We evaluated 2 combinations of existing antimicrobials for treatment of gonorrhea: gentamicin/azithromycin and gemifloxacin/azithromycin. Both regimens were efficacious, but many participants experienced gastrointestinal adverse events. These combinations may be useful options for patients who cannot be treated with ceftriaxone-based therapy.
Keywords: Neisseria gonorrhoeae, gonorrhea treatment, azithromycin, gentamicin, gemifloxacin
Abstract
Background. Ceftriaxone is the foundation of currently recommended gonorrhea treatment. There is an urgent need for backup treatment options for patients with cephalosporin allergy or infections due to suspected cephalosporin-resistant Neisseria gonorrhoeae. We evaluated the efficacy and tolerability of 2 combinations of existing noncephalosporin antimicrobials for treatment of patients with urogenital gonorrhea.
Methods. We conducted a randomized, multisite, open-label, noncomparative trial in 5 outpatient sexually transmitted disease clinic sites in Alabama, California, Maryland, and Pennsylvania. Patients aged 15–60 years diagnosed with uncomplicated urogenital gonorrhea were randomly assigned to either gentamicin 240 mg intramuscularly plus azithromycin 2 g orally, or gemifloxacin 320 mg orally plus azithromycin 2 g orally. The primary outcome was microbiological cure of urogenital infections (negative follow-up culture) at 10–17 days after treatment among 401 participants in the per protocol population.
Results. Microbiological cure was achieved by 100% (lower 1-sided exact 95% confidence interval [CI] bound, 98.5%) of 202 evaluable participants receiving gentamicin/azithromycin, and 99.5% (lower 1-sided exact 95% CI bound, 97.6%) of 199 evaluable participants receiving gemifloxacin/azithromycin. Gentamicin/azithromycin cured 10 of 10 pharyngeal infections and 1 of 1 rectal infection; gemifloxacin/azithromycin cured 15 of 15 pharyngeal and 5 of 5 rectal infections. Gastrointestinal adverse events were common in both arms.
Conclusions. Gentamicin/azithromycin and gemifloxacin/azithromycin were highly effective for treatment of urogenital gonorrhea. Gastrointestinal adverse events may limit routine use. These non-cephalosporin-based regimens may be useful alternative options for patients who cannot be treated with cephalosporin antimicrobials. Additional treatment options for gonorrhea are needed.
Clinical Trials Registration. NCT00926796.
(See the Editorial Commentary by Rice on pages 1092–4.)
The public health burden of Neisseria gonorrhoeae infections is substantial. Untreated or inadequately treated gonorrhea can cause epididymitis, pelvic inflammatory disease (PID), chronic pelvic pain, ectopic pregnancy, and tubal infertility [1, 2]. In resource-limited settings, childhood blindness from gonococcal ophthalmia neonatorum occurs in children born to infected mothers. Worldwide, approximately 106.1 million gonococcal infections are estimated to occur annually [3]. In the United States, gonorrhea is the second most commonly reported notifiable infection: 334 826 cases were reported in 2012 [4]. Many gonococcal infections go undetected or unreported; the Centers for Disease Control and Prevention (CDC) estimate that >800 000 infections occur annually in the United States among 15- to 49-year-olds [5]. The annual total direct medical cost of gonorrhea is estimated to be US$162.1 million [6].
Effective control and prevention of gonorrhea relies on prompt and effective antimicrobial therapy. However, since the introduction of antimicrobials in the 1930s, N. gonorrhoeae has progressively developed resistance to each class used for treatment, including sulfonamides, penicillins, tetracyclines, and second-generation fluoroquinolones such as ciprofloxacin [7–10]. By 2007, cephalosporin antimicrobials were the only remaining agents recommended by the CDC for empiric treatment of gonorrhea, and no new treatment options were on the horizon [10]. However, descriptions of patients with gonorrhea unsuccessfully treated with oral cephalosporins were already being reported from East Asia [11–13], and multiple countries reported increasing cephalosporin minimum inhibitory concentrations (MICs) [14].
To support public health preparedness and address the emerging threat of cephalosporin-resistant gonococcal infections, the CDC recognized that clinical efficacy and safety data on alternative therapeutic regimens for gonorrhea were urgently needed. Because no new antimicrobial treatment agents with robust efficacy data were available when this trial was designed, existing antimicrobials that were not recommended for treatment of gonorrhea were evaluated for use in combination therapy. Azithromycin monotherapy is effective for gonorrhea treatment but has not been recommended for routine use because of the ease with which N. gonorrhoeae can develop macrolide resistance [15–17]. Gentamicin, an injectable aminoglycoside that binds to the 30S ribosomal subunit and inhibits protein synthesis, has not been recommended in the United States for treatment of gonorrhea, but it has been used successfully in other countries for gonorrhea treatment, including Malawi [18]. It is chemically similar to spectinomycin (which is efficacious but not available in the United States [16]), widely available in the United States, and relatively inexpensive. Gemifloxacin, an oral fourth-generation fluoroquinolone, had not undergone clinical study for gonorrhea, but demonstrated in vitro activity against ciprofloxacin-resistant N. gonorrhoeae [19]. In vitro synergy testing of azithromycin and gemifloxacin suggested that gemifloxacin may have promise as an agent in combination therapy (CDC, unpublished data). In this trial, we evaluated the efficacy and tolerability of azithromycin plus either gentamicin or gemifloxacin for treatment of uncomplicated urogenital gonorrhea.
METHODS
Study Design
This study was a multicenter, randomized, open-label, noncomparative trial involving men and women with uncomplicated urogenital gonorrhea. Enrollment was conducted from May 2010 through November 2012. Study follow-up was completed in November 2012. The study was registered at ClinicalTrials.gov (NCT00926796).
The final protocol was approved by investigational review boards at each clinical site and the CDC. Participants provided written consent. The trial was monitored by an independent safety monitoring committee (SMC), which convened semiannually. Following the SMC meeting held in August 2012, the SMC recommended halting trial enrollment because continued participant accrual to targeted enrollment of 500 infected participants would be highly unlikely to alter the results.
Setting and Participants
Participant enrollment occurred in outpatient sexually transmitted disease (STD) clinics in Birmingham, Alabama; San Francisco and Los Angeles, California; Pittsburgh, Pennsylvania; and Baltimore, Maryland.
Patients were initially eligible for inclusion if they (1) were suspected to be infected with urethral or cervical N. gonorrhoeae (defined as untreated urethral or cervical N. gonorrhoeae identified by Gram stain demonstrating gram-negative intracellular diplococci, laboratory testing at a previous visit indicating gonorrhea, or untreated patients reporting anal, oral, or vaginal sexual contact in the past 60 days with someone diagnosed with gonorrhea), and (2) were willing to abstain from sexual intercourse or use condoms until follow-up was complete. Pregnancy tests were completed for all women; pregnant women were not enrolled.
Major exclusion criteria were age <15 years or >60 years, having a history of renal insufficiency, hepatic insufficiency, cardiac arrhythmia, neuromuscular disorders, rheumatoid arthritis, or tendon disorders; prior receipt of kidney, lung, or heart transplants; pregnancy or lactation; allergy or prior adverse reaction to macrolides, aminoglycosides, or fluoroquinolones; concomitant infection requiring systemic antimicrobial therapy (besides chlamydia); receipt of systemic or intravaginal antimicrobials within 30 days of study enrollment, or current use of corticosteroids, immunosuppressive therapy, or cardiac antiarrhythmic medication; and clinically diagnosed abdominal pain related to PID, testicular pain, epididymitis, disseminated gonococcal infection, or genital ulcer disease. Women diagnosed with bacterial vaginosis (BV) at enrollment were enrolled if they were willing to defer BV treatment until the follow-up visit. Women who did not wish to defer BV treatment were withdrawn from the study and treated in accordance with local clinic protocols.
At enrollment, clinical information and culture specimens were collected, and participants were treated according to the randomized assignment. Participants later found to have negative enrollment cervical or urethral cultures for N. gonorrhoeae were deemed ineligible and were discontinued from the study.
Randomization and Interventions
Using a permuted blocked randomization scheme with stratification by study site and allocation by numbered envelopes, participants were randomly assigned treatment in a 1:1 ratio to treatment with either gentamicin 240 mg intramuscularly (or 5 mg/kg if ≤45 kg) plus azithromycin 2 g orally, or gemifloxacin 320 mg plus azithromycin 2 g given simultaneously as single oral doses. For those who received gentamicin 240 mg, 2 separate 3-mL injections of 40 mg/mL solution were administered. Azithromycin was provided as four 500-mg tablets. A small snack was provided prior to medication administration. Participants were observed for at least 30 minutes after medication administration and were instructed to return to the clinic or contact the study coordinator immediately if vomiting occurred within 30 minutes of departing the clinic. Those who vomited within 1 hour were discontinued from the study, re-treated per the local clinic standard of care, and asked to return in 10–17 days for evaluation. Partners were evaluated and treated according to local clinic protocol.
Laboratory Procedures
At enrollment and follow-up, specimens for N. gonorrhoeae culture were collected from the urethra or cervix using polyester swabs. Pharyngeal and/or rectal specimens were collected if the participant reported exposure at the relevant anatomic site(s). Swabs were immediately smeared onto modified Thayer-Martin medium plates and placed into a candle jar or whirl bags with carbon dioxide (CO2) tablets. Cultures were either transferred to the local laboratory within 4 hours for incubation in 4%–7% CO2 or were stored at the clinic in a 4%–7% CO2 incubator and transferred to the local laboratory within 24 hours. Media were examined for N. gonorrhoeae at 24, 48, and 72 hours.
Neisseria gonorrhoeae isolates were frozen and shipped to the CDC Division of STD Prevention Laboratory Reference and Research Branch for confirmatory culture and agar dilution antimicrobial susceptibility testing. Results were interpreted according to Clinical and Laboratory Standards Institute (CLSI) criteria [20]. The CLSI does not define gonococcal susceptibility or resistance for azithromycin, gemifloxacin, or gentamicin. We categorized isolates with azithromycin MICs ≥2.0 µg/mL as exhibiting elevated azithromycin MICs. Gemifloxacin MICs ≥1 µg/mL were considered elevated [21]. Gentamicin MICs were classified as follows: susceptible, ≤4 µg/mL; intermediate susceptibility, 8–16 µg/mL; and resistant, ≥32 µg/mL [18].
Outcomes and Follow-up
The primary outcome measure was microbiologic cure, defined as a negative follow-up culture for urogenital N. gonorrhoeae 10–17 days after receipt of the study medications. Secondary outcome measures were microbiologic cure of pharyngeal and rectal infection, tolerability of each regimen, and antimicrobial susceptibility of enrollment isolates.
Statistical Analyses
This was not a comparative trial but rather a trial to establish efficacy data for 2 candidate regimens. Trial results will be used to assess whether either regimen meets the traditional CDC criteria for being a recommended (cure rate of >95% with a lower 95% confidence interval [CI] bound ≥95%) or alternative (cure rate of >95% with a lower 95% CI bound ≥90%) treatment for uncomplicated urogenital gonorrhea [22]. We anticipated a cure rate of 97% and lower 1-sided 95% CI bound of ≥95% and allowed for a 10% dropout rate. The target sample size was 250 infected participants per group.
The primary analysis used the per protocol (PP) population, which comprised all infected participants who (1) satisfied inclusion and exclusion criteria, (2) were randomized and treated, (3) returned for follow-up within 10–17 days, and (4) had an evaluable follow-up culture result. Participants who vomited within 1 hour were not included in the PP analysis. For each treatment group, we calculated the proportion of participants with urogenital gonorrhea who achieved microbiological cure and the exact binomial lower 1-sided 95% CI bound. Sensitivity analyses of microbiological efficacy were conducted using the modified intent-to-treat (mITT) population, which included all infected participants who satisfied inclusion and exclusion criteria and were randomized and treated. For the purposes of the mITT analyses, participants who were lost to follow up, vomited within 1 hour of drug administration, or whose follow-up culture results were not evaluable were considered to have failed treatment. We calculated the frequency of adverse events (AEs) among patients in the PP population and the safety population (all patients who received at least 1 dose of study medication, including those who vomited within 1 hour of drug administration). All analyses were performed using SAS version 9.3 (SAS Institute, Cary, North Carolina).
Role of the Funding Source
The study was designed by the investigators, the CDC, and the National Institute of Allergy and Infectious Diseases (NIAID) at the National Institutes of Health; sponsored by NIAID; and funded by NIAID and the CDC.
RESULTS
Participants
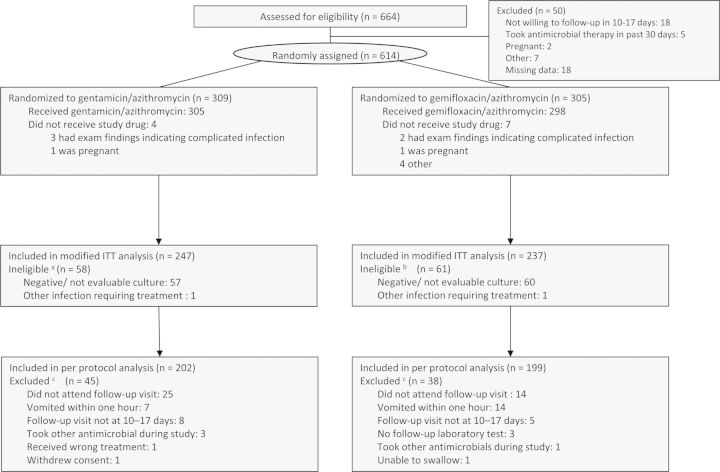
Of 664 participants with suspected gonorrhea, 614 were randomized (491 men, 121 women, and 2 participants with sex data missing), and 603 received study medication (Figure 1). Of those randomized and treated, 305 received gentamicin/azithromycin and 298 received gemifloxacin/azithromycin. One hundred nineteen individuals were found to be ineligible after randomization and treatment, of which 117 were due to negative enrollment cultures (58 were men and 59 were women).
Figure 1.
Study flow diagram. aThree of these participants vomited within 1 hour of study drug administration. bNine of these participants vomited within 1 hour of study drug administration. cParticipants may have been discontinued from the per protocol analysis for >1 reason, but only the primary reason is listed. Abbreviation: ITT, intent-to-treat.
Most participants were men, and approximately one-third of participants self-identified as men who have sex with men (MSM) (Table 1). Nearly half of the participants were enrolled in San Francisco. Of 401 participants, 152 (38%) reported sex between the initial and follow-up study visit, and 61 reported sex without a condom.
Table 1.
Selected Baseline Characteristics of Per Protocol Participants by Group
| Characteristics | Gentamicin + Azithromycin (n = 202) | Gemifloxacin + Azithromycin (n = 199) |
|---|---|---|
| Age, y, median (IQR) | 26 (22–35) | 29 (22–36) |
| Sex and sex of sex partner | ||
| Women | 19 (9.4) | 21 (10.6) |
| MSM | 67 (33.2) | 77 (38.7) |
| MSW | 116 (57.4) | 101 (50.8) |
| Self-identified race/ethnicity | ||
| Asian/Hawaiian/Pacific Islander | 6 (3.0) | 5 (2.5) |
| Non-Hispanic black | 126 (62.4) | 103 (51.8) |
| Non-Hispanic white | 44 (21.8) | 45 (22.6) |
| Hispanic or Latino | 18 (8.9) | 28 (14.1) |
| Multiracial | 7 (3.5) | 12 (6.0) |
| Other | 1 (0.5) | 6 (3.0) |
| Enrolling site | ||
| Baltimore, Maryland | 1 (0.5) | 2 (1.0) |
| Birmingham, Alabama | 60 (29.7) | 53 (26.6) |
| Los Angeles, California | 4 (2.0) | 5 (2.5) |
| Pittsburgh, Pennsylvania | 40 (19.8) | 38 (19.1) |
| San Francisco, California | 97 (48.0) | 101 (50.8) |
| Previous STD (by participant self-report) | ||
| Gonorrhea | 85 (42.1) | 92 (46.2) |
| Chlamydia | 82 (40.6) | 85 (42.7) |
| HIV infection (by participant self-report) | ||
| Positive | 19 (9.4) | 16 (8.0) |
| Negative | 159 (78.7) | 163 (81.9) |
| Unknown | 24 (11.9) | 20 (10.1) |
| Symptoms | ||
| Penile or vaginal discharge | 182 (90.1) | 179 (89.8) |
| Dysuria | 153 (75.7) | 138 (69.3) |
| Dyspareunia | 22 (10.9) | 23 (11.6) |
| Anal pain or discharge | 4 (2.0) | 2 (1.0) |
| Sore throat | 9 (4.5) | 14 (7.0) |
| Exam findings | ||
| Penile discharge (among men) | 177 (96.7) | 169 (94.9) |
| Vaginal discharge (among women) | 17 (89.5) | 20 (95.2) |
| Anal tenderness or discharge | 0 (0.0) | 1 (0.5) |
| Pharyngeal erythema or exudate | 6 (3.0) | 11 (5.5) |
| Additional infections diagnosed | ||
| Bacterial vaginosis (among women) | 9 (47.4) | 10 (47.6) |
| Chlamydiaa | 51 (25.9) | 47 (23.7) |
| Pharyngeal gonorrhea | 10 (5.0) | 15 (7.5) |
| Rectal gonorrhea | 1 (0.5) | 5 (2.5) |
Data are presented as No. (%) unless otherwise indicated.
Abbreviations: HIV, human immunodeficiency virus; IQR, interquartile range; MSM, men who have sex with men; MSW, men who report sex exclusively with women; STD, sexually transmitted disease.
a Denominators of 197 (gentamicin/azithromycin) and 198 (gemifloxacin/azithromycin) due to inevaluable results.
Efficacy
In the PP analysis, microbiological cure was achieved by 100% of participants with urogenital gonorrhea treated with gentamicin and azithromycin (lower 1-sided exact 95% CI bound, 98.5%) and by 99.5% (lower 1-sided exact 95% CI bound, 97.6%) of participants treated with gemifloxacin/azithromycin. One heterosexual male participant treated with gemifloxacin/azithromycin had N. gonorrhoeae isolated from a urethral swab collected at a follow-up visit. The MICs of this participant's pretherapy isolates of gemifloxacin, ciprofloxacin, and azithromycin were 0.004, 0.002, and 0.25 µg/mL, respectively (Supplementary Table 1). The posttherapy isolate was not available for susceptibility testing. He reported having vaginal sex without a condom between visits. All 25 participants with pharyngeal gonorrhea (15 received gemifloxacin/azithromycin and 10 received gentamicin/azithromycin) and 6 participants with rectal gonorrhea (5 received gemifloxacin/azithromycin, 1 received gentamicin/azithromycin) were microbiologically cured.
The mITT sensitivity analysis, which considers participants who vomited within 1 hour and those lost to follow-up as failing treatment, demonstrated gentamicin/azithromycin efficacy of 83.8% (lower 1-sided 95% CI bound, 80.0%) and gemifloxacin/azithromycin efficacy of 84.4% (lower 1-sided 95% CI bound, 80.5%) (Supplementary Table 2).
Tolerability
The most commonly reported AEs were mild to moderate gastrointestinal conditions. Among 202 PP participants in the gentamicin/azithromycin arm, 27.7% reported nausea, 18.8% reported diarrhea, and 7.4% reported vomiting (Table 2). Among 199 PP participants in the gemifloxacin/azithromycin arm, 37.2% reported nausea, 23.1% reported diarrhea, and 5% reported vomiting. No serious AEs occurred.
Table 2.
Percentage of Participants in the Per Protocol Analysis Reporting Adverse Events and Severitya
| Adverse Event | Gentamicin + Azithromycin (n = 202) | Gemifloxacin + Azithromycin (n = 199) |
|---|---|---|
| Nausea | ||
| Mild | 47 (23.3) | 58 (29.1) |
| Moderate | 9 (4.5) | 15 (7.5) |
| Severe | 0 (0.0) | 1 (0.5) |
| Vomiting | ||
| Mild | 13 (6.4) | 5 (2.5) |
| Moderate | 2 (1.0) | 4 (2.0) |
| Severe | 0 (0.0) | 1 (0.5) |
| Abdominal pain or discomfort | ||
| Mild | 10 (5.0) | 12 (6.0) |
| Moderate | 2 (1.0) | 9 (4.5) |
| Severe | 3 (1.5) | 0 (0.0) |
| Diarrhea | ||
| Mild | 30 (14.9) | 25 (12.6) |
| Moderate | 6 (3.0) | 20 (10.1) |
| Severe | 3 (1.0) | 1 (0.5) |
| Fatigue | ||
| Mild | 3 (1.5) | 4 (2.0) |
| Moderate | 1 (0.5) | 2 (1.0) |
| Severe | 0 (0.0) | 0 (0.0) |
| Dizziness | ||
| Mild | 4 (2.0) | 6 (3.0) |
| Moderate | 3 (1.5) | 1 (0.5) |
| Severe | 0 (0.0) | 0 (0.0) |
| Injection site pain | ||
| Mild | 1 (0.5) | 0 (0.0) |
| Moderate | 1 (0.5) | 0 (0.0) |
| Severe | 0 (0.0) | 0 (0.0) |
| Tendon disorder/tendonitis | ||
| Mild | 1 (0.5) | 2 (1.0) |
| Moderate | 0 (0.0) | 1 (0.5) |
| Severe | 0 (0.0) | 0 (0.0) |
Note: Some patients had >1 adverse event (AE). Mild: AEs require minimal or no treatment and do not interfere with the participant's daily activities. Moderate: AEs result in a low level of inconvenience or concern with the therapeutic measures. Moderate AEs may cause some interference with functioning. Severe: AEs interrupt a participant's usual daily activity and may require systemic drug therapy or other treatment. Severe AEs are usually incapacitating. See the Division of Microbiology and Infectious Diseases Adult Toxicity Tables for severity of specific syndromes, November 2007 (available at: http://www.niaid.nih.gov/LabsAndResources/resources/DMIDClinRsrch/Documents/dmidadulttox.pdf).
a AEs that occurred in >1% of participants in either arm are listed.
Among all 305 participants who received gentamicin/azithromycin (safety analysis), nearly 26% of 305 participants experienced nausea and 17% reported diarrhea (Supplementary Table 3A); 10 (3.3%) participants vomited within 1 hour of gentamicin/azithromycin administration (Figure 1). Among all 298 gemifloxacin/azithromycin recipients, 40% experienced nausea and 22% reported diarrhea (Supplementary Table 3B); 23 (7.7%) vomited within 1 hour of gemifloxacin/azithromycin administration (Figure 1).
Antimicrobial Susceptibility
From 396 PP participants, 421 pretreatment N. gonorrhoeae isolates were available for antimicrobial susceptibility testing (participants with pharyngeal or rectal infections may have contributed >1 pretreatment isolate). Elevated azithromycin MICs (≥2.0 µg/mL) were detected in 0.5% of isolates, and elevated gemifloxacin MICs (≥1.0 µg/mL) were detected in 17.1% of isolates (Table 3). Previous studies found gemifloxacin MICs to be 4-fold lower than ciprofloxacin MICs [19, 23, 24]. In contrast, our study found that gemifloxacin MICs of most isolates were the same as or 1–2 dilutions lower than the ciprofloxacin MICs. None of the isolates were resistant to gentamicin.
Table 3.
Antimicrobial Susceptibility of Pretreatment Neisseria gonorrhoeae Isolates Collected From Participants in the Per Protocol Analysis (n = 421)a
| Antimicrobial | MIC50, µg/mL | MIC90, µg/mL | Range, µg/mL | Percentage at or Above MIC Breakpoint | MIC Breakpoint for Resistance or Elevated MICs, µg/mL |
|---|---|---|---|---|---|
| Azithromycin | 0.25 | 0.5 | 0.03–16 | 0.5 | ≥2.0 |
| Cefixime | 0.015 | 0.06 | 0.001–1.0 | 1.4 | ≥0.25 |
| Ceftriaxone | 0.008 | 0.03 | 0.001–0.125 | 1.2 | ≥0.125 |
| Ciprofloxacin | 0.004 | 8.0 | 0.002–32.0 | 24.5 | ≥1.0 |
| Gemifloxacin | 0.004 | 2 | 0.001–8.0 | 17.1 | ≥1.0 |
| Gentamicin | 4 | 8 | 0.002–16 | 0 | ≥32.0 |
| Penicillin | 0.5 | 4 | 0.004–64 | 23.0 | ≥2.0 |
| Tetracycline | 0.5 | 16 | 0.03–>32 | 24.2 | ≥2.0 |
Abbreviations: MIC, minimum inhibitory concentration; MIC50, minimum inhibitory concentration required to inhibit growth of 50% of organisms; MIC90, minimum inhibitory concentration required to inhibit growth of 90% of organisms.
a Three hundred ninety-six participants provided a total of 421 isolates (participants with genital and extragenital infections may have contributed >1 pretreatment isolate).
DISCUSSION
Neisseria gonorrhoeae has acquired resistance to each antimicrobial recommended for treatment. As this trial was being conducted, gathering evidence pointed to emergence of gonococcal cephalosporin resistance. Multiple reports from Europe and recently, Toronto, Canada, described patients with gonorrhea who were unsuccessfully treated with oral cephalosporins [25–27]. Ceftriaxone-resistant isolates were identified in Japan and Europe [28–30]. Cefixime MICs increased in the United States, particularly in the western states and among MSM; in response, the CDC updated its STD treatment guidelines in 2012 to recommend dual therapy with ceftriaxone 250 mg as a single intramuscular dose plus either azithromycin 1 g orally or doxycycline 100 mg orally twice daily for a week as the only first-line treatment for gonorrhea [31]. In 2013, CDC named N. gonorrhoeae as one of 3 “urgent” antimicrobial threats [32]. Additional gonorrhea treatment options are needed.
This trial provides clinical data on 2 therapeutic options that may be useful for patients who cannot be treated with currently recommended ceftriaxone-based therapy, due to infection with ceftriaxone-resistant strains or severe cephalosporin allergy. Among participants included in the primary analysis, all urethral gonococcal infections were successfully treated with gentamicin/azithromycin, and nearly all urethral infections treated with gemifloxacin/azithromycin were cured. All of the rectal and pharyngeal gonococcal infections were cured, but only a small number of these nongenital infections were studied. Gastrointestinal AEs, especially mild nausea and diarrhea, were common. Some participants vomited within 1 hour of study drug administration, and those participants were not included in the primary analysis.
It is not entirely surprising that both combinations demonstrated excellent efficacy. As previously noted, azithromycin has demonstrated excellent efficacy as monotherapy [17], and gentamicin and gemifloxacin are active against N. gonorrhoeae. Prior to this trial, however, we lacked clinical efficacy and, importantly, safety data on the combination of these agents.
Although these combinations exhibited excellent efficacy, the burden of adverse events is likely to limit the routine use of these combinations. A substantial proportion of participants in both arms reported mild nausea, diarrhea, and vomiting, and 5% of all patients who received study drugs vomited within 1 hour. These results probably reflect the known tolerability profile of azithromycin 2 g administered orally [33]. A larger proportion of participants who received gemifloxacin/azithromycin seem to have experienced gastrointestinal AEs than participants who received gentamicin/azithromycin. This may reflect the additive contribution of gemifloxacin, which is associated with nausea, diarrhea, vomiting, and abdominal pain [34]. If prescribing either of these regimens, it might be prudent for clinicians to monitor the patient for vomiting after administration, so as to ensure adequate therapy.
Although inpatient gentamicin therapy is often limited because of potential nephro- or ototoxicity, the risk of toxicity has appeared low among healthy patients with normal renal function who received single-dose gentamicin treatment for gonorrhea [35–38]. Further investigation of the risk of nephro- or ototoxicity in young adults receiving single-dose gentamicin therapy might be useful, however. Clinicians must exercise caution when considering the use of these combinations for pregnant women: although azithromycin has been assigned to pregnancy class B by the US Food and Drug Administration, gemifloxacin has been assigned to pregnancy class C and gentamicin to pregnancy class D [33, 34, 39].
Published in vitro gemifloxacin susceptibility data indicate that gemifloxacin is active against N. gonorrhoeae, including isolates with ciprofloxacin resistance or mutations in gyrA and parC, possibly due to stronger inhibitory activity than other fluoroquinolones [19, 23, 24]. Although a gemifloxacin resistance MIC breakpoint has not been defined and the clinical relevance of the gemifloxacin MIC breakpoint used in this trial is unclear, it is nevertheless worrisome that a large percentage of isolates in this trial exhibited elevated gemifloxacin MICs. Many isolates exhibited gemifloxacin MICs that were the same as or only 1–2 dilutions lower than the ciprofloxacin MICs. Surveillance of gemifloxacin MICs and efforts to define the MIC associated with resistance may be warranted.
This study has several limitations. Because the design only included combination therapies, we are unable to define the efficacy of individual antimicrobials included in the regimens, and we are unable to clearly define the benefit of adding a second antimicrobial. A theoretical basis exists for using 2 antimicrobials to potentially delay emergence and spread of resistance, and combination therapy has been recommended for routine clinical care of gonorrhea since 2010 [16, 31]. However, the evaluation of newly developed antimicrobials should begin with the study of single agents, rather than antimicrobial combinations, so that efficacy and tolerability can initially be determined for each new drug. The study was not designed to provide the appropriate statistical power to obtain precise estimates of efficacy for pharyngeal and rectal gonococcal infections. Nonetheless, the results suggest that the studied treatments may be efficacious for extragenital infections. Enrollment of women proved challenging during the study, and many enrolled women were deemed ineligible because of negative baseline cultures. The relative underrepresentation of women might limit generalizability. These findings may not be applicable to patients aged >60 years or to those with significant comorbid medical conditions.
In summary, the results of this trial indicate that the combinations of azithromycin plus gentamicin or gemifloxacin exhibit excellent efficacy for treatment of uncomplicated urogenital gonorrhea. Cephalosporin resistance in N. gonorrhoeae is expected to emerge, and these combinations may be helpful for patients infected with ceftriaxone-resistant gonococci or patients with severe cephalosporin allergy. This trial provides much-needed data in the short term, but additional treatment options for gonorrhea are urgently needed.
Supplementary Data
Supplementary materials are available at Clinical Infectious Diseases online (http://cid.oxfordjournals.org). Supplementary materials consist of data provided by the author that are published to benefit the reader. The posted materials are not copyedited. The contents of all supplementary data are the sole responsibility of the authors. Questions or messages regarding errors should be addressed to the author.
Notes
Acknowledgments. The authors thank the patients involved in the study.
Author contributions. R. D. K. and P. C. M. had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Disclaimer. The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Financial support. This work was supported by the National Institute of Allergy and Infectious Diseases of the National Institutes of Health (grant number HHSN 26620040073C).
Potential conflicts of interest. All authors: No reported conflicts.
All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
APPENDIX
The authors thank the following contributors: Lori M. Newman (participated in study conception and design, served as initial principal investigator; CDC); Deborah Dowell (participated in study design, served as second principal investigator, secured IRB approval; CDC); Carolyn Deal (Chief, Sexually Transmitted Diseases Branch, National Institute of Allergy and Infectious Diseases [NIAID]); Jonathan Glock (clinical protocol manager; NIAID); Lalitha Venkatasubramanian (overall trial data management, developed data management plan, developed case report forms, generated monthly reports, review of manuscript; FHI360); Linda McNeil (operational oversight and guidance, reviewed study documents, contributed to significant study decisions; FHI360); Charlotte Perlowski (organizing conference calls, maintaining study records and documents; FHI360); Jeannette Y. Lee (data analysis; University of Arkansas for Medical Sciences); Shelly Lensing (data analysis; University of Arkansas for Medical Sciences); Nikole Trainor (clinical site coordinator, participant recruitment and enrollment; San Francisco Department of Public Health [SFDPH]); Shannon Fuller (participant recruitment and enrollment, data management; SFDPH); Amelia Herrera (research assistant, patient enrollment; SFDPH); Jonathan S. Carlson (laboratory culturing of N. gonorrhoeae; SFDPH Laboratory); Hanne Harbison (participant recruitment and enrollment, treatment and follow-up of participants; University of Alabama at Birmingham [UAB]); Connie Lenderman (operational oversight; UAB); Paula Dixon (conducted supplemental antimicrobial susceptibility testing; UAB); Allison Whittington (participant recruitment and enrollment, specimen collection; UAB and Jefferson County Department of Health, Birmingham, Alabama); Ingrid Macio (participant recruitment and enrollment, specimen collection, completion of case report forms; Allegheny County Health Department STD clinic and Magee-Womens Hospital of the University of Pittsburgh Medical Center [UPMC]); Carol Priest (participant recruitment and enrollment, specimen collection, treatment and follow-up of participants; Allegheny County Health Department STD clinic and Magee-Womens Hospital of the UPMC); Abi Jett (patient recruitment and enrollment; Magee-Womens Hospital of the UPMC); Tracy Campbell (participant recruitment and enrollment, completion of case report forms; Magee-Womens Hospital of the UPMC); Apurva Uniyal (project coordinator; University of Southern California, Keck School of Medicine); LaShawnda Royal (participant recruitment and enrollment, drug dispensing and accountability, completion of case report forms; Los Angeles County Department of Public Health [LACDPH]); Marisol Mejia (participant recruitment and enrollment, drug dispensing and accountability, completion of case report forms, shipping of specimens, management of IRB documents; LACDPH); Jennifer Vonghack (participant recruitment and enrollment, drug dispensing and accountability, completion of case report forms, management of IRB documents; LACDPH); Susan Tobias (participant recruitment and enrollment; Johns Hopkins University School of Medicine and the Baltimore City Health Department); Jonathan Zenilman (participated in study design, interpretation of study results; Johns Hopkins University School of Medicine). The members of the safety monitoring committee: Jill Long (medical oversight; NIAID); Alesia Harvey (data management; CDC); Kevin Pettus (conducted antimicrobial susceptibility testing; CDC); Samera Sharpe (conducted antimicrobial susceptibility testing; CDC).
References
- 1.Curran JW. Management of gonococcal pelvic inflammatory disease. Sex Transm Dis. 1979;6(2 suppl):174–80. doi: 10.1097/00007435-197904000-00024. [DOI] [PubMed] [Google Scholar]
- 2.Watson RA. Gonorrhea and acute epididymitis. Mil Med. 1979;144:785–7. [PubMed] [Google Scholar]
- 3.World Health Organization. Prevalence and incidence of selected sexually transmitted infections, Chlamydia trachomatis, Neisseria gonorrhoeae, syphilis, and Trichomonas vaginalis: methods and results used by WHO to generate 2005 estimates. Available at: http://whqlibdoc.who.int/publications/2011/9789241502450_eng.pdf . Accessed 18 March 2013. [Google Scholar]
- 4.Centers for Disease Control and Prevention. Sexually transmitted disease surveillance 2012. Available at: http://www.cdc.gov/std/stats12/default.htm . Accessed 25 April 2014. [Google Scholar]
- 5.Satterwhite CL, Torrone E, Meites E, et al. Sexually transmitted infections among US women and men: prevalence and incidence estimates, 2008. Sex Transm Dis. 2013;40:187–93. doi: 10.1097/OLQ.0b013e318286bb53. [DOI] [PubMed] [Google Scholar]
- 6.Owusu-Edusei K, Chesson HW, Gift TL, et al. The estimated direct medical cost of selected sexually transmitted infections in the United States, 2008. Sex Transm Dis. 2013;40:197–201. doi: 10.1097/OLQ.0b013e318285c6d2. [DOI] [PubMed] [Google Scholar]
- 7.Carpenter CM, Ackerman H, Winchester ME, Whittle J. Correlation of in vitro sulfonamide resistance of the gonococcus with results of sulfonamide therapy. Am J Public Health. 1944;34:250–4. doi: 10.2105/ajph.34.3.250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Centers for Disease Control and Prevention. Penicillinase-producing Neisseria gonorrhoeae—United States, 1986. MMWR Morb Mortal Wkly Rep. 1987;36:107–8. [PubMed] [Google Scholar]
- 9.Wiesner PJ, Holmes KK, Sparling PF, et al. Single doses of methacycline and doxycycline for gonorrhea: a cooperative study of the frequency and cause of treatment failure. J Infect Dis. 1973;127:461–6. doi: 10.1093/infdis/127.4.461. [DOI] [PubMed] [Google Scholar]
- 10.Centers for Disease Control and Prevention. Update to CDC's sexually transmitted diseases treatment guidelines, 2006: fluoroquinolones no longer recommended for treatment of gonococcal infections. MMWR Morb Mortal Wkly Rep. 2007;56:332–6. [PubMed] [Google Scholar]
- 11.Akasaka S, Muratani T, Yamada Y, Inatomi H, Takahashi K, Matsumoto T. Emergence of cephem- and aztreonam-high-resistant Neisseria gonorrhoeae that does not produce β-lactamase. J Infect Chemother. 2001;7:49–50. doi: 10.1007/s101560170034. [DOI] [PubMed] [Google Scholar]
- 12.Deguchi T, Yasuda M, Yokoi S, et al. Treatment of uncomplicated gonococcal urethritis by double-dosing of 200 mg cefixime at a 6-h interval. J Infect Chemother. 2003;9:35–9. doi: 10.1007/s10156-002-0204-8. [DOI] [PubMed] [Google Scholar]
- 13.Yokoi S, Deguchi T, Ozawa T, et al. Threat to cefixime treatment for gonorrhea. Emerg Infect Dis. 2007;13:1275–7. doi: 10.3201/eid1308.060948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kirkcaldy RD, Ballard RC, Dowell D. Gonococcal resistance: are cephalosporins next? Curr Infect Dis Rep. 2011;13:196–204. doi: 10.1007/s11908-011-0169-9. [DOI] [PubMed] [Google Scholar]
- 15.Centers for Disease Control and Prevention. Sexually transmitted diseases treatment guidelines, 2006. MMWR Recomm Rep. 2006;55(RR-11):1–94. [PubMed] [Google Scholar]
- 16.Centers for Disease Control and Prevention. Sexually transmitted diseases treatment guidelines, 2010. MMWR Recomm Rep. 2010;59(RR-12):1–110. [PubMed] [Google Scholar]
- 17.Handsfield HH, Dalu ZA, Martin DH, Douglas JM, Jr, McCarty JM, Schlossberg D. Multicenter trial of single-dose azithromycin vs. ceftriaxone in the treatment of uncomplicated gonorrhea. Sex Transm Dis. 1994;21:107–11. doi: 10.1097/00007435-199403000-00010. [DOI] [PubMed] [Google Scholar]
- 18.Brown LB, Krysiak R, Kamanga G, et al. Neisseria gonorrhoeae antimicrobial susceptibility in Lilongwe, Malawi, 2007. Sex Transm Dis. 2010;37:169–72. doi: 10.1097/OLQ.0b013e3181bf575c. [DOI] [PubMed] [Google Scholar]
- 19.Tanaka M, Tunoe H, Mochida O, et al. Antimicrobial activity of gemifloxacin (SB-265805), a newer fluoroquinolone, against clinical isolates of Neisseria gonorrhoeae, including fluoroquinolone-resistant isolates. Diagnost Microbiol Infect Dis. 2000;38:109–13. doi: 10.1016/s0732-8893(00)00180-2. [DOI] [PubMed] [Google Scholar]
- 20.Clinical Laboratory Standards Institute. Vol. 33. Wayne, PA: CLSI; 2013. Performance standards for antimicrobial susceptibility testing; 23rd informational supplement; pp. 100–2. CLSI document M100-S23. [Google Scholar]
- 21.Wise R, Andrews JM. The in-vitro activity and tentative breakpoint of gemifloxacin, a new fluoroquinolone. J Antimicrob Chemother. 1999;44:679–88. doi: 10.1093/jac/44.5.679. [DOI] [PubMed] [Google Scholar]
- 22.Moran JS, Levine WC. Drugs of choice for the treatment of uncomplicated gonococcal infections. Clin Infect Dis. 1995;20(suppl 1):S47–65. doi: 10.1093/clinids/20.supplement_1.s47. [DOI] [PubMed] [Google Scholar]
- 23.Ruiz J, Marco F, Sierra JM, et al. In vitro activity of gemifloxacin against clinical isolates of Neisseria gonorrhoeae with and without mutations in the gyrA gene. Int J Antimicrob Agents. 2003;22:73–6. doi: 10.1016/s0924-8579(03)00083-9. [DOI] [PubMed] [Google Scholar]
- 24.Pottumarthy S, Fritsche TR, Jones RN. Activity of gemifloxacin tested against Neisseria gonorrhoeae isolates including antimicrobial-resistant phenotypes. Diagn Microbiol Infect Dis. 2006;54:127–34. doi: 10.1016/j.diagmicrobio.2005.08.013. [DOI] [PubMed] [Google Scholar]
- 25.Ison CA, Hussey J, Sankar KN, Evans J, Alexander S. Gonorrhoea treatment failures to cefixime and azithromycin in England, 2010. Euro Surveill. 2011;16 pii:19833 Available at: http://www.eurosurveillance.org/ViewArticle.aspx?ArticleId=19833 . Accessed 9 June 2013. [PubMed] [Google Scholar]
- 26.Unemo M, Golparian D, Syversen G, Vestrheim DF, Moi H. Two cases of verified clinical failures using internationally recommended first-line cefixime for gonorrhoeae treatment, Norway, 2010. Euro Surveill. 2010;15 doi: 10.2807/ese.15.47.19721-en. pii: 19721. [DOI] [PubMed] [Google Scholar]
- 27.Allen VG, Mitterni L, Seah C, et al. Neisseria gonorrhoeae treatment failure and susceptibility to cefixime in Toronto, Canada. JAMA. 2013;309:163–70. doi: 10.1001/jama.2012.176575. [DOI] [PubMed] [Google Scholar]
- 28.Ohnishi M, Golparian D, Shimuta K, et al. Is Neisseria gonorrhoeae initiating a future era of untreatable gonorrhea? Detailed characterization of the first strain with high-level resistance to ceftriaxone. Antimicrob Agents Chemother. 2011;55:3538–45. doi: 10.1128/AAC.00325-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Unemo M, Golparian D, Nicholas R, Ohnishi M, Gallay A, Sednaoui P. High-level cefixime- and ceftriaxone-resistant Neisseria gonorrhoeae in Europe (France): novel penA mosaic allele in a successful international clone causes treatment failure. Antimicrob Agents Chemother. 2012;56:1273–80. doi: 10.1128/AAC.05760-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cámara J, Serra J, Ayats J, et al. Molecular characterization of two high-level ceftriaxone-resistant Neisseria gonorrhoeae isolates detected in Catalonia, Spain. J Antimicrob Chemother. 2012;67:1858–60. doi: 10.1093/jac/dks162. [DOI] [PubMed] [Google Scholar]
- 31.Centers for Disease Control and Prevention. Update to CDC's sexually transmitted diseases treatment guidelines, 2010: oral cephalosporins no longer a recommended treatment for gonococcal infections. MMWR Morb Mortal Wkly Rep. 2012;61:590–4. [PubMed] [Google Scholar]
- 32.Centers for Disease Control and Prevention. Antibiotic resistance threats in the United States, 2013. Available at: http://www.cdc.gov/drugresistance/threat-report-2013/pdf/ar-threats-2013-508.pdf#page=5 . Accessed 25 April 2014. [Google Scholar]
- 33.Zithromax (azithromycin tablets) and (azithromycin oral suspension) [package insert] New York: Pfizer; 2007. [Google Scholar]
- 34.Factive (gemifloxacin mesylate) tablets [package insert] Waltham, MA: Oscient Pharmaceuticals; 2008. [Google Scholar]
- 35.Hantschke D, Strauss P, Linzenmeier G, Gahlen D, Heller W. Treatment of gonorrhoea with single injections of gentamicin. Brit J Vener Dis. 1973;49:62–4. doi: 10.1136/sti.49.1.62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Tan NJ, Rajan VS, Pang R, Sng EH. Gentamicin in the treatment of infections due to penicillinase-producing gonococci. Brit J Vener Dis. 1980;56:394–6. doi: 10.1136/sti.56.6.394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hira SK, Attili VR, Kamanga J, Mkandawire O, Patel JS, Patel MI. Efficacy of gentamicin and kanamycin in the treatment of uncomplicated gonococcal urethritis in Zambia. Sex Transm Dis. 1985;12:52–4. doi: 10.1097/00007435-198501000-00011. [DOI] [PubMed] [Google Scholar]
- 38.Felarca A, Laqui EM, Ibarra LM. Gentamicin in gonococcal urethritis of Filipino males: dosage and response. J Infect Dis. 1971;124:S287–92. doi: 10.1093/infdis/124.supplement_1.s287. [DOI] [PubMed] [Google Scholar]
- 39.Gentamicin injection [package insert] Schaumberg, IL: APP Pharmaceuticals, LLC; 2008. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.