Abstract
Breast plasmacytoma (BP) is an extremely rare extramedullary manifestation of multiple myeloma (MM). We report the imaging findings of an unusual case in which BP was the initial presentation of MM. A 53-year-old woman with no contributory medical history underwent chest computed tomography to evaluate intermittent nocturnal anterior chest pain, and bilateral multiple breast masses were found. Following an ultrasound-guided core needle biopsy, these lesions were confirmed to be BP.
Keywords: Breast neoplasms, multiple myeloma, plasmacytoma, multidetector computed tomography, mammography, ultrasonography
Introduction
Multiple myeloma (MM), also known as plasma cell myeloma or plasmacytic myeloma, is a neoplastic disorder characterized by abnormal excessive proliferation of a single clone of plasma cells derived from B cells (1) and can involve extramedullary organs or tissues. A breast plasmacytoma (BP) is an extremely rare, extramedullary manifestation of MM that has been reported in several case reports. Here, we report an unusual initial presentation of MM, focusing on the imaging findings, comprising bilateral breast masses on chest computed tomography (CT), breast ultrasonography, and mammography, which were confirmed as BP with an ultrasound (US)-guided core needle biopsy.
Case report
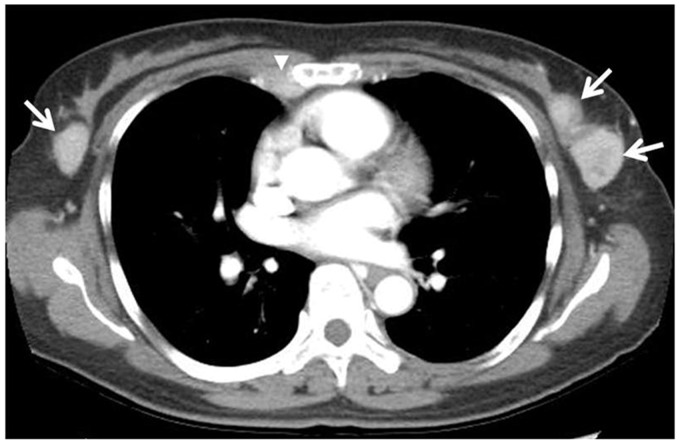
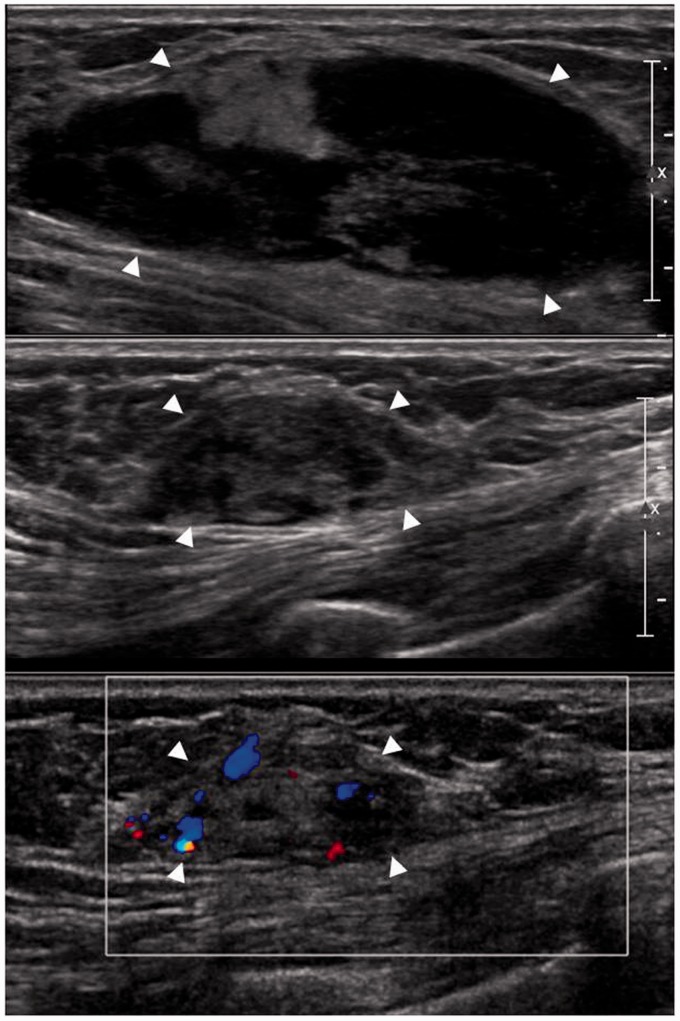
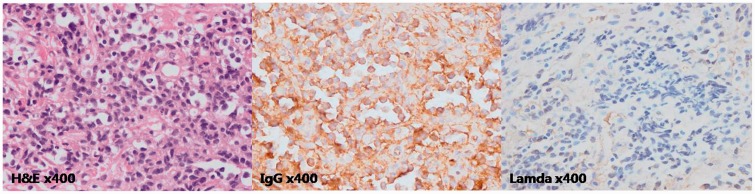
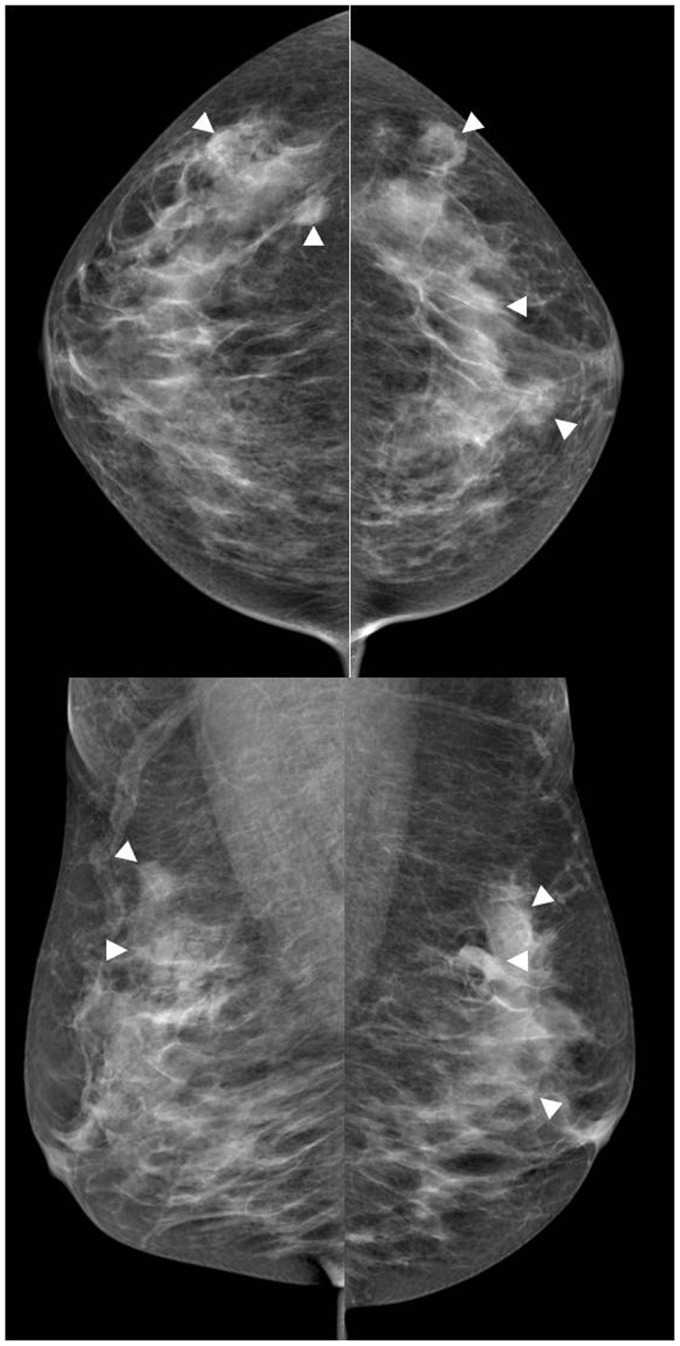
A 53-year-old woman visited our hospital complaining of intermittent nocturnal anterior chest pain for several months. Her medical history was non-contributory. Initial contrast-enhanced chest CT revealed several, variable-sized, oval to lobular, relatively circumscribed, well-enhanced masses in both breasts, with an enlarged right internal mammary lymph node (Fig. 1) and an enhanced pleural mass in the left hemithorax (not shown). The initial impression of these lesions was multifocal bilateral (cancer) metastases to the breast of unknown origin with pleural and right internal mammary lymph node metastases. An US evaluation of both breasts showed that the largest mass in each breast was oval, with an indistinct margin and heterogeneous echogenicity (Fig. 2, top and middle) with posterior acoustic enhancement at 2 o’clock in the left breast and 10 o’clock in the right breast. Color Doppler US showed that the masses had internal vascularity (Fig. 2, bottom). These masses were classified as category 4 A (low suspicion for malignancy) according to the Breast Imaging Reporting and Data System (BI-RADS) for US. Subsequently, the patient underwent US-guided core needle biopsies of both breasts. On immunohistochemical staining, the tissue was positive for CD79a, a B cell marker (2), IgG, and the lambda light chain (Fig. 3). Both breast masses were confirmed to be IgG lambda type plasma cell myeloma. A systemic evaluation of the patient revealed bone involvement in the spine, ribs, sternum, left scapula, sacrum, and both iliac bones on plain radiographs and CT. Therefore, the patient was diagnosed with secondary BP as an extramedullary presentation of MM. Accordingly, chemotherapy with thalidomide and dexamethasone was started 10 days after the initial US evaluation. On the day of chemotherapy initiation, mammography performed shortly after infusing the chemotherapeutic agents revealed multiple small circumscribed or indistinct margin, oval to round, bilateral breast masses (Fig. 4). US performed on the same day showed significant interval size reduction of the bilateral breast masses compared to the initial US (not shown). The largest lesion in the left breast at 2 o’clock direction had decreased from 5 cm to 3.5 cm in maximum diameter. On chest CT after 3 months (not shown), all of the breast lesions, the left pleural mass, and the right internal mammary lymph node showed a marked reduction in size.
Fig. 1.
The initial chest CT of a 53-year-old woman with intermittent nocturnal anterior chest pain showed bilateral, several enhancing breast masses (arrows), an enlarged right internal mammary lymph node (arrowhead), and a left pleural mass (not shown here).
Fig. 2.
Breast US of this patient revealed an oval, heterogeneous hypoechoic mass with a partly indistinct margin and posterior acoustic enhancement at left breast 2 o’clock direction (top) and a similar mass with internal vascularity on color Doppler US at right breast at 10 o’clock direction (middle and bottom).
Fig. 3.
Light photomicrographs of hematoxylin and eosin (left, ×400) and immunohistochemical stained core needle biopsy specimens of the bilateral breast masses were positive for IgG (middle, ×400) and the lambda light chain (right, ×400).
Fig. 4.
Initial mammography, performed immediate after the chemotherapy was started, revealed multiple small circumscribed or indistinct, oval to round masses in both breasts on the craniocaudal (top) and mediolateral oblique (bottom) views.
Discussion
Breast plasmacytoma is an extremely rare extramedullary manifestation of MM with an unknown prevalence. Surov et al. (3) reported that the prevalence of BP in their institution was 1.5% among patients with MM and that in 85% of the patients with BP, the breast involvement was a secondary event of MM. According to the reported cases, BP can manifest with diverse radiological findings on mammography and US (3). On mammography, it can present as dense, round or oval breast masses with well- or ill-defined margins and can also be identified as diffuse infiltration (3). On US, BP can appear as hypoechoic or echo-poor well-defined masses with hypervascularity on color Doppler, but it can also produce mixed hypo- to hyperechoic lesions with indistinct margins (3). The acoustic transmission and posterior features are also variable, showing posterior acoustic enhancement or no acoustic transmission, and even posterior acoustic shadowing (3).
In our patient, the breast masses were multiple, bilateral, circumscribed or ill-defined oval to round masses on mammography. If multiple, bilateral similar-appearing lesions with features with low suspicion of malignancy are seen on initial screening mammography, these lesions have a very high probability of being benign, such as multiple cysts or fibroadenomas (4,5). But any one of multiple lesions with suspicious findings requires further diagnostic evaluation. If the patient’s breast masses were found on screening mammography, these lesions would be categorized as BI-RADS category 0 (need additional imaging evaluation) due to their indistinct margins. All of the multiple, mammographic, bilateral breast masses of this patient showed only minor suspicious sonographic findings (6,7), such as indistinct margins, heterogeneous echogenicity, and posterior enhancement, not enough to be categorized as BI-RADS category 4 C (high suspicion for malignancy) or 5 (highly suggestive of malignancy). The current BI-RADS lexicon does not include breast CT, but clinical information from chest CT, such as pleural metastasis and metastatic internal mammary lymph nodes, can affect the management of breast masses.
The differential diagnosis of multiple bilateral breast masses includes both benign and malignant conditions. Malignant multiple bilateral masses are very uncommon, but radiologists should consider metastatic or hematological disease involving the breast when the imaging findings are suspicious. One study reported that the frequency of breast metastasis was 0.4% for all primary breast carcinomas (8). The most common sources of primary tumors of breast metastasis are lymphoma, followed by melanoma (8). Breast lymphoma accounts for approximately 0.04–0.7% of all breast malignancies and has non-specific imaging features (9). The US findings of breast lymphoma are diverse. Breast lymphoma usually appears as a hypoechoic solid mass with circumscribed or indistinct margins, but posterior acoustic enhancement, heterogeneous echo patterns, and hypo- and hyperechogenicity are all frequent in breast lymphoma (9). Breast metastases show a variety of US findings, such as well-defined circumscribed solid masses that are hyper- or hypoechoic, with posterior acoustic shadowing or without acoustic absorption (8). Because these sonographic findings of lymphoma and other metastatic breast malignancies are non-specific, a history of malignancy can help in making the diagnosis.
There are few reports on the CT findings of BP. The few reports on the radiological manifestations of plasmacytomas in other parts of the body indicate that extramedullary plasmacytomas are non-specific, but are compatible with solid tumors with invariable enhancement (10). In our case, the BP formed oval to lobular, well-enhanced masses in both breasts. This report is the first to present the CT findings of BP. Because specific radiological findings of BP have not been established, a definitive diagnosis of BP can be made only from the histopathology. In addition, a primary diagnosis of BP based on radiological or clinical features is difficult unless the patient has underlying multiple myeloma (3). Clinically, the most commonly reported clinical presentations of BP are as a palpable lump or skin edema (3); in this case, however, anterior chest pain was the initial presentation.
According to the literature, the main treatment of secondary BP is the same as for other localized plasmacytomas: systemic chemotherapy and/or local radiotherapy (1). Our patient showed a considerable reduction in the size of the bilateral breast masses on the post-chemotherapy US on the first day of chemotherapy. It is not clear whether the size reduction was attributed to the chemotherapy or spontaneous regression of the BP. However, the spontaneous regression of BP without treatment has never been reported. Although the time interval is too short to assess the therapeutic response to chemotherapy, this initial size reduction was thought to be caused by the chemotherapy.
In conclusion, BP has no specific radiological findings. When multiple bilateral breast masses are found incidentally, the differential diagnosis should include the secondary involvement of a hematological disorder, including BP, as well as metastatic malignancies and benign conditions such as fibroadenoma.
Conflict of interest
None declared.
References
- 1.Kyle RA, Gertz MA, Witzig TE, et al. Review of 1027 patients with newly diagnosed multiple myeloma. Mayo Clin Proc 2003; 78: 21–33. [DOI] [PubMed] [Google Scholar]
- 2.Chu PG, Arber DA. CD79: a review. Appl Immunohistochem. Mol Morphol 2001; 9: 97–106. [DOI] [PubMed] [Google Scholar]
- 3.Surov A, Holzhausen HJ, Ruschke K, et al. Breast plasmacytoma. ActaRadiol 2010; 51: 498–504. [DOI] [PubMed] [Google Scholar]
- 4.Berg WA, Sechtin AG, Marques H, et al. Cystic breast masses and the ACRIN 6666 experience. Radiol Clin North Am 2010; 48: 931–987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Leung JW, Sickles EA. Multiple bilateral masses detected on screening mammography: assessment of need for recall imaging. Am J Roentgenol 2000; 175: 23–29. [DOI] [PubMed] [Google Scholar]
- 6.Kim EK, Ko KH, Oh KK, et al. Clinical application of the BI-RADS final assessment to breast sonography in conjunction with mammography. Am J Roentgenol 2008; 190: 1209–1215. [DOI] [PubMed] [Google Scholar]
- 7.Yoon JH, Kim MJ, Moon HJ, et al. Subcategorization of ultrasonographic BI-RADS category 4: positive predictive value and clinical factors affecting it. Ultrasound Med Biol 2011; 37: 693–699. [DOI] [PubMed] [Google Scholar]
- 8.Vizcaino I, Torregrosa A, Higueras V, et al. Metastasis to the breast from extramammary malignancies: a report of four cases and a review of literature. Eur Radiol 2001; 11: 1659–1665. [DOI] [PubMed] [Google Scholar]
- 9.Shim E, Song SE, Seo BK, et al. Lymphoma affecting the breast: a pictorial review of multimodal imaging findings. J Breast Cancer 2013; 16: 254–265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ooi GC, Chim JC, Au WY, et al. Radiologic manifestations of primary solitary extramedullary and multiple solitary plasmacytomas. Am J Roentgenol 2006; 186: 821–827. [DOI] [PubMed] [Google Scholar]