Abstract
Background
The surgical population is aging, and greater numbers of surgical patients are being discharged to skilled nursing facilities. Post-acute care is a poorly understood but very important aspect of our healthcare system.
Methods
This systematic review examines the current body of literature surrounding the structural, process of care, and outcomes measurements for patients in skilled nursing facilities. English language articles published between 1998 and 2011 that purposed to examine nursing facility structure, process of care, and/or outcomes were included.
Results & Conclusions
Abstracts (2129) were screened and 102 articles were reviewed in full. Twenty-nine articles were included in the qualitative synthesis. The role of the care setting and care delivery in contributing to outcomes has not been well studied, and no strong conclusions can be made. This area of care currently represents a “black box” to practicing surgeons. An understanding of these factors maybe instrumental to determining future directions for research to maximize positive outcomes for these patients.
1. Background
Surgical interventions and care often reflect an acute insult and recovery phase. The post-acute phase of care and recovery is increasingly being provided in settings other than hospitals. Increasingly, patients are being discharged to dedicated rehabilitation facilities and skilled nursing facilities (SNFs) for post-acute care (PAC), rehabilitation, and recovery. This need for PAC is growing as the population ages. The factors associated with increased risk of institutional discharge are advanced age, prior placement in a nursing home, functional dependence with three or more activities of daily living (ADLs), significant extremity injury, maximum head abbreviated severity scale score ≥3, and lack of family or social support [1-4]. The total spending on SNF care was $150–160 billion in 2007, and 53%–60% of this care is paid for by public tax-payer funded sources (primarily Medicare and Medicaid) [5]. Adding to the cost, nearly one-quarter of PAC admissions to SNFs result in unplanned 30-d hospital readmissions [6-8].
PAC is a poorly understood but important aspect of our healthcare system. There is increasing evidence that the burden of disease related to acute surgical care extends well into the post-acute period. Many surgeons think of PAC as a transitional phase before returning home, but the increased mortality during this period challenges this assertion. Twenty-three percent of postoperative deaths occur after discharge [9], 59.3%–74.4% of deaths after traumatic injury occur after discharge [10,11], and 85.7% of elderly trauma patient deaths occur after leaving the hospital [12]. Population and hospital-based cohort studies have consistently demonstrated worse survival for intensive care unit, surgical, and trauma patients discharged to SNFs: risk of death is 1.6–3.9 times greater for patients discharged to SNF compared with those discharged home [10,11,13-18].
A greater burden of disease and injury severity contributes to the increased mortality of SNF patients; however, it is unclear if these baseline differences in the population discharged to SNF and the population discharged home completely explain the discrepancy. The role of the care setting in contributing to patient outcome and survival has not been well studied. This area of care currently represents something of a “black box”, and as researchers we lack a full understanding of exactly what PAC in an SNF looks like for our patients. Without this knowledge, we cannot appreciate fully how this period of PAC contributes to outcomes.
1.1. How quality is measured?
The classic Donabedian paradigm for assessing quality is a widely accepted conceptual framework for outcomes research, and consists of three core elements: structure, process, and outcome [19]. Although patient factors were not explicitly included in this paradigm, their inclusion in the overall measure of quality was implicit. Patient conditions are part of the antecedent conditions before delivery of care, similar to the structural components explored by the Donabedian construct. For the purposes of this health system evaluation, patient factors (demographics, disease and/or diagnosis, comorbidities, and so forth) will be considered as a separate core element but closely tied to structural components (SNF size and volume, staffing patterns, hospital affiliation, business model, availability of specific care, and so forth). The process is the actual care delivered to a patient (assistance with ADLs, physical therapy, medication monitoring and adjustment, counseling, and so forth.) and the outcome is the end result (mortality, readmission rates, changes in functional status, cost, and so forth).
This systematic review is intended to evaluate the literature with regard to the structure, process, and outcome of PAC in SNFs. Much of the information we have about PAC comes from the Minimum Data Set Resident Assessment Instrument (MDS, MDS-RAI), one available resource with information related to each of these three elements, and it has been used extensively in research and by many of the articles reviewed in the following. The MDS is part of the federally mandated process for assessment of all residents in Medicare or Medicaid certified SNFs. Since 1990, use of the MDS-RAI has been mandated in all SNFs and long-term care (LTC) facilities that receive Medicare or Medicaid reimbursement and transmission of data to the centers for Medicare and Medicaid has been mandated since 1998 [20]. The MDS contains ~400 data items and is intended to be a comprehensive assessment of each SNF resident’s demographic information, baseline functional capabilities, delivered care, and progress during the stay. MDS assessment forms must be completed for all residents in Medicare/Medicaid certified SNFs, regardless of reimbursement source. These assessments are typically performed by licensed health-care providers at the facility, and are required on admission to the facility, after any clinically significant patient event, quarterly throughout the year, and on discharge.
Specific items from the MDS have been used to develop quality indicators (QIs) across multiple domains of resident care. This information is not publically available at a localor facility-specific level.
2. Methods
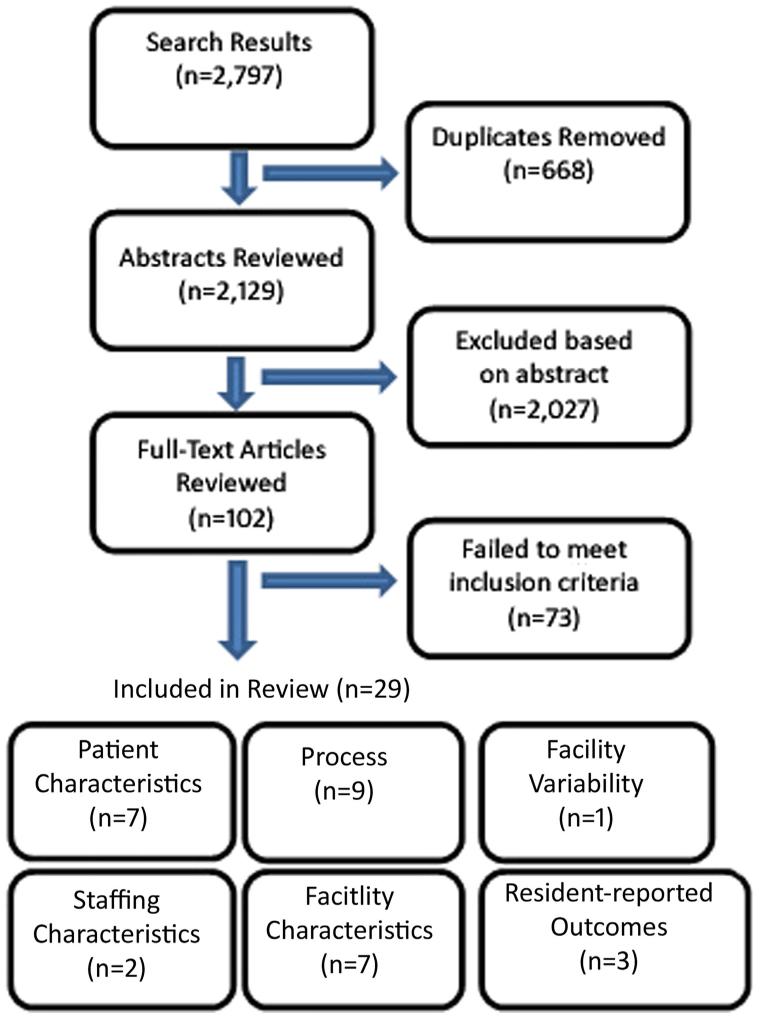
A comprehensive and systematic review of the literature was undertaken using PubMed. A medical librarian assisted in the construction and execution of the database searches. Specific terms searched can be found in Table 1. General inclusion criteria were as follows: English language full-text articles published between January 1998 and December 2011, publications reporting work with the clearly stated purpose of addressing elements of at least one of the three domains, and based on studies completed in the United States or Canada. Published work addressing any of these issues as a secondary aspect of work, but not as the primary objective, were excluded, as were studies addressing these questions in the setting of a specific non-surgical disease process or in patients identified as having a terminal illness. Additional inclusion and/or exclusion criteria specific for each sub-domain, when necessary, were as follows. For research, investigating the association between patient factors and outcomes, studies reporting models based solely on the use of other developed scores or indices were excluded. Investigations into the association between facility staffing characteristics and out-comes were limited to reports of work in the PAC population. Investigations addressing variability in outcomes were limited to studies attempting to make direct facility-level comparisons. Searches were conducted between 26 January 2012 and 25 February 2012. This initial search yielded 2797 entries (Figure). After removing duplicate results, 2129 titles and abstracts were screened and 101 articles were retrieved and reviewed in full independently by two authors (T.W.H. and P.A.-C.). The reviewing authors had no previous ties before agreeing to work on this review as part of a shared interest in long-term outcomes for surgical patients. The final list of articles was based on mutual agreement; there were no significant disagreements regarding specific articles to include. Reference lists from these articles were also reviewed for additional articles. Review of the reference lists identified two additional articles, of which one met inclusion criteria. Twenty-nine relevant studies are discussed in this review and characteristics of these studies can be found in Table 2. Because the subject matter of this review is purposefully broad, there was no specific tool or protocol used to abstract data and there was no attempt at quantitative synthesis. Risk of bias for individual studies included was assessed through collaborative discussion between authors and where applicable is mentioned in the text.
Table 1. Search terms.
| Search term | Results |
|---|---|
| “MDS” and (“outcome” or “mortality” or “readmission” or “death”) |
340 |
| (“Nursing home” or “SNF”) and (“volume” or “volume outcomes” or “volume-outcomes” or “characteristics” or “staffing”) and (“outcome” or “mortality” or “readmission” or “quality of care”) |
662 |
| (“Nursing home” or “SNF”) and (“care process” or “intervention” or “process assessment”) and (“outcome” or “mortality” or “readmission” or “quality of care”) |
619 |
| (“Nursing home” or “SNF”) and (“outcomes assessment” or “outcomes” or “quality” or “quality of care” or “quality of health care” or “quality- indicators”) and (“variability” or “facility-level” or “facility-level”) |
193 |
| (“Nursing home” or “SNF”) and (“resident-reported outcomes” or “resident-reported outcomes” or “patient-reported outcomes” or “patient-reported outcomes” or “quality of life”) and (“outcome” or “mortality” or “readmission” or “quality of care” or “quality”) |
983 |
Figure – Publication selection process. (For interpretation of the references to color in this figure, the reader is referred to the web version of this article.)
Table 2. Characteristics of studies.
| Author | Year | Study size | Study design | Outcomes assessed |
|---|---|---|---|---|
| Structure | ||||
| Patient characteristics | ||||
| Hirdes et al. | 2003 | 28,495 | Retrospective cohort | Mortality |
| Flacker and Kiely | 2003 | 136,794 | Retrospective cohort | Mortality |
| Porock et al. | 2005 | 43,510 | Retrospective cohort | Mortality |
| Porock et al. | 2010 | 43,510 | Retrospective cohort | Mortality |
| Van Dijk et al. | 2005 | 43,510 | Retrospective cohort | Mortality |
| Wallace and Prevost | 2006 | 21,852 | Retrospective cohort | Mortality |
| Lee and Rantz | 2008 | 38,591 | Retrospective cohort | Physical function |
| Facility staffing | ||||
| Decker | 2008 | 6623 | Retrospective cohort | Discharge outcome, mortality |
| Decker | 2008 | 4086 | Retrospective cohort | Discharge outcome, LOS, and mortality |
| Facility characteristics | ||||
| Li et al. | 2011 | 9336* | Retrospective cohort | Rehospitalization |
| Harrington et al. | 2002 | 13,953* | Retrospective cohort | Deficiency citations |
| Zimmerman et al. | 2002 | 2315 | Retrospective cohort | Infection, hospitalization |
| Flynn et al. | 2010 | 63* | Retrospective cohort | Pressure ulcers, deficiency citations |
| Intrator et al. | 2004 | 54,631 | Retrospective cohort | Preventable readmission |
| Jette et al. | 2005 | 4988 | Retrospective cohort | LOS, functional, and mental status |
| Horn et al. | 2010 | 147* | Retrospective cohort | High-risk pressure ulcer, incontinence, and declining ADLs |
| Process | ||||
| Berkowitz et al. | 2011 | 1* | Pre/post observational cohort |
Discharge disposition, mortality |
| Hill Westmoreland and Gruber- Baldini |
2005 | 462 | Retrospective cohort | Falls |
| Simmons et al. | 2003 | 400 | Cross-sectional cohort | Weight loss and related care |
| Schnelle et al. | 2003 | 779 | Cross-sectional cohort | Urinary incontinence and related care |
| Stevenson et al. | 2004 | 6947 | Cross-sectional cohort | Urinary tract infection |
| Schnelle et al. | 2004 | 413 | Cross-sectional cohort | Restraint use |
| Schnelle et al. | 2001 | 109 | Cross-sectional cohort | Depression |
| Simmons et al. | 2004 | 396 | Cross-sectional cohort | Depression related care |
| Bates-Jensen et al. | 2003 | 329 | Cross-sectional cohort | Pressure ulcers and related care |
| Outcomes | ||||
| Facility variability | ||||
| Porell and Caro | 1998 | 550* | Longitudinal cohort | Mortality, ADLs, incontinence, cognitive status, pressure ulcers, accidents, restraint use, contractures, and weight change |
| Resident-reported outcomes | ||||
| Hodlewsky and Decker | 2002 | 265 | Randomized contolled trial | Reliability of resident satisfaction surveys |
| Kane et al. | 2004 | 40* | Mixed-method | Quality of life scores |
Facility count.
3. Results
There was very little published information specifically addressing surgical or trauma patients discharged to SNFs. Most of the SNFs provide care for both PAC and long-stay residents within the same facility, inclusive of surgical and trauma patients. However, there is still much to be learned from these population-based studies.
3.1. Patient characteristics influencing outcomes
Six studies reported the development or validation of a model predicting mortality among SNF residents, and one study sought to identify factors predictive for changes in functional status (Table 3) [21-27]. One study reexamined and modified a predictive model previously developed by the same researchers. The most widely used models are the MDS-changes in health, end-stage disease, and symptoms and signs and the Minimum Data Set Mortality Risk Index (MMRI) [21,22]. The final MDS-changes in health, end-stage disease, and symptoms and signs assesses health instability using information found in the MDS on clinical signs and symptoms, deterioration in status, and chronic diseases. The MDS-MMRI predicts 6-mo mortality using 14 different variables and two interactions spanning demographic, disease process, clinical signs and symptoms, and adverse events. The MDS-MMRI was subsequently revised, removing complex calculations, to allow it to be more easily incorporated into clinical decision-making.
Table 3. Comparison of models predicting outcome based on patient factors.
| Authors | Tool | Outcome | Variables included in model |
|---|---|---|---|
| Hirdes et al. | MDS-CHESS | Mortality | Vomiting, dehydration, leaving food uneaten, shortness of breath, decline in cognitive or ADLs status, and end-stage disease |
| Flacker and Kiely | MRIS | Mortality | Cancer, shortness of breath, CHF, bedfast status, male sex, unstable condition, >25% food uneaten, low functional ability score, swallowing problem, bowel incontinence, BMI <23 |
| Porock et al. | MDS-MRI | Mortality | Cancer, sex, recent admission, shortness of breath, appetite, CHF, weight loss, renal failure, dehydration, age, cognitive deterioration, ADLs status, interactions between cancer and age and between ADL and cognitive deterioration |
| Van Dijk et al. | No model name | Mortality | Cancer, dementia, heart failure, renal failure, emphysema/COPD, diabetes mellitus, anemia, and interactions between age and cancer |
| Wallace and Prevost | SDI and PDS | Mortality | Poor cognitive status, poor functional status, bedfast, weight loss, fall, bowel incontinence, indwelling catheter, unstable diagnosis, high-stage pressure ulcers, terminal illness, and overall decline in status |
| Lee and Rantz | No model name | Functional status | Admission physical function, pressure ulcers, and urinary incontinence |
CHESS = changes in health, end-stage disease, and symptoms and signs; CHF = congestive heart failure; COPD = chronic obstructive pulmonary disease; BMI = body mass index; SDI = summative death index; PDS = probability of death score; MDS-MRI = minimum data set-modified mortality risk index; MRIS = mortality risk index score.
The 28 MDS 2.0 items used have been categorized for ease of comparison with other studies.
Comparison of these studies shows significant areas of overlap in predictors of mortality. Patient factors identified most frequently were cancer, congestive heart failure, declines in cognitive, functional or ADLs status, poor nutritional status, dehydration, and the presence of renal failure. Many of these are modifiable, and optimized treatment of these conditions is of paramount importance as these diagnoses increase both the risk of discharge to an institutional care facility as well as the risk of mortality as shown here. The findings also reinforce the importance of carefully assessing a patient’s nutritional status before elective surgery.
3.2. Structure
3.2.1. Infrastructure characteristics influencing outcomes
Studies examining infrastructural characteristics of SNF care that correlated with outcome measures fell into two broad categories: those that examined the role of nurse staffing and those that examined other aspects with or without investigating staffing levels. Studies investigating outcome associations with nurse staffing levels have had mixed results, but most of the studies have supported the positive association between increased nurse staffing and improved outcomes [28-32]. Additionally, multiple studies have investigated the relationship between staffing levels and quality of care. Among all nursing facility patients, multiple studies have demonstrated that increased registered nurse (RN) staffing, RN time spent on patient care tasks, and decreased RN turn-over are associated with improved outcomes as measured by the MDS QIs for pressure ulcers, urinary catheter use, physical restraint use, pain management as well as other measures including resident cognitive function, deterioration in ADLs self-performance, and number of hospitalizations [33-35].
Only recently has literature emerged examining the relationship between staffing and outcomes for short-stay residents admitted for PAC. In 2008, Decker [36] investigated the relationship between nursing staffing levels and discharge outcomes for residents admitted from hospitals versus those not admitted from hospitals. After controlling for patient demographics, clinical, and facility characteristics, greater RN staffing measured by hours of RN time per facility bed was positively associated with more stabilized and/or recovered discharges for residents admitted from hospitals, as well as for residents not admitted from the hospital whose stay was ≤30 d. They found no association for long-stay residents not admitted from a hospital.
In a follow-up study, Decker [37] further explored the relationship between staffing and readmission by delineating the role of nurse assistants, RNs, and physical therapists (PTs). After controlling for patient demographics, primary and secondary diagnoses, and other facility characteristics, regression analysis identified significant relationships between higher RN staffing levels and decreased length of stay (LOS) and decreased hospitalizations. Higher PT staffing levels were associated with increased rehabilitated and/or recovered outcomes at discharge, decreased LOS, and decreased deaths. Based on this limited literature, increased staffing levels may be associated with positive outcomes for short-stay patients in nursing homes.
The literature examining facility characteristics other than nurse staffing is more varied, and we identified studies examining characteristics including volume of PAC, intensity of therapy, non-nurse staffing levels, facility size, setting, business model (for-profit versus not-for-profit), hospital affiliation, and whether facilities were independent or part of a regional or national chain of facilities.
In 2011, Li et al. [38] reported that SNFs in the upper tertile for number of PAC admissions (>108 PAC admission) had 15% and 25% lower 30- and 90-d rehospitalization rates, respectively, compared with facilities in the lower tertile (<45 PAC admissions) after controlling for important patient-, clinical-, and facility-level covariates. This study suggests that positive volume–outcome relationships may exist for PAC, similar to that demonstrated for complex surgical procedures.
Harrington et al. [39] investigated the relationship between deficiency citations and ownership of nursing facilities and found that investor-owned nursing facilities had more deficiencies overall and in each category than non-profit facilities. They also noted that investor-owned facilities had lower staffing levels, but they did not explore for interaction or confounding between these two. Thus, the deficiencies seen could represent mixed-effects of ownership and staffing, or simply represent decreased quality associated with lower staffing.
Zimmerman et al. [40] reported that increased RN turnover rates were associated with both increased infection and hospitalization. Higher levels of licensed practical nurse staffing, higher intensity of care, and interestingly, higher levels of physical therapist and/or occupational therapist staffing were also associated with higher rates of infection. The data did not include resident-level information regarding the amount of physical therapy or occupational therapy provided, so it is unclear what this association represents. Facilities with a more debilitated resident population would be at a higher risk for infections while also requiring greater physical therapy or occupational therapy staffing to provide appropriate rehabilitative care for these residents. The researchers also reported higher rates of hospitalization for infection associated with for-profit facilities and facilities affiliated with a national or regional chain.
In 2004, Intrator et al. [41] reported that facilities employing nurse practitioners or physician assistants had lower rates of rehospitalization for Ambulatory Care Sensitive (ACS) diagnoses as defined by Culler et al. [42], but not for non-ACS diagnoses. They also reported higher rehospitalization rates for both ACS and non-ACS diagnoses at facilities with a for-profit business structure.
In 2005, Jette et al. [43] reported that increased physical, occupational, and/or speech therapy intensity was significantly associated with decreased LOS and improvements in the ADLs and executive control domains of the Functional Independence Measure. Although the researchers used comorbidities in their adjustment, they did not comment on whether there was an association between comorbidities and therapy intensity. It could be that the relationship observed between therapy intensity was confounded by the ability of patients with a decreased burden of disease to both participate in more therapy and be predisposed to shorter LOS.
Horn et al. [44] examined the relationship between resident and facility characteristics and facility performance on three quality measures (QMs) as follows: high-risk pressure ulcers (HRPU), low-risk incontinence (LRI), and decline in ADLs function. Several resident characteristics were associated with facility performance on these QMs. Higher rates of readmission which could be indicative of facility population or facility referral patterns were associated with better performance on the LRI QM. This association could have been because the resident was coded as short-stay on readmission, or because on readmission the resident was considered “high-risk” for incontinence. Bladder incontinence on admission was also associated with worse performance on the LRI metric. Similarly, higher rates of pressure ulcers on admission were associated with worse performance on the HRPU QM. The LRI and HRPU metrics are not currently risk adjusted for admission prevalence of bladder incontinence or pressure ulcers, respectively. The researchers also reported that state location was associated with decline in ADLs function. Specifically, states that used a case-mix adjustment to determine payment showed higher rates of declining ADLs function. The researchers concluded that the centers for Medicare and Medicaid risk-adjustment for these publicly reportable QMs should be altered to potentially include these resident and facility characteristics. They contend that this would allow for more accurate comparison of facilities based on the reported QMs.
This literature suggests that several facility-level factors including volume of PAC, ownership, staffing turnover, and staff makeup may contribute to patient outcomes. However, given the very small and heterogeneous nature of this literature, we feel no strong generalizable conclusions can be made yet.
3.3. Process
In 2011, Berkowitz et al. [45] published the results of a 6-mo pilot program to improve the discharge disposition of patients admitted to a single PAC SNF unit. Disposition was defined as discharge to community, transition to LTC, death, or rehospitalization. Specific care processes were implemented to improve disposition. Resident admission procedures were standardized, including aspects such as medication reconciliation, standard treatment protocols for common conditions, standardized goals of care discussion, and assessment of resident hospitalizations in the prior 6 mo. An automatic palliative care consult was performed for residents with greater than three admissions in that time frame. Multi-disciplinary root-cause analysis of acute readmissions was used to identify problems and assess the processes of care. They compared the results during the experimental period with a historical cohort from the same unit. At the end of the trial period, they reported a 20% decrease in acute readmissions, a 6% increase in discharges to the community, decreased transfers to LTC, and increased use of palliative services among those who died in the facility.
Several investigators have assessed the reliability, validity, and use of the MDS QIs as markers for specific processes of care. Hutchinson et al. [46] completed a systematic review of this topic in 2010. They assessed the literature regarding the reliability and validity of the MDS QIs in measuring specific process measures and their relationship to outcomes. However, several of the studies assessed not only the QI itself but whether specific processes of care indicative of high-quality care were present and/or different between SNFs reporting different QI scores [47-54]. Our review of the literature did not identify additional studies (not covered in the previous systematic review) and we will briefly summarize the findings.
The MDS QI items for falls was found to significantly underestimate the incidence of falls when compared with the medical record, and caution should be used when interpreting the MDS QI for falls [47]. The MDS QI for weight loss was found to discriminate facilities based on prevalence of weight loss, and did have some concordance with care processes including verbal prompting, social interaction, and assistance around meal times [48]. Facilities in the highest quartile (worst performing) had a population at greater risk for weight loss. The MDS QI for urinary incontinence did not discriminate facilities that provided additional assistance to prevent incontinence and was not associated with difference in care [49]. The MDS QI measure for urinary tract infections (UTI) was found to grossly overestimate the true incidence of UTI when compared with medical records [50]. The MDS QI for depression was found to be a more accurate measure for the ability of staff to identify depressive symptoms than for the incidence of depression, and was not correlated with the delivery of depression specific care processes [51,52]. The MDS QI for pressure ulcers did not reflect differences in care processes or quality of pressure-ulcer specific care, and likely represented differences in the accuracy of reporting and/or higher baseline prevalence of ulcers among facilities in the highest (lowest-performing) quartile [53]. The MDS QI for restraint use, which is intended to measure restraint use while out of bed, was found to accurately but inappropriately reflect restraint use while in bed [54].
Berkowitz et al. demonstrated that improved communication surrounding transition of care from the acute-care hospital setting to the nursing facility and standardized admission policies led to decreased rehospitalizations. Otherwise, there is very little strong data exploring the process of care within SNFs, and it is apparent to us from the current literature that the MDS QI metrics cannot confidently be used to assess quality of care within SNFs.
3.4. Outcomes
3.4.1. Assessment of facility-specific outcomes
In 1998, Porell and Caro compared individual facility outcomes using four health-based outcomes and five QIs at 550 nursing facilities in Massachusetts [55]. They found that after adjusting for case-mix, inter-facility and intra-facility quality varied widely, and that good performance at one time point was only modestly predictive of good performance at a future time point. They concluded that focus on specific measures of quality may be misleading because strong performance on one often coexisted with poor performance on another.
This work dovetails temporally with the development of the MDS QIs and the establishment of the Nursing Home Compare (NHC) program. The quality of specific SNFs receiving reimbursement through the centers for Medicare and Medicaid is reported through the NHC program, which began reporting deficiency citations in 1998 (www.medicare.gov/nhcompare). This system now scores individual nursing homes on the basis of three aspects: staffing levels, health inspections, and self-reported quality metrics based on 21 MDS indicators. In each aspect, facilities in the top 10% receive five stars, the bottom 20% receive one star, and the remaining 70% are scored with 23.67% each getting two, three, or four stars. Several of the studies from the previous section independently assessed the incidence or prevalence of outcomes such as UTIs and pressure ulcers as part of their investigation of the related MDS QI metrics, and most found that the information from independent assessment and/or medical chart review were discordant from the associated MDS QI metric. However, outside of the NHC rating, which does not provide information on the individual QI metrics, there are no publicly available performance data for the MDS QIs. To our knowledge, there is no available method to compare facility-specific performance on many outcome measures such as mortality, discharge disposition, or complication rates at nursing homes. Thus, the current literature only suggests significant inter-facility variability but does not provide tools to assess facility-specific outcomes.
3.4.2. Resident-reported outcomes
Work to identify and measure outcomes as reported by the nursing home resident has been ongoing since the 1986 Institute of Medicine report instructing the development and use of resident-reported outcomes. However, very little work exists correlating these outcomes with quality of care or other clinical outcomes. One study demonstrated significant bias in resident satisfaction surveys, casting significant doubt on the ubiquitous use of satisfaction surveys to assess and compare SNFs [56]. Structured resident interviews can be used to create aggregate facility-level quality of life scores and reliably differentiate facilities, and although these have not been correlated with other meaningful outcomes, the validity of resident self-reported quality of life in differentiating facilities makes it an attractive metric for future research exploring the relationship between care quality and resident-reported out-comes [57].
4. Conclusions
Assessments of quality in SNFs, especially related to surgical and trauma, are quite limited. The current body of literature does not allow us to make any strong conclusions regarding the relationships between the Donabedian constructs of structure, process, and outcome for PAC in nursing facilities. Further work to evaluate the relationship between structure, process, and outcome in SNFs is critical to performance improvement, and should be a focus of ongoing research evaluations by surgical researchers because the long-term success of surgical care in this population may be significantly influenced by the quality of PAC. The data has demonstrated that multiple patient factors contribute to long-term mortality among patients in SNFs, but the work exploring the relationship between facility characteristics and outcomes has been limited primarily to readmissions. Although we believe the MDS captures a wealth of data pertinent to the structure, process, and outcomes of PAC, the implementation of the current QIs is too limited in the ability to measure quality of care within individual SNFs. Further work is warranted to measure quality and outcomes and to allow site-to-site evaluation based on accurate, risk-adjusted comparisons of patient populations to turn the current “black box” into a glass house. As more patients are discharged to SNFs for PAC, a better understanding of the out-comes and determinants of outcomes at patient and facility levels is vital to the development of a learning healthcare system that improves results for patients discharged to SNFs.
Acknowledgment
This work was supported by National Institutes of Health training grant 1T32DK070555-01A1 and by the Washington State’s Life Science Discovery Fund and Agency for Healthcare Research and Quality Grant Number 1 R01 HS 20025-01 through the Surgical Care and Outcomes Assessment Program (SCOAP) and the Comparative Effectiveness Research Translation Network (CERTAIN).
Footnotes
Disclosure
The authors reported no proprietary or commercial interest in any product mentioned or concept discussed in the article.
Authors’ contributions: T.W.H., R.A., S.A., and D.R.F. contributed to the conception and design. T.W.H. and P.A.-C. did the data acquisition. T.W.H., P.A.-C., R.A., S.A., and D.R.F. did the analysis. T.W.H. did the first draft. T.W.H., P.A.-C., R.A., S.A., and D.R.F. did the critical revisions of the article.
None of the authors have any financial or personal conflicts of interests pertaining to this work.
references
- [1].Cuthbert JP, Corrigan JD, Harrison-Felix C, et al. Factors that predict acute hospitalization discharge disposition for adults with moderate to severe traumatic brain injury. Arch Phys Med Rehabil. 2011;92:721. doi: 10.1016/j.apmr.2010.12.023. [DOI] [PubMed] [Google Scholar]
- [2].Hagino T, Ochiai S, Sato E, Watanabe Y, Senga S, Haro H. Prognostic prediction in patients with hip fracture: risk factors predicting difficulties with discharge to own home. J Orthop Traumatol. 2011;12:77. doi: 10.1007/s10195-011-0138-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Lim HJ, Hoffmann R, Brasel K. Factors influencing discharge location after hospitalization resulting from a traumatic fall among older persons. J Trauma. 2007;63:902. doi: 10.1097/01.ta.0000240110.14909.71. [DOI] [PubMed] [Google Scholar]
- [4].Cram P, Lu X, Kaboli PJ, Vaughan-Sarrazin MS, Wolf BR. Clinical characteristics and outcomes of Medicare patients undergoing total hip arthroplasty, 1991-2008. JAMA. 2011;305:1560. doi: 10.1001/jama.2011.478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Medicare Payment Policy. 2010. [Google Scholar]
- [6].Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med. 2009;360:1418. doi: 10.1056/NEJMsa0803563. [DOI] [PubMed] [Google Scholar]
- [7].Mor Vincent P, Intrator Orna P, Zhanlian Feng P, David Grabowski P. The revolving door of rehospitalization from skilled nursing facilities. Health Aff. 2011;29:57. doi: 10.1377/hlthaff.2009.0629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Ouslander JG, Perloe M, Givens JH, Kluge L, Rutland T, Lamb G. Reducing potentially avoidable hospitalizations of nursing home residents: results of a pilot quality improvement project. J Am Med Directors Assoc. 2009;10:644. doi: 10.1016/j.jamda.2009.07.001. [DOI] [PubMed] [Google Scholar]
- [9].Yu P, Chang DC, Osen HB, Talamini MA. NSQIP reveals significant incidence of death following discharge. J Surg Res. 2011;170:e217. doi: 10.1016/j.jss.2011.05.040. [DOI] [PubMed] [Google Scholar]
- [10].Claridge JA, Leukhardt WH, Golob JF, McCoy AM, Malangoni MA. Moving beyond traditional measurement of mortality after injury: evaluation of risks for late death. J Am Coll Surg. 2010;210:788. doi: 10.1016/j.jamcollsurg.2009.12.035. [DOI] [PubMed] [Google Scholar]
- [11].Davidson GH, Hamlat CA, Rivara FP, Koepsell TD, Jurkovich GJ, Arbabi S. Long-term survival of adult trauma patients. JAMA. 2011;305:1001. doi: 10.1001/jama.2011.259. [DOI] [PubMed] [Google Scholar]
- [12].Fleischman RJ, Adams AL, Hedges JR, Ma OJ, Mullins RJ, Newgard CD. The optimum follow-up period for assessing mortality outcomes in injured older adults. J Am Geriatr Soc. 2010;58:1843. doi: 10.1111/j.1532-5415.2010.03065.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Legner VJ, Massarweh NN, Symons RG, McCormick WC, Flum DR. The significance of discharge to skilled care after abdominopelvic surgery in older adults. Ann Surg. 2009;249:250. doi: 10.1097/SLA.0b013e318195e12f. [DOI] [PubMed] [Google Scholar]
- [14].Colantonio A, Escobar MD, Chipman M, et al. Predictors of post-acute mortality following traumatic brain injury in a seriously injured population. J Trauma. 2008;64:876. doi: 10.1097/TA.0b013e31804d493e. [DOI] [PubMed] [Google Scholar]
- [15].Wunsch H, Guerra C, Barnato AE, Angus DC, Li G, Linde-Zwirble WT. Three-year outcomes for Medicare beneficiaries who survive intensive care. JAMA. 2010;303:849. doi: 10.1001/jama.2010.216. [DOI] [PubMed] [Google Scholar]
- [16].Cook CH, Martin LC, Howard B, Flancbaum LJ. Survival of critically ill surgical patients discharged to extended care facilities. J Am Coll Surg. 1999;189:437. doi: 10.1016/s1072-7515(99)00191-x. [DOI] [PubMed] [Google Scholar]
- [17].Ventura T, Harrison-Felix C, Carlson N, et al. Mortality after discharge from acute care hospitalization with traumatic brain injury: a population-based study. Arch Phys Med Rehabil. 2010;91:20. doi: 10.1016/j.apmr.2009.08.151. [DOI] [PubMed] [Google Scholar]
- [18].Aitken LM, Burmeister E, Lang J, Chaboyer W, Richmond TS. Characteristics and outcomes of injured older adults after hospital admission. J Am Geriatr Soc. 2010;58:442. doi: 10.1111/j.1532-5415.2010.02728.x. [DOI] [PubMed] [Google Scholar]
- [19].Donabedian A. The quality of medical care methods for assessing and monitoring the quality of. Science. 1978;200:856. doi: 10.1126/science.417400. [DOI] [PubMed] [Google Scholar]
- [20].Disposition of MDS 2.0. 2008. [Google Scholar]
- [21].Hirdes JP, Frijters DH, Teare GF. The MDS-CHESS scale: a new measure to predict mortality in institutionalized older people. J Am Geriatr Soc. 2003;51:96. doi: 10.1034/j.1601-5215.2002.51017.x. [DOI] [PubMed] [Google Scholar]
- [22].Porock D, Oliver DP, Zweig S, et al. Predicting death in the nursing home: development and validation of the 6-month minimum data set mortality risk index. J Gerontol A Biol Sci Med Sci. 2005;60:491. doi: 10.1093/gerona/60.4.491. [DOI] [PubMed] [Google Scholar]
- [23].Porock D, Parker-Oliver D, Petroski GF, Rantz M. The MDS mortality risk index: the evolution of a method for predicting 6-month mortality in nursing home residents. BMC Res Notes. 2010;3:200. doi: 10.1186/1756-0500-3-200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Flacker JM, Kiely DK. Mortality-related factors and 1-year survival in nursing home residents. J Am Geriatr Soc. 2003;51:213. doi: 10.1046/j.1532-5415.2003.51060.x. [DOI] [PubMed] [Google Scholar]
- [25].Van Dijk PTM, Mehr ÃDR, Ooms ME, et al. Comorbidity and 1-year mortality risks in nursing home residents. J Am Geriatr Soc. 2005;53:660. doi: 10.1111/j.1532-5415.2005.53216.x. [DOI] [PubMed] [Google Scholar]
- [26].Wallace JB, Prevost SS. Two methods for predicting limited life expectancy in nursing homes. J Nurs Scholarsh. 2006;38:148. doi: 10.1111/j.1547-5069.2006.00092.x. [DOI] [PubMed] [Google Scholar]
- [27].Lee J, Rantz M. Correlates of post-hospital physical function at 1 year in skilled nursing facility residents. J Adv Nurs. 2008;62:479. doi: 10.1111/j.1365-2648.2008.04612.x. [DOI] [PubMed] [Google Scholar]
- [28].Arling G, Kane RL, Mueller C, Bershadsky J, Degenholtz HB. Nursing effort and quality of care for nursing home residents. Gerontologist. 2007;47:672. doi: 10.1093/geront/47.5.672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Bates-Jensen BM, Schnelle JF, Alessi CA, Al-Samarrai NR, Levy-Storms LF. The effects of staffing on in-bed times of nursing home residents. J Am Geriatr Soc. 2004;52:931. doi: 10.1111/j.1532-5415.2004.52260.x. [DOI] [PubMed] [Google Scholar]
- [30].Bostick JE. Relationship of nursing personnel and nursing home care quality. J Nurs Care Qual. 2004;19:130. doi: 10.1097/00001786-200404000-00010. [DOI] [PubMed] [Google Scholar]
- [31].Kane RL. Commentary: nursing home staffing- more is necessary but not necessarily sufficient. Health Serv Res. 2004;39:251. doi: 10.1111/j.1475-6773.2004.00226.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Decker FH. Nursing staff and the outcomes of nursing home stays. Med Care. 2006;44:812. doi: 10.1097/01.mlr.0000218832.24637.2e. [DOI] [PubMed] [Google Scholar]
- [33].Castle NG, Anderson RA. Caregiver staffing in nursing homes and their influence on quality of care: using dynamic panel estimation methods. Med Care. 2011;49:545. doi: 10.1097/MLR.0b013e31820fbca9. [DOI] [PubMed] [Google Scholar]
- [34].Weech-Maldonado R, Meret-Hanke L, Neff MC, Mor V. Nurse staffing patterns and quality of care in nursing homes. Health Care Manage Rev. 2004;29:107. doi: 10.1097/00004010-200404000-00004. [DOI] [PubMed] [Google Scholar]
- [35].Horn BSD, Buerhaus P, Bergstrom N, Smout RJ. RN staffing time and outcomes of long-stay nursing home residents. Am J Nurs. 2005;105:58. doi: 10.1097/00000446-200511000-00028. [DOI] [PubMed] [Google Scholar]
- [36].Decker FH. The relationship of nursing staff to the hospitalization of nursing home residents. Res Nurs Health. 2008;31:238. doi: 10.1002/nur.20249. [DOI] [PubMed] [Google Scholar]
- [37].Decker FH. Outcomes and length of Medicare nursing home stays: the role of registered nurses and physical therapists. Am J Med Qual. 2008;23:465. doi: 10.1177/1062860608324173. [DOI] [PubMed] [Google Scholar]
- [38].Li Y, Cai X, Mukamel DB, Glance LG. The volume-outcome relationship in nursing home care. Med Care. 2010;48:52. doi: 10.1097/MLR.0b013e3181bd4603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Harrington C, Woolhandler S, Mullan J, Carrillo H, Himmelstein DU. The commercialization of medicine: does investor ownership of nursing homes compromise the quality of care? Int J Health Serv. 2002;32:315. doi: 10.2190/EBCN-WECV-C0NT-676R. [DOI] [PubMed] [Google Scholar]
- [40].Zimmerman S, Gruber-Baldini AL, Hebel JR, Sloane PD, Magaziner J. Nursing home facility risk factors for infection and hospitalization: importance of registered nurse turnover, administration, and social factors. J Am Geriatr Soc. 2002;50:1987. doi: 10.1046/j.1532-5415.2002.50610.x. [DOI] [PubMed] [Google Scholar]
- [41].Intrator O, Zinn J, Mor V. Nursing home characteristics and potentially preventable hospitalizations of long-stay residents. J Am Geriatr Soc. 2004;52:1730. doi: 10.1111/j.1532-5415.2004.52469.x. [DOI] [PubMed] [Google Scholar]
- [42].Culler SD, Parchman ML, Przybylski M. Factors related to potentially preventable hospitalizations among the elderly. Med Care. 1998;36:804. doi: 10.1097/00005650-199806000-00004. [DOI] [PubMed] [Google Scholar]
- [43].Jette DU, Warren RL, Wirtalla C. The relation between therapy intensity and outcomes of rehabilitation in skilled nursing facilities. Arch Phys Med Rehabil. 2005;86:373. doi: 10.1016/j.apmr.2004.10.018. [DOI] [PubMed] [Google Scholar]
- [44].Horn SD, Sharkey SS, Hudak S, et al. Beyond CMS quality measure adjustments: identifying key resident and nursing home facility factors associated with quality measures. J Am Med Directors Assoc. 2010;11:500. doi: 10.1016/j.jamda.2009.10.008. [DOI] [PubMed] [Google Scholar]
- [45].Berkowitz RE, Jones RN, Rieder R, et al. Improving disposition outcomes for patients in a geriatric skilled nursing facility. J Am Geriatr Soc. 2011;59:1130. doi: 10.1111/j.1532-5415.2011.03417.x. [DOI] [PubMed] [Google Scholar]
- [46].Hutchinson AM, Milke DL, Maisey S, et al. The resident assessment instrument-minimum data set 2.0 quality indicators:a systematic review. BMC Health Serv Res. 2010;10:166. doi: 10.1186/1472-6963-10-166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [47].Hill-Westmoreland EE, Gruber-Baldini AL. Falls documentation in nursing homes: agreement between the minimum data set and chart abstractions of medical and nursing documentation. J Am Geriatr Soc. 2005;53:268. doi: 10.1111/j.1532-5415.2005.53113.x. [DOI] [PubMed] [Google Scholar]
- [48].Simmons SF, Garcia ET, Cadogan MP, et al. The minimum data set weight-loss quality indicator: does it reflect differences in care processes related to weight loss? J Am Geriatr Soc. 2003;51:1410. doi: 10.1046/j.1532-5415.2003.51459.x. [DOI] [PubMed] [Google Scholar]
- [49].Schnelle JF, Cadogan MP, Yoshii J, et al. The minimum data set urinary incontinence quality indicators: do they reflect differences in care processes related to incontinence? Med Care. 2003;41:909. doi: 10.1097/00005650-200308000-00005. [DOI] [PubMed] [Google Scholar]
- [50].Stevenson KB, Moore JW, Sleeper B. Validity of the minimum data set in identifying urinary tract infections in residents of long-term care facilities. J Am Geriatr Soc. 2004;52:707. doi: 10.1111/j.1532-5415.2004.52206.x. [DOI] [PubMed] [Google Scholar]
- [51].Mcconnell ES, Schnelle JF, Wood S, Schnelle ER, Simmons SF. Measurement sensitivity and the minimum data set depression quality indicator. Gerontologist. 2001;41:401. doi: 10.1093/geront/41.3.401. [DOI] [PubMed] [Google Scholar]
- [52].Simmons SF, Cadogan MP, Cabrera GR, et al. The minimum data set depression quality indicator: does it reflect differences in care processes? Gerontologist. 2004;44:554. doi: 10.1093/geront/44.4.554. [DOI] [PubMed] [Google Scholar]
- [53].Bates-jensen BM, Cadogan M, Osterweil D. The minimum data set pressure ulcer indicator: does it reflect differences in care processes related to pressure ulcer prevention and treatment in nursing homes? J Am Geriatr Soc. 2003;51:1203. doi: 10.1046/j.1532-5415.2003.51403.x. [DOI] [PubMed] [Google Scholar]
- [54].Schnelle JF, Bates-Jensen BM, Levy-Storms L, et al. The minimum data set prevalence of restraint quality indicator: does it reflect differences in care? Gerontologist. 2004;44:245. doi: 10.1093/geront/44.2.245. [DOI] [PubMed] [Google Scholar]
- [55].Porell F, Caro FG. Facility-level outcome performance measures for nursing homes. Gerontologist. 1998;38:665. doi: 10.1093/geront/38.6.665. [DOI] [PubMed] [Google Scholar]
- [56].Hodlewsky RT, Decker FH. The problem of bias when nursing facility staff administer customer satisfaction surveys. Jt Comm J Qual Improv. 2002;28:546. doi: 10.1016/s1070-3241(02)28058-x. [DOI] [PubMed] [Google Scholar]
- [57].Kane RL, Bershadsky B, Kane RA, et al. Using resident reports of quality of life to distinguish among nursing homes. Gerontologist. 2004;44:624. doi: 10.1093/geront/44.5.624. [DOI] [PubMed] [Google Scholar]