Abstract
Recent studies suggest the ‘Lewinnek safe zone’ for acetabular component position is outdated. We used a large prospective institutional registry to determine if there is a ‘safe zone’ exists for acetabular component position within which the risk of hip dislocation is low and if other patient and implant factors affect the risk of hip dislocation. Patients who reported a dislocation event within six months after hip replacement surgery were identified, and acetabular component position was measured with anteroposterior radiographs. The frequency of dislocation was 2.1% (147 of 7040 patients). No significant difference was found in the number of dislocated hips among the zones. Dislocators <50 years old were less active preoperatively than nondislocators (p=0.006). Acetabular component position alone is not protective against instability.
Introduction
Dislocation is a common complication after total hip arthroplasty (THA)[1] with a reported frequency after primary THA from 0.1 to 9%[2–7]. The etiology of hip dislocation is multifactorial with surgical, patient, and implant factors all implicated[8–12]. While many studies associated one or two factors with dislocation, only a few provided a multivarible risk analysis, since such an approach requires a large study population. The largest study to date (21,047 primary THAs) found an increased dislocation risk with use of a smaller femoral head with the greatest risk associated with the posterolateral surgical approach[8]. This study provided useful information on factors such as head size and approach, but the authors did not use radiographic data to measure acetabular component position, which is also considered a major factor affecting the risk of dislocation[9,10].
In perhaps the most quoted article on the topic, Lewinnek et al. in 1978 determined where best to position an acetabular component for low risk of dislocation[9]. They defined a ‘safe zone’ based on analysis of 113 radiographs of THAs, of which 9 had gone on to dislocate. Despite the small number of patients who were analyzed, the ‘Lewinnek safe zone’ has become the most widely accepted range within which to position an acetabular component. Though recently considered as outdated by some[13–15], no new ‘safe zone’ has emerged. To reexamine the concept of a radiographic ‘safe zone’ for low risk of hip dislocation and to determine what other factors might influence the risk of a dislocation, we used a large prospective institutional registry to follow 7,040 primary THA patients for a minimum of six months after surgery.
We sought to determine if a ‘safe zone’ exists for acetabular component position, as measured on an anteroposterior (AP) radiograph, within which the risk of hip dislocation is low and if other patient and implant factors affect the risk of hip dislocation.
Patients and Methods
From 2007 to 2012, 19,449 patients (22,097 hip procedures) were recorded in an IRB-approved prospective total joint replacement registry. All patients who underwent primary THA were prospectively enrolled, of which 9,107 patients consented to participate in the registry. Baseline measurements of patient demographics, preoperative health status, medical comorbitities, and clinical outcome measurements were collected. An adverse event report questionnaire was mailed to all consented patients six months following their hip surgery. 7,263 patients completed the survey (an 80% compliance). To account for the potentially confounding effect of ultra-large femoral heads, patients with metal-on-metal THAs were excluded, leaving data from 7,040 primary THA patients for use in our risk analysis.
Demographic data were collected from patients’ electronic medical records and from reported outcome measures; the latter included pre- and post-op Lower Extremity Activity Scores (LEAS). LEAS is a validated instrument comprised of a single question with 18 levels of activity (from 1: bedbound to 18: participating in vigorous sports)[16]. Patients were contacted by mail to determine whether a dislocation had occurred in the intervening six months and to survey other complications that occurred subsequent to discharge from the index hospitalization. Dislocation was defined as an event in which the hip required reduction at a hospital.
The cohort is described in Table 1. There were 292 bilateral patients (4.2%), each with the same bearing type and head size implanted in both hips. No bilateral patient suffered dislocations in both hips during the study period, so our results did not change when the analysis was done using number of hips or number of patients. Therefore, we report our results as number of patients. Ninety-eight percent of the THAs were performed using the posterolateral approach. Bearing types included metal-on-crosslinked polyethylene (3,747 patients), ceramic-on-crosslinked polyethylene (1,760), metal-on-conventional polyethylene (582), ceramic-on-conventional polyethylene (619), and ceramic-on-ceramic (332). “Ceramic” femoral heads included 1,613 alumina (CeramTec, Plochingen, Germany) and 1,098 oxidized zirconium (Oxinium, Smith & Nephew, Memphis, TN) heads. Femoral head sizes were <28mm (73), 28mm (1,703), 32mm (3,773), 36mm (1,434), and >36mm (57).
Table 1.
Patient factors and risk of dislocation after primary THA
| Patient Factors | All Patients N = 7040 |
No Dislocation N = 6893 |
Dislocation N = 147 |
p-value |
|---|---|---|---|---|
| Age (mean ± sd) | 66 ±11 | 66 ±11 | 68 ±13 | 0.01 † |
| LEAS (mean ± sd) | 10 ± 3 | 10 ± 3 | 9 ± 3 | 0.001 § |
| % Female | 57.7% | 57.7% | 59.2% | 0.72 ¶ |
| BMI (mean ± sd) | 28 ± 6 | 28 ± 6 | 27 ± 5 | 0.24 † |
| Bilateral hips | 4.2% | 4.2% | 3.4% | 0.62 ¶ |
| Primary Diagnosis | 93.8% OA, 2.4% RA, 3.8% Other | 93.8% OA, 2.4% RA, 3.8% Other | 91.8% OA, 2.7% RA, 5.5% Other | 0.72 ¶ |
two sample t-test
Wilcoxon rank-sum test
Chi-square test
Radiographic analysis
AP pelvic radiographs were available for all patients via our institutional picture archiving and communication system (PACS, Sectra Imtec AB, Linköping, Sweden). Acetabular component inclination and anteversion angles were measured using the Ein Bild Röntgen Analyse software (EBRA, University of Innsbruck, Austria). The software utilizes a geometric comparison of a pelvic reference-point system with the outline of the acetabular component and femoral head using a comparability algorithm to make the measurements from a single radiograph[17,18]. The EBRA definition of inclination angle is the angle between the longitudinal axis and the acetabular axis when this is projected onto the coronal plane; anteversion angle is the angle between the acetabular axis and the coronal plane[19]. When acetabular component version was less than 10° (n=49), anteversion or retroversion was confirmed using additional available imaging (i.e., computed tomography scans and cross-table lateral radiographs).
Patient Matching
To examine the influence of acetabular component position on dislocation, postoperative AP radiographs of hips that dislocated were matched one to one with AP radiographs of stable hips. Patients were matched by age (± 5 years), BMI (± 2.5), pre-operative activity level (LEAS scores ± 2), sex (exact), laterality (exact, unilateral or bilateral THA), implant bearing surface (exact), and head size (exact). For 32 patients, BMI or LEAS information was unavailable; these patients were matched on the remaining characteristics. The quality of matching was evaluated by calculating the standardized difference (difference in means or proportions divided by standard error) for each characteristic. A poor match, or imbalance, was defined as a standardized difference >0.2[20].
Finding a 5° difference in inclination and anteversion between dislocators and nondislocators was considered clinically important, since in the best case scenario, 5° would be the expected accuracy of a surgeon trying to manually position a component in a desired location[21]. A power calculation was performed to estimate the sample size needed to detect a 5° difference between dislocators and nondislocators. A sample of 140 matched patients achieved 99% power with an estimated standard deviation of 10° and a significance level of 0.05. Upon radiographic review, we excluded 5 dislocations, one each for chronic pubic symphysis diastasis, constrained all polyethylene component, and developmental dysplasia of the hip with previous osteotomy, and two for periprosthetic fracture around a femoral stem.
Statistical analysis
Descriptive and inferential statistics were presented for demographics and patient reported outcomes. Intergroup variables and radiographic parameters were compared between patients with and without dislocation. Continuous variables were summarized using means and standard deviations or medians and quartiles, and a two-sample Student t-test or Wilcoxon rank-sum test was used to find differences. Categorical variables were reported as frequencies and proportions, and were compared using Chi-square or Fisher exact tests. Multiple logistic regressions were performed to identify risk factors for dislocation, including demographic factors (age, sex, BMI), laterality (bilateral or unilateral), and implant factors (head size and bearing type).
Inclination and anteversion angles were measured as independent continuous variables. Differences in these angles between matched patients who did and did not dislocate were compared using two-sample Student T-tests. To test combinations of both inclination and anteversion on the risk of dislocation, zones were defined based on different cutoff points (± 5°, ± 10°, ± 15° boundaries) for every 1° throughout the entire range of anteversion and inclination angles. Chi-square tests were performed to compare the number of dislocated and stable hips inside and outside of each zone, controlling for multiple comparisons using the False Discovery Rate (FDR) method. All tests were two-sided with a significance level of 0.05. All analyses were conducted using SAS for Windows 9.3 (SAS Institute Inc., Cary, NC).
Results
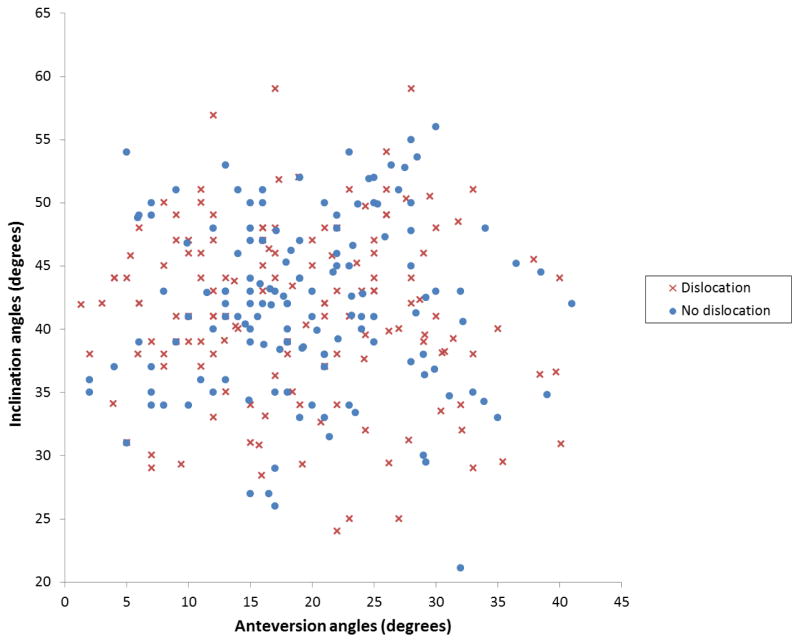
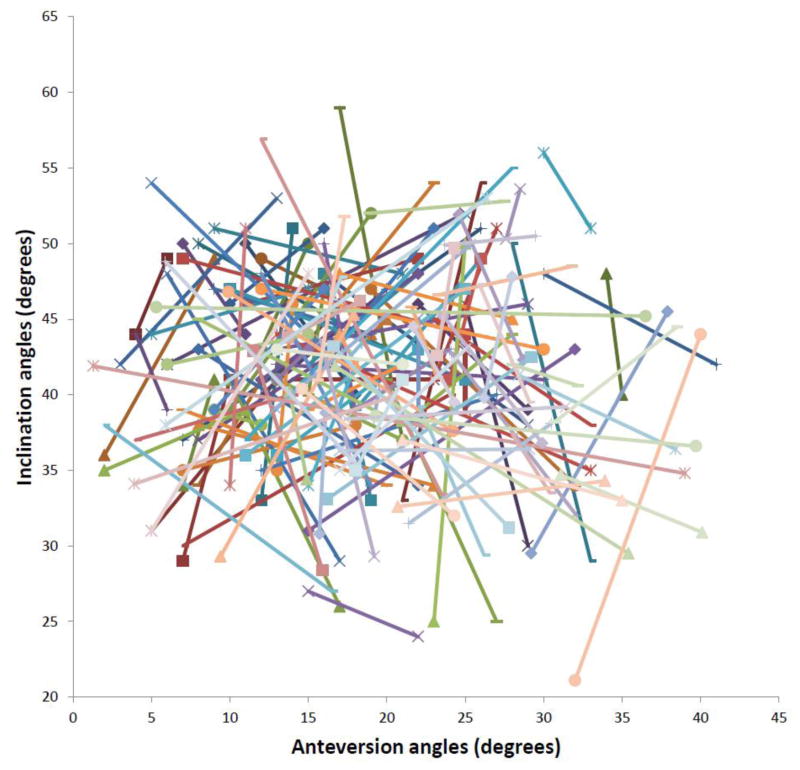
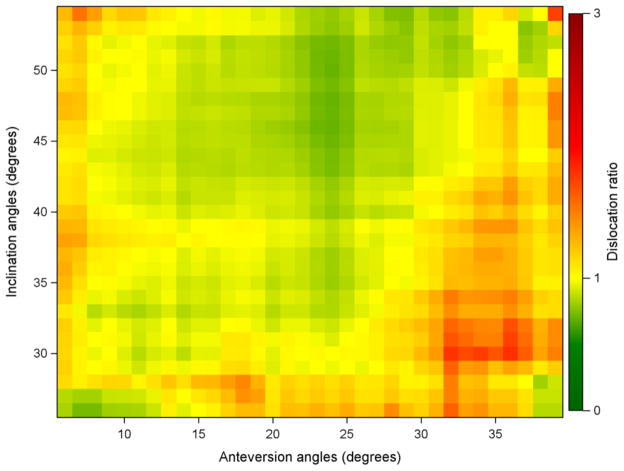
The frequency of dislocation over the six months following primary THA was 2.1% (147 of 7040 patients). The quality of matching patients was high, with all imbalances well below 0.2 (Table 2). No difference was found in acetabular inclination (p=0.42) or anteversion (p=0.50) angles between dislocators and nondislocators (Fig. 1). Differences in inclination and anteversion between matched patients were inconsistent (Fig. 2). Hips that went on to dislocate were found in all zones (even zones with ± 5° boundaries) within 5° to 40° anteversion and 25° to 55° inclination. No significant differences were found among any zone comparisons. Figure 3 shows the dislocation ratio (ratio of dislocators to nondislocators inside a zone) for zones with boundaries of ±10° inclination and ± 10° anteversion at every 1° of inclination and anteversion. A dislocation ratio of <1.0 means that there were fewer dislocators than nondislocators in a zone, a ratio of 1.0 means an equal number of dislocators and nondislocators, and a ratio >1.0 means there were more dislocators in a zone. Light green or yellow pixels show close to equal numbers of dislocators and nondislocators. If a ‘safe zone’ were present, it would appear dark green in color (ratio = 0). The lowest dislocation ratio was 0.70 (59 dislocators and 84 nondislocators) in the zone of 48° ± 10° inclination and 24° ± 10° anteversion. The ‘Lewinneksafe zone’ is at 40° inclination and 15° anteversion, with a dislocation ratio of 0.90 (yellow in color) and contains 163 of 284 (57%) hips from our cohort, including 78 of 142 (54%) dislocators.
Table 2.
Standardized differences before and after matching
| Matching variables | Before matching | After matching |
|---|---|---|
|
| ||
| Age | 0.341 | 0.024 |
|
| ||
| BMI | 0.076 | 0.028 |
|
| ||
| LEAS | 0.044 | 0.008 |
|
| ||
| Female sex | 0.134 | 0.0 |
|
| ||
| Head size | 0.525 | 0.01 |
|
| ||
| Bilateral | 0.115 | 0.0 |
|
| ||
| Bearing types | C on C 0.016 | 0.0 |
| C on P 0.081 | 0.0 | |
| C on XP 0.078 | 0.0 | |
| M on P 0.189 | 0.0 | |
| M on XP 0.191 | 0.0 | |
Figure 1.
A scatter plot of the inclination angle versus the anteversion angle for the 142 dislocators and the 142 nondislocators to which they were matched.
Figure 2.
The same scatter plot is shown as in Figure 1, but with the matched pairs connected with straight lines. If a ‘safe zone’ existed, the nondislocators would be within the zone, the dislocators would lie outside the zone, so the straight lines would all emanate from near the center of the plot.
Figure 3.
A color plot shows every pixel at 1° increments; each pixel is a safe zone with boundaries of ±10° anteversion and ± 10° inclination. For example, the red box located at 32° anteversion and 30° inclination reflects the dislocation ratio for the box-shaped zone with boundaries from 22° to 42° anteversion and 20° to 40° inclination. Since the color of the box is orange, the dislocation ratio for the zone is close to 1.5, with more dislocators than nondislocators. The light green and yellow pixels depict ratios close to 1.0 (an equal number of dislocators and nondislocators). The ‘Lewinnek safe zone’ is the pixel at 15° anteversion and 40° inclination; it is light green (ratio = 0.9). If it were a ‘safe zone’, it would be dark green in color (ratio = 0).
Dislocators were significantly older (68.3 ± 13 vs. 66 ± 11.2 years, p=0.012) and less active (LEAS of 8.5 ± 3 vs. 9.5 ± 3.2, p=0.001) compared to nondislocators (Table 1). Patients <50 years old had a 1.90 times higher risk of dislocation (95% confidence interval 1.20–3.01; p=0.007), and patients ≥70 years old had 2.28 times higher risk of dislocation (95% confidence interval 1.15–4.58; p=0.019), compared to patients between 50 and 69 years of age. Dislocators <50 years old were less active preoperatively than nondislocators (median LEAS of 7 vs. 10, p=0.006; Table 3). No differences were found in original diagnosis (p = 0.61) or sex (p = 0.58) between dislocators and nondislocators who were <50 years old. Age and activity level were the only factors found to be significant predictors for dislocation. When controlling for age and activity level, no association was found with respect to sex or BMI.
Table 3.
Age and activity level affected risk of dislocation
| No Dislocation N = 6893 |
Dislocation N = 147 |
||
|---|---|---|---|
|
| |||
| Age group | LEAS Median [q1, q3] | LEAS Median [q1, q3] | p-values§ |
| < 50 years | 10 [8,13] | 7 [6,9] | 0.006 |
| 50–69 years | 10 [7,12] | 8 [7,12] | 0.03 |
| ≤ 70 years | 8 [7,11] | 7 [6,10] | 0.22 |
Wilcoxon rank-sum test
Bearing type (p=0.16) and head size (p=0.34) were not significantly different between dislocators and nondislocators. The trend was that risk of dislocation decreased with head size (2.7% for heads ≤28mm, 2.5% for 28mm, 2.1% for 32mm, 1.5% for 36mm, and 1.8% for heads ≥36mm in diameter), but this finding did not reach significance. The risk of dislocation was 1.5% for ceramic-on-ceramic, 1.5% for ceramic-on-crosslinked polyethylene, 2.2% for metal-on-crosslinked polyethylene, 2.4% for ceramic-on-conventional polyethylene, and 3.1% for metal-on-conventional polyethylene. Within each bearing type, no difference was found between head size and dislocation, though the trend was decreased risk with larger femoral heads (Table 4).
Table 4.
Risk of dislocation for femoral head sizes and bearing types
| Bearing types | 28mm | 32mm | 36mm | p-values † |
|---|---|---|---|---|
| M on XP | 2.4% n = 1085 |
2.2% n = 1954 |
1.9% n = 642 |
0.93 |
| C on XP | 2.2% n = 186 |
1.7% n = 841 |
1.2% n = 681 |
0.58 |
| M on PE | 3.9% n = 195 |
2.7% n = 369 |
0% n = 6 |
0.28 |
| C on PE | 2.9% n = 206 |
2.2% n = 413 |
N/A | 0.50 |
| C on C | 0% n = 31 |
2.0% n = 196 |
1.0% n = 105 |
0.48 |
Cochran-Armitage Trend Test
Discussion
Hip dislocation is a distressing event for patients and surgeons, and prevention has been studied for as long as THAs have been performed[22]. The orthopaedic community generally accepts that malposition of the acetabular component outside of a ‘safe zone’ contributes to dislocation, since the orientation of THA components directly impacts the arc of motion and therefore the likelihood of impingement. To reduce the risk of dislocation, a ‘safe zone’ was defined in previous small cohort studies with as few as 5 dislocations (Table 5). However, the exact location of the ‘safe zone’ remains controversial, so we reexamined the concept of a radiographic ‘safe zone’ for low risk of dislocation. Unfortunately, our results suggest that a truly ‘safe zone’ based upon acetabular position alone does not exist.
Table 5.
Comparison of current results to those in the recent literature evaluating acetabular component position and dislocation
| Authors | Year | # patients with dislocation | # patients in series | Factors affecting dislocation | Safe zone |
|---|---|---|---|---|---|
| Lewinnek et al. | 1978 | 9 | 300 | Surgical approach and acetabular cup orientation | Inclination 40° ± 10° Anteverison 15° ± 10° |
| McCollum et al. | 1990 | 5 | 441 | Acetabular cup orientation | Inclination 40° ± 10° Anteverison 30° ± 10° |
| Paterno et al. | 1997 | 17 | 391 | Age, excessive alcohol intake | Did not find a difference in inclination |
| Jolles et al. | 2002 | 21 | 2,023 | Acetabular cup orientation, surgeon volume, patient motor skills and ASA score | Anteversion between 40° and 60° |
| Robinson et al. | 2012 | 9 | 668 | THA position (acetabular and femoral offset) | Inclination 40° ± 10° |
| Esposito et al. | 2014 | 147 | 7,040 | Age and activity score | Did not find a safe zone |
Our study has several limitations. The first is the use of a software program to measure inclination and anteversion angles from 2D radiographs. An AP radiograph cannot reliably account for sagittal pelvic tilt or pelvic rotation, which affects the functional position of an acetabular component[23,24]. Also, we could not measure femoral anteversion, an essential element in determining impingement free arc of motion[25,26]. Second, to determine the occurrence of dislocation, we relied upon self-reported data, which can be quite variable[27,28]. However, we previously tested for concordance between self-reported and surgeon assessed short-term complications after primary THA in the same registry used for the current study, and found that patients reliably self-reported hip dislocation[29]. Third, we limited our study to dislocations that occurred within six months after primary THA. Hip dislocations may increase with time[30–32], and dislocations at later times may be affected by different factors than those that we examined. However, dislocation is usually detected in the first 3 to 6 months after surgery[33]. And finally, we did not consider other factors that have been reported to affect the risk of dislocation, such as posterior capsule repair[34] and soft tissue or abduction tensioning[5,35]. Despite these limitations, the strength of our study is that it represents the largest cohort of THA patients prospectively analyzed for dislocation. With our registry information, we could examine multiple factors in a large patient population.
In many respects, our results are not surprising. Hip instability is multifactorial. What is clear from our data is that acetabular component position alone is not protective against dislocation. In a recent study, only 47% of 1883 THAs fell within a ‘safe zone’ similar to the ‘Lewinnek safe zone’[36]. The authors suggested that their high frequency of component malposition, as measured on AP radiographs, would increase the risk of dislocation. Our study does not support this conclusion; surgeons cannot predict early instability by measuring acetabular component position alone with AP radiographs. Radiographs from over half the dislocators (57%) showed the component to be positioned in the ‘Lewinnek safe zone’. A ‘safe zone’ may be considered ‘safe’ if it has two or three times fewer dislocators (ratio = 0.5 or 0.33). The green zones in Figure 3 should not be misconstrued as ‘safe’, since the lowest dislocation ratio in any given zone of anteversion and inclination was only 0.70 (41% dislocators and 59% nondislocators).
A few explanations exist in support of our findings. For example, we did not consider the contribution of femoral implant position to stability. The concept of combined anteversion[25,26] appears reasonable from a mechanical standpoint and certainly merits further study. Also, several studies described the impact of changes in functional acetabular component position relative to pelvic alignment[23,24], alterations that may prove to be significant in affecting outcome after THA. Finally, the biologic aspect of hip reconstruction should not be overlooked. The extent of healing of the soft tissue envelope following THA may affect joint stability; however, assessing the impact of this factor is difficult.
We found that patient age affected the risk of hip dislocation in a bimodal fashion with younger (<50 years) and older (≥70 years) patients both at higher risk. This is the first report of younger, less active patients having a higher frequency of dislocation. Developmental dysplasia, prior hip fracture, and female sex have been associated with increased risk of dislocation[37,38], but we did not find a difference in original diagnosis or sex in patients <50 years old. Other studies also found that older patients (>80 years) have a two- to three-fold increase in dislocation rate[6,12,37]. One study found that older patients with a preoperative femoral fracture had a higher risk[6], and another found a greater age disparity between dislocators and nondislocators in revision THA patients with a history of excessive alcohol intake[12]. The risk of dislocation in our patients was in the 1 to 3% range that is traditionally accepted as the incidence after primary THA[4,35,39]. The dislocations were all short-term (within six months of surgery) and likely mechanical in nature, where changes in body position during rising from a chair or reaching forward for an object can cause soft tissue or prosthetic impingement. The hip dislocations in our study were likely unassociated with wear, osteolysis, or adverse local tissue reactions, which usually take years to occur in hips without metal-on-metal bearings.
In the 1980s, surgeons began using larger femoral head sizes to increase the head-to-neck ratio and therefore increase the range of motion before impingement[10,40,41]. The result has been a decrease in the frequency of dislocation[8,42]. We did not find a significant difference in bearing type or head size, but we did find a trend showing larger head sizes associated with a lower risk of dislocation (2.5% for 28mm heads vs. 1.5% of 36mm heads). The decrease in dislocation frequency was not large with 28mm, 32mm, and 36mm heads, and 98% of THAs in our cohort were performed using the posterior approach, which has a historically higher dislocation rate than the anterior and transtrochanteric approaches[8,31,43]. Reports emphasizing the role of soft tissue repair of the capsule and external rotators have impacted instability rates. Pellici et al.[34] reported no dislocations in 395 hips with 26mm and 28mm heads when using a formal capsule repair after a posterior approach.
Our data show that the radiographic acetabular ‘safe zone’ that has been widely used since 1978 does not guarantee decreased risk of hip dislocation. This does not imply that component position is not important. Surgeons should still take care when placing THA components, because the success of a THA depends not only on stability, but also on wear and range of motion[13–15,44]. Since radiographs provide only 2D information, we are performing additional research with 3D imaging technology (i.e., CT scans and EOS® imaging) to study the effect of pelvic tilt on component orientation during functional positions. Navigation technology allows surgeons to accurately place THAs in any desired position[21,45], but the question of where to place an acetabular component remains. In conclusion, our results support the notion that hip dislocation is multivariate in etiology and that acetabular component position alone is not completely protective against instability. It appears that no ‘safe zone’ exists when it comes to component position.
Supplementary Material
Acknowledgments
This study utilized an implant registry developed with funding from the Agency for Healthcare Research and Quality through a Center for Education and Research on Therapeutics grant (CERTs; Agency of Health Research and Quality RFA-HS-05-14). Research reported in this publication was also supported by the National Institute of Arthritis and Musculoskeletal and Skin Diseases of the National Institutes of Health under Award Number AR007281.
Footnotes
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Bozic KJ, Kurtz SM, Lau E, Ong K, Vail TP, Berry DJ. The Epidemiology of Revision Total Hip Arthroplasty in the United States. J Bone Jt Surg. 2009;91:128–33. doi: 10.2106/JBJS.H.00155. [DOI] [PubMed] [Google Scholar]
- 2.Amstutz HC, Kody MH. Hip Arthroplasty. New York: Churchill Livingstone; 1991. Dislocation and subluxation; pp. 429–48. [Google Scholar]
- 3.Beaulé PE, Schmalzried TP, Udomkiat P, Amstutz HC. Jumbo femoral head for the treatment of recurrent dislocation following total hip replacement. J Bone Joint Surg Am. 2002;84-A:256–63. doi: 10.2106/00004623-200202000-00013. [DOI] [PubMed] [Google Scholar]
- 4.Blom AW, Rogers M, Taylor AH, Pattison G, Whitehouse S, Bannister GC. Dislocation Following Total Hip Replacement: The Avon Orthopaedic Centre Experience. Ann R Coll Surg Engl. 2008;90:658–62. doi: 10.1308/003588408X318156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Eftekhar NS. Dislocation and instability complicating low friction arthroplasty of the hip joint. Clin Orthop. 1976:120–5. [PubMed] [Google Scholar]
- 6.Ekelund A, Rydell N, Nilsson OS. Total hip arthroplasty in patients 80 years of age and older. Clin Orthop. 1992:101–6. [PubMed] [Google Scholar]
- 7.Parvizi J, Picinic E, Sharkey PF. Revision total hip arthroplasty for instability: surgical techniques and principles. J Bone Joint Surg Am. 2008;90:1134–42. [PubMed] [Google Scholar]
- 8.Berry DJ, von Knoch M, Schleck CD, Harmsen WS. Effect of femoral head diameter and operative approach on risk of dislocation after primary total hip arthroplasty. J Bone Joint Surg Am. 2005;87:2456–63. doi: 10.2106/JBJS.D.02860. [DOI] [PubMed] [Google Scholar]
- 9.Lewinnek GE, Lewis JL, Tarr R, Compere CL, Zimmerman JR. Dislocations after total hip-replacement arthroplasties. J Bone Joint Surg Am. 1978;60:217–20. [PubMed] [Google Scholar]
- 10.McCollum DE, Gray WJ. Dislocation after total hip arthroplasty. Causes and prevention. Clin Orthop. 1990:159–70. [PubMed] [Google Scholar]
- 11.Padgett DE, Lipman J, Robie B, Nestor BJ. Influence of total hip design on dislocation: a computer model and clinical analysis. Clin Orthop. 2006;447:48–52. doi: 10.1097/01.blo.0000218748.30236.40. [DOI] [PubMed] [Google Scholar]
- 12.Paterno SA, Lachiewicz PF, Kelley SS. The influence of patient-related factors and the position of the acetabular component on the rate of dislocation after total hip replacement. J Bone Joint Surg Am. 1997;79:1202–10. doi: 10.2106/00004623-199708000-00013. [DOI] [PubMed] [Google Scholar]
- 13.Eilander W, Harris SJ, Henkus HE, Cobb JP, Hogervorst T. Functional acetabular component position with supine total hip replacement. Bone Jt J. 2013;95-B:1326–31. doi: 10.1302/0301-620X.95B10.31446. [DOI] [PubMed] [Google Scholar]
- 14.Liu F, Gross TP. A Safe Zone for Acetabular Component Position in Metal-On-Metal Hip Resurfacing Arthroplasty: Winner of the 2012 HAP PAUL Award. J Arthroplasty. 2013;28:1224–30. doi: 10.1016/j.arth.2013.02.033. [DOI] [PubMed] [Google Scholar]
- 15.Murphy WS, Klingenstein G, Murphy SB, Zheng G. Pelvic tilt is minimally changed by total hip arthroplasty. Clin Orthop. 2013;471:417–21. doi: 10.1007/s11999-012-2581-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Saleh KJ, Mulhall KJ, Bershadsky B, Ghomrawi HM, White LE, Buyea CM, et al. Development and validation of a lower-extremity activity scale. Use for patients treated with revision total knee arthroplasty. J Bone Joint Surg Am. 2005;87:1985–94. doi: 10.2106/JBJS.D.02564. [DOI] [PubMed] [Google Scholar]
- 17.Hendrich C, Bahlmann J, Eulert J. Migration of the uncemented Harris-Galante acetabular cup: results of the einbildroentgenanalyse (EBRA) method. J Arthroplasty. 1997;12:889–95. doi: 10.1016/s0883-5403(97)90158-3. [DOI] [PubMed] [Google Scholar]
- 18.Krismer M, Bauer R, Tschupik J, Mayrhofer P. EBRA: A method to measure migration of acetabular components. J Biomech. 1995;28:1225–36. doi: 10.1016/0021-9290(94)00177-6. [DOI] [PubMed] [Google Scholar]
- 19.Murray DW. The definition and measurement of acetabular orientation. J Bone Joint Surg Br. 1993;75:228–32. doi: 10.1302/0301-620X.75B2.8444942. [DOI] [PubMed] [Google Scholar]
- 20.Cohen J. Statistical power analysis for the behavioral sciences. 2. Hillsdale, NJ: Lawrence Earlbaum Associates; 1988. [Google Scholar]
- 21.Nawabi DH, Conditt MA, Ranawat AS, Dunbar NJ, Jones J, Banks S, et al. Haptically guided robotic technology in total hip arthroplasty: a cadaveric investigation. Proc Inst Mech Eng [H] 2013;227:302–9. doi: 10.1177/0954411912468540. [DOI] [PubMed] [Google Scholar]
- 22.Charnley J. Low Friction Arthroplasty of the Hip: Theory and Practice. Berlin: Springer-Verlag; 1979. [Google Scholar]
- 23.Lazennec JY, Brusson A, Rousseau MA. Lumbar-pelvic-femoral balance on sitting and standing lateral radiographs. Orthop Traumatol Surg Res OTSR. 2013;99:S87–103. doi: 10.1016/j.otsr.2012.12.003. [DOI] [PubMed] [Google Scholar]
- 24.Lazennec JY, Riwan A, Gravez F, Rousseau MA, Mora N, Gorin M, et al. Hip spine relationships: application to total hip arthroplasty. Hip Int J Clin Exp Res Hip Pathol Ther. 2007;17 (Suppl 5):S91–104. [PubMed] [Google Scholar]
- 25.Dorr LD, Malik A, Dastane M, Wan Z. Combined anteversion technique for total hip arthroplasty. Clin Orthop. 2009;467:119–27. doi: 10.1007/s11999-008-0598-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ranawat CS, Maynard MJ. Modern techniques of cemented total hip arthroplasty. Tech Orthop. 1991;6:17–25. [Google Scholar]
- 27.Linet MS, Harlow SD, McLaughlin JK, McCaffrey LD. A comparison of interview data and medical records for previous medical conditions and surgery. J Clin Epidemiol. 1989;42:1207–13. doi: 10.1016/0895-4356(89)90119-4. [DOI] [PubMed] [Google Scholar]
- 28.Marshall SF, Deapen D, Allen M, Anton-Culver H, Bernstein L, Horn-Ross PL, et al. Validating California teachers study self-reports of recent hospitalization: comparison with California hospital discharge data. Am J Epidemiol. 2003;158:1012–20. doi: 10.1093/aje/kwg256. [DOI] [PubMed] [Google Scholar]
- 29.Greenbaum JN, Bornstein LJ, Lyman S, Alexiades MM, Westrich GH. The Validity of Self-Report as a Technique for Measuring Short-Term Complications After Total Hip Arthroplasty in a Joint Replacement Registry. J Arthroplasty. 2012;27:1310–5. doi: 10.1016/j.arth.2011.10.031. [DOI] [PubMed] [Google Scholar]
- 30.Berry DJ. Unstable total hip arthroplasty: detailed overview. Instr Course Lect. 2001;50:265–74. [PubMed] [Google Scholar]
- 31.Coventry MB. Late dislocations in patients with Charnley total hip arthroplasty. J Bone Joint Surg Am. 1985;67:832–41. [PubMed] [Google Scholar]
- 32.Hedlundh U, Ahnfelt L, Hybbinette CH, Wallinder L, Weckström J, Fredin H. Dislocations and the femoral head size in primary total hip arthroplasty. Clin Orthop. 1996:226–33. [PubMed] [Google Scholar]
- 33.Padgett DE, Warashina H. The unstable total hip replacement. Clin Orthop. 2004:72–9. doi: 10.1097/00003086-200403000-00011. [DOI] [PubMed] [Google Scholar]
- 34.Pellicci PM, Bostrom M, Poss R. Posterior approach to total hip replacement using enhanced posterior soft tissue repair. Clin Orthop. 1998:224–8. doi: 10.1097/00003086-199810000-00023. [DOI] [PubMed] [Google Scholar]
- 35.Robinson M, Bornstein L, Mennear B, Bostrom M, Nestor B, Padgett D, et al. Effect of restoration of combined offset on stability of large head THA. Hip Int J Clin Exp Res Hip Pathol Ther. 2012;22:248–53. doi: 10.5301/HIP.2012.9283. [DOI] [PubMed] [Google Scholar]
- 36.Callanan MC, Jarrett B, Bragdon CR, Zurakowski D, Rubash HE, Freiberg AA, et al. The John Charnley Award: Risk Factors for Cup Malpositioning: Quality Improvement Through a Joint Registry at a Tertiary Hospital. Clin Orthop. 2011;469:319–29. doi: 10.1007/s11999-010-1487-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Morrey BF. Difficult complications after hip joint replacement. Dislocation. Clin Orthop. 1997:179–87. [PubMed] [Google Scholar]
- 38.Woo RY, Morrey BF. Dislocations after total hip arthroplasty. J Bone Joint Surg Am. 1982;64:1295–306. [PubMed] [Google Scholar]
- 39.Fackler CD, Poss R. Dislocation in total hip arthroplasties. Clin Orthop. 1980:169–78. [PubMed] [Google Scholar]
- 40.Amstutz HC, Lodwig RM, Schurman DJ, Hodgson AG. Range of motion studies for total hip replacements. A comparative study with a new experimental apparatus. Clin Orthop. 1975:124–30. doi: 10.1097/00003086-197509000-00016. [DOI] [PubMed] [Google Scholar]
- 41.Fraser GA, Wroblewski BM. Revision of the Charnley low-friction arthroplasty for recurrent or irreducible dislocation. J Bone Joint Surg Br. 1981;63B:552–5. doi: 10.1302/0301-620X.63B4.7298683. [DOI] [PubMed] [Google Scholar]
- 42.Kelley SS, Lachiewicz PF, Hickman JM, Paterno SM. Relationship of femoral head and acetabular size to the prevalence of dislocation. Clin Orthop. 1998:163–70. doi: 10.1097/00003086-199810000-00017. [DOI] [PubMed] [Google Scholar]
- 43.Mallory TH, Lombardi AV, Jr, Fada RA, Herrington SM, Eberle RW. Dislocation after total hip arthroplasty using the anterolateral abductor split approach. Clin Orthop. 1999:166–72. [PubMed] [Google Scholar]
- 44.Esposito CI, Walter WL, Roques A, Tuke MA, Zicat BA, Walsh WR, et al. Wear in alumina-on-alumina ceramic total hip replacements: a retrieval analysis of edge loading. J Bone Joint Surg Br. 2012;94:901–7. doi: 10.1302/0301-620X.94B7.29115. [DOI] [PubMed] [Google Scholar]
- 45.Dorr LD, Malik A, Wan Z, Long WT, Harris M. Precision and bias of imageless computer navigation and surgeon estimates for acetabular component position. Clin Orthop. 2007;465:92–9. doi: 10.1097/BLO.0b013e3181560c51. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.