09.001. [DOI] [PubMed] [Google Scholar]; Patel M, Mones J, Leys A, Zlateva G, Shah SN. Quality of life in patients with age-related macular degeneration: results from the VI.S.I.O.N. trial. European VitreoRetinal Society; Poster Session; 2006. [accessed 13 March 2013]. Available at www.evrs.eu/2006-evrs-congress-cannes/poster-session-amdanti-angiogenesis. [Google Scholar]; Rakic JM, Blaise P, Foidart JM, Gragoudas ES, Adamis AP, Feinsod M. Pegaptanib and age-related macular degeneration. New England Journal of Medicine. 2005;352(16):1720–1. doi: 10.1056/NEJM200504213521619. [DOI] [PubMed] [Google Scholar]; Singerman LI. Two-year systemic safety of pegaptanib in patients with neovascular age-related macular degeneration: results of the V.I.S.I.O.N. trials. The Macula Society. 2006:120. [Google Scholar]; Singerman LJ, Masonson H, Patel M, Adamis AP, Buggage R, Cunningham E, et al. Pegaptanib sodium for neovascular age-related macular degeneration: third-year safety results of the VEGF Inhibition Study in Ocular Neovascularisation (VISION) trial. British Journal of Ophthalmology. 2008;92(12):1606–11. doi: 10.1136/bjo.2007.132597. [DOI] [PMC free article] [PubMed] [Google Scholar]; Sjolie AK, Mortensen KK, Hansen MH. Antiangiogenesis therapy of age-related macular degeneration. Ugeskrift for Laeger. 2005;167(35):3267. [PubMed] [Google Scholar]; VEGF Inhibition Study in Ocular Neovascularization (VISION) Clinical Trial Group. Chakravarthy U, Adamis AP, Cunningham ET, Jr, Goldbaum M, Guyer DR, et al. Year 2 efficacy results of 2 randomized controlled clinical trials of pegaptanib for neovascular age-related macular degeneration. Ophthalmology. 2006;113(9):1508. doi: 10.1016/j.ophtha.2006.02.064. [DOI] [PubMed] [Google Scholar]; VEGF Inhibition Study in Ocular Neovascularization (VISION) Clinical Trial Group, . D’Amico DJ, Masonson HN, Patel M, Adamis AP, Cunningham ET, et al. Pegaptanib sodium for neovascular age-related macular degeneration: two-year safety results of the two prospective, multicenter, controlled clinical trials. Ophthalmology. 2006;113(6):1001. doi: 10.1016/j.ophtha.2006.02.027. [DOI] [PubMed] [Google Scholar]; Zlateva G, Patel M, Shah SN. Quality of life in patients with age-related macular degeneration: results from the VISION study. Investigative Ophthalmology and Visual Science. 2006;47 doi: 10.1038/sj.eye.6702900. ARVO E-abstract 2152. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
- Bashshur 2007 {published data only}.Bashshur ZF, Schakal A, Hamam RN, El Haibi CP, Jaafar R, Noureddin BN. Intravitreal bevacizumab vs verteporfin photodynamic therapy for neovascular age-related macular degeneration. Archives of Ophthalmology. 2007;125(10):1357–61. doi: 10.1001/archopht.125.10.1357. [DOI] [PubMed] [Google Scholar]
- BEAT-AMD 2009 {published data only}.Schmid-Kubista KE, Krebs I, Gruenberger B, Schueller J, Binder S. Systemic bevacizumab therapy for exudative neovascular age-related macular degeneration (BEAT-AMD-Study) Investigative Ophthalmology and Visual Science. 2008;49:ARVO E-abstract 304. doi: 10.1136/bjo.2008.144410. [DOI] [PubMed] [Google Scholar]; Schmid-Kubista KE, Krebs I, Gruenberger B, Zeiler F, Schueller J, Binder S. Systemic bevacizumab (Avastin®) therapy for exudative neovascular age-related macular degeneration. The BEAT-AMD-Study. British Journal of Ophthalmology. 2009;93(7):914–9. doi: 10.1136/bjo.2008.144410. [DOI] [PubMed] [Google Scholar]
- Bolz 2008 {published data only}.Bolz M, Pruente C, Benesch T, Ritter M, Deak G, Golbaz I, et al. The relevance of measuring central retinal thickness during intra-vitreal therapy with ranibizumab: analyzing a multi-center clinical trial. Investigative Ophthalmology and Visual Science. 2008;49 ARVO E-abstract 5576. [Google Scholar]
- Cohen 2008 {published data only}.Cohen SY, Bremond-Gignac D, Quentel G, Mimoun G, Citterio T, Bisot-Locard S, et al. Cost-effectiveness sequential modeling of ranibizumab versus usual care in age-related macular degeneration. Graefe’s Archive for Clinical and Experimental Ophthalmology. 2008;246(11):1527–34. doi: 10.1007/s00417-008-0890-8. [DOI] [PubMed] [Google Scholar]
- Costagliola 2010 {published data only}.Costagliola C, Romano MR, Rinaldi M, dell’Omo R, Chiosi F, Menzione M, Semeraro F. Low fluence rate photodynamic therapy combined with intravitreal bevacizumab for neovascular age-related macular degeneration. British Journal of Ophthalmology. 2010;94(2):180–4. doi: 10.1136/bjo.2009.159343. [DOI] [PubMed] [Google Scholar]
- Earnshaw 2007 {published data only}.Earnshaw SR, Moride Y, Rochon S. Cost-effectiveness of pegaptanib compared to photodynamic therapy with verteporfin and to standard care in the treatment of subfoveal wet age-related macular degeneration in Canada. Clinical Therapeutics. 2007;29(9):2096–106. doi: 10.1016/j.clinthera.2007.09.001. [DOI] [PubMed] [Google Scholar]
- Erdokur 2009 {published data only}.Erdokur O, Tetikoglu M, Ozturk M, Elcioglu M. Results of comparison in use to alternative therapy methods for subfoveal choroidal neovascularization secondary to age-related macular degeneration. Retina-Vitreus. 2009;17(4):245–50. [Google Scholar]
- EXTEND-I 2008 {published data only}.Tano Y. The safety and efficacy of ranibizumab in Japanese patients with subfoveal choroidal neovascularization secondary to age-related macular degeneration: 12-month results from the phase I/II EXTEND-I study. Investigative Ophthalmology and Visual Science. 2008;49:ARVO E-abstract 272. [Google Scholar]; Tano Y, Ohji M EXTEND-I Study Group. EXTEND-I: safety and efficacy of ranibizumab in Japanese patients with subfoveal choroidal neovascularization secondary to age-related macular degeneration. Acta Ophthalmologica. 2010;88(3):309–16. doi: 10.1111/j.1755-3768.2009.01843.x. [DOI] [PubMed] [Google Scholar]
- Eyetech Study 2003 {published data only}.Eyetech Study Group. Anti-vascular endothelial growth factor therapy for subfoveal choroidal neovascularization secondary to age-related macular degeneration: phase II study results. Ophthalmology. 2003;110(5):979–86. doi: 10.1016/S0161-6420(03)00085-X. [DOI] [PubMed] [Google Scholar]
- Falkenstein 2007 {published data only}.Falkenstein IA, Cheng L, Morrison VL, Kozak I, Tammewar AM, Freeman WR. Standardized visual acuity results associated with primary versus secondary bevacizumab (Avastin®) treatment for choroidal neovascularization in age-related macular degeneration. Retina. 2007;27(6):701–6. doi: 10.1097/IAE.0b013e3180654240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fletcher 2008 {published data only}.Fletcher EC, Lade RJ, Adewoyin T, Chong NV. Computerized model of cost-utility analysis for treatment of age-related macular degeneration. Ophthalmology. 2008;115(12):2192–8. doi: 10.1016/j.ophtha.2008.07.018. [DOI] [PubMed] [Google Scholar]
- FOCUS 2006 {published and unpublished data}.Antoszyk AN, Tuomi L, Chung CY, Singh A FOCUS Study Group. Ranibizumab combined with verteporfin photodynamic therapy in neovascular age-related macular degeneration (FOCUS): year 2 results. American Journal of Ophthalmology. 2008;145(5):862–74. doi: 10.1016/j.ajo.2007.12.029. [DOI] [PubMed] [Google Scholar]; Heier JS, Boyer DS, Ciulla TA, Ferrone PJ, Jumber MJ, Gentile RC, et al. Ranibizumab combined with verteporfin photodynamic therapy in neovascular age-related macular degeneration: year 1 results of the FOCUS study. Archives of Ophthalmology. 2006;124(11):1532–42. doi: 10.1001/archopht.124.11.1532. [DOI] [PubMed] [Google Scholar]; Heier JS FOCUS Study Group. Intravitreal ranibizumab with verteporfin photodynamic therapy for neovascular age-related macular degeneration: year one results. Program and abstracts of the American Society of Retina Specialists 23rd Annual Meeting; 2005 July 16–20; Montreal. 2005. [Google Scholar]
- Hahn 2007 {published data only}.Hahn R, Sacu S, Michels S, Varga A, Weigert G, Geitzenauer W, et al. Intravitreal bevacizumab versus verteporfin and intravitreal triamcinolone acetonide in patients with neovascular age-related macula degeneration. Der Ophthalmologe. 2007;104(7):588–93. doi: 10.1007/s00347-007-1547-4. [DOI] [PubMed] [Google Scholar]
- Hatta 2010 {published data only}.Hatta Y, Ishikawa K, Nishihara H, Ozawa S, Ito Y, Terasaki H. Effect of photodynamic therapy alone or combined with posterior subtenon triamcinolone acetonide or intravitreal bevacizumab on choroidal hypofluorescence by indocyanine green angiography. Retina. 2010;30(3):495–502. doi: 10.1097/IAE.0b013e3181bcedbe. [DOI] [PubMed] [Google Scholar]
- Heier 2006 {published data only}.Heier JS, Antoszyk AN, Pavan PR, Leff SR, Rosenfeld PJ, Ciulla TA, et al. Ranibizumab for treatment of neovascular age-related macular degeneration: a phase I/II multicenter, controlled, multidose study. Ophthalmology. 2006;113(4):642, e1–4. doi: 10.1016/j.ophtha.2005.10.052. [DOI] [PubMed] [Google Scholar]
- Hernandez-Pastor 2008 {published data only}.Hernandez-Pastor LJ, Ortega A, Garcia-Layana A, Giraldez J. Cost-effectiveness of ranibizumab compared with photodynamic treatment of neovascular age-related macular degeneration. Clinical Therapeutics. 2008;30(12):2436–51. doi: 10.1016/j.clinthera.2008.12.025. [DOI] [PubMed] [Google Scholar]
- Hernandez-Pastor 2010 {published data only}.Hernandez-Pastor LJ, Ortega A, Garcia-Layana A, Giraldez J. Cost-effectiveness of ranibizumab compared with pegaptanib in neovascular age-related macular degeneration. Investigative Ophthalmology and Visual Science. 2010;248(4):467–76. doi: 10.1007/s00417-009-1156-9. [DOI] [PubMed] [Google Scholar]
- Javitt 2008 {published data only}.Javitt JC, Zlateva GP, Earnshaw SR, Pleil AM, Graham CN, Brogan AJ, et al. Cost-effectiveness model for neovascular age-related macular degeneration: comparing early and late treatment with pegaptanib sodium based on visual acuity. Value in Health. 2008;11(4):563–74. doi: 10.1111/j.1524-4733.2007.00283.x. [DOI] [PubMed] [Google Scholar]
- Lai 2009 {published data only}.Lai TY, Liu DT, Chan KP, Luk FO, Pang CP, Lam DS. Visual outcomes and growth factor changes of two dosages of intravitreal bevacizumab for neovascular age-related macular degeneration: a randomized, controlled trial. Retina. 2009;29(9):1218–26. doi: 10.1097/IAE.0b013e3181b32c45. [DOI] [PubMed] [Google Scholar]
- Lazic 2007 {published data only}.Lazic R, Gabric N. Verteporfin therapy and intravitreal bevacizumab combined and alone in choroidal neovascularization due to age-related macular degeneration. Ophthalmology. 2007;114(6):1179–85. doi: 10.1016/j.ophtha.2007.03.006. [DOI] [PubMed] [Google Scholar]
- Li 2012 {published data only}.Fang K, Tian J, Qing X, Li S, Hou J, Li J, et al. Predictors of visual response to intravitreal bevacizumab for treatment of neovascular age-related macular degeneration. Journal of Ophthalmology. 2013;2013:676049. doi: 10.1155/2013/676049. [DOI] [PMC free article] [PubMed] [Google Scholar]; Li X, Hu Y, Sun X, Zhang J, Zhang M Neovascular Age-Related Macular Degeneration Treatment Trial Using Bevacizumab (NATTB) Bevacizumab for neovascular age-related macular degeneration in China. Ophthalmology. 2012;119(10):2087–93. doi: 10.1016/j.ophtha.2012.05.016. [DOI] [PubMed] [Google Scholar]
- Li 2013 {published data only}.Li J, Zhang H, Sun P, Gu F, Liu ZL. Bevacizumab vs ranibizumab for neovascular age-related macular degeneration in Chinese patients. International Journal of Ophthalmology. 2013;6(2):169–73. doi: 10.3980/j.issn.2222-3959.2013.02.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matthe 2011 {published data only}.Matthe E, Sandner D. Monotherapy of exudative age-related macular degeneration with ranibizumab in patients at cardiovascular risk. Advantages of ranibizumab compared to a combination with pegaptanib. Der Ophthalmologe. 2011;108(4):337–41. doi: 10.1007/s00347-010-2300-y. [DOI] [PubMed] [Google Scholar]
- MIRA-1 2005 {published data only}.Pulido JS, Anderson WB, Jr, Flynn JT, Lichter PR, Sanders D. Multicenter prospective, randomized, double-masked, placebo-controlled study of rheopheresis to treat neovascular age-related macular degeneration: Interim analysis. Transactions of the American Ophthalmological Society. 2002;100:85–107. [PMC free article] [PubMed] [Google Scholar]; Pulido JS, Sanders D, Klingel R. Rheopheresis for age-related macular degeneration: clinical results and putative mechanism of action. Canadian Journal of Ophthalmology. 2005;40(3):332–40. doi: 10.1016/S0008-4182(05)80076-6. [DOI] [PubMed] [Google Scholar]
- Modarres 2009 {published data only}.Modarres M, Naseripour M, Falavarjani KG, Nikeghbali A, Hashemi M, Parvaresh MM. Intravitreal injection of 2.5 mg versus 1.25 mg bevacizumab (Avastin®) for treatment of CNV associated with AMD. Retina. 2009;29(3):319–24. doi: 10.1097/IAE.0b013e318198148e. [DOI] [PubMed] [Google Scholar]
- Neubauer 2007 {published data only}.Neubauer AS, Holz FG, Schrader W, Back EI, Kuhn T, Hirneiss C, et al. Cost-utility analysis of ranibizumab (Lucentis®) in neovascular macular degeneration. Klinische Monatsblatter fur Augenheilkunde. 2007;224(9):727–32. doi: 10.1055/s-2007-963470. [DOI] [PubMed] [Google Scholar]
- Nguyen 2006 {published data only}.Nguyen QD, Shah SM, Hafiz G, Quinlan E, Sung J, Chu K, et al. A phase I trial of an IV-administered vascular endothelial growth factor trap for treatment in patients with choroidal neovascularization due to age-related macular degeneration. Ophthalmology. 2006;113(9):1522. doi: 10.1016/j.ophtha.2006.05.055. [DOI] [PubMed] [Google Scholar]
- Nowak 2012 {published data only}.Nowak MS, Jurowski P, Grzybowski A, Go R, Pastuszka M, Kapica A, et al. A prospective study on different methods for the treatment of choroidal neovascularization. The efficacy of verteporfin photodynamic therapy, intravitreal bevacizumab and transpupillary thermotherapy in patients with neovascular age-related macular degeneration. Medical Science Monitor. 2012;18(6):CR374–80. doi: 10.12659/MSM.882907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parodi 2012 {published data only}.Parodi MB, Cascavilla M, Papayannis A, Kontadakis DS, Bandello F, Iacono P. Intravitreal bevacizumab in advanced-stage neovascular age-related macular degeneration with visual acuity lower than 20/200. Archives of Ophthalmology. 2012;130(7):934–5. doi: 10.1001/archophthalmol.2011.2617. [DOI] [PubMed] [Google Scholar]
- PERSPECTIVES 2012 {published data only}.Chakravarthy U, Staurenghi G, Kwok K, Tressler CS, Buggage R PERSPECTIVES Study Group. Treating early choroidal neovascularisation with pegaptanib sodium in patients with neovascular age-related macular degeneration: findings of the PERSPECTIVES study. British Journal of Ophthalmology. 2012;96(10):1351–4. doi: 10.1136/bjophthalmol-2011-301444. [DOI] [PubMed] [Google Scholar]
- Raftery 2007 {published data only}.Raftery J, Clegg A, Jones J, Tan SC, Lotery A. Ranibizumab (Lucentis®) versus bevacizumab (Avastin®): modelling cost effectiveness. British Journal of Ophthalmology. 2007;91(9):1244–6. doi: 10.1136/bjo.2007.116616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- SAILOR 2009 {published data only}.Boyer DS, Heier JS, Brown DM, Francom SF, Ianchulev T, Rubio RG. A Phase IIIb study to evaluate the safety of ranibizumab in subjects with neovascular age-related macular degeneration. Ophthalmology. 2009;116(9):1731–9. doi: 10.1016/j.ophtha.2009.05.024. [DOI] [PubMed] [Google Scholar]; Reichel E, Francom S, Rubio R. Ranibizumab (Lucentis®) safety in previously treated and newly diagnosed patients with neovascular age-related macular degeneration (AMD): the SAILOR study. The Macula Society. 2008:168. [Google Scholar]
- Schmid-Kubista 2011 {published data only}.Schmid-Kubista KE, Krebs I, Ansari-Shahrezaei S, Haas P, Hagen S, Binder S. Comparing treatment of neovascular age-related macular degeneration with sequential intravitreal Avastin and Macugen versus intravitreal mono-therapy-a pilot study. Current Eye Research. 2011;36(10):958–63. doi: 10.3109/02713683.2011.597536. [DOI] [PubMed] [Google Scholar]
- SUMMIT 2007 {published data only}.Slakter JS DENALI Study Group. Combination therapy with verteporfin PDT and ranibizumab for subfoveal choroidal neovascularization due to AMD. Investigative Ophthalmology and Visual Science. 2007;48:E-Abstract 1817. [Google Scholar]
- Suñer 2009 {published data only}.Suñer IJ, Kokame GT, Yu E, Ward J, Dolan C, Bressler NM. Responsiveness of NEI VFQ-25 to changes in visual acuity in neovascular AMD: validation studies from two phase 3 clinical trials. Investigative Ophthalmology and Visual Science. 2009;50(8):3629–35. doi: 10.1167/iovs.08-3225. [DOI] [PubMed] [Google Scholar]
- Tano 2008 {published data only}.Tano Y Pegaptanib Sodium Multi-center Study Group. Pegaptanib sodium one-year treatment study for neovascular age-related macular degeneration. Nippon Ganka Gakkai Zasshi. 2008;112(7):590–600. [PubMed] [Google Scholar]
- Vallance 2010 {published data only}.Vallance JH, Johnson B, Majid MA, Banerjee S, Mandal K, Bailey CC. A randomised prospective double-masked exploratory study comparing combination photodynamic treatment and intravitreal ranibizumab vs intravitreal ranibizumab monotherapy in the treatment of neovascular age-related macular degeneration. Eye. 2010;24(10):1561–7. doi: 10.1038/eye.2010.84. [DOI] [PubMed] [Google Scholar]
- VERITAS 2006 {published data only}.Mieler WF The VERITAS trial. VERITAS - The rationale and design of a combination therapy trial for wet AMD. Investigative Ophthalmology & Visual Science. 2006;47:E-Abstract 5232. [Google Scholar]
- VIEW 2014 {published data only}.Schmidt-Erfurth U, Kaiser PK, Korobelnik JF, Brown DM, Chong V, Nguyen QD, et al. Intravitreal aflibercept injection for neovascular age-related macular degeneration: ninety-six-week results of the VIEW studies. Ophthalmology. 2014;121(1):193–201. doi: 10.1016/j.ophtha.2013.08.011. [DOI] [PubMed] [Google Scholar]
- Wolowacz 2007 {published data only}.Wolowacz SE, Roskell N, Kelly S, Maciver FM, Brand CS. Cost effectiveness of pegaptanib for the treatment of age-related macular degeneration in the UK. Pharmacoeconomics. 2007;25(10):863–79. doi: 10.2165/00019053-200725100-00005. [DOI] [PubMed] [Google Scholar]
- Zehetner 2013 {published data only}.Zehetner C, Kirchmair R, Huber S, Kralinger MT, Kieselbach GF. Plasma levels of vascular endothelial growth factor before and after intravitreal injection of bevacizumab, ranibizumab and pegaptanib in patients with age-related macular degeneration, and in patients with diabetic macular oedema. British Journal of Ophthalmology. 2013;97(4):454–9. doi: 10.1136/bjophthalmol-2012-302451. [DOI] [PubMed] [Google Scholar]
References to studies awaiting assessment
- NCT00087763 {unpublished data only}. NCT00087763. [accessed 14 August 2013];A phase II prospective, randomized, double-masked, sham-controlled, dose-ranging, multicenter trial to assess the effect of pegaptanib sodium on foveal thickening in patients with exudative subfoveal age-related macular degeneration (AMD) clinicaltrials.gov/show/NCT00087763.
References to ongoing studies
- NCT00531336 {unpublished data only}. NCT00531336. Comparison of combined therapy of intravitreal injection of Avastin and Macugen versus monotherapy. [accessed 6 August 2013];The MAAM Study - a pilot study. clinicaltrials.gov/show/NCT00531336.
- NCT00559715 {unpublished data only}. NCT00559715. [accessed 14 August 2013];Prevention of vision loss in patients with age-related macular degeneration (AMD) by Intravitreal Injection of Bevacizumab and Ranibizumab (VIBERA) clinicaltrials.gov/show/NCT00559715.
- NCT01127360 {unpublished data only}. NCT01127360. Lucentis compared to Avastin study. [accessed 11 January 2013];A randomized, double blind, prospective multicenter study comparing the effect of intravitreal injection of Bevacizumab (Avastin) to Ranibizumab (Lucentis) when given to patients with exudative (wet) age-related macular degeneration. clinicaltrials.gov/show/NCT01127360.
- NCT01319188 {unpublished data only}. NCT01319188. [accessed 17 May 2013];Ranibizumab for age-related macular degeneration and the risk of arterial thromboembolic events (RATE) clinicaltrials.gov/show/NCT01319188.
- NCT02036723 {unpublished data only}. NCT02036723. [accessed 4 April 2014];Multicentre double blind randomized clinical study evaluating the efficacy and safety of BCD-021 (CJSC BIOCAD, Russia) and Lucentis® (Novartis Pharmaceuticals Canada Inc.) in patients with neovascular wet age-related macular degeneration. clinicaltrials.gov/show/NCT02036723.
- NTR1704 {unpublished data only}. [accessed 17 May 2013];Comparison of bevacizumab (Avastin) and ranibizumab (Lucentis) in exudative age-related macular degeneration. www.trialregister.nl/trialreg/admin/rctview.asp?TC=1704.
Additional references
- Aiello 1994.Aiello LP, Avery RL, Arrigg PG, Keyt BA, Jampel HD, Shah ST, et al. Vascular endothelial growth factor in ocular fluid of patients with diabetic retinopathy and other retinal disorders. New England Journal of Medicine. 1994;331(22):1480–7. doi: 10.1056/NEJM199412013312203. [DOI] [PubMed] [Google Scholar]
- AREDS 2001.Age-Related Eye Disease Study Research Group. A randomized, placebo-controlled, clinical trial of high-dose supplementation with vitamins C and E, beta carotene, and zinc for age-related macular degeneration and vision loss: AREDS report no. 8. Archives of Ophthalmology. 2001;119(10):1414–36. doi: 10.1001/archopht.119.10.1417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- AREDS2 2013.Age-Related Eye Disease Study 2 Research Group. Lutein + zeaxanthin and omega-3 fatty acids for age-related macular degeneration: the Age-Related Eye Disease Study 2 (AREDS2) randomized clinical trial. JAMA. 2013;309(19):2005–15. doi: 10.1001/jama.2013.4997. [DOI] [PubMed] [Google Scholar]
- Boekhoorn 2007.Boekhoorn SS, Vingerling JR, Witteman JCM, Hofman A, de Jong PT. C-reactive protein level and risk of aging macula disorder: The Rotterdam Study. Archives of Ophthalmology. 2007;125(10):1396–401. doi: 10.1001/archopht.125.10.1396. [DOI] [PubMed] [Google Scholar]
- Bourne 2014.Bourne RR, Jonas JB, Flaxman SR, Keeffe J, Leasher J, Naidoo K, et al. Prevalence and causes of vision loss in high-income countries and in Eastern and Central Europe: 1990–2010. British Journal of Ophthalmology. 2014;98(5):629–38. doi: 10.1136/bjophthalmol-2013-304033. [DOI] [PubMed] [Google Scholar]
- Brown 2008.Brown MM, Brown GC, Brown HC, Peet J. A value-based medicine analysis of ranibizumab for the treatment of subfoveal neovascular macular degeneration. Ophthalmology. 2008;115(6):1039–45. doi: 10.1016/j.ophtha.2007.08.033. [DOI] [PubMed] [Google Scholar]
- Bunce 2006.Bunce C, Wormald R. Leading causes of certification for blindness and partial sight in England & Wales. BMC Public Health. 2006;6:58. doi: 10.1186/1471-2458-6-58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carneiro 2012.Carneiro AM, Mendonca LS, Falcao MS, Fonseca SL, Brandao EM, Falcao-Reis FM. Comparative study of 1+PRN ranibizumab versus bevacizumab in the clinical setting. Clinical Ophthalmology. 2012;6:1149–57. doi: 10.2147/OPTH.S33017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CMS 2014.Centers for Medicare and Medicaid Services. [accessed 9 April 2014];Billing and coding information regarding uses, including off-label uses, of bevacizumab and ranibizumab, for the treatment of ophthalmological diseases. Document ID A49034. www.cms.gov/medicare-coverage-database.
- Cohen 2014.Cohen D. Roche and Novartis colluded over wet AMD drugs, says Italian regulator. BMJ. 2014;348:g2006. doi: 10.1136/bmj.g2006. [DOI] [PubMed] [Google Scholar]
- Congdon 2004.Congdon N, O’Colmain B, Klaver CC, Klein R, Muñoz B, Friedman DS, et al. Causes and prevalence of visual impairment among adults in the United States. Archives of Ophthalmology. 2004;122(4):477–85. doi: 10.1001/archopht.122.4.477. [DOI] [PubMed] [Google Scholar]
- de Juan 2013.de Juan E, Laganovska G, Loewenstein A, Alster Y, Erickson S. First in-human results of a refillable drug delivery implant providing sustained release of ranibizumab in patients with neovascular AMD. Macula Society. 2013:136–7. [Google Scholar]
- Deangelis 2007.Deangelis MM, Ji F, Kim IK, Adams S, Capone A, Jr, Ott J, et al. Cigarette smoking, CFH, APOE, ELOVL4, and risk of neovascular age-related macular degeneration. Archives of Ophthalmology. 2007;125(1):49–54. doi: 10.1001/archopht.125.1.49. [DOI] [PubMed] [Google Scholar]
- Deeks 2011.Deeks JJ, Higgins JPT, Altman DG, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0. The Cochrane Collaboration; 2011. Chapter 9: Analysing data and undertaking meta-analyses. (updated March 2011) Available from www.cochrane-handbook.org. [Google Scholar]
- EOP 1003.Eyetech Pharmaceuticals, Inc, Pfizer. Inc. Pegaptanib sodium injection in the treatment of neovascular age-related macular degeneration; and FDA. [accessed 20 December 2011];Macugen® (pegaptanib sodium injection) for the treatment of neovascular age-related macular degeneration. www.fda.gov/ohrms/dockets/ac/04/briefing/2004-4053b1.htm.
- EOP 1004.Eyetech Pharmaceuticals, Inc, Pfizer. Inc. Pegaptanib sodium injection in the treatment of neovascular age-related macular degeneration; and FDA. [accessed 20 December 2011];Macugen® (pegaptanib sodium injection) for the treatment of neovascular age-related macular degeneration. www.fda.gov/ohrms/dockets/ac/04/briefing/2004-4053b1.htm.
- Friedman 2004.Friedman DS, O’Colmain BJ, Muñoz B, Tomany SC, McCarty C, de Jong PT, et al. Prevalence of age-related macular degeneration in the United States. Archives of Ophthalmology. 2004;122(4):564–72. doi: 10.1001/archopht.122.4.564. [DOI] [PubMed] [Google Scholar]
- Ghafour 1983.Ghafour IM, Allan D, Foulds WS. Common causes of blindness and visual handicap in the west of Scotland. British Journal of Ophthalmology. 1983;67(4):209–13. doi: 10.1136/bjo.67.4.209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gillies 2014.Gillies MC, Walton RJ, Arnold JJ, McAllister IL, Simpson JM, Hunyor AP, et al. Comparison of outcomes from a phase 3 study of age-related macular degeneration with a matched, observational cohort. Ophthalmology. 2014;121(3):676–81. doi: 10.1016/j.ophtha.2013.09.050. [DOI] [PubMed] [Google Scholar]
- Glanville 2006.Glanville JM, Lefebvre C, Miles JN, Camosso-Stefinovic J. How to identify randomized controlled trials in MEDLINE: ten years on. Journal of the Medical Library Association. 2006;94(2):130–6. [PMC free article] [PubMed] [Google Scholar]
- Gragoudas 2004.Gragoudas ES, Adamis AP, Cunningham ET, Jr, Feinsod M, Guyer DR the VEGF Inhibition Study in Ocular Neovascularization Clinical Trial Group. Pegaptanib for neovascular age-related macular degeneration. New England Journal of Medicine. 2004;351(27):2805–16. doi: 10.1056/NEJMoa042760. [DOI] [PubMed] [Google Scholar]
- Haddad 2006.Haddad S, Chen CA, Santangelo SL, Seddon JM. The genetics of age-related macular degeneration: A review of progress to date. Survey of Ophthalmology. 2006;51(4):316–63. doi: 10.1016/j.survophthal.2006.05.001. [DOI] [PubMed] [Google Scholar]
- Higgins 2011.Higgins JPT, Altman DG, Sterne JAC, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0. The Cochrane Collaboration; 2011. Chapter 8: Assessing risk of bias in included studies. (updated March 2011) Available from www.cochrane-handbook.org. [Google Scholar]
- Holz 2013.Holz FG, Bandello F, Gillies M, Mitchell P, Osborne A, Sheidow T, et al. Safety of ranibizumab in routine clinical practice: 1-year retrospective pooled analysis of four European neovascular AMD registries within the LUMINOUS programme. British Journal of Ophthalmology. 2013;97(9):1161–7. doi: 10.1136/bjophthalmol-2013-303232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hyman 1987.Hyman L. Epidemiology of eye disease in the elderly. Eye. 1987;1(Pt 2):330–41. doi: 10.1038/eye.1987.53. [DOI] [PubMed] [Google Scholar]
- Ip 2008.Ip MS, Scott IU, Brown GC, Brown MM, Ho AC, Huang SS, et al. Anti-vascular endothelial growth factor pharmacotherapy for age-related macular degeneration: a report by the American Academy of Ophthalmology. Ophthalmology. 2008;115(10):1837–46. doi: 10.1016/j.ophtha.2008.08.012. [DOI] [PubMed] [Google Scholar]
- Klein 2008.Klein R, Knudtson MD, Cruickshanks KJ, Klein BE. Further observations on the association between smoking and the long-term incidence and progression of age-related macular degeneration. Archives of Ophthalmology. 2008;126(1):115–21. doi: 10.1001/archopht.126.1.115. [DOI] [PubMed] [Google Scholar]
- Kvanta 1996.Kvanta A, Algvere PV, Berglin L, Seregard S. Subfoveal fibrovascular membranes in age-related macular degeneration express vascular endothelial growth factor. Investigative Ophthalmology & Visual Science. 1996;37(9):1929–34. [PubMed] [Google Scholar]
- Leibowitz 1980.Leibowitz HM, Krueger DE, Maunder LR, Milton RC, Kini MM, Kahn HA, et al. The Framingham Eye Study monograph: An ophthalmological and epidemiological study of cataract, glaucoma, diabetic retinopathy, macular degeneration, and visual acuity in a general population of 2631 adults, 1973–1975. Survey of Ophthalmology. 1980;24(Suppl):335–610. [PubMed] [Google Scholar]
- Lopez 1996.Lopez PF, Sippy BD, Lambert HM, Thach AB, Hinton DR. Transdifferentiated retinal pigment epithelial cells are immunoreactive for vascular endothelial growth factor in surgically excised age-related macular degeneration-related choroidal neovascular membranes. Investigative Ophthalmology and Visual Science. 1996;37(5):855–68. [PubMed] [Google Scholar]
- Mitchell 2002.Mitchell P, Wang JJ, Smith W, Leeder SR. Smoking and the 5-year incidence of age-related maculopathy: the Blue Mountains Eye Study. Archives Ophthalmology. 2002;120(10):1357–63. doi: 10.1001/archopht.120.10.1357. [DOI] [PubMed] [Google Scholar]
- Mitchell 2011.Mitchell P. A systematic review of the efficacy and safety outcomes of anti-VEGF agents used for treating neovascular age-related macular degeneration: comparison of ranibizumab and bevacizumab. Current Medical Research and Opinion. 2011;27(7):1465–75. doi: 10.1185/03007995.2011.585394. [DOI] [PubMed] [Google Scholar]
- Moja 2014.Moja L, Lucenteforte E, Kwag KH, Bertele V, Campomori A, Chakravarthy U, et al. Systemic safety of bevacizumab versus ranibizumab for neovascular age-related macular degeneration. Cochrane Database of Systematic Reviews. 2014;(7) doi: 10.1002/14651858.CD011230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MPSG 1991.Macular Photocoagulation Study Group. Argon laser photocoagulation for neovascular maculopathy Five-year results from randomized clinical trials Macular Photocoagulation Study Group. Archives of Ophthalmology. 1991;109(8):1109–14. [PubMed] [Google Scholar]
- Owen 2003.Owen CG, Fletcher AE, Donoghue M, Rudnicka AR. How big is the burden of visual loss caused by age related macular degeneration in the United Kingdom? British Journal of Ophthalmology. 2003;87(3):312–7. doi: 10.1136/bjo.87.3.312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rasmussen 2014.Rasmussen A, Sander B. Long-term longitudinal study of patients treated with ranibizumab for neovascular age-related macular degeneration. Current Opinion in Ophthalmology. 2014;25(3):158–63. doi: 10.1097/ICU.0000000000000050. [DOI] [PubMed] [Google Scholar]
- RevMan 2012.Review Manager (RevMan) [Computer program]. Version 5.2. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration; 2012. [Google Scholar]
- Rofagha 2013.Rofagha S, Bhisitkul RB, Boyer DS, Sadda SR, Zhang K. Seven-year outcomes in ranibizumab-treated patients in ANCHOR, MARINA, and HORIZON: a multicenter cohort study (SEVEN-UP) Ophthalmology. 2013;120(11):2292–9. doi: 10.1016/j.ophtha.2013.03.046. [DOI] [PubMed] [Google Scholar]
- Schaumberg 2007.Schaumberg DA, Hankinson SE, Guo Q, Rimm E, Hunter DJ. A prospective study of 2 major age-related macular degeneration susceptibility alleles and interactions with modifiable risk factors. Archives of Ophthalmology. 2007;125(1):55–62. doi: 10.1001/archopht.125.1.55. [DOI] [PubMed] [Google Scholar]
- Schmucker 2010.Schmucker C, Ehlken C, Hansen LL, Antes G, Agostini HT, Lelgemann M. Intravitreal bevacizumab (Avastin) vs. ranibizumab (Lucentis) for the treatment of age-related macular degeneration: a systematic review. Current Opinion in Ophthalmology. 2010;21(3):218–26. doi: 10.1097/ICU.0b013e3283386783. [DOI] [PubMed] [Google Scholar]
- Schmucker 2012.Schmucker C, Ehlken C, Agostini HT, Antes G, Ruecker G, Lelgemann M, et al. A safety review and meta-analyses of bevacizumab and ranibizumab: off-label versus goldstandard. PloS One. 2012;7(8):e42701. doi: 10.1371/journal.pone.0042701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seddon 2006.Seddon JM, George S, Rosner B, Klein ML. CFH gene variant, Y402H, and smoking, body mass index, environmental associations with advanced age-related macular degeneration. Human Heredity. 2006;61(3):157–65. doi: 10.1159/000094141. [DOI] [PubMed] [Google Scholar]
- Smith 1996.Smith W, Mitchell P, Leeder SR. Smoking and age-related maculopathy. The Blue Mountains Eye Study. Archives of Ophthalmology. 1996;114(12):1518–23. doi: 10.1001/archopht.1996.01100140716016. [DOI] [PubMed] [Google Scholar]
- SST 20.Submacular Surgery Trials Research Group. Solomon SD, Jefferys JL, Hawkins BS, Bressler NM. Incident choroidal neovascularization in fellow eyes of patients with unilateral subfoveal choroidal neovascularization secondary to age-related macular degeneration: SST report No. 20 from the Submacular Surgery Trials Research Group. Archives of Ophthalmology. 2007;125(10):1323–30. doi: 10.1001/archopht.125.10.1323. [DOI] [PubMed] [Google Scholar]
- Stein 2014.Stein JD, Newman-Casey PA, Mrinalini T, Lee PP, Hutton DW. Cost-effectiveness of bevacizumab and ranibizumab for newly diagnosed neovascular macular degeneration. Ophthalmology. 2014;121(4):936–45. doi: 10.1016/j.ophtha.2013.10.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tielsch 1994.Tielsch JA. Prevent Blindness. Illinois: Schaumberg; 1994. Vision problems in the US: a report on blindness and vision impairment in adults age 40 and older. [Google Scholar]
- Ting 2002.Ting TD, Oh M, Cox TA, Meyer CH, Toth CA. Decreased visual acuity associated with cystoid macular edema in neovascular age-related macular degeneration. Archives of Ophthalmology. 2002;120(6):731–7. doi: 10.1001/archopht.120.6.731. [DOI] [PubMed] [Google Scholar]
- Van Kerckhoven 2001.Van Kerckhoven W, Lafaut B, Follens I, De Laey JJ. Features of age-related macular degeneration on optical coherence tomography. Bulletin de la Societe Belge d’ Ophtalmologie. 2001;281:75–84. [PubMed] [Google Scholar]
- Virgili 2007.Virgili G, Bini A. Laser photocoagulation for neovascular age-related macular degeneration. Cochrane Database of Systematic Reviews. 2007;(3) doi: 10.1002/14651858.CD004763.pub2. [DOI] [PubMed] [Google Scholar]
- Wormald 2007.Wormald R, Evans J, Smeeth L, Henshaw K. Photodynamic therapy for neovascular age-related macular degeneration. Cochrane Database of Systematic Reviews. 2007;(3) doi: 10.1002/14651858.CD002030.pub2. [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
- Krzystolik 2005.Krzystolik MG, Woodcome HA, Reddy U. Antiangiogenic therapy with anti-vascular endothelial growth factor modalities for neovascular age-related macular degeneration. Cochrane Database of Systematic Reviews. 2005;(1) doi: 10.1002/14651858.CD005139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vedula 2008.Vedula SS, Krzystolik M. Antiangiogenic therapy with anti-vascular endothelial growth factor modalities for neovascular age-related macular degeneration. Cochrane Database of Systematic Reviews. 2008;(2) doi: 10.1002/14651858.CD005139.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]