An 18-year-old African American adolescent presented with 1 week of fever, headache, and left arm and leg weakness. On examination, he had scrotal ulcers, left hemiparesis, dysarthria, and bilateral dysmetria. There was no uveitis or papilledema, but he had a history of recurrent oral ulcers. The cerebrospinal fluid (CSF) was remarkable for moderate lymphocytic pleocytosis to 175/µL but was negative for infectious etiologies. Oligoclonal bands were absent from the CSF and an immunoglobulin index was normal. A serum workup for rheumatological disease including erythrocyte sedimentation rate, C-reactive protein, antinuclear antibody, rheumatoid factor, angiotensin-converting enzyme, anti-Ro, and anti-La antibodies was unrevealing.
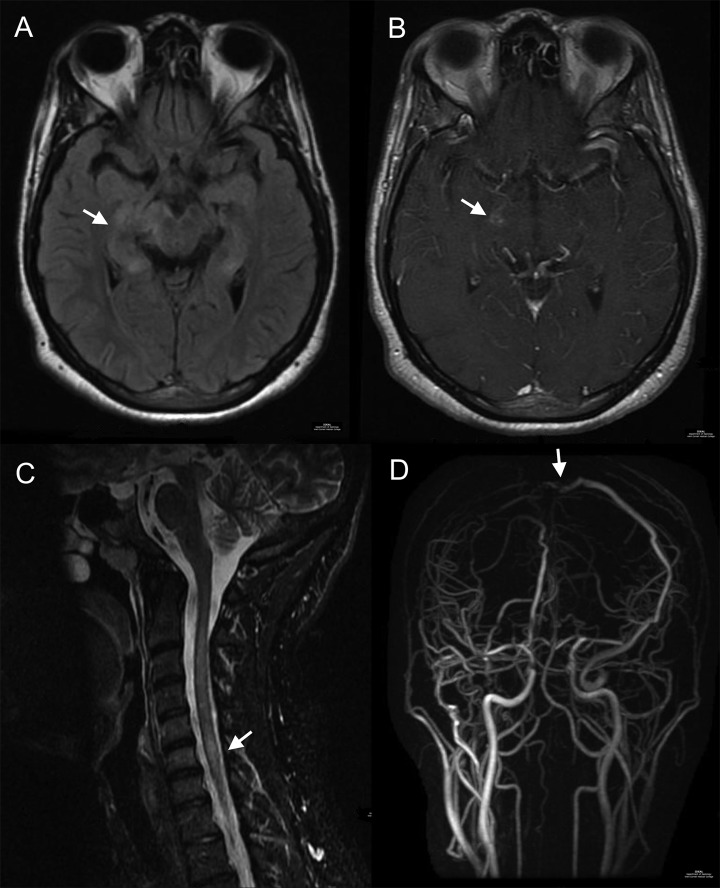
Magnetic resonance imaging of the brain showed T2-weighted hyperintensities with enhancement from the left internal capsule to the pons. Additionally, there were nonenhancing foci of T2-weighted hyperintensities in the right paracentral lobule, left corona radiata, hippocampi, and cervical spine (Figure 1A and B). A head magnetic resonance venogram revealed near occlusion of the superior sagittal sinus (Figure 1D). A hypercoagulable workup including antiphospholipid antibodies was negative. Based on the clinical presentation and radiographic findings, a diagnosis of neuro-Behçet disease (NBD) was made. Treatment with therapeutic low-molecular-weight heparin, high-dose intravenous corticosteroids, and cyclophosphamide resulted in significant neurological improvement.
Figure 1.
Neuroimaging in neuro-Behçet disease: fluid-attenuated inversion recovery (FLAIR) sequence (A) shows hyperintensities in the right cerebral peduncle and hippocampi. T1-postcontrast sequence (B) shows enhancement in the right thalamus. Cervical FLAIR sequence (C) shows intramedullary hyperintensity. Magnetic resonance venogram (D) shows stenosis of the superior sagittal sinus.
Neurological complications of Behçet disease are rare, typically reported as a 1% to 3% incidence in all cases of Behçet disease.1 This case illustrates some of the typical manifestations of NBD, which often include meningoencephalitis, parenchymal lesions, cerebral venous thrombosis, and aneurysm formation.1,2
Acknowledgments
The authors would like to acknowledge the contributions of Sumit Niogi and the Imaging Data Evaluation and Analytics Lab (IDEAL) of the Department of Radiology at Weill Cornell Medical College in supplying the images for this publication.
Footnotes
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Al-Araji A, Kidd DP. Neuro-Behçet's disease: epidemiology, clinical characteristics, and management. Lancet Neurol. 2009;8(2):192–204. [DOI] [PubMed] [Google Scholar]
- 2. Akman-Demir G, Serdaroglu P, Tasçi B. Clinical patterns of neurological involvement in Behçet's disease: evaluation of 200 patients. Neuro-Behçet study group. Brain. 1999;122(pt 11):2171–2182. [DOI] [PubMed] [Google Scholar]