Abstract
Background:
One of the least researched areas in orthopaedic pediatrics is the safety and effectiveness of joint replacement, in part because it is uncommon and is undertaken for a wide range of conditions not common for adult joint replacement. This study used data from the AOANJRR (Australian Orthopaedic Association National Joint Replacement Registry) to analyze the use of total hip arthroplasty (THA) and total knee arthroplasty (TKA) in the pediatric population and to provide preliminary data on the outcome of these procedures.
Methods:
The AOANJRR, which is part of the ICOR (International Consortium of Orthopaedic Registries), provided information on pediatric procedures reported to the registry by hospitals undertaking arthroplasty procedures in Australia. All THA and TKA procedures reported to the registry from 1999 to 2012 were included. The cumulative percent revision and the hazard ratio from Cox proportional-hazards models were used for analysis. All tests were two-tailed, with a 5% level of significance. Additionally, an overview of the literature is presented to provide a point of reference.
Results:
Primary conventional THA was performed in 297 patients twenty years of age or younger; the cumulative percent revision at five years was 4.5%. Primary conventional THA was performed in 975 young adults twenty-one to thirty years of age; the cumulative percent revision at five years was 5.4%. Primary THA was performed in 105 patients twenty years of age or younger; the cumulative percent revision at five years was 4.6%. Primary TKA was performed in 159 young adults twenty-one to thirty years of age; the cumulative percent revision at five years was 10.3%.
Conclusions:
Compared with older adults, pediatric patients and young adults undergoing THA and TKA have very different diagnoses, including a high prevalence of tumor. Although the reported rate of revision surgery is currently similar to that for older patients, the number of reported procedures and the follow-up period remain limited. It is important for registries to continue to collect and analyze data relevant to this cohort and to coordinate these activities in order to better understand the safety and effectiveness of joint arthroplasty in the pediatric population.
One of the least researched areas in pediatric orthopaedics is the safety and effectiveness of joint replacement. Joint replacement in this age group is relatively uncommon and is used to treat conditions that are not common reasons for adult joint replacement. Degenerative joint disease, in particular osteoarthritis, is the principal diagnosis responsible for almost 90% of primary total hip arthroplasties (THAs) and >90% of primary total knee arthroplasties (TKAs) in the adult population. In contrast, end-stage juvenile inflammatory arthritis, severe developmental dysplasia (developmental dislocation) of the hip, various causes of osteonecrosis, and tumors are some of the most common reasons for joint replacement in pediatric patients1-7. The treatment of severe articular and periarticular disease in young people is controversial, with many researchers advocating conservative therapies or alternative operative approaches while others recommend that joint replacement be considered depending on the diagnosis, degree of disability, and long-term outlook for the child5.
To our knowledge, the number of pediatric patients in the U.S. receiving joint replacement is unknown. Although uncommon, it is possible that a considerable number have undergone this surgery. It has been estimated that 10,000 to 30,000 patients less than twenty-five years of age have undergone joint replacement procedures in the last five years, and it is likely that many of those are pediatric patients8. It can also be anticipated that the rate of joint replacement in pediatric patients will increase, particularly given the popularity of this surgery and the incidence of diagnoses that may result in joint replacement surgery. Currently, over 294,000 individuals younger than twenty-one years of age are estimated to have juvenile arthritis9.
To our knowledge, the outcome of joint replacement in this age group is unknown. It is possible that such patients have more complications and earlier revision compared with the adult population, and there are several reasons for suspecting this to be the case. The surgery is potentially more difficult and more extensive at this age, and some of the diagnoses leading to joint replacement are likely to be associated with increased surgical risks6. Pediatric patients may require smaller, more complex, or customized implants, which may also be associated with an increased rate of early revision. Knowing the outcome of joint replacement surgery in this population is particularly important as many pediatric patients receiving joint replacement can be expected to have a normal or nearly normal life expectancy. In adults, joint replacement is usually the final solution to the management of a degenerative joint. In pediatric patients, however, it is likely to be the first step in the life-long orthopaedic management of the affected joint, which will involve subsequent arthroplasty procedures on that joint. As repeated revision procedures are associated with increasingly less satisfactory outcomes, it is imperative that the aim of the first procedure be to obtain the best outcome possible in the clinical circumstance10.
The current literature is inadequate to determine outcomes. It consists of small case series with variable diagnoses and variable implants, making interpretation difficult10. Additionally, many of the studies do not refer to pediatric patients per se, but instead include young adults or middle-aged patients undergoing joint replacement who have a history of a pediatric condition such as juvenile arthritis that has led to either THA or TKA. In comparison with joint replacement surgery in the adult population, there are evident gaps in our knowledge. Fundamental issues such as the choice of bearing surface and fixation have not been addressed11. It is imperative that intermediate to long-term outcome studies be undertaken to determine the most effective treatment strategies in this population.
The low rate of joint replacement in pediatric patients means that it is difficult to obtain adequate numbers by means of a conventional study design. In contrast, registries are particularly effective at providing information on rare events. The present study made use of a national registry to determine the utilization of hip and knee replacement in the pediatric population and to provide preliminary data on the outcome of those procedures.
Materials and Methods
As part of the current series of ICOR (International Consortium of Orthopaedic Registries) projects, the AOANJRR (Australian Orthopaedic Association National Joint Replacement Registry) was asked to provide information on pediatric procedures reported to the registry. The AOANJRR commenced data collection in September 1999. Implementation was performed in a staged manner across the Australian states and territories, becoming fully national during 2002. Data are collected from all hospitals (both government and private) performing arthroplasty procedures. The AOANJRR has extensive validation processes, including use of a sequential multilevel matching process against health department unit data provided to the registry by each of the states and territories. Each hospital in Australia is required to report separation data to its relevant state or territory health department; separation data detail all admissions to hospitals, including the diagnosis and any procedures performed. Matching this to existing registry data enables the AOANJRR to identify the small number of unreported procedures. Following the retrieval of any unreported records and checking of mismatched data, the registry is able to obtain an almost complete and accurate data set relating to hip and knee arthroplasty in Australia.
The present study included all THA and TKA procedures reported to the registry up to the end of December 2012. The outcomes of patients younger than twenty-one years of age were compared with those of patients twenty-one to thirty, thirty-one to forty, and forty-one to fifty years of age. The principal outcome measure was the time to the first revision, assessed by means of both the number of revisions per 100 observed component years and Kaplan-Meier estimates of survivorship.
The cumulative percent revision at a certain time (e.g., five years) is the complement of the Kaplan-Meier survivorship function at that time (expressed as a probability) multiplied by 100. This percentage accounts for right-censoring due to death and “closure” of the database at the time of analysis. Confidence intervals for the cumulative percent revision are unadjusted pointwise Greenwood estimates.
Hazard ratios (HRs) from Cox proportional-hazards models, adjusting for age and sex where appropriate, were used to compare revision rates. For each model, the assumption of proportional hazards was checked analytically. If the interaction between the predictor and the logarithm of the time since surgery was significant in the standard Cox model, then a time-varying model was estimated. In that model, time points were chosen iteratively until the assumption of proportionality was met, and the HR for each selected time period was then calculated. If we report an HR value without specifying the time period, the HR is over the entire follow-up period. A p value of 0.05 (two-sided) was considered significant.
Results
Hip Replacement
The AOANJRR identified 297 primary THAs performed in patients younger than twenty-one years of age during the study period. This represents 0.08% of all THA procedures reported during that time. Approximately 55% of the patients were female. Osteonecrosis (29% of procedures) and osteoarthritis (28%) were the most common diagnoses. However, 12% had various types of dysplasia and 15% had autoimmune arthritis reported as the primary diagnosis. An additional 9% involved treatment for a bone tumor. Conventional THA (85%) was the most frequently used procedure, followed by total hip resurfacing (9%). Cementless fixation was used in 69% of procedures, and hybrid fixation involving cementation of only the femoral component was used in 21%.
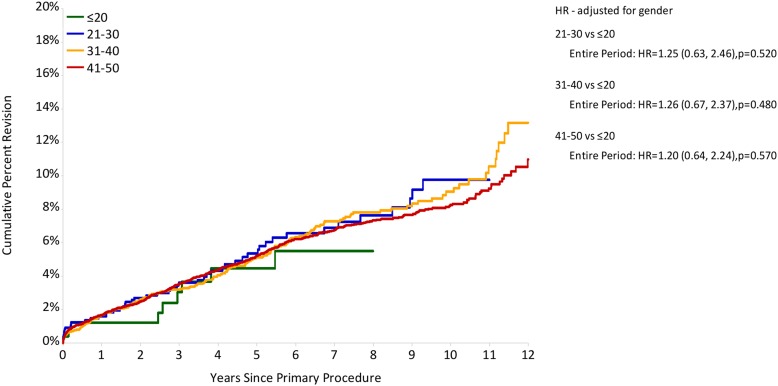
The cumulative percent revision at five years was 4.5% (95% CI [confidence interval], 2.2% to 8.9%) in patients younger than twenty-one years of age (Fig. 1). No sex difference was observed. Twenty-eight of the procedures in this age group had involved hip resurfacing arthroplasty; one of these required revision at three years and eight months. Five-year mortality was significantly higher if the patient had a primary diagnosis of tumor (34%) compared with all other diagnoses (2%) (HR = 11.39, 95% CI = 2.98 to 45.5, p < 0.001).
Fig. 1.
Cumulative percent revision of primary conventional THAs according to age group (in years). The HRs (with 95% CIs) and p values for the comparisons between groups are also given.
A total of 975 conventional THA procedures were performed in patients twenty-one to thirty years of age. The cumulative percent revision at five years in this group was 5.4% (95% CI, 3.9% to 7.3%), which was higher than that in any of the other three age groups, although not significantly so (Fig. 1).
The most common bearing surface for conventional hip arthroplasty in patients younger than twenty-one years of age was ceramic-on-ceramic (40%), followed by metal-on-XLPE (cross-linked polyethylene) and metal-on-metal (22% each). Ceramic-on-XLPE bearings were less common (8%), and metal-on-conventional polyethylene was used in 4%. The number of revisions (ten) was too small to permit meaningful comparisons to determine the effect of the bearing surface.
One in every three revisions in patients younger than twenty-one years of age was caused by loosening and/or osteolysis, making this the most common cause for revision. Prosthesis dislocation and infection were the next most common causes, each causing 18% of revisions.
Knee Replacement
The AOANJRR identified 105 primary TKAs performed in patients younger than twenty-one years of age during the study period. This represents 0.025% of all TKA procedures reported during that time. Approximately 35% of these patients were female. The most common diagnosis was tumor (77%), followed by some form of juvenile arthritis (17%).
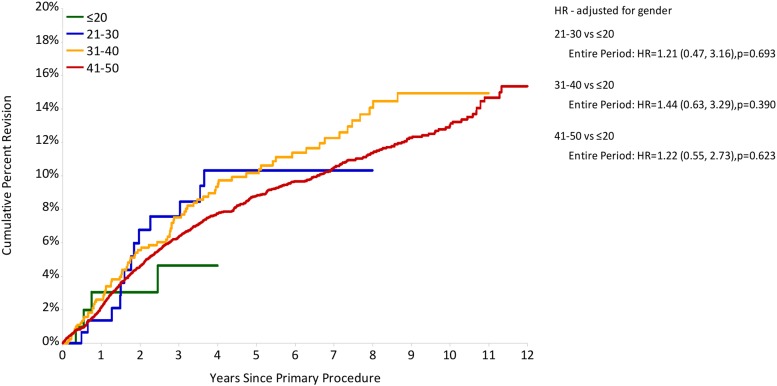
The cumulative percent revision at four years was 4.6% in this group (Fig. 2). No sex-related difference was observed. The overall five-year mortality rate was 35%. The most common bearing surface in this age group was metal-on-non-cross-linked polyethylene (98%).
Fig. 2.
Cumulative percent revision of primary conventional TKAs according to age group (in years). The HRs (with 95% CIs) and p values for the comparisons between groups are also given.
A total of 159 primary TKAs were performed in patients twenty-one to thirty years of age; 55% of these patients were female. The cumulative percent revision at four years was 10.3% in this age group; after the first year, the rate was consistently four times higher in male than in female patients.
Fourteen revisions were performed in patients twenty-one to thirty years of age, with the most common reason being infection (n = 6).
Discussion
Current literature on pediatric patients is limited because of the small number of arthroplasty procedures performed in this age group. Most of the articles available include both pediatric patients and younger adults, as the frequency of arthroplasty procedures remains relatively low even in an expanded group of patients younger than fifty-five years of age12. To evaluate the consistency of the results from the present study with the literature, we conducted a focused review of all available literature for arthroplasty patients younger than thirty years of age. We also included studies with a mixture of young adult and younger patients if the mean age did not exceed thirty-five years.
Literature on THA
Twenty-two studies with a total of 684 patients and 1011 THAs were identified by the literature search and reviewed; all of these studies included at least some patients younger than twenty-one years of age (Table I).
TABLE I.
Overview of the Literature Focused on THA in Cohorts That Included Patients Younger Than Thirty-one Years of Age*
| Authors | Year | No. of Patients/Hips | Revision Rate (%) | Mean Follow-up (yr) | Mean Age at Surgery (Range) (yr) | Most Common Stated Diagnoses |
| Roach and Paradies15 | 1984 | 6/10 | 33.0 | 7.9 | 13.2 (9-16) | Arthritis |
| Ruddlesdin et al.16 | 1986 | 42/75 | 14.0 | 5.4 | 14 (11-17) | JCA |
| Lachiewicz et al.17 | 1986 | 34/62 | 3.0 | 6.0 | 26 (NR) | JRA |
| Learmonth et al.18 | 1989 | 7/14 | 0 | 8.5 | 16 (12-22) | JCA |
| Witt et al.19† | 1991 | 54/96 | 25.0 | 11.5 | 16.7 (NR) | JCA |
| Cage et al.20 | 1992 | 17/22 | 3.4 | 10.6 | 18.4 (14-20) | NR |
| Maric and Haynes21 | 1993 | 17/17 | 7.7 | 9.3 | 18 (14-20) | NR |
| Hyder et al.22 | 1996 | 22/26 | 7.7 | 6.5 | 24 (17-30) | Perthes, PTA |
| Torchia et al.13 | 1996 | 50/63 | 42.9 | 11.0 | 17 (11-19) | JRA, CD, trauma, tumors |
| Chmell et al.14 | 1997 | 39/66 | 35.0 | 15.1 | 19.9 (11-29) | JRA |
| Kumar and Swann23 | 1998 | 16/25 | 12.0 | 4.5 | 24.9 (15-39) | SOD, JCA |
| Sochart and Porter24 | 1998 | 55/83 | 30.0 | 20.0 | 24.9 (17-29) | AS, CD, JRA, OA |
| Bessette et al.25 | 2003 | 11/15 | 33.0 | 13.6 | 16.5 (10-20) | NR |
| Dudkiewicz et al.26 | 2003 | 56/69 | 11.6 | 7.4 | 23.2 (14-29) | JRA, TA, DDH |
| Kitsoulis et al.27 | 2006 | 10/20 | 1.5 | 9.2 | 15.8 (13-24) | JCA |
| Restrepo et al.28 | 2008 | 25/35 | 3.0 | 6.6 | 17.6 (13.5-20) | AVN, JRA, DDH, SD, Perthes, OA, PTA, PRC |
| Wangen et al.29 | 2008 | 44/49 | 48.9 | 13 | 25 (15-30) | OA |
| Busch et al.30 | 2010 | 48/69 | 11.6 | 2.0 | 24.6 (16-29) | JRA, OFH |
| Clohisy et al.5 | 2010 | 88/102 | 7.0 | 2.0 | 20.0 (12-25) | ON, OA |
| Girard et al.31 | 2010 | 35/48 | 8.3 | 9.0 | 25 (15-30) | OFH |
| Finkbone et al.32 | 2012 | 19/24 | 4.0 | 2.4 | 16.4 (12-20) | AVN, JRA |
| Kamath et al.33 | 2012 | 18/21 | 5.5 | 4.1 | 18 (13-20) | CIO, SIO, SCD |
JCA = juvenile chronic arthritis, NR = not reported, JRA = juvenile rheumatoid arthritis, Perthes = Legg-Calvé-Perthes disease, PTA = posttraumatic arthritis, CD = congenital dysplasia, SOD = systemic onset disease, AS = ankylosing spondylitis, OA = osteoarthritis, TA = traumatic arthritis, DDH = developmental dislocation (dysplasia) of the hip, AVN = avascular necrosis, SD = spondyloepiphyseal dysplasia, PRC = pseudo rheumatoid chondrodysplasia, ON = osteonecrosis, OFH = osteonecrosis of femoral head, CIO = chemotherapy-induced osteonecrosis, SIO = steroid-induced osteonecrosis, and SCD = sickle cell disease. Note that some of the stated diagnoses (e.g., avascular necrosis and osteonecrosis) are equivalent.
Ruddlesdin et al. reported on twenty-nine of these cases in 1986.
The main reasons for THA in the 684 patients were juvenile arthritis, developmental dysplasia of the hip (including dislocation), and less commonly tumor, trauma, and spondyloepiphyseal dysplasia. The mean age at the time of surgery ranged from 13.2 to twenty-six years, and nine of the twenty-two reviewed studies included only patients younger than twenty-one years of age (Table I). All but one study reported the occurrence of revisions. The most common revision diagnosis was aseptic loosening of either the acetabular or the femoral component, with some reports of a higher incidence of acetabular loosening13. Other reasons for revision included prosthesis wear and femoral fracture. There was a general consensus that THA greatly decreased pain and greatly increased function in this population. However, some investigators found revision rates that led them to conclude that this procedure should be reserved for select patients in whom the benefits outweighed the risks13,14.
Literature on TKA
Nine studies with a total of 328 patients and 538 TKAs were identified by the literature search and reviewed; eight of these included at least some patients younger than twenty-one years of age (Table II).
TABLE II.
Overview of the Literature Focused on TKA in Cohorts That Included Patients Younger Than Thirty-one Years of Age*
| Authors | Year | No. of Patients/Knees | Revision Rate (%) | Mean Follow-up (yr) | Mean Age at Surgery (Range) (yr) | Most Common Stated Diagnoses |
| Sarokhan et al.7 | 1983 | 17/29 | 14.0 | 5.9 | 23.0 (13-39) | JRA |
| Carmichael and Chaplin34 | 1986 | 13/25 | 0 | 5.1 | 7.2 (1-15) | JRA |
| Boublik et al.35 | 1993 | 14/22 | 4.5 | 3.9 | 26.0 (NR) | JRA |
| Parvizi et al.36 | 2003 | 13/25 | 16.0 | 10.7 | 17.0 (13-19) | JRA |
| Palmer et al.4 | 2005 | 8/15 | 20.0 | 15.5 | 16.8 (NR) | JRA |
| Thomas et al.37 | 2005 | 10/17 | 0 | 6.0 | 22.4 (15-40) | JRA |
| Jolles and Bogoch38 | 2008 | 14/22 | 0 | 8.0 | 33.0 (15-42) | JRA |
| Malviya et al.3 | 2010 | 20/34 | 41.5† | 16.0 | NR | JRA |
| Heyse et al.6 | 2014 | 219/349 | 8.9 | 12.0 | 28.9 (11-58) | JRA |
JRA = juvenile rheumatoid arthritis, and NR = not reported.
Calculated from survivorship.
The main reason for TKA in the 328 patients was juvenile arthritis. The mean age ranged from 7.2 to 33.0 years. The most common reason for revision was infection; this was followed by loosening, which was thought to be due to a high activity level in these patients6. Additionally, stiffness was reported as a reason for revision in some patients. A small number of case studies indicated no revisions (Table II), and the follow-up duration in these studies was reasonable, suggesting that limited follow-up was not the reason. In most studies, mean range of motion improved, and quality of life likewise improved in the patients who regained mobility after the procedure.
Conclusions
Overall, the data from one of the largest national joint replacement registries in the world are consistent with the current literature. The present study has, however, established that joint arthroplasty in the pediatric population is rare. Only eighty of every 100,000 hip replacements and twenty-five of every 100,000 knee replacements were performed in patients younger than twenty-one years of age. In addition, the Australian registry data have provided a more comprehensive overview of the use of hip and knee replacement in this patient group at a national level, including a more complete perspective on the reasons for the procedure, the types of procedures performed, and the types of prostheses used. Despite the small sample size, the outcomes indicate that both hip and knee arthroplasty in this patient population can yield results similar to those of the same procedures in adults twenty-one to fifty years of age.
There remains a clear need, however, for long-term studies with larger numbers of patients to enable surgeons and regulators to better understand the effectiveness and safety of hip and knee implants in pediatric patients and young adults. Pediatric patients and young adults without conditions that seriously limit their life expectancy are likely to have more active lifestyles and require repeated surgery to maintain joint function. There is no evidence regarding the effectiveness of repeated surgery in this age group. In order to improve the data regarding primary procedures and fill the gap in knowledge regarding the outcome of revision procedures, it is essential that registries and other larger data repositories continue to collect relevant data.
In conclusion, patients younger than twenty-one years of age and those twenty-one to thirty years of age who undergo hip and knee arthroplasty have very different diagnoses compared with older adults, including a high prevalence of tumor. Although the rate of revision surgery currently appears similar to that in older patients, the number of reported procedures and the follow-up duration remain limited. It is important for registries to continue to collect and analyze data relevant to this cohort and to coordinate these activities in order to better understand the safety and effectiveness of joint arthroplasty in the pediatric population.
Footnotes
Disclosure: One or more of the authors received payments or services, either directly or indirectly (i.e., via his or her institution), from a third party in support of an aspect of this work. None of the authors, or their institution(s), have had any financial relationship, in the thirty-six months prior to submission of this work, with any entity in the biomedical arena that could be perceived to influence or have the potential to influence what is written in this work. In addition, no author has had any other relationships, or has engaged in any other activities, that could be perceived to influence or have the potential to influence what is written in this work. The complete Disclosures of Potential Conflicts of Interest submitted by authors are always provided with the online version of the article.
References
- 1.Thillemann TM, Pedersen AB, Johnsen SP, Søballe K; Danish Hip Arthroplasty Registry. Implant survival after primary total hip arthroplasty due to childhood hip disorders: results from the Danish Hip Arthroplasty Registry. Acta Orthop. 2008December;79(6):769-76. [DOI] [PubMed] [Google Scholar]
- 2.Engesaeter IO, Lie SA, Lehmann TG, Furnes O, Vollset SE, Engesaeter LB. Neonatal hip instability and risk of total hip replacement in young adulthood: follow-up of 2,218,596 newborns from the Medical Birth Registry of Norway in the Norwegian Arthroplasty Register. Acta Orthop. 2008June;79(3):321-6. [DOI] [PubMed] [Google Scholar]
- 3.Malviya A, Foster HE, Avery P, Weir DJ, Deehan DJ. Long term outcome following knee replacement in patients with juvenile idiopathic arthritis. Knee. 2010October;17(5):340-4 Epub 2009 Dec 4. [DOI] [PubMed] [Google Scholar]
- 4.Palmer DH, Mulhall KJ, Thompson CA, Severson EP, Santos ER, Saleh KJ. Total knee arthroplasty in juvenile rheumatoid arthritis. J Bone Joint Surg Am. 2005July;87(7):1510-4. [DOI] [PubMed] [Google Scholar]
- 5.Clohisy JC, Oryhon JM, Seyler TM, Wells CW, Liu SS, Callaghan JJ, Mont MA. Function and fixation of total hip arthroplasty in patients 25 years of age or younger. Clin Orthop Relat Res. 2010December;468(12):3207-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Heyse TJ, Ries MD, Bellemans J, Goodman SB, Scott RD, Wright TM, Lipman JD, Schwarzkopf R, Figgie MP. Total knee arthroplasty in patients with juvenile idiopathic arthritis. Clin Orthop Relat Res. 2014January;472(1):147-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sarokhan AJ, Scott RD, Thomas WH, Sledge CB, Ewald FC, Cloos DW. Total knee arthroplasty in juvenile rheumatoid arthritis. J Bone Joint Surg Am. 1983October;65(8):1071-80. [PubMed] [Google Scholar]
- 8.Agency for Healthcare Research and Quality. Welcome to H•CUPnet. http://hcupnet.ahrq.gov/. Accessed 2011 Jan 14. [DOI] [PubMed]
- 9.Arthritis Foundation. Juvenile arthritis fact sheet. http://www.arthritis.org/ja-fact-sheet.php. Accessed 2011 Jan 15.
- 10.Jäger M, Begg MJ, Ready J, Bittersohl B, Millis M, Krauspe R, Thornhill TS. Primary total hip replacement in childhood, adolescence and young patients: quality and outcome of clinical studies. Technol Health Care. 2008;16(3):195-214. [PubMed] [Google Scholar]
- 11.Jäger M, Endres S, Wilke A. [Total hip replacement in childhood, adolescence and young patients: a review of the literature] [German]. Z Orthop Ihre Grenzgeb. 2004Mar-Apr;142(2):194-212. [DOI] [PubMed] [Google Scholar]
- 12.Graves S, Davidson D, de Steiger R, Tomkins A. Adelaide, Australia: Australian Orthopaedic Association National Joint Replacement Registry; 2012. Hip and knee arthroplasty. Annual report 2012. https://aoanjrr.dmac.adelaide.edu.au/documents/10180/60142/Annual%20Report%202012?version=1.3&t=1361226543157. Accessed 30 Nov 2013.
- 13.Torchia ME, Klassen RA, Bianco AJ. Total hip arthroplasty with cement in patients less than twenty years old. Long-term results. J Bone Joint Surg Am. 1996July;78(7):995-1003. [DOI] [PubMed] [Google Scholar]
- 14.Chmell MJ, Scott RD, Thomas WH, Sledge CB. Total hip arthroplasty with cement for juvenile rheumatoid arthritis. Results at a minimum of ten years in patients less than thirty years old. J Bone Joint Surg Am. 1997January;79(1):44-52. [DOI] [PubMed] [Google Scholar]
- 15.Roach JW, Paradies LH. Total hip arthroplasty performed during adolescence. J Pediatr Orthop. 1984August;4(4):418-21. [DOI] [PubMed] [Google Scholar]
- 16.Ruddlesdin C, Ansell BM, Arden GP, Swann M. Total hip replacement in pediatric patients with juvenile chronic arthritis. J Bone Joint Surg Br. 1986March;68(2):218-22. [DOI] [PubMed] [Google Scholar]
- 17.Lachiewicz PF, McCaskill B, Inglis A, Ranawat CS, Rosenstein BD. Total hip arthroplasty in juvenile rheumatoid arthritis. Two to eleven-year results. J Bone Joint Surg Am. 1986April;68(4):502-8. [PubMed] [Google Scholar]
- 18.Learmonth ID, Heywood AW, Kaye J, Dall D. Radiological loosening after cemented hip replacement for juvenile chronic arthritis. J Bone Joint Surg Br. 1989March;71(2):209-12. [DOI] [PubMed] [Google Scholar]
- 19.Witt JD, Swann M, Ansell BM. Total hip replacement for juvenile chronic arthritis. J Bone Joint Surg Br. 1991September;73(5):770-3. [DOI] [PubMed] [Google Scholar]
- 20.Cage DJ, Granberry WM, Tullos HS. Long-term results of total arthroplasty in adolescents with debilitating polyarthropathy. Clin Orthop Relat Res. 1992October;283:156-62. [PubMed] [Google Scholar]
- 21.Maric Z, Haynes RJ. Total hip arthroplasty in juvenile rheumatoid arthritis. Clin Orthop Relat Res. 1993May;290:197-9. [PubMed] [Google Scholar]
- 22.Hyder N, Nevelos AB, Barabas TG. Cementless ceramic hip arthroplasties in patients less than 30 years old. J Arthroplasty. 1996September;11(6):679-86. [DOI] [PubMed] [Google Scholar]
- 23.Kumar MN, Swann M. Uncemented total hip arthroplasty in young patients with juvenile chronic arthritis. Ann R Coll Surg Engl. 1998May;80(3):203-9. [PMC free article] [PubMed] [Google Scholar]
- 24.Sochart DH, Porter ML. Long-term results of cemented Charnley low-friction arthroplasty in patients aged less than 30 years. J Arthroplasty. 1998February;13(2):123-31. [DOI] [PubMed] [Google Scholar]
- 25.Bessette BJ, Fassier F, Tanzer M, Brooks CE. Total hip arthroplasty in patients younger than 21 years: a minimum, 10-year follow-up. Can J Surg. 2003August;46(4):257-62. [PMC free article] [PubMed] [Google Scholar]
- 26.Dudkiewicz I, Salai M, Israeli A, Amit Y, Chechick A. Total hip arthroplasty in patients younger than 30 years of age. Isr Med Assoc J. 2003October;5(10):709-12. [PubMed] [Google Scholar]
- 27.Kitsoulis PB, Stafilas KS, Siamopoulou A, Soucacos PN, Xenakis TA. Total hip arthroplasty in pediatric patients with juvenile chronic arthritis: long-term results. J Pediatr Orthop. 2006Jan-Feb;26(1):8-12. [DOI] [PubMed] [Google Scholar]
- 28.Restrepo C, Lettich T, Roberts N, Parvizi J, Hozack WJ. Uncemented total hip arthroplasty in patients less than twenty-years. Acta Orthop Belg. 2008October;74(5):615-22. [PubMed] [Google Scholar]
- 29.Wangen H, Lereim P, Holm I, Gunderson R, Reikerås O. Hip arthroplasty in patients younger than 30 years: excellent ten to 16-year follow-up results with a HA-coated stem. Int Orthop. 2008April;32(2):203-8 Epub 2007 Feb 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Busch V, Klarenbeek R, Slooff T, Schreurs BW, Gardeniers J. Cemented hip designs are a reasonable option in young patients. Clin Orthop Relat Res. 2010December;468(12):3214-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Girard J, Bocquet D, Autissier G, Fouilleron N, Fron D, Migaud H. Metal-on-metal hip arthroplasty in patients thirty years of age or younger. J Bone Joint Surg Am. 2010October20;92(14):2419-26. [DOI] [PubMed] [Google Scholar]
- 32.Finkbone PR, Severson EP, Cabanela ME, Trousdale RT. Ceramic-on-ceramic total hip arthroplasty in patients younger than 20 years. J Arthroplasty. 2012February;27(2):213-9 Epub 2011 Aug 9. [DOI] [PubMed] [Google Scholar]
- 33.Kamath AF, Sheth NP, Hosalkar HH, Babatunde OM, Lee GC, Nelson CL. Modern total hip arthroplasty in patients younger than 21 years. J Arthroplasty. 2012March;27(3):402-8 Epub 2011 Jul 1. [DOI] [PubMed] [Google Scholar]
- 34.Carmichael E, Chaplin DM. Total knee arthroplasty in juvenile rheumatoid arthritis. A seven-year follow-up study. Clin Orthop Relat Res. 1986September;210:192-200. [PubMed] [Google Scholar]
- 35.Boublik M, Tsahakis PJ, Scott RD. Cementless total knee arthroplasty in juvenile onset rheumatoid arthritis. Clin Orthop Relat Res. 1993January;286:88-93. [PubMed] [Google Scholar]
- 36.Parvizi J, Lajam CM, Trousdale RT, Shaughnessy WJ, Cabanela ME. Total knee arthroplasty in young patients with juvenile rheumatoid arthritis. J Bone Joint Surg Am. 2003June;85(6):1090-4. [DOI] [PubMed] [Google Scholar]
- 37.Thomas A, Rojer D, Imrie S, Goodman SB. Cemented total knee arthroplasty in patients with juvenile rheumatoid arthritis. Clin Orthop Relat Res. 2005April;433:140-6. [DOI] [PubMed] [Google Scholar]
- 38.Jolles BM, Bogoch ER. Quality of life after TKA for patients with juvenile rheumatoid arthritis. Clin Orthop Relat Res. 2008January;466(1):167-78 Epub 2008 Jan 3. [DOI] [PMC free article] [PubMed] [Google Scholar]