Abstract
Hospitals are challenged with reevaluating their hospital’s transitional care practices, to reduce 30-day readmission rates, prevent adverse events, and ensure a safe transition of patients from hospital to home. Despite the increasing attention to transitional care, there are few published studies that have shown significant reductions in readmission rates, particularly for patients with stroke and other neurologic diagnoses. Successful hospital-initiated transitional care programs include a “bridging” strategy with both predischarge and postdischarge interventions and dedicated transitions provider involved at multiple points in time. Although multicomponent strategies including patient engagement, use of a dedicated transition provider, and facilitation of communication with outpatient providers require time and resources, there is evidence that neurohospitalists can implement a transitional care program with the aim of improving patient safety across the continuum of care.
Keywords: transitional care, readmissions, adverse events, patient, quality of health care, stroke, penalties, hospitalists, Centers for Medicare and Medicaid Services
Introduction
The weeks following hospitalization remain a particularly challenging time for patients. Approximately 1 in 5 patients experience adverse events such as adverse drug events (ADEs) and hospital-related complications during this period.1-3 Unfortunately, readmission to the hospital after discharge is common—nearly 20% of hospitalized older Medicare patients will be readmitted within 30 days.1
A broad spectrum of adverse events can occur after discharge, including both diagnostic and therapeutic errors, but ADEs are particularly common and harmful, leading to hospitalizations and readmissions.4,5 Recent studies indicate that nearly 100 000 elderly patients are hospitalized every year due to ADEs.6 Patients with stroke represent a population at high risk of recurrent cerebrovascular events, recurrent hospitalization within 1 year of the index admission, higher rates of disability, and increased mortality.7,8 Ensuring safe care transitions for neurologic patients with complex, chronic illnesses such as stroke, demyelinating diseases, epilepsy, and neuromuscular conditions will remain an important patient safety issue for neurohospitalists.9
Transitional care, or the care patients receive as they move between health care settings and providers, involves bridging care gaps across different health care settings, including hospitalizations and outpatient visits.10,11 Hospital-based transitional care interventions aim to smooth the transition from the inpatient to the outpatient setting and prevent unnecessary readmissions and adverse events.
Several national policy initiatives have recently been implemented to encourage improvements in transitional care in response to the cost related to adverse events and readmissions. The Centers for Medicare & Medicaid Services (CMS) already publicly report hospitals’ risk-adjusted 30-day readmission rates for patients hospitalized with pneumonia, acute myocardial infarction, and congestive heart failure (CHF).12 In the near future, it is anticipated that other diagnoses including neurologic conditions such as stroke may be included.13 The centers recently announced that more than 2000 hospitals would have financial penalties of up to 1% of Medicare reimbursements because of high readmission rates.14 The partnership for patients initiative aimed to decrease preventable readmissions by 20% by the end of 2013 and identified improving transitional care as an opportunity to reduce health care expenditures.15 Together, these policies constitute a mandate to hospitals to improve transitional care when patients are discharged from the hospital.
Highly targeted, disease-specific transitional care strategies have shown modest success in reducing readmissions for CHF, chronic obstructive pulmonary disease, and asthma, but for neurological diseases little is known about effective transitional care strategies. Several systematic reviews have identified a range of interventions that have been studied,16-19 but the effect of these interventions on readmissions or other important markers of postdischarge patient safety such as emergency department (ED) visits and posthospitalization adverse events is lacking.
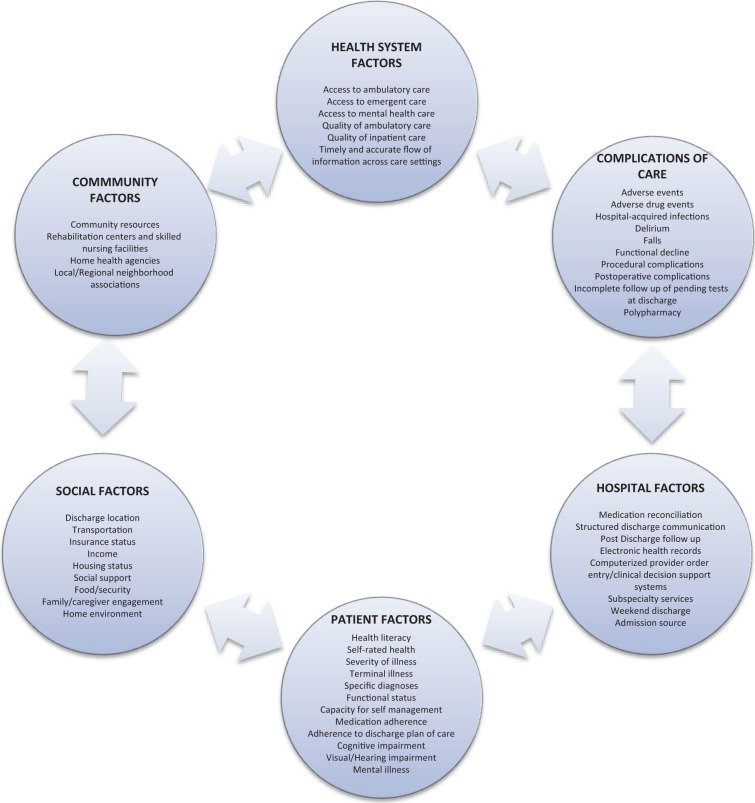
Nearly 20% of 30-day readmissions, based on published studies of readmissions risk factors,20 are likely preventable, and hospital readmission rates are in large part influenced by other factors outside of the hospital domain including poor social support, poverty, and access to outpatient care (Figure 1).21-23 A recent retrospective review of discharges for stroke and other cerebrovascular diseases to a single academic medical center found that 53% of the readmissions were potentially avoidable and included reported gaps in care coordination, lack of timely follow-up, and inadequate instructions at discharge.24 Despite these challenges, progress is being made at preventing readmissions, as CMS recently reported that 30-day readmission rates for Medicare patients have declined between 2007 and 2012.25
Figure 1.
Factors involved in hospital readmission.
In this era, focusing on high-value, low-cost alternatives to care, transitional care strategies require a considerable utilization of human resources to be effective; on the other hand, transitional care strategies focus on what is important to neurohospitalists and patients—improving the quality of care that is delivered with a focus on patient safety and connecting health care systems. This narrative review will focus on a description of transitional care strategies, summarize the effectiveness of several published transitional care programs, and outline specific recommendations for the neurohospitalist.
Transitional Care: Definitions, Risk, and Strategies
Definition of Strategies and Adverse Events
A “transitional care strategy” is an intervention or a group of interventions initiated prior to hospital discharge with the aim of ensuring the safe and effective transition of patients from the setting to setting, such as from the hospital to home. Specific interventions have been previously classified based on a taxonomy grouped into the following 3 categories: predischarge, postdischarge, and “bridging” (including both pre- and postdischarge components; Table 1).17,26-30
Table 1.
Taxonomy of Interventions to Improve Transitional Care at Hospital Discharge.
| Predischarge interventions | Assessment of risk of adverse events or readmissions |
| Patient engagement (eg, patient or caregiver education) | |
| Creation of an individualized patient record (customized document in lay language containing clinical and educational information for patients’ use after discharge) | |
| Facilitation of communication with outpatient providers | |
| Multidisciplinary discharge planning team | |
| Dedicated transition provider (who has in-person or phone contact with the patient before and after discharge) | |
| Medication reconciliation | |
| Postdischarge interventions | Outreach to patients (including follow-up phone calls, patient-activated hotlines, and home visits) |
| Facilitation of clinical follow-up (including facilitated ambulatory provider follow-up) | |
| Medication reconciliation after discharge | |
| Bridging interventions | Inclusion of at least 1 predischarge component and at least 1 postdischarge component |
Postdischarge adverse events may include any of the following patient experiences representing clinically meaningful injuries occurring after hospital discharge: new or worsening symptoms, laboratory abnormalities necessitating a change in clinical management and injuries (such as ADEs, falls, or hospital-acquired infections) attributable at least in part to hospital care. This definition was based on classifications used in prior studies that analyzed the epidemiology of postdischarge adverse events.3,4 In the research literature, readmission has been classified as an adverse event and has been measured at 30-day, 60-day, 90-day, and 6-month readmission rates from index hospitalization.
Risk of Readmission and Adverse Events
It is difficult to predict exactly which patients will be readmitted to the hospital or experience an adverse event. Certain patient populations, including older adults, the chronically ill and those hospitalized with stroke, are at greater risk in the posthospitalization period due to gaps in health care quality, transition through multiple sites of care, and increased hand offs between providers.1,3,17,31-33 Several studies identified poor functional status at hospital discharge, advanced age, psychiatric illness, and limited access to social support services as risk factors for readmission to the hospital and worse outcomes in neurologic patients.34-36 A systematic review evaluating predictors of readmission after stroke did not find risk-standardized models to compare or predict readmissions across hospitals.37
Despite the lack of standardized prediction models, older adults and those with multiple chronic illnesses make up a majority of admissions and readmissions to the inpatient neurology service. Patients with stroke are readmitted for cerebrovascular, cardiac, and noncardiac conditions such as urinary tract infection, pneumonia, and hip fracture.8,38,39
Selected Transitional Care Strategies
The following 4 transitional care strategies described have been highlighted based on the evidence from several published controlled trials showing effectiveness in reducing readmissions (Table 2).
Table 2.
Highlighted Hospital-Based Transitional Care Programs.
| Programs | Strategies | Description/Effectiveness |
|---|---|---|
| Care Transitions Intervention40-43 | Patient engagement Individualized patient record Dedicated transition provider Facilitation of communication to outpatient providers Outreach Medication reconciliation | Focuses on 4 domains of care including self management skills |
| Studied in several settings | ||
| CCT40,43 and RCT41,42 | ||
| Decreased 30-day readmission rates: ARR 4.9%,40 ARR 3.6%,41 and ARR 5.8%43 | ||
| Decreased 90-day readmission rates: ARR 5.8%41 and ARR 21.7%42 | ||
| 30-Day ED visits: ARR 3.2% (NS)40 | ||
| Transitional Care Model44-47 | Patient engagement Individualized patient record Dedicated transition provider Facilitation of communication to outpatient providers Facilitated clinical follow-up Outreach | Nurse-led program studied in geriatric patients, intensive outreach with home and telephone follow-up |
| RCT | ||
| Decreased 90-day readmission rates: ARR 16.8%44 (within 24 weeks), ARR 48.0%,45 and ARR 13%46 (within 6 weeks) | ||
| ED visits (within 24 week): NS44,47 | ||
| Adverse events (postdischarge infection) ARR 16.7% (NS)45 | ||
| Project RED48 | Patient engagement Individualized patient record Dedicated transition provider Facilitation of communication to outpatient provider Multidisciplinary team Outreach Medication reconciliation (predischarge and postdischarge) | Team-based program included pharmacist outreach and medication reconciliation |
| RCT | ||
| Decreased 30-day readmission rates: ARR 5.8% (NS) | ||
| Decreased 30-day ED visits: ARR 8.0% | ||
| Project BOOST49-52 | Patient engagement Multidisciplinary team Outreach Medication reconciliation Risk assessment | Multicenter QI program with mentored implementation |
| CCT49 and pre–post study51 | ||
| Decreased 30-day readmission rates: ARR 2%51 and ARR 5.9%49 |
Abbreviations: ARR, absolute risk reduction; CCT, clinical controlled trial (nonrandomized); ED, emergency department; NS, not significant; QI, quality improvement; RCT, randomized controlled trial; RED, Reengineered Discharge; BOOST, Better Outcomes for Older Adults Through Safe Transitions.
Care Transitions Intervention
The Care Transitions Intervention (CTI) is a multicomponent program originally developed by Eric Coleman from the University of Colorado and has been implemented at several hospital sites.40-43 Published studies included older adults admitted with stroke and chronic illnesses. The goals of the CTI are to facilitate patient engagement and promote direct patient and caregiver involvement in self-management following hospitalization including the necessary skills to be able to navigate the health care system. There are 4 pillars or domains including (1) medication management, (2) development of a personal health record that is carried from site to site, (3) close follow-up with a primary provider, and (4) the identification of “red flags” and indications that would prompt patients to contact providers. The “transition coach,” an advanced practice nurse, performs postdischarge home visits and telephone calls emphasizing patient engagement and self-management in the care of chronic diseases. The program has been studied in several different acute care settings with statistically significant reductions in 30-day readmissions conducted in managed care systems, capitated delivery systems, and Medicare fee-for-service populations.
The Transitional Care Model
The Transitional Care Model (TCM) is another nationally recognized transitional care program led by Mary Naylor at the University of Pennsylvania. The TCM includes a strategy focusing on hospital-based discharge planning and home follow-up for chronically ill high-risk older adults and has also been studied in older adults with CHF and myocardial infarction.44-47 Published studies did not specifically note whether patients had a neurologic diagnosis. A transitional care nurse (TCN) follows patients from the hospital to home, facilitates communication with outpatient providers, and performs a series of home visits and telephone follow-up calls in the posthospitalization period. The TCM emphasizes a multidisciplinary approach to patient care led by the TCN who remains in contact with other providers including physicians, nurses, social workers, discharge planners, and pharmacists. Several studies have demonstrated reduction in readmission rates at 60 and 90 days.
Project RED
Project Reengineered Discharge (RED) has been studied in the general medicine population at an urban safety net hospital and is focused on an multidisciplinary approach to patient care coordinated by a nurse discharge advocate (DA).48 The DA engages patients during the hospitalization and provides clinical information and an individualized and illustrated posthospitalization plan. Following discharge, a pharmacist performs the telephone follow-up including a medication review with direct communication to the primary outpatient provider. The initial study did not specify whether enrolled patients had a neurologic diagnosis. Project RED demonstrated significant reductions in hospital utilization, defined by combined ED visits and readmissions, within 30 days of discharge during the index hospitalization by approximately 30% among patients in the study.
Project BOOST
Project Better Outcomes for Older Adults Through Safe Transitions (BOOST) is a transitional care program supported by the Society of Hospital Medicine.49-52 This quality improvement collaborative has been implemented across the United States in different hospital settings, focusing on general medicine populations, both medical and medical–surgical patient populations. Mentors, hospitalist experts in the field of quality improvement and transitions in care, facilitate the development and implementation of a BOOST site-specific program that addresses the needs of each hospital. The BOOST toolkit includes several interventions including risk assessment, medication reconciliation, discharge checklist, and a multidisciplinary team-based approach to the discharge process. A recent study of 30 hospitals showed modest reductions in readmission rates, although only 11 hospitals provided data for the study.51
Strategies for the neurologic patients
Several studies have evaluated the effectiveness of transitional care programs targeting patients with stroke. A systematic review of 27 transitional care studies of patients with acute stroke concluded that a limited number of studies provided low-to-moderate strength evidence that interventions initiated in the hospital improved some outcomes, including reducing the number of hospital days and improving physical activity, but did not affect readmissions or mortality.34 Despite the lack of evidence that these studies decreased health care utilization or adverse events, study authors concluded that hospital-initiated strategies focusing on coordination of care were important determinants of improved health care in this patient population. Specific interventions, such as secondary stroke prevention (antithrombotic, antihypertensive, and lipid-lowering agents), screening for dysphagia, and reducing urinary catheter use in the hospital have been shown in published studies to reduce readmissions and postdischarge adverse events such as cerebrovascular accidents, pneumonia, and catheter-associated urinary tract infections.53-59 Neurohospitalists are in a position to have a direct impact on patient care beyond the hospitalization period by implementing interventions that can improve quality of care, reduce cost, and reduce the risks associated with preventable readmissions and adverse events.
Common Features of Effective Strategies
All these programs have several similarities. All the general programs and many of the stroke programs include bridging interventions with a dedicated transition provider, either a nurse or case manager as the clinical leader. There is an overriding emphasis on having an advocate facilitating coordination of care and outreach to patients following hospitalization. Neurologic patients, like general medicine populations, benefit from strategies that focus on improving communication across sites, outreach, and patient engagement.
Implementation Considerations and Cost
Description of many transitional care programs has included a time line and description of the interventions, but there is little information provided on cost, the resources needed to implement the strategy, and efforts to ensure sustainability.
Discussion
In this review, we presented a framework for characterizing transitional care strategies aimed at reducing hospital readmissions and postdischarge adverse events and highlighted 4 nationally recognized programs. Nearly, all successful transitional care strategies that have been published in the last 20 years have included bridging interventions and mostly rely on a clinical lead, a dedicated transition provider, who has contact with patients before and after discharge. Three of these strategies, the CTI, Project BOOST, and the TCM have been successfully implemented and evaluated in multiple patient populations and health care systems, and a similar intervention, Project RED, has been implemented in a safety net system. Although these strategies are relatively intensive and likely require considerable resources, there is evidence that these strategies are effective. However, information on implementation, sustainability, and cost is still lacking. More evidence is needed to draw conclusions about the impact of these particular strategies on those with acute neurologic illness.
Recommendations for the Neurohospitalist
Hospitals and neurohospitalists are now faced with a challenge of deciding what to provide for patients in the transitional period following hospitalization that will reduce readmissions and thus avoid financial penalties. The research in this area points toward the relative success with multidisciplinary, multicomponent strategies using bridging interventions and a dedicated transitions clinician. Strategies such as the CTI, TCM, Project RED, and Project BOOST have been studied and replicated across the United States. Clearly, there are differences that are inherent within each hospital network including internal factors, culture, community, and geography that will need consideration. There is no “one size fits all” strategy in transitional care. The basic elements of a successful transitional care strategy include patient engagement, use of a dedicated transitions provider, medication management (including medication reconciliation), facilitation of communication with outpatient providers, and patient outreach (Table 3). Additional disease-specific interventions for the neurology patient population may also be incorporated into a strategy including home care for disease monitoring protocols, medication adherence, symptom management protocols, and direct communication with rehabilitation programs.
Table 3.
Summary Recommendations for the Neurohospitalist.
| Obtain data on 30-day readmission rates (all cause and disease- or unit-specific rates) |
| Consider your hospital’s quality improvement and patient safety infrastructure—electronic health record, prior experience with quality improvement initiatives |
| Create a interdisciplinary team and find champions |
| Identify outcomes to measure (30-day readmission rates, adverse drug events, or medication errors) |
| Implement a bundled (multicomponent) strategy that includes patient engagement, transitions provider, medication reconciliation, facilitation of communication, and patient outreach |
| Incorporate disease-specific interventions (secondary stroke prevention and dysphagia screening) |
Neurohospitalists, both as primary providers and as consultants, are uniquely positioned and provide expertise on efforts that improve transitional care for a broad range of patients. For example, neurohospitalists could include lead-specific initiatives such as screening for delirium and dysphagia in patients with cerebrovascular and neurologic diseases or could partner with medicine hospitalists on institution-wide efforts such as the broader transitional care strategies described previously.60-62 As consultants, neurohospitalists can make specific evidence-based recommendations that reduce the risk of readmission and other adverse events, such as secondary stroke prevention measures.
In light of the published research on transitional care and the importance of improving quality of care and addressing preventable readmissions, there are several practical recommendations that should be addressed for all patients admitted by the neurohospitalist:
Patient engagement, including counseling on medication management, red flags, disease-specific management strategies, and resources for addressing postdischarge issues.
Communication with outpatient providers, including rehabilitation and skilled nursing facility staff to ensure appropriate follow-up, medication reconciliation, and management.
Outreach, through either a follow-up telephone call service or home visit, if applicable, to ensure a safe transition.
Footnotes
Authors’ Note: All statements expressed in this work are those of the authors and should not in any way be construed as official opinions or positions of the University of California, San Francisco, AHRQ, or the US Department of Health and Human Services.
Declaration of Conflicting Interests: The authors declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article. Stephanie Rennke is a consultant for the Society of Hospital Medicine’s Project BOOST.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported in part by funding from the Agency for Healthcare Research and Quality (AHRQ), US Department of Health and Human Services (contract no. HHSA-290-2007-10062I).
References
- 1. Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med. 2009;360 (14):1418–1428. [DOI] [PubMed] [Google Scholar]
- 2. Jha AK, Joynt KE, Orav EJ, Epstein AM. The long-term effect of premier pay for performance on patient outcomes. N Engl J Med. 2012;366 (17):1606–1615. [DOI] [PubMed] [Google Scholar]
- 3. Forster AJ, Murff HJ, Peterson JF, Gandhi TK, Bates DW. The incidence and severity of adverse events affecting patients after discharge from the hospital. Ann Intern Med. 2003;138 (3):161–167. [DOI] [PubMed] [Google Scholar]
- 4. Forster AJ, Clark HD, Menard A, et al. Adverse events among medical patients after discharge from hospital. CMAJ. 2004;170 (3):345–349. [PMC free article] [PubMed] [Google Scholar]
- 5. Mestieg M, Helbostad JL, Sletvold O, Røsstad T, Saltvedt I. Unwanted incidents during transition of geriatric patients from hospital to home: a prospective observation study. BMC Health Serv Res. 2010;10:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Budnitz DS, Lovegrove MC, Shehab N, Richards CL. Emergency hospitalizations for adverse drug events in older Americans. N Engl J Med. 2011;365 (21):2002–2012. [DOI] [PubMed] [Google Scholar]
- 7. Samsa GP, Bian J, Lipscomb J, Matchar DB. Epidemiology of recurrent cerebral infarction: a Medicare claims-based comparison of first and recurrent strokes on 2-year survival and cost. Stroke. 1999;30 (2):338–349. [DOI] [PubMed] [Google Scholar]
- 8. Fonarow GC, Smith EE, Reeves MJ, et al. Hospital-level variation in mortality and rehospitalization for Medicare beneficiaries with acute ischemic stroke. Stroke. 2011;42 (1):159–166. [DOI] [PubMed] [Google Scholar]
- 9. Douglas VC, Scott BJ, Berg G, Freeman WD, Josephson SA. Effect of a neurohospitalist service on outcomes at an academic medical center. Neurology. 2012;79 (10):988–994. [DOI] [PubMed] [Google Scholar]
- 10. Coleman EA, Boult C. Improving the quality of transitional care for persons with complex care needs. J Am Geriatr Soc. 2003;51 (4):556–557. [DOI] [PubMed] [Google Scholar]
- 11. Naylor M, Keating SA. Transitional care. Am J Nurs. 2008;108 (9 suppl):58–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. U.S. Department of Health & Human Services. Hospital Compare. www.hospitalcompare.hhs.gov Accessed June 15, 2013.
- 13. Josephson SA, Johnston SC, Hauser SL. The neurologic revolving door: time to pay attention to readmissions. Ann Neurol. 2013;73 (5):A5–A6. [DOI] [PubMed] [Google Scholar]
- 14. Rau J. Armed with bigger fines, Medicare to punish 2,225 hospitals for excess readmissions. Kaiser Health News. August 02, 2013 http://www.kaiserhealthnews.org/Stories/2013/August/02/readmission-penalties-medicare-hospitals-year-two.aspx Page 1. Accessed August 4, 2013.
- 15. Partnership for Patients, Center for Medicare and Medicaid Innovation. http://www.innovations.cms.gov/initiatives/Partnership-for-Patients/index.html Accessed July 17, 2013.
- 16. Hansen LO, Young RS, Hinami K, Leung A, Williams MV. Interventions to reduce 30-day rehospitalization: a systematic review. Ann Intern Med. 2011;155 (8):520–528. [DOI] [PubMed] [Google Scholar]
- 17. Naylor MD, Aiken LH, Kurtzman ET, Olds DM, Hirschman KB. The importance of transitional care in achieving health reform. Health Aff (Millwood). 2011;30 (4):746–754. [DOI] [PubMed] [Google Scholar]
- 18. Shekelle PG, Wachter RM, Pronovost P. Methods. In: Shekelle PG, Wachter RM, Pronovost PJ, Schoelles K, McDonald KM, Dy SM, Shojania K, Reston J, Berger Z, Johnsen B, Larkin JW, Lucas S, Martinez K, Motala A, Newberry SJ, Noble M, Pfoh E, Ranji SR, Rennke S, Schmidt E, Shanman R, Sullivan N, Sun F, Tipton K, Treadwell JR, Tsou A, Vaiana ME, Weaver SJ, Wilson R, Winters BD, eds. Making Health Care Safer II: An Updated Critical Analysis of the Evidence for Patient Safety Practices. Comparative Effectiveness Review. (Prepared by the Southern California-RAND Evidence-based Practice Center under Contract No. HHSA290200710062I.) Rockville, MD: Agency for Healthcare Research and Quality; 2013:chapter 2 http://www.ahrq.gov/research/findings/evidence-based-reports/ptsafetysum.html Accessed July 20, 2013. [Google Scholar]
- 19. Hesselink G, Schoonhoven L, Barach P, et al. Improving patient handovers from hospital to primary care: a systematic review. Ann Intern Med. 2012;157 (6):417–428. [DOI] [PubMed] [Google Scholar]
- 20. van Walraven C, Jennings A, Taljaard M, et al. Incidence of potentially avoidable urgent readmissions and their relation to all-cause urgent readmissions. CMAJ. 2011;183 (14):E1067–E1072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Joynt KE, Orav EJ, Jha AK. Thirty-day readmission rates for Medicare beneficiaries by race and site of care. JAMA. 2011;305 (7):675–681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Philbin EF, Dec GW, Jenkins PL, DiSalvo TG. Socioeconomic status as an independent risk factor for hospital readmission for heart failure. Am J Cardiol. 2001;87 (12):1367–1371. [DOI] [PubMed] [Google Scholar]
- 23. Joynt KE, Jha AK. Thirty-day readmissions—truth and consequences. N Engl J Med. 2012;366 (15):1366–1369. [DOI] [PubMed] [Google Scholar]
- 24. Nahab F, Takesaka J, Mailyan E, et al. Avoidable 30-day readmissions among patients with stroke and other cerebrovascular disease. Neurohospitalist. 2012;2 (1):7–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Gerhardt G, Yemane A, Hickman P, et al. Medicare readmission rates showed meaningful decline in 2012. Medicare Mediaid Res Rev. 2013;3(2):E1–E11 http://www.cms.gov/mmrr/Briefs/B2013/mmrr-2013-003-02-b01.html Accessed July 24, 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Chiu WK, Newcomer R. A systematic review of nurse-assisted case management to improve hospital discharge transition outcomes for the elderly. Prof Case Manag. 2007;12 (6):330–336. [DOI] [PubMed] [Google Scholar]
- 27. Mistiaen P, Francke AL, Poot E. Interventions aimed at reducing problems in adult patients discharged from hospital to home: a systematic meta-review. BMC Health Serv Res. 2007;7:47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Parker SG, Peet SM, McPherson A, et al. A systematic review of discharge arrangements for older people. Health Technol Assess. 2002;6 (4):1–183. [DOI] [PubMed] [Google Scholar]
- 29. Richards S, Coast J. Interventions to improve access to health and social care after discharge from hospital: a systematic review. J Health Serv Res Policy. 2003;8 (3):171–179. [DOI] [PubMed] [Google Scholar]
- 30. Shepperd S, Lannin NA, Clemson LM, McCluskey A, Cameron ID, Barras SL. Discharge planning from hospital to home. Cochrane Database Syst Rev. 2013;1:CD000313 doi:10.1002/14651858.CD000313.pub4. [DOI] [PubMed] [Google Scholar]
- 31. Schoen C, Osborn R, How SK, Doty MM, Peugh J. In chronic condition: experiences of patients with complex health care needs, in eight countries. Health Aff (Millwood). 2009;28(1):w1–w16. [DOI] [PubMed] [Google Scholar]
- 32. Allaudeen N, Vidyarthi A, Maselli J, Auerbach A. Redefining readmission risk factors for general medicine patients. J Hosp Med. 2011;6 (2):54–60. [DOI] [PubMed] [Google Scholar]
- 33. Feigenbaum P, Neuwirth E, Trowbridge L, et al. Factors contributing to all-cause 30-day readmissions: a structured case series across 18 hospitals. Med Care. 2012;50 (7):599–605. [DOI] [PubMed] [Google Scholar]
- 34. Prvu Bettger J, Alexander KP, Dolor RJ, et al. Transitional care after hospitalization for acute stroke or myocardial infarction: a systematic review. Ann Intern Med. 2012;157 (6):407–416. [DOI] [PubMed] [Google Scholar]
- 35. Tseng MC, Lin HJ. Readmission after hospitalization for stroke in Taiwan: results from a national sample. J Neurol Sci. 2009;284 (1-2):52–55. [DOI] [PubMed] [Google Scholar]
- 36. Wilson SJ, Kincade P, Saling MM, Bladin PF. Patient readmission and support utilization following anterior temporal lobectomy. Seizure. 1999;8 (1):20–25. [DOI] [PubMed] [Google Scholar]
- 37. Lichtman JH, Leifheit-Limson EC, Jones SB, et al. Predictors of hospital readmission after stroke: a systematic review. Stroke. 2010;41 (11):2525–2533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Lakshminarayan K, Schissel C, Anderson DC, et al. Five-year rehospitalization outcomes in a cohort of patients with acute ischemic stroke: Medicare linkage study. Stroke. 2011;42 (6):1556–1562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Bhattacharya P, Khanal D, Madhavan R, Chaturvedi S. Why do ischemic stroke and transient ischemic attack patients get readmitted? J Neurol Sci. 2011;307 (1-2):50–54. [DOI] [PubMed] [Google Scholar]
- 40. Coleman EA, Smith JD, Frank JC, Min SJ, Parry C, Kramer AM. Preparing patients and caregivers to participate in care delivered across settings: the Care Transitions Intervention. J Am Ger Soc. 2004;52 (11):1817–1825. [DOI] [PubMed] [Google Scholar]
- 41. Coleman EA, Parry C, Chalmers S, Min SJ. The Care Transitions Intervention: results of a randomized controlled trial. Arch Intern Med. 2006;166 (17):1822–1828. [DOI] [PubMed] [Google Scholar]
- 42. Parry C, Min SJ, Chugh A, Chalmers S, Coleman EA. Further application of the Care Transitions Intervention: results of a randomized controlled trial conducted in a fee-for-service setting. Home Health Care Serv Q. 2009;28 (2-3):84–99. [DOI] [PubMed] [Google Scholar]
- 43. Voss R, Gardner R, Baier R, Butterfield K, Lehrman S, Gravenstein S. The Care Transitions Intervention: translating from efficacy to effectiveness. Arch Intern Med. 2011;171 (14):1232–1237. [DOI] [PubMed] [Google Scholar]
- 44. Naylor MD, Brooten D, Campbell R, et al. Comprehensive discharge planning and home follow-up of hospitalized elders: a randomized clinical trial. JAMA. 1999;281 (7):613–620. [DOI] [PubMed] [Google Scholar]
- 45. Naylor MD. Comprehensive discharge planning for hospitalized elderly: a pilot study. Nurs Res. 1990;39 (3):156–161. [PubMed] [Google Scholar]
- 46. Naylor M, Brooten D, Jones R, Lavizzo-Mourey R, Mezey M, Pauly M. Comprehensive discharge planning for the hospitalized elderly: a randomized clinical trial. Ann Intern Med. 1994;120 (12):999–1006. [DOI] [PubMed] [Google Scholar]
- 47. Naylor MD, Brooten DA, Campbell RL, Maislin G, McCauley KM, Schwartz JS. Transitional care of older adults hospitalized with heart failure: a randomized, controlled trial. J Am Geriatr Soc. 2004;52 (5):675–684. [DOI] [PubMed] [Google Scholar]
- 48. Jack BW, Chetty VK, Anthony D, et al. A reengineered hospital discharge program to decrease rehospitalization: a randomized trial. Ann Intern Med. 2009;150 (3):178–187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Wilkinson ST, Pal A, Couldry RJ. Impacting readmission rates and patient satisfaction: results of a discharge pharmacist pilot program. Hosp Pharm. 2011;46 (11):876–883. [Google Scholar]
- 50. Maynard GA, Budnitz TL, Nickel WK, et al. 2011 John M. Eisenberg Patient Safety and Quality Awards. Mentored implementation: building leaders and achieving results through a collaborative improvement model. Innovation in patient safety and quality at the national level. Jt Comm J Qual Patient Saf. 2012;38 (7):301–310. [DOI] [PubMed] [Google Scholar]
- 51. Hansen LO, Greenwald JL, Budnitz T, et al. Project BOOST: effectiveness of a multihospital effort to reduce rehospitalization. J Hosp Med. 2013;8 (8):421–427. [DOI] [PubMed] [Google Scholar]
- 52. Society of Hospital Medicine, Project BOOST. http://www.hospitalmedicine.org Accessed January 5, 2014.
- 53. Rahiman A, Saver JL, Porter V, et al. In-hospital initiation of secondary prevention is associated with improved vascular outcomes at 3 months. J Stroke Cerebrovasc Dis. 2008;17 (1):5–8. [DOI] [PubMed] [Google Scholar]
- 54. Amarenco P, Goldstein LB, Messig M, et al. Relative and cumulative effects of lipid and blood pressure control in the stroke prevention by aggressive reduction in cholesterol levels trial. Stroke. 2009;40 (7):2486–2492. [DOI] [PubMed] [Google Scholar]
- 55. Schwamm LH, Fonarow GC, Reeves MJ, et al. Get With the Guidelines-Stroke is associated with sustained improvement in care for patients hospitalized with acute stroke or transient ischemic attack. Circulation. 2009:119 (1):107–115. [DOI] [PubMed] [Google Scholar]
- 56. Titsworth WL, Abram J, Fullerton A, et al. Prospective quality initiative to maximize dysphagia screening reduces hospital-acquired pneumonia prevalence in patients with stroke. Stroke. 2013;44 (11):3154–3160. [DOI] [PubMed] [Google Scholar]
- 57. Hinchey JA, Shepard T, Furie K, et al. Formal dysphagia screening protocols prevent pneumonia. Stroke. 2005;36 (9):1972–1976. [DOI] [PubMed] [Google Scholar]
- 58. Meddings J, Krein SL, Fakih MG, et al. Reducing unnecessary urinary catheter use and other strategies to prevent catheter-associated urinary tract infections: brief update review. In: Shekelle PG, Wachter RM, Pronovost PJ, Schoelles K, McDonald KM, Dy SM, Shojania K, Reston J, Berger Z, Johnsen B, Larkin JW, Lucas S, Martinez K, Motala A, Newberry SJ, Noble M, Pfoh E, Ranji SR, Rennke S, Schmidt E, Shanman R, Sullivan N, Sun F, Tipton K, Treadwell JR, Tsou A, Vaiana ME, Weaver SJ, Wilson R, Winters BD, eds. Making Health Care Safer II: An Updated Critical Analysis of the Evidence for Patient Safety Practices. Comparative Effectiveness Review No. 211. (Prepared by the Southern California-RAND Evidence-based Practice Center under Contract No. 290-2007-10062-I.) AHRQ Publication No. 13-E001-EF Rockville, MD: Agency for Healthcare Research and Quality; 2013:chapter 9 www.ahrq.gov/research/findings/evidence-based-reports/ptsafetyuptp.html Accessed July 12, 2013. [Google Scholar]
- 59. Douglas VC, Hessler CS, Dhaliwal G, et al. The AWOL tool: derivation and validation of a delirium prediction rule. J Hosp Med. 2013;8 (9):493–499. [DOI] [PubMed] [Google Scholar]
- 60. Kertscher B, Speyer R, Palmieri M, Plant C. Bedside screening to detect oropharyngeal dysphagia in patients with neurological disorders: an updated systematic review. 2014:29 (2):204–212. [DOI] [PubMed] [Google Scholar]
- 61. Schnipper JL, Kirwin JL, Cotugno MC, et al. Role of pharmacist counseling in preventing adverse drug events after hospitalization. Arch Intern Med. 2006;166 (5):565–571. [DOI] [PubMed] [Google Scholar]
- 62. Levetan CS. Effect of hyperglycemia on stroke outcomes. Endocr Pract. 2004;10 (suppl 2):34–39. [DOI] [PubMed] [Google Scholar]