Abstract
Computerized provider order entry (CPOE) systems allow physicians to prescribe patient services electronically. In hospitals, CPOE essentially eliminates the need for handwritten paper orders and achieves cost savings through increased efficiency. The purpose of this research study was to examine the benefits of and barriers to CPOE adoption in hospitals to determine the effects on medical errors and adverse drug events (ADEs) and examine cost and savings associated with the implementation of this newly mandated technology. This study followed a methodology using the basic principles of a systematic review and referenced 50 sources. CPOE systems in hospitals were found to be capable of reducing medical errors and ADEs, especially when CPOE systems are bundled with clinical decision support systems designed to alert physicians and other healthcare providers of pending lab or medical errors. However, CPOE systems face major barriers associated with adoption in a hospital system, mainly high implementation costs and physicians’ resistance to change.
Keywords: computerized provider order entry, medical errors, adverse drug events, hospitals, cost, meaningful use
Introduction
The Health Information Technology for Economic and Clinical Health (HITECH) Act, part of the American Recovery and Reinvestment Act (ARRA), was put into place in 2009.1 The goals of using health information technology (HIT) are to improve patient care, decrease medical errors, decrease costs, and advance the health of the population.2 Once the standards for the meaningful use of a certified electronic health record (EHR) have been met, providers of Medicare and Medicaid services would be eligible to receive financial incentives. Meaningful use has been described as using certified EHR technology in a “meaningful way” with the purpose of improving patient care.3 The EHR is an electronic record of patient health information in the healthcare delivery system that connects organizations such as hospitals and medical clinics to transmit and exchange health information.4 After the entity can demonstrate meaningful use, the Centers for Medicare and Medicaid Services (CMS) pays $44,000 for Medicare and $63,750 for Medicaid to any eligible provider (EP), eligible hospitals, or critical access hospital for the adoption and implementation of EHRs. Hospital payments have been based on a $2 million base amount.5 To ensure that a facility receives the financial incentives, 14 core objectives and five menu objectives must be met to demonstrate meaningful use.6 As of March 2012, payments to eligible hospitals totaled about $3 billion. Eighty-five percent of hospitals surveyed in a study reported that they planned to take advantage of meaningful use payments by 2015.7
The Meaningful Use program has three stages. Requirements increase at each stage, while incentive amounts decrease.8 All three stages involve the use of a computerized provider order entry (CPOE) system. CPOE systems allow physicians to prescribe patient services electronically. In the first stage, CPOE needs to be utilized at least 30 percent of the time with eligible patients. Over the course of the next two stages, the percentage increases up to 80 percent of all eligible patients.9 CPOE utilization in stage 1 has been designed to deal with the idea that preventable medical errors start as soon as the provider handwrites a prescription. Under the meaningful use mandate, which required developing and implementing an operational CPOE system, 57 percent of primary care physicians reported having an EHR system by the end of 2011.10
Approximately 200,000 people die every year in the United States as a result of preventable medical errors.11 The majority of medical mistakes happen when the physician orders services and prescriptions for the patient. Physicians using a paper prescription pad often do not have legible handwriting, and prescriptions often are not able to be read by the individuals who process and prepare them for the patient.12 Another 770,000 patient injuries and deaths are due to adverse drug events (ADEs).13 If the pharmacist is not able to read a prescription handwritten by the physician, the patient is at risk of ADEs. ADEs are negative reactions to drugs, which may result in longer hospital stays, increased medical costs, permanent disability, and even death.14 A CPOE system may be the solution to decrease the number of ADEs in a hospital, enhance patient safety, and decrease preventable medical errors.15 In addition, CPOE, a software system designed to be utilized in a hospital, has the ability to resolve other problems in the hospital setting, such as by removing abbreviations and acronyms and increasing order speed through the use of electronically ordered services and prescriptions.16
Many factors other than practice size must be considered when examining CPOE adoption rates. Hospitals that have a higher bed capacity are more likely to adopt CPOE than smaller hospitals because increased funds are available to spend.17
The US government has been offering financial incentives for hospitals to adopt EHRs, which may help offset the cost of implementing a CPOE system.18 Hospitals that do not comply with the meaningful use mandate will begin to receive lower reimbursement rates as a penalty.19 The HITECH Act will allow penalties to be implemented in 2015.20 If Medicare EPs and hospitals do not adopt EHRs and successfully demonstrate meaningful use by 2015, the fee schedule amounts for covered professional services will be decreased by 1 percent each year up to 5 percent in 2020.21
The purpose of this research study was to examine the benefits of and barriers to CPOE adoption in hospitals to determine the effects on medical errors and ADEs and to examine cost and savings associated with the implementation of this newly mandated technology.
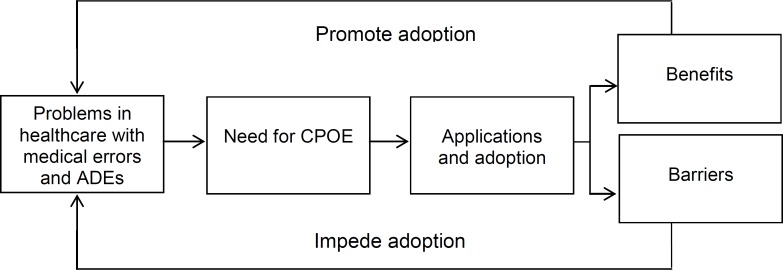
The research approach of this review followed the steps and research framework utilized by Yao, Chu, and Li.22 Figure 1 displays the process of CPOE adoption in healthcare. To research how CPOE systems can help improve the prescription process in the hospital, the first requirement is to identify the existing problems with CPOE adoption and the benefits of its adoption in the hospital. Solutions can then be identified to resolve or partially resolve these challenges. The use of the conceptual framework of this study was appropriate because it addressed the process of adopting and utilizing any HIT system.23 The technology adoption process works much like any project development system in that it is circular; it starts with problems and issues, and needs are determined before a solution is created and initialized. In this case, the solution is the utilization of a CPOE system. After the CPOE system has been adopted, the process includes an assessment of the benefits of and barriers to the use of CPOE, and the process starts over so that the barriers can be addressed and the benefits assessed (see Figure 1). The use of this conceptual framework in the present study is applicable because the focus of both studies is to show how new technologies can be applied to healthcare settings to improve the care of patients. In addition, this approach has been successfully replicated in previous studies, supporting its internal validity.24, 25, 26
Figure 1.
Research Framework for the Study of CPOE Adoption in Healthcare
ADE, adverse drug event; CPOE, computerized provider order entry.
Source: Yao, W., C. H. Chu, and Z. Li. “The Use of RFID in Healthcare: Benefits and Barriers.” Proceedings of the 2010 IEEE International Conference on RFID-Technology and Applications (2010): 128–34.
Methods
The methodology for the examination of the benefits of and barriers to CPOE adoption followed the basic principles of a systematic review. The study was conducted in three stages: (1) identifying the literature and collecting the data, (2) analyzing and evaluating the literature found, and (3) categorizing the literature.
Step 1: Literature Identification and Collection
The literature review and review of case studies was performed in January to May 2013 and September 2013 to March 2014. The Academic Search Premier, PubMed, ProQuest, ScienceDirect, and Google Scholar electronic databases were searched for the terms “CPOE” OR “Computerized Physician Order Entry” OR “Electronic Prescribing” AND “Medical Errors” OR “ADEs” OR “Adoption” OR “Implementation” AND “Meaningful Use” OR “HITECH.” Reputable websites from the Agency for Healthcare Research and Quality, Health Affairs, and CMS were also used. Citations and abstracts identified in the search were also assessed to identify relevant articles.
Step 2: Literature Analysis
Literature was selected for review on the basis of governmental acts, meaningful use, and benefits of and barriers to CPOE implementation. Inclusion and exclusion criteria were as follows: Only articles published from 2005 to 2014 were utilized. The search was restricted to sources attainable as full texts and written in the English language. Only primary and secondary data from articles, reports, reviews, and research studies written in the United States were included in this research study.
The methodology and results of the identified texts were analyzed, and key papers were identified and included within the research query. From a total of 154 references found, 51 citations were used for this study. The results were structured with subheadings that described the benefits of and barriers to implementation and adoption of CPOE systems. The literature search was conducted by three reviewers (K.C., R.H., and M.C.) and was validated by one (A.C.), who acted as the second reader and also double-checked that references met the research study inclusion criteria.
Step 3: Literature Categorization
Abstracts of the articles were reviewed first to determine the relevancy of the data to the study. If academic articles and studies were found to be appropriate from the abstract reviews, the data were analyzed and categories were generated on the basis of the findings. The findings are presented in the following section under the subheadings of benefits of and barriers to CPOE adoption.
Results
Benefits of CPOE Adoption
Multiple benefits can be gained from adopting and implementing CPOE systems. The benefits for patients, as a hospital transitions from paper charts to CPOE systems, are of the most importance. One of the main purposes of switching from paper to CPOE is to increase the accessibility of the patient's medical records; the switch to CPOE also creates the ability for a physician to work off-site from home or another office and still have access to information about a patient's past visits.27 Devine et al. reported that switching from handwritten paper prescriptions to electronic prescribing resulted in an estimated 70 percent reduction in medication errors.28 (See Table 1.) The same study identified additional benefits, besides medical error reduction, for an independent medical group. These benefits included reduction in prescription ordering by the physicians, increased coordination of care, and complete support by the organization to help ensure the successful implementation of the new system. Another study of CPOE that measured preimplementation data from February to July 2007 and postimplementation data from March to May 2008 found that the average time from the moment a physician ordered a service to the moment the patient received the service decreased from 100 to 64 minutes.29 (See Table 1.)
Table 1.
CPOE System Implementation and Adoption Outcomes
| Author(s) and Year | Study Design | Outcome |
|---|---|---|
| Devine et al. (2010) | Pretest-posttest study of CPOE implementation | 70 percent reduction in medication errors |
| Mattison et al. (2010) | Pretest-posttest study of CPOE implementation | Significant decrease of inappropriate medication orders |
| Gabow and Mehler (2011) | Postimplementation study of CPOE | Out of 112 medical centers, Denver Health was rated first and had the lowest mortality ratio. |
| Cartmill et al. (2012) | Pretest-posttest study of CPOE implementation | Average time from ordering to administration decreased from 100 to 64 minutes. |
| Magid et al. (2012) | Posttest study of CPOE implementation | Decrease in duplicate orders by 84.8 percent |
| Jozefczyk et al. (2013) | Pretest-posttest study of CPOE implementation | Increase in orders with no opportunity for medication errors from 42 percent to 98 percent |
| Zimlichman et al. (2013) | Posttest study of CPOE with CDSSs | ADE costs that were avoided ranged from $7 to $16 million. |
ADE, adverse drug event; CDSS, clinical decision support system; CPOE, computerized provider order entry.
Sources: Cartmill, R. S., J. M. Walker, M. A. Blosky, R. L. Brown, S. Djurkovic, D. B. Dunham, D. Gardill, M. T. Haupt, D. Parry, T. B. Wetterneck, et al. “Impact of Electronic Order Management on the Timeliness of Antibiotic Administration in Critical Care Patients.” International Journal of Medical Informatics 81, no. 11 (2012): 782–91.
Devine, E. B., E. C. Williams, D. P. Martin, D. F. Sittig, P. Tarczy-Hornoch, T. H. Payne, and S. D. Sullivan. “Prescriber and Staff Perceptions of an Electronic Prescribing System in Primary Care: A Qualitative Assessment.” BMC Medical Informatics and Decision Making 10, no. 72 (2010): 72–83.
Gabow, P. A., and P. S. Mehler. “A Broad and Structured Approach to Improving Patient Safety and Quality: Lessons from Denver Health.” Health Affairs 30, no. 4 (2011): 612–18.
Jozefczyk, K. G., W. K. Kennedy, M. J. Lin, J. Achatz, M. D. Glass, W. S. Eidam, and M. J. Melroy. “Computerized Prescriber Order Entry and Opportunities for Medication Errors: Comparison to Tradition Paper-based Order Entry.” Journal of Pharmacy Practice 26, no. 4 (2013): 434–37.
Magid, S., C. Forrer, and S. Shaha. “Duplicate Orders: An Unintended Consequence of Computerized Provider/Physician Order Entry (CPOE) Implementation: Analysis and Mitigation Strategies.” Applied Clinical Informatics 3, no. 4 (2012): 377–91.
Mattison, M. L., K. A. Afonso, L. H. Ngo, and K. J. Mukamal. “Preventing Potentially Inappropriate Medication Use in Hospitalized Older Patients with a Computerized Provider Order Entry Warning System.” Archives of Internal Medicine 170, no. 15 (2010): 1331–36.
Zimlichman, E., C. Keohane, C. Franz, W. L. Everett, D. L. Seger, C. Yoon, A. A. Leung, B. Cadet, M. Coffey, N. E. Kaufman, and D. W. Bates. “Return on Investment for Vendor Computerized Physician Order Entry in Four Community Hospitals: The Importance of Decision Support.” Joint Commission Journal on Quality and Patient Safety/Joint Commission Resources 39, no. 7 (2013): 312–18.
CPOE Use for Prevention of Medical Errors
Individual hospitals can tailor CPOE systems to fit their needs. Once an organization has determined the main problems that need to be addressed, whether they are the needs of a certain age group or increased medical errors that occur during certain procedures, the healthcare setting can implement a system within the CPOE system to decrease the problems. For example, a 2004 study looked at a Massachusetts medical center that was experiencing problems with potentially inappropriate medications given to older patients. Programmers were hired to institute a program within the CPOE that would alert physicians as soon as a patient's medication order was placed.30 The researchers found that the alert system managed to prevent a large number of inappropriate medication orders for the older patients. Additionally, the CPOE system was found to be successful in preventing medical errors at the facility.31 (See Table 1.)
Because preventable medical errors and ADEs continue to exist and have increased from 98,000 reported cases in 2000 to 210,000 cases in 2013, it is crucial for safety that hospitals implement a CPOE system to be utilized by their clinical staff and providers.32 A 2012 study estimated that utilizing a CPOE system could potentially reduce medical errors by as much as 48 percent.33 CPOE has been around since the 1970s, but only recently has it become more popular in the wake of the financial incentives and the HITECH mandate, and it has been found to be very effective in hospital facilities. In a 2013 study, the Institute for Healthcare Improvement and the Commonwealth Fund reported that 34 percent of hospitals have adopted and implemented CPOE, with a 12.5 percent reduction in medication errors resulting from using CPOE to process medication orders.34 (See Table 1.)
CPOE System Use for Functionality
CPOE systems can also coexist with clinical decision support systems (CDSSs). CDSSs offer additional functions for the provider to use, such as drug interaction checks, drug allergy checks, and prompts for the provider about when to order a service for a patient.35 (See Table 2.)
Table 2.
Benefits of CPOE Implementation
| Benefit | Details | Citation |
|---|---|---|
| Medical error reduction | Meta-analysis study in 2008 estimated 12.5 percent reduction in medication errors, or about 17.4 million medication errors averted in the United States in one year by using CPOE. | Radley et al. (2013) |
| Prescribing errors decreased 91 percent with implementation of CPOE. | Aronsky et al. (2007) | |
| Cost reduction | Brigham and Women's Hospital saved $28 million over the course of 10 years by reducing medical errors and ADEs. | Kaushal et al. (2006) |
| CDSS integration | Alert systems prevented a significant amount of potentially inappropriate medication orders, with the number of inappropriate orders dropping by 20 to 30 percent. | Mattison et al. (2010) |
| Drug interaction checks, drug allergy checks, and prompts for the provider about when to order a service for a patient reduced ADEs 7 to 10 times out of every 100 hospital admissions. | Kaushal and Bates (2013) | |
| CPOE with CDSSs decreased prescribing errors or ADEs as much as 55 to 86 percent. | Bates (2010); Georgiou et al. (2013) | |
| Duplicate test check | Physicians have instant access to their patients’ EHRs and their prior test results. | Callen et al. (2006) |
| Checking for tests that had been performed saved $92,000 per year. | Levick et al. (2013) | |
| Once a test has been selected, alerts let the physician know if that patient has previously had the test done. | Baron and Dighe (2011) | |
| Interruptive/nonint erruptive pop-ups | Interruptive alerts only pop up for serious issues, whereas noninterruptive alerts pop up for issues that are not crucial. | Baron and Dighe (2011) |
ADE, adverse drug event; CDSS, clinical decision support system; CPOE, computerized provider order entry.
Sources: Aronsky, D., P. E. Johnston, G. Jenkins, L. R. Waitman, D. W. Frelix, I. Jones, and N. R. Patel. “The Effect of Implementing Computerized Provider Order Entry on Medication Prescribing Errors in an Emergency Department.” AMIA Annual Symposium Proceedings (2007): 863.
Baron, J. M., and A. S. Dighe. “Computerized Provider Order Entry in the Clinical Laboratory.” Journal of Pathology Informatics 2, no. 35 (2011). Available at http://www.jpathinformatics.org/text.asp?2011/2/1/35/83740 (accessed November 15, 2013).
Bates, D. W. “CPOE and Clinical Decision Support in Hospitals: Getting the Benefits.” Archives of Internal Medicine 170, no. 17 (2010): 1583–85.
Callen, J. L., J. L. Westbrook, and J. Braithwaite. “The Effect of Physicians’ Long-Term Use of CPOE on Their Test Management Work Practices.” Journal of the American Medical Informatics Association 13, no. 6 (2006): 643–52.
Georgiou, A., M. Prgomet, R. Paoloni, N. Creswick, A. Hordern, S. Walter, and J. Westbrook. “The Effect of Computerized Provider Order Entry Systems on Clinical Care and Work Processes in Emergency Departments: A Systematic Review of the Quantitative Literature.” Annals of Emergency Medicine 61, no. 6 (2013): 644–53.
Kaushal, R., and D. W. Bates. “Computerized Physician Order Entry (CPOE) with Clinical Decision Support Systems (CDSS).” Agency for Healthcare Research and Quality. 2013. Available at http://psnet.ahrq.gov/primer.aspx?primerID=6 (accessed January 27, 2014).
Kaushal, R., A. K. Jha, C. Franz, J. Glaser, K. D. Shetty, T. Jaggi, B. Middleton, G. J. Kuperman, R. Khorasani, M. Tanasijevic, D. W. Bates, and Brigham and Women's Hospital CPOE Working Group. “Return on Investment for a Computerized Physician Order Entry System.” Journal of the American Medical Informatics Association 13, no. 3 (2006): 261–66.
Levick, D. L., G. Stern, C. D. Meyerhoefer, A. Levick, and D. Pucklavage. “Reducing Unnecessary Testing in a CPOE System through Implementation of a Targeted CDS Intervention.” BMC Medical Informatics and Decision Making 13, no. 43 (2013).
Mattison, M. L., K. A. Afonso, L. H. Ngo, and K. J. Mukamal. “Preventing Potentially Inappropriate Medication Use in Hospitalized Older Patients with a Computerized Provider Order Entry Warning System.” Archives of Internal Medicine 170, no. 15 (2010): 1331–36.
Radley, D. C., M. R. Wasserman, L. E. Olsho, S. J. Shoemaker, M. D. Spranca, and B. Bradshaw. “Reduction in Medication Errors in Hospitals Due to Adoption of Computerized Provider Order Entry Systems.” Journal of the American Medical Informatics Association 20, no. 3 (2013): 470–76.
CPOE Use and Cost Savings
Jha et al. estimated that $8 billion was wasted in 2004 because of patients’ receiving duplicate tests.36 Patients who are continuously in and out of hospitals often do not realize that duplicate tests have been performed. Reducing healthcare costs to the patient and hospital is just one of the many perks that a CPOE system can provide. By utilizing a CPOE system, the ordering physician can have instant access to a patient's EHR and all of the patient's prior test results.37 (See Table 2.) CPOE systems have also been cost effective, with reports of cost savings due to avoided ADEs ranging from $7 to $16 million and annual cost savings of $92,000 due to a reduction in tests performed.38 Brigham and Women's Hospital spent $11.8 million to adopt and implement a CPOE system. Despite the significant cost, the CPOE system managed to save the hospital more than $28 million over the course of 10 years.39 (See Table 2.)
According to Baron and Dighe, interruptive or noninterruptive pop-up alerts can be installed within a CPOE system to decrease unnecessary testing.40 The same authors also reported that pop-ups can be used to inform a physician if a requested test has been previously performed. Interruptive pop-ups halt the physician from proceeding with the order, whereas noninterruptive pop-ups inform the physician but do not prevent the physician from placing an order. (See Table 2.)
Barriers to CPOE Adoption
The reality of CPOE implementation is that it does have its fair share of problems to overcome; some problems include system interoperability, faulty programming, and system crashes. However, the main barrier to implementing CPOE has been cost. In 2005, a study of CPOE implementation reported that costs could range from a “low” cost scenario of $1.3 million for implementation of the system in critical access hospitals, $2.0 million for rural referral hospitals, and $1.9 million for urban hospitals to a “high” cost scenario of about $2.1 million for critical access and rural hospitals and $4.4 million for urban hospitals (Table 3).41 Often, small hospitals cannot afford an EHR system despite the fact that CPOE can reduce medical errors and ADEs.42 Furthermore, only 30 percent of small hospitals (less than 100 beds) and 28 percent of rural hospitals have adopted CPOE, compared to 56 percent of large hospitals (more than 400 beds) and 53 percent of teaching hospitals with more than 20 residents.43
Table 3.
Barriers to CPOE Implementation
| Barrier | Details | Citation |
|---|---|---|
| Cost | CPOE implementation cost ranged from $1.3 million in critical care and rural hospitals to $4.4 million in urban hospitals. | Ohsfeldt et al. (2005) |
| Brigham and Women's Hospital spent $11.8 million dollars to implement CPOE. | Kaushal et al. (2006) | |
| Cost was found to be the number one barrier to adopting CPOE. | Goldzweig et al. (2009) | |
| Physician hesitation | Patient satisfaction does not decrease with physicians using CPOE systems. | Irani et al. (2009) |
| Lack of system interoperability | Lack of interoperability with other systems hinders the physician's ability to access a patient's medical record. | Yaffee (2011) |
| User errors | Errors include selecting the wrong dosage route, inappropriate product, or incorrect dosage and missing drug allergies. Prescribing errors occur in 0.3 to 39.1 percent of medication orders for hospital inpatients, and harm due to prescribing errors has been reported in approximately 1 percent of inpatients. | Reckmann et al. (2009) |
ADE, adverse drug event; CDSS, clinical decision support system; CPOE, computerized provider order entry.
Sources: Goldzwieg, C. L., A. Towfigh, M. Maglione, and P. G. Shekelle. “Costs and Benefits of Health Information Technology: New Trends from the Literature.” Health Affairs 28, no. 2 (2009): 282–93.
Irani, J. S., J. L. Middleton, R. Marfatia, E. T. Omana, and F. D'Amico. “The Use of Electronic Health Records in the Exam Room and Patient Satisfaction: A Systematic Review.” Journal of the American Board of Family Medicine 22, no. 5 (2009): 553–62.
Kaushal, R., A. K. Jha, C. Franz, J. Glaser, K. D. Shetty, T. Jaggi, B. Middleton, G. J. Kuperman, R. Khorasani, M. Tanasijevic, D. W. Bates, and Brigham and Women's Hospital CPOE Working Group. “Return on Investment for a Computerized Physician Order Entry System.” Journal of the American Medical Informatics Association 13, no. 3 (2006): 261–66.
Ohsfeldt, R. L., M. M. Ward, J. E. Schneider, M. Jaana, T. R. Miller, Y. Lei, and D. S. Wakefield. “Implementation of Hospital Computerized Physician Order Entry Systems in a Rural State: Feasibility and Financial Impact.” Journal of the American Medical Informatics Association 12, no. 1 (2005): 20–27.
Reckmann, M., J. Westbrook, Y. Koh, C. Lo, and R. Day. “Does Computerized Provider Order Entry Reduce Prescribing Errors for Hospital Inpatients? A Systematic Review.” Journal of the American Medical Informatics Association 16, no. 5 (2009): 613–23.
Yaffee, A. “Financing the Pulp to Digital Phenomenon.” Journal of Health & Biomedical Law 7, no. 2 (2011): 325–71.
New errors introduced by CPOE that must be taken into consideration include the selection of an inappropriate product or an incorrect dose, frequency, or formulation from a drop-down menu; the inappropriate use or selection of default doses; and missed drug allergies.44 (See Table 3.)
Physicians’ hesitation to adopt CPOE is another barrier to implementing a CPOE system. Physicians are typically set in their ways and hesitant to change. Patient satisfaction is another concern of physicians. Providers tend to think that patients will not be satisfied by the loss of eye contact, decreased opportunity for psychosocial communication, and less sensitivity to the patient from missed nonverbal cues.45 These concerns have been measured by rating patient satisfaction before and after the implementation of a CPOE system. The results of the measurements have shown no significant decrease in patient satisfaction; therefore, providers should have no reason to fear decrease of patient satisfaction after the adoption of a CPOE system (see Table 3).46
Some CDSSs have been created to flag so many different kinds of alerts for the physician that the alerts can be overwhelming. Physicians can ignore the alerts, which can cause problems if a certain pop-up deals with a life-threatening drug that was prescribed to a patient. This phenomenon is commonly known as “alert fatigue.” Having the system specifically tailored to a certain type of patient or a certain age group may help minimize the excessive alerts presented to the physician.47
Unfortunately, many CPOE systems lack the ability to communicate with each other, and this lack of interoperability with other systems is a hindrance to the provider's ability to access the patient's medical record (see Table 3).48 In a few rare cases, implementing a CPOE system has been reported to cause more harm than good. One study found that before CPOE implementation, 60 out of 331 total errors (18 percent) were rated as being of major severity, and after CPOE implementation, 23 out of 44 errors (52 percent) were rated as major. In this study, a significant increase was observed in the proportion of errors rated as major.49
Discussion
The purpose of this study was to examine the benefits of and barriers to adopting CPOE systems in hospitals to determine the effects on medical errors and ADEs and to examine cost and savings associated with this technology. The results of this study suggest that implementing CPOE has had positive effects on reducing the number of avoidable medical errors. However, large and teaching hospitals are adopting CPOE at a faster rate compared to small and rural hospitals because of the cost of adoption and implementation of CPOE systems and the fact that large and teaching hospitals have greater capital funds for investment in this new technology.
Because preventable medical errors and ADEs continue to increase, it is important for hospitals to implement a CPOE system for providers and clinical staff to utilize. The findings of this study suggest that a CPOE system with CDSS capability can be used to diminish individual facilities’ preventable medical errors and ADEs and in turn save the medical facility millions of dollars.
Patients and hospital employees should know all aspects of adopting a CPOE system so that they can get the most benefit from the system. Technical support needs to be accessible at all hours of the day.50 CPOE has been seen as a significant technology to enhance patient safety. Other systems should be integrated with CPOE for its use to be successful. Those systems could consist of CDSS and EHR systems to maximize the impact of reducing medical errors.51 CPOE has gained popularity among hospitals because of the mandate for the implementation and meaningful use of HIT and the incentives and penalties a facility can receive. These incentives demand efforts to change the way healthcare is provided in the United States. Despite the existing barriers for hospitals to adopt and implement a CPOE system, the barriers have not been significant enough to outweigh the HITECH mandate to adopt this technology. With any new technological system, implementation barriers will be always present, but the benefits of CPOE clearly outweigh the barriers when it comes to improving the care of hospital patients.
The CPOE adoption and implementation process can take a long time. It has been anticipated that the incentives, along with the standards for meaningful use of CPOE among hospitals and private providers, will increase CPOE adoption significantly over the next 10 to 15 years. Extensive studies need to be done to make sure the most effective system for each individual organization is adopted. Ensuring that hospital physicians are on board with this new technological change is crucial. Designating a physician champion—a CPOE-supporting physician—would be an ideal way to get other physicians involved in the implementation and also to educate physicians about this new technological change. For CPOE implementation to be successful, input from all those who will be utilizing the system on how the CPOE system will be arranged and what will be included in it will be necessary.
Limitations
This literature review was limited because of the restrictions in the search strategy used, such as the number of databases accessed. Publication and researcher bias may have affected the selection of sources used and the quality of research identified during the analysis. Also, because the mandate for CPOE is fairly new, fewer facilities that have fully adopted the system are available to be examined, thus limiting the amount of useful searchable publications. Performing a systematic review with stringent criteria and measuring the effect of sources or weighing the sources for complete accuracy, relevance, and reliability was out of the scope of this review, given the highly dissimilar qualities of the data.
Practical Implications and Recommendations
The adoption and implementation of a CPOE system can be a prolonged process because of physician and staff resistance to the new system and some technical barriers. Training needs to be available for all authorized personnel using the system, in particular for physicians. Hospitals are open 24 hours a day and seven days a week, so the hospital employees need to know and fully understand the system. Providing 24/7 technical support for weeks after the system goes live is necessary. If all employees are trained and ready for the change from paper to electronic forms, the transition process should go more smoothly. Order set creation should be established by each department or section and validated by the medical staff who will use the system. Also, determining which decision support rules go in the system and which do not should also be important in the day-to-day use of a CPOE system. Improved or new standards must be met in areas such as interfacing with systems from different vendors for information transfer among providers, pharmacists, payers, and pharmacy benefit managers. Standardization also needs to be applied to terminologies. Usable dictionaries for medication ordering that support standard use are needed. Standard terminologies must also be established to create assessment procedures and for the shared representation of medication dosages, allergies, and reactions.
Additional research need to be done to obtain more information about the costs of implementation and benefits of CPOE adoption, as well as the importance and effectiveness of CPOE as one of the leading systems for the reduction of medical errors and ADEs. Further studies will be required to address the needs of rural and small hospitals. Most articles reviewed focused on large academic medical centers and large city hospitals, but variations in resources may have an effect on the process and the rate of CPOE adoption. Finally, a systematic review and/or meta-analysis should be performed to obtain a more precise measurement of the benefits of and barriers to CPOE implementation.
Conclusion
CPOE systems have the potential to be an effective solution for limiting hospital medical errors and ADEs experienced in the United States. CPOE adoption can facilitate the reduction of medical errors and ADEs as well as creating cost savings in hospitals. CPOE also supplies providers with additional clinical knowledge and patient-related information that is intelligently filtered and presented at appropriate times. CPOE adoption and implementation has been part of a comprehensive process of updating and re-engineering entire hospital information systems and associated processes. CPOE systems can be integrated with other systems to increase patient safety and improve the quality of patient care. The cost of CPOE adoption and implementation is still a main barrier, especially for small and rural hospitals.
Better estimates of the financial impact of CPOE in smaller hospitals are needed to completely assess its financial feasibility. The success of the adoption and implementation of a CPOE system in urban hospitals depends on teamwork among medical staff, clinical support services, and the hospital administration. Specifically, the establishment of the mandate and standards for meaningful use by CMS, and the financial incentives and penalties established by the HITECH Act, have promoted CPOE as a secure way of transferring physician orders that will help hospitals improve their efficiency and achieve cost savings, while allowing physicians and other healthcare providers to provide better quality of care.
Contributor Information
Krista Charles, Krista Charles, MS, is an alumni of the Healthcare Program of the College of Business at Marshall University, Graduate College, in South Charleston, West Virginia..
Margaret Cannon, Margaret Cannon, MS, is an alumni of the Healthcare Program of the College of Business at Marshall University, Graduate College, in South Charleston, West Virginia..
Robert Hall, Robert Hall, MS, is an alumni of the Healthcare Program of the College of Business at Marshall University, Graduate College, in South Charleston, West Virginia..
Alberto Coustasse, Alberto Coustasse, DrPH, MD, MBA MPH, is an associate professor of the Healthcare Program of the College of Business at Marshall University, Graduate College, in South Charleston, West Virginia..
Notes
- 1.US Department of Health and Human Services. “HITECH Act Enforcement Interim Final Rule.” 2013. Available at http://www.hhs.gov/ocr/privacy/hipaa/administrative/enforcementrule/hitechenforcementifr.html (accessed November 24, 2013).
- 2.Bloomrosen M., Starren J., Lorenzi N. M., Ash J. S., Patel V. L., Shortliffe E. H. Anticipating and Addressing the Unintended Consequences of Health IT and Policy: A Report from the AMIA 2009 Health Policy Meeting. Journal of the American Medical Informatics Association. 2011;18(1):82–90. doi: 10.1136/jamia.2010.007567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.US Department of Health and Human Services, Indian Health Service. “Meaningful Use.” 2013. Available at http://www.ihs.gov/meaningfuluse/index.cfm?module=faq (accessed October 25, 2013).
- 4.Healthcare Information and Management Systems Society. “Electronic Health Records.” 2013. Available at http://www.himss.org/library/ehr/ (accessed March 5, 2013).
- 5.Centers for Medicare and Medicaid Services. “Medicare and Medicaid EHR Incentive Program Basis.” 2013. Available at http://www.cms.gov/Regulations-and-Guidance/Legislation/EHRIncentivePrograms/Basics.html (accessed November 24, 2013).
- 6.Jha A. K., DesRoches C. M., Kralovec P. D., Joshi M. S. A Progress Report on Electronic Health Records in U.S. Hospitals. Health Affairs. 2010;29(10):1951–57. doi: 10.1377/hlthaff.2010.0502. [DOI] [PubMed] [Google Scholar]
- 7.Silow-Carroll S., Edwards J. N., Rodin D. Using Electronic Health Records to Improve Quality and Efficiency: The Experiences of Leading Hospitals. The Commonwealth Fund; July 2012. Available at http://www.commonwealthfund.org/∼/media/Files/Publications/Issue%20Brief/2012/Jul/1608_SilowCarroll_using_EHRs_improve_quality.pdf (accessed October 28, 2013). [PubMed] [Google Scholar]
- 8.Bowes W. “Assessing Readiness for Meeting Meaningful Use: Identifying Electronic Health Record Functionality and Measuring Levels of Adoption.” AMIA Annual Symposium Proceedings (2010): 66–70. [PMC free article] [PubMed]
- 9.Jones S. S., Heaton P., Friedberg M. W., Schneider E. C. Today's ‘Meaningful Use’ Standard for Medication Orders by Hospitals May Save Few Lives; Later Stages May Do More. Health Affairs. 2011;30(10):2005–12. doi: 10.1377/hlthaff.2011.0245. [DOI] [PubMed] [Google Scholar]
- 10.Hsiao C., Decker S. L., Hing E., Sisk J. E. Most Physicians Were Eligible for Federal Incentives in 2011, But Few Had EHR Systems That Met Meaningful-Use Criteria. Health Affairs. 2011;31(5):1100–1107. doi: 10.1377/hlthaff.2011.1315. [DOI] [PubMed] [Google Scholar]
- 11.Andel C., Davidow S. L., Hollander M., Moreno D. A. The Economics of Health Care Quality and Medical Errors. Journal of Health Care Finance. 2012;39(1):39–50. [PubMed] [Google Scholar]
- 12.Ibid.
- 13.US Department of Health and Human Services, Agency for Healthcare Research and Quality. Research in Action, no. 1. Rockville, MD: Agency for Healthcare Research and Quality; 2001. Reducing and Preventing Adverse Drug Events to Decrease Hospital Costs. March Available at http://www.ahrq.gov/research/findings/factsheets/errors-safety/aderia/index.html (accessed November 24, 2013). [Google Scholar]
- 14.Du D. T., Goldsmith J., Aikin K. J., Encinosa W. E., Nardinelli C. Despite 2007 Law Requiring FDA Hotline to Be Included in Print Drug Ads, Reporting on Adverse Drug Events by Consumers Still Low. Health Affairs. 2012;31(5):1022–29. doi: 10.1377/hlthaff.2010.1004. [DOI] [PubMed] [Google Scholar]
- 15.Jones S. S., Heaton P., Friedberg M. W.Schneider E. C. “Today's ‘Meaningful Use’ Standard for Medication Orders by Hospitals May Save Few Lives; Later Stages May Do More.” [DOI] [PubMed]
- 16.Cucina R.Papadakis M. A., McPhee S. J.Rabow M. W. “Information Technology in Patient Care.” Medical Diagnosis & Treatment 2013http://www.accessmedicine.com/content.aspx?aID=779189 (accessed November 24, 2013).
- 17.Furukawa M. F., Raghu T. S., Spaulding T. J., Vinze A. Adoption of Health Information Technology for Medication Safety in U.S. Hospitals. Health Affairs. 2006;27(3):865–75. doi: 10.1377/hlthaff.27.3.865. [DOI] [PubMed] [Google Scholar]
- 18.GE Healthcare. “American Recovery and Reinvestment Act of 2009 HITECH Act for Healthcare.” 2009. Available at http://www.gehealthcare.com/usen/hit/docs/ARRA-GEHCIT-FAQ-022709.pdf (accessed March 14, 2014).
- 19.Harrison R., Lyerla F. Using Nursing Clinical Decision Support Systems to Achieve Meaningful Use. Computers, Informatics, Nursing. 2012;30(7):380–85. doi: 10.1097/NCN.0b013e31823eb813. [DOI] [PubMed] [Google Scholar]
- 20.US Department of Health and Human Services. “Health IT Adoption and the New Challenges Faced by Solo and Small Group Healthcare Practices.” 2011. Available at http://www.hhs.gov/asl/testify/2009/06/t20090624a.html (accessed April 26, 2013).
- 21.HealthIT.gov. “Are There Penalties for Providers Who Don't Switch to Electronic Health Records (EHR)?” 2013. Available at http://www.healthit.gov/providers-professionals/faqs/are-there-penalties-providers-who-don%E2%80%99t-switch-electronic-health-record (accessed October 28, 2013).
- 22.Yao W., Chu C. H.Li Z. “The Use of RFID in Healthcare: Benefits and Barriers.” Proceedings of the 2010 IEEE International Conference on RFID-Technology and Applications (2010): 128–34.
- 23.Ibid.
- 24.Coustasse A., Tomblin S.Slack C. “Impact of Radio-Frequency Identification (RFID) Technologies on the Hospital Supply Chain: A Literature Review.” Perspectives in Health Information Management (Fall 2013). [PMC free article] [PubMed]
- 25.Deslich S., Coustasse A. Expanding Technology in the ICU. Telemedicine and e-Health. 2014;20(5):485–92. doi: 10.1089/tmj.2013.0102. [DOI] [PubMed] [Google Scholar]
- 26.Porterfield A., Engelbert K.Coustasse A. “Electronic Prescribing: Improving the Efficiency and Accuracy of Prescribing in the Ambulatory Care Setting.” Perspectives in Health Information Management (Spring 2014). [PMC free article] [PubMed]
- 27.Yaffee A. Financing the Pulp to Digital Phenomenon. Journal of Health & Biomedical Law. 2011;7(2):325–71. [Google Scholar]
- 28.Devine E. B., Williams E. C., Martin D. P., Sittig D. F., Tarczy-Hornoch P., Payne T. H., Sullivan S. D. Prescriber and Staff Perceptions of an Electronic Prescribing System in Primary Care: A Qualitative Assessment. BMC Medical Informatics and Decision Making. 2010;10(72) doi: 10.1186/1472-6947-10-72. ;): 72–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cartmill R. S., Walker J. M., Blosky M. A., Brown R. L., Djurkovic S., Dunham D. B., Gardill D., Haupt M. T., Parry D., Wetterneck T. B., et al. Impact of Electronic Order Management on the Timeliness of Antibiotic Administration in Critical Care Patients. International Journal of Medical Informatics. 2012;81(11):782–91. doi: 10.1016/j.ijmedinf.2012.07.011. [DOI] [PubMed] [Google Scholar]
- 30.Mattison M. L., Afonso K. A., Ngo L. H., Mukamal K. J. Preventing Potentially Inappropriate Medication Use in Hospitalized Older Patients with a Computerized Provider Order Entry Warning System. Archives of Internal Medicine. 2010;170(15):1331–36. doi: 10.1001/archinternmed.2010.244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ibid.
- 32.Keel J. F.Jennings A.How to Architect the Best CPOE Approach North Carolina Healthcare Information & Communications Alliance (NCHICA) 2014. Available at http://www.nchica.org/Resources/Best%20CPOE%20Approach%20033004.pdf (accessed February 6, 2014).
- 33.Radley D. C., Wasserman M. R., Olsho L. E., Shoemaker S. J., Spranca M. D., Bradshaw B. Reduction in Medication Errors in Hospitals Due to Adoption of Computerized Provider Order Entry Systems. Journal of the American Medical Informatics Association. 2013;20(3):470–76. doi: 10.1136/amiajnl-2012-001241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ibid.
- 35.Kaushal R., Bates D. W. Computerized Physician Order Entry (CPOE) with Clinical Decision Support Systems (CDSS) Agency for Healthcare Research and Quality; 2013. Available at http://psnet.ahrq.gov/primer.aspx?primerID=6 (accessed January 27, 2014). [Google Scholar]
- 36.Jha A. K., Chan D. C., Ridgway A. B., Franz C., Bates D. W. Improving Safety and Eliminating Redundant Tests: Cutting Costs in U.S. Hospitals. Health Affairs. 2009;28(5):1475–84. doi: 10.1377/hlthaff.28.5.1475. [DOI] [PubMed] [Google Scholar]
- 37.Callen J. L., Westbrook J. L., Braithwaite J. The Effect of Physicians’ Long-Term Use of CPOE on Their Test Management Work Practices. Journal of the American Medical Informatics Association. 2006;13(6):643–52. doi: 10.1197/jamia.M2152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Levick D. L., Stern G., Meyerhoefer C. D., Levick A., Pucklavage D. Reducing Unnecessary Testing in a CPOE System through Implementation of a Targeted CDS Intervention. BMC Medical Informatics and Decision Making. 2013;13(43) doi: 10.1186/1472-6947-13-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kaushal R., Jha A. K., Franz C., Glaser J., Shetty K. D., Jaggi T., Middleton B., Kuperman G. J., Khorasani R., Tanasijevic M., Bates D. W. Brigham and Women's Hospital CPOE Working Group. Return on Investment for a Computerized Physician Order Entry System. Journal of the American Medical Informatics Association. 2006;13(3):261–66. doi: 10.1197/jamia.M1984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Baron J. M., Dighe A. S. Computerized Provider Order Entry in the Clinical Laboratory. Journal of Pathology Informatics. 2011;2(35) doi: 10.4103/2153-3539.83740. Available at http://www.jpathinformatics.org/text.asp?2011/2/1/35/83740 (accessed November 15, 2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ohsfeldt R. L., Ward M. M., Schneider J. E., Jaana M., Miller T. R., Lei Y., Wakefield D. S. Implementation of Hospital Computerized Physician Order Entry Systems in a Rural State: Feasibility and Financial Impact. Journal of the American Medical Informatics Association. 2005;12(1):20–27. doi: 10.1197/jamia.M1553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Furukawa M. F., Raghu T. S., Spaulding T. J.Vinze A. “Adoption of Health Information Technology for Medication Safety in U.S. Hospitals.” [DOI] [PubMed]
- 43.Radley D. C., Wasserman M. R., Olsho L. E., Shoemaker S. J., Spranca M. D.Bradshaw B. “Reduction in Medication Errors in Hospitals Due to Adoption of Computerized Provider Order Entry Systems.” [DOI] [PMC free article] [PubMed]
- 44.Reckmann M., Westbrook J., Koh Y., Lo C., Day R. Does Computerized Provider Order Entry Reduce Prescribing Errors for Hospital Inpatients? A Systematic Review. Journal of the American Medical Informatics Association. 2009;16(5):613–23. doi: 10.1197/jamia.M3050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Irani J. S., Middleton J. L., Marfatia R., Omana E. T., D'Amico F. The Use of Electronic Health Records in the Exam Room and Patient Satisfaction: A Systematic Review. Journal of the American Board of Family Medicine. 2009;22(5):553–62. doi: 10.3122/jabfm.2009.05.080259. [DOI] [PubMed] [Google Scholar]
- 46.Ibid.
- 47.Kesselheim A. S., Cresswell K., Phansalkar S., Bates D. W., Sheikh A. Clinical Decision Support Systems Could Be Modified to Reduce ‘Alert Fatigue’ While Still Minimizing the Risk of Litigation. Health Affairs. 2011;30(12):2310–17. doi: 10.1377/hlthaff.2010.1111. [DOI] [PubMed] [Google Scholar]
- 48.Yaffee A. “Financing the Pulp to Digital Phenomenon.”
- 49.Reckmann M., Westbrook J., Koh Y., Lo C.Day R. “Does Computerized Provider Order Entry Reduce Prescribing Errors for Hospital Inpatients? A Systematic Review.” [DOI] [PMC free article] [PubMed]
- 50.Kuperman G. J., Gibson R. F. Computer Physician Order Entry: Benefits, Costs, and Issues. Annals of Internal Medicine. 2003;139(1):31–39. doi: 10.7326/0003-4819-139-1-200307010-00010. [DOI] [PubMed] [Google Scholar]
- 51.Aarts J., Koppel R. Implementation of Computerized Physician Order Entry in Seven Countries. Health Affairs. 2009;28(2):404–14. doi: 10.1377/hlthaff.28.2.404. [DOI] [PubMed] [Google Scholar]