Abstract
Background. Applications of cost-effectiveness analysis do not typically incorporate effects on caregiver quality of life despite increasing evidence that these effects are measurable. Methods. Using a national sample of US adults, we conducted 2 cross-sectional surveys during December 2011 and January 2012. One version asked respondents to value their own experience as the family member of a person with a chronic illness (experienced sample), and the other version asked respondents to value hypothetical scenarios describing the experience of having a family member with a chronic illness (community sample). Conditions included Alzheimer’s disease/dementia, arthritis, cancer, and depression. Using standard gamble questions, respondents were asked to value the spillover effects of a family member’s illness. We used regression analysis to evaluate the disutility (loss in health-related quality of life) of having a family member with a chronic illness by condition and relationship type, controlling for the respondent’s own conditions and sociodemographic characteristics. Results. For the experienced sample (n = 1389), regression analyses suggested that greater spillover was associated with certain conditions (arthritis, depression) compared with other conditions (Alzheimer’s disease, cancer). For the community sample (n = 1205), regression analyses indicated that lower spillover was associated with condition (cancer) but not the type of relationship with the ill family member (parent, child, spouse). Conclusions. The effects of illness extend beyond the individual patient to include effects on caregivers of patients, parents of ill children, spouses, and other close family and household members. Cost-effectiveness analyses should consider the inclusion of health-related quality of life spillover effects in addition to caregiving time costs incurred by family members of ill individuals.
Keywords: health utility, cost-effectiveness analysis, caregivers, family, health-related quality of life
The effects of a family member’s illness on a caregiver’s quality of life have been well-documented.1,2 Some of this burden can be attributed to effects on the physical health of the caregiver, yet there is increasing evidence that the illness of a family member has substantial effects on a caregiver’s quality of life beyond the physical burden of caregiving as well as effects on family members who have less of a role in caregiving.3 However, the magnitude of these quality of life reductions for caregivers and other family members has not been well-documented.
Published guidelines for conducting cost-effectiveness analysis recommend the inclusion of caregiver effects.4 In the practice of cost-effectiveness analysis, however, the full scope of caregiver effects is not typically included. Typically included are direct costs associated with informal caregiving time, but quality of life reductions for the informal caregiver or other family members are not often included. This may be attributable, in part, to challenges in measuring the spillover effects on caregiver quality of life. A recent review reports that few studies have directly measured spillover on quality of life using health utility measures.5 Of these studies, results ranged from no effect on health-related quality of life (HRQoL) to a substantial and measurable negative effect on HRQoL attributable to having a family member with a chronic illness. Reported spillover varied by type of condition, relationship of ill family member, and patient age. Only 2 studies used direct elicitation methods to evaluate spillover; other studies relied on indirect methods that may not have appropriate domains for capturing spillover effects.
Other studies provide weights for instruments designed to capture the quality of life associated with the carer experience. Most of these studies have been conducted in countries other than the US and, more importantly, have included domains that go beyond those typically considered as part of the HRQoL construct, such as fulfillment and relational problems, and therefore may not be appropriate for the estimation of quality-adjusted life years in a cost-effectiveness analysis.6,7 These additional domains have been consistently identified with the carer experience8 but would require moving from conventional quality-adjusted life years to broader measures of health and well-being.9 This study uses traditional health utility elicitation techniques to value family spillover effects.
The objective of this study was to evaluate the feasibility of using a direct utility elicitation approach, the standard gamble, to measure spillover effects on HRQoL of having a family member with a chronic illness. A secondary objective was to assess whether spillover varied with type of illness, relationship, and patient age. Previous studies have suggested that spillover effects on quality of life were not limited to family members with caregiving responsibilities; therefore, we included family members with a wide range of caregiving roles to be able to determine the effect of the level of caregiving responsibility on spillover. We included both a community sample and an experienced sample to measure weights as recommended for inclusion in cost-effectiveness analyses and to explore the feasibility of valuing hypothetical spillover states.
Methods
The overall approach was to use internet-based surveys to elicit utilities for spillover health states using a direct utility elicitation approach. Direct elicitation questions used the standard gamble technique to value health states. Respondents were drawn from a national internet survey panel and included both community and experienced samples.
Study Participants
Data were collected using 2 national cross-sectional internet-based surveys during December 2011 and January 2012. The survey was administered by Knowledge Networks (now GfK). GfK is a survey research firm that maintains an internet panel of US adults and adolescents. Panel members are recruited using random digit dialing of both mobile and land lines and regular mail. If individuals agree to participate as panel members, they are asked whether they have internet access at home. If they do not have internet access, GfK provides them with internet access via tablet. Panel members who already have an internet connection prior to joining the panel are compensated with vouchers that can be used toward charges for their internet coverage. On average, panel members complete 3 or 4 surveys per month. Participants did not receive any additional compensation or incentive for completing this individual survey. The survey protocol was approved by the appropriate institutional review boards.
For the experienced sample, a “screener” questionnaire was used to identify panel members who had family members with 1 or more of 5 specific chronic conditions. Of 14,157 participants who were initially contacted, 8607 completed the screener. Panel members who met the screening criteria were then invited to participate in the valuation survey, and 1369 completed the survey. For the community sample, 2397 respondents were randomly sampled from the national US panel. Of those invited to participate, 1133 completed the survey.*
Survey Design
The experienced sample completed a survey valuing experienced health states (akin to “patient perspective” valuations) and the community sample completed a survey valuing hypothetical health states. The survey for the experienced sample asked respondents to value their own experience as the family member of a person with a chronic illness (experienced sample), and the survey for the community sample asked respondents to value hypothetical vignettes describing the experience of having a family member with a chronic illness (community sample). Chronic illnesses included in the survey were Alzheimer’s disease/dementia, arthritis, cancer, and depression.
For the experienced sample, respondents evaluated 1 of the 5 health states that they had self-identified as a condition for a family member. Data on respondent’s age and relationship with the patient were collected from the experienced sample to allow for comparison between the 2 samples.
For the community sample, respondents were randomized to 1 of 5 versions that varied the relationship (child, parent, spouse) and age of the ill family member (child, adult, senior) depending on the respondent’s age (e.g., a respondent >65 years of age would only be eligible to receive a scenario describing an adult spouse or a senior parent, while a 30-year-old respondent would be eligible to receive a child, spouse, or parent scenario) (Figure 1). The age of the hypothetical child with an illness was 5 years. Some combinations were not possible, such as child with dementia (Figure 1 describes the possible valuation sets). Respondents were then randomized to evaluate hypothetical health state descriptions for 2 of the 4 chronic conditions. The complete set of health state descriptions is available in Appendix Figure 1 (online).
Figure 1.
Experimental design by age, relationship, and condition.
*Respondents in the community sample were asked to value two hypothetical health states provided to them, resulting in 1872 observations.
Valuation Approach
All respondents valued spillover health states using both rating scale and standard gamble questions in that order. We included both approaches due to a concern that if spillover effects were small, the standard gamble might not be sensitive enough to detect a difference in HRQoL attributable to spillover. The rating scale was intended as an alternative method for respondents to start considering the value assigned to a health state from a quantitative perspective before introducing the standard gamble. Analyses presented in the results section are restricted to standard gamble responses.
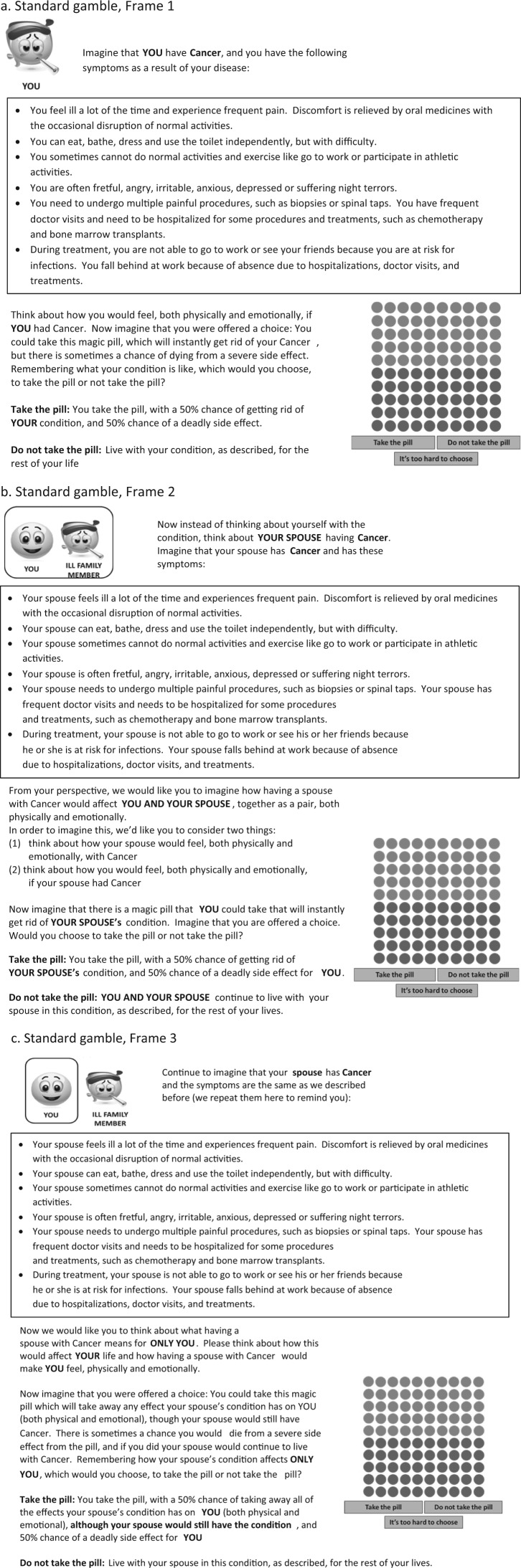
Respondents evaluated 3 question frames. Frame 1 asked the respondent to imagine how the respondent would feel if she herself had the hypothetical condition (“respondent”). Frame 2 asked the respondent to value a combined health state for both the ill family member with the hypothetical condition and the respondent as family member (“composite”). Frame 3 asked the respondent to value only her health as the family member (“spillover condition”). We provided visual aids to assist the respondent in conceptualizing the 3 different question frames. Figure 2 shows examples of the web-based standard gamble elicitation questions. Earlier research suggests that some experiences may lead to difficulties with 1 or both of these tasks. Frame 2 (composite) responds to reports that parents may not be able to disentangle effects of an ill child on the parent-child dyad. Frame 3 isolates the spillover effect but may be conceptually difficult for respondents to assess meaningfully.
Figure 2.
Standard gamble questions.
Standard gamble questions included a dot graphic to improve comprehension of probability choices (Figure 2).10 The bisection algorithm was used. Three decision rules were used to exit the standard gamble algorithm: precision of 0.01 utility at the “end of the branch,” toggling back and forth between the same 2 values more than 3 times, or selecting the third box labeled “too hard to choose.” For the last 2 exit rules, the value midpoint between the 2 last values was identified as the final value.
Survey Development
Survey development included extensive pretesting with cognitive interviews (n = 36) and a formal pilot test (n = 185) to ensure understanding of the survey frames and wording of the hypothetical health states. Pre- and pilot testing included both experienced and community respondents. A separate pretest was conducted for adolescent respondents to evaluate any additional instructions that might be necessary for this sample. The wording in the survey was targeted to an eighth grade reading level. The relatively large number of cognitive pretests reflects the complexity of the valuation task, especially for community respondents. Standard gamble questions included pop-up screens to alert respondents to illogical answers (e.g., choosing to accept a choice that included a risk of death when the other choice included 100% perfect health).
Analysis
Summary statistics were evaluated for Frame 1 (Respondent), Frame 2 (Composite), and Frame 3 (Spillover) standard gamble scores. We used regression analysis to evaluate the disutility associated with having a family member with a chronic illness. Disutility is defined as the loss in utility, calculated as 1 minus the utility of the health state being valued. The dependent variable was Frame 2 (composite) standard gamble disutility. Frame 3 spillover disutility was hypothesized to be a subset of the composite disutility assessed in Frame 2, which includes HRQoL for both respondent and ill family member.
The key independent variables were Frame 3 disutility for each condition. Frame 3 disutility by condition was evaluated using 4 interaction variables consisting of Frame 3 disutility and each specific condition, and the main effects for Frame 3 disutility and each condition. The most common condition was used as the comparison group. Additional covariates included type of relationship and the respondent’s characteristics including sociodemographics (age, education, sex, marital status, household income, household size, race/ethnicity), whether the respondent had internet access at the time of joining the panel, level of confidence in standard gamble responses, level of caregiving responsibility, and the respondent’s own health conditions. Analyses were run separately for community and experienced samples, but 1 set of models analyzed the combined sample set to test for systematic differences between community and experienced respondents. For the community sample, generalized estimating equation (GEE) regression models with negative binomial (log link) and Gaussian (identity link) distributions were evaluated. The GEE models allowed us to account for correlated responses per respondent. In the experienced sample, standard negative binomial and ordinary least squares (OLS) regression models were compared. Model fit was evaluated using the Akaike information criterion (AIC) in the experienced sample and using quasi-likelihood under the independence model criterion (QIC) in the community sample.11,12
A second set of analyses was run with some respondents excluded. Observations were excluded in this secondary analysis if respondents answered fewer than half of the valuation questions, provided the same non-zero responses for all health states/frames, or failed a logic test on the standard gamble questions. Respondents were identified as having failed the logic test if they indicated on the standard gamble that they would “take the pill” even when there was 100% chance of death or would “not take the pill” when there was a 100% chance of perfect health, even after receiving detailed reminder prompts. (These included a rephrasing of the choice that was being presented and the question “Are you sure this is what you mean?”) Only individual responses were excluded from the analytic dataset for failing the logic test; all other responses from the same respondent were included.
We simulated adjusted standard gamble disutilities for specific version, condition, and sample combinations based on the regression results from primary models. Simulated disutilities were derived from regression results using mean values for variables other than the variable of interest.
Results
Respondent Characteristics
Community Sample
Respondents in the community sample were 18 years and older and were randomly invited to participate from the existing panel of the GfK KnowledgeSample (n = 1133).13 Respondent characteristics for the community sample were similar to the US general adult population14 with some notable exceptions. Respondents were more likely to be white, to be older than 60 years, to have more education, and to have a higher reported income than the general US population. The majority of respondents (>80%) had household internet access prior to joining the panel. About half of the respondents had some familiarity with the condition described in the hypothetical scenario (48%). However, few respondents had a family member with 1 of the conditions (21%), and only 6% of the overall sample had any caregiving responsibilities (less than one-third of those with ill family members) (Table 1).
Table 1.
Respondent Characteristics
| Experienced (n = 1369) | Community (n = 1133) | |
|---|---|---|
| Age | ||
| ≥60 | 36.0% (493) | 31.5% (357) |
| 45-59 | 27.5% (376) | 31.0% (351) |
| 30-44 | 14.6% (200) | 22.3% (253) |
| 18-29 | 14.5% (198) | 15.2% (172) |
| <18 | 7.5% (102) | NA |
| Race/ethnicity | ||
| White non-Hispanic | 75.9% (1039) | 75.8% (859) |
| Black non-Hispanic | 6.4% (87) | 8.7% (98) |
| Hispanic | 10.2% (140) | 9.9% (112) |
| Other non-Hispanic | 7.5% (103) | 5.7% (64) |
| Gender | ||
| Female | 50.0% (685) | 53.3% (604) |
| Education | ||
| Bachelor’s degree or higher | 22.5% (308) | 26.9% (305) |
| Some college | 26.8% (367) | 29.1% (330) |
| High school | 31.7% (434) | 32.2% (365) |
| Less than high school, adults | 11.5% (158) | 11.7% (133) |
| Less than high school, adolescents | 7.5% (102) | NA |
| Marital status | ||
| Married/living with partner | 70.6% (966) | 64.3% (728) |
| Never married | 21.6% (295) | 19.2% (217) |
| Divorced/separated | 6.1% (83) | 11.7% (132) |
| Widowed | 1.8% (25) | 4.9% (56) |
| Household income | ||
| <$30,000 | 27.0% (370) | 25.7% (291) |
| $30,000-$59,999 | 30.0% (410) | 28.2% (319) |
| $60,000-$99,999 | 24.0% (329) | 24.5% (277) |
| ≥$100,000 | 19.0% (260) | 21.7% (246) |
| Household size | ||
| 1 | 5.7% (78) | 17.5% (198) |
| 2 | 46.3% (634) | 38.4% (435) |
| 3 | 18.5% (253) | 17.0% (192) |
| 4 | 15.8% (216) | 15.7% (178) |
| 5 | 8.0% (109) | 6.7% (76) |
| ≥6 | 5.8% (79) | 4.8% (54) |
| Household internet access | ||
| Yes | 85.6% (1172) | 81.2% (920) |
| Survey versiona | ||
| Ill family member: child | 6.6% (90) | 27.9% (316) |
| Ill family member: spouse | 57.2% (783) | 34.6% (392) |
| Ill family member: parent | 36.3% (496) | 37.5% (425) |
| Health stateb | ||
| Alzheimer’s or dementia | 6.3% (86) | 12.8% (239) |
| Arthritis | 45.0% (616) | 23.3% (436) |
| Cancer | 12.1% (166) | 31.3% (586) |
| Depression | 36.6% (501) | 32.6% (611) |
| Disease experience | ||
| Yes | NA | 62.8% (712) |
| No | NA | 37.2% (421) |
| Caregiving responsibilitiesb | ||
| All | 10.3% (141) | 1.9% (21) |
| Many | 13.2% (180) | 1.9% (21) |
| Some | 15.1% (206) | 3.4% (38) |
| Few | 8.0% (109) | 2.2% (25) |
| None | 53.3% (730) | 19.2% (217) |
| Did not care for anyone | NA | 70.9% (803) |
| Refused | 0.2% (3) | 0.7% (8) |
| Confidence in standard gamble responses | ||
| Very confident | 37.8% (518) | 30.0% (340) |
| Somewhat confident | 50.9% (697) | 52.7% (597) |
| Not confident | 7.5% (103) | 10.9% (124) |
| They were total guesses | 3.5% (48) | 5.5% (62) |
| Refused | 0.2% (3) | 0.9% (10) |
Note: NA = not applicable. Values given as % (n).
Survey version reflects the ill family member the respondent was asked to consider throughout the survey. The ill parent could have been a parent (<65 years) or an elderly parent (≥65 years); the ill child could have been a child (<18 years) or an adult child (≥18 years).
Respondents in the community sample were asked to value 2 hypothetical health states provided to them. The respondent’s highest level of caregiving responsibility is reported.
Experienced Sample
Respondents in the experienced sample were more likely to be older than the US population; more than 60% of respondents were 45 years or older (n = 1267). The experienced sample also included adolescents (ages 11-17 years) who were recruited separately from the adult sample (n = 102). The adolescent and adult experienced samples were combined for the analysis (n = 1369). Respondents in the experienced sample were also more likely to be white, more likely to be married, and more likely to have 2 or more household members compared with the general US population. Gender, education, and household income were similar to the community sample. More than 85% had internet access prior to joining the panel. For most respondents in the experienced sample, the ill family member was a spouse (57%); 36% had an ill parent and 7% had an ill child. Arthritis was the most frequent condition (45%), followed by depression (37%). Fewer respondents had family members with cancer (12%) or Alzheimer’s disease/dementia (6%). Very few respondents reported experience with a family member with cerebral palsy (n = 20); these observations were excluded from the analysis. Level of caregiving responsibilities varied: 10% of respondents reported being exclusively responsible for caregiving; 36% reported being responsible for some portion of caregiving tasks; and 53% reported having no caregiving responsibilities for the ill family member.
Standard Gamble Values
Unadjusted median disutility scores were smallest for Frame 3 (spillover only) scenarios. Median disutility scores for Frame 1 (respondent), which asked the respondent to evaluate the condition for themselves, were greater than median Frame 3 spillover disutility scores. Median disutility for Frame 2 (composite) scenario was typically between Frame 1 and Frame 3 scores (Appendix Figure 2). Frame 1 was provided to the respondents as a warm-up exercise for the spillover valuation and is not included in the regression analyses (Table 2).
Table 2.
Summary Statistics: Standard Gamble Disutilities by Condition, Sample, and Frame
| a. Standard Gamble Disutilities by Condition, Experienced Sample | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Condition | Frame | n | s | Minimum | 2.5%ile | 5%ile | 25%ile | Median | 75%ile | 95%ile | 97.5%ile | Maximum | |
| Alzheimer’s | 1 | 76 | 0.46 | 0.30 | 0.00 | 0.01 | 0.02 | 0.20 | 0.50 | 0.66 | 1.00 | 1.00 | 1.00 |
| 2 | 77 | 0.38 | 0.29 | 0.00 | 0.00 | 0.00 | 0.11 | 0.39 | 0.51 | 0.91 | 1.00 | 1.00 | |
| 3 | 74 | 0.30 | 0.26 | 0.00 | 0.00 | 0.00 | 0.05 | 0.26 | 0.50 | 0.75 | 0.99 | 1.00 | |
| Arthritis | 1 | 580 | 0.23 | 0.23 | 0.00 | 0.01 | 0.00 | 0.03 | 0.17 | 0.43 | 0.62 | 0.76 | 1.00 |
| 2 | 585 | 0.24 | 0.23 | 0.00 | 0.00 | 0.00 | 0.05 | 0.19 | 0.45 | 0.62 | 0.77 | 1.00 | |
| 3 | 536 | 0.22 | 0.24 | 0.00 | 0.00 | 0.00 | 0.02 | 0.12 | 0.39 | 0.63 | 0.87 | 1.00 | |
| Cancer | 1 | 155 | 0.39 | 0.27 | 0.00 | 0.00 | 0.01 | 0.17 | 0.39 | 0.52 | 0.99 | 1.00 | 1.00 |
| 2 | 153 | 0.38 | 0.27 | 0.00 | 0.00 | 0.01 | 0.17 | 0.38 | 0.51 | 0.96 | 1.00 | 1.00 | |
| 3 | 141 | 0.30 | 0.27 | 0.00 | 0.00 | 0.00 | 0.05 | 0.27 | 0.50 | 0.75 | 1.00 | 1.00 | |
| Depression | 1 | 475 | 0.28 | 0.24 | 0.00 | 0.00 | 0.00 | 0.05 | 0.27 | 0.50 | 0.67 | 0.88 | 1.00 |
| 2 | 473 | 0.29 | 0.26 | 0.00 | 0.00 | 0.00 | 0.05 | 0.27 | 0.50 | 0.75 | 1.00 | 1.00 | |
| 3 | 445 | 0.25 | 0.25 | 0.00 | 0.00 | 0.00 | 0.02 | 0.18 | 0.50 | 0.75 | 0.87 | 1.00 | |
| Total | 1 | 1286 | 0.28 | 0.25 | 0.00 | 0.00 | 0.00 | 0.06 | 0.25 | 0.50 | 0.75 | 0.95 | 1.00 |
| 2 | 1288 | 0.28 | 0.25 | 0.00 | 0.00 | 0.00 | 0.05 | 0.27 | 0.50 | 0.77 | 0.96 | 1.00 | |
| 3 | 1196 | 0.25 | 0.25 | 0.00 | 0.00 | 0.00 | 0.02 | 0.17 | 0.50 | 0.75 | 0.88 | 1.00 | |
| b. Standard Gamble Disutilities by Condition, Community Sample | |||||||||||||
| Condition | Frame | n | s | Minimum | 2.5%ile | 5%ile | 25%ile | Median | 75%ile | 95%ile | 97.5%ile | Maximum | |
| Alzheimer’s | 1 | 223 | 0.38 | 0.28 | 0.00 | 0.00 | 0.00 | 0.12 | 0.39 | 0.51 | 0.99 | 1.00 | 1.00 |
| 2 | 224 | 0.30 | 0.24 | 0.00 | 0.00 | 0.00 | 0.06 | 0.28 | 0.50 | 0.69 | 0.85 | 1.00 | |
| 3 | 206 | 0.25 | 0.24 | 0.00 | 0.00 | 0.00 | 0.02 | 0.21 | 0.50 | 0.62 | 0.76 | 1.00 | |
| Arthritis | 1 | 408 | 0.27 | 0.24 | 0.00 | 0.00 | 0.00 | 0.07 | 0.24 | 0.50 | 0.70 | 0.88 | 1.00 |
| 2 | 406 | 0.27 | 0.24 | 0.00 | 0.00 | 0.00 | 0.06 | 0.24 | 0.50 | 0.63 | 0.87 | 1.00 | |
| 3 | 382 | 0.27 | 0.25 | 0.00 | 0.00 | 0.00 | 0.05 | 0.20 | 0.50 | 0.74 | 0.99 | 1.00 | |
| Cancer | 1 | 539 | 0.37 | 0.27 | 0.00 | 0.00 | 0.01 | 0.13 | 0.38 | 0.51 | 1.00 | 1.00 | 1.00 |
| 2 | 552 | 0.34 | 0.26 | 0.00 | 0.00 | 0.00 | 0.11 | 0.31 | 0.51 | 0.88 | 1.00 | 1.00 | |
| 3 | 506 | 0.27 | 0.25 | 0.00 | 0.00 | 0.00 | 0.02 | 0.25 | 0.50 | 0.75 | 0.94 | 1.00 | |
| Depression | 1 | 575 | 0.30 | 0.25 | 0.00 | 0.00 | 0.00 | 0.07 | 0.27 | 0.50 | 0.75 | 1.00 | 1.00 |
| 2 | 580 | 0.30 | 0.25 | 0.00 | 0.00 | 0.00 | 0.06 | 0.27 | 0.50 | 0.72 | 0.97 | 1.00 | |
| 3 | 541 | 0.26 | 0.24 | 0.00 | 0.00 | 0.00 | 0.02 | 0.20 | 0.50 | 0.63 | 0.82 | 1.00 | |
| Total | 1 | 1745 | 0.33 | 0.26 | 0.00 | 0.00 | 0.00 | 0.11 | 0.27 | 0.51 | 0.88 | 1.00 | 1.00 |
| 2 | 1762 | 0.30 | 0.25 | 0.00 | 0.00 | 0.00 | 0.07 | 0.27 | 0.50 | 0.75 | 0.99 | 1.00 | |
| 3 | 1635 | 0.26 | 0.25 | 0.00 | 0.00 | 0.00 | 0.02 | 0.20 | 0.50 | 0.69 | 0.90 | 1.00 | |
Regression analyses for the community sample standard gamble models used GEE with a negative binomial distribution (log link) as this specification demonstrated a better fit according to AIC. Regression analyses for the experienced sample standard gamble models used a negative binomial model specification. For both samples, condition and spillover (Frame 3 disutility) were significant predictors of Frame 2 composite disutility (Table 3).
Table 3.
Effects of Condition and Respondent Characteristics on Standard Gamble Disutilities (No Exclusions)
| Standard Gamble Disutilities, Experienced Sample |
Standard Gamble Disutilities, Community Sample |
Standard Gamble Disutilities, Combined Sample |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Variables | Coef () | P Value | IRR | Coef () | P Value | IRR | Coef () | P Value | IRR |
| Intercept | 2.13 (0.06) | 0.000a | 8.44 | 2.19 (0.08) | 0.000a | 8.91 | 2.10 (0.06) | 0.000a | 8.19 |
| Alzheimer’s | 0.91 (0.18) | 0.000a | 2.50 | 0.34 (0.12) | 0.005a | 1.40 | 0.55 (0.10) | 0.000a | 1.73 |
| Arthritis | Ref | 1.00 | Ref | 1.00 | Ref | 1.00 | |||
| Cancer | 0.94 (0.13) | 0.000a | 2.55 | 0.63 (0.10) | 0.000a | 1.88 | 0.75 (0.08) | 0.000a | 2.13 |
| Depression | 0.30 (0.09) | 0.001a | 1.34 | 0.17 (0.09) | 0.070 | 1.18 | 0.25 (0.07) | 0.000a | 1.28 |
| Frame 3 disutility | 0.04 (0.00) | 0.000a | 1.04 | 0.03 (0.00) | 0.000a | 1.03 | 0.03 (0.00) | 0.000a | 1.03 |
| Alzheimer’s * Frame 3 disutilityb | −0.02 (0.00) | 0.000a | 0.98 | −0.01 (0.00) | 0.099 | 0.99 | −0.01 (0.00) | 0.000a | 0.99 |
| Arthritis * Frame 3 disutilityb | Ref | ||||||||
| Cancer * Frame 3 disutilityb | −0.02 (0.00) | 0.000a | 0.98 | −0.01 (0.00) | 0.000a | 0.99 | −0.01 (0.00) | 0.000a | 0.99 |
| Depression * Frame 3 disutilityb | −0.01 (0.00) | 0.016a | 0.99 | 0.00 (0.00) | 0.575 | 1.00 | 0.00 (0.00) | 0.022a | 1.00 |
| Sample (0 = Comm, 1 = Exp) | 0.09 (0.04) | 0.052 | 1.09 | ||||||
| Child version | 0.16 (0.12) | 0.198 | 1.17 | 0.08 (0.08) | 0.323 | 1.08 | 0.08 (0.07) | 0.220 | 1.09 |
| Spouse version (Ref) | Ref | 1.00 | Ref | 1.00 | Ref | 1.00 | |||
| Parent version | 0.01 (0.06) | 0.810 | 1.01 | 0.09 (0.07) | 0.160 | 1.10 | 0.05 (0.05) | 0.243 | 1.06 |
Note: Coef = coefficient; Comm = community; Exp = experienced; IRR = incidence rate ratio.
P < .05.
Interaction terms.
We assessed spillover disutility for specific conditions using interaction terms. A larger value for spillover disutility implies more spillover; in other words, larger values of spillover disutility can be interpreted as larger losses in HRQoL for a respondent with an ill family member. Simply put, an individual who reports more spillover disutility from having an ill family member has worse HRQoL than an individual who reports less (or no) spillover disutility. The analysis used interaction terms between Frame 3 disutility and the ill person’s condition to indicate the condition-specific spillover disutility, calculated as the sum of the coefficients between Frame 3 disutility and the interaction terms. A significant negative interaction term therefore indicated less spillover disutility for that condition relative to the reference group (arthritis). For experienced respondents, spillover disutility (i.e., loss in HRQoL) was significantly smaller for Alzheimer’s disease, cancer, and depression compared with arthritis. For community respondents, spillover disutility was significantly smaller for cancer compared with arthritis and was statistically the same for Alzheimer’s disease/dementia and depression compared with arthritis. Spillover did not vary significantly with type of ill family member for experienced or community respondents (Table 3).
Results for these key variables were consistent for models that included additional sociodemographic and other respondent characteristics. In these additional models, sociodemographic characteristics and caregiving experience were not significant for the community sample (Appendix Table 1).
Simulated Results
Using the regression results from Table 3, we simulated projected Frame 2 Composite and Frame 3 Spillover disutilities by version, condition, and sample (Figure 3).
Figure 3.
Adjusted standard gamble disutilities by version, condition, and sample (simulated).
Simulated spillover showed more variation for the experienced sample than for the community sample. For the experienced sample, there was variation across relationship and condition. Spillover disutilities were largest for an ill child. For an ill spouse, spillover was smallest for arthritis and largest for Alzheimer’s disease or dementia. For an ill parent, spillover was larger for arthritis and depression. For the community sample, spillover amounts were similar across most conditions but were slightly larger for an ill child with cancer or depression.
Secondary Analyses
Secondary analyses excluded observations if they met certain exclusion criteria (Appendix Table 2). This resulted in analytic samples of 960 for the community sample and 778 for the experienced sample (Appendix Table 3). When the sample was restricted to include only respondents who passed consistency and logic tests, results were similar for all of the regression analyses (Appendix Table 4).
Discussion
Using a direct elicitation approach, we found evidence of spillover disutility for an ill family member. Measured spillover varied by condition and family member. The magnitude of detected spillover is sufficient to argue for the inclusion of spillover effects on quality of life in economic evaluations of health interventions, at least for some conditions. In particular, we found that individuals who had family members with Alzheimer’s disease, cancer, and depression reported less spillover, meaning fewer effects on their own health-related quality of life from having an ill family member, than reported family members who had relatives with arthritis. In community perspective evaluations of spillover, we found less spillover for family members of people with cancer compared with family members of people with arthritis, which were similar to those of family members of people with Alzheimer’s disease and depression. Though these differences were statistically significant, the overall magnitude of spillover disutility from having an ill family member was similar for all 4 conditions and for both those with experience with spillover and community perspective evaluations.
The simulated results differ somewhat from the measured results. Since the simulated results predict spillover for specific combinations of condition and relationship using the regression equations for the measured results, the spillover for a simulated family member will incorporate results for both statistically significant and nonsignificant variables. The simulated results can be viewed as an alternative approach to understanding the regression results.
The literature includes few studies that have evaluated spillover effects for a family member’s illness on an individual’s quality of life. Our recent literature review found that spillover varied by condition and relationship.5 Three studies did not find any loss in HRQoL associated with spillover effects of ill family members, while 12 studies identified a loss in HRQoL associated with having an ill family member. In these 12 studies, the magnitude of measured spillover varied widely. Thirteen of the 15 studies used indirect utility instruments to measure spillover disutility. This study adds to the literature by providing a new framing approach to directly measuring spillover using standard gamble questions.
Both caregiving and caring for an ill person create spillover. Bobinac and others15 differentiate these 2 distinct effects by using the terms “caregiving effect” to refer to the welfare effects of providing informal care and “family effect” to refer to the influence of a patient on others’ well-being. Few of the respondents in our sample reported substantial caregiving responsibilities. Participants in the experienced sample were recruited based on the criterion of having an ill family member with 1 of a set of prespecified conditions. Using this recruitment approach, 53% of the experienced sample reported no (informal) caregiving responsibilities for the ill family member and only 10% reported having primary responsibility for caregiving. When controlling for level of caregiving responsibility in the regression analyses, this variable was not a significant predictor of spillover. We conducted additional stratified analyses grouping respondents into 3 levels of caregiving (all, few/some/many, none) and found no significant differences across caregiving levels (results not shown). Therefore, we provide additional evidence of measurable family effects even when controlling for caregiver effects.
The effect of individual conditions on spillover was not necessarily in the anticipated direction. For example, spillover associated with cancer was smaller than that associated with arthritis for the experienced sample. It is possible that the different durations associated with these conditions could contribute to the difference in spillover. That is, the duration for living with a cancer patient may be shorter than for arthritis, leading to a difference in HRQoL if it becomes more difficult to deal with a condition the longer one’s family member is ill. We did not collect data on duration of the experienced condition and cannot test this hypothesis, but this would be an important focus for future research. Prior research on spillover effects among a US sample using EQ-5D scores identified unexpected positive spillover from cancer in a household member under certain circumstances, suggesting that cancer may have some unique features in spillover effects.16 Similarly, there may be differential effects of conditions that affect mental or physical health that could differentially affect spillover. Accompanying qualitative research with survey respondents in the experienced sample suggests that spillover is a multifaceted experience across domains that extend beyond HRQoL and includes aspects of expectation and prognosis that we would not expect to fully capture in traditional utility measures such as the standard gamble.17 We therefore place more weight on the consistent evidence of spillover effects across our sample than in differences across conditions, recognizing that additional research on capturing the entirety of these effects is needed to fully understand the nuance of experience.
The relationship between the patient and family member was not a significant predictor of spillover disutility in our results; we found no evidence of a consistent relationship between type of ill family member and spillover disutility across samples and conditions. In particular, some have noted the likelihood of family spillover effects for childhood conditions.18,19 We conducted exploratory analyses on rating scale responses, and these are reported separately. In these exploratory analyses, we observed differential effects for ill parents and children compared with ill spouses in the rating scale disutility score models but not in the standard gamble models.20 Given possible ceiling effects for the standard gamble (insensitivity to small effects), it might not have been possible to detect a different effect by type of ill family member if the magnitude of spillover itself is small.
The patient/community dichotomy observed in utility values was explored in our study as well as the existence of spillover effects. Guidelines for cost-effectiveness analysis recommend the use of community weights for inclusion in a reference case analysis.4 We measured spillover disutility for both a community and an experienced sample and found similar results for both. We did find a trend toward greater spillover disutility for experienced respondents and less discrimination across conditions and type of ill family member for community respondents compared with experienced. This difference may indicate increased difficulty in imagining a caregiving health state. Our direct utility elicitation approach may therefore result in an undervaluation of community perspective spillover effects, similar to the differences between measured community and experienced ratings for mental and physical health. Or it may be that differences in perspective do not exist for spillover utility. Further research will be needed to determine optimal methods of eliciting community perspective values for spillover utility.
Limitations of our study include the measurement task, data analysis, sample composition, and health state scenario descriptions. Given the challenges and novelty of the spillover valuation tasks, the ordering of frames and valuation approaches were not randomized within the survey. We intentionally administered the rating scale questions first as a warm-up exercise prior to the standard gamble questions. We also developed the 3 frames specifically to aid the respondent in understanding and isolating the effects of spillover from the condition itself. As a result, we are unable to assess possible ordering effects in this analysis. Another limitation relates to the model specifications used to analyze standard gamble responses. Because the community sample includes multiple responses per respondent and the experienced sample does not, different model specifications were selected for each sample analysis, which may limit direct comparability between the models in our results. A further limitation is that the experienced sample contained adolescents whereas the community sample did not. This was due in part to our hypothesis that adolescents would have more difficulty conceptualizing a hypothetical spillover vignette and partly due to constraints of our research budget. We also did not specify duration as part of the health state descriptions and, as a result, respondents may have used different assumptions regarding remaining lifespan for the ill family member. Importantly, assumptions regarding lifespan could have varied systematically by illness (e.g., respondents could have consistently imagined a shorter life expectancy for cancer patients than for arthritis patients). This could have affected standard gamble responses and is a feature of study design that could be explored in future studies.
Our approach highlights the challenges of measuring spillover effects. Other considerations that we did not address include the definition of spillover itself. Other studies of caregiver and/or spillover effects of illness have included domains outside of those that are typically considered to define HRQoL but address broader determinants of well-being such as the quality of interpersonal relationships and life fulfillment.8 If empirical data support the inclusion of these domains in the caregiver experience, this complicates the development of recommendations for the inclusion of spillover effects in economic evaluation. The theoretical framework for quality-adjusted life years is restricted to HRQoL and does not support the inclusion on extra-individual and non-health effects. One could argue that spillover effects must be limited to those that are consistent with the conventional definition of quality-adjusted life years. However, an individual’s illness may have an effect on family members and may not be limited to HRQoL domains. If this is the case, as evidence to date suggests, then it is important for future studies of spillover effects to substantiate the existence of these effects and to include measures of well-being as well as HRQoL.
Conclusion
Incorporating family spillover effects into economic evaluations will require additional research. Our study has shown that it is feasible to measure spillover effects using direct elicitation approaches and that measured spillover varies with characteristics of the spillover condition. Increasing attention is being paid to whether such family effects should be included in an economic evaluation.1,21-23 While it is typical to include the time costs for informal care in a cost-effectiveness analysis, the quality of life effects are not typically included. This may be, at least in part, due to the potential difficulties of eliciting spillover disutilities as well as the relatively scant amount of information available on the magnitude of spillover effects for specific conditions (let alone type of relationship). We propose one possible method for valuing family effects of spillover and urge others to collect data and also test new methods for measuring spillover effects. Accurate measurement of spillover effects is a necessary precondition for incorporation into economic evaluation, which is another frontier for the complete assessment of disease burden and intervention benefit.
Footnotes
Financial support for this research study was provided by awards from the National Institute of Nursing Research (5R01NR011880) and the Agency for Health Care Research and Quality (K02 HS014010). The funding agreement ensured the authors’ independence in designing the study, interpreting the data, and writing and publishing the report.
The content is solely the responsibility of the authors. Preliminary results from this study were presented at the 4th biennial conference of the American Society of Health Economists, Minneapolis, MN, June 2012, and the 34th Annual Meeting of the Society for Medical Decision Making, Phoenix, AZ, October, 2012.
Supplementary material for this article is available on the Medical Decision Making Web site at http://mdm.sagepub.com/supplemental.
Two additional conditions were included in an initial launch of the community perspective sample, asthma and cerebral palsy. In the final launch, these conditions were omitted to address issues of completion time (so that respondents evaluated 2 instead of 3 hypothetical conditions). For the experienced sample, cerebral palsy was also initially included as 1 of the conditions, but small sample size for this condition group prevented analysis so these 20 observations were excluded from the analysis.
References
- 1. Brouwer WBF. Too important to ignore: informal caregivers and other significant others. PharmacoEconomics. 2006;24(1):39–41. [DOI] [PubMed] [Google Scholar]
- 2. Bobinac A, van Exel NJ, Rutten FF, Brouwer WB. Health effects in significant others: separating family and care-giving effects. Med Decis Making. 2011;31(2):292–8. [DOI] [PubMed] [Google Scholar]
- 3. Wittenberg E, Saada A, Prosser LA. How illness affects family members: domains of well-being affected by “spillover.” Conference Proceedings for the 34th Annual Meeting of the Society for Medical Decision Making; 2012 October 17–20; Phoenix, AZ. [Google Scholar]
- 4. Gold MR, Siegel JE, Russell LB, Weinstein MC, eds. Cost-Effectiveness in Health and Medicine. New York: Oxford University Press; 1996. [Google Scholar]
- 5. Wittenberg E, Prosser LA. Disutility of illness for caregivers and families: a systematic review of the literature. PharmacoEconomics. 2013;31(6):489–500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Al-Janabi H, Flynn TN, Coast J. Estimation of a preference-based carer experience scale. Med Decis Making. 2011;31(3):458–68. [DOI] [PubMed] [Google Scholar]
- 7. Hoefman RJ, van Exel J, Rose JM, van de Wetering EJ, Brouwer WB. A discrete choice experiment to obtain a tariff for valuing informal care situations measured with the CarerQol instrument. Med Decis Making. 2014;34(1):84–96. [DOI] [PubMed] [Google Scholar]
- 8. Al-Janabi H, Coast J, Flynn TN. What do people value when they provide unpaid care for an older person? A meta-ethnography with interview follow-up. Soc Sci Med. 2008;67(1):111–21. [DOI] [PubMed] [Google Scholar]
- 9. Al-Janabi H, Flynn TN, Coast J. QALYs and carers. PharmacoEconomics. 2011;29(12):1015–23. [DOI] [PubMed] [Google Scholar]
- 10. Corso P, Hammitt J, Graham J. Valuing mortality-risk reduction: using visual aids to improve the validity of contingent valuation. J Risk Uncertainty. 2001;23(2):165–84. [Google Scholar]
- 11. StataCorp. Stata 8 Base Reference Manual. College Station (TX): Stata Press; 2003.
- 12. Pan W. Akaike’s information criterion in generalized estimating equations. Biometrics. 2001;57(1):120–5. [DOI] [PubMed] [Google Scholar]
- 13. GfK. KnowledgePanel design summary. Available from: URL: http://www.knowledgenetworks.com/knpanel/KNPanel-Design-Summary.html
- 14. U.S. Census Bureau, Statistical Abstract of the United States. Available from: URL: http://www.census.gov/compendia/statab/
- 15. Bobinac A, van Exel NJ, Rutten FF, Brouwer WB. Caring for and caring about: disentangling the caregiver effect and the family effect. J Health Econ. 2010;29(4):549–56. [DOI] [PubMed] [Google Scholar]
- 16. Wittenberg E, Ritter GA, Prosser LA. Evidence of spillover of illness among household members: EQ-5D scores from a U.S. sample. Med Decis Making. 2013;33(2):235–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Wittenberg E, Saada A, Prosser LA. How illness affects family members: a qualitative interview survey. The Patient. 2013;6(4):257–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Prosser LA, Hammitt JK, Keren R. Measuring health preferences for use in cost-utility and cost-benefit analyses of interventions in children: theoretical and methodological considerations. PharmacoEconomics. 2007;25(9):713–26. [DOI] [PubMed] [Google Scholar]
- 19. Brouer WBF, van Exel NJA, Tilford JM. Incorporating caregiver and family effects in economic evaluations of child health. In: Ungar WJ, ed. Economic Evaluation in Child Health. New York: Oxford University Press; 2010. p 55–76. [Google Scholar]
- 20. Lavelle TA, Wittenberg E, Lamarand K, Prosser LA. Variation in the spillover effects of illness on parents, spouses and children of the chronically ill. Appl Health Econ Health Policy. 2014;12(2):117–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Garber AM, Sculpher MJ. Cost effectiveness and payment policy. In: Pauly M, McGuire T, Pedro PB, eds. Handbook of Health Economics. New York: Elsevier; 2011. p 471–97. [Google Scholar]
- 22. Meltzer DO, Smith PC. Theoretical issues relevant to the economic evaluation of health technologies. In: Pauly M, McGuire T, Pedro PB, eds. Handbook of Health Economics. New York: Elsevier; 2011. p 433–69. [Google Scholar]
- 23. Basu A, Meltzer D. Implications of spillover effects within the family for medical cost-effectiveness analysis. J Health Econ. 2005;24(4):751–73. [DOI] [PubMed] [Google Scholar]