Abstract
Background:
Mobile-bearing total knee prostheses were designed to reduce wear and improve implant survivorship following total knee arthroplasty. However, the benefit of mobile-bearing total knee arthroplasty remains unproven. Both mobile-bearing and fixed-bearing total knee arthroplasty implants are available in posterior-stabilized and non-posterior-stabilized designs. With the latter, the implant does not recreate the function of the posterior cruciate ligament (PCL) with a posterior-stabilizing cam mechanism. The purpose of the present study was to compare mobile-bearing, non-posterior-stabilized devices with fixed-bearing, non-posterior-stabilized devices used in total knee arthroplasty through a novel multinational study design.
Methods:
Through the use of a distributed health data network, primary total knee arthroplasties performed for osteoarthritis from 2001 to 2010 were identified from six national and regional total joint arthroplasty registries. Multivariate meta-analysis was performed with use of linear mixed models, with the primary outcome of interest being revision for any reason. Survival probabilities and their standard errors were extracted from each registry for each unique combination of the covariates.
Results:
A total of 319,616 patients (60% female) underwent non-posterior-stabilized total knee arthroplasty. A fixed-bearing, non-posterior-stabilized design was used in 258,190 (81%) of the knees and a mobile-bearing, non-posterior-stabilized design in 61,426 (19%) of the knees. Sixty-nine percent of the patients who received a fixed-bearing implant were over sixty-five years of age, compared with 63% of those who received a mobile-bearing implant. Mobile-bearing designs had a higher risk of revision, with a hazard ratio of 1.43 (95% confidence interval, 1.36 to 1.51; p < 0.001).
Conclusions:
Previous comparisons of mobile-bearing and fixed-bearing total knee arthroplasty outcomes have been inconclusive. The current study utilized an advanced, harmonized distributed analysis of six national and regional joint-replacement registries. To our knowledge, it is the largest analysis of mobile-bearing total knee arthroplasty to date. Mobile-bearing, non-posterior-stabilized designs presented a greater risk of failure than was found for fixed-bearing, non-posterior-stabilized designs. Caution should be used in the selection of the mobile-bearing non-posterior-stabilized design for total knee replacement.
Mobile-bearing total knee prostheses were developed to reduce wear of articular bearing surfaces following total knee arthroplasty. To our knowledge, no clinical study has demonstrated the superiority of mobile-bearing compared with conventional fixed-bearing total knee arthroplasty, but the promise of wear reduction has led to continued interest in mobile-bearing total knee replacement. The LCS (Low Contact Stress, DePuy Synthes), the original mobile-bearing total knee arthroplasty implant, has been used in patients worldwide since 19771.
Reports are conflicting regarding the revision rate associated with the LCS implant2,3. Prior studies have not demonstrated the superiority of mobile-bearing compared with fixed-bearing total knee arthroplasty, despite the increased cost associated with mobile-bearing implants4. The LCS implant was identified as a risk factor for revision of primary total knee arthroplasty in some studies3,5, but not in other studies6,7.
Mobile-bearing total knee arthroplasty implants are available in posterior-stabilized and non-posterior-stabilized design options. With the latter, the implant does not recreate the function of the posterior cruciate ligament (PCL) with a posterior-stabilizing cam mechanism. The LCS is an example of a mobile-bearing, non-posterior-stabilized implant. Fixed-bearing total knee implants are also available in posterior-stabilized and non-posterior-stabilized designs.
The specific aim of this study was to compare the implant survivorship of mobile-bearing, non-posterior-stabilized total knee arthroplasty with that of fixed-bearing, non-posterior-stabilized total knee arthroplasty. A multiregistry, collaborative approach was utilized to increase the sample size and for greater generalizability of the practices of surgeons globally.
Materials and Methods
A distributed health data network was developed by the International Consortium of Orthopaedic Registries (ICOR) and used in this study to reduce barriers to participation (e.g., involving data security, privacy, proprietary information, and legal issues) relative to an approach involving a centralized data warehouse8-10. A distributed health data network is a decentralized model that allows secure storage and analysis of data from multiple registries11. Generally, the data from each registry are standardized and provided at the level of aggregation that is most suitable for the detailed analysis of interest. The aggregated data are combined across registries12.
The first step undertaken in developing the research network was to evaluate the variation in international practice. All interested registries participated in decision-making on key variables to be included for analytic purposes. Next, each contributing registry provided data depicting the mean values and proportions of patient and procedure-related characteristics. Six national and regional registries (Kaiser Permanente in the U.S., Swedish Knee Registry, the Emilia-Romagna region in Italy, the Catalan region in Spain, Norway, and Australia) formed the basis of the study collaboration.
The study compared mobile-bearing with fixed-bearing non-posterior-stabilized total knee arthroplasty. The study included only osteoarthritis patients who had undergone total knee procedures from 2001 to 2010 and excluded posterior-stabilized knees, and constrained and hinged devices, as well as reverse hybrid fixation (cemented femur and cementless tibial components). The outcome of interest was time to first revision for any reason. The distribution of implants by registry and by age, sex, fixation, and patella resurfacing characteristics is shown in Table I.
TABLE I.
Included Implants by Registry, Age, Sex, Fixation, and Patella Resurfacing*
| Registry (No. [%]) |
||||||
| U.S., KP | Australia | Italy, E-R | Sweden | Norway | Spain, C | |
| Fixed non-PS | ||||||
| Age in yr | ||||||
| <45 | 102 (0.7) | 671 (0.5) | 13 (0.2) | 247 (0.3) | 58 (0.4) | 4 (0) |
| 45-55 | 1343 (9) | 9319 (6.9) | 119 (2.1) | 3980 (5.1) | 670 (4.6) | 56 (0.5) |
| 56-65 | 4634 (30.9) | 34,801 (25.9) | 786 (13.9) | 19,242 (24.5) | 3430 (23.8) | 719 (6.8) |
| >65 | 8904 (59.4) | 89,369 (66.6) | 4731 (83.7) | 54,976 (70.1) | 10,258 (71.2) | 9758 (92.6) |
| Sex | ||||||
| Male | 5573 (37.2) | 57,330 (42.7) | 1464 (25.9) | 31,357 (40) | 4657 (32.3) | 2885 (27.4) |
| Female | 9410 (62.8) | 76,830 (57.3) | 4185 (74.1) | 47,088 (60) | 9759 (67.7) | 7652 (72.6) |
| Fixation | ||||||
| Uncemented | 627 (4.2) | 32,401 (24.2) | 619 (11) | 1042 (1.3) | 385 (2.7) | 594 (5.6) |
| Hybrid | 1828 (12.2) | 40,572 (30.2) | 278 (4.9) | 49 (0.1) | 1926 (13.4) | 3511 (33.3) |
| Cemented | 12,528 (83.6) | 61,187 (45.6) | 4752 (84.1) | 77,354 (98.6) | 12,105 (84) | 6432 (61) |
| Patella resurfacing | ||||||
| No resurfacing | 608 (4.1) | 78,553 (58.6) | 5457 (96.6) | 73,639 (93.9) | 13,785 (95.6) | 7536 (71.5) |
| Resurfacing | 14,375 (95.9) | 55,607 (41.4) | 192 (3.4) | 4806 (6.1) | 631 (4.4) | 3001 (28.5) |
| Mobile non-PS | ||||||
| Age in yr | ||||||
| <45 | 26 (1.4) | 309 (0.6) | 6 (0.2) | 14 (2) | 34 (0.4) | 0 (0) |
| 45-55 | 377 (20.9) | 4012 (8.4) | 60 (2.1) | 145 (20.9) | 469 (5.6) | 1 (1.1) |
| 56-65 | 937 (52.1) | 13,552 (28.5) | 432 (14.9) | 360 (51.8) | 1957 (23.4) | 5 (5.6) |
| >65 | 460 (25.6) | 29,703 (62.4) | 2410 (82.9) | 176 (25.3) | 5898 (70.6) | 83 (93.3) |
| Sex | ||||||
| Male | 792 (44) | 20,672 (43.5) | 777 (26.7) | 318 (45.8) | 2656 (31.8) | 27 (30.3) |
| Female | 1008 (56) | 26,904 (56.5) | 2131 (73.3) | 377 (54.2) | 5702 (68.2) | 62 (69.7) |
| Fixation | ||||||
| Uncemented | 248 (13.8) | 23,507 (49.4) | 153 (5.3) | 0 (0) | 507 (6.1) | 27 (30.3) |
| Hybrid | 433 (24.1) | 11,464 (24.1) | 434 (14.9) | 0 (0) | 651 (7.8) | 2 (2.2) |
| Cemented | 1119 (62.2) | 12,605 (26.5) | 2321 (79.8) | 695 (100) | 7200 (86.1) | 60 (67.4) |
| Patella resurfacing | ||||||
| No resurfacing | 58 (3.2) | 31,998 (67.3) | 2816 (96.8) | 667 (96) | 8089 (96.8) | 81 (91) |
| Resurfacing | 1742 (96.8) | 15,578 (32.7) | 92 (3.2) | 28 (4) | 269 (3.2) | 8 (9) |
Non-PS = non-posterior-stabilized, KP = Kaiser Permanente, E-R = Emilia-Romagna region, and C = Catalan region.
Statistical Analyses
Multivariate meta-analysis was performed with use of linear mixed models, with survival probability as the unit of analysis13. The models estimated the residual covariances with the precise method reported previously14, and implemented a transformation15-17 to ensure that the models could be fit with existing SAS software (SAS Institute). Survival probabilities and their standard errors were extracted from each registry for each unique combination of the covariates (for example, patella resurfacing, implant fixation, and age) at each distinct event time. Each unique combination was grouped into yearly time intervals, with only the earliest observation in each interval retained.
We fitted two models, one that treated the registries as a set of fixed effects and the other that treated them as random effects. Both models included an intercept, fixed versus mobile-bearing, age, sex, fixation, resurfacing, piecewise constant function of time, residual variance fixed at 1, and either random effects for intercept and fixed versus mobile-bearing, or fixed registry effects. Although the random-effects model offers some inferential advantage for combining studies18,19, with the limited numbers of contributing registries, the estimated between-registry variation in the random-effects model can be quite inaccurate. Further, the absence of randomization for mobility and stabilization groups could lead to confounding due to registry-level effects. The random-effects model does not address this issue, but the fixed-effects model does20,21. Therefore, preference would be given to interpretation of the fixed-effects model, particularly if the parameter estimates are substantially different in the fixed-effects model compared with those in the random-effects model20,21.
The results of the fixed-effects model are presented below and in Table II, and the results of the random-effects model are included in the Appendix. SAS version 9.2 was used for all analyses. Additional details regarding the model fitting are given in the Appendix.
TABLE II.
Fixed-Effects Model*
| Hazard Ratio (95% CI) | P Value | |
| Time in yr | ||
| 0 to 1 | Ref. | |
| 1 to 2 | 9.76 (8.38-11.37) | <0.001 |
| 2 to 3 | 18.94 (16.23-22.09) | <0.001 |
| 3 to 4 | 24.35 (20.86-28.42) | <0.001 |
| 4 to 5 | 28.30 (24.24-33.04) | <0.001 |
| 5 to 6 | 31.34 (26.84-36.60) | <0.001 |
| 6 to 7 | 34.06 (29.15-39.78) | <0.001 |
| 7 to 8 | 36.73 (31.44-42.92) | <0.001 |
| 8 to 9 | 39.17 (33.50-45.80) | <0.001 |
| 9 to 10 | 43.94 (37.34-51.70) | <0.001 |
| Sex | ||
| Male | Ref. | |
| Female | 0.91 (0.87-0.95) | <0.001 |
| Age in yr | ||
| >65 | Ref. | |
| ≤65 | 0.56 (0.53-0.58) | <0.001 |
| Patella resurfacing | ||
| No | Ref. | |
| Patella resurfaced | 0.84 (0.79-0.88) | <0.001 |
| Fixation | ||
| Cemented | Ref. | |
| Uncemented | 1.13 (1.06-1.20) | 0.002 |
| Hybrid | 0.99 (0.94-1.06) | 0.867 |
| Fixed registry effects† | — | — |
| Implant design | ||
| Fixed non-posterior-stabilized | Ref. | |
| Mobile non-posterior-stabilized | 1.43 (1.36-1.51) | <0.001 |
Results are based on an iterative solution that updates the residual covariances until convergence. Confidence intervals (CIs) are based on a Z distribution. The estimated intercept was −6.417 (standard error, 0.085).
Fixed registry effects were included in this model, but the results are omitted from this table because a precondition of data sharing was no reporting of comparisons between registries.
Results
A total of 319,616 patients (60% female) who received non-posterior-stabilized knee implants were included in the study. In 258,190 (81%) of the knees, a fixed-bearing design was used, and in 61,426 (19%) of the knees, a mobile-bearing design was used. Sixty-nine percent of the patients who received the fixed-bearing implants were over sixty-five years of age, compared with 63% of those who received the mobile-bearing implants. Five-year revision rates varied across the six participating registries, ranging from 1.8% to 3.5%. Distribution of implants by registry and by age, sex, fixation, and resurfacing characteristics is shown in Table I.
The most commonly used mobile-bearing and fixed-bearing total knee implants included in the analysis are presented in Table III. The majority of the mobile-bearing implants were rotating-platform designs.
TABLE III.
Commonly Used Total Knee Arthroplasty Implants Included in Analysis
| Design | Implant |
| Fixed-bearing, non-posterior-stabilized | NexGen (Zimmer) |
| P.F.C. Sigma (DePuy Synthes) | |
| Genesis II (Smith & Nephew) | |
| Profix (Smith & Nephew) | |
| Scorpio (Stryker) | |
| Vanguard (Biomet) | |
| AGC (Anatomic Graduated Component; Biomet) | |
| Tricon (Smith & Nephew) | |
| ADVANCE (Wright Medical) | |
| Mobile-bearing, non-posterior-stabilized | LCS (Low Contact Stress; DePuy Synthes) |
| P.F.C. Sigma Rotating Platform (DePuy Synthes) | |
| RBK (Global Orthopaedic Technology) | |
| TC-Plus Solution (Smith & Nephew) | |
| Total Articulating Cementless Knee (Waldemar Link) | |
| Rotaglide (Corin Medical) |
TABLE IV.
Random-Effects Model*
| Hazard Ratio (95% CI) | P Value | |
| Time in yr | ||
| 0 to 1 | Ref. | |
| 1 to 2 | 9.77 (8.38-11.38) | <0.001 |
| 2 to 3 | 18.95 (16.24-22.12) | <0.001 |
| 3 to 4 | 24.37 (20.88-28.46) | <0.001 |
| 4 to 5 | 28.34 (24.26-33.09) | <0.001 |
| 5 to 6 | 31.38 (26.86-36.65) | <0.001 |
| 6 to 7 | 33.91 (29.02-39.61) | <0.001 |
| 7 to 8 | 36.77 (31.46-42.98) | <0.001 |
| 8 to 9 | 39.22 (33.53-45.88) | <0.001 |
| 9 to 10 | 44.00 (37.38-51.80) | <0.001 |
| Sex | ||
| Male | Ref. | |
| Female | 0.91 (0.87-0.95) | <0.001 |
| Age in yr | ||
| >65 | Ref. | |
| ≤65 | 0.56 (0.54-0.58) | <0.001 |
| Patella resurfacing | ||
| No | Ref. | |
| Patella resurfaced | 0.84 (0.79-0.88) | <0.001 |
| Fixation | ||
| Cemented | Ref. | |
| Uncemented | 1.12 (1.05-1.19) | <0.001 |
| Hybrid | 0.99 (0.93-1.06) | 0.862 |
| Implant design | ||
| Fixed non-posterior-stabilized | Ref. | |
| Mobile non-posterior-stabilized | 1.45 (1.08-1.93) | 0.024 |
Results are based on an iterative solution that updates the residual covariances until convergence. The model is estimated with use of restricted maximum likelihood (REML). Our simulations indicated that an optimal strategy for confidence interval (CI) construction in the presence of random effects was to use tK−1 for fixed parameters with corresponding random effects, and to use tn−p otherwise. This is the approach taken in the construction of the CIs and p values reported in this table. The estimated intercept was −6.233 (standard error, 0.134), the random effect intercept was 0.065 (standard error, 0.043), and the random effect for implant design was 0.039 (standard error, 0.050).
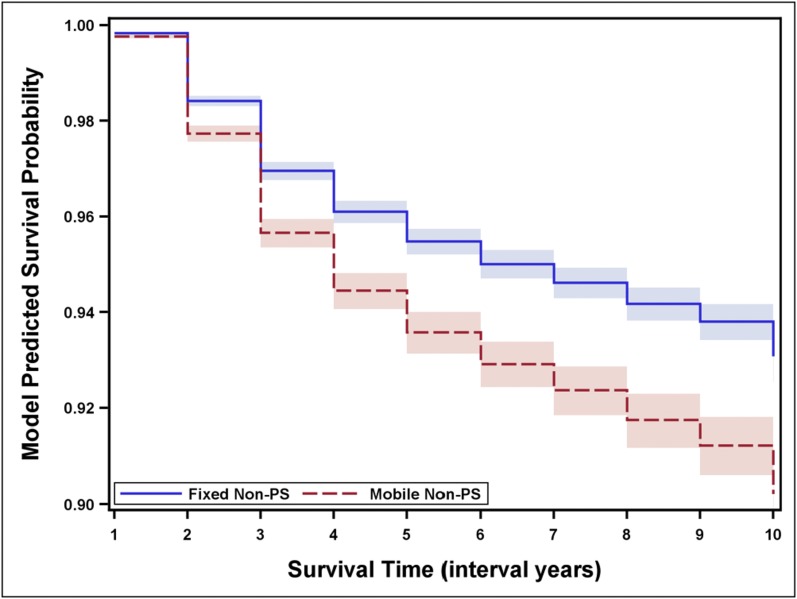
Interpretation of the results focuses on the fixed-effects model, with the results of the random-effects model presented in the Appendix. We were unable to detect a significant effect for a two-way interaction between prosthesis and either: time, age, sex, patella resurfacing, or fixation. The overall effect was a hazard ratio (HR) of 1.43 (95% confidence interval [CI], 1.36 to 1.51; p < 0.001), indicating greater risk of revision for mobile-bearing knee implants. However, in the first year, the magnitude of this effect was higher (HR, 1.90 [95% CI, 1.39 to 2.61]; p < 0.001), than in the subsequent nine years (HR, 1.43 [95% CI, 1.36 to 1.51]; p < 0.001). The findings from the fixed-effects model without a time interaction effect are depicted in Table II. Figure 1 depicts the model-predicted survival for fixed and mobile non-posterior-stabilized implants according to the fixed-effects model.
Fig. 1.
Model-predicted survival probability. The x-axis values of 1 to 10 correspond to the interval years (zero to one through nine to ten years). The graphs depict the fixed-effects model, results of which are also shown in Table II. Confidence intervals (shaded areas) are based on a Z distribution. Non-PS = non-posterior-stabilized.
Discussion
In this multiregistry analysis, mobile-bearing, non-posterior-stabilized total knee arthroplasty was identified as a risk factor for revision. Combining data elements among the registries, much like in a prospective multicenter study, increased the sample size and thereby improved precision and statistical power, which is particularly important for rare events such as revisions. Challenges to data sharing among multiple registries were managed with a decentralized data warehouse with sharing of aggregate-level data, leading to an unprecedented collaboration among six joint-replacement registries located in different countries.
The LCS implant was the first commercially available mobile-bearing total knee arthroplasty implant and continues to be used by orthopaedic surgeons worldwide. In addition to the LCS implant, other mobile-bearing, non-posterior-stabilized designs are commercially available, and many of these were included in the current analysis. The surgical implantation of the LCS design entails resection of the PCL without incorporating a cam mechanism. Most commercially available fixed-bearing total knee arthroplasties in the U.S. recreate the function of the PCL using a cam mechanism, but non-posterior-stabilized versions do exist. These designs incorporate a raised anterior lip of the tibial insert. The current study indicated, in the absence of a posterior-stabilizing cam mechanism, increased risk of revision following mobile-bearing compared with fixed-bearing total knee arthroplasty.
Different results have been reported for mobile-bearing total knee arthroplasty implants22-25. A well-conducted prospective, randomized trial did not show any significant differences between mobile-bearing and fixed-bearing total knee arthroplasty regarding function but was not large enough to look at revision occurrence6. One meta-analysis found similar functional outcomes2, and another, a lower rate of revision associated with mobile-bearing total knee arthroplasty7. However, analysis of the Kaiser Permanente total joint registry determined that the adjusted revision risk of the LCS implant was two times higher than that for fixed-bearing total knee replacements5. In the 2011 annual report of the Australian Orthopaedic Association registry, the ten-year cumulative percent revision for the LCS was 7.4 (95% CI, 6.4 to 8.7) compared with 2.7 (95% CI, 2.1 to 3.5) for the NexGen CR, a fixed-bearing implant26. Similarly, a Norwegian study identified the LCS and LCS Complete implants as having a six to seven-times higher risk for tibial component loosening compared with fixed-bearing total knee implants3.
To our knowledge, our study was more powerful than any previous investigation, and its major strength was the inclusion of the largest sample size of mobile-bearing and fixed-bearing total knee replacements reported to date. While understanding the reasons for reoperation is important, the implant survivorship itself is a very valuable outcome from the patient perspective. One limitation of this study is that mobile-bearing total knee arthroplasties are performed much less frequently than are fixed-bearing total knee arthroplasties. Mobile-bearing total knee arthroplasties represent 1.2% to 30% of the volume of primary total knee arthroplasty in annual reports of total knee registries. Hence, patient selection for mobile-bearing or fixed-bearing total knee arthroplasty might be based on factors other than surgeon preference, with some potential of selection bias.
In conclusion, non-posterior-stabilized, mobile-bearing total knee arthroplasty was identified as a revision risk factor for primary total knee arthroplasty in a unique international collaboration of six joint-replacement registries. Although this observation was clear, the results should not be extrapolated to all mobile-bearing total knee arthroplasties, as there are other designs of mobile-bearing implants, including those that incorporate a cam mechanism. Despite challenges of data sharing among large institutions, the methodology utilized in the collaboration of multiple registries in this study can be replicated for other clinical research questions.
Appendix—Details of the Model Fitting
For the models described, we chose to retain observations with a standard error of <0.025, given simulations indicating increased bias, increased root-mean-squared error, and poorer coverage when observations with greater degrees of imprecision (resulting from sparse data for certain covariate combinations) were retained. This particular threshold was based on both the simulation results and a sensitivity analysis of the effect on model parameters when various levels of restriction (0.05, 0.025, 0.0125) were applied.
The fixed-effects model was based on the random-effects model selected. For the random-effects model, we initially considered interactions with time in our model. The interaction terms were based on intervals of time: zero to one year through nine to ten years. A likelihood ratio test using maximum likelihood estimation found insufficient evidence of improvement as a result of including the interaction of prosthesis and time in the model, χ2 (9) = 14.37, p = 0.110. Examination of the point estimates suggested a more parsimonious specification of time for the interaction, (zero to one year versus one to ten years). However, this failed to reach significance as well, χ2 (1) = 3.24, p = 0.072. As an exploratory measure, we also examined whether there was evidence of a two-way interaction between prosthesis and either: resurfacing, fixation, age, or sex. A global test of all of these two-way interactions indicated no evidence of an effect, χ2 (5) = 5.74, p = 0.332.
Acknowledgments
Note: The authors thank Abby Isaacs, Rebecca Love, and Lucas Romero for analytic and organizational support. They also acknowledge Danica Marinac-Dabic, MD, PhD, for leadership and substantial contributions to the success of ICOR.
Footnotes
Disclosure: One or more of the authors received payments or services, either directly or indirectly (i.e., via his or her institution), from a third party in support of an aspect of this work. In addition, one or more of the authors, or his or her institution, has had a financial relationship, in the thirty-six months prior to submission of this work, with an entity in the biomedical arena that could be perceived to influence or have the potential to influence what is written in this work. Also, one or more of the authors has a patent or patents, planned, pending, or issued, that is broadly relevant to the work. No author has had any other relationships, or has engaged in any other activities, that could be perceived to influence or have the potential to influence what is written in this work. The complete Disclosures of Potential Conflicts of Interest submitted by authors are always provided with the online version of the article.
References
- 1.DePuy. Products, LCS complete knee system. http://www.depuy.com/healthcare-professionals/product-details/lcs-completetrade-knee-system?s=search_132878001489110&i=137&consulta=t&keyword=&company=0&specialty=254&category=0&focus=0&family=0&sorting=title&sorting_type=asc&ajax=0&page=6&per_page=25. Accessed 2014 Jun 5.
- 2.Paxton EW, Furnes O, Namba RS, Inacio MC, Fenstad AM, Havelin LI. Comparison of the Norwegian knee arthroplasty register and a United States arthroplasty registry. J Bone Joint Surg Am. 2011December21;93(Suppl 3):20-30. [DOI] [PubMed] [Google Scholar]
- 3.Gøthesen O, Espehaug B, Havelin L, Petursson G, Lygre S, Ellison P, Hallan G, Furnes O. Survival rates and causes of revision in cemented primary total knee replacement: a report from the Norwegian Arthroplasty Register 1994-2009. Bone Joint J. 2013May;95-B(5):636-42. [DOI] [PubMed] [Google Scholar]
- 4.Smith H, Jan M, Mahomed NN, Davey JR, Gandhi R. Meta-analysis and systematic review of clinical outcomes comparing mobile bearing and fixed bearing total knee arthroplasty. J Arthroplasty. 2011December;26(8):1205-13 Epub 2011 Feb 04. [DOI] [PubMed] [Google Scholar]
- 5.Namba RS, Inacio MC, Paxton EW, Ake CF, Wang C, Gross TP, Marinac-Dabic D, Sedrakyan A. Risk of revision for fixed versus mobile-bearing primary total knee replacements. J Bone Joint Surg Am. 2012November7;94(21):1929-35. [DOI] [PubMed] [Google Scholar]
- 6.Gioe TJ, Glynn J, Sembrano J, Suthers K, Santos ER, Singh J. Mobile and fixed-bearing (all-polyethylene tibial component) total knee arthroplasty designs. A prospective randomized trial. J Bone Joint Surg Am. 2009September;91(9):2104-12. [DOI] [PubMed] [Google Scholar]
- 7.Carothers JT, Kim RH, Dennis DA, Southworth C. Mobile-bearing total knee arthroplasty: a meta-analysis. J Arthroplasty. 2011June;26(4):537-42 Epub 2010 Jul 14. [DOI] [PubMed] [Google Scholar]
- 8.Brown JS, Holmes JH, Shah K, Hall K, Lazarus R, Platt R. Distributed health data networks: a practical and preferred approach to multi-institutional evaluations of comparative effectiveness, safety, and quality of care. Med Care. 2010June;48(6)(Suppl):S45-51. [DOI] [PubMed] [Google Scholar]
- 9.Sedrakyan A, Paxton EW, Marinac-Dabic D. Stages and tools for multinational collaboration: the perspective from the coordinating center of the International Consortium of Orthopaedic Registries (ICOR). J Bone Joint Surg Am. 2011December21;93(Suppl 3):76-80. [DOI] [PubMed] [Google Scholar]
- 10.Robertsson O, Knutson K, Lewold S, Lidgren L. The Swedish Knee Arthroplasty Register 1975-1997: an update with special emphasis on 41,223 knees operated on in 1988-1997. Acta Orthop Scand. 2001October;72(5):503-13. [DOI] [PubMed] [Google Scholar]
- 11.Maro JC, Platt R, Holmes JH, Strom BL, Hennessy S, Lazarus R, Brown JS. Design of a national distributed health data network. Ann Intern Med. 2009September1;151(5):341-4 Epub 2009 Jul 28. [DOI] [PubMed] [Google Scholar]
- 12.Sedrakyan A, Paxton EW, Phillips C, Namba R, Funahashi T, Barber T, Sculco T, Padgett D, Wright T, Marinac-Dabic D. The International Consortium of Orthopaedic Registries: overview and summary. J Bone Joint Surg Am. 2011December21;93(Suppl 3):1-12. [DOI] [PubMed] [Google Scholar]
- 13.Arends LR, Hunink MG, Stijnen T. Meta-analysis of summary survival curve data. Stat Med. 2008September30;27(22):4381-96. [DOI] [PubMed] [Google Scholar]
- 14.Dear KB. Iterative generalized least squares for meta-analysis of survival data at multiple times. Biometrics. 1994December;50(4):989-1002. [PubMed] [Google Scholar]
- 15.Kutner MH, Nachtsheim CJ, Neter J, Li W. Applied linear statistical models. 5th ed.Boston: McGraw-Hill Irwin; 2005. [Google Scholar]
- 16.Kalaian HA, Raudenbush SW. A multivariate mixed linear model for meta-analysis. Psychol Methods. 1996;1:227-35. [Google Scholar]
- 17.Cheung MWL. A model for integrating fixed-, random-, and mixed-effects meta-analyses into structural equation modeling. Psychol Methods. 2008September;13(3):182-202. [DOI] [PubMed] [Google Scholar]
- 18.DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986September;7(3):177-88. [DOI] [PubMed] [Google Scholar]
- 19.Hedges LV, Vevea JL. Fixed- and random-effects models in meta-analysis. Psychol Methods. 1998;3(4):486-504. [Google Scholar]
- 20.Localio AR, Berlin JA, Ten Have TR, Kimmel SE. Adjustments for center in multicenter studies: an overview. Ann Intern Med. 2001July17;135(2):112-23. [DOI] [PubMed] [Google Scholar]
- 21.Allison PD. Fixed Effects Regression Models. Thousand Oaks, CA: Sage; 2009. [Google Scholar]
- 22.Bailey O, Ferguson K, Crawfurd E, James P, May PA, Brown S, Blyth M, Leach WJ. No clinical difference between fixed- and mobile-bearing cruciate-retaining total knee arthroplasty: a prospective randomized study. Knee Surg Sports Traumatol Arthrosc. 2014February9 Epub 2014 Feb 9. [DOI] [PubMed] [Google Scholar]
- 23.Bistolfi A, Massazza G, Lee GC, Deledda D, Berchialla P, Crova M. Comparison of fixed and mobile-bearing total knee arthroplasty at a mean follow-up of 116 months. J Bone Joint Surg Am. 2013June19;95(12):e83. [DOI] [PubMed] [Google Scholar]
- 24.Bo ZD, Liao L, Zhao JM, Wei QJ, Ding XF, Yang B. Mobile bearing or fixed bearing? A meta-analysis of outcomes comparing mobile bearing and fixed bearing bilateral total knee replacements. Knee. 2014March;21(2):374-81 Epub 2013 Oct 24. [DOI] [PubMed] [Google Scholar]
- 25.Luna JT, Sembrano JN, Gioe TJ. Mobile and fixed-bearing (all-polyethylene tibial component) total knee arthroplasty designs: surgical technique. J Bone Joint Surg Am. 2010September;92(Suppl 1 Pt 2):240-9. [DOI] [PubMed] [Google Scholar]
- 26.Graves S, Davidson D, de Steiger R, Tompkins A. Australian Orthopaedic Association National Joint Replacement Registry. Hip and Knee Arthroplasty 2011 Annual Report. 2011. https://aoanjrr.dmac.adelaide.edu.au/documents/10180/44800/Annual%20Report%202011?version=1.2&t=1347337258367. Accessed 2014 May 9.