Abstract
The results of randomized controlled trials and systematic reviews have suggested reduced radiographic wear in highly cross-linked polyethylene compared with conventional polyethylene in primary total hip arthroplasty. However, longer-term clinical results have not been thoroughly examined, to our knowledge. The purpose of this study was to compare the risk of revision for metal-on-conventional and metal-on-highly cross-linked total hip arthroplasty bearing surfaces with use of a distributed data network of six national and regional registries (Kaiser Permanente, HealthEast, the Emilia-Romagna region in Italy, the Catalan region in Spain, Norway, and Australia). Inclusion criteria were osteoarthritis as the primary diagnosis, cementless implant fixation, and a patient age of forty-five to sixty-four years. These criteria resulted in a sample of 16,571 primary total hip arthroplasties. Multivariate meta-analysis was performed with use of linear mixed models, with survival probability as the unit of analysis. The results of a fixed-effects model suggested that there was insufficient evidence of a difference in risk of revision between bearing surfaces (hazard ratio, 1.20 [95% confidence interval, 0.80 to 1.79]; p = 0.384). Highly cross-linked polyethylene does not appear to have a reduced risk of revision in this subgroup of total hip arthroplasty patients. Arthroplasties involving highly cross-linked polyethylene do not appear to have an increased risk of revision in this subgroup of total hip arthroplasty patients.
Total hip arthroplasty is an effective procedure with long-term survival rates of more than 85% at twenty years of follow-up1,2. Despite the effectiveness of this procedure, some total hip arthroplasties require revision, usually because of wear and osteolysis. These revision procedures are associated with an increased risk of complications, re-revision, and patient mortality3,4. In addition, the demand for revision total hip arthroplasty is projected to increase substantially through 20305. As a result, technological advances in bearing surfaces have been introduced with the aim of increasing the longevity of total hip arthroplasty implants by reducing wear and associated osteolysis and loosening. Highly cross-linked polyethylene is one example of a bearing-surface advancement introduced into the market for this purpose6.
The results of two systematic reviews and a meta-analysis have suggested that the use of highly cross-linked polyethylene is associated with a reduced risk of radiographic wear and a lower rate of femoral head penetration6-8. In addition, the authors of several small, single-center randomized controlled trials have reported lower rates of femoral head penetration and wear in highly cross-linked polyethylene compared with conventional polyethylene9-12. Although the authors of these studies provided short-term radiographic findings, in only a few studies have the authors examined the longer-term clinical results of total hip arthroplasty with conventional and highly cross-linked polyethylene in specific subgroups of patients. The authors of one large cohort study reported a lower risk of revision for cementless highly cross-linked polyethylene compared with conventional polyethylene, but the difference did not reach significance13. Results from another U.S registry study and the annual reports from the Australian Orthopaedic Association National Joint Replacement Registry indicated an increased risk of revision in total hip arthroplasties involving conventional polyethylene compared with arthroplasties involving highly cross-linked polyethylene14-18. These registry findings are critical, since they provide adequate statistical power and longer-term clinical outcomes. In addition, registry findings provide real-world data in a variety of patient, hospital, and surgeon settings, which increases the generalizability of the findings. For these reasons, the findings of national and regional registry studies are relevant. Aggregating data from multiple registries across different countries further enhances the statistical power and allows greater generalization of the findings when comparing the performance of bearing surfaces in hip arthroplasty internationally.
Therefore, the purpose of this study was to compare the risk of revision for arthroplasties involving metal-on-conventional polyethylene implants with that for arthroplasties involving metal-on-highly cross-linked polyethylene implants with use of data from five different countries provided by six regional and national registries.
Materials and Methods
Data Collection
A distributed health data network was created by the International Consortium of Orthopaedic Registries (ICOR) and used in this study to lower barriers to participation (for example, concerns regarding data security, privacy, proprietary information, and legal issues) relative to a centralized data warehouse approach19,20. A distributed health data network is a decentralized model that permits secure storage and analysis of data from numerous registries21. In general, the data from each registry are standardized and given at the level of aggregation that is most suitable for the detailed analysis of interest, with the aggregated data combined across registries22.
SAS programs (version 9.2; SAS Institute, Cary, North Carolina) were developed at the coordinating center and tested by participating registries (the Australian Orthopaedic Association National Joint Replacement Registry, Catalan Arthroplasty Register, Register of the Orthopaedic Prosthetic Implants (Emilia-Romagna region, Italy), HealthEast Registry, Kaiser Permanente National Joint Replacement Registry, and Norwegian Arthroplasty Register). Each registry applied the program to its database behind secure firewalls. The participating registries then shared aggregate-level crosstabs, Cox regression results, and implant survival probabilities with the ICOR coordinating center for statistical analysis.
Inclusion and Exclusion Criteria
This study includes only osteoarthritis patients who underwent total hip procedures from 2001 to 2010. The outcome of interest was the time to the first revision for any reason. We compared metal-on-conventional polyethylene implants with a head size of <32 mm with metal-on-highly cross-linked polyethylene implants (head sizes of <32, 32, and >32 mm). The choice to use metal-on-conventional polyethylene implants with a head size of <32 mm was based on limited data for larger head sizes with conventional polyethylene in all registries for the fixation method and age groupings under study (see below). The choice to use metal-on-highly cross-linked polyethylene implants with all head sizes was based on our finding of no evidence to support a head-size effect with that bearing surface within the designated fixation method and age groupings23. Further, there is a potentially complex relationship that exists between fixation method, patient age, and time to revision24. In order to limit the potential confounding effect of patient age and fixation method on bearing-surface groups, we limited the study to patients with cementless procedures who were within the age range of forty-five to sixty-four years. This sample restriction allowed us to better isolate the effect of wear associated with specific bearing-surface and head-size combinations.
Statistical Analyses
Multivariate meta-analysis was performed with use of linear mixed models, with implant survival probability as the unit of analysis25. The models estimated the residual covariances with the precise method reported previously26 and also implemented a transformation27,28 to ensure that the models could be fitted with use of existing SAS software. Implant survival probabilities and their standard errors were extracted from each registry for each unique combination of the covariates (for example, bearing surface, head size, and patient age) at each distinct event time. Each unique combination was grouped into yearly time intervals, with only the earliest observation in that interval retained.
We fitted two models: one treating registries as a set of fixed effects and the other treating them as random effects. The random-effects model offers some inferential advantage for combining studies29,30. However, with few observational data and few registries, the estimated between-registry variation in the random-effects model can be rather inaccurate. Further, the absence of randomization for bearing-surface and head-size groups could lead to confounding because of registry-level effects, which the random-effects model does not address but the fixed-effects model does31,32. Therefore, we determined that preference would be given to interpretation of the fixed-effects model, particularly when the parameter estimates were substantially different in the fixed-effects model compared with those in the random-effects model31,32.
The results of the fixed-effects model and those of the model without fixed effects to represent registries are given in Table I and the Appendix (Table III), respectively. Additional details regarding the model fitting are given in the Appendix. SAS (version 9.2) was used for all of the analyses.
TABLE I.
Fixed-Effects Model*
| Hazard Ratio† (95% CI) | P Value† | |
| Time in yr | ||
| 0 to 1 | Ref. | |
| 1 to 2 | 6.54 (4.63-9.24) | <0.001 |
| 2 to 3 | 8.13 (5.73-11.52) | <0.001 |
| 3 to 4 | 9.19 (6.46-13.07) | <0.001 |
| 4 to 5 | 10.01 (7.03-14.26) | <0.001 |
| 5 to 6 | 10.75 (7.52-15.37) | <0.001 |
| 6 to 7 | 11.67 (8.14-16.74) | <0.001 |
| 7 to 8 | 14.38 (9.78-21.14) | <0.001 |
| 8 to 9 | 14.26 (9.53-21.34) | <0.001 |
| Sex | ||
| Male | Ref. | |
| Female | 1.05 (0.85-1.31) | 0.653 |
| Age in yr | ||
| 45 to 54 | Ref. | |
| 55 to 64 | 0.77 (0.58-1.02) | 0.068 |
| Bearing surface | ||
| Metal on highly cross-linked polyethylene (all head sizes) | Ref. | |
| Metal on conventional polyethylene (head size <32 mm) | 1.20 (0.80-1.79) | 0.384 |
Results are based on an iterative solution that updates the residual covariances until convergence with use of restricted maximum likelihood
Confidence intervals (CIs) and p values are based on a Z distribution. The estimated intercept was −5.571 (standard error, 0.209).
TABLE III.
No Fixed-Effects Model*
| Hazard Ratio (95% CI) | P Value | |
| Time in yr | ||
| 0 to 1 | Ref. | |
| 1 to 2 | 6.103 (4.396-8.474) | <0.001 |
| 2 to 3 | 7.590 (5.456-10.558) | <0.001 |
| 3 to 4 | 8.584 (6.158-11.965) | <0.001 |
| 4 to 5 | 9.354 (6.708-13.042) | <0.001 |
| 5 to 6 | 10.057 (7.181-14.086) | <0.001 |
| 6 to 7 | 10.939 (7.794-15.354) | <0.001 |
| 7 to 8 | 13.540 (9.410-19.483) | <0.001 |
| 8 to 9 | 13.402 (9.140-19.651) | <0.001 |
| Sex | ||
| Male | Ref. | |
| Female | 1.041 (0.838-1.294) | 0.716 |
| Age in yr | ||
| 45 to 54 | Ref. | |
| 55 to 64 | 0.765 (0.579-1.011) | 0.060 |
| Bearing surface | ||
| Metal on highly cross-linked polyethylene (all head sizes) | Ref. | |
| Metal on conventional polyethylene (head size <32 mm) | 1.315 (0.945-1.830) | 0.104 |
Results are based on an iterative solution that updates the residual covariances until convergence with use of restricted maximum likelihood. Confidence intervals (CIs) and p values are based on a Z distribution. The estimated intercept was −5.520 (standard error, 0.202).
Results
A total of 16,571 total hip arthroplasties were included in this study; 51% (8501) were in female patients. The five-year rate of revision surgery ranged from 1.9% to 3.2% among the registries. Descriptive data for metal-on-highly cross-linked polyethylene (all head sizes) and metal-on-conventional polyethylene (head size of <32 mm) implants are presented in Table II.
TABLE II.
Included Implants by Registry, Bearing Surface, Head Size, Age, and Sex
| Registry*
(no. [%]) |
||||||
| U.S., KP | Australia | Italy, E-R | U.S., HE | Norway | Spain, C | |
| Metal on highly cross-linked polyethylene | ||||||
| Head size <32 mm | ||||||
| Age, 45 to 54 yr | 194 (23.0) | 1109 (24.3) | 26 (10.4) | 56 (32.9) | 33 (22.1) | 30 (30.9) |
| Age, 55 to 64 yr | 648 (77.0) | 3462 (75.7) | 224 (89.6) | 114 (67.1) | 116 (77.9) | 67 (69.1) |
| Male | 275 (32.7) | 2110 (46.2) | 121 (48.4) | 63 (37.1) | 51 (34.2) | 61 (62.9) |
| Female | 567 (67.3) | 2461 (53.8) | 129 (51.6) | 107 (62.9) | 98 (65.8) | 36 (37.1) |
| Head size = 32 mm | ||||||
| Age, 45 to 54 yr | 347 (18.6) | 554 (21.2) | 1 (12.5) | 23 (30.3) | 3 (21.4) | 14 (25.5) |
| Age, 55 to 64 yr | 1516 (81.4) | 2062 (78.8) | 7 (87.5) | 53 (69.7) | 11 (78.6) | 41 (74.5) |
| Male | 723 (38.8) | 1253 (47.9) | 1 (12.5) | 42 (55.3) | 6 (42.9) | 28 (50.9) |
| Female | 1140 (61.2) | 1363 (52.1) | 7 (87.5) | 34 (44.7) | 8 (57.1) | 27 (49.1) |
| Head size >32 mm | ||||||
| Age, 45 to 54 yr | 352 (19.3) | 367 (22.2) | 6 (22.2) | 15 (14.2) | 2 (40.0) | 7 (14.3) |
| Age, 55 to 64 yr | 1471 (80.7) | 1284 (77.8) | 21 (77.8) | 91 (85.8) | 3 (60.0) | 42 (85.7) |
| Male | 1020 (56.0) | 1060 (64.2) | 23 (85.2) | 71 (67.0) | 5 (100.0) | 30 (61.2) |
| Female | 803 (44.0) | 591 (35.8) | 4 (14.8) | 35 (33.0) | 0 (0.0) | 19 (38.8) |
| Metal on conventional polyethylene | ||||||
| Head size <32 mm | ||||||
| Age, 45 to 54 yr | 40 (27.8) | 283 (27.9) | 77 (12.7) | 4 (66.7) | 54 (22.2) | 39 (20.6) |
| Age, 55 to 64 yr | 104 (72.2) | 730 (72.1) | 527 (87.3) | 2 (33.3) | 189 (77.8) | 150 (79.4) |
| Male | 71 (49.3) | 537 (53.0) | 287 (47.5) | 4 (66.7) | 104 (42.8) | 124 (65.6) |
| Female | 73 (50.7) | 476 (47.0) | 317 (52.5) | 2 (33.3) | 139 (57.2) | 65 (34.4) |
The values are given as the number of each, with the percentage in parentheses. KP = Kaiser Permanente, E-R = Emilia-Romagna region, HE = HealthEast, and C = Catalan region.
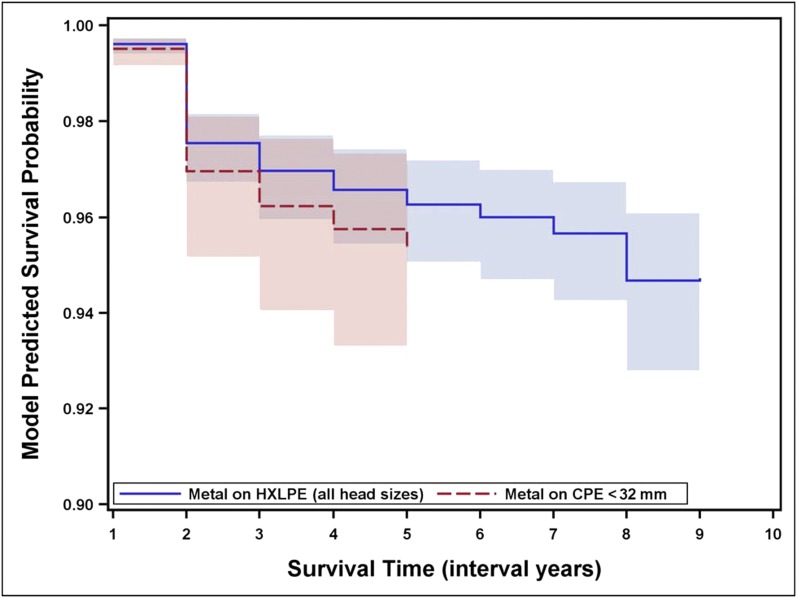
We fitted a fixed-effects model that included an intercept, bearing surface, age, sex, piecewise constant function of time, and residual variance fixed at one, as well as dummy variables to represent registries (Table I). Most notable from this model is the observation that there was insufficient evidence of a difference in revision rates between bearing surfaces, with the point estimate indicating a more harmful effect of metal on conventional polyethylene that was not significant (hazard ratio, 1.20 [95% confidence interval, 0.80 to 1.79]; p = 0.384). Survival probabilities (estimated from the fixed-effects model) for these bearing surfaces over time are shown in Figure 1.
Fig. 1.
Model-predicted survival of metal-on-conventional polyethylene implants with head sizes of <32 mm and metal-on-highly cross-linked polyethylene implants with any head size. The shading indicates the 95% confidence interval. HXLPE = highly cross-linked polyethylene, and CPE = conventional polyethylene.
Discussion
To our knowledge, this is the largest international study comparing highly cross-linked and conventional polyethylene, in 16,571 cementless total hip arthroplasties in patients forty-five to sixty-four years old. With data from five countries and six regional and national registries, this study is also one of the first international collaborations among registries. Although cumulative revision rates were higher in the group with conventional polyethylene, this difference did not reach significance in the adjusted multivariable model.
These study findings contribute clinical survivorship data to prior randomized controlled trials and systematic reviews suggesting radiographic wear and penetration6,8-12. Although the hazard ratio in our adjusted model was in the same direction as those in prior studies, our results did not reach significance within the selected subgroup of cementless total hip arthroplasty patients between forty-five and sixty-four years of age. These findings are similar to those reported by Howard et al.13. Our study findings differ from those previously published by national and international registries14-18. The results may vary because of differences in study samples. Specifically, the use of highly cross-linked polyethylene may not have had as large of an effect in this specific subgroup as it did in more diverse cohorts that included all fixation methods, all head sizes, and a wider range of patient ages. Inclusion of data from multiple countries in this specific subgroup of patients with varying durations of follow-up may have also contributed to the difference in findings.
The strengths of this study include the large international sample size and “real-world” registry findings with high external validity, representative of community-based practice and varying surgeon training, skill levels, and hospital characteristics. Although our study has strong external validity, internal validity may be criticized because of the observational nature of the data. In our study, we addressed this limitation by statistically adjusting for potential confounding variables in our multivariable model. Our focus on cementless total hip arthroplasties in patients forty-five to sixty-four years old was aimed at reducing patient-age and fixation-method factors as study confounders. While reducing the impact of head-size variation, these inclusion and exclusion criteria resulted in a specific focus on a smaller subgroup of patients, which in turn yielded lower statistical power. Another perceived limitation of this study may be the lack of patient-reported functional outcomes. However, highly cross-linked polyethylene was introduced to increase implant longevity and the ultimate measure of longevity is revision surgery, thus justifying our study end point. In addition, selection criteria may differ for conventional polyethylene and highly cross-linked polyethylene. Highly cross-linked polyethylene may be used more frequently in higher-risk patients such as those with a higher activity level. Although activity level was not included in this study, patient age may serve as a proxy for activity level and was adjusted for in the multivariable model. The duration of follow-up may also be a limitation, since highly cross-linked polyethylene was introduced to reduce the wear and associated osteolysis that typically occur with longer follow-up times. While the average follow-up rate in the registries is >90%, some registries have shorter follow-up than others and data may still be limited in scope and therefore not appropriate to support a marketing application in the United States. Finally, this study does not take into account specific device or implant performance. Substantial variation among different manufacturers and implants of conventional and highly cross-linked polyethylene throughout the world is not accounted for in registry data. Variation among different manufacturers and implants of both conventional and highly cross-linked polyethylene has been reported by national registries17,33.
In conclusion, in this international study of 16,571 cementless total hip arthroplasties in patients forty-five to sixty-four years of age we did not find a difference in risk of revision for conventional polyethylene compared with highly cross-linked polyethylene. Unlike other technologies introduced into the market such as metal-on-metal bearing surfaces, highly cross-linked polyethylene does not appear to have an increased risk of revision in total hip arthroplasty. Future studies are necessary to examine the impact of highly cross-linked polyethylene and conventional polyethylene in total hip arthroplasty in a wider range of patients, including those with cemented fixation, patients sixty-five years of age and older, and with longer study follow-up.
Appendix—Details of the Model Fitting
Data Inclusion
For the models described here, we chose to retain observations with a standard error of <0.0125, given that the simulations indicated increased bias, root-mean-squared error, and poorer coverage when observations with large degrees of imprecision (resulting from sparse data for certain covariate combinations) were retained. The 0.0125 threshold was based on both the simulation results and a sensitivity analysis comparing the effect on model parameters when different levels of restriction (0.05, 0.025, and 0.0125) were applied.
Model Selection
The fixed-effects model was based on the random-effects model selected. We began with a model that included an intercept, bearing surface, age, sex, piecewise constant function of time, bearing surface by time interaction, random intercept, random treatment effect, and residual variance fixed at one. A random effect for neither the intercept nor the bearing surface was warranted based on a point estimate that was near zero (i.e., <1.0 × 10−10) and was therefore not included. The interaction terms were based on intervals of time: zero to two years and two to five years. A test of the interaction terms, χ2 (1) = 0.01, was not significant (p = 0.915); therefore, these terms were not included.
Acknowledgments
Note: The authors acknowledge Abby Isaacs, Rebecca Love, and Lucas Romero for their analytic and organizational support. They also acknowledge Danica Marinac-Dabic, MD, PhD, for leadership and substantial contributions to the success of ICOR.
Footnotes
Disclosure: One or more of the authors received payments or services, either directly or indirectly (i.e., via his or her institution), from a third party in support of an aspect of this work. In addition, one or more of the authors, or his or her institution, has had a financial relationship, in the thirty-six months prior to submission of this work, with an entity in the biomedical arena that could be perceived to influence or have the potential to influence what is written in this work. Also, one or more of the authors has a patent or patents, planned, pending, or issued, that is broadly relevant to the work. No author has had any other relationships, or has engaged in any other activities, that could be perceived to influence or have the potential to influence what is written in this work. The complete Disclosures of Potential Conflicts of Interest submitted by authors are always provided with the online version of the article.
References
- 1.Berry DJ, Harmsen WS, Cabanela ME, Morrey BF. Twenty-five-year survivorship of two thousand consecutive primary Charnley total hip replacements: factors affecting survivorship of acetabular and femoral components. J Bone Joint Surg Am. 2002February;84(2):171-7. [DOI] [PubMed] [Google Scholar]
- 2.Schulte KR, Callaghan JJ, Kelley SS, Johnston RC. The outcome of Charnley total hip arthroplasty with cement after a minimum twenty-year follow-up. The results of one surgeon. J Bone Joint Surg Am. 1993July;75(7):961-75. [DOI] [PubMed] [Google Scholar]
- 3.Ong KL, Lau E, Suggs J, Kurtz SM, Manley MT. Risk of subsequent revision after primary and revision total joint arthroplasty. Clin Orthop Relat Res. 2010November;468(11):3070-6 Epub 2010 May 25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wolf BR, Lu X, Li Y, Callaghan JJ, Cram P. Adverse outcomes in hip arthroplasty: long-term trends. J Bone Joint Surg Am. 2012July18;94(14):e103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007April;89(4):780-5. [DOI] [PubMed] [Google Scholar]
- 6.Kurtz SM, Gawel HA, Patel JD. History and systematic review of wear and osteolysis outcomes for first-generation highly crosslinked polyethylene. Clin Orthop Relat Res. 2011August;469(8):2262-77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kuzyk PR, Saccone M, Sprague S, Simunovic N, Bhandari M, Schemitsch EH. Cross-linked versus conventional polyethylene for total hip replacement: a meta-analysis of randomised controlled trials. J Bone Joint Surg Br. 2011May;93(5):593-600. [DOI] [PubMed] [Google Scholar]
- 8.Mu Z, Tian J, Wu T, Yang J, Pei F. A systematic review of radiological outcomes of highly cross-linked polyethylene versus conventional polyethylene in total hip arthroplasty. Int Orthop. 2009June;33(3):599-604 Epub 2009 Jan 29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Calvert GT, Devane PA, Fielden J, Adams K, Horne JG. A double-blind, prospective, randomized controlled trial comparing highly cross-linked and conventional polyethylene in primary total hip arthroplasty. J Arthroplasty. 2009June;24(4):505-10 Epub 2008 Jun 10. [DOI] [PubMed] [Google Scholar]
- 10.Geerdink CH, Grimm B, Ramakrishnan R, Rondhuis J, Verburg AJ, Tonino AJ. Crosslinked polyethylene compared to conventional polyethylene in total hip replacement: pre-clinical evaluation, in-vitro testing and prospective clinical follow-up study. Acta Orthop. 2006October;77(5):719-25. [DOI] [PubMed] [Google Scholar]
- 11.McCalden RW, MacDonald SJ, Rorabeck CH, Bourne RB, Chess DG, Charron KD. Wear rate of highly cross-linked polyethylene in total hip arthroplasty. A randomized controlled trial. J Bone Joint Surg Am. 2009April;91(4):773-82. [DOI] [PubMed] [Google Scholar]
- 12.Thomas GE, Simpson DJ, Mehmood S, Taylor A, McLardy-Smith P, Gill HS, Murray DW, Glyn-Jones S. The seven-year wear of highly cross-linked polyethylene in total hip arthroplasty: a double-blind, randomized controlled trial using radiostereometric analysis. J Bone Joint Surg Am. 2011April20;93(8):716-22. [DOI] [PubMed] [Google Scholar]
- 13.Howard JL, Kremers HM, Loechler YA, Schleck CD, Harmsen WS, Berry DJ, Cabanela ME, Hanssen AD, Pagnano MW, Trousdale RT, Lewallen DG. Comparative survival of uncemented acetabular components following primary total hip arthroplasty. J Bone Joint Surg Am. 2011September7;93(17):1597-604. [DOI] [PubMed] [Google Scholar]
- 14.Australian Orthopaedic Association National Joint Replacement Registry. Hip and knee arthroplasty: annual report. Adelaide: AOA. 2010. https://aoanjrr.dmac.adelaide.edu.au/documents/10180/42844/Annual%20Report%202010?version=1.1&t=1349406187793. Accessed 2014 May 6.
- 15.Australian Orthopaedic Association National Joint Replacement Registry. Hip and knee arthroplasty: annual report. Adelaide: AOA. 2011. https://aoanjrr.dmac.adelaide.edu.au/documents/10180/44800/Annual%20Report%202011?version=1.2&t=1347337258367. Accessed 2014 May 6.
- 16.Australian Orthopaedic Association National Joint Replacement Registry. Hip and knee arthroplasty: annual report. Adelaide: AOA. 2012. https://aoanjrr.dmac.adelaide.edu.au/documents/10180/60142/Annual%20Report%202012?version=1.3&t=1361226543157. Accessed 2014 May 6.
- 17.Australian Orthopaedic Association National Joint Replacement Registry. Hip and knee arthroplasty: annual report. Adelaide: AOA. 2013. https://aoanjrr.dmac.adelaide.edu.au/documents/10180/127202/Annual%20Report%202013?version=1.2&t=1385685288617. Accessed 2014 May 6.
- 18.Paxton EW, Namba RS, Maletis GB, Khatod M, Yue EJ, Davies M, Low RB Jr, Wyatt RW, Inacio MC, Funahashi TT. A prospective study of 80,000 total joint and 5000 anterior cruciate ligament reconstruction procedures in a community-based registry in the United States. J Bone Joint Surg Am. 2010December;92(Suppl 2):117-32. [DOI] [PubMed] [Google Scholar]
- 19.Brown JS, Holmes JH, Shah K, Hall K, Lazarus R, Platt R. Distributed health data networks: a practical and preferred approach to multi-institutional evaluations of comparative effectiveness, safety, and quality of care. Med Care. 2010June;48(6)(Suppl):S45-51. [DOI] [PubMed] [Google Scholar]
- 20.Sedrakyan A, Paxton EW, Marinac-Dabic D. Stages and tools for multinational collaboration: the perspective from the coordinating center of the International Consortium of Orthopaedic Registries (ICOR). J Bone Joint Surg Am. 2011December21;93(Suppl 3):76-80. [DOI] [PubMed] [Google Scholar]
- 21.Maro JC, Platt R, Holmes JH, Strom BL, Hennessy S, Lazarus R, Brown JS. Design of a national distributed health data network. Ann Intern Med. 2009September1;151(5):341-4 Epub 2009 Jul 28. [DOI] [PubMed] [Google Scholar]
- 22.Sedrakyan A, Paxton EW, Phillips C, Namba R, Funahashi T, Barber T, Sculco T, Padgett D, Wright T, Marinac-Dabic D. The International Consortium of Orthopaedic Registries: overview and summary. J Bone Joint Surg Am. 2011December21;93(Suppl 3):1-12. [DOI] [PubMed] [Google Scholar]
- 23.Allepuz A, Havelin L, Barber T, Sedrakyan A, Graves S, Bordini B, Hoeffel D, Cafri G, Paxton E. Effect of femoral head size on metal-on-HXLPE hip arthroplasty outcome in a combined analysis of six international registries. J Bone Joint Surg Am. 2014December17;96(Suppl 1):12-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Stea S, Comfort T, Sedrakyan A, Havelin L, Marinelli M, Barber T, Paxton E, Banerjee S, Isaacs A, Graves S. Multinational comprehensive evaluation of the fixation method used in hip replacement: interaction with age in context. J Bone Joint Surg Am. 2014December17;96(Suppl 1):42-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Arends LR, Hunink MG, Stijnen T. Meta-analysis of summary survival curve data. Stat Med. 2008September30;27(22):4381-96. [DOI] [PubMed] [Google Scholar]
- 26.Dear KB. Iterative generalized least squares for meta-analysis of survival data at multiple times. Biometrics. 1994December;50(4):989-1002. [PubMed] [Google Scholar]
- 27.Kalaian HA, Raudenbush SW. A multivariate mixed linear model for meta-analysis. Psychol Methods. 1996;1:227-35. [Google Scholar]
- 28.Kutner MH, Nachtsheim CJ, Neter J, Li W. Applied linear statistical models. Boston, MA: McGraw-Hill Irwin; 2005. [Google Scholar]
- 29.DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986September;7(3):177-88. [DOI] [PubMed] [Google Scholar]
- 30.Hedges LV, Vevea JL. Fixed- and random-effects models in meta-analysis. Psychol Methods. 1998;3:486-504. [Google Scholar]
- 31.Allison PD. Fixed effects regression models. Thousand Oaks, CA: Sage Publications, Inc; 2009. [Google Scholar]
- 32.Localio AR, Berlin JA, Ten Have TR, Kimmel SE. Adjustments for center in multicenter studies: an overview. Ann Intern Med. 2001July17;135(2):112-23. [DOI] [PubMed] [Google Scholar]
- 33.National Joint Registry for England and Wales. 10th Annual Report 2013. http://www.njrcentre.org.uk/njrcentre/Portals/0/Documents/England/Reports/10th_annual_report/NJR%2010th%20Annual%20Report%202013%20B.pdf. Accessed 2014 May 6.