Skeletal muscle adapts to a prolonged reduction in physical activity by decreasing muscle fibre size and protein content. This physiological response is commonly termed disuse atrophy. It is most clearly stimulated by conditions that reduce mechanical loading of postural or respiratory muscles in the absence of disease and neural deficits. Examples of such conditions include bed rest, joint immobilization, limb suspension, microgravity and mechanical ventilation. In muscle disuse, as in all atrophic processes, the rate of proteolysis exceeds the rate of protein synthesis causing net loss of protein. A dispassionate review of the literature shows that both aspects of muscle protein homeostasis are disrupted by prolonged disuse. Proteolysis increases and synthesis declines. These changes have additive effects, contributing jointly to protein loss and muscle atrophy. The relative magnitudes of these contributions have not been measured directly and are not known. Therefore, like most scientists, we are resolutely ecumenical on the issue of proteolysis vs. synthesis. In contrast, a few individuals fervently argue that disuse atrophy is caused by decreased protein synthesis and that proteolysis is unimportant. This viewpoint has created unnecessary controversy in the literature and heated discussion at scientific conferences. This controversy is the focus of our CrossTalk debate.
To be clear, the ‘dominant mechanism’ of disuse atrophy is not known. Rates of proteolysis vs. protein synthesis cannot be quantified using existing methods nor can differences in these rates be measured directly. Attempts to estimate these values must be based on first principles, must involve untested assumptions, and cannot be validated experimentally. This makes it impossible to assign ‘dominance’ with scientific rigor. Instead of speculating on this issue, we will present evidence for the biological importance of proteolysis in disuse atrophy. The extent of peer-reviewed research, the diversity of experimental approaches, and the level of mechanistic detail make a compelling case for our position that proteolysis is essential for disuse atrophy.
Disuse stimulates proteolysis
For almost four decades, we have known that disuse promotes atrophy of skeletal muscle by stimulating protein breakdown. This process involves the co-activation of multiple proteolytic mechanisms that have complementary roles in degrading muscle protein. The ubiquitin–proteasome pathway is the dominant mechanism of protein breakdown during muscle atrophy (Bodine, 2013). Disuse activates this pathway in muscle, as shown by three lines of evidence: First, muscle increases the expression of key gene products that regulate pathway activity. Mechanical unloading stimulates a rise in mRNA for the polyubiquitin gene, E2 ubiquitin conjugating proteins, E3 ubiquitin ligases, and subunits of the proteasome complex (Taillandier et al. 1996; Ikemoto et al. 2001; Jones et al. 2004; Nikawa et al. 2004; Hussain et al. 2010). Gene targets of particular interest are MAFbx/atrogin1 and MuRF1, two muscle-specific E3 ligases that regulate muscle atrophy in a variety of experimental models (Bodine et al. 2001). Like virtually all conditions of muscle wasting, MAFbx/atrogin1 and MuRF1 mRNA are increased in disuse atrophy. This response has been documented in diaphragm of mechanically ventilated humans and rodents (DeRuisseau et al. 2005; Levine et al. 2008, 2011; Hussain et al. 2010), limb muscles of humans after bed rest, lower limb suspension, or knee immobilization (Jones et al. 2004; de Boer et al. 2007; Abadi et al. 2009; Gustafsson et al. 2010; Reich et al. 2010; Wall et al. 2014), and limb muscles of rodents after hindlimb unloading, limb immobilization, or spaceflight (Nikawa et al. 2004; Senf et al. 2008; Andrianjafiniony et al. 2010). Second, upregulation of these pathway elements has the predicted outcome: ubiquitin conjugation to muscle proteins is increased in both humans and rodents (Ikemoto et al. 2001; DeRuisseau et al. 2005; Abadi et al. 2009; Ferreira et al. 2009; Levine et al. 2011; Brocca et al. 2012). Third, unloading increases the proteolytic activities of the 20S- and 26S-proteasome complexes. This occurs in human and rodent muscles (Ikemoto et al. 2001; Shanely et al. 2002; Levine et al. 2011), facilitating breakdown of ubiquitin-conjugated proteins.
Muscle proteases and autophagy are also activated during disuse atrophy. This is particularly well documented for the cysteine-aspartic protease family, i.e. the caspases. The original discovery that unloading increases caspase-3 mRNA in the human diaphragm (Levine et al. 2008) led to animal studies confirming that caspase-3 enzyme activity is increased in unloaded diaphragm and limb muscles (Ferreira et al. 2009; Nelson et al. 2012; Talbert et al. 2013). Other members of the caspase family that are upregulated by unloading include caspase-6, -8, -9 and -12 (Taillandier et al. 1996; Andrianjafiniony et al. 2010). Calpain, a calcium-dependent protease, exhibits a similar response. Mechanical unloading of either diaphragm or limb muscle causes an increase in calpain mRNA and calpain activity (Taillandier et al. 1996; Shanely et al. 2002; DeRuisseau et al. 2005; Ferreira et al. 2009; Andrianjafiniony et al. 2010; Nelson et al. 2012; Talbert et al. 2013). Finally, emerging evidence indicates that autophagy via the lysosomal system is also increased during disuse atrophy of human and rodent muscles (Taillandier et al. 1996; Ikemoto et al. 2001; Andrianjafiniony et al. 2010; Hussain et al. 2010; Brocca et al. 2012). In aggregate, unloading activates all major proteolytic mechanisms – the ubiquitin–proteasome pathway, protease activity, and autophagy – thereby promoting the degradation of large molecular weight myofibrillar proteins, cytosolic proteins and smaller polypeptide residues.
Upregulation of proteolytic mechanisms (above) increases protein breakdown in unloaded skeletal muscle. This fact has been demonstrated in rodents using limb immobilization, hindlimb unloading, and mechanical ventilation (Goldspink, 1977; Loughna et al. 1987; Shanely et al. 2002) and in humans using unilateral lower limb suspension (Tesch et al. 2008). The latter study employed an innovative microdialysis technique to measure interstitial levels of 3-methylhistidine, an endogenous biomarker of myofibrillar degradation. Unloading for 3 days increased 3-methylhistidine levels by over 40%: evidence of increased breakdown of myofibrillar protein. This finding is consistent with recent evidence that human muscle undergoes significant atrophy within 2–5 days of being unloaded (Grosu et al. 2012; Suetta et al. 2012; Wall et al. 2014) and shows that greater protein breakdown is fundamental to the disuse atrophy process across species.
Conclusion
It is clear that proteolysis plays an important role in disuse atrophy, perhaps the most important role. This conclusion is firmly rooted in modern interdisciplinary biology (Fig. 1A). It incorporates what we know about muscle cell signalling, gene expression at the mRNA and protein levels, protein biochemistry, proteasome and protease activities, and regulation of protein breakdown. Plus it is inclusive, applying equally to postural and respiratory muscles of rodents and humans.
Figure 1. Word clouds illustrating the experimental approaches used to assess proteolysis (A) and protein synthesis (B) during disuse atrophy.
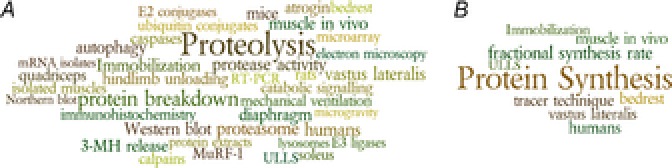
3-MH, 3-methylhistidine; ULLS, unilateral lower limb suspension.
How can our learned opponent and a handful of other skeptics reject the preponderance of evidence on this issue? Historically, the position that proteolysis is unimportant has derived from measurements of fractional synthesis rate (FSR) in human vastus lateralis muscle during disuse. FSR data have been used to estimate the importance of synthesis based on first principles and assumptions that are either unstated or untested. This narrow approach (Fig. 1B), based on one end-point from one muscle of one species, has been justified by arguments that rodent models of disuse are ‘heuristically misleading’, that ‘dynamic’ FSR data are inherently more valid than ‘snapshot’ (i.e. any other) measurements, and that approaches which yield different outcomes are flawed and unreliable (Rennie et al. 2010). Such a position leaves little room for open-minded inquiry or free exchange of ideas. We must move beyond an either/or approach in order to broaden our understanding and advance the field. The time has come to acknowledge the fact that proteolysis is an essential component of disuse atrophy.
Call for comments
Readers are invited to give their views on this and the accompanying CrossTalk articles in this issue by submitting a brief (250 word) comment. Comments may be submitted up to 6 weeks after publication of the article, at which point the discussion will close and the CrossTalk authors will be invited to submit a ‘Last Word’. Please email your comment to journals@physoc.org.
Additional information
Competing interests
None declared.
Funding
This work was supported by the U.S. National Institute of Arthritis, Musculoskeletal, and Skin Diseases grants R01AR060209 (to A.R.J.), R01AR062083 (to M.B.R.), U.S. National Institute of Diabetes and Digestive and Kidney Diseases grant DK75801 (to S.C.B.), and U.S. Veterans Administration Rehabilitation Research and Development grant E7766R (to S.C.B.).
References
- Abadi A, Glover EI, Isfort RJ, Raha S, Safdar A, Yasuda N, Kaczor JJ, Melov S, Hubbard A, Qu X, Phillips SM, Tarnopolsky M. Limb immobilization induces a coordinate down-regulation of mitochondrial and other metabolic pathways in men and women. PLoS One. 2009;4:e6518. doi: 10.1371/journal.pone.0006518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andrianjafiniony T, Dupre-Aucouturier S, Letexier D, Couchoux H, Desplanches D. Oxidative stress, apoptosis, and proteolysis in skeletal muscle repair after unloading. Am J Physiol Cell Physiol. 2010;299:C307–C315. doi: 10.1152/ajpcell.00069.2010. [DOI] [PubMed] [Google Scholar]
- Bodine SC. Disuse-induced muscle wasting. Int J Biochem Cell Biol. 2013;45:2200–2208. doi: 10.1016/j.biocel.2013.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bodine SC, Latres E, Baumhueter S, Lai VK, Nunez L, Clarke BA, Poueymirou WT, Panaro FJ, Na E, Dharmarajan K, Pan ZQ, Valenzuela DM, DeChiara TM, Stitt TN, Yancopoulos GD, Glass DJ. Identification of ubiquitin ligases required for skeletal muscle atrophy. Science. 2001;294:1704–1708. doi: 10.1126/science.1065874. [DOI] [PubMed] [Google Scholar]
- Brocca L, Cannavino J, Coletto L, Biolo G, Sandri M, Bottinelli R, Pellegrino MA. The time course of the adaptations of human muscle proteome to bed rest and the underlying mechanisms. J Physiol. 2012;590:5211–5230. doi: 10.1113/jphysiol.2012.240267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Boer MD, Selby A, Atherton P, Smith K, Seynnes OR, Maganaris CN, Maffulli N, Movin T, Narici MV, Rennie MJ. The temporal responses of protein synthesis, gene expression and cell signalling in human quadriceps muscle and patellar tendon to disuse. J Physiol. 2007;585:241–251. doi: 10.1113/jphysiol.2007.142828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeRuisseau KC, Kavazis AN, Deering MA, Falk DJ, Van Gammeren D, Yimlamai T, Ordway GA, Powers SK. Mechanical ventilation induces alterations of the ubiquitin-proteasome pathway in the diaphragm. J Appl Physiol (1985) 2005;98:1314–1321. doi: 10.1152/japplphysiol.00993.2004. [DOI] [PubMed] [Google Scholar]
- Ferreira R, Vitorino R, Neuparth MJ, Appell HJ, Duarte JA, Amado F. Proteolysis activation and proteome alterations in murine skeletal muscle submitted to 1 week of hindlimb suspension. Eur J Appl Physiol. 2009;107:553–563. doi: 10.1007/s00421-009-1151-1. [DOI] [PubMed] [Google Scholar]
- Goldspink DF( The influence of immobilization and stretch on protein turnover of rat skeletal muscle. J Physiol. 1977;264:267–282. doi: 10.1113/jphysiol.1977.sp011667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grosu HB, Lee YI, Lee J, Eden E, Eikermann M, Rose KM. Diaphragm muscle thinning in patients who are mechanically ventilated. Chest. 2012;142:1455–1460. doi: 10.1378/chest.11-1638. [DOI] [PubMed] [Google Scholar]
- Gustafsson T, Osterlund T, Flanagan JN, von Waldén F, Trappe TA, Linnehan RM, Tesch PA. Effects of 3 days unloading on molecular regulators of muscle size in humans. J Appl Physiol (1985) 2010;109:721–727. doi: 10.1152/japplphysiol.00110.2009. [DOI] [PubMed] [Google Scholar]
- Hussain SN, Mofarrahi M, Sigala I, Kim HC, Vassilakopoulos T, Maltais F, Bellenis I, Chaturvedi R, Gottfried SB, Metrakos P, Danialou G, Matecki S, Jaber S, Petrof BJ, Goldberg P. Mechanical ventilation-induced diaphragm disuse in humans triggers autophagy. Am J Respir Crit Care Med. 2010;182:1377–1386. doi: 10.1164/rccm.201002-0234OC. [DOI] [PubMed] [Google Scholar]
- Ikemoto M, Nikawa T, Takeda S, Watanabe C, Kitano T, Baldwin KM, Izumi R, Nonaka I, Towatari T, Teshima S, Rokutan K, Kishi K. Space shuttle flight (sts-90) enhances degradation of rat myosin heavy chain in association with activation of ubiquitin-proteasome pathway. FASEB J. 2001;15:1279–1281. doi: 10.1096/fj.00-0629fje. [DOI] [PubMed] [Google Scholar]
- Jones SW, Hill RJ, Krasney PA, O'Conner B, Peirce N, Greenhaff PL. Disuse atrophy and exercise rehabilitation in humans profoundly affects the expression of genes associated with the regulation of skeletal muscle mass. FASEB J. 2004;18:1025–1027. doi: 10.1096/fj.03-1228fje. [DOI] [PubMed] [Google Scholar]
- Levine S, Biswas C, Dierov J, Barsotti R, Shrager JB, Nguyen T, Sonnad S, Kucharchzuk JC, Kaiser LR, Singhal S, Budak MT. Increased proteolysis, myosin depletion, and atrophic AKT-FOXO signaling in human diaphragm disuse. Am J Respir Crit Care Med. 2011;183:483–490. doi: 10.1164/rccm.200910-1487OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levine S, Nguyen T, Taylor N, Friscia ME, Budak MT, Rothenberg P, Zhu J, Sachdeva R, Sonnad S, Kaiser LR, Rubinstein NA, Powers SK, Shrager JB. Rapid disuse atrophy of diaphragm fibers in mechanically ventilated humans. N Engl J Med. 2008;358:1327–1335. doi: 10.1056/NEJMoa070447. [DOI] [PubMed] [Google Scholar]
- Loughna PT, Goldspink DF, Goldspink G. Effects of hypokinesia and hypodynamia upon protein-turnover in hindlimb muscles of the rat. Aviat Space Environ Med. 1987;58:A133–A138. [PubMed] [Google Scholar]
- Nelson WB, Smuder AJ, Hudson MB, Talbert EE, Powers SK. Cross-talk between the calpain and caspase-3 proteolytic systems in the diaphragm during prolonged mechanical ventilation. Crit Care Med. 2012;40:1857–1863. doi: 10.1097/CCM.0b013e318246bb5d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nikawa T, Ishidoh K, Hirasaka K, Ishihara I, Ikemoto M, Kano M, Kominami E, Nonaka I, Ogawa T, Adams GR, Baldwin KM, Yasui N, Kishi K, Takeda S. Skeletal muscle gene expression in space-flown rats. FASEB J. 2004;18:522–524. doi: 10.1096/fj.03-0419fje. [DOI] [PubMed] [Google Scholar]
- Reich KA, Chen YW, Thompson PD, Hoffman EP, Clarkson PM. Forty-eight hours of unloading and 24 h of reloading lead to changes in global gene expression patterns related to ubiquitination and oxidative stress in humans. J Appl Physiol (1985) 2010;109:1404–1415. doi: 10.1152/japplphysiol.00444.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rennie MJ, Selby A, Atherton P, Smith K, Kumar V, Glover EL, Philips SM. Facts, noise and wishful thinking: Muscle protein turnover in aging and human disuse atrophy. Scand J Med Sci Sports. 2010;20:5–9. doi: 10.1111/j.1600-0838.2009.00967.x. [DOI] [PubMed] [Google Scholar]
- Senf SM, Dodd SL, McClung JM, Judge AR. Hsp70 overexpression inhibits NF-κB and Foxo3a transcriptional activities and prevents skeletal muscle atrophy. FASEB J. 2008;22:3836–3845. doi: 10.1096/fj.08-110163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shanely RA, Zergeroglu MA, Lennon SL, Sugiura T, Yimlamai T, Enns D, Belcastro A, Powers SK. Mechanical ventilation- induced diaphragmatic atrophy is associated with oxidative injury and increased proteolytic activity. Am J Respir Crit Care Med. 2002;166:1369–1374. doi: 10.1164/rccm.200202-088OC. [DOI] [PubMed] [Google Scholar]
- Suetta C, Frandsen U, Jensen L, Jensen MM, Jespersen JG, Hvid LG, Bayer M, Petersson SJ, Schroder HD, Andersen JL, Heinemeier KM, Aagaard P, Schjerling P, Kjaer M. Aging affects the transcriptional regulation of human skeletal muscle disuse atrophy. PLoS One. 2012;7:e51238. doi: 10.1371/journal.pone.0051238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taillandier D, Aurousseau E, Meynial-Denis D, Bechet D, Ferrara M, Cottin P, Ducastaing A, Bigard X, Guezennec CY, Schmid HP, Attaix D. Coordinate activation of lysosomal, Ca2+-activated and ATP-ubiquitin-dependent proteinases in the unweighted rat soleus muscle. Biochem J. 1996;316:65–72. doi: 10.1042/bj3160065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Talbert EE, Smuder AJ, Min K, Kwon OS, Powers SK. Calpain and caspase-3 play required roles in immobilization-induced limb muscle atrophy. J Appl Physiol (1985) 2013;114:1482–1489. doi: 10.1152/japplphysiol.00925.2012. [DOI] [PubMed] [Google Scholar]
- Tesch PA, von Walden F, Gustafsson T, Linnehan RM, Trappe TA. Skeletal muscle proteolysis in response to short-term unloading in humans. J Appl Physiol (1985) 2008;105:902–906. doi: 10.1152/japplphysiol.90558.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wall BT, Dirks ML, Snijders T, Senden JM, Dolmans J, van Loon LJ. Substantial skeletal muscle loss occurs during only 5 days of disuse. Acta Physiol (Oxf) 2014;210:600–611. doi: 10.1111/apha.12190. [DOI] [PubMed] [Google Scholar]


