ABSTRACT
Introduction:
COPD (Chronic Obstructive Pulmonary Disease) is characterized by airflow limitation that is not fully reversible and that can lead to respiratory failure.
Objective:
to show the changes of arterial blood gases in COPD during the 4 -year evolution of illness.
Material and Methods:
The research was done on patients suffering from COPD treated at the Clinic “Podhrastovi” during 2006 and 2007 year. The tested parameters were examined from the date of receiving patient with COPD to hospital treatment in 2006 and 2007 and then followed prospectively until 2010 or 2011 year (the follow-up period was 4 years). There were total 199 treated patients who were chosen at random and regularly attended the control examinations. The study was conducted on adult patients of both sexes, different age group. In each patient the duration of illness was recorded so is sex, age, data of smoking habits, information about the regularity of taking bronchodilator therapy during remissions of disease, about the treatment of disease exacerbations, results of blood gases analysis as follows : pH value, PaO2 (partial pressure of oxygen in arterial blood), PaCO2 (partial pressure of carbon dioxide in arterial blood). All these parameters were measured at the beginning and at the end of each hospital treatment. We took in elaboration data obtained in the beginning of the first hospitalization and at the end of the last hospitalization or at the last control in outpatient department when patient was in stable state. Patients were divided into three groups according to the number of exacerbations per year.
Results:
there is the statistically significant decrease of PaO2 (p<0.01) and pH, (p<0.05) and an increase of PaCO2 (p<0.01) during follow-up period. But in patients regularly treated in phases of remission and exacerbations of illness the course of illness is slower. The decrease of pH and PaO2 and increase of PaCO2 is statistically significantly smaller in those received regular treatment in phases of remissions (P values are respectively <0.05, <0.01 and <0.01) and exacerbations of illness (p values are respectively: <0.01, <0.01 and <0.05).
Conclusion:
COPD is characterized with airflow limitation which is progressive in the course of illness, and by the changes in arterial blood gases that can lead to respiratory failure, but that course may be made slower using appropriate treatment during remission and exacerbations of diseases.
Keywords: COPD, pH value, PaO2, PaCO2, treatment, respiratory failure
1. INTRODUCTION
COPD is one of the major causes of chronic morbidity and mortality worldwide. It is the fourth leading cause of death in the world (1), and further increases in its prevalence and mortality can be predicted in the coming decades (2, 3). COPD is a pulmonary disease with significant extrapulmonary effects that may contribute to the severity of illness. Its pulmonary component is characterized by airflow limitation that is not fully reversible (4), usually is progressive and can lead to respiratory failure (1).
Systemic manifestations and co-morbidities in COPD are body weight loss, skeletal muscle wasting, cachexia, osteoporosis, right heart failure, cardiac ischemia, cardiac arrhythmias, anemia, hypoalbuminaemia, diabetes, cognitive deficits, depression (5, 6). Co-morbidities are common for people with COPD because organ systems work differently when they do not receive enough oxygen.
Cigarette smoking is the most common risk factor for COPD, although in many countries, various kinds of air pollution have also been identified as COPD risk factors (1, 4, 7).
The chronic airflow limitation of COPD is caused by a mixture of small airway disease (obstructive bronchiolitis) and parenchymal destruction (emphysema), the relative contributions of which vary from person to person (1). Chronic inflammation causes structural changes and narrowing of small airways. Destruction of the lung parenchyma leads to the loss of alveolar attachments to the small airways and decreases lung elastic recoil; these changes diminish the ability of the airways to remain open during expiration (8, 9, 10, 11). So in COPD inflammation causes small airway disease (airway inflammation, airway remodelling) and parenchymal destruction that all lead to airflow limitation (9, 11,12).
1.1. Respiratory failure in COPD
Because of these anatomic changes in pulmonary tissue and consecutive airflow limitation respiratory failure can develop. For the body to function normally, ventilation must meet the metabolic demand of body tissue. Thus, metabolic tissue consumption of oxygen must be equal to the oxygen taken up in the blood from alveolar gas. Or, metabolic tissue production of carbon dioxide must be equal to the amount of carbon dioxide blown off at the alveoli. Respiratory failure is defined as a PaO2< 60 mmHg (8kPa) and is divided into type I and type II depending on PaCO2.
Type I of respiratory failure: PaCO2< 45 mmHg (6kPa)–normal or low; PaO2 is low (hypoxemia); this represents a ventilation/perfusion mismatch; we talk about partial respiratory insufficiency.
Type II of respiratory failure: PaCO2> 45 mmHg (6kPa), PaO2< 60 mmHg (8kPa). Both PaO2 and PaCO2 indicate that lungs are not well ventilated; we talk about a global or hypoventilation respiratory insufficiency.
In Clinic “ Podhrastovi ” we have a stand that if after two weeks of bronchodilator therapy with 24-hour oxygen therapy (for two weeks) there is no normalization of arterial blood gases it can be saying about the chronic respiratory failure (13, 14). The acutissation of chronic respiratory failure is caused either by worsening of primary disorder–COPD or by superimposed secondary illnesses such as pneumonia.
The pH of the intracellular and extracellular compartments must be tightly controlled to the body to function efficiently, or at all. The normal arterial pH lies in narrow range: 7.35-7.45 ([H+] range 45-35 mmol/L). An acid -base disturbance arises when arterial pH lies outside that range. If pH is less than 7.35 an acidosis is present, if pH is greater than 7.45 the alkalosis is present. Tight control on blood pH is achieved by a combination of blood buffers and the respiratory and renal systems which make adjustments to return pH toward its normal levels.
Acidosis can be caused by either of: a rise in PaCO2 or fall in HCO3. Alkalosis can be caused by either of: a fall in PaCO2 or rise in HCO3. When the primary change is in CO2 we name the disturbance respiratory, and when primary change is in bicarbonate, we name the disturbance metabolic.
It is clear that lung diseases affect gas exchange and therefore PaCO2 have major affection on body's acid-base status. It is also clear that while the respiratory system can act quickly to compensate for metabolic disturbance it will take time for compensation to take place in respiratory disease; the renal system cannot act as quickly. It is seen in clinical practice; a change in bicarbonates is characteristic of chronic lung disease rather than in acute.
1.2. Treatment of COPD
Although COPD is progressive illness it has periods of remission and exacerbations. An exacerbation of COPD is defined as an event in the common course of the disease characterized by a change in the patient's baseline dyspnea, cough, and/or sputum production that is beyond common day-to-day variations, that is acute in onset, and may warrant a change in regular medication (1). In severe exacerbations the patient may be unable to maintain normal blood gases that can lead to respiratory failure. Respiratory failure is the leading cause of death in patients with COPD and is most often hypercapnic (type II).
The treatment of COPD shows some differences in phases of remission and exacerbation. Bronchodilator medications are central to symptom management in COPD. Inhaled therapy is preferred (1, 14).
1.3.1. Bronchodilators in stable COPD
The choice between β2-agonist, anticholinergics, theophylline, or combination therapy depends on availability and individual response in terms of symptom relief and side effects. Bronchodilators are prescribed on an as-needed or on a regular basis to prevent or reduce symptoms. Long-acting inhaled bronchodilators are more effective and convenient than treatment with short-acting bronchodilators. Combining bronchodilators may improve efficacy and decrease the risk of side effects compared to increasing the dose of a single bronchodilator (1). Today the combined inhaled bronchodilators (corticosteroids and laba- long acting β2-agonist) are preferred (1, 14).
1.3.2. Treatment of COPD exacerbations
It is needed to: assess severity of symptoms, blood gases, chest X-ray. It is also needed to administering controlled oxygen therapy and repeating arterial blood gas measurement after 30-60 minutes. As to use of bronchodilators: – increase doses and/or frequency is needed, and so combination β2-agonists and anticholinergics, using spacers or air-driven nebulizers, adding intravenous methylxanthines, if needed, adding oral or intravenous corticosteroids. Antibiotics (oral or intravenous) are administrated when signs of bacterial infection are presented. Non-invasive mechanical ventilation (NIMV) in some patients according to level of blood gases. At all time: – monitor fluid balance and nutrition, considering subcutaneous heparin. Identifying and treatment of associated conditions (e.g. heart failure, cardiac arrhythmias) (1).
2. OBJECTIVE
Objective of our study is to show the changes of arterial blood gases in COPD during the four–year evolution of illness.
3. MATERIAL AND METHODS
The research was done prospectively on patients suffering from COPD treated at the Clinic “Podhrastovi” during 2006 and 2007 year. The tested parameters were examined from the date of receiving patient with COPD to hospital treatment in 2006 and 2007 and then followed prospectively until 2010 or 2011 year (the follow-up period was 4 years). There were total 199 treated patients who were chosen at random and regularly attended the control examinations. The study was conducted on adult patients of both sexes, different age groups.
In each patient the duration of illness was recorded so is sex, age, data of smoking habits, information about the regularity of taking bronchodilatatory therapy during remissions of disease, about the treatment of disease exacerbations, results of blood gases analysis : pH value, PaO2, PaCO2. All these parameters were measured at the beginning and at the end of each hospital treatment. We took in elaboration data obtained in the beginning of the first and at the end of the last hospitalization or at the last control in outpatient department when patient was in stable state.
Patients were divided into three groups according to the number of exacerbations per year : 1st group made of 65 patients with one or less exacerbation per year, 2nd group made of 65 patients with 2-3 exacerbations per year, 3rd group made of 69 patients with more than 3 exacerbations of disease per year.
Smoking habits imply the duration of smoking in years, the number of cigarettes smoked per a day. The complete anty obstructive therapy involves antibiotics, combined spray therapy (inhaled corticosteroids and long acting β-agonists), eventually anticholinergic, corticosteroids and methylxanthines (either orally or intravenously). Data were collected from patients’ hospital charts in phases of exacerbations and data during remissions were taken from the competent pulmonologist of Houses of Health or Counseling Department of Clinic “Podhrastovi”.
4. RESULTS
The average age of patients in 1st group is 57.36 years, in 2nd group 61.57 and in 3rd group 61.58 years. Patients with 1 or less exacerbations per year are statistically significantly younger than patients with 2-3 (p=0.05) and patients with more than 3 exacerbations per year (p=0.05). There is no statistic significant difference between two last groups.
There are 149 (74.87%) males and 50 (25.13%) females: in the 1st group are 44(67.69%) males and 21 (32.31%) females, in 2nd group 51 (78.46%) males and 14 (21.54%) females, in the 3rd group are 54 (78.26%) males and 15(21.74%) females. The number of male patients is statistically significantly bigger than females (p= 0.01). There are not statistically significant differences in sex according to the number of exacerbations of diseases per year. Chisquared tests are respectively: 2.716 and 1.218, 2 degrees of freedom. There is 157 (78.89%) smokers and 42(21.11%) non –smokers. In the 1st group there is 42(64.62%), in the 2nd group 54(83.08%) and in the 3rd group 61(88.41%) of smokers. There is high statistically significant difference in the number of smokers and non-smokers (p=0.01). The greatest number of non-smokers is in patients with the least number of exacerbations. Chi-squared test=12.367, the level of significance: p=0.01, 2 degrees of freedom. It is significant that 91. 05% of smokers have been smoking more than 20 years.
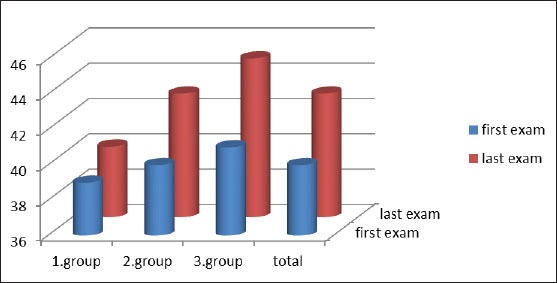
The average duration of illness (at the last examination) is 10.51 years. In the 1st group it is 8 years, the 2nd group 10.82 and in the 3rd group 12.70 years. The number of exacerbations is statistically significantly bigger in patients with the longer duration of illness. The levels of significance are: between first and second group p=0.05, between first and third group p=0.05, between second and third group p=0.10. The number of patients using regular therapy in the phases of remission of illness is statistically significantly smaller than number of patients not using therapy (p<0.05.) (Figure 1). There are not statistically significant differences in receiving therapy according to the number of exacerbations of illness per year. Chi-squared test= 3.124; 2 degrees of freedom). (Figure 2). In patients with bigger number of exacerbations there is less number of them who received complete therapy in phases of illness exacerbations. Chi- squared test = 9.307, level of significance: p<0.01, 2 degrees of freedom (Figure 3).
Figure 1.
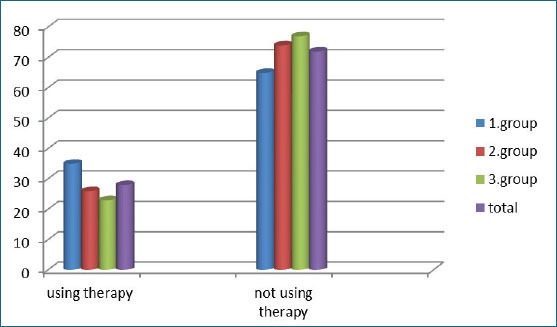
Using therapy in phases of COPD –remissions in groups of patients expressed as percentage of examined patients
Figure 2.
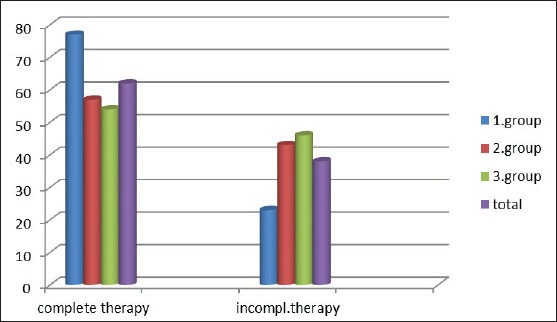
Using therapy in phases of COPD –exacerbations in groups of patients expressed as percentage of examined patients
Figure 3.
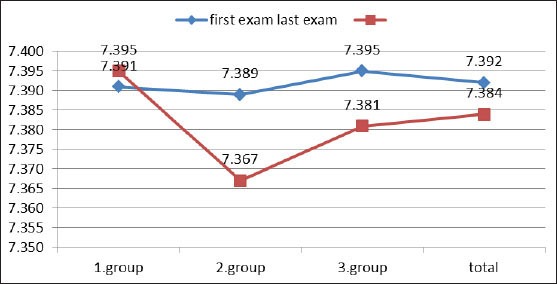
The average measured pH values of arterial blood at the first and last examination
In all patients, in second and third group pH value of arterial blood decreased statistically significantly in the follow-up period (p< 0.05 for all patients, and for second and third group). In the second and third group difference of pH value is statistically significantly bigger than in first group. P values are respectively: p<0.01 and p<0.01. In the first group there is not statistically significant change of pH value (Figure 4)
Figure 4.
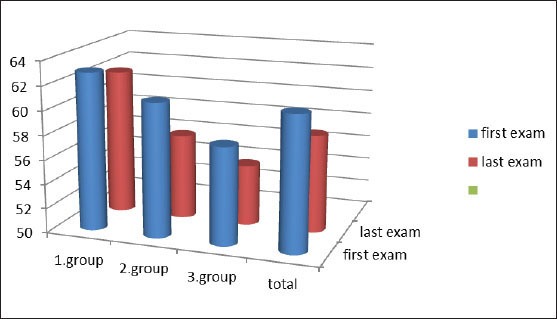
The average measured values of PaO2 (mmHg) at the first and last examination
In all patients, in second and third group PaO2 decreased statistically significantly in the follow-up period (p< 0.01 for all patients, and for second and third group). In the second and third group decrease of PaO2 is statistically significantly bigger than in first group. P values are respectively: p<0.01 and p<0.01. In the first group decrease of PaO2 is not statistically significant (Figure 5).
Figure 5.
The average measured values of PaCO2 (mmHg) at the first and last examination
In all patients, in second and third group PaCO2 increased statistically significantly in the follow-up period (p< 0.01 for all patients, and for second and third group). In the second and third group increase of PaCO2 is statistically significantly bigger than in first group. P values are respectively: p<0.01 and p<0.01. In the first group increase of PaCO2 is not statistically significant (Table 1).
Table 1.
The average measured values of pH, PaO2 and PaCO2 at first and last examination according to the use of therapy in phases of COPD remissions
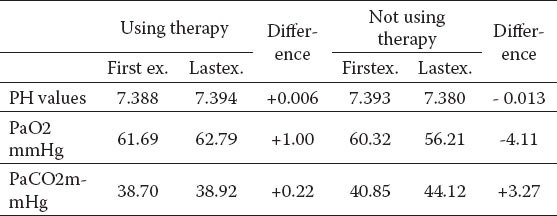
In patients using regular therapy during remissions of COPD there is increase in values of pH, PaO2 and PaCO2 during follow-up period that is not statistically significant. In patients not using therapy there is statistically significant decrease in PaO2 and statistically significant increase in PaCO2 values (p < 0.01 for both).
The difference of measured changes of parameters between patients using and not using therapy is statistically significant for PaO2 and PaCO2 (p<0.01 for both) and not statistically significant for pH (Table 2).
Table 2.
The average measured values of pH, PaO2 and PaCO2 at last examination according to the use of therapy in phases of COPD remissions
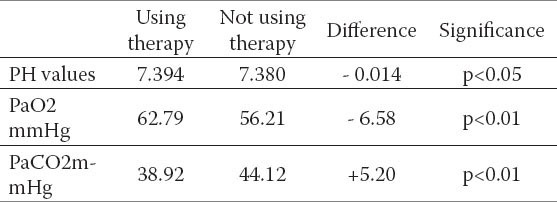
The difference in values of pH, PaO2 and PaCO2 at the last examination shows significant difference between those using and those not using regular therapy in the phases of COPD remissions during follow-up period (Table 3).
Table 3.
The average measured values of pH, PaO2 and PaCO2 at first and last examination according to the use of therapy in phases of COPD exacerbations
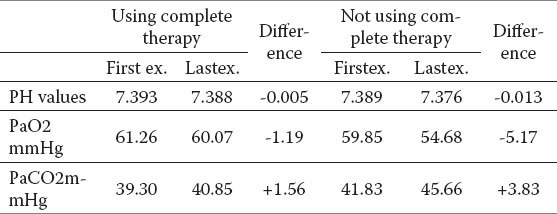
Table 4.
The values of pH, PaO2 and PaCO2 at last examination according to the use of therapy in phases of COPD exacerbations
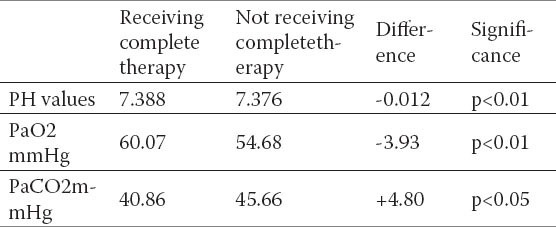
In all patients with COPD there is the decrease of pH, PaO2 and increase of PaCO2 during follow-up period but in patients receiving complete therapy during exacerbations of COPD the changes are statistically significantly smaller than in patients not using complete therapy. The difference of measured changes of parameters between patients using complete and using not complete therapy is statistically significant. For pH: p< 0.01, for PaO2: p<0.01, and for PaCO2: p< 0.05.
The difference in values of PH, PaO2 and PaCO2 at the last examination shows significant difference between those receiving and those not receiving complete therapy in phases of COPD exacerbations during the follow-up period.
5. DISCUSSION
COPD is one of the major causes of chronic morbidity and mortality worldwide. It is the fourth leading cause of death in the world (1) It is a pulmonary disease with significant extrapulmonary effects. Its pulmonary component is characterized by airflow limitation that is not fully reversible (4), is usually progressive and can lead to respiratory failure (1). Cigarette smoking is the most common risk factor for COPD.
Respiratory failure is defined as a PaO2< 60 mmHg (8kPa) and is divided into type I and type II depending on PaCO2. Type I of respiratory failure: PaCO2< 45 mmHg (6kPa), PaO2 is low (hypoxemia); this represents a ventilation/perfusion mismatch. Type II of respiratory failure: PaCO2> 45 mmHg (6kPa) and PaO2< 60 mmHg (8kPa). Both PaO2 and PaCO2 indicate that lungs are not well ventilated.
Cigarette smoking is the most common risk factor for COPD. The real role of smoking in accelerating the course of COPD and in the development or respiratory failure in patients with COPD could not be clearly determined in this study because of large number of smokers in this sample (78.89% of patients were smokers) and 91.05% of them have been smoking more than 20 years. The biggest number of non-smokers was in patients with one or fewer exacerbations per year; and knowing that a bigger number of exacerbations lead to faster damage of lung function-ventilation in the course of COPD; these data indirectly indicate that cigarette smoking leads to faster damage of lung function; and disturbance in pulmonary ventilation leads to disturbance in gas exchange.
In the phases of illness- remissions therapy (the maintenance therapy) is most often taken by those with one or less disease exacerbation per year, and most rarely taken by patients with more than three exacerbations per year which indicate the importance of taking therapy continuously that lessen bronchial inflammation and so the response to environmental factors –such as viruses, bacterias, air-pollution (1, 14). The more expressed bronchial inflammation causes easier the development of COPD exacerbations when pulmonary ventilation worsen and make worse the gases exchange that can lead to respiratory failure.
Number of exacerbations per year and receiving full therapy in these phases are close connected. The number of exacerbations per year is statistically significantly bigger in patients not taking full therapy. It implicate the importance of treating of each exacerbation that leads to less sequels on bronchial mucosa (airway re- modulation), because on more damaged bronchial mucosa it is easier for disease to exacerbate by doing of various environmental factors (1,14).
In phases of COPD exacerbations there is the expressed worsening of bronchial obstruction, bronchial mucosal edema and sputum production, so that pulmonary ventilation is decreased that leads to disturbance in gas exchanges in lungs. We considered why patients have not been given full therapy in phases of exacerbations of illness although all of them have been treated in hospital. That is because we didn’t have apparatuses for non-invasive ventilation until 2010. year, that many patients refused non-invasive ventilation, that we were not in the habit to give anticholinergics, that many of patients had diabetes that is the contraindication for corticosteroids, that many of them couldn’t stand 24-hour oxygen therapy, that some of patients had allergy to proper antibiotics, and that we had no always full monitoring of using spray bronchodilators in conscious patients.
In all patients with COPD there is the decrease of pH and PaO2 and an increase of PaCO2 during follow-up period that indicates that airflow limitation is progressive but in patients taking regular therapy treatment during remissions and exacerbations of illness both pH and PaO2 are statistically significantly bigger and PaCO2 is statistically significantly smaller in comparison with patents not taking full therapy. These results indicate the importance of rapid- in right time inclusion of bronchodilator therapy to slow the progression of disease and preventing or postponing the development of respiratory failure.
6. CONCLUSION
The basic characteristic of COPD is airflow limitation. The course of COPD is progressive and can lead to respiratory failure, but the course of disease may be made slower with appropriate continuous therapy using in phases of remissions and appropriate treatment of exacerbations of illness. The regular using of therapy during the remissions of illness prevents or delays the occurrence of exacerbations of disease. There is the importance of vigorous treatment of each disease exacerbation because of better recovery of the inflamed bronchial mucosa for it leads to remaining of less number of mucosal changes –sequels. All that damage of bronchial mucosa can lead to impairment lung ventilation that cusses the impairment of gases exchanges that can lead to development of respiratory failure. There is the importance of ceasing smoking, and avoidance of other environmental factors causing the acutissation of COPD.
Footnotes
CONFLICT OF INTEREST: NONE DECLARED
REFERENCES
- 1.GOLD (Global Initiative for Chronic Obstructive Lung Disease) - global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease-revised. 2006. pp. 1–100. Http//www.goldcopd.org . [PubMed]
- 2.Geneva: World Health Organization; 2000. World Health Report. Available from URL: http://www.who.int/whr/2000/en/statistics.htm . [Google Scholar]
- 3.Lopez AD, Shibuya K, Rao C, Mathers CD, Hansell AL, et al. Chronic obstructive pulmonary disease: current burden and future projections. Eur Respir J. 2006;27(2):397–412. doi: 10.1183/09031936.06.00025805. [DOI] [PubMed] [Google Scholar]
- 4.Soriano JB, Visick GT, Muellerova H, Payvandi N, Hansell AL. Patterns of comorbidities in newly diagnosed COPD and asthma in primary care. Chest. 2005;128(4):2099–2107. doi: 10.1378/chest.128.4.2099. [DOI] [PubMed] [Google Scholar]
- 5.Agusti AG. Systemic effects of chronic obstructive pulmonary disease. Proc Am Thorac Soc. 2005;2(4):367–370. doi: 10.1513/pats.200504-026SR. [DOI] [PubMed] [Google Scholar]
- 6.Van Weel C, Schellevis FG. Comorbidity and guidelines: conflicting interests. Lancet. 2006;367(9510):550–551. doi: 10.1016/S0140-6736(06)68198-1. [DOI] [PubMed] [Google Scholar]
- 7.Eisner MD, Balmes J, Katz BP, Trupin L, Yelin E, Blanc P. Lifetime environmental tobacco smoke exposure and the risk of chronic obstructive pulmonary disease. Environ Health Perspect. 2005;4:7–15. doi: 10.1186/1476-069X-4-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Barnes PJ, Shapiro SD, Pauwels RA. Chronic obstructive pulmonary disease: molecular and cellular mechanisms. Eur Respir J. 2003;22(4):672–688. doi: 10.1183/09031936.03.00040703. [DOI] [PubMed] [Google Scholar]
- 9.Hogg JC. Pathophysiology of airflow limitation in chronic obstructive pulmonary disease. Lancet. 2004;364(9435):709–721. doi: 10.1016/S0140-6736(04)16900-6. [DOI] [PubMed] [Google Scholar]
- 10.Saetta M, Turato G, Maestrelli P, Mapp CE, Fabbri LM. Cellular and structural bases of chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2001;163(6):1304–1309. doi: 10.1164/ajrccm.163.6.2009116. [DOI] [PubMed] [Google Scholar]
- 11.Hogg JC, Chu F, Utokaparch S, Woods R, Elliott WM, et al. The nature of small-airway obstruction in chronic obstructive pulmonary disease. N Engl J Med. 2004;350(26):2645–2653. doi: 10.1056/NEJMoa032158. [DOI] [PubMed] [Google Scholar]
- 12.Cosio MG, Majo J. Inflammation of the airways and lung parenchyma in COPD: role of T cells. Chest. 2002;121(5 Suppl):160S–165S. doi: 10.1378/chest.121.5_suppl.160s. [DOI] [PubMed] [Google Scholar]
- 13.Hamzagić H. U: Savremene mogućnosti kliničke fiziologije disanja. Sarajevo: Univerzitetska knjiga; 1999. Testovi za ispitivanje plućne funkcije; pp. 116–259. [Google Scholar]
- 14.Cukic V, Lovre V, Dragisic D, Ustamujić A. Asthma and chronic obstructive pulmonary disease (COPD) - differences and similarities. Mater Sociomed. 2012 Jun;24(2):100–105. doi: 10.5455/msm.2012.24.100-105. [DOI] [PMC free article] [PubMed] [Google Scholar]


