Dear Sir,
We write to present a case report of primary malignant melanoma of the lacrimal sac.
Tumors of the lacrimal sac are rare, and most of them are benign and of epithelial origin[1]. Malignant melanoma of the lacrimal sac is even rarer accounting for 5% of lacrimal sac tumors and 0.7% of ocular melanoma[2],[3]. To our knowledge, only 27 cases with complete clinical information have ever been reported worldwide in English literature[4]–[8]. The disease has an insidious onset and masquerades as a chronic dacryocystitis. As a result, it is difficult to identify at an early stage. However, an early diagnosis is essential, because it is potentially lethal progression if therapy is delayed or inadequate.
CASE HISTORY
A 65-year-old female patient complained of a 1y history of epiphora and a slowly progressive swell in the right medial canthal area (Figure 1A). Two months before seeking medical attention, she experienced occasional bloody discharge from the right eye and epistaxis from the right nasal cavity, without any pain or visual disturbance. The patient had no previous history of regional surgery or trauma, nor history of a cutaneous or mucosal primary melanoma.
Figure 1. Photos of CT and gross specimen.
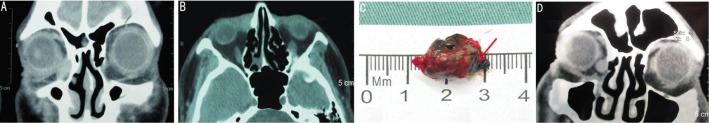
A: Photo of the patient showed edema of the right medial canthal area; B: Coronal CT scans showed a soft tissue mass in the right lacrimal sac (arrow); C: En bloc resection of the melanoma, whose transverse section was dark (arrow); D: CT showed local recurrence of melanoma one year later (arrow).
Physical examination revealed a localized well-defined non-tender palpable mass at the right medial canthus. Computed tomography (CT) showed a soft tissue mass in the fossa of the right lacrimal sac, appearing along with an enlargement of the lacrimal sac, without bony destruction (Figure 1B). The mass had a relatively clear boundary, neither infiltrating the surrounding soft tissue nor extending into the orbital cavity or nasolacrimal duct. There was no associated enlargement of the cervical lymph nodes. A dacryocystectomy was performed. A dark-red soft mass, without surrounding tissue invasion, was removed from the fossa of the right lacrimal sac. Its transverse section was completely dark (Figure 1C). Intraoperative frozen section of the mass revealed a malignant melanoma. Wide local excision was then performed, including surrounding soft tissues within 5 mm and the local periosteum.
Histopathological examination of the surgical specimen showed solid growth of malignant cells characterized by melanin pigmentation (Figure 2A). The depigmented tumor cells showed hyperchromatic nuclei with prominent nucleoli and numerous heteromorphic nuclei (Figure 2B). The features confirmed the diagnosis of malignant melanoma. A complete metastatic workup including CT of the head and neck, chest, abdomen and pelvis failed to reveal lymphadenopathy or other evidence of metastasis. By the ninth post-operative month, the patient had no evidence of local recurrence or metastasis. One-year follow-up revealed local recurrence without metastasis (Figure 1D). Then, resection of the recrudescent melanoma and local adjuvant irradiation therapy were ordered.
Figure 2. Photos of the specimen.
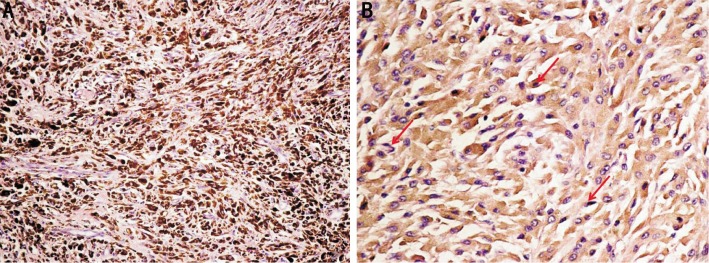
A: Heavy melanin pigmentation produced by tumor cells; B: Depigmented tumor cells showed oval nuclei with increased chromatin, prominent nucleoli and numerous abnormal mitoses (arrow). (Hematoxylin eosin staining, original magnifications: A, 200; B, 400).
DISCUSSION
The skin is most commonly affected by malignant melanoma, accounting for about 4% of all skin cancers and resulting in more than 77% of skin cancer deaths. Compared with cutaneous malignant melanoma, mucosal melanoma is rare and behaves far more aggressively. Patients with mucosal melanoma generally have a poorer prognosis despite aggressive treatment. Primary malignant melanoma of the lacrimal sac is extremely rare, because melanocytes are not normally found in the tissues of the lacrimal duct system. Most researchers believe that these melanocytes originate in the neural crest or migrate from the conjunctival sac during embryologic development.
Primary malignant melanomas of the lacrimal sac have an insidious onset and develop similar symptoms to chronic dacryocystitis, the features of which along with limited early visibility result in delayed diagnosis and poorer prognosis. Gleizal et al[4] noted that patients with primary malignant melanomas of the lacrimal sac presented with epiphora (65%), bloody discharge (35%) and pain (10%). Most patients develop a palpable or visible mass at the medial canthus, usually six months after epiphora. The average age of onset was 59y (range 38-80y). There was no significant gender difference.
The treatment varies with size and extent of the tumor, which may range from only a dacryocystectomy to wide en bloc resection, post-operative radiotherapy, chemotherapy and immunotherapy in a variety of combinations[9]. Recently, Shuman et al[10] retrospectively studied 52 patients with head and neck mucosal melanoma. With a median follow-up of 97mo, they find that the median overall survival and the disease-free survival are 52mo and 15mo respectively and surgery is the primary treatment modality. Positive surgical margins predict poorer overall survival, but the outcomes of the patients requiring re-excision to achieve negative margins are not significantly different from those of the patients initially with negative surgical margins. Early diagnosis and thorough excision are the key factors associated with improved overall survival. They also demonstrated that adjuvant radiotherapy and/or chemotherapy is not linked with an improved outcome. However, some researchers thought otherwise, who believe high-energy radiotherapy to be beneficial, regardless of the fact that melanoma is found radioresistant, as wide surgical resection in the head and neck region is often difficult[11]. Furthermore, Shuman suggested that a systemic treatment is needed because head and neck mucosal melanomas see high rates of locoregional recurrence and distant metastasis.
CONCLUSION
In summary, malignant melanoma of the lacrimal sac is extremely rare and could be difficult to diagnose because of its similar symptoms and signs to chronic dacryocystitis. In dealing with persistent dacryocystitis, especially in older patients, ophthalmologists should consider the possibility of a malignant melanoma. CT scanning is important for diagnosis. While the optimal management of the condition is not established, early diagnosis and wide excision with negative surgical margins seem to be the most effective approach. Further studies with larger patient populations and longer follow-up are needed to determine the outcomes of treatment.
Acknowledgments
Conflicts of Interest: Ren M, None; Zeng JH, None; Luo QL, None; Bi F, None; Chen J, None.
REFERENCES
- 1.Stefanyszyn MA, Hidayat AA, Pe'er JJ, Flanagan JC. Lacrimal sac tumors. Ophthal Plast Reconstr Surg. 1994;10(3):169–184. doi: 10.1097/00002341-199409000-00005. [DOI] [PubMed] [Google Scholar]
- 2.Owens RM, Wax MK, Kostik D, Linberg JV, Hogg J. Malignant melanoma of the lacrimal sac. Otolaryngol Head Neck Surg. 1995;113(5):634–640. doi: 10.1177/019459989511300520. [DOI] [PubMed] [Google Scholar]
- 3.Richtig E, Langmann G, Müllner K, Smolle J. Ocular melanoma: epidemiology, clinical presentation and relationship with dysplastic nevi. Ophthalmologica. 2004;218(2):111–114. doi: 10.1159/000076146. [DOI] [PubMed] [Google Scholar]
- 4.Gleizal A, Kodjikian L, Lebreton F, Beziat JL. Early CT-scan for chronic lacrimal duct symptoms - case report of a malignant melanoma of the lacrimal sac and review of the literature. J Craniomaxillofac Surg. 2005;33(3):201–204. doi: 10.1016/j.jcms.2005.01.012. [DOI] [PubMed] [Google Scholar]
- 5.Sitole S, Zender CA, Ahmad AZ, Hammadeh R, Petruzzelli GJ. Lacrimal sac melanoma. Ophthal Plast Reconstr Surg. 2007;23(5):417–419. doi: 10.1097/IOP.0b013e31814db537. [DOI] [PubMed] [Google Scholar]
- 6.Nam JH, Kim SM, Choi JH, Lee YK, Baek JH, Jang TJ, Park KU. Primary malignant melanoma of the lacrimal sac: a case report. Korean J Intern Med. 2006;21(4):248–251. doi: 10.3904/kjim.2006.21.4.248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Li YJ, Zhu SJ, Yan H, Han J, Wang D, Xu S. Primary malignant melanoma of the lacrimal sac. BMJ Case Rep. 2012;13:2012. doi: 10.1136/bcr-2012-006349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pujari A, Ali MJ, Mulay K, Naik MN, Honavar SG. The black lacrimal sac: a clinicopathological correlation of a malignant melanoma with anterior lacrimal crest infiltration. Int Ophthalmol. 2014;34(1):111–115. doi: 10.1007/s10792-013-9743-5. [DOI] [PubMed] [Google Scholar]
- 9.Fishman G, Ophir D. Malignant melanoma of the lacrimal sac: a case study. Am J Otolaryngol. 1999;20(5):336–339. doi: 10.1016/s0196-0709(99)90038-8. [DOI] [PubMed] [Google Scholar]
- 10.Shuman AG, Light E, Olsen SH, Pynnonen MA, Taylor JM, Johnson TM, Bradford CR. Mucosal melanoma of the head and neck: predictors of prognosis. Arch Otolaryngol Head Neck Surg. 2011;137(4):331–337. doi: 10.1001/archoto.2011.46. [DOI] [PubMed] [Google Scholar]
- 11.Gavriel H, McArthur G, Sizeland A, Henderson M. Review: mucosal melanoma of the head and neck. Melanoma Res. 2011;21(4):257–266. doi: 10.1097/CMR.0b013e3283470ffd. [DOI] [PubMed] [Google Scholar]


