Abstract
Background
Quality care for patients with cancer often requires access to specialty providers, but little is known about barriers to referring cancer patients for specialized care. Referral barriers may also lessen physician career satisfaction. We aimed to determine factors associated with these barriers and whether greater barriers are associated with low career satisfaction.
Methods
In this cross-sectional study, we studied 1,562 primary care physicians (PCPs) and 2,144 specialists responding to the multi-regional Cancer Care Outcomes Research and Surveillance Consortium Physician Survey. We assessed the prevalence of physician-reported barriers to referring cancer patients (restricted provider networks, pre-authorization requirements, patient inability to pay, lack of surgical sub-specialists, excessive patient travel time) for more specialized care. We averaged the five items to calculate a barrier score. We used multivariable linear regression to determine physician and practice setting characteristics associated with the barrier score, and multivariable logistic regression to analyze the association of the barrier score with physician career satisfaction.
Results
Three in five physicians reported always, usually, or sometimes encountering any barrier to cancer patient specialty referrals. In adjusted analyses of PCPs and specialists, international medical graduates, physicians practicing in solo or government-owned practices, or who had <90% patients in managed care plans had higher barrier scores than others (P<.05). High barrier scores were associated with lower physician career satisfaction among PCPs and specialists (P<.05).
Conclusions
Many physicians experience barriers to specialty referral for cancer patients. Uniform systems for providing and tracking timely referrals may enhance care and promote physician career satisfaction.
Keywords: Delivery of Health Care, Job Satisfaction, Neoplasms, Referrals and Consultation
Introduction
Quality care for patients with cancer often requires access to specialty providers. Patients who do not receive specialty care in a timely manner are more likely to have poor outcomes and report low satisfaction with care.1,2 Furthermore, impediments to specialty referral may delay treatment in patients with cancer, a disease in which timeliness can be a critical determinant of survival and quality of life.3,4 Studies have shown that patient characteristics such as financial constraints5,6 and excessive travel time7–10 are barriers to managing the cancer itself. However, little is known about physician and practice characteristics that may pose barriers to physicians in referring their cancer patients for more specialized care.
In addition, barriers to referring cancer patients to specialists may frustrate physicians caring for cancer patients. Surveys have documented that 28–53% of U.S. physicians across specialties report symptoms of burnout.11–13 We hypothesize that barriers to referring cancer patients to specialists may be associated with physician career dissatisfaction.
We assessed the prevalence of, and physician and practice characteristics associated with, physician-reported barriers to referring cancer patients for more specialized care by primary care physicians (PCPs) and specialists, and also assessed the association of referral barriers with physician-reported career satisfaction.
Methods
Study participants
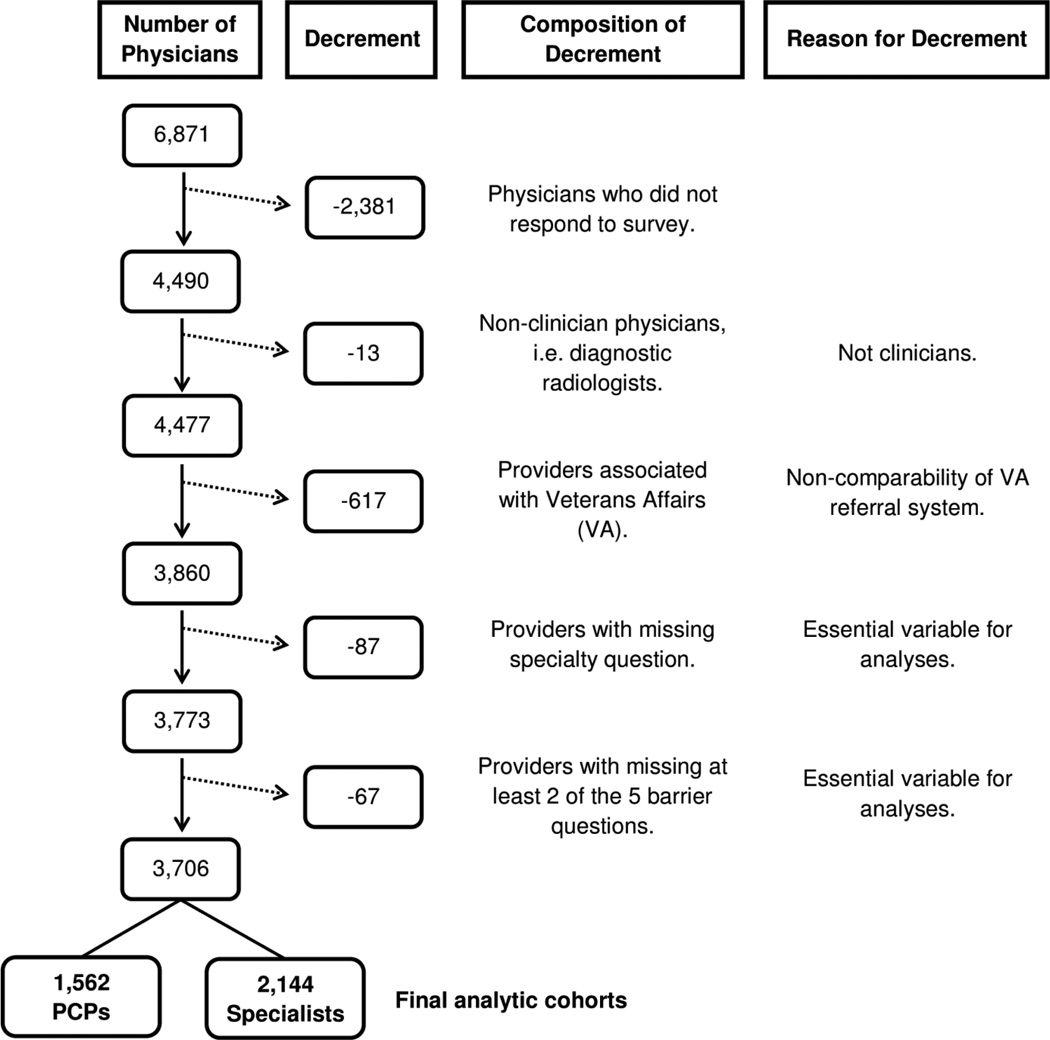
Data were collected through the physician survey component of the Cancer Care Outcomes Research and Surveillance (CanCORS) Consortium,14 a national observational study of over 10,000 patients diagnosed with lung or colorectal cancer from 2003–2005.15,16 This demographically representative, population-based cohort included patients from Northern California, Los Angeles County, North Carolina, Iowa, Alabama, or one of five integrated health care systems.17 Of 6,871 physicians identified by study patients as having a key role in their cancer care, 65% responded. We restricted the sample to 1,562 PCPs (internists, family physicians, general practitioners, geriatricians) and 2,144 specialists (surgeons, medical oncologists, radiation oncologists, other medical specialists) who met criteria described in Figure 1.
Figure 1. Selection of Analytic Cohorts.
Flowchart describes selection of two cohorts, PCPs and specialists (defined in Methods), for multivariable analyses of barriers to referring cancer patients for more specialized care. For physician career satisfaction analyses, 51 additional physicians (26 PCPs and 25 specialists) who did not respond to the career satisfaction question were excluded, yielding 1,536 PCPs and 2,119 specialists.
Although Veterans Affairs (VA) was included as a CanCORS site, VA physicians practice in a uniform health care system with distributed sites, and in our sample were systematically different from other CanCORS providers in ways central to analyses. For example, 81% of staff VA physicians practiced in hospitals vs. 14–30% of physicians in other sites. Accordingly, we present analyses excluding VA physicians. Sensitivity analyses including VA physicians showed that VA affiliation was not significantly associated with referral barriers or career satisfaction. Survey data collection procedures were approved by human subjects committees at participating institutions.14
Barriers to specialist referral
Dependent variable
Physicians were asked on the survey, “How often does each factor listed below prevent you from referring your patients with cancer to the provider of your choice for more specialized care?” 1) Restricted provider networks; 2) Pre-authorization requirements; 3) Patient lack of ability to pay; 4) Lack of surgical sub-specialists; and 5) Excessive patient travel time. Response options were provided using a five-point Likert scale: 1=Never, 2=Rarely, 3=Sometimes, 4=Usually, 5=Always. After calculating high inter-item reliability across the five items (Cronbach’s alpha=0.81), we incorporated all items into a single score (range 1–5) by summing individual scores, then dividing this sum by the number of barrier items to which each physician responded. Logarithmic transformation of this barrier score yielded similar results in multivariable analyses. We present analyses using the non-transformed score.
Independent variables
Physician and practice characteristics hypothesized to be associated with barriers were included in multivariable modeling if they 1) showed a significant (P<.05) relationship with the barrier score in bivariate analysis of variance testing, and 2) were not highly correlated with other independent variables (Pearson’s r<.35) (Table 1). Age and gender were included because we considered them relevant.
Table 1.
Characteristics of Physicians Caring for Patients with Lung and/or Colorectal Cancer
| No. of Patients (%) | |||
|---|---|---|---|
| Primary Care Physician n=1,562 |
Specialty Physician n=2,144 |
Pa | |
| Physician characteristics | |||
| Gender | <.01 | ||
| Male | 1,201(77) | 1,861(87) | |
| Female | 361(23) | 283(13) | |
| Age | <.01 | ||
| <40 years | 267(17) | 327(15) | |
| 40–59 years | 1,067(68) | 1,422(66) | |
| 60+ years | 228(15) | 395(18) | |
| Specialty | - | ||
| Surgeon | 841(39) | ||
| Medical oncologist | 493(23) | ||
| Radiation oncologist | 223(10) | ||
| Other medical specialist | 587(27) | ||
| International medical graduate | .99 | ||
| Yes | 333(16) | ||
| No | 1,321(85) | 1,811(85) | |
| Board-certified | <.01 | ||
| Yes | 1,406(90) | 2,014(94) | |
| No | 156(10) | 130(6) | |
| Teaching medical students/residents | <.01 | ||
| Yes | 525(34) | 1,031(48) | |
| No | 1,037(66) | 1,113(52) | |
| Practice characteristics | |||
| Practice setting | <.01 | ||
| Hospital | 126(8) | 869(41) | |
| Office | |||
| Solo | 353(23) | 299(14) | |
| Single-specialty | 397(25) | 588(27) | |
| Multi-specialty | 566(36) | 330(15) | |
| Other | 82(5) | 27(1) | |
| Community health center | 38(2) | 30(1) | |
| Government-owned practice | .92 | ||
| Yes | 33(2) | 44(2) | |
| No | 1,528(98) | 2,099(98) | |
| Practice size (# physicians) | .34 | ||
| <20 | 1,152(74) | 1,738(81) | |
| 20+ | 410(26) | 406(19) | |
| % patients in managed care plans | .02 | ||
| <30% | 407(26) | 602(28) | |
| 30–89% | 743(48) | 1,092(51) | |
| 90–100% | 413(26) | 450(21) | |
| # medical record components always availableb | .32 | ||
| 0 | 14(<1) | 5(<1) | |
| 1 | 23(1) | 7(<1) | |
| 2 | 39(3) | 33(2) | |
| 3 | 119(8) | 126(6) | |
| 4 | 167(11) | 255(12) | |
| 5 | 234(15) | 407(19) | |
| 6 | 964(62) | 1,311(61) | |
| Income increase from referring patients | <.01 | ||
| Yes | 15(1) | 47(2) | |
| No | 1,521(99) | 2,072(98) | |
| Data collection site | <.01 | ||
| Cancer Research Network—5 HMOsc | 202(13) | 179(8) | |
| Northern California—8 counties | 340(22) | 565(26) | |
| State of Alabama | 210(13) | 326(15) | |
| Los Angeles County | 409(26) | 562(26) | |
| State of Iowa | 235(15) | 205(10) | |
| State of North Carolina—22 counties | 166(11) | 307(14) | |
| Physician experiences | |||
| Barrier score | <.01 | ||
| 1.0–1.9 | 716(46) | 852(40) | |
| 2.0–2.9 | 657(42) | 1011(48) | |
| 3.0–3.9 | 152(19) | 234(11) | |
| 4.0–5.0 | 27(1) | 23(1) | |
| Career satisfaction | <.01 | ||
| Very satisfied | 623(40) | 1,053(49) | |
| Somewhat satisfied | 644(41) | 798(37) | |
| Neither satisfied nor dissatisfied | 100(6) | 75(4) | |
| Somewhat dissatisfied | 158(10) | 183(9) | |
| Very dissatisfied | 37(2) | 35(2) | |
Differences between PCPs and specialists were tested using Wilcoxon-Mann-Whitney for ordinal variables and chi-square for categorical variables.
Medical record components include cancer surgery operative, chemotherapy treatment plan or summary, radiation therapy treatment plan or summary, general medicine, radiology imaging, and pathology notes/reports.
Health Maintenance Organization
Statistical analysis
We used multivariable linear regression to estimate the independent effects of physician and practice characteristics on physician-reported barriers to referring cancer patients for more specialized care. Results are reported as β-coefficients, representing a higher or lower barrier score along the original 5-point Likert scale compared with the reference. For example, a β-coefficient of -1 corresponds to a one-step reduction on the Likert scale, e.g. “rarely” to “never.” Separate models were estimated for PCPs and specialists. Item non-response rate was <3% of observations for all variables except practice size and percent patients in managed care plans, which were 6% and 9%, respectively. We used multiple imputation to account for missing data for independent variables in all analyses.18 Analyses were performed using Stata 12.
Physician career satisfaction
Measuring career satisfaction
Physicians were asked, “Thinking very generally about your satisfaction with your overall career in medicine, would you say that you are currently:” 1=Very dissatisfied, 2=Somewhat dissatisfied, 3=Neither satisfied nor dissatisfied, 4=Somewhat satisfied, 5=Very satisfied. We created a dichotomous dependent variable of very or somewhat satisfied vs. not.
Statistical analysis
We used multivariable logistic regression to estimate the independent effect of the barrier score on physician career satisfaction. We included all independent variables meeting criteria for the barriers model, and a variable indicating whether the physician’s income was likely to increase from referring patients to specialists. Separate models were estimated for PCPs and specialists. To adjust for potential selection effects in estimating the association of higher (3.0–5.0) barrier scores vs. lower (<3.0) barrier scores, we applied inverse probability weights derived from doubly robust propensity scores to participants with lower barrier scores. These weights were incorporated in logistic regression models for physician career satisfaction, yielding doubly robust estimates of the association.19 Since this approach did not alter results compared with an unweighted model, we used the standard regression results, from which we computed the predicted probability of being very or somewhat satisfied for each respondent, holding all other variables at their observed values. We report the average of these predicted probabilities.
Results
Characteristics of cohort
Compared with PCPs, specialists were more often male, >60-years-old, and board-certified; and more likely to teach, practice in hospitals or multi-specialty office settings, have proportionately fewer patients in managed care plans, and report income increases from referring patients (Table 1). Specialists were less often in solo practice.
Prevalence of barriers to referral
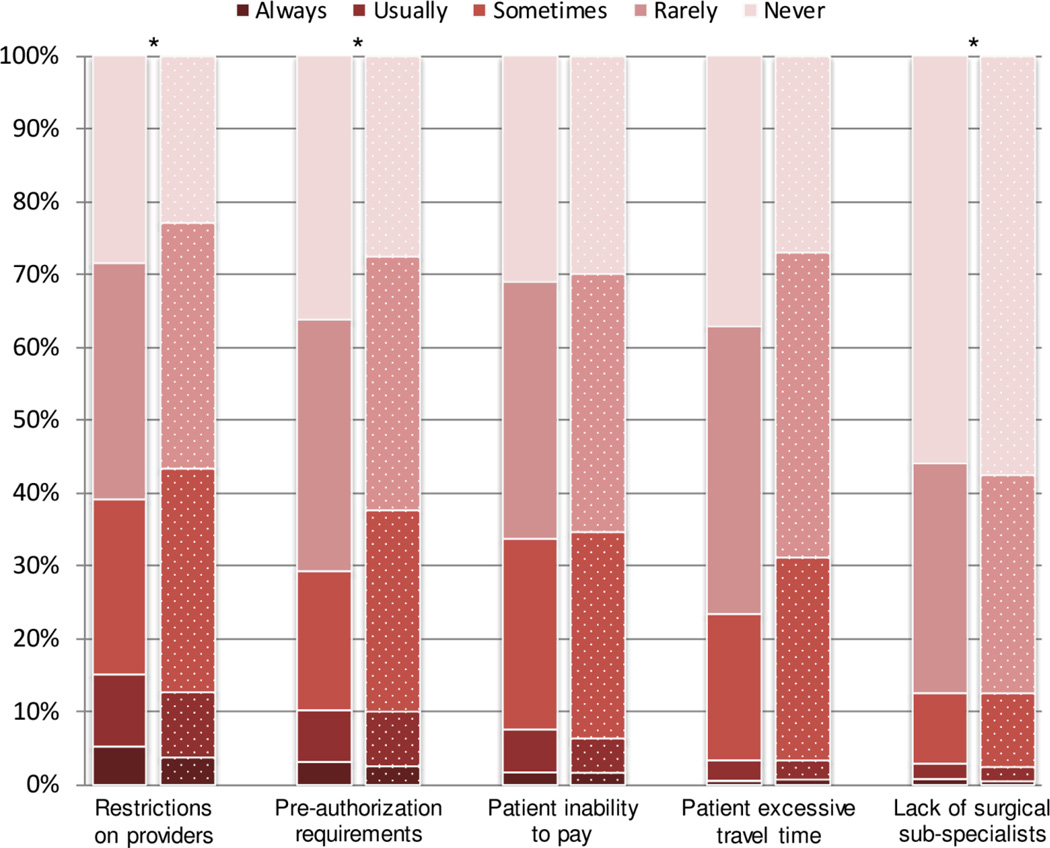
Three in five physicians reported always, usually, or sometimes encountering at least one barrier to specialist referral for cancer patients. Physicians reported always, usually, or sometimes encountering barriers associated with restricted provider networks (42%), preauthorization requirements (34%), patient inability to pay (34%), excessive patient travel time (28%), and lack of surgical sub-specialists (13%) (Figure 2). The overall mean barrier score was 2.0 (median 2.0, SD 0.72).
Figure 2. Distribution of Physician-Reported Barriers to Referring Cancer Patients for Specialized Care.
Bar graph shows distribution of the five referral barriers. Solid bars represent PCPs, and dotted bars, specialists.
*P<.01 using chi-square test.
Factors associated with barriers to referral in multivariable analysis
Among both PCPs and specialists, proportion of patients in managed care plans was the variable most strongly associated with higher barrier score (Table 2). Compared with physicians who reported a high (90–100%) proportion of patients in managed care plans, physicians with intermediate (30–89%) or low (<30%) proportion of managed care patients had higher barrier scores (β=0.46 for both PCPs and specialists for intermediate; and β=0.28 for PCPs and β=0.46 for specialists for low; P<.05 for all). Results were similar when we excluded respondents who reported 90–100% patients in managed care plans, when we removed the managed care variable from the model, and when we calculated the barrier score using only barriers commonly associated with managed care (restrictions on providers and pre-authorization requirements).
Table 2.
Factors Associated with Barriers to Specialist Referral, Stratified by Specialty Type, Adjusted.
| Primary Care Physician n=1,562 |
Specialist Physician n=2,144 |
|||
|---|---|---|---|---|
| β-coefficienta | 95% CI | β-coefficienta | 95% CI | |
| Male gender | 0.03 | −0.06, 0.11 | 0.07 | −0.02, 0.15 |
| Age | ||||
| <40 years | −0.02 | −0.11, 0.07 | 0.10 | 0.02, 0.18 |
| 40–59 years | Reference | Reference | ||
| 60+ years | −0.15 | −0.25, −0.04 | −0.04 | −0.11, 0.03 |
| Specialty | ||||
| Surgeon | Reference | |||
| Medical oncologist | 0.31 | 0.23, 0.39 | ||
| Radiation oncologist | 0.38 | 0.28, 0.48 | ||
| Other medical specialist | −0.10 | −0.17, −0.03 | ||
| International medical graduate | 0.34 | 0.25, 0.44 | 0.28 | 0.20, 0.35 |
| Not board-certified | 0.17 | 0.05, 0.29 | 0.05 | −0.06, 0.16 |
| No teaching medical students/residents | 0.04 | −0.03, 0.11 | 0.04 | −0.02, 0.10 |
| Practice setting | ||||
| Hospital | Reference | Reference | ||
| Office | ||||
| Solo | 0.20 | 0.03, 0.36 | 0.21 | 0.11, 0.31 |
| Single-specialty | 0.06 | −0.09, 0.21 | 0.10 | 0.03, 0.18 |
| Multi-specialty | −0.03 | −0.18, 0.11 | −0.05 | −0.15, 0.04 |
| Other | −0.04 | −0.24, 0.15 | 0.01 | −0.25, 0.26 |
| Community health center | 0.34 | 0.08, 0.60 | 0.12 | −0.10, 0.35 |
| Government-owned practice | 0.36 | 0.11, 0.61 | 0.27 | 0.06, 0.47 |
| Small practice size (<20 physicians) | 0.13 | 0.04, 0.23 | 0.04 | −0.04, 0.11 |
| Percent patients in managed care plans | ||||
| <30% | 0.28 | 0.16, 0.41 | 0.46 | 0.31, 0.61 |
| 30–89% | 0.46 | 0.36, 0.56 | 0.51 | 0.39, 0.63 |
| 90–100% | Reference | Reference | ||
| Availability of medical record components | −0.08 | −0.10, −0.05 | −0.04 | −0.07, −0.01 |
| Data collection site | ||||
| Cancer Research Network—5 HMOs | Reference | Reference | ||
| Northern California—8 counties | −0.08 | −0.21, 0.05 | −0.06 | −0.17, 0.05 |
| State of Alabama | 0.00 | −0.16, 0.16 | −0.07 | −0.21, 0.06 |
| Los Angeles County | 0.06 | −0.07, 0.18 | 0.05 | −0.06, 0.16 |
| State of Iowa | 0.14 | −0.01, 0.29 | −0.02 | −0.16, 0.12 |
| State of North Carolina—22 counties | 0.13 | −0.29, 0.02 | −0.10 | −0.23, 0.02 |
β-coefficients represent a higher or lower barrier score compared with the reference, and correspond to the original five-point Likert scale, e.g. −1.0 may correspond to “never” compared with “rarely.”
Among both PCPs and specialists, international medical graduates (IMGs) had higher barrier scores than United States/Canadian graduates (β=0.34 and 0.28, respectively; both P<.01), as did physicians in solo vs. hospital practices (β=0.20 and 0.21; P=.02 and P<.01), and those in government-owned practices (β=0.36 and 0.27; P<.01 and P=.01). Greater availability of medical records was associated with lower barrier scores (β=−0.08 and −0.04; both P<.01).
Among PCPs, non-board-certified physicians had higher barrier scores than those who were (β=0.17; P<.01), as did physicians in community health center (CHC) vs. hospital-based practices (β=0.34; P=.01) and those in practices with <20 physicians (β=0.13; P<.01). Physicians age 60+ years had lower barrier scores than those 40–59 (β=−0.15; P<.01).
Among specialists, physicians age <40 years vs. 40–59 had higher barrier scores (β=0.10; P=.01), as did medical or radiation oncologists vs. surgeons (β=0.31 and 0.38; both P<.01), and those in single specialty office vs. hospital practices (β=0.10; P<.01). Other medical specialists reported fewer barriers (β=−0.10; P<.01) than did surgeons.
Career satisfaction
Eighty-one percent of PCPs and 87% of specialists reported being very or somewhat satisfied with their careers (P<.01) (Table 1).
After adjustment, physicians with higher (4.0–5.0) referral barrier scores were less likely to be very or somewhat satisfied with their careers than those with lower (1.0–1.9) scores (65% vs. 84% among PCPs and 71% vs. 88% among specialists; both P<.01) (Table 3). Variables significantly (P<.05) associated with higher likelihood of being very or somewhat satisfied included age <40 or 60+ years vs. 40–59 years, medical or radiation oncologist vs. surgeon, teaching medical students or residents, greater medical record availability, and reporting income increases from referring patients (Table 3).
Table 3.
Predicted Probabilities of Being Very/Somewhat Satisfied with Career, Stratified by Specialty Type, Adjusted.
| Primary Care Physician n=1,536 |
Specialist Physician n=2,119 |
|||||
|---|---|---|---|---|---|---|
| Predicted probability |
95% CI | Pa | Predicted probability |
95% CI | Pa | |
| Barrier scoreb | ||||||
| 1.0–1.9 | 84.2% | 82.2–86.2 | Reference | 88.1 | 86.3–89.9 | Reference |
| 2.0–2.9 | 82.3% | 80.2–84.4 | .19 | 86.1 | 84.2–88.0 | .09 |
| 3.0–3.9 | 80.4%) | 76.2–84.5 | .11 | 84.0 | 80.3–87.7 | .04 |
| 4.0–5.0 | 65.1% | 51.6–78.6 | <.01 | 70.9 | 58.4–83.4 | <.01 |
| Gender | ||||||
| Male | 82.1% | 80.6–83.7 | .22 | 86.3 | 84.9–87.8 | .23 |
| Female | 84.2% | 81.2–87.2 | Reference | 88.0 | 85.3–90.7 | Reference |
| Age | ||||||
| <40 years | 85.4% | 82.2–88.5 | .02 | 88.8 | 86.2–91.5 | .02 |
| 40–59 years | 81.3% | 79.6–83.0 | Reference | 85.5 | 83.8–87.2 | Reference |
| 60+ years | 85.3% | 82.4–88.2 | .02 | 88.5 | 86.0–91.0 | .03 |
| Specialty | ||||||
| Surgeon | 84.2 | 81.7–86.7 | Reference | |||
| Medical oncologist | 88.3 | 85.4–91.2 | .04 | |||
| Radiation oncologist | 91.8 | 88.1–95.5 | <.01 | |||
| Other medical specialist | 86.4 | 83.6–89.2 | .26 | |||
| International medical graduate | ||||||
| Yes | 83.7% | 80.6–86.7 | .47 | 87.3 | 84.6–90.0 | .52 |
| No | 82.4% | 80.8–83.9 | Reference | 86.4 | 84.9–87.9 | Reference |
| Board-certified | ||||||
| Yes | 83.1% | 81.7–84.6 | Reference | 86.8 | 85.3–88.2 | Reference |
| No | 78.4% | 73.4–83.4 | .07 | 83.3 | 78.9–87.7 | .12 |
| Teaching medical students/residents | ||||||
| Yes | 86.3% | 84.3–88.3 | Reference | 88.9 | 87.3–90.6 | Reference |
| No | 80.8% | 79.1–82.6 | <.01 | 84.3 | 82.3–86.3 | <.01 |
| Practice setting | ||||||
| Hospital | 85.3% | 82.8–87.8 | Reference | 86.9 | 84.6–89.2 | Reference |
| Office | ||||||
| Solo | 78.7% | 75.2–82.3 | <.01 | 86.4 | 80.0–86.7 | .09 |
| Single-specialty | 85.2% | 82.7–87.7 | .95 | 87.9 | 85.6–90.1 | .57 |
| Multi-specialty | 84.1% | 81.5–86.7 | .51 | 87.2 | 84.4–89.9 | .88 |
| Other | 74.0% | 65.7–82.3 | .01 | 79.0 | 71.4–86.7 | .049 |
| Community health center | 84.1% | 73.5–92.5 | .65 | 86.0 | 77.7–94.3 | .83 |
| Government-owned practice | ||||||
| Yes | 84.1% | 74.6–93.6 | .75 | 88.1 | 80.5–95.7 | .69 |
| No | 82.6% | 81.2–84.0 | Reference | 86.5 | 85.1–88.0 | Reference |
| Practice size (# physicians) | ||||||
| <20 | 82.7% | 81.1–84.4 | .79 | 86.6 | 85.0–88.1 | .98 |
| 20+ | 82.2% | 78.9–85.5 | Reference | 86.5 | 83.5–9.5 | Reference |
| % patients in managed care plans | ||||||
| <30% | 84.1% | 81.5–86.7 | .20 | 87.4 | 85.1–89.7 | .36 |
| 30–89% | 82.5% | 80.5–84.5 | .53 | 86.4 | 84.6–88.2 | .67 |
| 90–100% | 81.2% | 78.0–84.5 | Reference | 85.7 | 82.7–88.7 | Reference |
| # medical record components always available | ||||||
| 0–3 | 75.8% | 71.2–80.3 | Reference | 81.1 | 77.0–85.2 | Reference |
| 4–6 | 83.6% | 82.2–85.1 | <.01 | 87.0 | 85.6–88.5 | <.01 |
| Income increase from referring patients | ||||||
| Yes | 95.2% | 89.8–100.0 | <.01 | 96.4 | 92.3–100.0 | <.01 |
| No | 82.5% | 81.1–83.9 | Reference | 86.3 | 84.8–87.8 | Reference |
| Data collection site | ||||||
| Cancer Research Network—5 HMOs | 83.3% | 79.1–87.5 | Reference | 87.0 | 83.3–90.7 | Reference |
| Northern California—8 counties | 84.0% | 81.5–86.5 | .78 | 87.4 | 85.2–89.7 | .85 |
| State of Alabama | 85.4% | 82.1–88.8 | .46 | 89.1 | 86.3–91.8 | .39 |
| Los Angeles County | 80.7% | 78.1–83.4 | .31 | 84.9 | 82.5–87.3 | .31 |
| State of Iowa | 81.6% | 77.5–85.7 | .56 | 86.0 | 82.4–89.5 | .67 |
| State of North Carolina—22 counties | 81.2% | 77.4–85.1 | .48 | 85.3 | 82.1–88.6 | .49 |
Significance values obtained from multivariable logistic regression.
A higher barrier score reflects higher frequency of reporting barriers to specialist referral.
Among PCPs, solo office practice setting was associated with lower likelihood of being very or somewhat satisfied vs. hospital practice (P<.01).
Among specialists, barrier scores 3.0–3.9 and 4.0–5.0 compared with 1.0–1.9 were associated with lower likelihood of being very or somewhat satisfied (both P≤.04). Medical and radiation oncologists were more satisfied than surgeons (P=.04 and <.01, respectively).
Discussion
Among 1,562 PCPs and 2,144 specialists caring for patients with cancer, three in five physicians reported always, usually, or sometimes encountering at least one barrier to referring cancer patients for more specialized care. In multivariable analyses of both cohorts, most variables significantly associated with barriers were related to practice setting. Referral barriers were significantly associated with lower physician career satisfaction.
Barriers to referrals for more specialized care
Providers reported experiencing each of the five barriers, although the frequency varied by the specific barrier. The most frequently reported barriers were provider network restrictions and pre-authorization requirements, policies that were originally developed to control use of services and reduce unnecessary costs. A trend toward easing these restrictions emerged when limited access to specialists tainted public sentiment toward managed care.20 There is a current trend towards more restrictive physician networks in some insurance products available in state and federal exchanges, and in some contracts of Accountable Care Organizations (ACOs) with health plans. It will be important that physicians maintain the ability to refer patients to high-quality providers. While patient-centered medical homes and neighborhoods are intended to enhance access and coordinated care between referring physicians and specialty consultants, these programs’ organizational and payment models are still developing, so their actual impact on referrals is not yet known.21 This is an important research area that needs additional investigation.
In adjusted analyses, several physician and practice characteristics were associated with physicians’ report of barriers to referral. PCPs and specialists with a high proportion of patients in managed care plans had lower barrier scores than those with a low or intermediate proportion, consistent with previous studies,22,23 but seemingly contradictory to our aforementioned finding that the two most frequently reported barriers were originally developed by managed care organizations. These physicians may practice in integrated settings with streamlined referral systems, in-network specialists, and insured patients. Conversely, we found that physicians in solo or small practices were more likely to report barriers to specialist referral than those in hospital-based or larger practices. Further research exploring these findings is warranted.
The least frequently reported barriers were lack of surgical subspecialists and excessive patient travel time. Literature regarding surgical subspecialist availability is sparse, but extensive centralization of cancer surgery has resulted in increased patient travel time,10 which may hinder access to quality cancer care. Longer travel time has been correlated with more advanced stage at cancer diagnosis and suboptimal or non-receipt of cancer treatment.7,9,24,25 However, in our study, excessive travel time was not reported to be an important barrier to specialist referral. While this finding may reflect poor communication between clinicians and patients, evidence shows that distance issues are sufficiently discussed,26 suggesting that our finding is valid.
Government practice ownership was associated with more reported barriers to specialist referral. Since VA physicians were excluded from the cohort, we assumed that the remaining physicians who reported government ownership practiced at public hospitals and/or clinics, which are more likely to serve patient populations of low socioeconomic status.27 Our finding may reflect these physicians’ cancer patients’ compromised access to specialized care. Among PCPs, CHC practice setting was associated with greater report of barriers to referral than hospital practice setting, which may reflect financial and transportation barriers faced by the patient population, and that fewer physicians may be willing to see uninsured, under-insured, or Medicaid patients.
Greater availability of medical records, likely a marker for access to information technology,28 was associated with lower report of referral barriers. Physicians who reported high availability of medical records may practice with an electronic health record (EHR) and/or electronic referral system, which potentially facilitate care coordination.29,30 Given growing interest in improving the coordination of primary and specialty care, especially through ACOs and patient-centered medical homes,31 our data suggest that implementation of information technology may serve as a strategy for reducing barriers to specialist referral for cancer patients.
Among PCPs, IMGs reported more barriers to specialist referral than United States/Canadian graduates. IMGs are more likely to practice in Health Professional Shortage Areas (HPSAs), and HPSA residents are more likely to be uninsured and have less healthcare access, which may explain our finding.32,33 Furthermore, studies have suggested IMGs lack sufficient communication training and face isolation during residency, which may influence their referral networks.34,35
Career satisfaction
Physicians caring for cancer patients reported being generally satisfied with their careers. Specialists were more likely to be satisfied than PCPs, consistent with recent evidence.11 Physicians who reported more referral barriers reported lower career satisfaction. This may be an indicator of the increased stress, time, and energy physicians experience in navigating barriers to referrals, as well as the frustration accompanying a physician’s inability to work autonomously and provide high-quality care.36 The potential ramifications of physician dissatisfaction and burnout are serious, as they may impact patient care and physician mental health, wellness, and workforce retention.11,37–41
Strengths/limitations
Strengths of our study include large sample size, geographic diversity of respondents, and inclusion of physicians directly involved in cancer care across multiple specialties. However, our self-reported data may be subject to selection bias and socially desirable response bias. Also, the data did not allow adjustment for physicians’ clustering within shared practices. Clustering adjustment was limited to study site fixed effects. It is also unknown whether barriers perceived by physicians correlate with those perceived by their patients; this may an area of further research. Finally, we used a single item to assess physician satisfaction; additional research looking at related topics such as physician burnout could provide a broader picture of the impact of referral barriers on physicians.11
Conclusions
PCPs and specialists in large, highly-managed care practices, which likely had established strategies to facilitate referrals across disciplines, reported fewer barriers to referring cancer patients for more specialized care than did physicians in small practices or with fewer managed care patients. High barrier scores were associated with lower physician career satisfaction. Integrated, uniform systems for providing timely referrals may promote cancer patient care and physician career satisfaction.
Acknowledgments
Funding sources: Financial assistance for Daniel Kwon was provided by the Short Term Training Program from DGSOM. Other authors received support from CanCORS Consortium NCI grant (2 U01 CA093344-06).
Footnotes
Financial disclosures: None.
Informed consent: Survey data collection procedures were approved by human subjects committees at participating institutions.
Contributor Information
Daniel H. Kwon, David Geffen School of Medicine (DGSOM) at University of California, Los Angeles (UCLA)
Diana M. Tisnado, Department of Medicine, Division of General Internal Medicine & Health Services Research, UCLA, Veterans Affairs, Greater Los Angeles
Nancy L. Keating, Department of Health Care Policy, Harvard Medical School, Department of Internal Medicine, Division of General Internal Medicine, Brigham and Women's Hospital, Boston, MA
Carrie N. Klabunde, Division of Cancer Control and Population Sciences, National Cancer Institute, Bethesda, MD
John L. Adams, RAND Corporation, Santa Monica, CA
Afshin Rastegar, RAND Corporation, Santa Monica, CA
Mark C. Hornbrook, Kaiser Permanente Northwest, Portland, OR
Katherine L. Kahn, Division of General Internal Medicine & Health Services Research, DGSOM at UCLA and RAND Corporation, Santa Monica, CA.
References
- 1.Baena-Canada JM, Ramirez-Daffos P, Cortes-Carmona C, Rosado-Varela P, Nieto-Vera J, Benitez-Rodriguez E. Follow-up of long-term survivors of breast cancer in primary care versus specialist attention. Fam Pract. 2013;30:525–532. doi: 10.1093/fampra/cmt030. [DOI] [PubMed] [Google Scholar]
- 2.Hillner BE, Smith TJ, Desch CE. Hospital and physician volume or specialization and outcomes in cancer treatment: importance in quality of cancer care. J Clin Oncol. 2000;18:2327–2340. doi: 10.1200/JCO.2000.18.11.2327. [DOI] [PubMed] [Google Scholar]
- 3.Haynes AB, Chiang Y, Feig BW, et al. Association between delays in adjuvant chemotherapy for stage III colon cancer and increased mortality. J Clin Oncol. 2012;30(suppl4) abstr541. [Google Scholar]
- 4.Luo R, Giordano SH, Freeman JL, Zhang D, Goodwin JS. Referral to medical oncology: a crucial step in the treatment of older patients with stage III colon cancer. Oncologist. 2006;11:1025–1033. doi: 10.1634/theoncologist.11-9-1025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Coburn N, Fulton J, Pearlman DN, Law C, DiPaolo B, Cady B. Treatment variation by insurance status for breast cancer patients. Breast J. 2008;14:128–134. doi: 10.1111/j.1524-4741.2007.00542.x. [DOI] [PubMed] [Google Scholar]
- 6.Kent EE, Forsythe LP, Yabroff KR, et al. Are survivors who report cancer-related financial problems more likely to forgo or delay medical care? Cancer. 2013;119:3710–3717. doi: 10.1002/cncr.28262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Holmes JA, Carpenter WR, Wu Y, et al. Impact of distance to a urologist on early diagnosis of prostate cancer among black and white patients. J Urol. 2012;187:883–888. doi: 10.1016/j.juro.2011.10.156. [DOI] [PubMed] [Google Scholar]
- 8.Onega T, Duell EJ, Shi X, Wang D, Demidenko E, Goodman D. Geographic access to cancer care in the U.S. Cancer. 2008;112:909–918. doi: 10.1002/cncr.23229. [DOI] [PubMed] [Google Scholar]
- 9.Onitilo A, Miskowiak D, Broton M, et al. PS1-41: Geographical Access to Mammography Services and Stage of Breast Cancer at Initial Diagnosis in Wisconsin. Clin Med Res. 2013;11:131. [Google Scholar]
- 10.Stitzenberg KB, Sigurdson ER, Egleston BL, Starkey RB, Meropol NJ. Centralization of cancer surgery: implications for patient access to optimal care. J Clin Oncol. 2009;27:4671–4678. doi: 10.1200/JCO.2008.20.1715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shanafelt T, Dyrbye L. Oncologist burnout: causes, consequences, and responses. J Clin Oncol. 2012;30:1235–1241. doi: 10.1200/JCO.2011.39.7380. [DOI] [PubMed] [Google Scholar]
- 12.Shanafelt TD, Boone S, Tan L, et al. Burnout and satisfaction with work-life balance among US physicians relative to the general US population. Arch Intern Med. 2012;172:1377–1385. doi: 10.1001/archinternmed.2012.3199. [DOI] [PubMed] [Google Scholar]
- 13.Shanafelt TD, Gradishar WJ, Kosty M, et al. Burnout and Career Satisfaction Among US Oncologists. J Clin Oncol. 2014;32:678–686. doi: 10.1200/JCO.2013.51.8480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Keating NL, Landrum MB, Klabunde CN, et al. Adjuvant chemotherapy for stage III colon cancer: do physicians agree about the importance of patient age and comorbidity? J Clin Oncol. 2008;26:2532–2537. doi: 10.1200/JCO.2007.15.9434. [DOI] [PubMed] [Google Scholar]
- 15.Ayanian JZ, Chrischilles EA, Fletcher RH, et al. Understanding cancer treatment and outcomes: the Cancer Care Outcomes Research and Surveillance Consortium. J Clin Oncol. 2004;22:2992–2996. doi: 10.1200/JCO.2004.06.020. [DOI] [PubMed] [Google Scholar]
- 16.Klabunde CN, Ambs A, Keating NL, et al. The role of primary care physicians in cancer care. J Gen Intern Med. 2009;24:1029–1036. doi: 10.1007/s11606-009-1058-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Catalano PJ, Ayanian JZ, Weeks JC, et al. Representativeness of participants in the cancer care outcomes research and surveillance consortium relative to the surveillance, epidemiology, and end results program. Med Care. 2013;51:e9–e15. doi: 10.1097/MLR.0b013e318222a711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.He Y, Zaslavsky AM, Landrum MB, Harrington D, Catalon P. Multiple imputation in a large-scale complex survey: a practical guide. Stat Methods in Med Res. 2010;19:653–670. doi: 10.1177/0962280208101273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bang H, Robins JM. Doubly robust estimation in missing data and causal inference models. Biometrics. 2005;61:962–973. doi: 10.1111/j.1541-0420.2005.00377.x. [DOI] [PubMed] [Google Scholar]
- 20.Harris KM. Can high quality overcome consumer resistance to restricted provider access? Evidence from a health plan choice experiment. Health Serv Res. 2002;37:551–571. doi: 10.1111/1475-6773.00037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mehta AJ, Macklis RM. Overview of accountable care organizations for oncology specialists. J Oncol Pract. 2013;9:216–221. doi: 10.1200/JOP.2012.000760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Forrest CB, Nutting PA, von Schrader S, Rohde C, Starfield B. Primary care physician specialty referral decision making: patient, physician, and health care system determinants. Med Decis Making. 2006;26:76–85. doi: 10.1177/0272989X05284110. [DOI] [PubMed] [Google Scholar]
- 23.Grembowski DE, Martin D, Diehr P, et al. Managed care, access to specialists, and outcomes among primary care patients with pain. Health Serv Res. 2003;38:1–19. doi: 10.1111/1475-6773.00102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Crawford SM, Sauerzapf V, Haynes R, Forman D, Jones AP. Social and geographical factors affecting access to treatment of colorectal cancer: a cancer registry study. BMJ Open. 2012;2:e000410. doi: 10.1136/bmjopen-2011-000410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jemal A, Ward E, Wu X, Martin HJ, McLaughlin CC, Thun MJ. Geographic patterns of prostate cancer mortality and variations in access to medical care in the United States. Cancer Epidemiol Biomarkers Prev. 2005;14:590–595. doi: 10.1158/1055-9965.EPI-04-0522. [DOI] [PubMed] [Google Scholar]
- 26.Groux P, Szucs T. Geographic disparities in access to cancer care: do patients in outlying areas talk about their access problems to their general practitioners and medical oncologists and how does that impact on the choice of chemotherapy? Eur J Cancer Care. 2013;22:746–753. doi: 10.1111/ecc.12096. [DOI] [PubMed] [Google Scholar]
- 27.Fraze T, Elixhauser A, Holmquist L, Johann J. Public Hospitals in the United States. [Accessed September 30, 2010];2008 http://www.hcup-us.ahrq.gov/reports/statbriefs/sb95.pdf. [PubMed]
- 28.Hier DB, Rothschild A, LeMaistre A, Keeler J. Differing faculty and housestaff acceptance of an electronic health record. Int J Med Inform. 2005;74:657–662. doi: 10.1016/j.ijmedinf.2005.03.006. [DOI] [PubMed] [Google Scholar]
- 29.Buntin MB, Burke MF, Hoaglin MC, Blumenthal D. The benefits of health information technology: a review of the recent literature shows predominantly positive results. Health Aff. 2011;30:464–471. doi: 10.1377/hlthaff.2011.0178. [DOI] [PubMed] [Google Scholar]
- 30.Chen AH, Murphy EJ, Yee HF., Jr eReferral--a new model for integrated care. N Engl J Med. 2013;368:2450–2453. doi: 10.1056/NEJMp1215594. [DOI] [PubMed] [Google Scholar]
- 31.Mehr SR. Applying accountable care to oncology: developing an oncology ACO. Am J Manag Care. 2013;19:E2. [PubMed] [Google Scholar]
- 32.Hart LG, Skillman SM, Fordyce M, Thompson M, Hagopian A, Konrad TR. International medical graduate physicians in the United States: changes since 1981. Health Aff. 2007;26:1159–1169. doi: 10.1377/hlthaff.26.4.1159. [DOI] [PubMed] [Google Scholar]
- 33.Liu JJ. Health professional shortage and health status and health care access. J Health Care Poor Underserved. 2007;18:590–598. doi: 10.1353/hpu.2007.0062. [DOI] [PubMed] [Google Scholar]
- 34.Chen PG, Curry LA, Bernheim SM, Berg D, Gozu A, Nunez-Smith M. Professional challenges of non-U.S.-born international medical graduates and recommendations for support during residency training. Acad Med. 2011;86:1383–1388. doi: 10.1097/ACM.0b013e31823035e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Dorgan KA, Lang F, Floyd M, Kemp E. International medical graduate-patient communication: a qualitative analysis of perceived barriers. Acad Med. 2009;84:1567–1575. doi: 10.1097/ACM.0b013e3181baf5b1. [DOI] [PubMed] [Google Scholar]
- 36.Friedberg MW, Chen PG, Van Busum KR, et al. Factors Affecting Physician Professional Satisfaction and Their Implications for Patient Care, Health Systems, and Health Policy. RAND Corporation. 2013 [PMC free article] [PubMed] [Google Scholar]
- 37.DiMatteo MR, Sherbourne CD, Hays RD, et al. Physicians' characteristics influence patients' adherence to medical treatment: results from the Medical Outcomes Study. Health Psychol. 1993;12:93–102. doi: 10.1037/0278-6133.12.2.93. [DOI] [PubMed] [Google Scholar]
- 38.Oreskovich MR, Kaups KL, Balch CM, et al. Prevalence of alcohol use disorders among American surgeons. Arch Surg. 2012;147:168–174. doi: 10.1001/archsurg.2011.1481. [DOI] [PubMed] [Google Scholar]
- 39.Shanafelt TD, Raymond M, Kosty M, et al. Satisfaction With Work-Life Balance and the Career and Retirement Plans of US Oncologists. J Clin Oncol. 2014;32:1127–1135. doi: 10.1200/JCO.2013.53.4560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wallace JE, Lemaire JB, Ghali WA. Physician wellness: a missing quality indicator. Lancet. 2009;374:1714–1721. doi: 10.1016/S0140-6736(09)61424-0. [DOI] [PubMed] [Google Scholar]
- 41.West CP, Huschka MM, Novotny PJ, et al. Association of perceived medical errors with resident distress and empathy: a prospective longitudinal study. JAMA. 2006;296:1071–1078. doi: 10.1001/jama.296.9.1071. [DOI] [PubMed] [Google Scholar]