Abstract
The obesity epidemic calls for greater dissemination of nutrition-related programs, yet there remain few studies of the dissemination process. This study, guided by elements of the RE-AIM model, describes the statewide dissemination of a simple, point-of-purchase restaurant intervention. Conducted in rural counties of the Midwest, United States, the study targeted randomly selected, non-chain, family-style restaurants. Owners were recruited through mail, then telephone follow-up. Data were collected through telephone at baseline, and 3, 6, 12 and 18 months post-adoption. Using mixed methods, measures captured the program adoption rate, characteristics of adopters and non-adopters, program implementation and maintenance issues, and owner and customer satisfaction. Analyses involved descriptive statistics and summaries of qualitative data. The program adoption rate was 28%. Adopters were similar to responding non-adopters demographically, but varied in attitudes. The majority of restaurants maintained the program for at least 12 months. Adopters and their customers expressed satisfaction with the program. With some adjustments, the RE-AIM model was helpful in guiding evaluation of this process. Results provide implications for future dissemination of this and other programs with regard to research procedures and potential barriers that may be encountered. Research on alternative strategies for widespread dissemination of such programs is needed in this and other settings.
Introduction
The obesity epidemic has led public health leaders to call for the development and widespread dissemination of effective programs and policies addressing nutrition-related behaviors [1-3]. Due to the established complexity of these behaviors, multi-component interventions are often designed in hopes of demonstrating a significant effect. One challenge of even very well-tested, multi-component interventions is that they may require resources beyond the capacity of many community settings [1, 4]. Designing and testing interventions in very close collaboration with community sites that would actually implement them (e.g. clinics, schools and worksites) helps to reduce this problem, but subsequent widespread dissemination to other settings that may be less motivated, experienced or resourced still remains a challenge [4, 5]. This has led to increased interest in research on the dissemination and implementation process itself [6].
There remain a relatively small number of published studies involving widespread dissemination of nutrition-related programs [4, 7-9]. And in particular, there is much more to learn about successful dissemination of health promotion programs to rural areas. Health promotion in the context of rural communities, in general, is understudied. Such communities often have few resources and lack extensive experience in implementing nutrition-related programs, thus, implementing complex programs may be especially problematic [10, 11]. This report describes the statewide dissemination of a simple, point-of-purchase intervention to rural, owner-operated restaurants. The intervention was designed with dissemination in mind, working in close collaboration with rural restaurant owners. This dissemination study, together with earlier study phases, was guided by the RE-AIM model [12, 13]. This model, with its major dimensions of Reach, Effectiveness, Adoption, Implementation and Maintenance, has been utilized in many other studies to plan and evaluate interventions and policies, attending to both internal and external validity issues. Although earlier phases examined the reach and effectiveness of this restaurant program [14], the purpose of this phase of the study was to examine the adoption rate of the program and to describe implementation and maintenance issues.
Previous study phases
The restaurant intervention itself is described in detail elsewhere and is summarized here [14]. This intervention targeted owner-operated restaurants in a rural Midwest state because they are not affected by recent menu labeling laws, and at the same time, are most likely to serve families. Although point-of-purchase interventions such as this are expected to result in only modest behavioral changes at the individual level, the population impact on health is anticipated to be substantial [15]. In preliminary work, it was learned that owners were not willing to change their menus or be trained to prepare food more healthfully because of their fear of losing regular customers. Thus, the collaboratively devised and tested intervention involved placement of table signs that encourage customers to ask for healthy adjustments or options when ordering; for example, have meat baked or broiled instead of fried, toppings on the side or smaller portions for some items. The options listed on the table signs were adjustments that were already available, but not advertised. Owners also placed signs in the front window or entryway that stated ‘Ask About our Healthy Options Program’. The program was initially tested in one restaurant using a pre–post design, then in four additional restaurants where a baseline and three follow-up customer surveys were conducted over the course of a year (a total of 1031 surveys). Customer survey results were extremely consistent across all restaurants and over time, with 70% of customers stating they noticed the signs (reach) and 34% stating the signs affected their order (effectiveness). The positive response of the owners and customers led to this next phase of study, a statewide dissemination.
Methods
Participation and recruitment
All study procedures were approved by the Institutional Review Board of the University of Iowa. Following the recommendations of the RE-AIM model [12], a denominator of restaurants was established so that an intervention adoption rate could be determined. A denominator of 100 rural, owner-operated restaurants was identified using the publicly available, electronic, searchable database of licensed restaurants in the state. This number was selected after considering the likely adoption rate given results in another restaurant dissemination study [9], and the study resources (time and staff) available to conduct the follow-up contacts with adopters. Figure 1 outlines the selection process. The overall intent was to identify restaurants that were similar to those that participated in the earlier studies of the intervention. Of the 99 counties in the state, 88 were identified as rural, which was defined as having no city with 50 000 or more residents [16]. The licensing database allowed identification and exclusion of chains, catering businesses, bars and those in business for <1 year, leaving a sample of 445 restaurants. These were contacted by phone to confirm whether they met inclusion criteria of being family-style, sit-down restaurants, open at least 5 days per week, full menu and not primarily specialty/ethnic (e.g. bakery, pizza and Chinese). Some were excluded at this stage because they had disconnected phone numbers and were presumed closed. This process left 286 restaurants to which additional exclusion criteria were applied: not located on an interstate, not in a town with a college or university and not in a town with over 20 000 residents and adjacent to a metro area. From the resultant list of 223, 100 restaurants were selected. First, one restaurant was selected from each county (83 rural counties had at least one eligible restaurant at this stage). Second, an additional 16 restaurants were selected from counties with high poverty rates (12–17%) from different towns than those already chosen. This was an attempt to assure representation from areas that are often unreached by health promotion programs. Finally, to reach 100, one restaurant was chosen from the first alphabetically listed county with a restaurant meeting all criteria. In the final denominator of 100 restaurants, there were no counties with more than two restaurants selected, and none were in the same town.
Fig. 1.
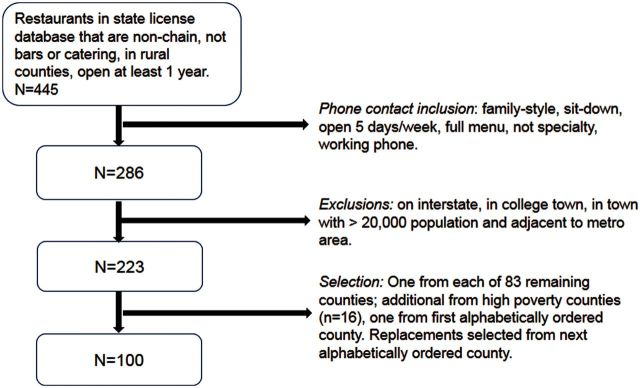
Restaurant sample selection process.
Restaurants were recruited in batches of approximately 25 over a period of 6 months. First, the list of restaurants in the batch was sent to a state health department collaborator who forwarded the list through e-mail to directors of county health departments whose counties had at least one restaurant on the list. This communication included a letter from the research team explaining the study and asking the director to contact the owners of the restaurants in their county to let them know a mailing would soon arrive from the researchers inviting them to take part in the study. Thus, the purpose of this contact from the director was solely to provide a local ‘heads up’ regarding the study, not to secure consent from the owners. Two weeks after this communication, a mailing was sent to the restaurant owner that included a brochure describing the free program, and a letter which informed the owner that this project was a research study. The letter explained that, if they consented to participate, they would be asked to complete a brief telephone interview prior to implementation of the intervention and at 3, 6, 12 and 18 months after implementation. On a return form, a list of healthy options for the table signs was provided which was derived from the previous studies. The list also included a blank space for other options desired by the owner. Owners were instructed to choose up to seven healthy options for their table signs, to indicate whether they wanted a window/entry sign and to indicate the name of the local newspaper(s) where they would like a press release about their participation to be sent.
Three weeks after the invitational mailing, owners were contacted by telephone to confirm the information on the return form if it was already submitted, or if it was not, to ask the owner if they received the mailing and/or had any questions about the study. If verbal consent was obtained at that time, the baseline interview was conducted. A second mailing was sent if needed, followed by additional telephone contact. If the telephone number of the restaurant was found to be disconnected or had no answer after multiple attempts at different days and times, the restaurant was removed from the denominator and replaced with another restaurant following selection procedures outlined above, i.e. selecting from the counties in alphabetical order where there remained eligible restaurants. There were 25 such replacements made to retain the denominator of 100.
Follow-up with adopters
Adopters were mailed the table and window signs. After confirming placement of the signs, a press release describing the restaurant’s participation in the study was sent to the preferred local newspaper. Adopters were contacted by phone for interviews at 3, 6, 12 and 18 months after adoption. When restaurants were co-owned, the person who originally consented to participate in the study was asked to complete all follow-up interviews.
Measures
The baseline telephone interview assessed characteristics of the owner and the restaurant through a mix of quantitative and open-ended, short answer items. These data were collected for descriptive purposes and/or to compare adopters with non-adopters. This interview took ∼5–10 min. Owners were asked the main reason, and any other reasons, they decided to participate or not to participate in the study; whether anything would make it easier for them to participate; whether they were contacted about the study by their local health department (yes/no) and whether they talked with anyone else prior to making the decision to participate (yes/no; with whom). Respondents were also asked whether they had participated in a healthy eating program before (yes/no; name of program) and whether they have tried on their own to provide more healthy options (yes/no) and what those efforts entailed. Owners were asked how important it is to them to provide healthy food options for their customers (not at all important/somewhat important/very important). Items about the restaurant included asking how many years the restaurant has been in business, how many customers are served in an average week and the owner’s confidence level that the restaurant will still be in business 2 years from now (not at all confident/somewhat confident/very confident). Finally, owners were asked to provide their age, highest level of education completed (<high school/high school/2-year or trade/4-year college/graduate school) and gender (if not already ascertained).
The follow-up surveys were focused on implementation and maintenance of the program. Owners were asked whether all the table signs were in place and if not, why not. They were also asked to describe any comments received from customers or wait staff about the program since the last time they were interviewed, and whether there is anything they would change about the program. Owners were asked to describe any changes to their menu offerings since the last time they were interviewed that would make it easier for customers to make healthy choices. At the 12-month follow-up only, owners were asked how much they would have been willing to pay for the program, if anything.
Data management and analysis
Quantitative data obtained from telephone surveys were double entered for later descriptive analysis using SPSS (SPSS version 20; IBM Corp., Armonk, NY, 2011). The adoption rate was calculated as the number of owners who agreed to participate in the program divided by denominator (100). Chi-square analyses and t-tests were used to compare data from adopters and non-adopters. Qualitative (short answer) data were reviewed and categorized into themes at each time point by two study team members using a consensus process. Due to the strong similarities in these categorized data across the follow-up time points, these were combined and summarized for each survey question.
Results
A total of 28 restaurants adopted the program (i.e. adoption rate = 28%) representing 26 counties well-distributed across the state. All adopters completed the majority of the baseline survey, along with 33 of the 72 non-adopters. Gender of the owner was ascertained for all 100 owners. The number of calls required to secure an adoption decision ranged from 0 (return forms submitted prior to any phone contact) to 35 calls, with a median of 6.0 for adopters, and a range of 1–28 calls, median 3.5, for non-adopters. Typically, when multiple calls were made, the phone was answered but the owner was not available at the moment.
Characteristics of adopters versus non-adopters
Table I shows characteristics of the program adopters and non-adopters and their restaurants. Adopters were more likely than non-adopters to have tried to make healthy changes to their offerings in the past (P = 0.02), to think that it is important for them to provide healthy options (P = 0.001), and to be more confident that their restaurant would still be open in 2 years (P = 0.03). No demographic or other differences were noted on the quantitative items.
Table I.
Characteristics of adopters versus non-adopters completing the baseline surveya
| Characteristic | Adopters N = 28 | Non-adopters N = 33 | P-valueb |
|---|---|---|---|
| % Women (total n = 100; n, %) | 21 (75) | 47 (65) | 0.35 |
| Mean age (SD) | 53 (10.9) | 51.9 (8.9) | 0.74 |
| Education completed (n, %) | 0.37 | ||
| Less than high school | 0 | 2 (5) | |
| High school | 16 (57) | 13 (42) | |
| 2-year/trade | 6 (21) | 10 (32) | |
| 4-year college | 6 (21) | 5 (16) | |
| Graduate school | 0 | 1 (3) | |
| Mean number of years in business (SD) | 17.3 (20.0) | 18.8 (19.0) | 0.77 |
| Mean number of customers per week (SD) | 840 (610.0) | 892 (1316.6) | 0.86 |
| Contacted by local health department (yes; n, %) | 8 (29) | 2 (6) | 0.06 |
| Spoke with other about adoption decision (yes; n, %) | 9 (32) | 7 (21) | 0.33 |
| Tried on own to provide healthy options (yes; n, %) | 24 (86) | 19 (58) | 0.02 |
| Importance of providing healthy options (n, %) | 0.001 | ||
| Not at all important | 0 | 2 (6) | |
| Somewhat important | 4 (14) | 17 (52) | |
| Very important | 24 (86) | 13 (39) | |
| How confident the restaurant will still be in business 2 years from now (n, %) | 0.03 | ||
| Not at all confident | 0 | 7 (21) | |
| Somewhat confident | 6 (21) | 6 (18) | |
| Very confident | 22 (79) | 19 (58) |
aThere were 72 non-adopters; however, only 33 of these were willing to complete the baseline survey. Gender information was available for all 100 participants.
bChi-square or t-test as appropriate.
With regard to the short answer items, the top reasons for adopting the program were: it lets customers know what options the restaurant has, the restaurant already provides healthy options so the program is consistent with this and the program promotes awareness of nutrition and healthy eating and they want to help others. The top reasons for not adopting the program were: no time, not interested, no healthy options available, small restaurant and already provide healthy options. Most owners who consulted another person in the adoption decision consulted a spouse. Only one owner (an adopter) stated that they participated in a restaurant healthy eating program in the past, but they did not remember the name of it. Of those who stated that they had tried on their own to provide healthy options, the most common examples of changes were: providing fresh food, fruits and vegetables; grilled or low-fat foods; healthy salads; promoting a healthy option through a ‘special’; adding more choices within a food group; offering homemade foods and personalizing orders.
Implementation
On average, owners requested 20 table signs (SD 10.8), with a range of 4–50. Table II indicates the healthy options that adopters chose to have on their table signs. Options selected by at least 75% of owners included: low-fat salad dressing, meat/fish that is grilled or baked instead of fried, whole wheat breads, toppings available on the side and smaller portions available for some items. Twenty-five owners (89%) also requested a window/entryway sign.
Table II.
Program adopters’ selections for their table signs (n = 28)
| Option | Selected by adopter n (%) |
|---|---|
| Whole wheat breads | 26 (93) |
| Low-fat salad dressing | 25 (89) |
| Smaller portions available for some items | 23 (82) |
| Meat/fish that is grilled or baked instead of fried | 22 (79) |
| Toppings available on the side | 22 (79) |
| Low-fat milk | 20 (71) |
| Vegetable side options available | 19 (68) |
| Other | 17 (61) |
| Fruit side options available | 11 (39) |
| Leave out one or more high-fat ingredients | 8 (29) |
| Low-fat dessert | 3 (11) |
All owners who requested signs subsequently reported placing them on the tables. In follow-up surveys, a few variations in implementation were noted. For example, one restaurant reported removing the signs temporarily so that there would be room for Christmas decorations. Another temporarily exchanged the list of healthy options for an advertisement of a motorcycle event in a subset of the signs. One owner reported they removed the signs temporarily and then returned them at a later date so that the signs would be freshly noticed by customers.
Maintenance
Of the 28 restaurants that adopted the program, there were 14 who reported still using the table signs at the 18-month follow-up point. One restaurant closed between the baseline and 3-month follow-up, a second closed between the 3- and 6-month follow-up, four discontinued the signs between the 6- and 12-month follow-up and eight discontinued the signs between the 12- and 18-month follow-up, one of these upon closing the restaurant. Two restaurant owners indicated they may place the signs out again at a later date. Thus, the sample sizes at 3-, 6-, 12- and 18-month assessments were 27, 26, 22 and 14, respectively. For those that did not close, the primary reasons given for removing the signs were that customers were not paying attention to them anymore and signs were in the way of other things they wanted to put on the table.
When asked if the window/entry sign was still in place, most owners responded ‘yes’, with 74%, 73%, 68% and 67% at each time point, respectively. The reasons given for removal were that they discontinued the program and the sign did not stay in place well.
In response to whether they had made any healthy changes to their menu since the last telephone interview, 44%, 38%, 29% and 48% at each time point said yes. The most common changes reported across time points were: adding more fresh fruit or vegetables; more salads; more grilled items and more low-fat/calorie items, especially salad dressing.
Understandably, owners had fewer novel customer comments to report as the program continued over time. While some owners could not recall any specific customer comments, the most frequent customer comments included: they like or appreciate the program, customers made specific reference to items on the sign when ordering or asked questions about healthy items. Owners did not report any outright negative reactions from customers.
The follow-up survey asked about comments the owner had received from wait staff, and this generated only a few, though all positive, responses regarding wait staff satisfaction with the program. When asked whether they would change anything about the program, most owners responded no (89%; 88%, 75% and 86%, respectively, across the 3-, 6-, 12- and 18-month follow-up points). The few who responded yes to this question suggested the following changes: change appearance of the sign (e.g. add decorative pictures or designs), put signs out intermittently to keep it fresh, add more information about the healthy options and/or advertise the program more.
At the 12-month follow-up only, owners were asked what they would have been willing to pay for the program if it were not free. All owners initially responded that free would be best. Those that offered an amount suggested amounts of 10, 20 (two owners), 50 and 75 dollars. The cost of the plastic table sign holders was <$2.00 each. The average total cost of materials provided to each restaurant (table signs and laminated window sign) was $98.00.
Discussion
This study demonstrated the successful adoption of a simple point-of-purchase intervention in 28% of rural restaurants invited to participate, with the majority maintaining the program for at least 12 months. Given the novelty of both the program and the setting, these adoption results are difficult to compare to other studies. A recent systematic review of restaurant studies identified this program as the only one focused on rural populations [17]. In addition, most studies do not report an adoption rate; however, the Shape Up Somerville program conducted in family-style restaurants in an urban setting also reported a 28% adoption rate [9]. That program provided a ‘seal of approval’ if a restaurant offered smaller sized portions, fruits or vegetables as side dishes or entrees, low-fat or non-fat dairy products, and also highlighted healthier options on a menu board, menu or other signage. Compared with the present study, implementation required more work for owners (e.g. marking menus) and many owners did not follow through with all required components. Recruitment was also conducted face-to-face rather than through mailings and phone calls.
Other findings provide insight into how dissemination might be improved in the future for this or similar programs. Reasons for non-adoption were provided by those willing to complete a baseline survey but are unknown for the remainder. Interestingly, those who were least secure about the future financial viability of their restaurant were less likely to adopt the program, perhaps seeing involvement in the study as just ‘one more thing’ to distract them from the business. This barrier could be very difficult to overcome in future dissemination efforts. Other restaurant studies have also reported time constraints and/or general disinterest as barriers to participation [9, 17, 18]. Also, the program was presented as part of a research study and it is possible that, despite a generally favorable attitude toward offering healthy options, some restaurant owners were wary of participating in research. It appears that only a portion of local health department directors contacted the owners as requested, which may have also reduced the odds of adoption. Our previous experience with rural, local health departments suggests that they are often overwhelmed with completing their required duties and have little time or resources for health promotion. Future studies should explore other local mechanisms for approaching owners about program adoption and perhaps include some remuneration for engaging in this process. All adopters indicated great interest in newspaper coverage of their participation in the program, which is consistent with other restaurant studies [9, 17, 18]. Media coverage may serve as an incentive to adopt the program and/or as an encouragement to maintain participation.
Results regarding the most preferred options for the table signs may be helpful in informing other restaurant-based interventions. For example, few owners have fresh fruit available on a regular basis and they therefore declined to list this on their table signs, while having low-fat dressing or whole wheat bread was fairly common. Restaurant owners may be more amenable to changing some menu items compared with others and these could be targeted in future interventions.
The program was successfully maintained for at least 12 months in most restaurants, and for at least 18 months in many. Overall, the program appears to start a ‘conversation’ of sorts between customers, wait staff and owners about the offerings in restaurants, with the potential to increase the availability of healthy options over time. Such an exchange may make the signs themselves eventually unnecessary.
Early applications of the RE-AIM model were focused on more traditional health education or health promotion programs and their implementation into fairly complex settings such as clinics and schools. Researchers have since noted that dissemination of policies [19] and dissemination of built environment interventions [20] may require some adjustment to measurement of model elements. Similarly, some aspects of the RE-AIM model were difficult to apply given the nature and setting of this program. For example, the simplicity of the program meant that no training was required, and the notion of ‘staff-level adoption rates’ was not relevant [13]. The simplicity of implementation also left little to evaluate in that realm though some minor variations in sign placement were noted. Some tasks, such as creating the signs and press releases with an electronic template, were completed by researchers. If these tasks were left to the owners, a local health department or a community coalition, the implementation findings may also have been different. Given the very brief nature of this point-of-purchase intervention, indicators of individual-level attrition and broader outcomes such as quality of life were not feasible to capture. Also, measurement of the primary dimensions of RE-AIM occurred in phases over time, rather than in one study. It was not feasible, or deemed necessary, to repeat the customer surveys in this statewide dissemination phase. As others have noted, a phased approach to RE-AIM model application may be needed in other situations as well [21].
Limitations of the study include the specific nature and setting of the program, such that results may not apply in other settings or with programs that are significantly different. There are, however, many rural areas within the country, and also many low-resource communities for whom the findings will be helpful when considering program dissemination. Having a larger number of adopters could have yielded additional, important information and more interpretable data regarding trends over time (e.g. reports of changing menu items). The comparison between adopters and non-adopters, however, appeared to be adequate to detect differences in relevant attitudes. Data were self-reported and adopters were self-selected and found to be more interested in healthy options than non-adopters which might affect responses to survey items in some way. Telescoping of recall could also have resulted in over-reporting on some items. With very few widespread dissemination studies to compare with, it is difficult to judge the extent to which the adoption rate obtained in this study could be improved, and there is much more work to be done in this area of research. It is likely the simplicity of the program contributed to its successful implementation and maintenance.
Overall, this program was appreciated and maintained by owners who adopted it and appeared to be acceptable to their customers. The formative and collaborative work conducted with similar restaurants prior to broader dissemination likely contributed to successful program implementation and maintenance. This study provides evidence that there remain some challenges to widespread dissemination of even a fairly simple and free health promotion program. Research on alternative strategies for widespread program dissemination is needed in this and other settings.
Conflict of interest statement
None declared.
Funding
This journal article was supported by Cooperative Agreement Number 1-U48DP001902-01 from the Centers for Disease Control and Prevention. The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
References
- 1.Glasgow RE, Green LW, Klesges LM, et al. External validity: we need to do more. Ann Behav Med. 2006;31(2):105–8. doi: 10.1207/s15324796abm3102_1. [DOI] [PubMed] [Google Scholar]
- 2.Miller AL, Krusky AM, Franzen S, et al. Partnering to translate evidence-based programs to community settings: bridging the gap between research and practice. Health Promot Pract. 2012;13(4):559–66. doi: 10.1177/1524839912438749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Glanz K. Behavioral research contributions and needs in cancer prevention and control: dietary change. Prev Med. 1997;26(5):S43–S55. doi: 10.1006/pmed.1997.0209. [DOI] [PubMed] [Google Scholar]
- 4.Allicock M, Campbell MK, Valle CG, et al. Evaluating the dissemination of Body & Soul, an evidence-based fruit and vegetable intake intervention: challenges for dissemination and implementation research. J Nutr Educ Behav. 2012;44(6):530–8. doi: 10.1016/j.jneb.2011.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Klesges LM, Estabrooks PA, Dzewaltowski DA, et al. Beginning with the application in mind: designing and planning health behavior change interventions to enhance dissemination. Ann Behav Med. 2005;29(Suppl.):66–75. doi: 10.1207/s15324796abm2902s_10. [DOI] [PubMed] [Google Scholar]
- 6.NIH Office of Behavioral and Social Sciences Research. Dissemination and Implementation. Available at: http://obssr.od.nih.gov/scientific_areas/translation/dissemination_and_implementation/index.aspx. Cited: 3 January 2013. Accessed: 21 February 2013. [Google Scholar]
- 7.Dunton GF, Lagloire R, Robertson T. Using the RE-AIM framework to evaluate the statewide dissemination of a school-based physical activity and nutrition curriculum: “Exercise Your Options”. Am J Health Promot. 2009;23(4):229–32. doi: 10.4278/ajhp.071211129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Harvey-Berino J, Ewing J, Flynn B, et al. Statewide dissemination of a nutrition program: show the way to 5-a-day. J Nutr Educ. 1998;30:29–36. [Google Scholar]
- 9.Economos CD, Folta SC, Goldberg J, et al. A community-based restaurant initiative to increase availability of healthy menu options in Somerville, Massachusetts: Shape Up Somerville. Prev Chronic Dis. 2009;6(3):A102. [PMC free article] [PubMed] [Google Scholar]
- 10.Hartley D. Rural health disparities, population health, and rural culture. Am J Public Health. 2004;94(10):1675–8. doi: 10.2105/ajph.94.10.1675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gale J, Coburn A. The Characteristics and Roles of Rural Health Clinics in the United States: A Chartbook. 2003. Available at: http://muskie.usm.maine.edu/Publications/rural/RHChartbook03.pdf Cited 7 December 2010. Accessed: 21 February 2013. [Google Scholar]
- 12.Glasgow R. RE-AIM Framework. 2006. Available at: http://www.re-aim.org. Accessed: 21 February 2013. [Google Scholar]
- 13.Kessler RS, Purcell EP, Glasgow RE, et al. What does it mean to “employ” the RE-AIM model? Eval Health Prof. 2013;36(1):44–66. doi: 10.1177/0163278712446066. [DOI] [PubMed] [Google Scholar]
- 14.Nothwehr F, Snetselaar L, Dawson JD, et al. Promoting healthy choices in non-chain restaurants: effects of a simple cue to customers. Health Promot Pract. doi: 10.1177/1524839912437368. (published online 9 October 2012). DOI: 10.1177/1524839912437368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kuo T, Jarosz CJ, Simon P, et al. Menu labeling as a potential strategy for combating the obesity epidemic: a health impact assessment. Am J Public Health. 2009;99(9):1680–6. doi: 10.2105/AJPH.2008.153023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hall SA, Kaufman JS, Ricketts TC. Defining urban and rural areas in U.S. epidemiologic studies. J Urban Health. 2006;83(2):162–75. doi: 10.1007/s11524-005-9016-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gittelsohn J, Lee-Kwan SH, Batorsky B. Community-based interventions in prepared-food sources: a systematic review. Prev Chronic Dis. 2013;10:E180. doi: 10.5888/pcd10.130073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Britt JW, Frandsen K, Leng K, et al. Feasibility of voluntary menu labeling among locally owned restaurants. Health Promot Pract. 2011;12(1):18–24. doi: 10.1177/1524839910386182. [DOI] [PubMed] [Google Scholar]
- 19.Jilcott S, Ammerman A, Sommers J, et al. Applying the RE-AIM framework to assess the public health impact of policy change. Ann Behav Med. 2007;34(2):105–14. doi: 10.1007/BF02872666. [DOI] [PubMed] [Google Scholar]
- 20.King DK, Glasgow RE, Leeman-Castillo B. Reaiming RE-AIM: using the model to plan, implement, and evaluate the effects of environmental change approaches to enhancing population health. Am J Public Health. 2010;100(11):2076–84. doi: 10.2105/AJPH.2009.190959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Estabrooks PA, Allen KC. Updating, employing, and adapting: a commentary on what does it mean to “employ” the RE-AIM model. Eval Health Prof. 2013;36(1):67–72. doi: 10.1177/0163278712460546. [DOI] [PubMed] [Google Scholar]


