Abstract
Background & aims: Ileo-colonic strictures are common complication of Crohn’s disease (CD), and may result in repeated endoscopic or surgical therapy with a risk of further complications, such as perforation or short bowel syndrome. Strictures develop as a consequence of tissue remodelling and fibrosis due to chronic inflammation. This study compares the outcome of CD patients undergoing primarily endoscopic treatment with those undergoing surgery at an university hospital. Methods: In this study we retrospectively included 88 CD patients with intestinal strictures (37 males, 51 females, mean age 40 years, range 19-65 years) of both our medical and our surgical department, who underwent either surgical or endoscopic therapy between January 2002 and January 2006 with prospective, controlled follow-up, extended till January 2010 (mean follow-up period: 5 years; range 4-8 years). The primary end-point was operation- and symptom-free time. Patients were primarily divided into four groups: only surgical therapy, only endoscopic therapy, endoscopy with subsequent surgery, and initial surgical therapy followed by endoscopic dilations. Results: 53% of all patients remained surgery-free with mean follow-up of 49 months; a single endoscopic dilation was sufficient enough in 9 patients to achieve a surgery-free time of 51 months, other patients required up to 5 dilations. The average interval between first and second dilation was 6.5 months, between second and third 10.5 months. In the group of patients with only endoscopic therapy, surgery- and symptom-free time was shorter, as compared to the group of only surgical therapy. We found that stenoses in the surgical group with an average length of 6.5 cm were as expected longer, as compared to the endoscopic group (3 cm, ranging from 2-4 cm). The surgery-free time was 49 months (42-71 months, P = 0.723) with a symptom-free time of 12 months (4.5-46 months, P = 0.921). In the group of only surgically treated patients, 68.4% of the patients had only one stenosis, 18.4% had 2-3 stenoses and 13.2% more than 3 stenoses. In all patients the surgery- and symptoms- free time was 69 months (57-83 months, P = 0.850 and 0.908). The other two groups showed similar results. We found no significant effect of characteristic of stenosis (length, inflammation, the number of stenoses), injection of prednisolone, disease activity at the time of dilation and medication at the time of dilation on the long-term outcome. Importantly, the success of symptom free time correlated with the diameter of the balloon. Conclusions: Endoscopic dilation should be considered as a first-line therapy for short, accessible, fibrotic strictures. Careful patient selection and proper diagnostic imaging pre-procedure are essential requirements for safe and successful treatment. The balloon diameter seems to correlate positively with the long term outcome of dilation. However, at ever shorter intervals between endoscopic interventions, surgery should be discussed as an option for further treatment.
Keywords: Crohn’s disease, intestinal stricture, endoscopic dilation, strictureplasty
Introduction
Crohn’s disease (CD) is characterized by chronic, recurrent, transmural inflammation, which as a consequence of partial healing and localized fibrosis may lead to intestinal strictures, often resulting in repeated surgery [1,6,14]. The strictures develop due to chronic inflammation leading to tissue remodelling, mesenchymal (fibroblastic) cell proliferation, hyperplasia and fibrosis [26]. They are usually defined as a constant luminal narrowing with a pre-stenotic dilation and obstructive clinical symptoms. The stenotic segments predominate in the terminal ileum, ileocolonic anastomosis and the rectum [19,26].
The prevalence of small bowel stenosis has ranged in recent studies from 20% to 40% in patients with ileal disease, and from 7% to 15% in patients with colonic disease [25]. Despite advances in medical therapy with immunosuppressive agents, including anti-tumour necrosis factor (TNF) antibodies, intestinal strictures remain a clinical challenge in CD [29]. Immunomodulatory therapy may suppress inflammation before, during and after successful dilation of all types of Crohn’s stricture, but there is also concern that the enhanced mucosal healing may exaggerate existing strictures [10,21,33].
Although resection of stenotic or perforated intestinal segments is often unavoidable, without achieving mucosa healing, surgical remission will be only temporary [30]. Endoscopically, more than 70% of patients will have new lesions within a year and 40% will be symptomatic within 4 years [15]. The majority of CD patients still is in need for surgery within 10 years of diagnosis [32].
Since repeated bowel resections may result in short bowel syndrome, the quest for bowel-conserving strategies over the last 25 years has introduced both endoscopic balloon dilation and surgical resection and, later, strictureplasty in clinical practice [26,30].
Successful endoscopic dilation of anastomotic strictures in CD using through-the-scope (TTS) rigid balloons was first reported in 1981 and has emerged as an alternative to surgical treatment for selected patients [29]. Challenges for the endoscopist include achieving endoscopic access to the distal end of the stenosis, successful passage of the balloon catheter through the stricture to allow inspection and to obtain adequate dilation while minimizing the risk of major complications [2,21].
In endoscopic terms, dilation of CD stricture is a relatively high risk procedure with reported perforation rates up to 11%, but with immediate success rates ranging from 71% to 100% [29,31]. The degree of dilation depends on the location and calibre of the stricture; most short strictures in the colon or ileum can be dilated to 15-20 mm [21]. The radiological assessment, careful patient selection, an experienced endoscopist, and access to the appropriate equipment and facilities are all essential requirements for a safe and successful procedure, where the alleviation of obstructive symptoms is most important goal [21].
Strictureplasty for CD was introduced at the end of the 1970s by Lee and Papaioannou to avoid massive resections in patients affected with multiple strictures [11]. This procedure is particularly indicated in following cases: for skip lesions, to avoid broad resection of healthy segments or multiple resections; for multiple strictures localized in long segments of the small bowel; for patients with previous resections, to preserve the small-bowel length avoiding a short bowel syndrome [9]. Furthermore, for patients who have recurrent ileocolic anastomotic strictures or patients with obstruction from strictures of the duodenum, to avoid gastrojejunostomy or duodenopancreatectomy [28].
The use of strictureplasty in CD has become increasingly common; most surgeons use similar techniques of Heineke-Mikulicz (H-M) repair for shorter lesions and Finney repair for longer lesions [9,27]. The H-M is still most applicable to stricture less than 10 cm in length [27]. This technique is analogous to H-M pyloroplasty; a longitudinal enterotomy is made extending 1 to 2 cm into the normal bowel with enterotomy, closed transversely with one or two layers of absorbable sutures [27].
Long-term outcome of both endoscopic and surgical therapies has been reported very controversial, since in most cohorts follow-up was limited to less than 3 years and the individual cohorts report on a relatively small number of patients; the influence of endoscopic and clinical disease activity at the time of dilation, and the influence of concomitant medical therapy on the outcome of stricture dilation, is largely unknown [15,26].
To our best knowledge there have been no studies, comparing both surgical and endoscopic therapy of intestinal strictures of CD in terms of long term outcome. Therefore, the aim of this study was to analyze results of our clinical experience with endoscopic and surgical (resection and strictureplasty) therapy, such evaluating long-term safety and efficacy of these procedures in a large referral center cohort, incorporating characteristics of stricture (length, anastomosis, inflammation etc.), length of the operation-free interval, influence of disease activity and medication.
Patients and methods
In this study we retrospectively included 88 CD patients (37 males, 51 females, mean age 40 years, range 19-65 years) who underwent either surgical or endoscopic therapy for symptomatic intestinal strictures at the medical and surgical departments, university hospital Erlangen, between January 2002 and January 2010.
Patients were identified by a search of our hospital registry. Retrospective chart analysis was performed to exclude non-CD strictures. To achieve a mean follow-up period of 5 years (4 to 8 years), we did not include the patients after January 2006. We followed up the patients prospectively till January 2010, where 68 patients were examined in our outpatient clinic; 20 patients could not participate on clinical evaluation and were contacted per telephone with questionnaire. The study has been approved by the ethics committee of our hospital.
The patients were primarily divided into four groups: patients, who underwent only surgical therapy, only endoscopic therapy, endoscopic procedures with following surgery, or initial surgical treatment with following endoscopic dilation/s.
Long-term efficacy of endoscopic balloon dilation compared to surgical therapy, defined as clinical absence of obstructive symptoms (symptoms-free time, months) and avoidance of surgery (surgery- or operation-free time, months), was chosen as the primary endpoint. Secondary endpoints included impact of the disease duration, type and site of the previous surgery, number, type, length and localization of the strictures, disease activity (Harvey-Bradshaw Index, HBI), inflammation at the site of stenosis, medication, TTS balloon diameter, injection of prednisolone after dilation.
The activity of the CD was evaluated using the HBI (Harvey-Bradshaw Index) score as follows:
Remission < 5 points, Mild disease 5-7 points, Moderate disease 8-16 points, Severe disease > 16 points.
HBI evaluates patient’s general well-being (for the previous day), abdominal pain (for the previous day), number of liquid stools per day (for the previous day, score 1 per movement), abdominal mass and also the presence of such complications as arthralgia, uveitis, erythema nodosum, aphthous ulcers, pyoderma gangrenosum, anal fissure, new fistula, abscess (additional score 1 per item).
Exclusion criteria were inflammatory processes in the immediate proximity of the intestine to be dilated or resected (intestinal perforation, fistulas, abscesses, peritonitis).
All the patients were admitted because of obstructive symptoms such as abdominal pain, cramps, bloating and vomiting. The strictures were assessed using high-definition sonography, and also CT/MRI enteroclysis to evaluate the stricture (type, length), to exclude intestinal fistulas and angulation. The treatment options of stenoses included intensification of anti-inflammatory medication, endoscopic balloon dilation, and surgery (resection or stricturoplasty). The strictures were considered suitable for endoscopic dilation if they were endoscopically accessible and < 6 cm in length.
Colonoscopies with hydrostatic balloon dilation were performed under conscious sedation with midazolam/pethidin or midazolam/disoprivan to perceive a possibly imminent perforation by the patient’s utterance of pain. Microvasive Rigiflex through the scope balloons (TTS, Boston Scientific Microvasive, MA, USA) with a diameter of 15-18 mm were used. Three types of balloon were used: 50 mm (length) × 18 mm (diameter), 80 mm × 18 mm and 80 mm × 20 mm.
The introduction of the balloon into the stricture was done under visual or radiological control. During the endoscopic procedure the TTS balloon was filled with water to a pressure of 35 psi, and was insufflated by a multistep inflation using the Alliance Integrated Inflation System (Boston Scientific, Microvasive, MA, USA). After filling up to a diameter of 15 mm, the pressure inside the balloon was maintained for at least 2 min, and the dilation was repeated once or twice, when necessary. An additional inflation of the balloon to 18 mm for 2 min. was performed if the first dilation did not allow passage of the endoscope through the stenosis. This technique was used to minimize the risk of perforation. At the first dilation, specimens were taken out of the strictures to rule out malignancy.
The passage of the scope through the stricture was attempted in all patients and was used to define therapeutic success. After dilation patients were observed for at least one hour or until resolution of abdominal pain in our recovery room. In the case of persisting pain or abdominal distension, a plain abdominal x-ray was obtained and patients were referred for surgery in case of perforation. In case of unsatisfactory dilation, the treatment was repeated two days later. Complications were defined as perforation, active bleeding with the need of an endoscopic re-intervention or the transfusion of blood, and also abdominal pain after balloon dilation.
Descriptive statistics were used to analyze patient demographics. The results were expressed as the mean or median (range). Kolmogorov-Smirnov test was used to prove the numbers of normal distribution; because of the deviations from the normal distribution the U test and Kruskal-Wallis test were used to analyze the data. Probability estimates were given with the 95% confidence interval (95% CI); padj < 0.05 was considered to be significant. For the implementation of the statistical calculations SPSS 18 (SPSS Inc.an IBM Company, Chicago, IL) was used.
Results
In total, 206 treatments were performed (160 dilations, 46 operations). 67% of the patients received an open laparotomy, 14 patients were treated using laparoscopy; 4 times strictureplasty was performed. The median age of the patient at the treatment was 40 years (range 19-65 years), 60.2% women. After intervention, there were no deaths, anastomotic leaks, fistulas, or abscesses. In five cases of endoscopic balloon dilation, a perforation occurred and open laparotomy had to be performed. All 160 dilations were performed using a TTS Boston Scientific Rigiflex balloon.
Only endoscopy group
Twenty patients with a mean age of 39.4 years (range 19 to 63 years; 55% women), who were treated only by endoscopic dilation, had a mean CD disease duration of 12.5 years (11-18 years). 35% were smokers. 10% of stenoses were located in the duodenum, 50% in the ileum (Figure 1).
Figure 1.
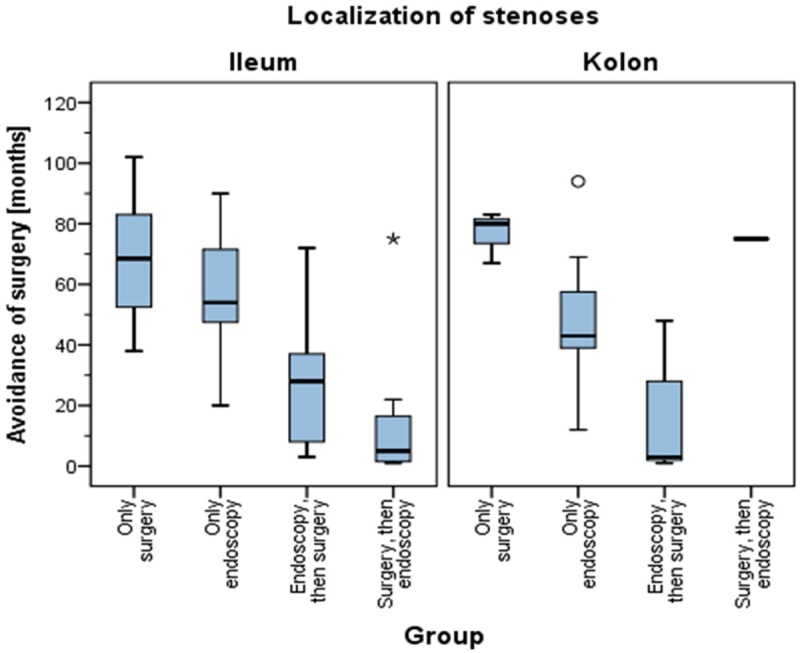
Localization of stenosis.
55% of the patients had previous surgery: 64% an ileocoecal resection; 18% a right hemicolectomy; subtotal colectomy at 9%. The stenosis developed in 25% at the site of anastomosis (Figure 2). 75% had one stenosis, 25% had 2 stenoses.
Figure 2.
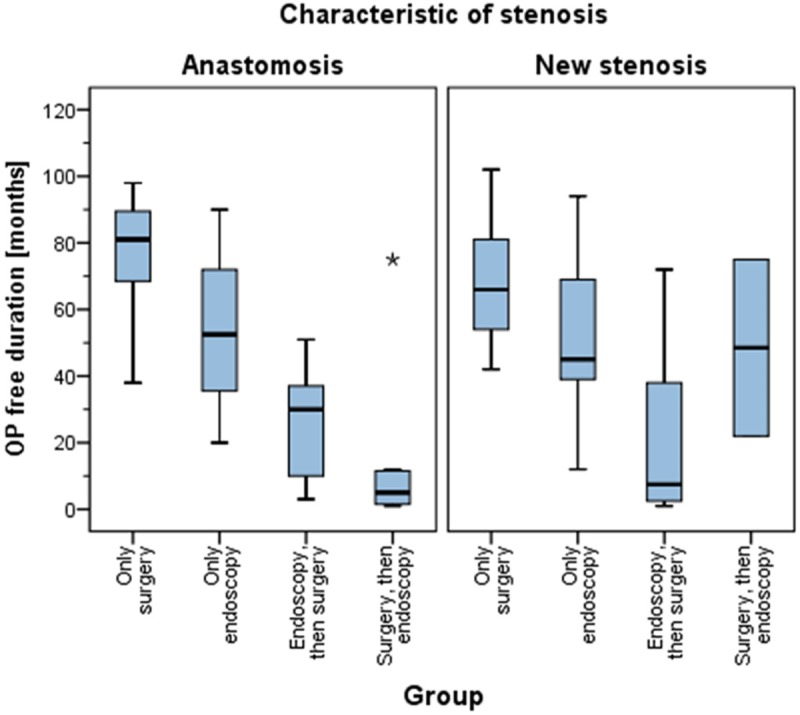
Characteristic of stenosis (anastomosis vs. De-novo stenosis).
The diameter of TTS balloon was 16 mm in median (range 10-20 mm), 100% passage of endoscope after dilation. The average stenosis length in this group was 3 cm (range 2-4 cm, P = 0.676); the median operation-free time was 52 months (range 39-71 months, P = 0.839) and symptoms-free time of 21 months (range 5-44 months, P = 0.336) (Figure 3).
Figure 3.
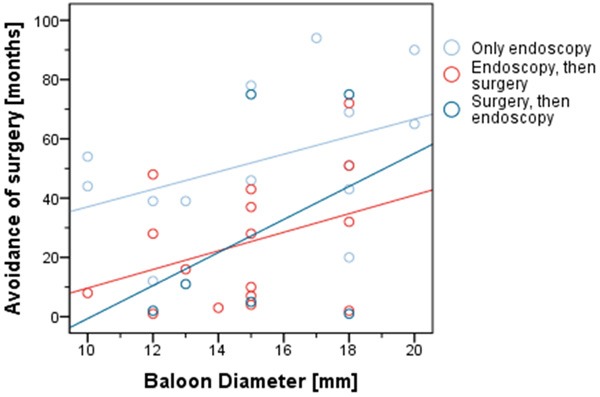
Correlation of surgery-free time to the diameter of TTS balloon.
The length of 2 stenoses was in average 5 cm (3-8 cm, P = 0.119) with surgery-free time of 54 months (19-76 months, P = 0.723) and symptoms-free time of 8 months (4-49 months, P = 0.921). The second balloon dilation was performed in average after 6.5 months (range 3 to 15.5 months); the third after 10.5 months (range 3-16 months), the fourth after 5 months (range 2-6 months). 30% of the patients received immunosuppressants (cortisone, AZA or 6-MP), 35% received 5-ASA, 30% were taking no medication; 3% received infliximab. In 3 cases (15%) the medication remained unchanged after balloon dilation and in 17 (85%) cases the therapy was intensified.
At the time of endoscopic balloon dilation 45% of the patients had accordingly to HBI score mild, 50% moderate disease activity; 5% were in remission (Figure 4). At the end of follow-up period 15% were in remission, 55% had mild and 40% moderate clinical activity.
Figure 4.
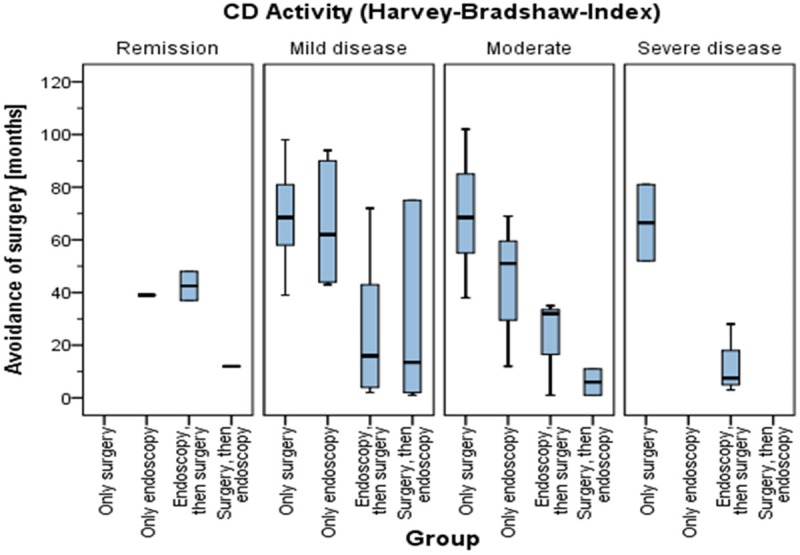
The correlation the disease activity (HBI) to the surgery-free time.
Only surgery group
The group consisted of 37 patients, aged 22 to 83 years (mean 44.63 years), 55% women. The duration of CD on average was 11 years (1-20 years). 61% were admitted due to acute intestinal obstruction. 8% of the stenoses were located in the jejunum, 84% in ileum. 50% had previous CD-related operations. 74% underwent an ileocoecal resection; 16% a right hemicolectomy. The stenosis developed in 29% at the site of the anastomosis. 68% patients had one stenosis, 18% 2-3 stenoses, 13% had more than 3 stenoses. 66% patients had an inflammatory stenosis. 67% patients received an open laparotomy. The stenoses in this group were in average 7 cm of length (4-11 cm, P = 0.418) with the median surgery-free time of 69 months (55-83 months, P = 0.850), the symptoms- free time of 68 months (55-83 months, P = 0.911). Four patients were operated during the follow-up period 2 times with the surgery-free time of 64 months (range 58-76 months). Patients with 2-3 stenoses had a length of stenosis in average of 5 cm (3-10 cm), with surgery- and symptoms-free duration of 69 months (42-86 months, P = 0.908 and P = 0.850, respectively). 44.7% were receiving immunosuppressants (cortisone, AZA or 6-MP), 23.4% received 5-ASA, and 28.9% were taking no medications.
47% had at the time of surgery accordingly to HBI mild disease, 48% moderate, 2 (5%)-severely active disease. At the end of follow-up (early 2010) 19 patients (50%) had mild and 18 (47%) moderate activity of CD, 3% were in remission (Figure 4).
The group of patients who underwent surgical treatment first, and then developed strictures again, that were dilated using TTS balloon, 89% had one stenosis, 11% 2-3 stenoses. In patients with one stenosis, the stenosis length in average was 4 cm (3-8 cm, P = 0.508), the surgery-free time of 22 months (5-41 months, P = 0.673), the symptoms-free time of 4 months (3-14 months, P = 0.777). In two patients with 2-3 stenoses, the stenoses were 6 cm and 8 cm in length, P = 0.508, the surgery-free time was 2 and 37 months (P = 0.673), the symptoms-free time 2 and 12 months, P = 0.777.
Smoking behaviour
In the group of endoscopic dilation at the time of treatment, 7 patients (35%) were smokers, 9 (45%) non-smokers; 4 patients (20%) had unknown smoking habits. Of the patients who required surgery during the course after balloon dilation, 6 (33%) smokers were at the time of treatment, 10 (56%) non-smokers.
Previous operations
63.6% of all the patients have had an operation previously. In average, a first balloon dilation was performed after 8.5 years (range 5.5 to 16 years) of surgery. A following operation was done after 11 years (range 6-14) of the previous operation. The most common operation in the entire patient population was the ileocoecal resection (66.1%), followed by right-sided hemicolectomy (21.4%).
Influence of stenosis characteristic (anastomosis or new stenosis)
In the total study cohort, 39.8% of patients had their stenosis at the anastomosis site (Figure 2). The both groups of patients with surgical or endoscopic therapy show similar number of anastomotic strictures: 29% for operated patients, 25% patients with endoscopic balloon dilation.
Patients who were treated only surgically, had an anastomotic stenosis in average of 4 cm in length (3.5 to 6 cm, P = 0.055) with surgically stenosis-free time of 81 months (range 68-92 months). The newly formed stenosis was in average 8 cm of length (range 4-15 cm, P = 0.054) with an operation-free period of 66 months (range 53-82 months, P = 0.101) and a symptoms-free time of 62 months (range 53-82 months, P = 0.088).
Patients who were treated only endoscopically, had an average stenosis at the anastomosis of 2 cm length (range 1-10 cm, P = 0.676) with operation-free period of 52 months (range 28-81 months, P = 0.839) and stenosis-free time of 51 months (range 4.5 to 60 months, P = 0.336). The newly formed stenosis were in average 3 cm long (2-4 cm, P = 0.676) with surgery- free period of 45 months (39-71 months, P = 0.839) and stenosis-free period of 12 months (4-23 months, P = 0.336).
Patients who were treated primarily by endoscopy and then had surgery, had an anastomotic stenosis at 4 cm in average (range 2.5-8 cm, P = 0.536) with surgery-free period of 30 months (range 8.5 to 39 months, P = 0.315) and stenosis-free time of 4 months (range 3-13 months, P = 0.897). The newly formed stenosis were also on average 4 cm (range 4-8 cm, P = 0.536) with op-free period of 7.5 months (range 2-43 months) (P = 0.315) and stenosis-free time of 5 months (range 2-15 months, P = 0.897).
Patients who were treated primarily with surgery and then underwent endoscopy, had an average length of stenosis at the anastomosis of 2 cm (range, 1-8 cm, P = 0.889) with surgery-free period of 5 months (range 1-12 months, P = 0.111) and symptoms-free period of 2 months (range 1-16 months, P = 0.727). The newly formed stenosis was 3.5 cm in average (range 1.5 to 4 cm, P = 0.889) with surgery-free period of 49 months (range 16.5 to 56.5 months, P = 0.111) and symptoms- free period of 3 months (range 3-5 months, P = 0.727).
Inflammatory vs. fibrotic strictures
In the group of surgically treated patients 37% of the stenoses were fibrotic (Figure 5). Of the endoscopically treated stenoses, 55% of the patients showed inflammation signs at the site of stenosis, appeared upon dilation. The inflammatory stenoses with 7.5 cm in average (range 5-15 cm) were longer than the fibrotic stenosis with average length of 4 cm (range 3-7 cm, P = 0.044). The mean surgery-free period for inflammatory stenoses was 46 months (range 20-69 months, P = 0.805), symptoms- free time of 10 months in average (range 4-21 months, P = 0.237). The fibrotic strictures showed operation-free period of 51 months (range 39-78 months, P = 0.805), and symptoms-free time of 5 months in average (range 5-63 months, P = 0.237).
Figure 5.
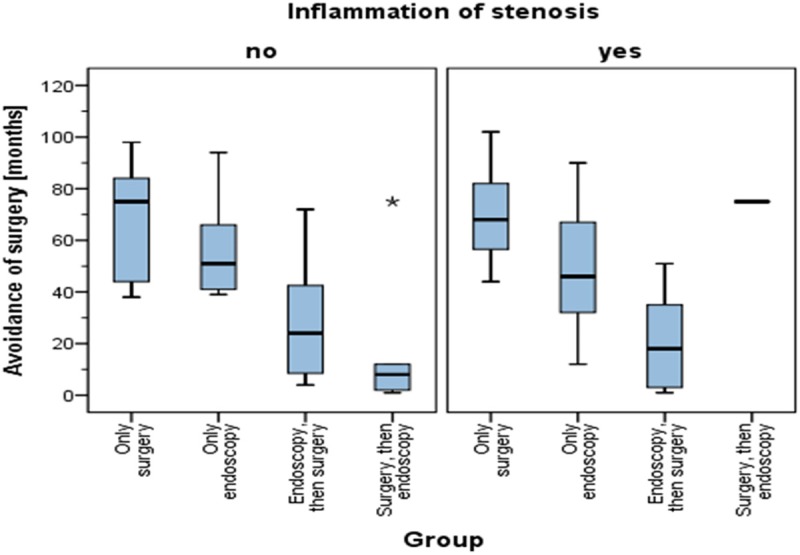
Avoidance of surgery (months) in inflammatory vs. fibrotic strictures.
In the group of endoscopy, followed by surgery, stenoses with signs of inflammation had an average length of 5 cm (range 3 to 8.5 cm, P = 0.428), operation-free time was 18 months (range 3-37 months, P = 0.315), symptoms-free time of 3 months (range 2-10 months, P = 0.122). The fibrotic strictures were 4cm long (3-5 cm, P = 0.428), the operation-free period 24 months (8-45 months, P = 0.315), the symptoms-free time of 7 months (4-15 months, P = 0,122).
The role of prednisolone injection
In all endoscopically treated patients 14 (30%) received mucosal prednisolone injection upon dilation. The operation-free time was 43 months (range 30-49 months, P = 0.112), the symptoms-free time 6 months (range 5-33 months, P = 0.775, Figure 6). The group who did not receive the prednisolone injection showed a surgery-free period of 65 months (42-84 months, P = 0.112), the symptoms-free time 12 months (range 3.5 to 48 months, P = 0.775).
Figure 6.
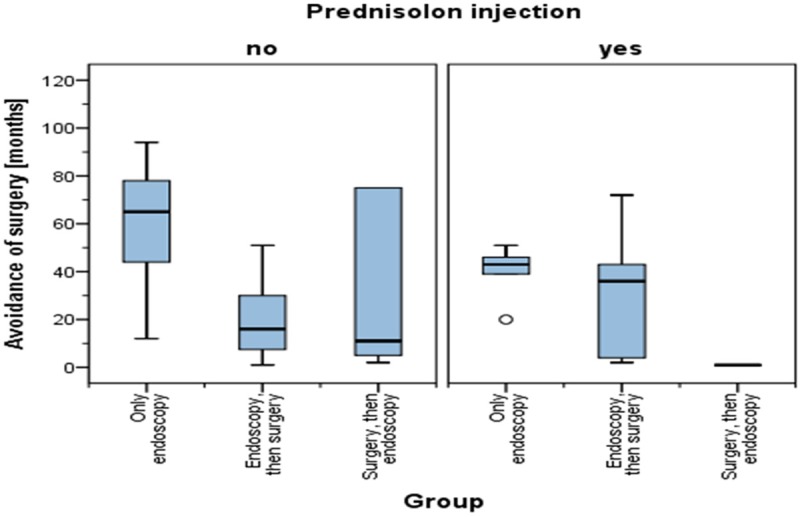
The role of prednisolone injection after the endoscopic dilation in terms of surgery-free time.
Medication
In the whole cohort of patients, 24 (28%) did not take any specific CD medication. The most common reason for this was a spontaneous discontinuation of medication after achieving subjective remission. Anti-inflammatory drugs (e.g. mesalazine) were taken by 22 (25%) of the patients; immunosuppressive drugs (corticosteroids, AZA, MTX) took 39 (45%) patients. Only one patient (1%) received infliximab that time. In 61% cases the medication remained unchanged after stenosis therapy.
In the group of endoscopically treated patients, medication remained unchanged in 3 patients (15%); in 17 (85%) cases the therapy was intensified. CD patients without specific medication had a surgery-free period of 72 months (range 52-93 months), symptoms-free period of 32 months (range 4-57 months). Patients with anti-inflammatory therapy remained after balloon dilation 55 months (range 42-71 months) without surgery and 12 months (range 5-41 months) symptoms-free (data not shown). Patients treated with immunosuppressants had a surgery-free period of 39 months (range 20-46 months) and a stenosis-free period of 10 months (range 2-23 months).
Disease activity
In the group of patients treated only by surgery 18 (47%) had mild and 47% moderate active disease accordingly to HBI, 2 (6%) severe disease (Figure 4). The surgery- and symptoms-free time in this group were in average 69 months (range 56-82 months) for mild active disease, patients with moderate activity showed 69 months (range 55-85 months); and for severe activity 67 months (range 39-72 months).
In the group of only endoscopically treated patients 9 (45%) had mild and 10 (50%) moderate disease activity; 1 patient was in remission. The surgery-free period in patients with mild CD was 62 months in average (range 44-91 months), patients of moderate disease activity showed 51 months (20-65 months). The symptoms-free time was similar for both groups: 12 months for the mild activity and 13.5 months for moderate activity.
Surgical treatment: planed vs. emergency operation
In 14 patients (39%) the operation was planned, 22 (61%) were operated on an emergency basis, of which 5 (14%) as a complication of an endoscopic procedure. The average length of stenosis by planed operation was 5 cm (range 4-10 cm, P = 0.481) with surgery- and symptoms-free time of 65 months (range 52-84 months, P = 0.761 and 0.860, respectively). The length of stenosis of the patients, who were operated on emergency basis was 8 cm in average (range 4-15 cm, P = 0.481) with an operation-free period of 69 months (range 53-83 months, P = 0.761) and a stenosis-free period of 68 months (range 53 -83 months, P = 0.860).
Discussion
The long term success of endoscopic balloon dilation as well as the surgery of CD strictures depends on many factors. In our patients cohort, a single balloon dilation was sufficient enough for 9 patients to remain 49 months (P = 0.723) surgery-free; yet other patients needed further dilations. In other patients up to five dilations were required. The median interval between the first and the second dilation was 6.5 months, between the second and third dilation 10.5 months. Further dilations were required after a much shorter period of 4-5 months. In our study, the inflammation at the stenosis site did not affect the long-term success rate (P = 0.805 for surgery-free period and P = 0.237 for stenosis-free time).
By dividing our patients accordingly to their medical charts into four groups, we were able to evaluate and compare both endoscopic and surgical therapy in terms of long-term outcome. In the group of patients with only endoscopic therapy, symptoms-free time was in general shorter compared to the group of only surgical therapy.
We described that stenoses in the surgical group with an average length of 6.5 cm were as expected longer, as compared to the endoscopic group (3.0 cm in average). Also the inflammatory stenoses with 7.5 cm (range 5-15 cm) were significantly longer than the fibrotic stenoses with average length of 4 cm (range 3-7 cm). The statistical difference in terms of surgery- and stenosis-free time with P = 0.044 was significant between these different characteristics of stenoses. This result shows the effectiveness of endoscopic balloon dilation of fibrotic stenosis < 4 cm and correlates well to the study data of Froehlich at al [4].
Stienecker reported that only 20% of patients with stenosis required an operation after 81 months [24]. Hassan et al reported a long-term success rate of 58% over 33 months [7]. In the surgical group, the surgery-free time was 69 months in average. In this group, 16 (35%) patients developed new stenoses; four patients (8.7%) underwent surgery for the second time, and in 12 patients (24%) the stenosis was treated endoscopically. These results are comparable with other studies, e.g. Thienpont reported 76% of surgery-free time after a follow-up of 5.8 years [26]. About 20-60% of patients had a clinical relapse in the first year after surgery, and 15-50% needed reoperation within 5 years [26]. In our patient cohort 35 patients were operated on an emergency basis, in 25 patients the operation was scheduled.
The development of new strictures in our patients’ cohort was not only due to recurrent character of CD itself, but also as a consequence of spontaneous withdrawal of the medication, upon reaching a subjective remission. From the literature it is known that about 60% of the patients develop strictures or fistulas in the course of their disease; 54% of these complications appear within 30 days after withdrawal of medication [9].
In many cases the form of CD is of importance. Here, one must distinguish between fibrotic and inflammatory strictures [4]. Endoscopic dilation is mostly successful in fibrotic strictures. But there are also some factors, influencing the course of the disease such as medication or smoking [23]. If the patient is poorly controlled with medication, the new stenosis might develop after the operation because of persistent mucosal inflammation [18].
Unfortunately, the authors could not find any prospective randomized studies, which compare different dilation techniques and the influence of various factors on the long-term success; also the studies evaluating influence of prednisolone injection into the stenosis upon balloon dilation showed different results. Some studies could not find any significant difference between patients with and without steroid injection. Others report a better outcome after prednisolone injection [5]. In our patient population 30% of the patients received prednisolone injection; the data showed no statistical significance (surgery-free time with P = 0.112 and symptoms-free time with P = 0.775).
The effect on long-term success of endoscopic dilation of CD stenoses has been analyzed in some other studies. Hofmann et al found that smoking and the presence of ulcers are at the stenosis site predictsa worse outcome of balloon dilation [8]. Sabaté et al described nicotine consumption as a positive predictive factor for surgery [20]. Seksik showed in his study that the risk of stenosis development increases with dose of nicotine, e.g. the smokers with less than 15 cigarettes a day have about 40% of risk of endoscopic recurrence after surgery; in heavy smokers is the risk about 75% [22].
The damaging effect of cigarette smoking in CD is associated with a higher risk of developing CD, an increase in its clinical activity, a lower quality of life, more frequent complications, an increased need for immunosuppressive drugs, and faster recurrences after surgery [22]. Studies have shown that smokers tend to have a complicated course of disease, with increased incidence of complications and penetrating strictures. Also there are higher recurrence rates compared to non-smokers [3]. But reducing the number of cigarettes does not improve the disease course alone; even passive smoking contributes to the rate of relapse and complications.
In our patients, data about nicotine consumption were only available for the endoscopically treated patients. 7 patients (35%) were smokers, 9 patients (45%) non-smokers; in 4 patients (20%) smoking habit was unknown. Of the patients who were initially treated endoscopically and could not avoid surgery, 6 (33%) were smokers and 10 (56%) non-smokers. The proportion of smokers was similar in both groups. Due to the high percentage of patients whose smoking behavior was unknown, no definitive statement can be made in terms of influence of smoking on the long-term outcome of CD strictures. Given the known harmful effect of nicotine, the nicotine abstinence should be recommended in general [16].
The medication has an additional effect on the symptoms-free period after the balloon dilation or surgery. The main goal of drug therapy is induction and maintenance of remission. The choice of appropriate medication depends on many factors: disease activity, localization, concomitant diseases, response to therapy etc.
Reinisch et al could demonstrate in a randomized double-blind study, that administration of azathioprine was more effective in reducing the rate of endoscopic and clinical relapse, as compared to mesalazine [17]. Authors could not find any prospective randomized studies that examined the role of drug therapy in the prevention of relapse after endoscopic balloon dilation. But there are some retrospective studies, with results similar to our study, showing that the established medical therapy in addition to other factors ameliorate the long-term success of endoscopic therapy. Our analyzes showed that patients who received anti-inflammatory or immunosuppressive therapy, had a better outcome as compared to the patients who received no drugs or withdrew the medication.
Louis et al describes a fibrostenotic phenotype of CD, which is found in about 10% of newly diagnosed and 20%-30% of patients after 10 years after the diagnosis [12,13]. From this point of view, the patients who withdrew their medication upon achieving clinical remission, and managed to stay symptom-free at the end of the follow-up time, had either very low activity of the disease or mainly fibrostenotic phenotype [12,13].
Conclusion
Intestinal stenoses are common complication of CD, associated with increased morbidity in affected patients [21]. About 60% of all CD patients develop strictures or fistulas during the course of the disease. The cumulative likelihood of resection for CD patients is 10% per year, 70-90% over the course of the disease. Around 70% of the patients develop mucosal inflammation within the first postoperative year, 20-60% of the patients show clinical relapse; and 15-50% might need re-operation within 5 years [15]. The endoscopic balloon dilation of CD strictures is most effective by short segment stenosis of fibrotic phenotype, where in our study 53% of the patients remained surgery-free with median follow-up of 49 months after a single dilation. Repeated dilation is a valid option, but the length of the symptom-free interval will be the main parameter used to decide between surgery and re-do endoscopic dilation [30]. Furthermore, we could show that de-novo inflammatory stenoses are associated with an increased risk of complications. This study cannot offer at the moment any statistically valid treatment algorithm. The optimal strategy for the stenosis has to be found individually, taken into account the medical history, medication and clinical risk factors of each patient in general. Hereby, indication for intervention should be discussed interdisciplinary in complex cases.
Disclosure of conflict of interest
None.
Abbreviations
- CD
Crohn’s disease
- H-M
Heineke-Mikulicz
- TTS
through the scope
References
- 1.Atreya I, Atreya R, Neurath MF. NF-kappaB in inflammatory bowel disease. J Intern Med. 2008;263:591–596. doi: 10.1111/j.1365-2796.2008.01953.x. [DOI] [PubMed] [Google Scholar]
- 2.Dasari BV, McKay D, Gardiner K. Laparoscopic versus Open surgery for small bowel Crohn’s disease. Cochrane Database Syst Rev. 2011:CD006956. doi: 10.1002/14651858.CD006956.pub2. [DOI] [PubMed] [Google Scholar]
- 3.Engel MA, Neurath MF. New pathophysiological insights and modern treatment of IBD. J Gastroenterol. 2010;45:571–83. doi: 10.1007/s00535-010-0219-3. [DOI] [PubMed] [Google Scholar]
- 4.Froehlich F, Juillerat P, Mottet C, Pittet V, Felley C, Vader JP, Gonvers JJ, Michetti P. Fibrostenotic Crohn’s disease. Digestion. 2007;76:113–115. doi: 10.1159/000111025. [DOI] [PubMed] [Google Scholar]
- 5.Gelbmann CM, Rogler G, Gross V, Gierend M, Bregenzer N, Andus T, Scholmerich J. Prior bowel resections, perianal disease, and a high initial Crohn’s disease activity index are associated with corticosteroid resistance in active Crohn’s disease. Am J Gastroenterol. 2002;97:1438–1445. doi: 10.1111/j.1572-0241.2002.05685.x. [DOI] [PubMed] [Google Scholar]
- 6.Ghosh N, Chaki R, Mandal V, Lin GD, Mandal SC. Mechanisms and efficacy of immunobiologic therapies for inflammatory bowel diseases. Int Rev Immunol. 2010;29:4–37. doi: 10.3109/08830180903437212. [DOI] [PubMed] [Google Scholar]
- 7.Hassan C, Zullo A, De Francesco V, Ierardi E, Giustini M, Pitidis A, Taggi F, Winn S, Morini S. Systematic review: Endoscopic dilatation in Crohn’s disease. Aliment Pharmacol Ther. 2007;26:1457–1464. doi: 10.1111/j.1365-2036.2007.03532.x. [DOI] [PubMed] [Google Scholar]
- 8.Hoffmann JC, Heller F, Faiss S, von Lampe B, Kroesen AJ, Wahnschaffe U, Schulzke JD, Zeitz M, Bojarski C. Through the endoscope balloon dilation of ileocolonic strictures: prognostic factors, complications, and effectiveness. Int J Colorectal Dis. 2008;23:689–696. doi: 10.1007/s00384-008-0461-9. [DOI] [PubMed] [Google Scholar]
- 9.Kessler H, Mudter J, Hohenberger W. Recent results of laparoscopic surgery in inflammatory bowel disease. World J Gastroenterol. 2011;17:1116–1125. doi: 10.3748/wjg.v17.i9.1116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kiesslich R, Neurath MF. What new endoscopic imaging modalities will become important in the diagnosis of IBD? Inflamm Bowel Dis. 2008;14(Suppl 2):S172–176. doi: 10.1002/ibd.20715. [DOI] [PubMed] [Google Scholar]
- 11.Lee EC, Papaioannou N. Minimal surgery for chronic obstruction in patients with extensive or universal Crohn’s disease. Ann R Coll Surg Engl. 1982;64:229–233. [PMC free article] [PubMed] [Google Scholar]
- 12.Louis E, Reenaers C, Belaiche J. Does the behavior of Crohn’s disease change over time? Inflamm Bowel Dis. 2008;14(Suppl 2):S54–55. doi: 10.1002/ibd.20561. [DOI] [PubMed] [Google Scholar]
- 13.Louis E, Reenaers C, Belaiche J. Does the phenotype at diagnosis (e.g., fibrostenosing, inflammatory, perforating) predict the course of Crohn’s disease? Inflamm Bowel Dis. 2008;14(Suppl 2):S59–60. doi: 10.1002/ibd.20559. [DOI] [PubMed] [Google Scholar]
- 14.Mudter J, Neurath MF. Insight into Crohn’s disease pathomorphology. Abdom Imaging. 2012;37:921–926. doi: 10.1007/s00261-012-9885-3. [DOI] [PubMed] [Google Scholar]
- 15.Mueller T, Rieder B, Bechtner G, Pfeiffer A. The response of Crohn’s strictures to endoscopic balloon dilation. Aliment Pharmacol Ther. 2010;31:634–639. doi: 10.1111/j.1365-2036.2009.04225.x. [DOI] [PubMed] [Google Scholar]
- 16.Nielsen OH, Bjerrum JT, Csillag C, Nielsen FC, Olsen J. Influence of smoking on colonic gene expression profile in Crohn’s disease. PLoS One. 2009;4:e6210. doi: 10.1371/journal.pone.0006210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Reinisch W, Angelberger S, Petritsch W, Shonova O, Lukas M, Bar-Meir S, Teml A, Schaeffeler E, Schwab M, Dilger K, Greinwald R, Mueller R, Stange EF, Herrlinger KR. Azathioprine versus mesalazine for prevention of postoperative clinical recurrence in patients with Crohn’s disease with endoscopic recurrence: efficacy and safety results of a randomised, double-blind, double-dummy, multicentre trial. Gut. 2010;59:752–759. doi: 10.1136/gut.2009.194159. [DOI] [PubMed] [Google Scholar]
- 18.Reinisch W, Stange EF. Efficacy of azathioprine versus mesalazine in postoperative Crohn’s disease-the authors’ response. Gut. 2011;60:739–740. doi: 10.1136/gut.2010.226928. [DOI] [PubMed] [Google Scholar]
- 19.Rutgeerts P, Geboes K, Vantrappen G, Beyls J, Kerremans R, Hiele M. Predictability of the postoperative course of Crohn’s disease. Gastroenterology. 1990;99:956–963. doi: 10.1016/0016-5085(90)90613-6. [DOI] [PubMed] [Google Scholar]
- 20.Sabate JM, Villarejo J, Bouhnik Y, Allez M, Gornet JM, Vahedi K, Modigliani R, Lemann M. Hydrostatic balloon dilatation of Crohn’s strictures. Aliment Pharmacol Ther. 2003;18:409–413. doi: 10.1046/j.1365-2036.2003.01715.x. [DOI] [PubMed] [Google Scholar]
- 21.Saunders BP, Brown GJ, Lemann M, Rutgeerts P. Balloon dilation of ileocolonic strictures in Crohn’s disease. Endoscopy. 2004;36:1001–1007. doi: 10.1055/s-2004-825962. [DOI] [PubMed] [Google Scholar]
- 22.Seksik P, Nion-Larmurier I, Sokol H, Beaugerie L, Cosnes J. Effects of light smoking consumption on the clinical course of Crohn’s disease. Inflamm Bowel Dis. 2009;15:734–741. doi: 10.1002/ibd.20828. [DOI] [PubMed] [Google Scholar]
- 23.Sokol H, Seksik P, Nion-Larmurier I, Vienne A, Beaugerie L, Cosnes J. Current smoking, not duration of remission, delays Crohn’s disease relapse following azathioprine withdrawal. Inflamm Bowel Dis. 2010;16:362–363. doi: 10.1002/ibd.20981. [DOI] [PubMed] [Google Scholar]
- 24.Stienecker K, Gleichmann D, Neumayer U, Glaser HJ, Tonus C. Long-term results of endoscopic balloon dilatation of lower gastrointestinal tract strictures in Crohn’s disease: a prospective study. World J Gastroenterol. 2009;15:2623–2627. doi: 10.3748/wjg.15.2623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Swaminath A, Lichtiger S. Dilation of colonic strictures by intralesional injection of infliximab in patients with Crohn’s colitis. Inflamm Bowel Dis. 2008;14:213–216. doi: 10.1002/ibd.20318. [DOI] [PubMed] [Google Scholar]
- 26.Thienpont C, D’Hoore A, Vermeire S, Demedts I, Bisschops R, Coremans G, Rutgeerts P, Van Assche G. Long-term outcome of endoscopic dilatation in patients with Crohn’s disease is not affected by disease activity or medical therapy. Gut. 2010;59:320–324. doi: 10.1136/gut.2009.180182. [DOI] [PubMed] [Google Scholar]
- 27.Tichansky D, Cagir B, Yoo E, Marcus SM, Fry RD. Strictureplasty for Crohn’s disease: meta-analysis. Dis Colon Rectum. 2000;43:911–919. doi: 10.1007/BF02237350. [DOI] [PubMed] [Google Scholar]
- 28.Tonelli F, Ficari F. Strictureplasty in Crohn’s disease: surgical option. Dis Colon Rectum. 2000;43:920–926. doi: 10.1007/BF02237351. [DOI] [PubMed] [Google Scholar]
- 29.Van Assche G, Vermeire S, Rutgeerts P. Endoscopic therapy of strictures in Crohn’s disease. Inflamm Bowel Dis. 2007;13:356–358. doi: 10.1002/ibd.20091. discussion 362-353. [DOI] [PubMed] [Google Scholar]
- 30.Van Assche G, Vermeire S, Rutgeerts P. What can we expect from endoscopic dilation of the stenotic tract in Crohn’s disease? Inflamm Bowel Dis. 2008;14(Suppl 2):S275–276. doi: 10.1002/ibd.20648. [DOI] [PubMed] [Google Scholar]
- 31.Van Assche G, Vermeire S, Rutgeerts P. The potential for disease modification in Crohn’s disease. Nat Rev Gastroenterol Hepatol. 2010;7:79–85. doi: 10.1038/nrgastro.2009.220. [DOI] [PubMed] [Google Scholar]
- 32.Vermeire S, van Assche G, Rutgeerts P. Review article: Altering the natural history of Crohn’s disease--evidence for and against current therapies. Aliment Pharmacol Ther. 2007;25:3–12. doi: 10.1111/j.1365-2036.2006.03134.x. [DOI] [PubMed] [Google Scholar]
- 33.Wibmer AG, Kroesen AJ, Grone J, Buhr HJ, Ritz JP. Comparison of strictureplasty and endoscopic balloon dilatation for stricturing Crohn’s disease--review of the literature. Int J Colorectal Dis. 2010;25:1149–1157. doi: 10.1007/s00384-010-1010-x. [DOI] [PubMed] [Google Scholar]


