Abstract
Background:
The rapid decline in use of conventional total hip replacement with a large femoral head size and a metal-on-metal bearing surface might lead to increased popularity of ceramic-on-ceramic bearings as another hard-on-hard alternative that allows implantation of a larger head. We sought to address comparative effectiveness of ceramic-on-ceramic and metal-on-HXLPE (highly cross-linked polyethylene) implants by utilizing the distributed health data network of the ICOR (International Consortium of Orthopaedic Registries), an unprecedented collaboration of national and regional registries and the U.S. FDA (Food and Drug Administration).
Methods:
A distributed health data network was developed by the ICOR and used in this study. The data from each registry are standardized and provided at a level of aggregation most suitable for the detailed analysis of interest. The data are combined across registries for comprehensive assessments. The ICOR coordinating center and study steering committee defined the inclusion criteria for this study as total hip arthroplasty performed without cement from 2001 to 2010 in patients forty-five to sixty-four years of age with osteoarthritis. Six national and regional registries (Kaiser Permanente and HealthEast in the U.S., Emilia-Romagna region in Italy, Catalan region in Spain, Norway, and Australia) participated in this study. Multivariate meta-analysis was performed with use of linear mixed models, with survival probability as the unit of analysis. We present the results of the fixed-effects model and include the results of the random-effects model in an appendix. SAS version 9.2 was used for all analyses. We first compared femoral head sizes of >28 mm and ≤28 mm within ceramic-on-ceramic implants and then compared ceramic-on-ceramic with metal-on-HXLPE.
Results:
A total of 34,985 patients were included; 52% were female. We found a lower risk of revision associated with use of ceramic-on-ceramic implants when a larger head size was used (HR [hazard ratio] = 0.73, 95% CI [confidence interval] = 0.60 to 0.88, p = 0.001). Use of smaller-head-size ceramic-on-ceramic bearings was associated with a higher risk of failure compared with metal-on-HXLPE bearings (HR = 1.36, 95% CI = 1.09 to 1.68, p = 0.006). Use of large-head-size ceramic-on-ceramic bearings was associated with a small protective effect relative to metal-on-HXLPE bearings (not subdivided by head size) in years zero to two, but this difference dissipated over the longer term.
Conclusions:
Our multinational study based on a harmonized, distributed network showed that use of ceramic-on-ceramic implants with a smaller head size in total hip arthroplasty without cement was associated with a higher risk of revision compared with metal-on-HXLPE and >28-mm ceramic-on-ceramic implants. These findings warrant careful reflection by regulatory and clinical communities and wide dissemination to patients for informed decision-making regarding such surgery.
More than 700,000 joint replacements, including more than 270,000 hip replacements, are performed annually in the United States alone1. Hip replacement is generally safe and effective, particularly when bearings such as metal-on-highly cross-linked polyethylene (M-HXLPE) are used. However, patients who receive hip implants can require revision surgery to replace the implant as a result of infection, dislocation, wear, instability, loosening, or other types of mechanical failure2-9. The risk of revision surgery can be mitigated by selection of better-performing bearings.
Rapid evolution of technology has brought a number of alternative bearings to the market. The alternatives aim to further improve postoperative functional and patient-reported outcomes, lower dislocation and loosening rates, and increase longevity through decreased wear-induced osteolysis and loosening. Recently, stemmed (conventional) metal-on-metal bearings with large femoral heads were attractive to surgeons as they were intended to reduce the risk of dislocation and improve the functional outcomes. However, evidence now shows that these devices are associated with unacceptably high rates of revision and potentially extensive soft-tissue damage leading to serious disability. In addition, high serum metal ion levels have been reported to occur in many cases. Patients with these implants need to have regular measurement of the metal ion levels in their blood and, if symptoms warrant it, regular MRA (magnetic resonance arthrography) examinations to assess the extent of any local soft-tissue damage10.
As the use of metal-on-metal conventional total hip replacement with a large femoral head size is rapidly declining, alternative hard-on-hard bearings such as ceramic-on-ceramic (C-C) that also allow implantation of a larger head size might become more popular. In the U.S., interest in C-C bearings started after multiple publications based on an FDA IDE (Food and Drug Administration Investigational Device Exemption) trial, a part of the pre-market application process, that compared C-C with metal-on-polyethylene (M-P) bearings11-15. That study had randomized and nonrandomized arms and indicated a substantially lower occurrence of revision in the C-C arms compared with the M-P arm even after ten years of follow-up15. However, C-C implants have various limitations such as breakage, squeaking (audible component-related noise), liner chipping, and canting16,17. Furthermore, many annual reports of national registries have not shown any advantage associated with use of C-C implants, and one national registry reported a higher revision rate associated with C-C implants compared with ceramic-on-polyethylene (C-P) bearings18.
We sought to investigate the comparative effectiveness of C-C and M-P implants by utilizing the distributed health data network of the ICOR (International Consortium of Orthopaedic Registries), a collaboration of these registries with the U.S. FDA that includes most of the countries and health plans that maintain orthopaedic registries with the requisite level of detailed patient and implant information19.
Materials and Methods
The distributed health data network developed by the ICOR was utilized in this study to reduce barriers to participation (e.g., involving data security, legal issues, proprietary information, and privacy) compared with an approach involving a centralized data warehouse20,21. A distributed health data network represents a decentralized model that allows secure storage and analysis of data from various registries22. Generally, the data from each registry are standardized (e.g., data elements are operationalized) and provided at a level of aggregation most suitable for the detailed analysis of interest, then ultimately combined across registries19.
The first step undertaken in the development of the health data network was an evaluation of the variation in international practice patterns (including patient selection, technology use, and procedural details). All interested registries participated, and a methodology committee discussed inclusion of key variables for analytic purposes. Next, each registry with an interest in participating completed simple tables indicating the means and proportions of patient and procedural characteristics.
Six national and regional registries (Kaiser Permanente and HealthEast in the U.S., Emilia-Romagna region in Italy, Catalan region in Spain, Norway, and Australia) participated in the present study. The ICOR coordinating center and study steering committee defined the inclusion criteria as total hip arthroplasty performed without cement from 2001 to 2010 in patients forty-five to sixty-four years of age with osteoarthritis. The inclusion criteria were defined to limit the potentially complex confounding and interactive effects of the fixation method and age on the relationship between the bearing surfaces being compared and the outcome. This sample restriction allowed us to pragmatically evaluate the effect of the bearing surface choice as an independent variable. The outcome of interest was the time to the first revision (for any reason). We focused on the outcome of C-C implants with two head-size ranges, >28 mm and ≤28 mm, in comparison with each other and with M-HXLPE implants with any head size. The choice of M-HXLPE as the control group was based on our initial research, in which the risk of revision of this bearing type was similar across all head sizes23, and the consensus by the ICOR steering committee that it is among the best-performing bearings and could be treated as a standard against which to compare all other bearings.
We first determined whether there was a difference between C-C implants with head sizes of >28 mm and ≤28 mm. Based on the findings in that analysis, we then compared these two types of C-C implants with all M-HXLPE implants.
Statistical Analyses
Multivariate meta-analyses were performed with use of linear mixed models, with the profile of each patient as the unit of analysis24. The models estimated the residual covariances according to a previously described method25, and a transformation26,27 was also performed to ensure that the models could be fitted with existing software (SAS version 9.2; SAS Institute, Cary, North Carolina). The survival probability and associated standard error (SE) were extracted from each registry for each possible combination of the covariates (e.g., bearing, head size, age) for each postoperative year; if multiple time points within a postoperative year were available for a given patient profile, only the earliest observation in that interval was retained. We fitted two models, one treating the registries as a set of fixed effects and another treating the registries as random effects. Although the random-effects model offers some inferential advantage for combining studies28,29, the estimates of the differences among registries in this model can be quite inaccurate with limited observational data per registry. Furthermore, the absence of randomization according to bearing surface and head size could lead to confounding resulting from registry-level effects; such confounding is addressed by the fixed-effects model but not by the random-effects model30,31. Therefore, we gave preference to interpretation of the fixed-effects model, particularly if the parameter estimates differed substantially between the fixed and random-effects models30,31. The results of the fixed-effects models are presented in Table I, and the results of the random-effects model are presented in Table III in the Appendix. SAS version 9.2 was used for all analyses. Additional information regarding the fitting of the models is given in the Appendix.
TABLE I.
Results of the Fixed-Registry-Effects Analysis Comparing C-C and M-HXLPE Implants
| Hazard Ratio (95% CI)* |
||
| >28-mm C-C, Relative to All M-HXLPE† | ≤28-mm C-C, Relative to All M-HXLPE‡ | |
| Time in yr | ||
| 0 to 1 | Ref. | Ref. |
| 1 to 2 | 6.72 (5.07-8.92) | 5.74 (4.20-7.80) |
| 2 to 3 | 8.24 (6.16-11.01) | 7.00 (5.11-9.59) |
| 3 to 4 | 9.88 (7.37-13.24) | 7.98 (5.82-10.95) |
| 4 to 5 | 10.84 (8.08-14.55) | 8.80 (6.40-12.08) |
| 5 to 6 | 12.11 (9.00-16.30) | 9.73 (7.07-13.40) |
| 6 to 7 | 13.04 (9.64-17.63) | 10.41 (7.54-14.36) |
| 7 to 8 | 15.19 (11.12-20.75) | 12.08 (8.67-16.83) |
| 8 to 9 | 15.84 (11.29-22.21) | 12.52 (8.65-18.11) |
| 9 to 10 | NA | 14.09 (9.10-21.81) |
| Sex | ||
| Male | Ref. | Ref. |
| Female | 1.09 (0.93-1.28) | 0.98 (0.81-1.19) |
| Age in yr | ||
| 45 to 54 | Ref. | Ref. |
| 55 to 64 | 0.80 (0.66-0.96) | 0.89 (0.71-1.12) |
| Fixed registry effects§ | — | — |
| Bearing surface and size | ||
| Overall | NA | 1.36 (1.09-1.68) |
| 0 to 2 yr# | 0.77 (0.63-0.93) | NA |
| 2 to 6 yr# | 0.88 (0.74-1.05) | NA |
| 6 to 9 yr# | 0.93 (0.77-1.12) | NA |
Results are based on an iterative solution that updates the residual covariances until convergence. Confidence intervals are based on a Z distribution. NA = not applicable.
The estimated intercept was −5.69 (SE, 0.17).
The estimated intercept was −5.51 (SE, 0.19).
Fixed registry effects were included in this model, but the results are omitted from this table because a precondition of data sharing was no reporting of comparisons among registries.
The bearing effects over time are based on a combination of the main and interaction effects from the model.
TABLE III.
Results of the Random-Effects Analysis Comparing C-C and M-HXLPE Implants
| Hazard Ratio (95% CI)* |
||
| >28-mm C-C, Relative to All M-HXLPE† | ≤28-mm C-C, Relative to All M-HXLPE‡ | |
| Time in yr | ||
| 0 to 1 | Ref. | Ref. |
| 1 to 2 | 6.59 (4.98-8.71) | 5.94 (4.35-8.11) |
| 2 to 3 | 8.09 (6.08-10.76) | 7.27 (5.31-9.95) |
| 3 to 4 | 9.66 (7.25-12.88) | 8.29 (6.05-11.37) |
| 4 to 5 | 10.59 (7.94-14.13) | 9.15 (6.67-12.56) |
| 5 to 6 | 11.82 (8.84-15.80) | 10.14 (7.37-13.94) |
| 6 to 7 | 12.74 (9.49-17.11) | 10.85 (7.88-14.96) |
| 7 to 8 | 14.82 (10.93-20.09) | 12.63 (9.08-17.56) |
| 8 to 9 | 15.45 (11.10-21.52) | 13.11 (9.07-18.94) |
| 9 to 10 | NA | 14.74 (9.52-22.82) |
| Sex | ||
| Male | Ref. | Ref. |
| Female | 1.08 (0.93-1.27) | 0.97 (0.80-1.18) |
| Age in yr | ||
| 45 to 54 | Ref. | Ref. |
| 55 to 64 | 0.81 (0.68-0.97) | 0.87 (0.70-1.10) |
| Bearing surface and size | ||
| Overall | NA | 1.10 (0.43-2.85) |
| 0 to 2 yr§ | 0.80 (0.67-0.96) | NA |
| 2 to 6 yr§ | 0.92 (0.78-1.08) | NA |
| 6 to 9 yr§ | 0.96 (0.81-1.15) | NA |
Results are based on an iterative solution that updates the residual covariances until convergence. Confidence intervals for the C-C >28-mm model are based on a Z distribution. Our simulations indicated that an optimal strategy for CI construction in the presence of random effects was to use tκ − 1 for fixed parameters with corresponding random effects and to use tn − p otherwise (where κ − 1 and n − p indicate the degrees of freedom for the t distribution, κ is the number of registries, n is the number of observations, and p is the number of fixed effects); this is the approach taken in construction of the CIs for the C-C ≤28-mm model. NA = not applicable.
The estimated intercept was −5.69 (SE, 1.17).
The estimated intercept was −5.56 (SE, 0.18), and the bearing surface random effect was 0.08 (SE, 0.12).
The bearing effects over time are based on a combination of the main and interaction effects from the model.
Results
A total of 34,985 total hip arthroplasties were included; 52% were female. The five-year overall rate of revision surgery varies from 1.9% to 3.2% among the registries. Additional descriptive data for the C-C and M-HXLPE bearing groups are presented in Table II.
TABLE II.
Included Implants According to Registry, Bearing Surface, Head Size, Age, and Sex
| Registry*
(no. [%]) |
||||||
| U.S., KP | Australia | Italy, E-R | U.S., HE | Norway | Spain, C | |
| Ceramic-on-ceramic | ||||||
| Head size, >28 mm | ||||||
| Age, 45-54 yr | 109 (38.2) | 3772 (28.9) | 443 (19.8) | 56 (49.6) | 143 (21.6) | 31 (25.2) |
| Age, 55-64 yr | 176 (61.8) | 9278 (71.1) | 1796 (80.2) | 57 (50.4) | 520 (78.4) | 92 (74.8) |
| Male | 142 (49.8) | 6744 (51.7) | 1072 (47.9) | 70 (61.9) | 268 (40.4) | 81 (65.9) |
| Female | 143 (50.2) | 6306 (48.3) | 1167 (52.1) | 43 (38.1) | 395 (59.6) | 42 (34.1) |
| Head size, ≤28 mm | ||||||
| Age, 45-54 yr | 8 (53.3) | 873 (33.1) | 256 (23.2) | 4 (36.4) | 88 (28.9) | 22 (34.9) |
| Age, 55-64 yr | 7 (46.7) | 1768 (66.9) | 849 (76.8) | 7 (63.6) | 217 (71.1) | 41 (65.1) |
| Male | 0 (0) | 838 (31.7) | 463 (41.9) | 0 (0.0) | 95 (31.1) | 27 (42.9) |
| Female | 15 (100) | 1803 (68.3) | 642 (58.1) | 11 (100.0) | 210 (68.9) | 36 (57.1) |
| Metal-on-HXLPE, all head sizes | ||||||
| Age, 45-54 yr | 893 (19.7) | 2030 (23.0) | 33 (11.6) | 94 (26.7) | 38 (22.6) | 51 (25.4) |
| Age, 55-64 yr | 3635 (80.3) | 6808 (77.0) | 252 (88.4) | 258 (73.3) | 130 (77.4) | 150 (74.6) |
| Male | 2018 (44.6) | 4423 (50.0) | 145 (50.9) | 176 (50.0) | 62 (36.9) | 119 (59.2) |
| Female | 2510 (55.4) | 4415 (50.0) | 140 (49.1) | 176 (50.0) | 106 (63.1) | 82 (40.8) |
KP = Kaiser Permanente, E-R = Emilia-Romagna region, HE = HealthEast, and C = Catalan region.
Comparison Between C-C Implants with >28-mm and ≤28-mm Head Sizes
The fixed-effects model treated registry membership as a set of fixed effects and included variables representing head size, the intercept, postoperative year (e.g., the first postoperative year), age, sex, and residual variance fixed at 1. This model indicated a lower risk of C-C implant revision associated with use of larger compared with smaller head size (HR [hazard ratio] = 0.73, 95% CI [confidence interval] = 0.60 to 0.88, p = 0.001). Based on the results of this fixed-effects model, there was sufficient evidence to warrant comparing these C-C bearing groups separately with M-HXLPE bearings.
Comparison Between >28-mm C-C Implants and M-HXLPE Implants with Any Head Size
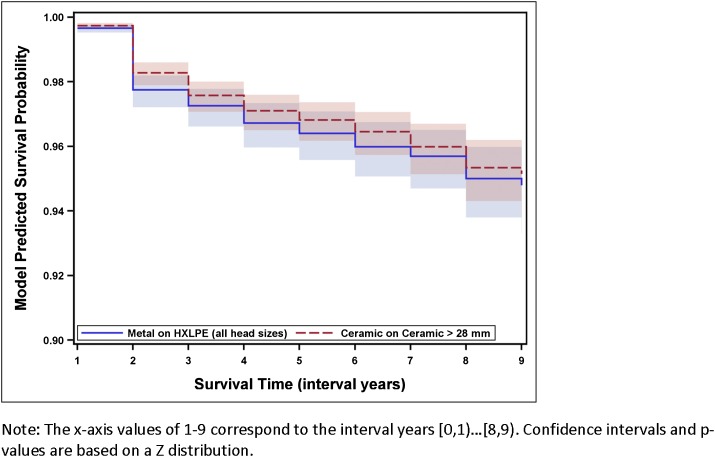
The fixed-effects model fitted for this comparison was similar to the one described above except that the comparison was between two different bearing materials and a time-by-bearing interaction was included. A difference in the revision risk was found but varied over time (Table I and Fig. 1). In years zero to two, use of C-C bearings with a large head size was associated with a protective effect compared with M-HXLPE bearings of any head size (HR = 0.77, 95% CI = 0.63 to 0.93, p = 0.008). However, this protective effect dissipated over time (HR = 0.88, 95% CI = 0.74 to 1.05, p = 0.159 in years two to six; and HR = 0.93, 95% CI = 0.77 to 1.12, p = 0.436 in years six to nine).
Fig. 1.
Predicted survival for CC bearings with a head size of >28 mm compared with M-HXLPE bearings of any head size according to the fixed-effects model. The shaded regions indicate the 95% confidence intervals.
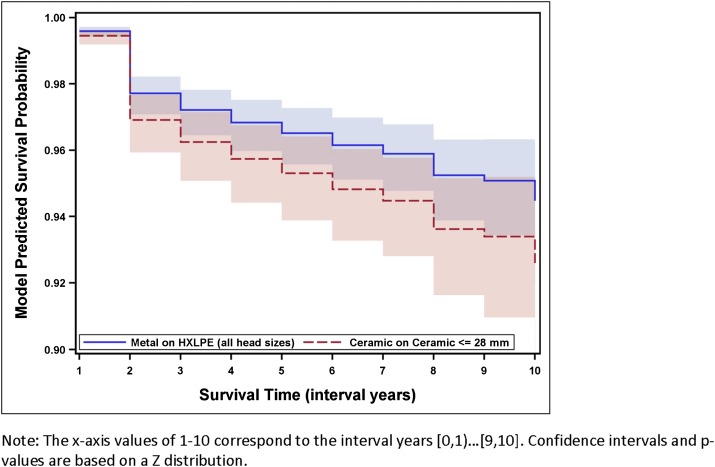
Comparison Between ≤28-mm C-C Implants and M-HXLPE Implants with Any Head Size
The fixed-effects model fitted for this comparison included only a main effect for the bearing surface and revealed that smaller C-C bearings were associated with a higher risk of failure compared with M-HXLPE bearings (HR = 1.36, 95% CI = 1.09 to 1.68, p = 0.006) (Table I and Fig. 2).
Fig. 2.
Predicted survival for CC bearings with a head size of ≤28 mm compared with M-HXLPE bearings of any head size according to the fixed-effects model. The shaded regions indicate the 95% confidence intervals.
Discussion
In this multinational study that included six national and regional registries, we found that use of C-C implants with a smaller (≤28-mm) head size was associated with a 36% higher risk of revision compared with use of M-HXLPE implants. Differences in the risk of revision surgery represent a good measure of comparative device performance, and a higher risk of revision needs to be communicated to patients and considered by clinical, industry, and regulatory stakeholders. Use of C-C implants with a relatively large (>28-mm) head size provided a protective effect in the first two years but thereafter was not significantly different from use of M-HXLPE. This means that the selection of a large-size C-C bearing rather than M-HXLPE would prevent fewer than one in every 500 patients from requiring a revision within two years, and it would result in no difference in later time periods. In addition, the benefit of >28-mm C-C bearings might be even smaller or disappear entirely if the comparison group were restricted to >28-mm M-HXLPE bearings. Although we did not find a significant head size effect within M-HXLPE bearings in our analyses presented elsewhere in this supplement23, the existence of small differences is still possible. The selection of C-C implants might also have cost implications for hospitals and surgeons.
Our study utilized prospectively collected data that currently cover >50% of C-C hip replacements performed worldwide. We focused on an age group of forty-five to sixty-four years and noncemented fixation, as C-C bearings are more likely to be selected in younger patients and are almost exclusively cementless on the acetabular side. Patients younger than forty-five years of age are less likely to have osteoarthritis, and excluding that patient group helps address potential biases related to a higher proportion of alternate diagnoses in the C-C group. However, we believe that there are no anatomic or clinical factors that will limit applicability of our study results to all age groups.
Although improved functional outcome may be a potential justification for the use of C-C bearings, to our knowledge there is no evidence to suggest that the use of such bearings is associated with better function. Several studies with various follow-up durations have compared C-C bearings with C-P bearings15,32-37; most had both baseline and postoperative measurements. In addition, one trial compared C-C with M-P bearings; this had only postoperative measurements11-14. Harris hip scores, both at baseline and at the time of follow-up, were very similar in the two bearing groups in all studies that compared C-C with other bearing surfaces.
Published data related to the revision risk after use of C-C implants are limited. Several small and underpowered comparative studies reported revision information for the C-C cohort as a whole but not according to the head size of the implants. Four studies compared C-C with C-P bearings and found no qualitative or quantitative differences between the groups with respect to revision occurrence38. However, one well-designed study indicated substantially more intraoperative device and wound complications associated with C-C compared with C-P bearings32. The previously mentioned trial comparing C-C with M-P bearings11-15 indicated a substantially lower occurrence of revision in the C-C arms compared with the M-P arm even after ten years of follow-up. The comparison M-P group involved non-cross-linked polyethylene, and the authors did discuss the uncertainty regarding the applicability of their findings to M-HXLPE bearings. In addition, that isolated and relatively small study certainly does not carry considerable weight against the substantial evidence covered in the present study as well as reports from the registries for New Zealand and for England and Wales that also did not find advantages associated with the use of C-C implants. Although we did not include the New Zealand Registry in our meta-analysis because it was not compatible with our harmonized, distributed study design, we did obtain detailed information from that registry, and the data are likely to be aligned with our findings18. The registry for England and Wales also confirmed that smaller-size C-C implants are likely to be inferior to hard-on-soft (M-P and C-P) bearings39. However, data from that registry also do not show any advantage for larger-head-size C-C implants compared with M-P implants39.
Strengths and Limitations
Our study has several important strengths. By combining data from six registries, it represents the largest multinational prospective registry cohort involving a homogeneous population of young patients treated with total hip arthroplasty with noncemented implants and an osteoarthritis diagnosis. We compared C-C with M-HXLPE implants rather than with a mixed control group involving all types of polyethylene. Thus, the study is very generalizable. The maximum follow-up was ten years, and the study represents the most recent practice. We addressed the issues of confidentiality and privacy of the patients by using distributed analyses involving standardized syntax to extract aggregated data from each registry. This approach was therefore exempt from the need for institutional review board approval, and each registry’s legal approval was sufficient.
The limitations of the study include the less flexible statistical analysis permitted by the use of the registry consortium, as any change in the statistical syntax would make a new analysis of each registry necessary. The maximum follow-up was ten years in these series. Longer follow-up duration would allow for more comprehensive assessments. While the average follow-up rate in the registries is >90%, our study was based on a minimal data set, as it was limited by the data elements available from each registry. We did not validate the description of the implants in each group, as harmonization of implant databases across registries has not been completed. Some registries are larger than others. In addition, the limitation of observational data collected by registries might lead to difficulties in interpretation of survivorship findings in the context of premarket application. Therefore, such registry data would not be sufficient to support a marketing application in the U.S. We did not validate the description of the implants in each group, but harmonization of implant databases across registries is underway and few differences in implant classification have been found; consequently, this limitation is unlikely to affect our results. Some registries are larger than others or have more complete follow-up, and these may therefore have had a stronger influence on the results. Because of the large sample size, statistically significant differences were identified, but these were relatively small and readers must therefore also assess their clinical importance.
Conclusions
Our multinational study based on a harmonized, distributed network showed that smaller-head-size C-C implants are likely to have a higher risk of revision compared with both large-size C-C implants and M-HXLPE implants. At two years, noncemented >28-mm C-C implants were associated with a lower revision occurrence compared with M-HXLPE, but this difference was small and disappeared in the long term. The effect of especially large >36-mm C-C implants needs to be studied in the future. The findings of this study warrant careful reflection by regulatory and clinical communities, and they should be widely disseminated to patients for informed decision-making regarding such surgery.
Appendix—Details of the Model Fitting
Data Inclusion
In both types of models, we chose to retain observations with an SE of <0.0125, as our simulations indicated increased bias, increased root-mean-squared error, and poorer coverage when observations with large degrees of imprecision (resulting from sparse data for certain covariate combinations) were retained. This particular threshold was based on both the simulation results and a sensitivity analysis of the effect on the model parameters when various levels of restriction (0.05, 0.025, 0.0125) were applied.
Comparison of >28-mm and ≤28-mm C-C Bearings
Initially, we compared C-C bearings with head sizes of ≤28 and >28 mm. We began with a random-effects model that included head size, intercept, age, sex, time (represented as an integer), intercept and head-size random effects without a covariance (as a model with a covariance term would not converge), and residual variance fixed at 1. We considered the inclusion of a treatment-by-time interaction based on three indicator variables for time intervals of zero to two, two to four, four to six, and six to seven years in order to improve the precision of the estimation compared with the use of one-year intervals, but a likelihood-ratio test (maximum-likelihood estimation) yielded insufficient evidence of an improved fit (χ2[3] = 6.89, p = 0.076). The overall head size effect was nonsignificant, with the point estimate favoring a protective effect of larger head sizes (b = −0.121, SE = 0.209), but there was evidence that the effect varied across registries (σ2head size = 0.068, SE = 0.144), as did the intercept (σ2head size = 0.033, SE = 0.071). Examination of the EBLUPs (empirical best linear unbiased predictors) for the head-size effect indicated that the Australian registry produced the greatest evidence for a protective effect of larger head sizes (−0.23), followed by Norway (0.06), Kaiser Permanente in the U.S. (0.08), and Emilia-Romagna in Italy (0.09).
Comparison of >28-mm C-C and All M-HXLPE Bearings
We began with a random-effects model that included an intercept, bearing surface, age, sex, time (represented as an integer), bearing surface-by-time interaction, random intercept, random treatment effect, and residual variance fixed at 1. Neither a random effect for the intercept nor a random treatment effect was warranted, as these point estimates were near zero (<1.0 × 10−10). The interaction terms were initially based on time intervals of zero to two, two to four, four to six, six to eight, and eight to nine years. A test of the interaction terms was nonsignificant (χ2[4] = 6.76, p = 0.149), but we observed a pattern among the point estimates such that the interaction effects were approximately constant for the intervals of zero to two, two to six, and six to nine years. Refitting a model with these groupings did indicate a significant time-by-bearing condition interaction (χ2[2] = 6.25, p = 0.044). We therefore retained these interaction terms in the model (Table III).
Comparison of ≤28-mm C-C and All M-HXLPE Bearings
We began with a random-effects model that included an intercept, bearing surface, age, sex, time (represented as an integer), bearing surface-by-time interaction, random intercept, random treatment effect, and residual variance fixed at 1. A random effect for the intercept was not warranted, as indicated by a point estimate near zero (<1.0 × 10−10), and was removed. The interaction terms were based on time intervals of zero to two, two to four, four to six, and six to eight years. A test of the interaction terms was nonsignificant (χ2[3] = 0.84, p = 0.84); therefore, these terms were removed. The iterated model indicated that the overall head size effect was nonsignificant, with the point estimate favoring a harmful effect of small-head-size C-C implants (b = 0.097, SE = 0.221). However, there was evidence that the effect varied across registries (σ2head size = 0.080, SE = 0.144). Examination of the EBLUPs indicated that the Australian registry produced the greatest evidence for a harmful effect of small-head-size C-C implants (0.23), followed by Norway (−0.07) and Emilia-Romagna in Italy (−0.16).
Fixed-Effects Models
Each fixed-effects model was based on the random-effects model selected.
Acknowledgments
Note: The authors acknowledge Abby Isaacs, Rebecca Love, and Lucas Romero for superb analytic and organizational support. They also acknowledge Danica Marinac-Dabic, MD, PhD, for leadership and substantial contributions to the success of ICOR.
Footnotes
Disclosure: One or more of the authors received payments or services, either directly or indirectly (i.e., via his or her institution), from a third party in support of an aspect of this work. None of the authors, or their institution(s), have had any financial relationship, in the thirty-six months prior to submission of this work, with any entity in the biomedical arena that could be perceived to influence or have the potential to influence what is written in this work. In addition, no author has had any other relationships, or has engaged in any other activities, that could be perceived to influence or have the potential to influence what is written in this work. The complete Disclosures of Potential Conflicts of Interest submitted by authors are always provided with the online version of the article.
References
- 1.Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007April;89(4):780-5. [DOI] [PubMed] [Google Scholar]
- 2.Delaunay C, Hamadouche M, Girard J, Duhamel A; SoFCOT Group. What are the causes for failures of primary hip arthroplasties in France? Clin Orthop Relat Res. 2013December;471(12):3863-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Grupp TM, Weik T, Bloemer W, Knaebel HP. Modular titanium alloy neck adapter failures in hip replacement—failure mode analysis and influence of implant material. BMC Musculoskelet Disord. 2010;11:3 Epub 2010 Jan 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Werner BC, Brown TE. Instability after total hip arthroplasty. World J Orthop. 2012August18;3(8):122-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hooper GJ, Rothwell AG, Stringer M, Frampton C. Revision following cemented and uncemented primary total hip replacement: a seven-year analysis from the New Zealand Joint Registry. J Bone Joint Surg Br. 2009April;91(4):451-8. [DOI] [PubMed] [Google Scholar]
- 6.Jameson SS, Lees D, James P, Serrano-Pedraza I, Partington PF, Muller SD, Meek RM, Reed MR. Lower rates of dislocation with increased femoral head size after primary total hip replacement: a five-year analysis of NHS patients in England. J Bone Joint Surg Br. 2011July;93(7):876-80. [DOI] [PubMed] [Google Scholar]
- 7.Pedersen AB, Svendsson JE, Johnsen SP, Riis A, Overgaard S. Risk factors for revision due to infection after primary total hip arthroplasty. A population-based study of 80,756 primary procedures in the Danish Hip Arthroplasty Registry. Acta Orthop. 2010October;81(5):542-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mullins MM, Norbury W, Dowell JK, Heywood-Waddington M. Thirty-year results of a prospective study of Charnley total hip arthroplasty by the posterior approach. J Arthroplasty. 2007September;22(6):833-9. [DOI] [PubMed] [Google Scholar]
- 9.Ulrich SD, Seyler TM, Bennett D, Delanois RE, Saleh KJ, Thongtrangan I, Kuskowski M, Cheng EY, Sharkey PF, Parvizi J, Stiehl JB, Mont MA. Total hip arthroplasties: what are the reasons for revision? Int Orthop. 2008October;32(5):597-604 Epub 2007 Apr 19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Graves SE, Rothwell A, Tucker K, Jacobs JJ, Sedrakyan A. A multinational assessment of metal-on-metal bearings in hip replacement. J Bone Joint Surg Am. 2011December21;93(Suppl 3):43-7. [DOI] [PubMed] [Google Scholar]
- 11.Capello WN, Dantonio JA, Feinberg JR, Manley MT. Alternative bearing surfaces: alumina ceramic bearings for total hip arthroplasty. Instr Course Lect. 2005;54:171-6. [PubMed] [Google Scholar]
- 12.Capello WN, D’Antonio JA, Feinberg JR, Manley MT, Naughton M. Ceramic-on-ceramic total hip arthroplasty: update. J Arthroplasty. 2008October;23(7)(Suppl):39-43. [DOI] [PubMed] [Google Scholar]
- 13.D’Antonio J, Capello W, Manley M, Naughton M, Sutton K. Alumina ceramic bearings for total hip arthroplasty: five-year results of a prospective randomized study. Clin Orthop Relat Res. 2005July;436:164-71. [PubMed] [Google Scholar]
- 14.D’Antonio JA, Capello WN, Manley MT, Naughton M, Sutton K. A titanium-encased alumina ceramic bearing for total hip arthroplasty: 3- to 5-year results. Clin Orthop Relat Res. 2005December;441:151-8. [DOI] [PubMed] [Google Scholar]
- 15.D’Antonio JA, Capello WN, Naughton M. Ceramic bearings for total hip arthroplasty have high survivorship at 10 years. Clin Orthop Relat Res. 2012February;470(2):373-81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Traina F, De Fine M, Di Martino A, Faldini C. Fracture of ceramic bearing surfaces following total hip replacement: a systematic review. Biomed Res Int. 2013;2013:157247 Epub 2013 Jun 13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Traina F, De Fine M, Bordini B, Toni A. Risk factors for ceramic liner fracture after total hip arthroplasty. Hip Int. 2012Nov-Dec;22(6):607-14. [DOI] [PubMed] [Google Scholar]
- 18.New Zealand National Registry. Canterbury District Health Board. http://www.cdhb.govt.nz/njr/. Accessed 2010 Oct 14.
- 19.Sedrakyan A, Paxton EW, Phillips C, Namba R, Funahashi T, Barber T, Sculco T, Padgett D, Wright T, Marinac-Dabic D. The International Consortium of Orthopaedic Registries: overview and summary. J Bone Joint Surg Am. 2011December21;93(Suppl 3):1-12. [DOI] [PubMed] [Google Scholar]
- 20.Brown JS, Holmes JH, Shah K, Hall K, Lazarus R, Platt R. Distributed health data networks: a practical and preferred approach to multi-institutional evaluations of comparative effectiveness, safety, and quality of care. Med Care. 2010June;48(6)(Suppl):S45-51. [DOI] [PubMed] [Google Scholar]
- 21.Sedrakyan A, Paxton EW, Marinac-Dabic D. Stages and tools for multinational collaboration: the perspective from the coordinating center of the International Consortium of Orthopaedic Registries (ICOR). J Bone Joint Surg Am. 2011December21;93(Suppl 3):76-80. [DOI] [PubMed] [Google Scholar]
- 22.Maro JC, Platt R, Holmes JH, Strom BL, Hennessy S, Lazarus R, Brown JS. Design of a national distributed health data network. Ann Intern Med. 2009September1;151(5):341-4 Epub 2009 Jul 28. [DOI] [PubMed] [Google Scholar]
- 23.Allepuz A, Havelin L, Barber T, Sedrakyan A, Graves S, Bordini B, Hoeffel D, Cafri G, Paxton E. Evaluation of femoral head size on metal-on-HXLPE hip arthroplasty outcome in a combined analysis of six national and regional registries. J Bone Joint Surg Am. 2014December17;96(Suppl 1):12-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Arends LR, Hunink MG, Stijnen T. Meta-analysis of summary survival curve data. Stat Med. 2008September30;27(22):4381-96. [DOI] [PubMed] [Google Scholar]
- 25.Dear KB. Iterative generalized least squares for meta-analysis of survival data at multiple times. Biometrics. 1994December;50(4):989-1002. [PubMed] [Google Scholar]
- 26.Kutner MH, Nachtsheim C, Neter J, Li W. Applied linear statistical models. 5th ed.Boston: McGraw-Hill Irwin; 2005. [Google Scholar]
- 27.Kalaian HA, Raudenbush SW. A multivariate mixed linear model for meta-analysis. Psychol Methods. 1996;1(3):227-35. [Google Scholar]
- 28.DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986September;7(3):177-88. [DOI] [PubMed] [Google Scholar]
- 29.Hedges LV, Vevea JL. Fixed- and random-effects models in meta-analysis. Psychol Methods. 1998December;3(4):486-504. [Google Scholar]
- 30.Localio AR, Berlin JA, Ten Have TR, Kimmel SE. Adjustments for center in multicenter studies: an overview. Ann Intern Med. 2001July17;135(2):112-23. [DOI] [PubMed] [Google Scholar]
- 31.Allison PD. Fixed effects regression models (quantitative application in the social sciences). Thousand Oaks, CA: Sage; 2009. [Google Scholar]
- 32.Hamilton WG, McAuley JP, Dennis DA, Murphy JA, Blumenfeld TJ, Politi J. THA with Delta ceramic on ceramic: results of a multicenter investigational device exemption trial. Clin Orthop Relat Res. 2010February;468(2):358-66 Epub 2009 Sep 19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Poggie RA, Turgeon TR, Coutts RD. Failure analysis of a ceramic bearing acetabular component. J Bone Joint Surg Am. 2007February;89(2):367-75. [DOI] [PubMed] [Google Scholar]
- 34.Lombardi AV Jr, Berend KR, Seng BE, Clarke IC, Adams JB. Delta ceramic-on-alumina ceramic articulation in primary THA: prospective, randomized FDA-IDE study and retrieval analysis. Clin Orthop Relat Res. 2010February;468(2):367-74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kim YH, Kim JS, Choi YW, Kwon OR. Intermediate results of simultaneous alumina-on-alumina bearing and alumina-on-highly cross-linked polyethylene bearing total hip arthroplasties. J Arthroplasty. 2009September;24(6):885-91 Epub 2008 Jul 9. [DOI] [PubMed] [Google Scholar]
- 36.Ochs U, Ilchmann T, Ochs BG, Marx J, Brunnhuber K, Lüem M, Weise K. EBRA migration patterns of the Plasmacup with ceramic or polyethylene inserts: a randomised study. Z Orthop Unfall. 2007Sep-Oct;145(Suppl 1):S20-4. [DOI] [PubMed] [Google Scholar]
- 37.Bascarevic Z, Vukasinovic Z, Slavkovic N, Dulic B, Trajkovic G, Bascarevic V, Timotijevic S. Alumina-on-alumina ceramic versus metal-on-highly cross-linked polyethylene bearings in total hip arthroplasty: a comparative study. Int Orthop. 2010December;34(8):1129-35 Epub 2009 Nov 01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sedrakyan A, Normand SL, Dabic S, Jacobs S, Graves S, Marinac-Dabic D. Comparative assessment of implantable hip devices with different bearing surfaces: systematic appraisal of evidence. BMJ. 2011;343(29):d7434 Epub 2011 Nov 29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Smith AJ, Dieppe P, Vernon K, Porter M, Blom AW; National Joint Registry of England and Wales. Failure rates of stemmed metal-on-metal hip replacements: analysis of data from the National Joint Registry of England and Wales. Lancet. 2012March31;379(9822):1199-204 Epub 2012 Mar 13. [DOI] [PubMed] [Google Scholar]