Abstract
Irreversible electroporation (IRE) is an ablation technique that is being investigated as a potential treatment of pancreatic cancer. However, many of these patients have a metallic stent in the bile duct, which is recognized as a contraindication for IRE ablation. We report a case in which an IRE ablation in the region of the pancreatic head was performed on a patient with a metallic stent which led to severe complications. After the treatment, the patient suffered from several complications including perforation of the duodenum and transverse colon, and bleeding from a branch of the superior mesenteric artery which eventually lead to her death. Therefore, we believe it is important to be aware of this if an IRE ablation close to a metallic stent is considered.
Keywords: IRE, irreversible electroporation, pancreatic cancer, metallic stent, bowel perforation, bleeding, artery injury
Introduction
Irreversible electroporation (IRE) is an ablation technique that can be used in the local treatment of several types of tumors, including the lungs, kidneys, and the liver (1). Short electrical pulses are sent between needles placed around the tumor. This causes cell death without generating heat; thus, the technique can be used close to blood vessels, bile ducts, and bowel (2,3). In pancreatic cancer, the needles can be placed both through open surgery (4) and percutaneous by an interventional radiologist (5). Although a moderate rate of complications from IRE treatment of unresectable pancreatic cancer are reported (4–6), IRE treatment has not been fully tested in large series and all possible contraindications have yet to be defined. However, the manufacturers of the IRE equipment state that ablations close to metallic stents should be seen as a contraindication (7). In previous studies, patients with metallic bile duct stents have been excluded (5) or have had the stent surgically removed before treatment (4), the fear being that metallic filaments in the stent should conduct the electricity and get hot.
We report a case in which IRE ablation was performed in the region of the pancreatic head in spite of the patient having a metallic stent in the bile duct, which is considered a contraindication.
Case report
A 72-year-old woman, diagnosed with a 4 cm large, locally advanced pancreatic cancer (LAPC) in the pancreatic head (Fig. 1), received a self-expanding metallic stent in the common bile duct due to a biliary obstruction. The tumor treatment alternatives were discussed at a multidisciplinary conference and the patient was considered unresectable due to tumor encasement of the superior mesenteric artery and vein. Palliative treatment with gemcitabine was initiated, but was discontinued after only a short while due to severe diarrhea. The patient was deemed unsuitable for other types of chemotherapy and was assessed for IRE treatment at our hospital but was excluded due to the presence of the metallic stent. However, 5 months after diagnosis, the patient contacted a private clinic where she was accepted for and later underwent an IRE procedure.
Fig. 1.
CT of the large locally advanced pancreatic cancer encasing the mesenteric vessels making a surgical resection impossible.
After the IRE treatment the diarrhea continued and after 1 month she still suffered from increasing abdominal pain. Computed tomography (CT) revealed a small abscess and raised the suspicion of a bowel perforation (Fig. 2). As there was no sign of peritonitis, she was treated with antibiotics and subsequently sent home.
Fig. 2.
CT showing a fluid collection with gas bubbles close to the pancreas and the metallic stent, considered to represent an abscess.
Eight weeks after the IRE treatment, she still had extensive diarrhea and both clinical and laboratory signs of an infection. She was admitted to our hospital and was operated with a laparoscopic loop sigmoidostomy because of the diarrhea. Two days after surgery, she went into hypovolemic shock with a distended abdomen. Peritonitis, or hemorrhage, was suspected and she underwent emergency laparotomy. The surgeons found no hemorrhage but an extensive, well-organised abscess formation behind the transverse colon and both the transverse colon and the duodenum were perforated in close vicinity to the stent. A right hemicolectomy was performed and an attempt was made to suture the duodenum, with several drains being left in the abdomen.
Due to the damage to the duodenal wall, the suture did not hold and she received both a percutaneous gastrostomy and percutaneous transhepatic drain of the common bile duct postoperatively. Seventeen days after the laparotomy, she started to bleed and an angiography revealed a pseudoaneurysm on a pancreatic branch of the superior mesenteric artery. The bleeding was treated with a coil (Fig. 3), however, 3 days later she died from a further hemorrhage.
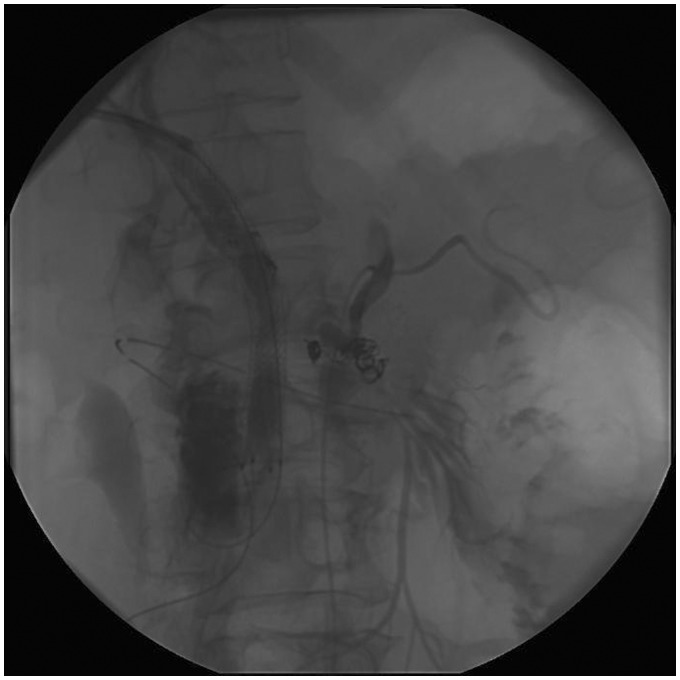
Fig. 3.
The coils after coiling the arterial bleeding from a branch of the superior mesenteric artery, note the proximity to the metallic stent in the bile duct.
Before this the patient signed an informed consent to publish her case.
Discussion
During IRE, short pulses of a direct current are delivered between two or more needles placed around the tumor area. Pulses of up to 3000 V are delivered between each needle pair. This creates pores in the cell membrane and causes cell death. As no heat is generated, treatment around vessels is possible and there is no risk of a heat-sink effect (8,9).
The indications for IRE treatment are not yet completely defined and most patients are treated within clinical trials.
The complications from IRE in the region of the pancreatic head previously described are moderate and include postprocedural pain, pancreatitis, subcutaneous hematoma, and portal vein thrombosis (4,5).
The manufactures of the IRE equipment (Angiodynamics System Queensbury, NY, USA) have stated several contraindications for IRE ablation (Table 1) (7). These contraindications include ablation in the vicinity of devices with metallic parts. To our knowledge, there has been no previously published description of complications when performing an IRE ablation close to a metallic stent in the bile duct.
Table 1.
Contraindications for IRE ablation.
| Contraindications for IRE ablation |
|---|
| Ablation of lesions in the thoracic area in the presence of implanted cardiac pacemakers or defibrillators |
| Ablation of lesions in the vicinity of implanted electronic devices or implanted devices with metal parts |
| Ablation of lesions of the eye, including the eyelids |
| Recent history of epilepsy or cardiac arrhythmia |
| Recent history of myocardial infarction |
In this particular case we cannot know whether the IRE treatment alone or the existence of the metallic stent in the treated tissue volume was the cause of the bowel perforation and pseudoaneurysm formation. However, the sites of the injuries are suggestive; therefore IRE ablations in patients with metallic stents close to the ablation zone should still be considered as an absolute contraindication. This is important as these patients often have few other treatment options and trying IRE ablation might be tempting. We must, however, warn against this. The removal of such a stents close to the intended ablation zone should be mandatory until further knowledge is gained.
In conclusion, the manufacturers of the IRE equipment have stated that IRE ablation in the vicinity of metallic parts is a contraindication. This case shows fatal complications when this was not adhered to and we would like to warn others from repeating this possible mistake.
Conflict of interest
None declared.
Funding
This case report received no specific grants from any funding agency in the public, commercial or not-for-profit sectors.
References
- 1.Thomson KR, Cheung W, Ellis SJ, et al. Investigation of the safety of irreversible electroporation in humans. J Vasc Interv Radiol 2011; 22: 611–621. [DOI] [PubMed] [Google Scholar]
- 2.Maor E, Ivorra A, Mitchel JJ, et al. Vascular smooth muscle cells ablation with endovascular non thermal irreversibel electroporation. J Vasc Interv Radiol 2010; 21: 1708–1715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kasivisvanathan V, Thapar A, Oskrochi Y, et al. Irreversible electroporation for focal ablation at the portahepatis. Cardiovasc Intervent Radiol 2012; 35: 1531–1534. [DOI] [PubMed] [Google Scholar]
- 4.Martin RC, 2nd, McFarland K, Ellis S, et al. Irreversible electroporation in locally advanced pancreatic cancer: potential improved overall survival. Ann Surg Onc 2013; 20(Suppl. 3): 443–449. [DOI] [PubMed] [Google Scholar]
- 5.Månsson C, Bergenfeldt M, Brahmstaedt R, et al. Safety and preliminary efficacy of ultrasound-guided percutaneous irreversible electroporation for treatment of localized pancreatic cancer. Anticancer Res 2014; 34: 289–293. [PubMed] [Google Scholar]
- 6.Narayan G, Hosein PJ, Arora G, et al. Percutaneous irreversible electroporation for downstaging and control of unresectable pancreatic adenocarcinoma. J Vasc Interv Radiol 2012; 23: 1613–1621. [DOI] [PubMed] [Google Scholar]
- 7.Angiodynamics [Internet].c 2010: The first surgical ablation system based on Irreversible Electroporation Technology. Available from: http://www.erickortzmd.com/wp-content/uploads/2011/04/NanoKnife.pdf.
- 8.Goldberg SN, Dupuy DE. Image-guided radiofrequency tumor ablation: challenges and opportunities. Part 1. J Vasc Interv Radiol 2001; 12: 1021–1032. [DOI] [PubMed] [Google Scholar]
- 9.Yu NC, Raman SS, Kim YJ, et al. Microwave liver ablation: influence of hepatic vein size on heat-sink effect in porcine model. J Vasc Interv Radiol 2008; 19: 1087–1092. [DOI] [PubMed] [Google Scholar]