Introduction
Measles remains a significant cause of childhood morbidity and mortality. Hallmark of the disease is a generalized immune suppression that can last for several weeks to months after resolution of measles virus (MV) infection [1]–[3], resulting in increased susceptibility to opportunistic infections [4]–[7]. At the same time, measles is associated with immune activation and induces strong MV-specific immune responses that confer lifelong immunity [8]. This contradiction is known as the “measles paradox'. Although measles-associated immune suppression has been a subject of study since the beginning of the 20th century [9], the importance of possible underlying mechanisms remains disputed.
The Immune System as “Viral Friend”
From the perspective of MV, cells of the immune system are both friend and foe. MV efficiently replicates in cells of the immune system, especially during the initial stages of the infection [10], [11]. However, the virus preferentially infects specific subsets of lymphocytes and dendritic cells (DCs). The relative susceptibility of these cells to MV infection is governed by their expression level of the cellular receptor CD150 [11]–[14]. Memory T-lymphocytes, which express CD150, are preferentially infected [13], [14]. In secondary and tertiary lymphoid tissues, the virus also replicates to high levels in follicular and marginal zone B-lymphocytes [10], [11], [13]. DCs can also be infected by MV [11], [15]–[17] and may serve as initial target cells [18], [19].
The Immune System as “Viral Foe”
In the majority of cases MV infection is self-limiting and induces strong virus-specific cellular and humoral immune responses resulting in lifelong immunity [20]. Virus neutralizing antibodies are an important correlate of protection against MV infection, but cytotoxic T-lymphocytes are crucial for clearance of infected cells [21]–[23]. Resolution of MV infection is associated with increased lymphoproliferation [8], [24] and enlargement of lymph nodes [13]. Thus, the immune system efficiently restricts MV replication and clears MV-infected cells.
Mechanisms of Measles Immune Suppression
Measles is associated with lymphopenia [25] and extensive depletion of lymphocytes from lymphoid tissues [13], [26], [27]. However, lymphocyte numbers return to normal within a week after clinical symptoms of measles have disappeared, while measles immune suppression extends for several weeks to months. Therefore, immune cell depletion was initially dismissed as a mechanism for measles immune suppression [3]. Alternative mechanisms have been proposed to explain measles-associated immune suppression, as summarized in Table 1. However, the relevance of these observations to enhanced susceptibility to opportunistic infections in vivo remains unclear.
Table 1. Reported mechanisms of measles immune suppression.
| Functional Impairment | |
| Mechanism | References |
| Suppression of lymphocyte proliferation | [41]–[45] |
| Altered cytokine profiles | [42], [43], [46]–[50] |
| Lymphoproliferation defect due to MV-infected DC | [15], [17], [51] |
| Immune modulation mediated by viral proteins | [44], [52]–[56] |
| Modulation of cell membrane components | [57], [58] |
| Inhibition of hematopoiesis | [59], [60] |
Is Suppressed Lymphoproliferation Important?
Reduced responsiveness of peripheral blood mononuclear cells to stimulation with mitogens in vitro has been considered an important mechanism underlying measles-associated immune suppression. Although the observations in these studies are not disputed, we find it difficult to reconcile this in vitro observation with the observed immune activation in vivo. Measles results in dramatic expansion of MV-specific lymphocytes followed by resolution of viremia and lymphopenia [8], [25], [28]. We recently demonstrated extensive lymphoproliferation in lymphoid tissues early after MV infection in vivo [13]. Thus, there is no evidence of suppressed lymphoproliferative responses, at least towards MV, in vivo. Rather, we believe that alterations in the composition of the peripheral lymphocyte populations before and after measles may explain these in vitro observations [13].
Do Dendritic Dells Play a Crucial Role?
DC subsets have been shown susceptible to MV infection in vitro [15]–[17] and in nonhuman primates in vivo [11], [19]. Therefore, it is likely that infection, depletion, or functional modulation of DCs contributes to measles-associated immune suppression. Nevertheless, antigen presentation does not seem to be impaired in vivo, as strong MV-specific immune responses develop during the acute stage of the disease.
Measles Damages the Respiratory Epithelium
Whereas MV targets CD150 to infect lymphoid and myeloid cells, the virus uses poliovirus receptor like 4 (also known as nectin-4) as an alternative cellular receptor to infect epithelial cells [29]–[31]. Whilst infection of epithelial cells contributes to viral transmission [32], MV also causes extensive epithelial damage in the respiratory tract [33], [34]. This epithelial injury may provide an opportunity for respiratory bacteria to adhere, replicate, and invade with increased efficiency [35].
Attenuated, Mild, Moderate, or Severe Morbillivirus Infections
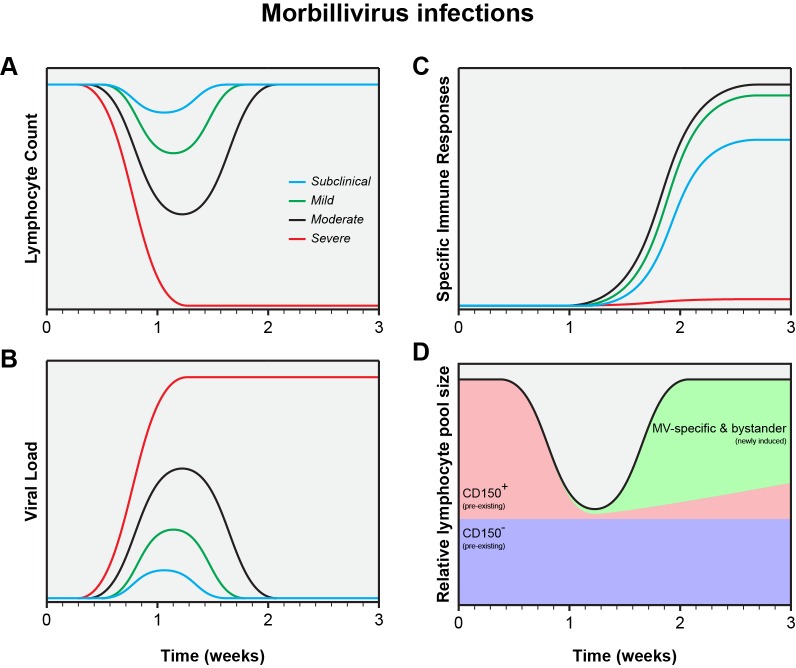
MV infections display a large variability in clinical severity, ranging from vaccination with attenuated viruses, via subclinical or mild infections, to severe disease. Closely related animal morbilliviruses may even overwhelm the immune system, resulting in functional paralysis and virtual absence of virus-specific immune responses [36]–[40]. This variation is also reflected in a wide range of levels of lymphopenia, viremia, and specific immune responses (Fig. 1A–C) [13]. Natural MV infection of the naive host will normally follow the pattern of either a mild or moderate infection as displayed in Fig. 1. Whereas mild measles results in limited depletion of pre-existing CD150+ memory lymphocytes, moderate measles is associated with infection and subsequent depletion of a large fraction of those lymphocytes (Fig. 1D). Whether this depletion is mediated by necrosis, apoptosis, pyroptosis, or cytotoxic T-cells remains to be determined, but the effect is always the same: to a varying degree, measles erases immunological memory.
Figure 1. Schematic representation of the measles paradox.
Different levels of lymphopenia (A), systemic virus loads (B), and virus-specific immune responses (C) after subclinical (blue), mild (green), moderate (black), or severe (red) morbillivirus infections. Panel D shows a model for immune suppression caused by moderate morbillivirus infection as shown in panels A, B, and C (adapted from [13]).
Future Directions: Studies in Naturally Infected Measles Patients
To improve our understanding of measles immune suppression, a transition from in vitro to in vivo studies is required. Two aspects are of crucial importance: viral tropism and depletion of immune cell subsets. We feel that it is important to characterize the phenotype of MV-infected cells during the prodromal phase of natural measles, with special emphasis on infection of DCs and memory lymphocytes. Furthermore, to address depletion of immune cell subsets, paired blood samples from children before and after measles will be required. Staining of immune cells specific for previously encountered pathogens, rather than functional assays, will allow us to distinguish between subset depletion and functional paralysis.
Conclusions
Experimental MV infections in animal models have demonstrated that percentages of infected lymphocyte subsets are higher than previously thought, especially in secondary and tertiary lymphoid tissues [11], [13]. We believe that measles immune suppression mainly results from depletion of immune cell subsets, which is masked by the rapid proliferation of MV-specific and bystander lymphocytes (Fig. 1D). This model is fully compatible with the measles paradox. Clinical studies are required to test our hypothesis that measles immune suppression is mainly a numbers game.
Acknowledgments
We thank Michael Mina, Paul Duprex, and Albert Osterhaus for critical comments to the manuscript.
Funding Statement
Measles pathogenesis studies in the macaque model were funded by the VIRGO project (grant number FES0908), ZonMw (grant number 91208012), MRC (grant number G0801001) and FNIH (grant number DUPREX09GCGH0). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Schneider-Schaulies S, Schneider-Schaulies J (2009) Measles virus-induced immunosuppression. Curr Top Microbiol Immunol 330: 243–269. [DOI] [PubMed] [Google Scholar]
- 2. Hahm B (2009) Hostile communication of measles virus with host innate immunity and dendritic cells. Curr Top Microbiol Immunol 330: 271–287. [DOI] [PubMed] [Google Scholar]
- 3. Griffin DE (2010) Measles virus-induced suppression of immune responses. Immunol Rev 236: 176–189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Beckford AP, Kaschula RO, Stephen C (1985) Factors associated with fatal cases of measles. A retrospective autopsy study. S Afr Med J 68: 858–863. [PubMed] [Google Scholar]
- 5. Akramuzzaman SM, Cutts FT, Wheeler JG, Hossain MJ (2000) Increased childhood morbidity after measles is short-term in urban Bangladesh. Am J Epidemiol 151: 723–735. [DOI] [PubMed] [Google Scholar]
- 6. Van den Hof S, Conyn-van Spaendonck MAE, van Steenbergen JE (2002) Measles epidemic in the Netherlands, 1999–2000. J Infect Dis 186: 1483–1486. [DOI] [PubMed] [Google Scholar]
- 7. Shanks GD, Lee SE, Howard A, Brundage JF (2011) Extreme mortality after first introduction of measles virus to the polynesian island of Rotuma, 1911. Am J Epidemiol 173: 1211–1222. [DOI] [PubMed] [Google Scholar]
- 8. Griffin DE, Ward BJ, Jauregui E, Johnson RT, Vaisberg A (1989) Immune activation in measles. N Engl J Med 320: 1667–1672. [DOI] [PubMed] [Google Scholar]
- 9. Von Pirquet CE (1908) Das Verhalten der kutanen Tuberkulin-reaktion während der Masern. Dtsch Med Wochenschr 34: 1297–1300. [Google Scholar]
- 10. McChesney MB, Miller CJ, Rota PA, Zhu Y, Antipa L, et al. (1997) Experimental measles I. Pathogenesis in the normal and the immunized host. Virology 233: 74–84. [DOI] [PubMed] [Google Scholar]
- 11. De Swart RL, Ludlow M, De Witte L, Yanagi Y, Van Amerongen G, et al. (2007) Predominant infection of CD150+ lymphocytes and dendritic cells during measles virus infection of macaques. PLoS Pathog 3: e178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Tatsuo H, Ono N, Tanaka K, Yanagi Y (2000) SLAM (CDw150) is a cellular receptor for measles virus. Nature 406: 893–897. [DOI] [PubMed] [Google Scholar]
- 13. De Vries RD, McQuaid S, Van Amerongen G, Yüksel S, Verburgh RJ, et al. (2012) Measles immune suppression: lessons from the macaque model. PLoS Pathog 8: e1002885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Condack C, Grivel JC, Devaux P, Margolis L, Cattaneo R (2007) Measles virus vaccine attenuation: suboptimal infection of lymphatic tissue and tropism alteration. J Infect Dis 196: 541–549. [DOI] [PubMed] [Google Scholar]
- 15. Grosjean I, Caux C, Bella C, Berger I, Wild F, et al. (1997) Measles virus infects human dendritic cells and blocks their allostimulatory properties for CD4+ T cells. J Exp Med 186: 801–812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Fugier-Vivier I, Servet-Delprat C, Rivailler P, Rissoan MC, Liu YJ, et al. (1997) Measles virus suppresses cell-mediated immunity by interfering with the survival and functions of dendritic and T cells. J Exp Med 186: 813–823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Schnorr JJ, Xanthakos S, Keikavoussi P, Kampgen E, Ter Meulen V, et al. (1997) Induction of maturation of human blood dendritic cell precursors by measles virus is associated with immmunosuppression. Proc Natl Acad Sci U S A 94: 5326–5331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Ferreira CS, Frenzke M, Leonard VH, Welstead GG, Richardson CD, et al. (2010) Measles virus infection of alveolar macrophages and dendritic cells precedes spread to lymphatic organs in transgenic mice expressing human signaling lymphocytic activation molecule (SLAM, CD150). J Virol 84: 3033–3042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Lemon K, De Vries RD, Mesman AW, McQuaid S, Van Amerongen G, et al. (2011) Early target cells of measles virus after aerosol infection of non-human primates. PLoS Pathog 7: e1001263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Moss WJ, Griffin DE (2012) Measles. Lancet 379: 153–164. [DOI] [PubMed] [Google Scholar]
- 21. Van Binnendijk RS, Poelen MCM, Kuijpers KC, Osterhaus ADME, UytdeHaag FGCM (1990) The predominance of CD8+ T cells after infection with measles virus suggests a role for CD8+ class I MHC-restricted cytotoxic T lymphocytes (CTL) in recovery from measles. J Immunol 144: 2394–2399. [PubMed] [Google Scholar]
- 22. Permar SR, Klumpp SA, Mansfield KG, Kim WK, Gorgone DA, et al. (2003) Role of CD8+ lymphocytes in control and clearance of measles virus infection of rhesus monkeys. J Virol 77: 4396–4400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. De Vries RD, Yüksel S, Osterhaus ADME, De Swart RL (2010) Specific CD8+ T-lymphocytes control dissemination of measles virus. Eur J Immunol 40: 388–395. [DOI] [PubMed] [Google Scholar]
- 24. Mongkolsapaya J, Jaye A, Callan MFC, Magnusen AF, McMichael AJ, et al. (1999) Antigen-specific expansion of cytotoxic T lymphocytes in acute measles virus infection. J Virol 73: 67–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Ryon JJ, Moss WJ, Monze M, Griffin DE (2002) Functional and phenotypic changes in circulating lymphocytes from hospitalized Zambian children with measles. Clin Diagn Lab Immunol 9: 994–1003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Finkeldey W (1931) Über Riesenzellbefunde in den Gaumenmandeln, zugleich ein Beitrag zur Histopathologie der Mandelveränderungen im Maserninkubationsstadium. Virchows Arch 281: 323–329. [Google Scholar]
- 27. Warthin AS (1931) Occurrence of numerous large giant cells in the tonsils and pharyngeal mucosa in the prodromal stage of measles. Arch Pathol 11: 864–874. [Google Scholar]
- 28. Lisse I, Samb B, Whittle H, Jensen H, Soumare M, et al. (1998) Acute and long-term changes in T-lymphocyte subsets in response to clinical and subclinical measles. A community study from rural Senegal. Scand J Infect Dis 30: 17–21. [DOI] [PubMed] [Google Scholar]
- 29. Noyce RS, Bondre DG, Ha MN, Lin LT, Sisson G, et al. (2011) Tumor cell marker PVRL4 (nectin 4) is an epithelial cell receptor for measles virus. PLoS Pathog 7: e1002240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Mühlebach MD, Mateo M, Sinn PL, Prufer S, Uhlig KM, et al. (2011) Adherens junction protein nectin-4 is the epithelial receptor for measles virus. Nature 480: 530–533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Pratakpiriya W, Seki F, Otsuki N, Sakai K, Fukuhara H, et al. (2012) Nectin4 is an epithelial cell receptor for canine distemper virus and involved in the neurovirulence. J Virol 86: 10207–10210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Racaniello V (2011) An exit strategy for measles virus. Science 334: 1650–1651. [DOI] [PubMed] [Google Scholar]
- 33. Ludlow M, Lemon K, De Vries RD, McQuaid S, Millar E, et al. (2013) Measles virus infection of epithelial cells in the macaque upper respiratory tract is mediated by sub-epithelial immune cells. J Virol 87: 4033–4042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Ludlow M, De Vries RD, Lemon K, McQuaid S, Millar E, et al. (2013) Infection of lymphoid tissues in the macaque upper respiratory tract contributes to the emergence of transmissible measles virus. J Gen Virol 94: 1933–1944. [DOI] [PubMed] [Google Scholar]
- 35. Vareille M, Kieninger E, Edwards MR, Regamey N (2011) The airway epithelium: soldier in the fight against respiratory viruses. Clin Microbiol Rev 24: 210–229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Beineke A, Puff C, Seehusen F, Baumgärtner W (2009) Pathogenesis and immunopathology of systemic and nervous canine distemper. Vet Immunol Immunopathol 127: 1–18. [DOI] [PubMed] [Google Scholar]
- 37. Nguyen DT, Ludlow M, Van Amerongen G, De Vries RD, Yüksel S, et al. (2012) Evaluation of synthetic infection-enhancing lipopeptides as adjuvants for a live-attenuated canine distemper virus vaccine administered intra-nasally to ferrets. Vaccine 30: 5073–5080. [DOI] [PubMed] [Google Scholar]
- 38. McCullough B, Krakowka S, Koestner A (1974) Experimental canine distemper virus-induced lymphoid depletion. Am J Pathol 74: 155–170. [PMC free article] [PubMed] [Google Scholar]
- 39. Von Messling V, Springfeld C, Devaux P, Cattaneo R (2003) A ferret model of canine distemper virus virulence and immunosuppression. J Virol 77: 12579–12591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Von Messling V, Milosevic D, Cattaneo R (2004) Tropism illuminated: lymphocyte-based pathways blazed by lethal morbillivirus through the host immune system. Proc Natl Acad Sci U S A 101: 14216–14421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Hirsch RL, Griffin DE, Johnson RT, Cooper SJ, Lindo de Soriano I, et al. (1984) Cellular immune responses during complicated and uncomplicated measles virus infections of man. Clin Immunol Immunopathol 31: 1–12. [DOI] [PubMed] [Google Scholar]
- 42. Ward BJ, Johnson RT, Vaisberg A, Jauregui E, Griffin DE (1991) Cytokine production in vitro and the lymphoproliferative defect of natural measles virus infection. Clin Immunol Immunopathol 61: 236–248. [DOI] [PubMed] [Google Scholar]
- 43. Griffin DE, Ward BJ (1993) Differential CD4 T cell activation in measles. J Infect Dis 168: 275–281. [DOI] [PubMed] [Google Scholar]
- 44. Schlender J, Schnorr JJ, Spielhofer P, Cathomen T, Cattaneo R, et al. (1996) Interaction of measles virus glycoproteins with the surface of uninfected peripheral blood lymphocytes induces immunosuppression in vitro. Proc Natl Acad Sci U S A 93: 13194–13199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Schnorr JJ, Seufert M, Schlender J, Borst J, Johnston ICD, et al. (1997) Cell cycle arrest rather than apoptosis is associated with measles virus contact-mediated immunosuppression in vitro. J Gen Virol 78: 3217–3226. [DOI] [PubMed] [Google Scholar]
- 46. Moussallem TM, Guedes F, Fernandes ER, Pagliari C, Lancellotti CLP, et al. (2007) Lung involvement in childhood measles: severe immune dysfunction revealed by quantitative immunohistochemistry. Hum Pathol 38: 1239–1247. [DOI] [PubMed] [Google Scholar]
- 47. Polack FP, Hoffman SJ, Moss WJ, Griffin DE (2002) Altered synthesis of interleukin-12 and type 1 and type 2 cytokines in rhesus macaques during measles and atypical measles. J Infect Dis 185: 13–19. [DOI] [PubMed] [Google Scholar]
- 48. Atabani SF, Byrnes AA, Jaye A, Kidd IM, Magnusen AF, et al. (2001) Natural measles causes prolonged suppression of interleukin-12 production. J Infect Dis 184: 1–9. [DOI] [PubMed] [Google Scholar]
- 49. Hoffman SJ, Polack FP, Hauer DA, Griffin DE (2003) Measles virus infection of rhesus macaques affects neutrophil expression of IL-12 and IL-10. Viral Immunol 16: 369–379. [DOI] [PubMed] [Google Scholar]
- 50. Karp CL, Wysocka M, Wahl LM, Ahearn JM, Cuomo PJ, et al. (1996) Mechanism of suppression of cell-mediated immunity by measles virus. Science 273: 228–231. [DOI] [PubMed] [Google Scholar]
- 51. Steineur MP, Grosjean I, Bella C, Kaiserlian D (1998) Langerhans cells are susceptible to measles virus infection and actively suppress T cell proliferation. Eur J Dermatol 8: 413–420. [PubMed] [Google Scholar]
- 52. Niewiesk S, Eisenhuth I, Fooks A, Clegg JC, Schnorr JJ, et al. (1997) Measles virus-induced immune suppression in the cotton rat (Sigmodon hispidus) model depends on viral glycoproteins. J Virol 71: 7214–7219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Avota E, Avots A, Niewiesk S, Kane LP, Bommhardt U, et al. (2001) Disruption of Akt kinase activation is important for immunosuppression induced by measles virus. Nat Med 7: 725–731. [DOI] [PubMed] [Google Scholar]
- 54. Marie JC, Saltel F, Escola JM, Jurdic P, Wild TF, et al. (2004) Cell surface delivery of the measles virus nucleoprotein: a viral strategy to induce immunosuppression. J Virol 78: 11952–11961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Kerdiles YM, Cherif B, Marie JC, Tremillon N, Blanquier B, et al. (2006) Immunomodulatory properties of morbillivirus nucleoproteins. Viral Immunol 19: 324–334. [DOI] [PubMed] [Google Scholar]
- 56. Kerdiles YM, Sellin CI, Druelle J, Horvat B (2006) Immunosuppression caused by measles virus: role of viral proteins. Rev Med Virol 16: 49–63. [DOI] [PubMed] [Google Scholar]
- 57. Gassert E, Avota E, Harms H, Krohne G, Gulbins E, et al. (2009) Induction of membrane ceramides: a novel strategy to interfere with T lymphocyte cytoskeletal reorganization in viral immunosuppression. PLoS Pathog 5: e1000623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Avota E, Schneider-Schaulies S (2014) The role of sphingomyelin breakdown in measles virus immunmodulation. Cell Physiol Biochem 34: 20–26. [DOI] [PubMed] [Google Scholar]
- 59. Manchester M, Smith KA, Eto DS, Perkin HB, Torbett BE (2002) Targeting and hematopoietic suppression of human CD34+ cells by measles virus. J Virol 76: 6636–6642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Boussaad I, Varagnolo L, Hornich V, Rieger L, Krockenberger M, et al. (2011) Wild-type measles virus interferes with short-term engraftment of human CD34+ hematopoietic progenitor cells. J Virol 85: 7710–7718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Addae MM, Komada Y, Taniguchi K, Kamiya T, Osei-Kwasi M, et al. (1998) Surface marker patterns of T cells and expression of interleukin-2 receptor in measles infection. Acta Paediatr Jpn 40: 7–13. [DOI] [PubMed] [Google Scholar]
- 62. Sullivan JL, Barry DW, Lucas SJ, Albrecht P (1975) Measles infection of human mononuclear cells. I. Acute infection of peripheral blood lymphocytes and monocytes. J Exp Med 142: 773–784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Huddlestone JR, Lampert PW, Oldstone MBA (1980) Virus-lymphocyte interactions: infection of Tg and Tm subsets by measles virus. Clin Immunol Immunopathol 15: 502–509. [DOI] [PubMed] [Google Scholar]
- 64. Ito M, Watanabe M, Ihara T, Kamiya H, Sakurai M (1997) Measles virus induces apoptotic cell death in lymphocytes activated with phorbol 12-myristate 13-acetate (PMA) plus calcium ionophore. Clin Exp Immunol 108: 266–271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Okada H, Kobune F, Sato TA, Kohama T, Takeuchi Y, et al. (2000) Extensive lymphopenia due to apoptosis of uninfected lymphocytes in acute measles patients. Arch Virol 145: 905–920. [DOI] [PubMed] [Google Scholar]
- 66. Pignata C, Fiore M, de Filippo S, Cavalcanti M, Gaetaniello L, et al. (1998) Apoptosis as a mechanism of peripheral blood mononuclear cell death after measles and varicella-zoster virus infections in children. Pediatr Res 43: 77–83. [DOI] [PubMed] [Google Scholar]
- 67. Vuorinen T, Peri P, Vainionpää R (2003) Measles virus induces apoptosis in uninfected bystander T cells and leads to granzyme B and caspase activation in peripheral blood mononuclear cell cultures. Eur J Clin Invest 33: 434–442. [DOI] [PubMed] [Google Scholar]
- 68. Servet-Delprat C, Vidalain PO, Azocar O, Le Deist F, Fischer A, et al. (2000) Consequences of Fas-mediated human dendritic cell apoptosis induced by measles virus. J Virol 74: 4387–4393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Servet-Delprat C, Vidalain PO, Bausinger H, Manie S, Le Deist F, et al. (2000) Measles virus induces abnormal differentiation of CD40 ligand-activated human dendritic cells. J Immunol 164: 1753–1760. [DOI] [PubMed] [Google Scholar]
- 70. Vidalain PO, Azocar O, Lamouille B, Astier A, Rabourdin-Combe C, et al. (2000) Measles virus induces functional TRAIL production by human dendritic cells. J Virol 74: 556–559. [DOI] [PMC free article] [PubMed] [Google Scholar]