Abstract
Introduction
Female sexual function changes considerably during pregnancy and the postpartum period. In addition, women's physical and mental health, endocrine secretion, and internal and external genitalia vary during these times. However, there are limited studies on the relationship between delivery and sexual function.
Aim
The present study aimed to demonstrate the association between sexual function and delivery mode.
Methods
Mothers who delivered a single baby at term were recruited for the study, and 435 mothers were analyzed.
Main Outcome Measures
The Female Sexual Function Questionnaire (SFQ28) scores and mothers' backgrounds were assessed at 6 months after delivery.
Results
The delivery mode affected the SFQ28 partner domain. Episiotomy affected the arousal (sensation) domain. Multiple regression analysis revealed that maternal age and cesarean section were significantly associated with several SHQ28 domains.
Conclusion
This study suggests that routine episiotomies at delivery should be avoided to improve postpartum maternal sexual function. Maternal age and cesarean section were found to affect postpartum sexual health.
Keywords: Female Sexual Function Questionnaire (SFQ28), Delivery Mode, Episiotomy
Introduction
Female sexual function changes considerably during pregnancy and the postpartum period. During this time, the perineum and pelvic floor muscles are damaged. During breastfeeding, prolactin secretion, which suppresses libido and stimulates estrogen secretion, is increased. Changes in female sexual function during pregnancy and the postpartum period are related to endocrine changes and anatomical change 1. In Japan, the term “sexless” is defined as a frequency of sexual intercourse of <1 time/month. Sexlessness is considered a social issue, and pregnancy and delivery are considered contributory factors 2. In the literature, approximately 80–95% of mothers return to sexual activity within 3 months of delivery 1, but this has not been proven in Japanese women 3. Women's physical and mental health, endocrine secretion, and internal and external genitalia vary during pregnancy and the postpartum period.
Several studies demonstrated the association between sexual function and delivery mode, episiotomy, and laceration 4–6. Other studies revealed no association between mode of delivery and sexual function 7–11. Yeniel and Petri reviewed the effect of pregnancy and mode of delivery on postpartum sexual function. There is no clear evidence of a relationship between the mode of delivery and changes in sexual function 12. There is controversy over the effect of mode of delivery episiotomy and perineal laceration on sexual function. To explore the hypothesis that sexual function is associated with mode of delivery and laceration is important, because sexual health is one of critical parts of maternal health. We planned the present study in Japanese postpartum women to investigate the relationship of sexual function with maternal status, delivery mode, episiotomy, and laceration.
Aim
The present study aimed to demonstrate relationships between sexual function and delivery mode. We determined sexual function by the Female Sexual Function Questionnaire (SFQ28), which consisted of the desire domain, the arousal (sensation) domain, the arousal (lubrication) domain, the arousal (cognitive) domain, the orgasm domain, the pain domain, the enjoyment domain, and the partner domain. Each factor of SFQ-28 was examined to improve delivery management and postpartum maternal health.
Methods
Participants
Mothers who delivered a single baby at term at Kawasaki University Hospital and related hospitals were recruited for this study during a postnatal examination >1 month after delivery. Six months following delivery, questionnaires were sent by mail to mothers who gave informed consent. Questionnaire responses were analyzed. The data were collected from November 2011 to June 2013. As shown in Figure 1, a total of 674 mothers were enrolled in the study. Informed consent was obtained from each patient. A total of 502 mothers returned questionnaires. Sixty-seven mothers were excluded because of incomplete answers of questionnaires. A total of 435 mothers were included in the study. This study was approved by the Ethical Committee of Kawasaki Medical School.
Figure 1.
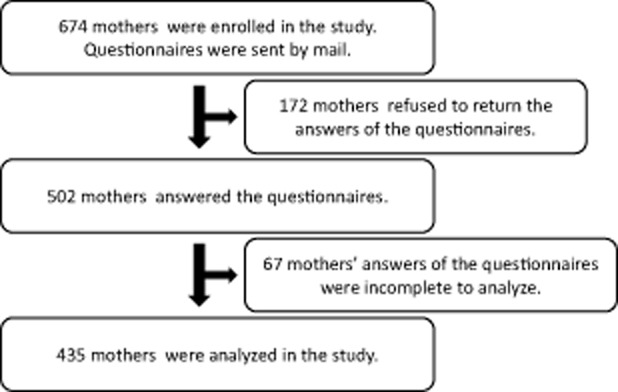
A flowchart of the present study.
Main Outcome Measures
The SFQ28
The SFQ28 is a self-reported measure of female sexual function and was developed to be multidimensional and patient centered. The SFQ28 addresses all aspects of the sexual response cycle (desire, arousal, orgasm) as well as pain, which is consistent with the criteria in the Diagnostic and Statistical Manual of Mental Disorders and the newly generated American Foundation for Urologic Disease definitions 13. We analyzed SFQ score as sexual function: the primary outcome.
Sociodemographic Items
The self-reported questionnaire included sociodemographic and medical items as follows: maternal age, educational level, occupational status, marital status, cohabiting status, partner's occupational status, obstetric history, and psychiatric history.
Statistical Analysis
Data are reported as mean ± standard deviation. Statistical significance was assessed using analysis of variance and the Wilcoxon signed-rank test with a 5% significance level. The correlation coefficients between two variables were determined by Spearman rank analysis. A multiple regression analysis was undertaken to identify the variables that predicted sexual health. We performed forward-backward stepwise selection method for a multiple regression analysis. The data were analyzed with IBM SPSS statistics ver. 20 (IBM, Armonk, NY, USA).
Results
Of the questionnaires that were sent, 435 completely answered questionnaires were returned. The means of maternal age, age at marriage, infant birth weight, and gestational weeks at delivery were 33.2 ± 4.4 years, 28.5 ± 4.0 years, 3,023 ± 424 g, and 39.2 ± 1.4 weeks, respectively. Two hundred and eighty-two (65%) participants had a vaginal delivery without oxytocin (Group A), 82 (19%) had a vaginal delivery with oxytocin (Group B), 21 (5%) delivered by an operative maneuver such as vacuum and forceps (Group C), 23 (5%) had preplanned cesarean sections (Group D), and 27 (6%) had emergency cesarean sections (Group E). There were no significant differences in maternal age, age at marriage, income, academic background, or cohabitation status among the five groups. There were significant differences in the number of children and parity among the five groups. The mean birth weight and gestational weeks in the planned cesarean section group were significantly lower and earlier, respectively. The scores indicating normal sexual function of the desire domain, the arousal (sensation) domain, the arousal (lubrication) domain, the arousal (cognitive) domain, the orgasm domain, the pain domain, the enjoyment domain, and the partner domain are more than 23, 14, 8, 8, 12, 12, 23, and 8, respectively. The numbers of mothers indicating normal sexual function of the desire domain, the arousal (sensation) domain, the arousal (lubrication) domain, the arousal (cognitive) domain, the orgasm domain, the pain domain, the enjoyment domain, and the partner domain were 1 (0.2%), 33 (7.6%), 5 (1.1%), 12 (2.8%), 7 (1.6%), 48 (11.0%), 7 (1.6%), and 362 (83.2%), respectively. The normal sexual function of postpartum Japanese women at 6 months after birth was very low.
Table 1 shows the related quotient (r value) to determine relationships among each category. Maternal age was significantly associated with the number of children and each SFQ28 domain. The number of children was significantly associated with the SFQ28 pain domain. Many SFQ28 domains were significantly associated with each other.
Table 1.
Related quotient (r value) among each SFQ28 domain
| Maternal age | Numbers of children |
SFQ28 |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Desire | Arousal (sensation) | Arousal (lubrication) | Arousal (cognitive) | Orgasm | Pain | Enjoyment | Partner | |||
| Maternal age | 1.000 | |||||||||
| Numbers of children | 0.202* | 1.000 | ||||||||
| Desire | −0.137* | −0.087 | 1.000 | |||||||
| Arousal (sensation) | −0.167* | 0.064 | 0.651* | 1.000 | ||||||
| Arousal (lubrication) | −0.206* | 0.061 | 0.642* | 0.924* | 1.000 | |||||
| Arousal (cognitive) | −0.178* | 0.057 | 0.685* | 0.926* | 0.940* | 1.000 | ||||
| Orgasm | −0.105* | 0.071 | 0.597* | 0.787* | 0.794* | 0.801* | 1.000 | |||
| Pain | −0.180* | 0.139* | 0.542* | 0.821* | 0.848* | 0.827* | 0.694* | 1.000 | ||
| Enjoyment | −0.167* | 0.010 | 0.737* | 0.892* | 0.903* | 0.922* | 0.820* | 0.819* | 1.000 | |
| Partner | 0.009 | 0.050 | 0.045 | −0.028 | −0.029 | 0.015 | 0.021 | −0.020 | 0.036 | 1.000 |
Significant difference (P < 0.05) between the two categories
SFQ28 = Female Sexual Function Questionnaire
Female sexual function was analyzed based on two different classifications. The first classification was based on the delivery mode, with classifications separated into a vaginal delivery group, including delivery with oxytocic agents (Group A + B), an operative delivery group (Group C), and a cesarean section group, including both planned and emergency cesarean sections (Group D + E). As shown in Figure 2, the score of the partner domain of Group A + B (vaginal delivery), Group C (portative delivery), and Group D + E (cesarean section) were 8.7 ± 2.2, 9.3 ± 1.2, and 9.1 ± 1.5, respectively. There were significant differences in the SFQ28 partner domains between the vaginal and operative delivery groups. There were also nonsignificant differences in the orgasm and pain domains. The score in the SFQ28 partner domain for the cesarean section group was nonsignificantly higher than that for the vaginal delivery group.
Figure 2.
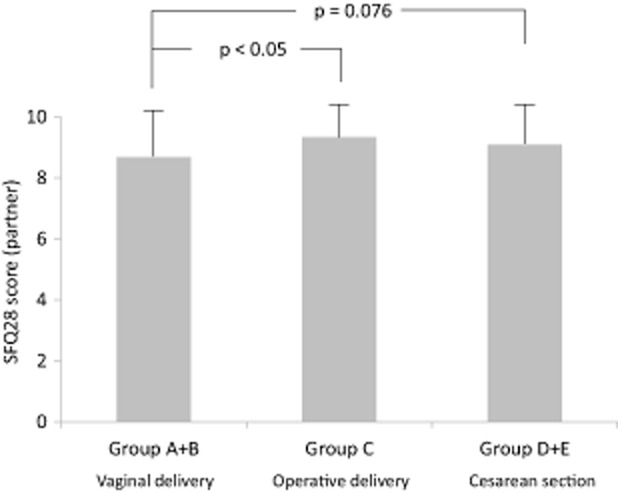
Female Sexual Function Questionnaire (SFQ28) partner domain score and the delivery mode. Data represent the mean ± standard deviation. Group A: vaginal delivery group, Group B: vaginal delivery with oxytocin group, Group C: operative delivery group, Group D: planned cesarean section group, Group E: emergency cesarean section group. The SFQ28 partner domain score for the vaginal delivery group was significantly higher than that of the operative delivery group.
The second classification was based on the condition of the perineum following delivery, with classifications separated into a no laceration group, an episiotomy group, a laceration group (up to a level three laceration) without episiotomy, and a cesarean section group. Table 2 presents the scores for each SFQ28 domain in each group; the domains include desire, arousal (lubrication), arousal (cognitive), orgasm, pain, enjoyment, and partner. The no laceration group was compared with the other groups. There was a nonsignificant difference in the SFQ28 arousal (lubrication) and orgasm domains between the no laceration and episiotomy groups. There were no statistical differences for any of the SFQ28 domains between the no laceration and cesarean section groups. As shown in Figure 3, the scores of the arousal (sensation) domain of the no laceration group, the episiotomy group, the laceration group, and the cesarean section group were 4.8 ± 5.8, 3.5 ± 4.7, 4.1 ± 5.4, and 3.8 ± 5.2, respectively. There was a significant difference in the arousal (sensation) domain between the no laceration and episiotomy groups. The incidence of sexlessness (no intercourse in 4 weeks) regardless of the husband's presence during delivery was found to be 56% and 58%, respectively, with no statistical difference.
Table 2.
Sexual activity (SFQ28 score) and laceration at delivery
| No laceration | Episiotomy | Laceration | Cesarean section | |
|---|---|---|---|---|
| Desire | 8.2 ± 3.6 | 8.3 ± 3.4 | 8.0 ± 3.5 | 9.1 ± 3.9 |
| Arousal (lubrication) | 2.7 ± 3.1 | 2.1 ± 2.9 | 2.4 ± 3.015 | 2.2 ± 2.9 |
| Arousal (cognitive) | 2.5 ± 3.0 | 2.0 ± 2.8 | 2.2 ± 2.9 | 2.1 ± 2.8 |
| Orgasm | 3.6 ± 4.6 | 2.8 ± 4.0 | 2.8 ± 4.2 | 3.5 ± 4.5 |
| Pain | 5.1 ± 5.6 | 4.1 ± 5.4 | 4.3 ± 5.4 | 4.0 ± 5.2 |
| Enjoyment | 8.4 ± 7.6 | 7.6 ± 7.3 | 7.5 ± 7.1 | 7.9 ± 7.6 |
| Partner | 8.9 ± 1.7 | 8.7 ± 2.2 | 8.7 ± 2.4 | 9.1 ± 1.5 |
Data represent the score of each domain of SFQ as mean ± standard deviation
SFQ28 = Female Sexual Function Questionnaire
Figure 3.
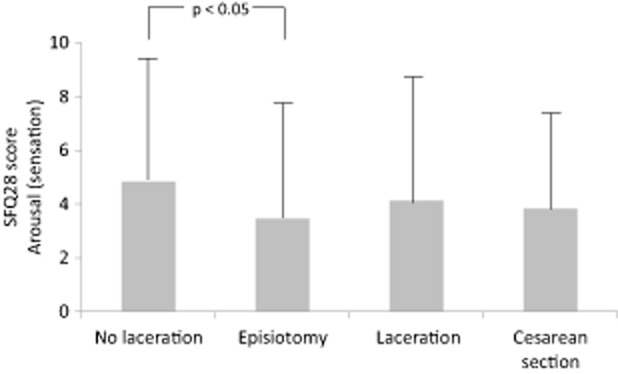
Female Sexual Function Questionnaire (SFQ28) arousal (sensation) domain score and laceration at delivery. Data represent the mean ± standard deviation. There was a significant difference in the arousal (sensation) domain between the no laceration and episiotomy groups.
Finally, a multiple regression analysis was performed to determine the variables that predicted sexual health. Maternal age and cesarean section were significant predictors of the SHQ28 domains of desire (P = 0.005 and P = 0.015, respectively), arousal (lubrication) (P = 0.003 and P = 0.032, respectively), and arousal (cognitive) (P = 0.007 and P = 0.036, respectively). Maternal age was a significant predictor of the enjoyment domain (P = 0.001). Associations of the SHQ28 orgasm domain with maternal age was P = 0.071. Associations of the SHQ28 pain domain with maternal age and cesarean section were P = 0.057 and P = 0.071, respectively.
Discussion
The present study is the first to analyze the association between maternal sexual function and maternal status, delivery mode, episiotomy, and laceration. There were significant differences in the SFQ28 partner domain between the vaginal and operative delivery groups. There were also nonsignificant differences in the orgasm and pain domains. The association between delivery mode and postpartum sexual activity is controversial. In a 12-month study of 912 pregnant women and their husbands, instrumental deliveries were associated with the highest and planned cesarean section with the lowest rate of long-term maternal and paternal sexual dysfunction 5. Our results were similar to Safarinejad et al.'s study 5, because of the similar timing of the examination. One study demonstrated that both cesarean section and perineal scars were associated with sexual malfunction 4. However, another study demonstrated that elective cesarean delivery was not associated with a protective effect on postpartum sexual function 8. Gungor et al. demonstrated that sexual dissatisfaction should not be assumed simply a product of the delivery mode. Individual, sociodemographic, lifestyle, and marital characteristics should also be taken into account 9. Mode of delivery history appeared to have minimal effect on sexual function at 6 years post-index delivery 7. Fehniger et al. reported the sexual function of women aged 40 years and older with at least one past child event. The sexual activities of women were not associated with a history of cesarean delivery compared with vaginal delivery alone. Women with a history of operative-assisted delivery were more likely to report low desire 10. Operative-associated delivery affected sexual function for a long time. Low partnership in the operative-assisted delivery in our study might affect the long-term sexual function. Because the interval between the delivery time and the study time differs in the studies, the association between delivery mode and postpartum sexual activity is controversial. Accordingly, further investigation is necessary to determine the relationship between maternal sexual health and the delivery mode.
In the present study, episiotomy had negative effects on sexual function in Japan. All SFQ28 domains were superior in mothers without laceration and episiotomy. However, we could not demonstrate the cause and the effect of episiotomy on sexual function because of our cross-sectional single-time point data. This was one of the limitations of the present study. Several studies have demonstrated a relation between the condition of the perineum after delivery and sexual function. Large lacerations (anal sphincter laceration) damaged the maternal sexual activity 14,15. In 55 postpartum women compared with women with intact perineum, those who had both episiotomy and second-degree perineal tears had lower levels of libido, orgasm, and sexual satisfaction and more pain during intercourse at 3 months after delivery 6. Another study demonstrated that there was no significant difference in sexual function 12–18 months after childbirth between women who delivered vaginally without episiotomy, heavy perineal laceration, or secondary operative interventions and women who underwent elective cesarean section 11. A meta-analysis revealed that evidence does not support maternal benefits traditionally ascribed to routine episiotomies. Routine episiotomies also have negative effects on maternal sexual function and activity. For instance, pain with intercourse was more common among women who underwent an episiotomy 16. Our results also supported the negative effects of episiotomies on female sexual function. Including the present study, we recommend that routine episiotomy be avoided at delivery to improve maternal sexual function after delivery.
We examined the incidence of sexlessness (no intercourse for 4 weeks) regardless of the husband's presence during delivery. Japanese are sexually hypoactive, and it is speculated that the husband's presence during delivery affects the postnatal sexual activity of the couple 3. However, there was no statistical difference in the incidence of sexlessness regardless of the husband's presence during delivery. This finding encourages husband's attendance to support his wife during delivery.
Multiple regression analysis revealed that maternal age and cesarean section were significantly associated with several SHQ28 domains. Maternal age and cesarean section affected postpartum sexual health. The negative effects of cesarean sections on maternal sexual health should be considered. A recent review revealed no clear evidence relating the delivery mode of delivery to changes in sexual function 12. However, the interval between delivery and the study and the ethnicity differed from the present study. Another study demonstrated that both cesarean and perineal scars were associated with sexual malfunction 4, and our study supported the previous study. The strengths of the present study were sample size and the same ethnical background; however, the limitation was that the present study was one-point examination and there was no predelivery assessment. Thus, further investigations are necessary to study the association between sexual health and the delivery mode.
Conclusion
Our study demonstrated that maternal age and cesarean section were significantly associated with several SHQ28 domains. Further investigation is necessary to determine the relationship between maternal sexual health and the delivery mode. To improve maternal sexual function after delivery, we recommend that routine episiotomy be avoided at delivery to improve postnatal maternal sexual function.
Acknowledgments
The authors thank Dr. Kaoru Miyake (Miyake Clinic), Dr. Takeshi Taniguchi (Taniguchi Hospital), and Dr. Haruyoshi Urano (Ikuryo Clinic) for recruiting the participants. This work was supported, in part, by Grants-in-Aid for Scientific Research (Nos. 21592118, 24592493) from the Ministry of Education, Science, and Culture of Japan (Tokyo, Japan), Health Labor Sciences Research Grant of Research on Child and Families (Tokyo, Japan), and research project grants 21-411, 25B-14, and 25G-6 from Kawasaki Medical School (Kurashiki, Japan).
References
- Johnson CE. Sexual health during pregnancy and the postpartum. J Sex Med. 2011;8:1267–1284. doi: 10.1111/j.1743-6109.2011.02223.x. [DOI] [PubMed] [Google Scholar]
- Abe T. Sexless couples and psychosextherapy. Sanfujinkachiryou. 1994;10:388–393. (in Japanese) [Google Scholar]
- Frequency of sexual intercourse and satisfaction. 2014. (in Japanese) Available at: http://www.durex.com/en-JP/SexualWellbeingSurvey/Fequency%20of%20Sex/pages/default.aspx.
- Lal M, Pattison HM, Allan TF, Callender R. Does post-caesarean dyspareunia reflect sexual malfunction, pelvic floor and perineal dysfunction? J Obstet Gynaecol. 2011;31:617–630. doi: 10.3109/01443615.2011.594915. [DOI] [PubMed] [Google Scholar]
- Safarinejad MR, Kolahi AA, Hosseini L. The effect of the mode of delivery on the quality of life, sexual function, and sexual satisfaction in primiparous women and their husbands. J Sex Med. 2009;6:1645–1667. doi: 10.1111/j.1743-6109.2009.01232.x. [DOI] [PubMed] [Google Scholar]
- Rathfisch G, Dikencik BK, Kizilkaya Beji N, Comert N, Tekirdag AI, Kadioglu A. Effects of perineal trauma on postpartum sexual function. J Adv Nurs. 2010;66:2640–2649. doi: 10.1111/j.1365-2648.2010.05428.x. [DOI] [PubMed] [Google Scholar]
- Dean N, Wilson D, Herbison P, Glazener C, Aung T, Macarthur C. Sexual function, delivery mode history, pelvic floor muscle exercises and incontinence: A cross-sectional study six years post-partum. Aust N Z J Obstet Gynaecol. 2008;48:302–311. doi: 10.1111/j.1479-828X.2008.00854.x. [DOI] [PubMed] [Google Scholar]
- Lurie S, Aizenberg M, Sulema V, Boaz M, Kovo M, Golan A, Sadan O. Sexual function after childbirth by the mode of delivery: A prospective study. Arch Gynecol Obstet. 2013;288:785–792. doi: 10.1007/s00404-013-2846-4. [DOI] [PubMed] [Google Scholar]
- Gungor S, Baser I, Ceyhan S, Karasahin E, Acikel CH. Mode of delivery and subsequent long-term sexual function of primiparous women. Int J Impot Res. 2007;19:358–365. doi: 10.1038/sj.ijir.3901546. [DOI] [PubMed] [Google Scholar]
- Fehniger JE, Brown JS, Creasman JM, Van Den Eeden SK, Thom DH, Subak LL, Huang AJ. Childbirth and female sexual function later in life. Obstet Gynecol. 2013;122:988–997. doi: 10.1097/AOG.0b013e3182a7f3fc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klein K, Worda C, Leipold H, Gruber C, Husslein P, Wenzl R. Does the mode of delivery influence sexual function after childbirth? J Womens Health (Larchmt) 2009;18:1227–1231. doi: 10.1089/jwh.2008.1198. [DOI] [PubMed] [Google Scholar]
- Yeniel AO, Petri E. Pregnancy, childbirth, and sexual function: Perceptions and facts. Int Urogynecol J. 2014;25:5–14. doi: 10.1007/s00192-013-2118-7. [DOI] [PubMed] [Google Scholar]
- Quirk FH, Heiman JR, Rosen RC, Laan E, Smith MD, Boolell M. Development of a sexual function questionnaire for clinical trials of female sexual dysfunction. J Womens Health Gend Based Med. 2002;11:277–289. doi: 10.1089/152460902753668475. [DOI] [PubMed] [Google Scholar]
- Brubaker L, Handa VL, Bradley CS, Connolly A, Moalli P, Brown MB, Weber A Pelvic Floor Disorders Network. Sexual function 6 months after first delivery. Obstet Gynecol. 2008;111:1040–1044. doi: 10.1097/AOG.0b013e318169cdee. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ejegård H, Ryding EL, Sjogren B. Sexuality after delivery with episiotomy: A long-term follow-up. Gynecol Obstet Invest. 2008;66:1–7. doi: 10.1159/000113464. [DOI] [PubMed] [Google Scholar]
- Hartmann K, Viswanathan M, Palmieri R, Gartlehner G, Thorp J, Jr, Lohr KN. Outcomes of routine episiotomy: A systematic review [Review] JAMA. 2005;293:2141–2148. doi: 10.1001/jama.293.17.2141. [DOI] [PubMed] [Google Scholar]


