Abstract
Skin cancers are rather uncommon malignancies comprising less than 1% of all the cancers in India. Saree cancer is a rare type of squamous cell carcinoma (SCC). Saree and dhoti are traditional male and female costumes respectively, which is unique to the Indian subcontinent. Constant wear of this clothing tightly around the waist results in changes in pigmentation and scaling of the skin, acanthosis, scar and ulceration and subsequent, gradual malignant changes. The process of repeated trauma over a long time and consequent interference with the healing process may rationalise the reason for malignant transformation. Few papers have been published on saree cancer, in main stream medical journals. We are presenting a rare case of saree cancer in a 68-year-old woman, with two distant bilateral ulceroproliferative growths in loin (Synchronous), along the waistline, which showed well-differentiated SCC on biopsy. Wide excision with rhomboid transposition flap was done bilaterally.
KEYWORDS: Rhomboid flap, saree cancer, skin cancer, squamous cell carcinoma
INTRODUCTION
Squamous cell carcinoma (SCC) is the second most common form of skin cancer after basal cell carcinoma. Risks for SCC include light-coloured skin, long-term sun exposure (UV rays), old age, exposure to certain chemicals, burns, old scars, some types of the human papilloma virus.
Saree is the Indian traditional female costume, which is her lifetime clothing. In 1945, Khanolkar and Suryabai described this cancer marked by hypopigmented and thickened scars which were more likely to progress into malignant lesion and termed it ‘dhoti cancer’ (a piece of cotton cloth worn to cover the lower part of the body in most parts of India).[1] The term “Saree Cancer” was first used in the Bombay Hospital Journal by Dr. Patil et al. from Bombay Hospital, India, and created quite a furor in Indian media recently.[2] Saree cancer is analogous to Marjolin's ulcer in aetiology, involving chronic inflammation.
Saree cancer is a type of SCC of the skin that occurs along the waistline in females wearing saree perpetually. Continual wearing of the tightly bound saree causes persistent irritation and friction resulting in scaling and changes in pigmentation of the skin and eventually resulting in malignant changes. It is a very rare type of cancer and is geographically distributed in the Indian subcontinent akin to Kangri cancer[3] in Kashmir. Medical literature on this poorly presented and understood SCC of the skin is sparse, and knowledge of its existence is less even in Indian medical fraternity.
CASE REPORT
A 68-year-old woman presented with chronic non-healing ulcers above the waistline on both flanks (lady was tying her saree with petticoat at this level) with duration of 8 months. Rapid progression of the ulcer on left flank with growth like lesion had been noticed since past 2 months. Both the ulcers were preceded by hypopigmented patches and chronic itching at the site for some years. She has been wearing saree since the age of 13 yrs. On clinical examination, an ulceroproliferative growth measuring 2 cm × 2.5 cm, with surrounding well-defined hypopigmented margin, was found on her left loin. Serosanguinous discharge was present from the lesion. On palpation, the ulcerproliferative growth was tender and was not fixed to the underlying structures. The surrounding skin was scaly. An ulcer measuring 2.5 cm × 5 cm with everted edge and surrounded by area of hypo and hyperpigmentation with induration was present on the right side of the waist [Figure 1]. Bilateral inguinal lymph nodes were multiple, nontender, discrete, firm and mobile. A wedge biopsy from both lesions showed a well differentiated SCC. Complete metastatic workup was done and was negative. The patient had no co-morbidities. Surgery was planned and wide excision of the growth with 2 cm margin and rhomboid transposition flaps on both sides was done [Figure 2]. On histopathology, the tumour was found to be composed of a hyperplastic epidermis with sheets of keratinocytes (with intercellular bridges) demonstrating intense mitotic activity, pleomorphism, and greatly enlarged hyperchromatic nuclei and scanty cytoplasm, suggestive of a well-differentiated SCC with free resection margin of at least 8 mm on all sides. Post-operative period was uneventful [Figures 3 and 4]. Inguinal lymphadenopathy resolved after an antibiotic course. Follow-up was done up to 8 months during which the patient remained disease free.
Figure 1.

Bilateral synchronous cancer lesions along the waist line
Figure 2.
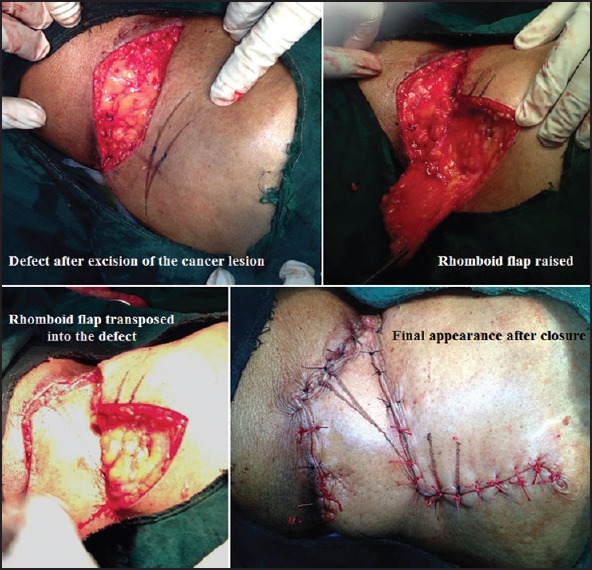
Per-operative serial pics
Figure 3.

Post operative day 15
Figure 4.

Post operative day 30
DISCUSSION
Saree cancer occurs along the waistline in females and is caused by chronic irritation of the skin leading to malignancy. The culprit seems to be petticoat (inner skirt worn underneath to anchor the saree) cord, which, if tied too tight around the same place on the waist day in and day out, can lead to dermatoses (atrophic and keratotic changes in the dermis) eventually leading to ulceration and subsequently malignancy. The persistent irritation of the tight petticoat cord and saree is compounded by the hot and humid tropical climate of the subcontinent and reluctant self hygiene, especially in Indian rural hinterland. This results in the accumulation of irritants (sweat, dust) within the cord tying area leading to itching and scratching. The amalgam of all the above reasons along with disinclination toward once health, usually results in these individuals hailing from rural area presenting to the sparse specialists available, late.
Similar skin changes have also been noted in women wearing “churidhars” (trousers tied with thread). Changes in pigmentation and mild scaling over the waist in Indian women have become very common and most women don’t notice it until it gets chronic. In urban area, the health conscious individual is prompt in consulting a specialist and receives timely healthcare thus halting the progression of the disease early.
It is postulated that with chronic repeated irritation to the ulcer, there is a continuous mitotic activity, as epidermal cells attempt to resurface the open defect. This vicious cycle of damage and repair can lead to a malignant change.[4] Lately, genetic postulations that involve the human leukocyte antigen (HLA) DR4 and mutations in the p53 and/or the FAS genes have been proposed.[5,6] In all known reported cases, the occurrence of the cancer has been at a single site and wide local excision together with skin grafting had been done. In our case, lesions were bilateral in loin (Synchronous) and rhomboid transposition flap was done for covering the defect. SCCs which develop on chronic skin lesions have a higher incidence of metastasis (9% to 36%) as compared to the carcinomas which arise in previously normal skin (1% to 10%).[7]
CONCLUSION
Awareness of the development of dermatoses in the waist area due to tight tying of the cord of the saree or petticoat is important so that. The onus also lies on the treating physician to identify such a lesion and act swiftly with evaluation and subsequent excision. Women who wear saree day in and out should be advised:
To tie saree around their waist laxly-especially in individuals with early skin changes in the form of pigmentation variation or scaling
To wear a petticoat underneath to anchor the saree
To use a broader belt instead of a cord (nada) in petticoats so as to spread the pressure evenly over a larger area[8]
To change the level at which sarees are tied intermittently
To use gown or elastic belt trousers at home
To maintain cleanliness of the part-more aptly applies for those working out and for rural folk
To regularly inspect the waistline[8]
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Khanolkar VR, Suryabai B. Cancer in relation to usages; Three new types in India. Arch Pathol (Chic) 1945;40:351–61. [PubMed] [Google Scholar]
- 2.Patil AS, Bakhshi GD, Puri YS, Gedham MC, Naik AV, Joshi RK. Saree cancer. Bombay Hosp J. 2005;47:302–3. [Google Scholar]
- 3.Kamble AK, Gokhale S. Saree Cancer: A case report. Int J Biol Med Res. 2012;3:1540–1. [Google Scholar]
- 4.Copcu E, Aktas A, Siºman N, Oztan Y. Thirty-one cases of Marjolin's ulcer. Clin Exp Dermatol. 2003;28:138–41. doi: 10.1046/j.1365-2230.2003.01210.x. [DOI] [PubMed] [Google Scholar]
- 5.Harland DL, Robinson WA, Franklin WA. Deletion of the p53 gene in a patient with aggressive burn scar carcinoma. J Trauma. 1997;42:104–7. doi: 10.1097/00005373-199701000-00018. [DOI] [PubMed] [Google Scholar]
- 6.Lee SH, Shin MS, Kim HS, Park WS, Kim SY, Jang JJ, et al. Somatic mutations of the Fas (Apo-1/CD95) gene in cutaneous squamous cell carcinoma arising from a burn scar. J Invest Dermatol. 2000;114:122–6. doi: 10.1046/j.1523-1747.2000.00819.x. [DOI] [PubMed] [Google Scholar]
- 7.Cruickshank AH, McConnell EM, Miller DG. Malignancy in scars, chronic ulcers, and sinuses. J Clin Pathol. 1963;16:573–80. doi: 10.1136/jcp.16.6.573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lal S, Bain J, Singh AK, Shukla PK. Saree Cancer: The malignant changes in chronic irritation. J Clin Diagn Res. 2012;6:896–8. [Google Scholar]


