Abstract
Housing for people living with HIV/AIDS has been linked to a number of positive physical and mental health outcomes, in addition to decreased sexual and drug-related risk behavior. The current study identified service priorities for people living with HIV/AIDS, services provided by HIV/AIDS housing agencies, and unmet service needs for people living with HIV/AIDS through a nationwide telephone survey of HIV/AIDS housing agencies in the United States. Housing, alcohol/drug treatment, and mental health services were identified as the three highest priorities for people living with HIV/AIDS and assistance finding employment, dental care, vocational assistance, and mental health services were the top needs not being met. Differences by geographical region were also examined. Findings indicate that while housing affords people living with HIV/AIDS access to services, there are still areas (e.g., mental health services) where gaps in linkages to care exist.
In the United States, 3.4-10.5% of the estimated 640,000 homeless are living with HIV/AIDS, with rates of HIV/AIDS higher in certain subsamples (e.g., men who have sex with men; National Alliance to End Homelessness, 2006/2012; National Coalition for the Homeless, 2009; Robertson et al., 2004). The rate of homelessness among people living with HIV/AIDS (PLWHA) is at least three times that of the general population (National Alliance to End Homelessness, 2006). Furthermore, about 50% of PLWHA are at risk for homelessness, which may be, in part, due to the financial costs of healthcare or unemployment due to HIV status (National Alliance to End Homelessness, 2006). Housing for PLWHA has been linked to better physical and mental health outcomes and proper use of health and social services (e.g., Kidder, Wolitski, Campsmith, & Nakamura, 2007a). To that end, current paper reports the results of a telephone-based nationwide survey of organizations that provide housing for PLWHA. The main foci of the current study were to identify: (a) service priorities for PLWHA, (b) services offered by HIV/AIDS housing organizations, (c) the percentage of residents who can access services not provided in-house by organizations, and (d) the percentage of agencies that report unmet service needs.
Homelessness has been related to a number of HIV risk behaviors in both HIV-negative (HIV-) and HIV-positive (HIV+) individuals. HIV- homeless individuals, compared to those who are housed, are more likely to have unprotected sex with a causal partner, share needles, and to have never used a sterile needle (Salazar et al., 2007). In addition, individuals who are unstably housed are more likely to contract HIV than those who are stably housed (Boileau, Bruneau, Al-Nachawati, Lamothe, & Vincelette, 2005). Centers for Disease Control and Prevention (CDC) surveillance data has shown that homeless PLWHA are more likely to have engaged in exchange sex, have a higher number of sex partners, and have unprotected sex with a HIV- or status unknown partner, compared to housed PLWHA (Kidder, Wolitski, Pals, & Campsmith, 2008). Homeless PLWHA were also more likely to screen positive for possible alcohol abuse, use illicit drugs, and inject drugs (Kidder et al., 2008), including injecting heroin daily (Palepu, Milloy, Kerr, Zhang, & Wood, 2011).
Homelessness is not only related to HIV risk behavior in PLWHA, but various health outcomes as well. Homeless PLWHA have higher rates of hepatitis, tuberculosis, and pneumocystis carinii pneumonia (Kidder et al., 2007a), diseases that are often comorbid with HIV/AIDS. Conversely, PLWHA who have stable housing report better physical health (Stewart, Cianfrini, & Walker, 2005) in addition to better mental health (Kidder et al., 2007a). Studies have found that homeless PLWHA are less likely to have ever taken, or to be currently taking, antiretrovirals (Kidder et al., 2007a; Leaver, Bargh, Dunn, & Hwang, 2007). Homeless PLWHA also report poorer adherence to antiretroviral therapy (Palepu et al., 2011) and poorer immune functioning (Kidder et al., 2007a). Finally, homeless PLWHA experience higher rates of mortality compared to housed counterparts (McMahon, Wanke, Terrin, Skinner, & Knox, 2011; Walley et al., 2008).
Two randomized controlled trials have examined the benefits of housing for PLWHA. Compared to PLWHA receiving only standard care (e.g., referrals to shelters, temporary housing assistance), those receiving permanent housing (Buchanan et al., 2009) or long-term rental assistance (Kidder et al., 2007b; Wolitski et al., 2010) were more likely to be housed and alive one year later, and have better immune functioning and mental health. Those receiving housing were marginally more likely to receive appropriate medical care, be on highly active antiretroviral therapy, and have fewer sexual partners and were marginally less likely to exchange sex and have sex with a HIV- or status unknown partner. The cost of the intervention, per participant, ranged from $10,048-$14,032 (Holtgrave et al., 2007). Given that the average PLWHA incurs $221,365 in treatment costs alone, this intervention is estimated to be cost effective if one out of every 64 participants is prevented from transmitting HIV to a seronegative individual (Holtgrave et al., 2007).
Housing not only increases engagement in recommended HIV health care (Aidala, Lee, Abramson, Messeri, & Siegler, 2007; Rumptz et al., 2007), housing increases the utilization of other health and social services. Housed PLWHA are more likely to receive myriad services, including case management, health care, transportation, food assistance, and HIV education and risk reduction information compared to PLWHA who are homeless (Kidder et al., 2007a). However, 35-83% of PLWHA report at least one need not being met (Pereyra et al., 2011; Wohl et al., 2011), with housing, health care (primary, dental, and mental), drug/alcohol treatment, and financial assistance being the most frequently unmet needs (Pereyra et al., 2011; Reif et al., 2011; Wohl et al., 2011; Young et al., 2005). PLWHA who have unmet service needs are more likely to be homeless (Leaver et al., 2007; Pereyra et al., 2011; Wohl et al., 2011). Furthermore, those with unmet needs were less likely to have satisfactory medical care (Young et al., 2005), to take antiretroviral therapy, and to be adherent to antiretroviral therapy (Reif et al., 2011).
The current study expands upon past research by conducting a nationwide survey of HIV housing organizations in an effort to capture the full picture of services offered and needed in relation to housing for PLWHA. Past research has found regional differences in rates of HIV/AIDS and outcomes for PLWHA, and we conjecture that these differences may at least in part be related to differences in services offered or needed. For example, PLWHA in the South are less likely to be on antiretrovirals (Meditz et al., 2011), and have the highest rate of mortality compared to PLWHA in other regions of the United States (Hanna, Selik, Tang, & Gange, 2012). The South also has the highest rate of AIDS diagnoses since the beginning of the epidemic, while current statistics suggest that the rate of AIDS diagnoses is increasing the fastest in the Midwest (CDC, 2012). These trends led us to undertake a regional approach to our analysis.
Method
Housing Agency Identification & Interview Procedure
To be eligible to participate, agencies must have been directly providing housing (e.g., apartment building, single occupancy hotel) for PLWHA at the time of the interview and been able to provide information pertaining only to residents with HIV/AIDS. Agencies that only provided indirect housing assistance (e.g., housing vouchers, rental assistance) were not eligible to participate. Agencies were identified using three HIV/AIDS housing/social services databases: (1) Housing Opportunities for Persons with AIDS (HOPWA; 2011) programs, grantees, and reports, (2) the CDC's (2011) National Prevention Information Network organization search, and (3) The Body's (2011) list of HIV/AIDS organization. Agencies that were identified as potentially providing housing for PLWHA were emailed an invitation to participate in the interview. Follow-up emails were sent two weeks later to agencies that did not respond. Agencies that indicated they were eligible to participate were scheduled to complete the interview at a later date. Agencies that did not respond to the second email were called and scheduled for an interview if eligible and willing to participate. From the 275 agencies contacted, 89 agencies, representing 32 different states, completed the interview. Agencies were grouped according to the four regions outlined by the CDC (2012; Northeast, South, Midwest, West). For a breakdown of participating agencies by region and state see Table 1.
Table 1.
Participating agencies by region and state.
| Region/State | Number of Agencies | Region/State | Number of Agencies |
|---|---|---|---|
| Northeast | 24 | Midwest | 11 |
| Connecticut | 6 | Illinois | 4 |
| Massachusetts | 4 | Indiana | 1 |
| New Jersey | 3 | Michigan | 1 |
| New York | 11 | Minnesota | 1 |
| South | 35 | Missouri | 1 |
| Alabama | 1 | Ohio | 2 |
| District of Columbia | 4 | Wisconsin | 1 |
| Delaware | 2 | West | 19 |
| Florida | 5 | Alaska | 1 |
| Georgia | 3 | Arizona | 2 |
| Louisiana | 2 | California | 6 |
| Maryland | 2 | Colorado | 1 |
| Mississippi | 1 | Hawaii | 1 |
| North Carolina | 3 | Nevada | 2 |
| Tennessee | 2 | Oregon | 3 |
| Texas | 5 | Washington | 3 |
| Virginia | 2 | ||
| West Virginia | 3 |
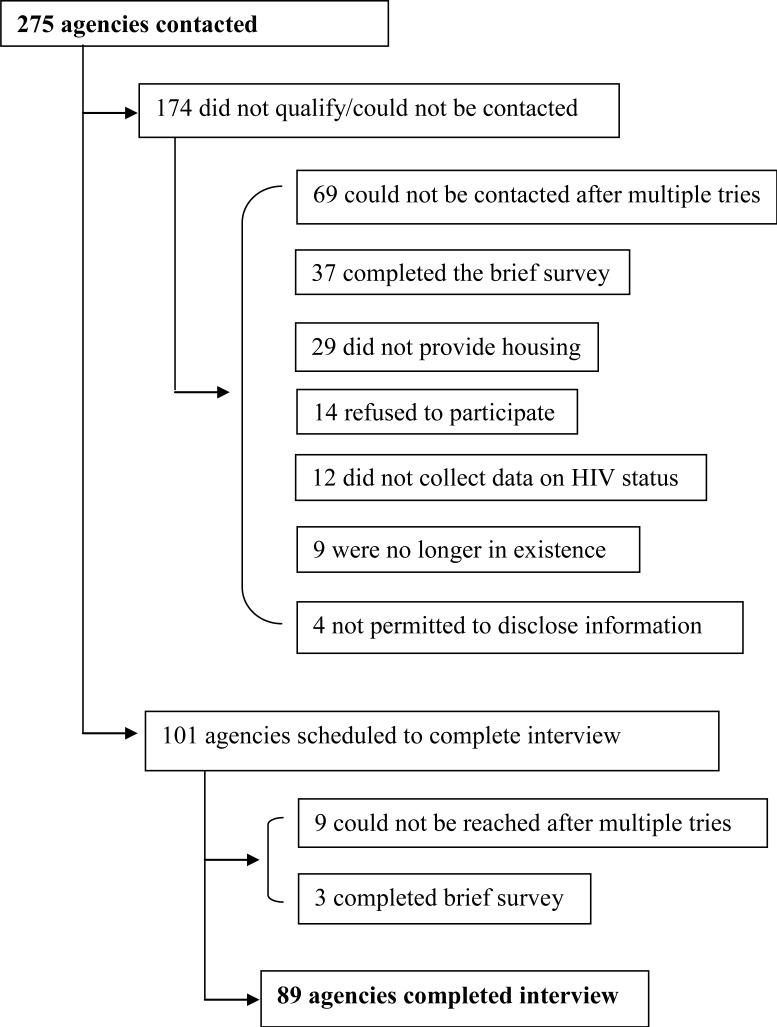
The interviews were conducted between April and August 2011 and took 60-90 minutes to complete. One of eight interviewers called the agency at the scheduled time and completed the interview. Representatives from the agencies who completed the interview were those most knowledgeable about the agency's housing program (e.g., executive director/CEO [21.3%], case manager/program coordinator [68.5%], direct service staff [5.6%]). Interviews, on average, were completed within three weeks of eligibility screening. Agencies that completed the survey were sent a $75 gift card to a national office supply chain store. Agencies that did not qualify for the study participated in a brief survey that asked the respondent to rank service priorities for PLWHA (see description of measure below). As this paper focuses on service housing agencies provided, these responses were not included in the present analyses. See Figure 1 for a flowchart of agency selection.
Figure 1.
Flow chart of HIV/AIDS housing agencies selected for interview.
Measures
The interview covered several areas of the agency's functioning as well as the demographic composition of residents and staff; only areas relevant to the present analyses are described below. Areas assessed in the interview but not described below include sources of funding, changes in the funding environment, policies and procedures (e.g., curfew, drug testing), facility characteristics (e.g., type of housing), and resident and staff member characteristics (e.g., sex, race). No information that could identify individual residents was collected.
General agency information
Agencies were asked the number of staff, residents, residents required for funding, and individuals on the wait-list for housing.
Services priorities for PLWHA
Agencies were asked whether various needs (e.g., housing, health care, employment) were a low, moderate, or high (scale of 0-2) priority for PLWHA in their community.
Service provision, access, and needs for PLWHA
Agencies were asked if they provided various services (e.g., primary health care, alcohol counseling, transportation) in-house to residents (Yes/No), if resident had access to the service (Yes/No), and if the need for that service was being met (Yes/No). Finally, organizations were asked if they offered medication adherence assistance to their residents (Yes/No).
Analyses
Agency characteristics by region were examined using one-way ANOVA. Due to positive skew and large standard deviations, agency variables were transformed using log10 transformation in order to provide more reliable estimates of the F-statistic (Tabachnick & Fidell, 2007). Means and standard deviations for the untransformed variables and transformed F-statistic results are presented in Table 2. To analyze service priorities by region, one-way ANOVAs were conducted (Table 3). Percent of agencies that offer services in-house, percent of residents that can access services, and percent of unmet service needs by region, and countrywide, are presented in Table 4; chi-square was used to examine if agency responses differed by region on any of these variables.
Table 2.
General characteristics of participating agencies.
| Overall | Northeast | South | Midwest | West | Result | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| M | SD | M | SD | M | SD | M | SD | M | SD | ||
| # of Direct Service Staff | 57.07 | 129.34 | 90.78* | 177.38 | 40.82* | 93.67 | 10.00* | 5.68 | 73.44 | 148.64 | F(3, 82) = 4.037, p = .010 |
| Capacity (# of possible residents) | 124.33 | 217.60 | 184.60 | 258.68 | 126.03 | 234.87 | 29.27 | 21.95 | 112.50 | 193.26 | F(3, 76) = 1.713, p = .171 |
| # of Current Residents | 109.56 | 205.12 | 135.13 | 236.79 | 104.41 | 203.56 | 25.18 | 21.26 | 136.68 | 224.20 | F(3, 83) = 1.242, p = .300 |
| # of Resident Required for Funding | 23.81 | 87.01 | 30.25 | 43.44 | 8.43 | 32.33 | 12.89 | 31.13 | 58.54 | 178.23 | F(3, 58) = 1.844, p = .149 |
| # of People on Wait List | 25.34 | 67.06 | 28.00 | 81.88 | 23.89 | 58.33 | 4.40 | 4.86 | 37.24 | 83.22 | F(3, 69) = 1.876, p = .142 |
significant difference between groups.
Note: F-values represent logio transformed values, M and SD represent raw values.
Table 3.
Service priorities for people living with HIV/AIDS by region, organized from highest to lowest overall priority.
| Service | Overall | Northeast | South | Midwest | West | F-test | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| M | SD | Rank | M | SD | Rank | M | SD | Rank | M | SD | Rank | M | SD | ||
| Housing | 1.85 | 0.41 | 1 | 1.92 | 0.41 | 1 | 1.86 | 0.36 | 1 | 1.64 | 0.51 | 1 | 1.89 | 0.46 | F(3, 85) = .13, p = .29 |
| Alcohol/Drug Treatment | 1.65 | 0.59 | 2 | 1.67 | 0.57 | 2 | 1.69 | 0.58 | 1 | 1.64 | 0.51 | 4 | 1.58 | 0.69 | F(3, 85) = 0.14, p = .94 |
| Mental Health Care | 1.56 | 0.66 | 3 | 1.58 | 0.65 | 5 | 1.51 | 0.70 | 3 | 1.45 | 0.69 | 3 | 1.68 | 0.58 | F(3, 85) = 0.38, p = .77 |
| Health Care | 1.53 | 0.68 | 3 | 1.58+ | 0.50 | 3 | 1.56+ | 0.66 | 6 | 1.00*+ | 1.00 | 2 | 1.74* | 0.56 | F(3, 84) = 3.12, p = .03 |
| Accessing HIV Treatments | 1.48 | 0.69 | 5 | 1.54 | 0.51 | 4 | 1.53 | 0.71 | 5 | 1.09 | 0.83 | 5 | 1.53 | 0.77 | F(3, 84) = 1.31, p = .28 |
| Social Support | 1.33 | 0.69 | 6 | 1.42 | 0.78 | 7 | 1.31 | 0.68 | 7 | 0.91 | 0.70 | 6 | 1.47 | 0.51 | F(3, 85) = 1.84, p = .15 |
| Accessing Food | 1.26 | 0.69 | 7 | 1.22 | 0.74 | 8 | 1.29 | 0.72 | 7 | 0.91 | 0.53 | 6 | 1.47 | 0.61 | F(3, 83) = 1.65, p = .18 |
| Employment | 1.17 | 0.72 | 8 | 1.04 | 0.71 | 6 | 1.44* | 0.71 | 4 | 1.18* | 0.60 | 8 | 0.84 | 0.69 | F(3, 83) = 3.44, p = .02 |
| Child Care | 0.78 | 0.79 | 10 | 0.75 | 0.74 | 10 | 0.80 | 0.83 | 7 | 0.91 | 0.83 | 9 | 0.72 | 0.83 | F(3, 84) = 0.14, p = .93 |
| Legal Aide | 0.77 | 0.61 | 9 | 0.88* | 0.61 | 8 | 0.91* | 0.59 | 10 | 0.82 | 0.60 | 10 | 0.37* | 0.50 | F(3, 82) = 3.94, p = .01 |
significant difference (p < .05)
marginal difference (p < .10)
Table 4.
Service provision, access, and need for PLWHA by region and across the United States.
| Primary Care | Dental Care | Eye Care | Mental Health Services | Alcohol Counseling | AA Meetings | Drug Counseling | NA Meetings | Support Groups | Religious/Spiritual Services | ||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Northeast | Offered in-house | 8.30 | 0.00 | 0.00 | 58.30 | 66.70 | 50.00 | 70.80 | 33.30 | 83.30 | 30.40 |
| Residents can access | 100.00 | 95.70 | 100.00 | 100.00 | 95.80 | 100.00 | 95.80 | 100.00 | 95.70 | 100.00 | |
| Need not being met | 4.30 | 26.10 | 9.10 | 30.40 | 16.70 | 4.20 | 8.30 | 4.20 | 8.70 | 9.10 | |
| South | Offered in-house | 20.00 | 2.90 | 2.90 | 40.00 | 42.90 | 31.40 | 47.10 | 28.60 | 73.50 | 25.70 |
| Residents can access | 100.00 | 97.10 | 94.30 | 100.00 | 97.10 | 97.10 | 97.10 | 97.10 | 91.20 | 100.00 | |
| Need not being met | 2.90 | 44.10 | 29.40 | 34.30 | 20.60 | 2.90 | 24.20 | 5.70 | 14.70 | 3.30 | |
| Midwest | Offered in-house | 0.00 | 0.00 | 0.00 | 36.40 | 54.50 | 27.30 | 54.50 | 27.30 | 63.60 | 18.20 |
| Residents can access | 90.90 | 100.00 | 90.90 | 94.40 | 100.00 | 100.00 | 100.00 | 100.00 | 100.00 | 100.00 | |
| Need not being met | 9.10 | 36.40 | 36.40 | 27.30 | 31.60 | 0.00 | 18.20 | 0.00 | 10.00 | 0.00 | |
| West | Offered in-house | 21.10 | 21.10 | 10.50 | 52.60 | 47.40 | 5.30 | 42.10 | 5.30 | 52.60 | 10.50 |
| Residents can access | 97.80 | 88.20 | 87.50 | 97.70 | 100.00 | 100.00 | 100.00 | 100.00 | 94.40 | 100.00 | |
| Need not being met | 8.00 | 63.20 | 46.70 | 44.40 | 22.70 | 0.00 | 21.10 | 5.30 | 22.20 | 6.30 | |
| Total | Offered in-house | 14.60 | 5.60 | 3.40 | 47.20 | 51.70 | 30.30 | 53.40 | 24.70 | 70.50 | 22.70 |
| Residents can access | 97.80 | 95.30 | 94.20 | 97.70 | 97.70 | 98.90 | 97.70 | 98.90 | 94.20 | 100.00 | |
| Need not being met | 8.00 | 42.50 | 28.00 | 34.50 | 22.70 | 2.20 | 18.40 | 4.50 | 14.10 | 5.10 |
| Region | DEBIs | Legal Services | Transportation | Vocational Assistance | Assistance Finding Employment | Domestic Violence Interventions | Crisis Counseling | |
|---|---|---|---|---|---|---|---|---|
| Northeast | Offered in-house | 45.80 | 26.10 | 54.20 | 37.50 | 37.50 | 45.80 | 62.50 |
| Residents can access | 72.70 | 100.00 | 100.00 | 95.80 | 87.50 | 100.00 | 95.80 | |
| Need not being met | 31.80 | 13.00 | 12.50 | 29.20 | 37.50 | 8.70 | 8.30 | |
| South | Offered in-house | 48.50 | 11.40 | 74.30 | 25.70 | 40.00 | 26.50 | 51.40 |
| Residents can access | 72.70 | 94.10 | 88.60 | 82.90 | 82.90 | 90.90 | 94.10 | |
| Need not being met | 34.40 | 21.90 | 31.40 | 51.50 | 54.30 | 28.10 | 20.60 | |
| Midwest | Offered in-house | 54.50 | 0.00 | 72.70 | 36.40 | 81.80 | 36.40 | 81.80 |
| Residents can access | 90.00 | 100.00 | 100.00 | 100.00 | 100.00 | 100.00 | 100.00 | |
| Need not being met | 20.00 | 9.10 | 27.30 | 18.20 | 27.30 | 18.20 | 10.00 | |
| West | Offered in-house | 21.10 | 5.30 | 73.70 | 21.10 | 36.80 | 31.60 | 57.90 |
| Residents can access | 73.30 | 100.00 | 100.00 | 100.00 | 100.00 | 89.50 | 94.70 | |
| Need not being met | 40.00 | 27.80 | 22.20 | 36.80 | 47.40 | 33.30 | 21.10 | |
| Total | Offered in-house | 42.50 | 12.50 | 68.50 | 29.20 | 43.80 | 34.10 | 59.60 |
| Residents can access | 75.00 | 97.70 | 95.50 | 92.10 | 89.90 | 94.30 | 95.50 | |
| Need not being met | 32.90 | 19.00 | 23.90 | 37.90 | 44.90 | 22.60 | 16.10 |
Results
Agency Characteristics
Agency characteristics by region can be found in Table 2. On average, agencies employed 57 staff members (Mdn = 14) and housed about 110 residents (Mdn = 25), with an average of 25 individuals (Mdn = 5) on the waiting list for housing. The average capacity for agencies was 124 residents (Mdn = 37), with 24 residents (Mdn = 0, or no minimum number of residents) required to receive funding. The only regional difference was that the Northeast employed a higher number of direct services staff than the Midwest and South.
HIV/AIDS Service Priorities
Overall and regional rankings of service priority can be found in Table 3. Across regions, the five highest service priorities were: (1) housing, (2) alcohol/drug treatment, (3) mental health care, (4) primary health care, and (5) accessing HIV treatments, followed by: (6) social support, (7) accessing food, (8) employment, (9) child care, and (10) legal aide. Some regional differences did emerge. Agencies in the Midwest ranked health care as a lower priority compared to the West, Northeast (marginal), and South (marginal). The Midwest also ranked employment as a lower priority than the South. Finally, the West ranked legal aid as a lower priority than the South and Northeast.
HIV/AIDS Service Provision, Access, and Need
The percent of: (a) agencies providing each service in-house, (b) residents who can access each service, and (c) unmet service needs by region can be found in Table 4. Overall, physical health care services (primary, dental, and eye care), religious services, and legal services were not typically offered in house. Other services, such as mental health services, alcohol and drug related services, support groups, evidenced-based interventions (DEBIs), transportation, vocational/employment assistance, domestic violence intervention, and crisis counseling were more commonly offered-in house. In all cases, almost 100% of residents had access to each of the services.
The highest percent of agencies reporting unmet service needs were in the following areas: assistance finding employment (44.9%), dental care (42.5%), vocational assistance (37.9%), mental health services (34.5%), DEBIs (32.9%), eye care (28.0%), transportation (23.9%), alcohol counseling (22.7%), and domestic violence interventions (22.6%). Service needs were almost completely met in regards to Alcoholics Anonymous (97.8%) and Narcotics Anonymous (95.5%) meetings, religious/spiritual services (94.9%), and primary health care (92.0%).
Some regional differences did emerge. Dental care was more likely to be offered in-house in the West (21.1%), χ2(3) = 11.12, p = .01; the need for eye care was cited as not being met by 46.7% of agencies in the West, χ2(3) = 6.90, p = .08; Alcoholics Anonymous was most likely to be offered in-house in the Northeast (50.0%) and least likely to be offered in the West (5.3%), χ2(3) = 10.10, p = .02. Furthermore, the Northeast (26.1%) was most likely to offer legal services in-house, and in-house legal services were not offered at all in the Midwest, χ2(3) = 6.40, p = .09; residents were less likely to be able to access transportation (88.6%), χ2(3) = 6.35, p = .096 and vocational assistance (82.9%), χ2(3) = 7.17, p = .067 in the South. Assistance finding employment was more likely to be offered in-house in the Midwest (81.8%), χ2(3) = 7.42, p = .06. Finally, 68.5% of agencies monitored medication adherence, with no differences emerging by region, χ2(3) = 2.98, p = .40.
Discussion
The current study aimed to identify service priorities and needs, by region, among a national sample of housing agencies that provide housing for PLWHA. Overall, the top five service priorities identified by agencies were: (1) housing, (2) alcohol/drug treatment, (3) mental health care, (4) primary health care, and (5) accessing HIV treatments. Consistent regional patterns were not identified, suggesting that these priorities may be national priorities. Mental health care, alcohol/drug counseling, support groups, DEBIs, transportation, vocational/employment, domestic violence, and crisis counseling were services most often offered in-house by agencies. Besides mental health care and alcohol/drug counseling, most services offered in-house were not identified as service priorities. Service priorities were services that are not offered in-house by agencies and therefore the extra step of linkage to care is necessary. Finally, the most common unmet service needs among housed PLWHA included employment/vocational assistance, dental care, mental health services, DEBIs, eye care, transportation, alcohol counseling, and domestic violence interventions.
Despite general agreement across regions as to the highest service priorities and unmet service needs, the highest priorities were not the top unmet needs. Top priorities were related to basic life needs (e.g., housing, primary health care) whereas unmet needs were related to rehabilitative services (e.g., employment/vocational assistance) and mental health (e.g., mental health services, alcohol counseling). Despite housing, unmet needs for some services (e.g., 44.9% for employment assistance) were still high and on par with findings from past studies (35-83%; Pereyra et al., 2011; Wohl et al., 2011). Medication adherence was monitored by over two-thirds of the agencies, which may explain why housed populations report better adherence outcomes (e.g., Palepu et al., 2011; Reif et al., 2011). Furthermore, now that basic life needs (e.g., access to primary health care and food) are met, individuals may be able to focus on adhering to medication regimens.
Housing may be a first step in linking PLWHA to medical care. In the present survey, almost 100% of agencies reported that residents have access to primary health care services. Housing does not just provide a roof over the head of residents, but provides linkage to other valuable services such as health care, substance use treatment, support groups, and transportation. However, despite reports that almost all residents had access to all services assessed, some service needs were still not met, suggesting a breakdown in linking residents to services that are available. For example, across regions, 97.70% of agencies report that residents have access to mental health services; however, over one-third of the agencies report mental health services as an unmet need. Future research could examine barriers to care for individuals in housing organizations and factors unique to housing organizations (e.g., being around similar others in a supportive environment) that may be related to better health outcomes for PLWHA in housing organizations.
The present study is the first of its kind, to our knowledge, to present data from a nationwide survey of agencies that provide housing for PLWHA. The survey was extensive in nature, covering several aspects of how the agency functions, and conducting phone interviews allowed for very low levels of missing data. Despite these strengths, the limitations of this study should be noted. Not all states were included in the survey and less than half of potentially eligible agencies completed the interview. To that end, sample size was low in some regions (e.g., N = 11 in the Midwest) limiting power to detect significant differences by region. Reporting bias may also be present. Agencies may not have disclosed the true extent of unmet service needs or may have inflated the percent of residents that have access to services in order to downplay the number of residents not linked to services. Finally, agencies were interviewed, not individual PLWHA; therefore, we are not able to draw conclusions about service priorities or needs of PLWHA, only those cited by the agencies that serve them.
Conclusion
The present study has implications for future research, interventions, and funding allocations. Future research should continue to explore housing provision as an intervention. However, particular attention should be paid to other needs, besides housing, that are being met through these interventions (e.g., medication adherence assistance, primary health care) and which services are most beneficial in increasing positive health outcomes (e.g., raising CD4 cell counts) and decreasing risk behaviors (e.g., unprotected sex). Future research can also explore how to fill unmet services needs, either through integration of these needs into interventions or exploring how to close gaps in linkages to care. Funding for service gaps should not only focus on housing, but on meeting unmet service needs to maximize the benefits of housing provision. By supporting rehabilitative services (e.g., job training), funders can provide the stepping stone necessary for formerly homeless PLWHA to become fully integrated into society.
Acknowledgements
This research was supported by Institutional National Research Service Award T32-MH074387 (PI: Seth C. Kalichman).
References
- Aidala AA, Lee G, Abramson DM, Messeri P, Siegler A. Housing need, housing assistance, and connection to HIV medical care. AIDS & Behavior. 2007;11:S101–S115. doi: 10.1007/s10461-007-9276-x. doi: 10.1007/s10461-007-9276-x. [DOI] [PubMed] [Google Scholar]
- Boileau C, Bruneau J, Al-Nachawati H, Lamothe F, Vincelette J. A prognostic model for HIV seroconversion among injection drug users as a tool for stratification in clinical trials. Epidemiology and Social Science. 2005;39:489–495. doi: 10.1097/01.qai.0000153424.56379.61. doi: 10.1097/01.qai.0000153424.56379.61. [DOI] [PubMed] [Google Scholar]
- Buchanan D, Kee R, Sadowski LS, Garcia D. The health impact of supportive housing for HIV-positive homeless patients: A randomized controlled trial. American Journal of Public Health. 2009;99:S675–S680. doi: 10.2105/AJPH.2008.137810. doi:10.2105/AJPH.2008.137810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention HIV surveillance report, 2010. 2012;22 http://www.cdc.gov/hiv/topics/surveillance/resources/reports/. Accessed 08 May 2012. [Google Scholar]
- Centers for Disease Control and Prevention [10 Feb 2011];National prevention information network organization. 2011 from http://www.cdcnpin.org/scripts/search/OrgSearch.aspx.
- Hanna DB, Selik RM, Tang T, Gange SJ. Disparities among US states in HIV-related mortality in persons with HIV infection, 2001-2007. AIDS. 2012;26:95–103. doi: 10.1097/QAD.0b013e32834dcf87. doi: 10.1097/QAD.0b013e32834dcf87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holtgrave DR, Briddell K, Little E, Bendixen AR, Hooper M, Kidder DP, Wolitski RJ, Harre D, Royal S, Aidala A. Cost and threshold analysis of housing as an HIV prevention intervention. AIDS & Behavior. 2007;11:S162–S166. doi: 10.1007/s10461-007-9274-z. doi: 10.1007/s10461-007-9274-z. [DOI] [PubMed] [Google Scholar]
- Housing Opportunities for Persons with AIDS [10 Feb 2011];Programs, grantees, and reports. 2011 from http://www.hudhre.info/hopwa/index.cfm?do=viewHopwaGrantee.
- Kidder DP, Wolitski RJ, Campsmith ML, Nakamura GV. Health status, health care use, medication adherence among homeless and housed people living with HIV/AIDS. American Journal of Public Health. 2007a;91:2238–2245. doi: 10.2105/AJPH.2006.090209. doi: 10.2105/AJPH.2006.090209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kidder DP, Wolitski RJ, Royal S, Aidala A, Courtenay-Quirk C, Holtgrave DR, Harre D, Sumartojo E, Stall R. Access to housing as a structural intervention for homeless and unstably housed people living with HIV: Rationale, methods, and implementation of the housing and health study. AIDS & Behavior. 2007b;11:S149–S161. doi: 10.1007/s10461-007-9249-0. doi: 10.1007/s10461-007-9249-0. [DOI] [PubMed] [Google Scholar]
- Kidder DP, Wolitski RJ, Pals SL, Campsmith ML. Housing status and HIV risk behaviors among homeless and housed persons with HIV. AIDS. 2008;49:451–455. doi: 10.1097/qai.0b013e31818a652c. doi: 10.1097/QAI.0b013e31818a652c. [DOI] [PubMed] [Google Scholar]
- Leaver C, Bargh G, Dunn J, Hwang S. The effects of housing status on health-related outcomes in people living with HIV: A systematic review of the literature. AIDS & Behavior. 2007;11:S85–S100. doi: 10.1007/s10461-007-9246-3. doi: 10.1007/s10461-007-9246-3. [DOI] [PubMed] [Google Scholar]
- McMahon J, Wanke C, Terrin N, Skinner S, Knox T. Poverty, hunger, education, and residential status impact survival in HIV. AIDS & Behavior. 2011;15:1503–1511. doi: 10.1007/s10461-010-9759-z. doi: 10.1007/s10461-010-9759-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meditz AL, MaWhinney S, Allshouse A, Feser W, Markowitz M, Little S, Connick E. Sex, race, and geographic region influence clinical outcomes following primary HIV-1 infection. The Journal of Infectious Diseases. 2011;203:442–451. doi: 10.1093/infdis/jiq085. doi: 10.1093/infdis/jiq085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Alliance to End Homelessness [27 Feb 2012];Homelessness and HIV/AIDS. 2006 from www.endhomlessness.org/files/1073_file_AIDSFacts.pdf.
- National Alliance to End Homelessness [27 Feb 2012];Snapshot of homelessness. 2012 from www.endhomlessness.org/section/about_homelessness/snapshot_of_homelessness.
- National Coalition for the Homeless [27 Feb 2012];HIV/AIDS and homelessness. 2009 from http://www.nationalhomeless.org/factsheets/hiv.html.
- Palepu A, Milloy M-J, Kerr T, Zhang R, Wood E. Homelessness and adherence to antiretroviral therapy among a cohort of HIV-infected injection drug users. Journal of Urban Health. 2011;88:545–555. doi: 10.1007/s11524-011-9562-9. doi: 10.1007/s11524-011-9562-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pereya M, Metsch LR, Tomar S, Valverde E, Jeanty Y, Messinger S, Boza H. Utilization of dental care services among low-income HIV-positive persons receiving primary care in South Florida. AIDS Care. 2011;23:98–106. doi: 10.1080/09540121.2010.498861. doi: 10.1080/09540121.2010.498861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reif S, Whetten K, Lowe K, Ostermann J. Association of unmet needs for support services with medication use and adherence among HIV-infected individuals in the southeastern United States. AIDS Care. 2006;18:277–283. doi: 10.1080/09540120500161868. doi: 10.1080/09540120500161868. [DOI] [PubMed] [Google Scholar]
- Robertson MJ, Clark RA, Charlebois ED, Tulsky J, Long HL, Bangsberg DR, Moss AR. HIV seroprevalence among homeless and marginally housed adults in San Francisco. American Journal of Public Health. 2004;94:1207–1217. doi: 10.2105/ajph.94.7.1207. doi: 10.2105/AJPH.94.7.1207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rumptz MH, Tobias C, Rajabiun S, Bradford J, Cabral H, Young R, Cunningham WE. Factors associated with engaging socially marginalized HIV-positive persons in primary care. AIDS Patient Care and STDs. 2007;21:S30–S29. doi: 10.1089/apc.2007.9989. doi: 10.1089/apc.2007.9989. [DOI] [PubMed] [Google Scholar]
- Salazar LF, Crosby RA, Holtgrave DR, Head S, Hadsock B, Todd J, Shouse RL. Homelessness and HIV-associated risk behavior among African American men who inject drugs and reside in the urban south of the United States. AIDS & Behavior. 2007;11:S70–S77. doi: 10.1007/s10461-007-9239-2. doi: 10.1007/s10461-007-9239-2. [DOI] [PubMed] [Google Scholar]
- Stewart KE, Cianfrini LR, Walker JF. Stress, social support and housing are related to health status among HIV-positive persons in the Deep South of the United States. AIDS Care. 2005;17:350–358. doi: 10.1080/09540120412331299780. doi: 10.1080/09540120412331299780. [DOI] [PubMed] [Google Scholar]
- Tabachnick BG, Fidell LS. Using multivariate statistics. 5th ed. Allyn and Bacon; Boston, MA: 2007. [Google Scholar]
- The Body [10 Feb 2012];United States HIV/AIDS organizations. 2011 from http://www.thebody.com/index/hotlines/other.html.
- Walley AY, Cheng DM, Libman H, Nunes D, Horsburgh CR, Saitz R, Samet JH. Recent drug use, homelessness, and increased short-term mortality in HIV-infected persons with alcohol problems. AIDS. 2008;22:415–420. doi: 10.1097/QAD.0b013e3282f423f8. doi: 10.1097/QAD.0b013e3282f423f8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wohl AR, Carlos JA, Tejero J, Dierst-Davies R, Daar ES, Khanlou H, Cadden J, Towner W, Frye D. Barriers and unmet need for supportive services for HIV patients in care in LA County, CA. AIDS Patient Care. 2011;25:525–532. doi: 10.1089/apc.2011.0149. doi: 10.1089/apc.2011.0149. [DOI] [PubMed] [Google Scholar]
- Wolitski RJ, Kidder DP, Pals SL, Royal S, Aidala A, Stall R, Holtgrave DR, Harre D, Courtenay-Quirk C. Randomized trial of the effects of housing assistance on the health and risk behaviors of homeless and unstably housed people living with HIV. AIDS & Behavior. 2010;14:493–503. doi: 10.1007/s10461-009-9643-x. doi: 10.1007/s10461-009-9643-x. [DOI] [PubMed] [Google Scholar]
- Young AS, Sullivan G, Bogart LM, Koegel P, Kanouse DE. Needs for services reported by adults with severe mental illness and HIV. Psychiatric Services. 2005;56:99–101. doi: 10.1176/appi.ps.56.1.99. doi: 10.1176/appi.ps.56.1.99. [DOI] [PubMed] [Google Scholar]