ABSTRACT
The study is designed to evaluate the influence of remifentanil/propofol anesthesia on ventilator-associated pneumonia (VAP) occurrence and respiratory support (RS) time after major cardiac surgery.
Material and methods:
In retrospective-prospective study we investigated the respiratory support time and VAP occurrence in group of 47 patients with remifentanil/propofol and 35 patients with fentanil/midazolam anesthesia after major cardiac surgery in period June 2009–December 2011. Groups are divided in subgroups depending of who underwent cardiac surgery with or without cardiopulmonary by pass (CPB).
Results:
The time of respiratory support (RS) was the shortest in remifentanil group without CPB (R/Off 63min ± 44.3 vs R/On 94min ± 49.2 p=0,22), but was longer in fentanil group (F/Off 142 min ± 102.2 vs F/On 212 min ± 102.2 p=0.0014). The duration of RS of ON pump remifentanil group was shorter than in ON pump fentanil group (R/On 94 min vs F/On 212 min p=0.0011). The time of RS of OFF pump remifentanil group was lower than in Off pump entangle group (R/Off 63min ± 44,3 vs F/Off 142min ± 102.2 p=0,021) with statistically significance. Ventilator–associated pneumonia was detected in 7 patients (8.5 %). Six patients (17.1%) were from entangle group and one patient (2.1%) from remifentanil group. The most common isolates were Pseudomonas aeruginosa in all patients and both Pseudomonas aeruginosa and Klebsiella pneumonia in one patient.
Conclusion:
The remifentanil anesthesia regimen in cardiac surgery decreases length of respiratory support duration and can prevent development of VAP. The role of remifentanil anesthesia in preventing VAP, as one of the most important risk factor of in-hospital mortality after cardiac surgery is still incompletely understood and should be investigated further.
Keywords: remifentanil/propofol anesthesia, ventilator-associated pneumonia, cardiac surgery
1. INTRODUCTION
We investigated the influence of remifentanil anesthesia on the time of RS and ventilator associated pneumonia (VAP) occurrence after cardiac surgery. Most cases of VAP are caused by bacterial pathogens that normally colonize the oropharynx and gut, or that are acquired via transmission by health-care workers from environmental surface or from other patients (1). VAP is the main infectious complication in cardiac surgery patients and associated with an important increase in morbidity and mortality (2). VAP incidence in patients with RS increases with its duration. Incidence of VAP when patient is with RS is about 50% in first four days (3). VAP mortality range according literature is from 33% to 50%, and VAP patients have two times bigger mortality rate rather than the similar patients without VAP (4,5). Extended and long lasting cardio surgical procedures demand prolonged intubation and respiratory support especially in patients who underwent cardiopulmonary by-pass, postoperative bleeding, massive blood transfusion and inotrope treatment (6). So, the VAP in early postoperative period may reduce operative benefits. The remifentanil anesthesia regimen in cardiac surgery decreases length of respiratory support, staying in ICU and hospital and can prevent VAP development (7).
2. PATIENTS AND METHODS
We investigate the time of respiratory support and VAP occurrence in retrospective-prospective study of 35 consecutive patients who underwent major cardiac surgery with fentanil anesthesia in Clinic for Cardiovascular Disease, University Clinical Center Tuzla, and 47 patients who underwent major cardiac surgery with remifentanil anesthesia in Clinical Hospital Mostar in period June 2009- December 2011.
Patients were divided in two groups. In the first fentanil (F) group induction agents were: fentanil (20-50 mcg/kg), midazolam (0.1-0.3mg/kg), pancuronium (0,04-0,08 mg/kg). Support agent for F group were: midazolam (3-4 mg /kg /h), fentanil 120-150 mcg/h, pancuronium 2 mg/h, and sevofluran MAC do 2 vol%. Remifentanil (R) group induction agents were the same as in F group, but support agent was propofol (50-100 mcg/kg/min) and remifentanil (0,1-2 mcg/kg/min). The group R of patients had 5mg diazepam iv and 5mg metamizol iv in ICU at admitting time. All patients were under standard preoperative procedure with central vena cava catheter. Samples of arterial blood gas analysis were taken from a catheter placed in the radial artery by Selding-ers technique. All patients had non-complicated intubation and ICU extubation.
We divided groups in two subgroups according to the using of CPB (Remifentanil On pump group and Fentanil On pump group) and two groups without using CPB (Remifentanil Off pump group and Fentanil Off pump group). In all groups we followed up the duration of respiratory support and noted microbiology verified VAP in early postoperative period. We excluded patients with ejection fraction under 40%, candidates for emergency surgery and patients who had preoperative inotrope therapy and blood transfusion.
3. RESULTS
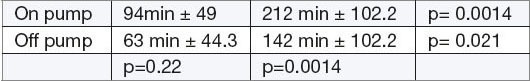
The study included 82 adults (47 patients in remifentanil and 35 patient in fentanil group). The two groups were similar with indication for surgery and duration anesthesia. There were 23 female patients (28%), 13 in remifentanil group and 10 in fentanil group, and 59 male patients (71.9 %), 34 (72.3%) from R group and 25 (71.4%) from F group. Mean age of male patients was 53.35±9.92 (range 45-74) and of female patients was 59,20±10.07 (range 54-75) with overall mean age 57.45±10.07 and range 45-75 years. The time of respiratory support (RS) was the shortest in remifentanil group without CPB (R/Off 63 min ± 44,3 vs R/On 94min ± 49,2, p=0,22), but was longer in fentanil group (F/Off 142 min ± 102,2 vs F/On 212 min ± 102,2 p=0,0014). The duration of RS of ON pump remifentanil group was shorter than in ON pump fentanil group (R/On 94 min vs F/On 212 min, p=0.0011). The time of RS of OFF pump remifentanil group was lower than in Off pump fentanil group (R/Off 63 min ± 44,3 vs F/Off 142 min ± 102,2, p=0,021) with statistically significance. All patients underwent CPB were longer time on respiratory support than patients without CPB. The results are showed in table 1.
Table 1.
R-group F-group
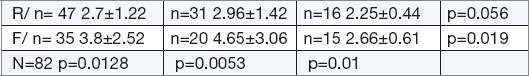
Two (4.7 %) patients from R group and 4(11.4 %) patients from F group had inotrope therapy. Ventilator–associated pneumonia were detected in 7 patients (8.5 %) after cardiac surgery, 6 patients (17.1%) from F (fentanil) group and 1 patient (2,1%) from R (Remifentanil) group. All of them were male. The most common isolates were Pseudomonas aeruginosa in all patients and both Pseudomonas aeruginosa and Klebsiella pneumonia in one patients. All patients with VAP received blood transfusion after surgery. There was no significance of CPB duration between Remifentanil and fentanil group (F 93.8 min± 6.53 vs R 89.6 min ± 7,9, p= 0,38). The time in ICU for Remifentanil group was 2.7±1.22 day and 3.8 ±2.52 for Fantail group with significance (p=0.0128). Patients from Remifentanil On pump group were 2.96±1,42 days, and patients from Remifentanil Off pump group were 2.25±0.22 days in ICU with no significance (p=0.056). The results are showed in Table 2.
Table 2.
On pump Off pump
4. DISCUSSION
VAP is leading cause for nosocomial mortality and morbidity (8). Patients undergoing heart surgery have higher frequency of developing VAP, especially in patients that require more than 48 hours of mechanical ventilation and is associated with high in-hospital mortality (7). Remifentanil may be beneficial in patients undergoing cardiac surgery because of provided safe and stable operating conditions and earlier tracheal extubation (9). Shorter time of respiratory support decreases risk for VAP occurrence.
CPB using in heart surgery increases intubation period and length of stay in ICU, but remifentanil decreases that periods. VAP incidence increases with longer period of respiratory support. Process of intubation, alone, is risk factor, but VAP incidence in noninvasive treatments is significantly lower. Perioperative and postoperative transfusion, reintubation and prolonged mechanical ventilation are independent risk factors for VAP in patients following cardiac surgery (10). Cardiac surgery without CPB decreases postoperative blood transfusion necessity. VAP patients have two time’s bigger mortality rate rather than the similar patients without VAP. The average ICU and in hospital time is longer for VAP patients about 4 to 13 days (4). One of the ways to decrease respiratory support time is using short-acting anesthetics to enable fast postoperative recovery. Remifentanil is ultra-short acting opioid and postoperative pain management should be planned carefully.
5. CONCLUSSION
Remifentanil/propofol anesthesia using in major cardiac surgery decreases respiratory support time and risk of VAP occurrence. We showed that risk factors for VAP occurrence are longer respiratory support time and cardiac surgery with CPB. Blood transfusion has important role and should be considered. The shortest length of stay in ICU had patients who underwent remifentanil anesthesia regimen in major cardiac surgery without CPB.
Footnotes
CONFLICT OF INTEREST: NONE DECLARED
REFERENCES
- 1.Park DR. The microbiology of ventilator-associated pneumonia. Res Care. 2005 Jun;50(6):763–765. [PubMed] [Google Scholar]
- 2.Tamayo E, Alvarez FJ, Martinez-Rafael B, Bustamante J, Bermejo-Martin JF, Fierro I, Eiros JM, Castrodeza J, Heredia M, Gomez-Herreras JI. Valladolid Sepsis Group. J Crit Care. 2012 Feb;27(1):18–25. doi: 10.1016/j.jcrc.2011.03.008. doi: 10.1016/jcrc. 20110.3008. Epub 2011 May 18. [DOI] [PubMed] [Google Scholar]
- 3.Bouza E, Perez A, Munoz A. Ventilator-associated pneumonia after heart surgery: a prospective analysis and the value of surveillance. Crit Care Med. 2003;32:1964–1970. doi: 10.1097/01.ccm.0000084807.15352.93. [DOI] [PubMed] [Google Scholar]
- 4.Sheng W, Chi YF, Hou WM, Sun L, Niu ZZ, Sun Y, Lin MS. Clinical analysisi of 105 of ventilatory-associated pneumonia after heart surgery. Zhonghua Xin Xue Guan Bing Za Zhi. 2012 Oct;40(10):825–829. [PubMed] [Google Scholar]
- 5.Wojkowska-Mach J, Baran M, Drwila R, Foryciarz E, Misiewska-Kaczur A, Romaniszyn D, Heczko PB. Ventilator-associated pneumonia after cardiac surgery. Anestezjol Intens Ter. 2009 Oct-Dec;41(4):224–229. [PubMed] [Google Scholar]
- 6.Pawar M, Meta Y, Khurana P, Chaudhary A, Kulkarni V, Trhan N. Ventilator-associated pneumonia: Incidence, risk factors, outcome, and micribiology. J Cardithorac Vasc Anesth. 2003 Feb;17(1):22–28. doi: 10.1053/jcan.2003.4. [DOI] [PubMed] [Google Scholar]
- 7.Lison S, Schill M, Conzen P. Fast-track cardiac anesthesia: efficacy and safety of remifentanil versus sufentanil. J Cardithorac Vasc Anesth. 2012 Feb;21(1):35–40. doi: 10.1053/j.jvca.2006.03.011. [DOI] [PubMed] [Google Scholar]
- 8.Lehmann A, Zeitler C, Thaler E, Isgro F, Boldt J. Comparison of two different anesthesia regimens in patients undergoing aortocoronary by-pass grafting surgery: Sufentanil-midazolam versus remifentanil-propofol. J Cardithorac Vasc Anesth. 2000 Avg;14(4):416–420. doi: 10.1053/jcan.2000.7945. [DOI] [PubMed] [Google Scholar]
- 9.Hortal J, Munoz P, Cuerpo G, Litvan H, Rossel PM, Bouza E Europen study Group on Nosocomial Infections; European Work Group of Cardiothoracic Intensivits. Crit Care. 2009;13(3) doi: 10.1186/cc7896. doi: 10.1186/cc7896. Epub 2009 May 22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Parker CM, Kutsogiannis J, Muscedere J. Ventilator-associated pneumonia caused by multidrug-resistant organisms or Pseudomonas aeruginosa: prevalence, incidence, risk factors, and outcomes. J Crit Care. 2008 Mar;23(1):18–26. doi: 10.1016/j.jcrc.2008.02.001. [DOI] [PubMed] [Google Scholar]


