Abstract
Background:
Fixation in total hip replacements remains a controversial topic, despite the high level of its success. Data obtained from major orthopaedic registries indicate that there are large differences among preferred fixation and survival results.
Methods:
Using a distributed registry data network, primary total hip arthroplasties performed for osteoarthritis from 2001 to 2010 were identified from six national and regional total joint arthroplasty registries. A multivariate meta-analysis was performed using linear mixed models with the primary outcome revision for any reason. Survival probabilities and their standard errors were extracted from each registry for each unique combination of the covariates. Fixation strategies were compared with regard to age group, sex, bearing, and femoral-head diameter. All comparisons were based on the random-effects model and the fixed-effects model.
Results:
In patients who were seventy-five years of age and older, uncemented fixation had a significantly higher risk of revision (p < 0.001) than hybrid fixation, with a hazard ratio of 1.575 (95% confidence interval, 1.389 to 1.786). We found a similar, if lesser, effect in the intermediate age group of sixty-five to seventy-four years (hazard ratio, 1.16 [95% confidence interval, 1.023 to 1.315]; p = 0.021) and in the younger age group of forty-five to sixty-four years (hazard ratio, 1.205 [95% confidence interval, 1.008 to 1.442]; p = 0.041). There were no significant differences between hybrid and cemented bearings across age groups.
Conclusions:
We conclude that cementless fixation should be avoided in older patients (those seventy-five years of age or older), although this evidence is less strong in patients of intermediate and younger ages.
Fixation in total hip replacement remains a controversial topic, despite the high level of its success. Cemented fixation was developed at the beginning of the arthroplasty experience in the late 1960s and remained the first choice in many countries, although in other countries it has been gradually replaced by uncemented or hybrid solutions. These alternative solutions have been developed mainly to overcome problems related to cement aging, microfractures, and late loosening occurring in long-lasting implants, when young or middle-aged patients are treated.
Data obtained from major orthopaedic registries indicate that there are large differences among countries for the preferred fixation. In Table I, data obtained from the last English-translated public report of major worldwide registries are presented. Data do not consider the age of patients, which represents one variable of major importance in the decision on the mode of fixation.
TABLE I.
Distribution of Fixation of Total Hip Replacement in 2012 (or Last Available Data) According to Major Registries Having at Least Six Years of Follow-up
| Country | Type of Registry | Year | No. of Primary Total Hip Replacements | Cemented | Uncemented | Hybrid | Reverse Hybrid (Cemented Cup) |
| Australia* | National | 2012 | 27,500 | 5% | 64% | 31%† | — |
| Sweden | National | 2010 | 16,000 | 68% | 15% | 2% | 15% |
| Norway* | National | 2009 | 7000 | 53% | 20% | 2% | 25% |
| Denmark | National | 2012 | 8000 | 16% | 68% | 16%† | — |
| England | National | 2012 | 86,500 | 33% | 46% | 18% | 3% |
| New Zealand | National | 2012 | 7500 | 14% | 45% | 41%† | — |
| Slovakia | National | 2011 | 5000 | 38% | 49% | 13% | <0.1% |
| Romania | National | 2011 | 5600 | 47% | 43% | 1% | 9% |
| Canada | National | 2011 | 14,000 | 1% | 83% | 16%† | — |
| Netherlands | National | 2012 | 24,000 | 21% | 72% | 7%† | — |
| United States* (Kaiser Permanente) | Community | 2010 | 5000 | 12% | 87% | 1% | 0% |
| United States* (HealthEast) | Community | 2010 | 596 | 4% | 96% | <1% | 0% |
| Italy* (R.I.P.O.) | Regional | 2012 | 6500 | 1% | 95% | 3.5% | 0.5% |
| Spain* (Catalan) | Regional | 2012 | 6000 | 10% | 70% | 20%† | — |
Registry-sharing data appear in the current paper.
These are cumulative values between the hybrid and reverse hybrid groups.
According to those registries, the trend in the choice of fixation generally indicates a decrease of totally cemented total hip replacements in all registries except that of New Zealand and an increase of reverse hybrid fixation in the registries of Sweden, Norway, and Denmark.
A survival analysis of different types of fixation gives controversial results, and comparisons among registry data are often difficult, as no standard exists on the presentation of results1. Age groups, for example, are not comparable, which makes conclusions difficult and inconsistent.
To overcome the problem, an innovative approach was set up, aimed at merging results obtained worldwide by six registries: the Australian Orthopaedic Association National Joint Replacement Registry, the Catalan Arthroplasty Register, the Emilia-Romagna Joint Registry R.I.P.O. (Registro dell’implantologia Protesica Ortopedica [Register of the Orthopaedic Prosthetic Implants]), the HealthEast Joint Replacement Registry, the Kaiser Permanente Total Joint Replacement Registry, and the Norwegian Arthroplasty Register2.
Survival analyses of total hip arthroplasty using different fixation methods (cemented, uncemented, and hybrid) were investigated in relation to age.
Materials and Methods
The Population Under Study
The above-mentioned registries shared their data. The present study included only patients with osteoarthritis undergoing hip surgery from 2001 to 2010, with implants using any one of five bearing surfaces: ceramic on ceramic, ceramic on conventional polyethylene, ceramic on highly cross-linked polyethylene, metal on highly cross-linked polyethylene, and metal on conventional polyethylene.
The exclusion criteria were inverse hybrid fixation (uncemented cup and cemented stem), as this is not a common practice in five of the six registries; cemented ceramic-on-ceramic bearings, as this is not a common practice and the potential sample was very small; and metal-on-metal implants because of possible bias introduced by this controversial articulation.
The end point is represented by the first revision of at least one component, for any reason. Reoperation with no component exchange was not an end point in the present study.
Statistical Analyses
SAS programs (SAS Institute, Cary, North Carolina) were developed at the coordinating center and were tested by participating registries to reduce barriers to participation (e.g., security, proprietary, legal, and privacy) relative to a centralized data warehouse approach3. Each registry applied the program to their database and then shared aggregate-level data, Cox regression results, and survival probabilities with the International Consortium of Orthopaedic Registries (ICOR) Coordinating Center for statistical analysis.
In this way, a distributed health data network was developed, creating a decentralized model that allows secure storage and analysis of data from different registries4.
A multivariate meta-analysis was performed using linear mixed models, with the survival probability as the unit of analysis5. The models estimate the residual covariances using the precise method reported before6 and implement a transformation7,8 to ensure that the models can be fit with existing software (SAS 9.2). The model is adjusted for bearing surface, head size (<32 mm and ≥32 mm), and sex. Two different models of analysis were applied, the details of which are presented in the Appendix.
The first model treats registry as a set of fixed effects and the second model treats registry as a random effect. Although the random-effects model offers some inferential advantage for combining studies9,10, with few observational data or registries, the estimated between-registry variation in the random-effects model can be quite inaccurate. Further, the absence of randomization for bearing or head-size groups could lead to confounding due to registry-level effects, which is not addressed by the random-effects model but is addressed by the fixed-effects model11,12. Therefore, preference would be given to interpretation of the fixed-effects model, particularly if the parameter estimates are substantially different in the fixed-effects model compared with the random-effects model.
Hence, we present the results of the fixed-effects model in Table II and include the results of the random-effects model in the Appendix. Both models come to the same conclusions.
TABLE II.
| Hazard Ratio‡ | P Value§ | |
| Time | ||
| Zero to one year | Reference | — |
| More than one year to two years | 4.284 (3.818 to 4.807) | <0.001 |
| More than two years to three years | 5.524 (4.919 to 6.202) | <0.001 |
| More than three years to four years | 6.555 (5.835 to 7.365) | <0.001 |
| More than four years to five years | 7.438 (6.616 to 8.362) | <0.001 |
| More than five years to six years | 8.335 (7.408 to 9.379) | <0.001 |
| More than six years to seven years | 9.478 (8.413 to 10.679) | <0.001 |
| More than seven years to eight years | 10.584 (9.378 to 11.945) | <0.001 |
| More than eight years to nine years | 12.138 (10.710 to 13.757) | <0.001 |
| More than nine years to ten years | 15.189 (13.073 to 17.647) | <0.001 |
| Sex | ||
| Male | Reference | — |
| Female | 0.804 (0.758 to 0.852) | <0.001 |
| Head size | ||
| <32 mm | Reference | — |
| ≥32 mm | 0.832 (0.768 to 0.903) | <0.001 |
| Bearing type | ||
| Ceramic on ceramic | Reference | — |
| Ceramic on conventional polyethylene | 0.974 (0.843 to 1.127) | 0.725 |
| Ceramic on highly cross-linked polyethylene | 1.078 (0.938 to 1.240) | 0.292 |
| Metal on conventional polyethylene | 1.047 (0.929 to 1.179) | 0.452 |
| Metal on highly cross-linked polyethylene | 0.820 (0.747 to 0.901) | <0.001 |
| Fixation effects by age | ||
| Hybrid, forty-five to more than seventy-five years | Reference | — |
| Uncemented, forty-five to sixty-four years | 1.205 (1.008 to 1.442) | 0.041 |
| Cemented, forty-five to sixty-four years | 1.093 (0.869 to 1.374) | 0.448 |
| Uncemented, sixty-five to seventy-four years | 1.160 (1.023 to 1.315) | 0.021 |
| Cemented, sixty-five to seventy-four years | 1.048 (0.898 to 1.223) | 0.552 |
| Uncemented, seventy-five years and more | 1.575 (1.389 to 1.786) | <0.001 |
| Cemented, seventy-five years and more | 0.919 (0.789 to 1.070) | 0.275 |
The estimate (and standard error) for the intercept was −5.232 ± 0.088.
Fixed registry effects were included in this model (five coefficients), but the results are omitted from this table because a precondition of data sharing was no reporting of between-registry comparisons.
The values are given as the hazard ratio, with the 95% CI, based on a normal distribution, in parentheses.
The p values are based on a normal distribution.
Results
The study includes 239,442 patients from across six registries, 59% of whom are female. Patients were classified into three age groups (forty-five to sixty-four years, sixty-five to seventy-four years, and seventy-five years or older), according to biological and physiological criteria. The distribution of the variable fixation among the three age groups and registries is presented in Figure 1. A complete description of the sample size by age, fixation, sex, bearing surface, head size, and registry is available in Table III.
Fig. 1.
Data set of analysis. The age group of forty-five to sixty-four years included 65,944 implants; the age group of sixty-five to seventy-four years included 87,959 implants, and the age group of seventy-five years or more included 85,539 implants. Globally, there are 126,148 uncemented implants, 60,502 hybrid implants, and 52,792 cemented implants. KP = Kaiser Permanente, E-R = Emilia-Romagna region, HE = HealthEast, and C = Catalan region.
TABLE III.
| Registry‡ |
||||||
| U.S. (Kaiser Permanente) | Australia | Italy (Emilia-Romagna) | U.S. (HealthEast) | Norway | Spain (Catalan) | |
| Age of forty-five to sixty-four years | ||||||
| Uncemented | ||||||
| Sex | ||||||
| Male | 3141 (43.6) | 14,799 (49.4) | 2448 (46.2) | 382 (46.1) | 1185 (39.1) | 491 (61.9) |
| Female | 4067 (56.4) | 15,147 (50.6) | 2849 (53.8) | 446 (53.9) | 1845 (60.9) | 302 (38.1) |
| Bearing type | ||||||
| Ceramic on ceramic | 300 (4.2) | 15,691 (52.4) | 3344 (63.1) | 124 (15) | 968 (31.9) | 186 (23.5) |
| Ceramic on conventional polyethylene | 25 (0.3) | 438 (1.5) | 729 (13.8) | 759 (25) | 113 (14.2) | |
| Ceramic on highly cross-linked polyethylene | 2184 (30.3) | 3894 (13) | 298 (5.6) | 346 (41.8) | 892 (29.4) | 89 (11.2) |
| Metal on conventional polyethylene | 171 (2.4) | 1085 (3.6) | 641 (12.1) | 6 (0.7) | 243 (8) | 204 (25.7) |
| Metal on highly cross-linked polyethylene | 4528 (62.8) | 8838 (29.5) | 285 (5.4) | 352 (42.5) | 168 (5.5) | 201 (25.3) |
| Head size | ||||||
| <32 mm | 1529 (21.2) | 9598 (32.1) | 2769 (52.3) | 267 (32.2) | 1936 (63.9) | 497 (62.7) |
| ≥32 mm | 5679 (78.8) | 20,348 (67.9) | 2528 (47.7) | 561 (67.8) | 1094 (36.1) | 296 (37.3) |
| Hybrid | ||||||
| Sex | ||||||
| Male | 106 (30.8) | 4649 (46.5) | 89 (44.5) | 29 (46) | 142 (39.9) | 14 (48.3) |
| Female | 238 (69.2) | 5352 (53.5) | 111 (55.5) | 34 (54) | 214 (60.1) | 15 (51.7) |
| Bearing type | ||||||
| Ceramic on ceramic | 3 (0.9) | 2603 (26) | 28 (14) | 22 (6.2) | ||
| Ceramic on conventional polyethylene | 108 (1.1) | 72 (36) | 92 (25.8) | 4 (13.8) | ||
| Ceramic on highly cross-linked polyethylene | 31 (9) | 1289 (12.9) | 3 (1.5) | 6 (9.5) | 25 (7) | 1 (3.4) |
| Metal on conventional polyethylene | 59 (17.2) | 805 (8) | 82 (41) | 187 (52.5) | 8 (27.6) | |
| Metal on highly cross-linked polyethylene | 251 (73) | 5196 (52) | 15 (7.5) | 57 (90.5) | 30 (8.4) | 16 (55.2) |
| Head size | ||||||
| <32 mm | 169 (49.1) | 5681 (56.8) | 182 (91) | 53 (84.1) | 314 (88.2) | 22 (75.9) |
| ≥32 mm | 175 (50.9) | 4320 (43.2) | 18 (9) | 10 (15.9) | 42 (11.8) | 7 (24.1) |
| Cemented | ||||||
| Sex | ||||||
| Male | 10 (38.5) | 1080 (46) | 11 (31.4) | 1845 (33.9) | ||
| Female | 16 (61.5) | 1267 (54) | 24 (68.6) | 3595 (66.1) | 1 (100) | |
| Bearing type | ||||||
| Ceramic on conventional polyethylene | 53 (2.3) | 24 (68.6) | 1973 (36.3) | |||
| Ceramic on highly cross-linked polyethylene | 6 (23.1) | 52 (2.2) | 75 (1.4) | |||
| Metal on conventional polyethylene | 3 (11.5) | 795 (33.9) | 11 (31.4) | 3296 (60.6) | 1 (100) | |
| Metal on highly cross-linked polyethylene | 17 (65.4) | 1447 (61.7) | 96 (1.8) | |||
| Head size | ||||||
| <32 mm | 9 (34.6) | 2225 (94.8) | 35 (100) | 5374 (98.8) | 1 (100) | |
| ≥32 mm | 17 (65.4) | 122 (5.2) | 66 (1.2) | |||
| Age of sixty-five to seventy-four years | ||||||
| Uncemented | ||||||
| Sex | ||||||
| Male | 2833 (40.3) | 13,559 (50) | 3859 (41.9) | 241 (42.7) | 634 (39.2) | 771 (57.7) |
| Female | 4202 (59.7) | 13,547 (50) | 5359 (58.1) | 323 (57.3) | 982 (60.8) | 565 (42.3) |
| Bearing type | ||||||
| Ceramic on ceramic | 39 (0.6) | 9506 (35.1) | 4308 (46.7) | 12 (2.1) | 557 (34.5) | 155 (11.6) |
| Ceramic on conventional polyethylene | 16 (0.2) | 590 (2.2) | 1871 (20.3) | 485 (30) | 148 (11.1) | |
| Ceramic on highly cross-linked polyethylene | 937 (13.3) | 3401 (12.5) | 641 (7) | 104 (18.4) | 341 (21.1) | 71 (5.3) |
| Metal on conventional polyethylene | 236 (3.4) | 1363 (5) | 1613 (17.5) | 3 (0.5) | 141 (8.7) | 556 (41.6) |
| Metal on highly cross-linked polyethylene | 5807 (82.5) | 12,246 (45.2) | 785 (8.5) | 445 (78.9) | 92 (5.7) | 406 (30.4) |
| Head size | ||||||
| <32 mm | 1373 (19.5) | 9573 (35.3) | 5310 (57.6) | 115 (20.4) | 971 (60.1) | 973 (72.8) |
| ≥32 mm | 5662 (80.5) | 17,533 (64.7) | 3908 (42.4) | 449 (79.6) | 645 (39.9) | 363 (27.2) |
| Hybrid | ||||||
| Sex | ||||||
| Male | 391 (31.8) | 7806 (42.1) | 523 (34.2) | 58 (29.3) | 90 (35.2) | 109 (46.2) |
| Female | 837 (68.2) | 10,742 (57.9) | 1008 (65.8) | 140 (70.7) | 166 (64.8) | 127 (53.8) |
| Bearing type | ||||||
| Ceramic on ceramic | 1974 (10.6) | 135 (8.8) | 1 (0.5) | 4 (1.6) | ||
| Ceramic on conventional polyethylene | 12 (1) | 189 (1) | 429 (28) | 29 (11.3) | 44 (18.6) | |
| Ceramic on highly cross-linked polyethylene | 49 (4) | 1573 (8.5) | 50 (3.3) | 6 (2.3) | 10 (4.2) | |
| Metal on conventional polyethylene | 355 (28.9) | 2057 (11.1) | 763 (49.8) | 10 (5.1) | 203 (79.3) | 113 (47.9) |
| Metal on highly cross-linked polyethylene | 812 (66.1) | 12,755 (68.8) | 154 (10.1) | 187 (94.4) | 14 (5.5) | 69 (29.2) |
| Head size | ||||||
| <32 mm | 592 (48.2) | 11,240 (60.6) | 1397 (91.2) | 127 (64.1) | 241 (94.1) | 211 (89.4) |
| ≥32 mm | 636 (51.8) | 7308 (39.4) | 134 (8.8) | 71 (35.9) | 15 (5.9) | 25 (10.6) |
| Cemented | ||||||
| Sex | ||||||
| Male | 11 (29.7) | 2304 (43) | 87 (29.3) | 4057 (30.3) | 4 (23.5) | |
| Female | 26 (70.3) | 3054 (57) | 210 (70.7) | 9321 (69.7) | 13 (76.5) | |
| Bearing type | ||||||
| Ceramic on conventional polyethylene | 82 (1.5) | 119 (40.1) | 3776 (28.2) | |||
| Ceramic on highly cross-linked polyethylene | 1 (2.7) | 71 (1.3) | 2 (0.7) | 208 (1.6) | ||
| Metal on conventional polyethylene | 6 (16.2) | 1930 (36) | 149 (50.2) | 8856 (66.2) | 17 (100) | |
| Metal on highly cross-linked polyethylene | 30 (81.1) | 3275 (61.1) | 27 (9.1) | 538 (4) | ||
| Head size | ||||||
| <32 mm | 13 (35.1) | 4850 (90.5) | 290 (97.6) | 12,965 (96.9) | 15 (88.2) | |
| ≥32 mm | 24 (64.9) | 508 (9.5) | 7 (2.4) | 413 (3.1) | 2 (11.8) | |
| Age of seventy-five years or more | ||||||
| Uncemented | ||||||
| Sex | ||||||
| Male | 1953 (37) | 7701 (43.8) | 2028 (35.1) | 152 (38.9) | 360 (31.6) | 879 (43.7) |
| Female | 3331 (63) | 9867 (56.2) | 3749 (64.9) | 239 (61.1) | 780 (68.4) | 1132 (56.3) |
| Bearing type | ||||||
| Ceramic on ceramic | 7 (0.1) | 3914 (22.3) | 1801 (31.2) | 1 (0.3) | 223 (19.6) | 64 (3.2) |
| Ceramic on conventional polyethylene | 11 (0.2) | 429 (2.4) | 1310 (22.7) | 386 (33.9) | 112 (5.6) | |
| Ceramic on highly cross-linked polyethylene | 369 (7) | 1799 (10.2) | 457 (7.9) | 24 (6.1) | 166 (14.6) | 89 (4.4) |
| Metal on conventional polyethylene | 234 (4.4) | 1199 (6.8) | 1491 (25.8) | 5 (1.3) | 220 (19.3) | 968 (48.1) |
| Metal on highly cross-linked polyethylene | 4663 (88.2) | 10,227 (58.2) | 718 (12.4) | 361 (92.3) | 145 (12.7) | 778 (38.7) |
| Head size | ||||||
| <32 mm | 990 (18.7) | 6459 (36.8) | 3498 (60.6) | 51 (13) | 787 (69) | 1600 (79.6) |
| ≥32 mm | 4294 (81.3) | 11,109 (63.2) | 2279 (39.4) | 340 (87) | 353 (31) | 411 (20.4) |
| Hybrid | ||||||
| Sex | ||||||
| Male | 523 (26.2) | 7658 (34.7) | 559 (31.9) | 103 (25.7) | 41 (25.8) | 472 (41.3) |
| Female | 1471 (73.8) | 14,407 (65.3) | 1191 (68.1) | 298 (74.3) | 118 (74.2) | 671 (58.7) |
| Bearing type | ||||||
| Ceramic on ceramic | 1177 (5.3) | 187 (10.7) | 2 (1.3) | 5 (0.4) | ||
| Ceramic on conventional polyethylene | 13 (0.7) | 141 (0.6) | 418 (23.9) | 16 (10.1) | 122 (10.7) | |
| Ceramic on highly cross-linked polyethylene | 58 (2.9) | 1167 (5.3) | 114 (6.5) | 3 (0.7) | 3 (1.9) | 11 (1) |
| Metal on conventional polyethylene | 421 (21.1) | 2363 (10.7) | 816 (46.6) | 22 (5.5) | 126 (79.2) | 652 (57) |
| Metal on highly cross-linked polyethylene | 1502 (75.3) | 17,217 (78) | 215 (12.3) | 376 (93.8) | 12 (7.5) | 353 (30.9) |
| Head size | ||||||
| <32 mm | 739 (37.1) | 12,440 (56.4) | 1482 (84.7) | 201 (50.1) | 151 (95) | 1000 (87.5) |
| ≥32 mm | 1255 (62.9) | 9625 (43.6) | 268 (15.3) | 200 (49.9) | 8 (5) | 143 (12.5) |
| Cemented | ||||||
| Sex | ||||||
| Male | 27 (27) | 2581 (33.4) | 416 (25.5) | 4241 (26.9) | 185 (30.2) | |
| Female | 73 (73) | 5146 (66.6) | 1216 (74.5) | 5 (100) | 11,539 (73.1) | 427 (69.8) |
| Bearing type | ||||||
| Ceramic on conventional polyethylene | 63 (0.8) | 244 (15) | 3902 (24.7) | 5 (0.8) | ||
| Ceramic on highly cross-linked polyethylene | 5 (5) | 79 (1) | 29 (1.8) | 161 (1) | ||
| Metal on conventional polyethylene | 13 (13) | 2927 (37.9) | 1031 (63.2) | 5 (100) | 11,078 (70.2) | 607 (99.2) |
| Metal on highly cross-linked polyethylene | 82 (82) | 4658 (60.3) | 328 (20.1) | 639 (4) | ||
| Head size | ||||||
| <32 mm | 17 (17) | 6364 (82.4) | 1600 (98) | 5 (100) | 14,918 (94.5) | 562 (91.8) |
| ≥32 mm | 83 (83) | 1363 (17.6) | 32 (2) | 862 (5.5) | 50 (8.2) | |
This table excludes patients under the age of forty-five years, reverse hybrids, and cemented ceramic-on-ceramic bearings.
Some cells of the table are empty because bearings and age groups are seldom implanted with certain modes of fixation. If the register has relatively few cases presented, it is possible that cells remain empty.
The values are given as the number of implants, with the percentage in parentheses.
The final survival model included the effects of age by fixation, sex, bearing surface, head size, time (in one-year intervals), and fixed registry effects (Table II).
For patients seventy-five years of age and older, uncemented fixation had a significantly higher risk of revision (p < 0.001) than hybrid fixation, with a hazard ratio of 1.575 (95% confidence interval [95% CI], 1.389 to 1.786). We also saw a similar, if lesser, effect in the intermediate age group of sixty-five to seventy-four years (hazard ratio, 1.16 [95% CI, 1.023 to 1.315]; p = 0.021) and in the younger age group of forty-five to sixty-four years (hazard ratio, 1.205 [95% CI, 1.008 to 1.442]; p = 0.041). There were no significant differences between hybrid and cemented bearings across age groups.
Female patients had a significantly lower risk of revision than male patients (p < 0.001).
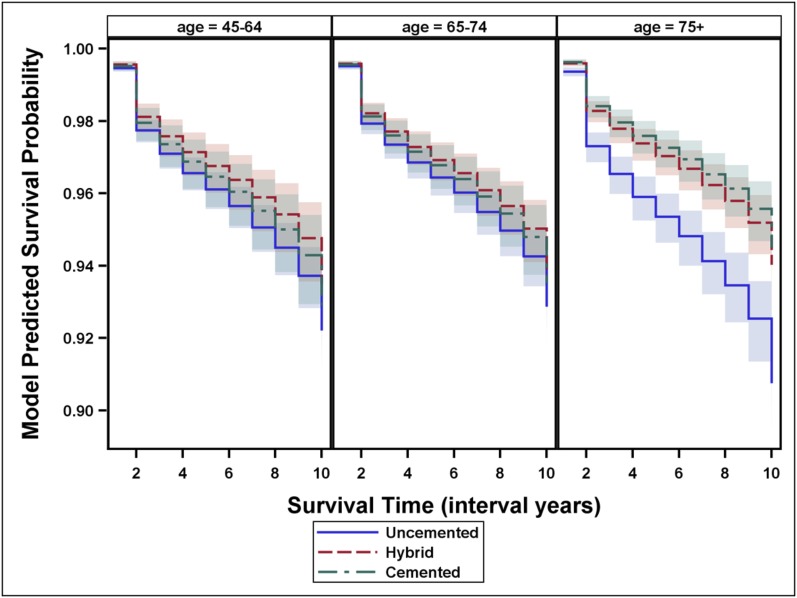
The fixed-effects model results are shown in Table II, and the estimated survival function is shown in Figure 2.
Fig. 2.
Model-predicted survival of uncemented, hybrid, and cemented hip replacements by age group. The predicted survival is a graphic representation of the fixed-effects model and not a survival curve. The x-axis values of 0 to 10 correspond to the interval years zero to one year to more than nine years to ten years. Confidence intervals are based on a normal distribution.
Discussion
We found an inferior result for uncemented total hip replacements compared with hybrids and cemented total hip replacements, especially in the older age group. In the other two groups, a similar result was obtained, but with lower statistical evidence.
The theme of fixation of total hip replacement is still debated because of the different approaches and practices of orthopaedic surgeons in different countries. In a report based on data from the Nordic Arthroplasty Register Association (NARA) of results on 347,899 implants from the period 1995 to 2011 performed in Sweden, Norway, Denmark, and Finland, Mäkelä et al.13 concluded that, when adjusted for age, sex, and diagnosis, the survival of cemented implants for total hip replacement was higher than that of uncemented implants in patients sixty-five years of age or older.
Similar results were obtained by Troelsen et al., who analyzed results extracted from the annual reports of seven national hip registries and verified that cemented fixation in patients older than seventy-five years results in the lowest risk of revision14. The difference between the age groups in the two papers13,14 is not marginal, because it is in the age range of sixty-five years to seventy-five years that the largest number of interventions occurs.
Different results were obtained in a randomized trial by Corten et al., who observed that a Kaplan-Meier survivorship analysis at twenty years revealed lower survival rates of cemented total hip replacements compared with uncemented total hip replacements15.
Single registries provide different results. In Australia, after adjustment for age and sex, and excluding larger head sizes, uncemented implants had a lower risk for revision than cemented implants when used to treat osteoarthrosis, but the difference was not significant. The Australian registry also had similar findings with no age stratification for all single age groups up to seventy-four years. Patients seventy-five years of age or older benefitted from cemented or hybrid fixation16.
On the contrary, registries of countries where cement is largely used in implants, such as Norway and Sweden, have reached different conclusions. Hailer et al.17 analyzed data on 170,413 implants for patients treated in Sweden from 1992 to 2007 and concluded that the survival of uncemented total hip replacements at ten years of follow-up is lower than that of cemented total hip replacements, and no age or diagnosis groups benefited from the use of uncemented fixation. In the Swedish experience, the reason for this is mainly attributed to the poor performance of uncemented cups.
The conclusions related to this fixation topic are of prominent interest not only for the safety of patients, but also for economics, as pointed out by many authors18-20. Some authors have concluded that the most cost-effective prostheses are hybrid prostheses in patients older than eighty-three years of age and cementless prostheses in patients younger than forty-three years of age. In the intermediate ages, there is a favorable situation for uncemented implants of a variable degree18. Other authors have concluded that cemented prostheses were the least costly type for total hip replacement; however, for most patient groups, hybrid prostheses were the most cost-effective, and uncemented prostheses did not provide sufficient improvement in health outcomes to justify their additional costs19.
Strengths and Limitations
The important strengths of our study included the largest multinational prospective registry cohort based on six registries situated in three continents, reflecting treatments on patients who are anthropologically different, using prosthetic devices that are only partially overlapping.
The limitations included the lack of knowledge on causes of failure of implants. Further, the data did not allow studying differences between brands of prostheses and cements, so it was not possible to identify outliers.
In conclusion, data obtained in the present analysis indicate that uncemented fixation should be avoided in older patients (seventy-five years of age or older), although this evidence is less strong in patients of the intermediate and youngest age groups.
Appendix—Details of the Model Fitting
For the models examining the effects of age and fixation on the time to revision, we examined the sensitivity of the results to outlier observations (all data and removing observations with standard errors of >0.05, >0.025, or >0.0125), and we determined that removing observations with a standard error of >0.025 would sufficiently limit the inaccuracies arising from observations providing unreliable information. The fixed-effects model was based on the random-effects model selected. We began with a model that includes fixed effects for intercept, sex, age, fixation, bearing surface, and time and registry-level random effects for intercept and residual variance fixed at 1. For the random-effects model, time was based on one-year intervals from zero to one year through nine to ten years. Likelihood ratio tests revealed that the interaction between age and fixation significantly improved (p < 0.001) the model fit (χ2(4) = 25.4826), and it was included in all subsequent models. In our final model, there was no evidence of improved fit (p = 1.0) when including age or fixation interactions with bearing surface or head size, sex, or time (χ2(120) = 34.4117). The results of the random-effects model are presented in Table IV.
TABLE IV.
Results from the Random-Effects Model*
| Hazard Ratio† | P Value | |
| Time | ||
| One year | Reference | — |
| More than one year to two years | 4.249 (3.819 to 4.727) | <0.001 |
| More than two years to three years | 5.479 (4.920 to 6.100) | <0.001 |
| More than three years to four years | 6.499 (5.834 to 7.240) | <0.001 |
| More than four years to five years | 7.374 (6.615 to 8.220) | <0.001 |
| More than five years to six years | 8.263 (7.407 to 9.218) | <0.001 |
| More than six years to seven years | 9.397 (8.413 to 10.496) | <0.001 |
| More than seven years to eight years | 10.497 (9.383 to 11.743) | <0.001 |
| More than eight years to nine years | 12.036 (10.717 to 13.518) | <0.001 |
| More than nine years to ten years | 15.057 (13.102 to 17.304) | <0.001 |
| Sex | ||
| Male | Reference | — |
| Female | 0.805 (0.763 to 0.850) | <0.001 |
| Head size | ||
| <32 mm | Reference | — |
| ≥32 mm | 0.836 (0.775 to 0.902) | <0.001 |
| Bearing type | ||
| Ceramic on ceramic | Reference | — |
| Ceramic on conventional polyethylene | 0.969 (0.846 to 1.111) | 0.655 |
| Ceramic on highly cross-linked polyethylene | 1.084 (0.952 to 1.234) | 0.226 |
| Metal on conventional polyethylene | 1.046 (0.936 to 1.169) | 0.426 |
| Metal on highly cross-linked polyethylene | 0.830 (0.760 to 0.907) | <0.001 |
| Fixation effects by age | ||
| Hybrid, forty-five to more than seventy-five years | Reference | — |
| Uncemented, forty-five to sixty-four years | 1.206 (1.021 to 1.423) | 0.028 |
| Cemented, forty-five to sixty-four years | 1.095 (0.884 to 1.357) | 0.406 |
| Uncemented, sixty-five to seventy-four years | 1.160 (1.032 to 1.304) | 0.013 |
| Cemented, sixty-five to seventy-four years | 1.051 (0.907 to 1.217) | 0.511 |
| Uncemented, seventy-five years or more | 1.559 (1.387 to 1.751) | <0.001 |
| Cemented, seventy-five years or more | 0.913 (0.790 to 1.055) | 0.217 |
The estimate (and the standard error) was −5.049 ± 0.091 for the fixed intercept and 0.013 ± 0.018 for the random intercept.
The values are given as the hazard ratio, with the 95% CI in parentheses.
Acknowledgments
Note: We thank all units submitting data to the registries; their data were essential for this study. We also gratefully acknowledge Lucas Romero and Rebecca Love for their superb organizational support.
Footnotes
Disclosure: One or more of the authors received payments or services, either directly or indirectly (i.e., via his or her institution), from a third party in support of an aspect of this work. None of the authors, or their institution(s), have had any financial relationship, in the thirty-six months prior to submission of this work, with any entity in the biomedical arena that could be perceived to influence or have the potential to influence what is written in this work. In addition, no author has had any other relationships, or has engaged in any other activities, that could be perceived to influence or have the potential to influence what is written in this work. The complete Disclosures of Potential Conflicts of Interest submitted by authors are always provided with the online version of the article.
References
- 1.Dunbar MJ. Cemented femoral fixation: the North Atlantic divide. Orthopedics. 2009September;32(9). [DOI] [PubMed] [Google Scholar]
- 2.Sedrakyan A, Paxton EW, Marinac-Dabic D. Stages and tools for multinational collaboration: the perspective from the coordinating center of the International Consortium of Orthopaedic Registries (ICOR). J Bone Joint Surg Am. 2011December21;93(Suppl 3):76-80. [DOI] [PubMed] [Google Scholar]
- 3.Brown JS, Holmes JH, Shah K, Hall K, Lazarus R, Platt R. Distributed health data networks: a practical and preferred approach to multi-institutional evaluations of comparative effectiveness, safety, and quality of care. Med Care. 2010June;48(6)(Suppl):S45-51. [DOI] [PubMed] [Google Scholar]
- 4.Maro JC, Platt R, Holmes JH, Strom BL, Hennessy S, Lazarus R, Brown JS. Design of a national distributed health data network. Ann Intern Med. 2009September1;151(5):341-4 Epub 2009 Jul 28. [DOI] [PubMed] [Google Scholar]
- 5.Arends LR, Hunink MG, Stijnen T. Meta-analysis of summary survival curve data. Stat Med. 2008September30;27(22):4381-96. [DOI] [PubMed] [Google Scholar]
- 6.Dear KB. Iterative generalized least squares for meta-analysis of survival data at multiple times. Biometrics. 1994December;50(4):989-1002. [PubMed] [Google Scholar]
- 7.Kalaian A, Raudenbush S. A multivariate mixed linear model for meta-analysis. Psychol Methods. 1996;1(3):227-35. [Google Scholar]
- 8.Kutner M, Nachtsheim C, Neter J, Applied linear statistical models. New York: McGraw-Hill/Irwin; 2004. [Google Scholar]
- 9.DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986September;7(3):177-88. [DOI] [PubMed] [Google Scholar]
- 10.Hedges LV, Vevea JL. Fixed- and random-effects models in meta-analysis. Psychol Methods. 1998;3:486-504. [Google Scholar]
- 11.Localio AR, Berlin JA, Ten Have TR, Kimmel SE. Adjustments for center in multicenter studies: an overview. Ann Intern Med. 2001July17;135(2):112-23. [DOI] [PubMed] [Google Scholar]
- 12.Allison PD. Fixed effects regression models. Thousand Oaks, CA: Sage Publications; 2009. [Google Scholar]
- 13.Mäkelä KT, Matilainen M, Pulkkinen P, Fenstad AM, Havelin L, Engesaeter L, Furnes O, Pedersen AB, Overgaard S, Kärrholm J, Malchau H, Garellick G, Ranstam J, Eskelinen A. Failure rate of cemented and uncemented total hip replacements: register study of combined Nordic database of four nations. BMJ. 2014;348:f7592 Epub 2014 Jan 13. [DOI] [PubMed] [Google Scholar]
- 14.Troelsen A, Malchau E, Sillesen N, Malchau H. A review of current fixation use and registry outcomes in total hip arthroplasty: the uncemented paradox. Clin Orthop Relat Res. 2013July;471(7):2052-9 Epub 2013 Mar 29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Corten K, Bourne RB, Charron KD, Au K, Rorabeck CH. What works best, a cemented or cementless primary total hip arthroplasty?: minimum 17-year followup of a randomized controlled trial. Clin Orthop Relat Res. 2011January;469(1):209-17 Epub 2010 Jul 13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Australian Orthopedic Association. National Joint Replacement Registry. Annual reports 2013. 2013. https://aoanjrr.dmac.adelaide.edu.au/en/annual-reports-2013. Accessed 2014 May 12.
- 17.Hailer NP, Garellick G, Kärrholm J. Uncemented and cemented primary total hip arthroplasty in the Swedish Hip Arthroplasty Register. Acta Orthop. 2010February;81(1):34-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Di Tanna GL, Ferro S, Cipriani F, Bordini B, Stea S, Toni A, Silipo F, Pirini G, Grilli R. Modeling the cost-effectiveness for cement-less and hybrid prosthesis in total hip replacement in Emilia Romagna, Italy. J Surg Res. 2011August;169(2):227-33 Epub 2009 Nov 11. [DOI] [PubMed] [Google Scholar]
- 19.Pennington M, Grieve R, Sekhon JS, Gregg P, Black N, van der Meulen JH. Cemented, cementless, and hybrid prostheses for total hip replacement: cost effectiveness analysis. BMJ. 2013February27;346:f1026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kallala R, Anderson P, Morris S, Haddad FS. The cost analysis of cemented versus cementless total hip replacement operations on the NHS. Bone Joint J. 2013July;95(7):874-6. [DOI] [PubMed] [Google Scholar]