ABSTRACT
Background:
In most countries chronic diseases lead to high health care costs and reduced productivity of people in society. The best way to reduce costs of health sector and increase the empowerment of people is prevention of chronic diseases and appropriate health activities management through monitoring of patients. To enjoy the full benefits of E-health, making use of methods and modern technologies is very important.
Methods:
this literature review articles were searched with keywords like Patient monitoring, Mobile Health, and Chronic Disease in Science Direct, Google Scholar and Pub Med databases without regard to the year of publications.
Results:
Applying remote medical diagnosis and monitoring system based on mobile health systems can help significantly to reduce health care costs, correct performance management particularly in chronic disease management. Also some challenges are in patient monitoring in general and specific aspects like threats to confidentiality and privacy, technology acceptance in general and lack of system interoperability with electronic health records and other IT tools, decrease in face to face communication between doctor and patient, sudden interruptions of telecommunication networks, and device and sensor type in specific aspect.
Conclusions:
It is obvious identifying the opportunities and challenges of mobile technology and reducing barriers, strengthening the positive points will have a significant role in the appropriate planning and promoting the achievements of the health care systems based on mobile and helps to design a roadmap for improvement of mobile health.
Keywords: Patient monitoring, Challenge, Advantage, Mobile Health, Chronic Disease
1. INTRODUCTION
In most countries chronic diseases lead to high health care costs and reduced productivity of people in society (1). In recent years, heart disease has been a major widespread public health problem in most countries. Heart disease is costly for healthcare systems in many countries (2). Diabetes is another common chronic disease in nearly all countries (2) and one of the most common metabolic diseases with an increasing incidence. Diabetes care may account for up to 15% of national health care budgets. (3) In chronic disease patients if monitoring of health situation is done with high quality in coordination with nutrition program and physician orders, the quality of care will improve dramatically (4). Modern technology tools should be used to the best advantage to reduce costs of health sector, increase the empowerment of people, improve the monitoring of patients through continuous assessment of symptoms and signs of disease and checking compliance with self-management programs and prevention of chronic diseases(5). Telemedicine is a main tool to remote health care delivery and home care. Fast and timely access to health information (6, 7), reduce medical errors (8), and increase coordination among health care professionals (9), reduce travelling and physical presence of patients in urban health centers in remote areas (10), education to patients and providers, (11) are some of the advantages of this technology in health domain. To gain full benefits of E-Health, making use of methods and modern technologies is very important. One of the innovations in the field of information technology in healthcare applications is mobile health systems. Apply remote medical diagnosis and monitoring system based on mobile health systems provides doctors and health care professionals access to central database and patient information. Mobile health could be a solution to overcome barriers of health service personnel, timely access to health information related to patient especially in emergency situations and prevent tests duplication, delay and error in suitable treatment to patient (10, 12).
While there is a potential advantage for mobile health programs, many challenges exit for developing and implementing these tools. Accordingly effective use of mobile devices in health systems requires extensive research and investigation of different aspects. One of these dimensions is study the benefit and obstacles of mobile devices. It is obvious identifying the opportunities and challenges of mobile technology and reducing barriers, strengthening the positive points will have a significant role in the appropriate planning and promoting the achievements of the health care systems based on mobile and helps to design a roadmap for improvement of mobile health.
2. M-HEALTH OPPORTUNITIES IN PATIENT MONITORING
Various systems are used to monitor the condition of patients with chronic disease. Regarding the researches we can say two type of eHealth systems use mobile devices for chronic diseases management, agent based systems and without agent.
Electronic systems without agent technology that mentioned in table 1 have advantages like: primary preventive, facilitate self-care, promotion quality of people life style, prevent unnecessary (re)hospitalizations, tele consultation, and provide full or some mobility for patients to do routine daily works.
Table 1.
Electronic Health System Characteristics in Chronic Disease Management
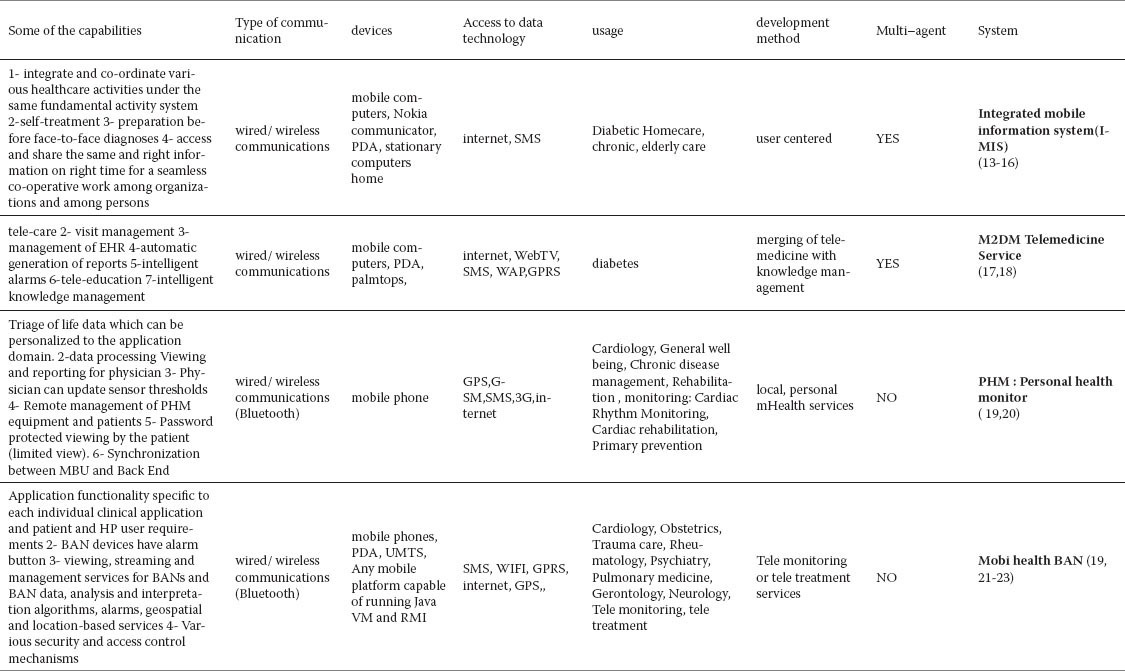
Local processing in the PHM system lead to exceeded the capacity of the mobile device and increase cost; but MobiHealth BAN transmit its data to a remote system or user and data processing can be applied at the server side.
Some of systems in table 1, implemented on a number of different PDAs and mobile phone platforms and others implemented on mobile phone. PDA with laptop and desktop computer can establish clear and transparent data sharing. Share data done through the user interface and function with ability of calculation and input and output devices that are compatible with other tools. Of course user interface design in PDA is associated with limitations such as resolution, small screen size, limited use of color and processing power, small-sized keyboard and mouse replacement with stylus pen.
In some of them is possible alarm to patient and/or provider, identify place of patient in emergency situation through GPS, patients access to some data. Mobile communication links against weather conditions and geographical status is vulnerable.
GSM provide easy access to telemedicine services without creating a private network for communications or spend large money but have bandwidth limitation and sometime lead to loss of information which is useful for health service professionals. 3G technologies are suitable for development national e-health systems based on Mobile with optimal cost. GPRS don’t have widely coverage and only be supported by the network service provider. UMTS when it is fully implemented can provide interoperability between networks, have nationwide coverage but is associated with challenges such as battery life tools and functional expenses.
Mobility requires the use of wireless devices. Devices are not wireless that cannot be fully mobile. When wireless communications coverage is expensive, system can use wired communications.
Recently health care systems shift towards high speed access to accurate health information and online health services, high quality health care, shared information to better decision-making. Dynamic health environment needs to high interoperability among professionals with different skills, various specialty and complicated process. Hence applying technology devices in this field is facing a lot of challenges.
For providing effective health care and shared information, all actions need to be coordinated. Interoperability and effective communication between professionals is necessary to facilitate decision making. In this way medical errors is reduced and quality of remote health care will be increased. To meets these needs, eHealth systems must be proactive in anticipating the health information needs, deliver it timely, support communications, and facilitate coordination among providers involved in delivering health services.
Agents’ researches are one of the new technologies in artificial intelligence areas, especially in the generation of practical solutions for real problems. One of the characteristic of agent is mobility, which is suitable for telemedicine and E-Health systems (24). Agents have the potential to assist in a wide range of activities in health care environments.
Study of agent- based systems that mentioned in table 1 and articles about the multi-agent systems shows that agents can maintain the autonomy of the collaborating participants, improve the performance of a computerized system in terms of interoperability, scalability and re configurability, integrate disparate operating environments, coordinate distributed data, such as patient records held in different departments within a hospital or in several hospitals. Also agent systems dynamically manage distributed data and resources, handle the complexity of solutions through decomposition, modeling and organizing the interrelationships between components. Agents are able to communicate between themselves in order to exchange any kind of information, provide remote care monitoring and information for elder people and chronic diseases, supply diagnosis decision-support, improve remote medical training and E-education; gather, compile and organize medical knowledge available on the Internet (13-18, 25-28).
IMIS system improves diabetics’ health care management with coordination mechanism through communication between agents, shared information, task delegation. Knowledge agent in M2DM system combined different analytic ways to diabetic monitoring data. So this system is very appropriate for identification intensity of abnormality, user awareness about data analysis results and alarms, providing real time feedback to patients, focuses patients and physician on future risk situations and prevent of them (13-18). Both agent systems use the web service to interact with different systems and provide various needs of users.
Agents apply for monitor certain procedures and signals in real world and react to anomalies situations. Agents run on the portable devices with limited capacity of gathering like PDA. These systems are generally based on the knowledge that are used to interpret data gained and identify anomalies.
As a whole according to multi agent health systems advantages in comparative other type of systems and challenges in health care systems, we can say use of agent as a new and modern technology to gain full advantages of E-Health is necessary and health systems must to move using agent-based applications.
3. M-HEALTH CHALLENGES IN PATIENT MONITORING
In spite of powerful role of mHealth, there are challenges in general and specific aspects associated with the use of technology. Some of the most common general difficulties are: organizational and technological barriers (29); user attitudes, technology acceptance (30, 31), and threats to confidentiality and privacy, legal, ethical and administrative barriers, costs of system implementation and maintenance (32), costly modern systems (33), sufficient investment (34). Also the most important challenges in specific aspects are poor design and implementation, lack of system interoperability with electronic health records and other IT tools (35), system compatibility with personal tasks (36), decrease in face to face communication between doctor and patient (37), ill-functioning of system that leads to medical errors and negative effects on care outcomes, patients and personnel (38), mistakes in documentation (35) e.g. data manipulation and re-writing, misrepresentation, and violation of patients’ legal rights. factor related to the tele communication industry include: reliability, sustainability of connections, sudden interruptions of telecommunication networks (39), scalability in terms of data rate and power and energy consumption; antenna design, quality of service(Qos), energy efficiency (40,41) weight of wearable devices, difficulty in some data processing due to the devices used in patient monitoring, the location of data collected which affects to accuracy of information, user training to use wearable system, wearable system market penetration (42).
4. DISCUSSION
Health care system faced with challenges such as weak interoperability and coordination among providers involved in patient treatment, sharing information and so on. Use of different electronic health systems in chronic diseases management has important advantages. Of course these systems have some limitations. In this article we classify chronic disease management systems in 2 groups: agent-based system and none agent. None agent systems have remarkable advantages like: improve quality of people life style, tele consultation, primary prevention, promotion self –care. Also they confront some limits. Dynamic health environment needs high speed access to real-time health information, high interoperability among different providers with various skills. Use of agent as a new and modern technology to benefit full advantages of E-Health is necessary and health systems must to move using agent-based applications.
Agent-based systems improve interoperability, maintain the autonomy of the collaborating participants, and communicate between themselves for exchange health information. Multi agent systems are inherently compatible with mobile devices. Architecture of these systems allows high interoperability and quality information management and appropriate sharing data. For accelerate chronic disease management systems based on artificial intelligence tools must be consider these items as following: 1- cultural readiness 2- provides the technical infrastructure required 3- application of appropriate mechanisms for security and privacy 4- appropriate investment 5- user involvement 6- private sector participation. In addition to these, in agent-based chronic disease management system structure, design and create a database backup has particular importance and a rich database must be designed in order to provide support of various training formats and tasks. Also for the users, especially elderly people to make use of the system special attention should be paid to the ease of use and user friendliness. Use of reminders for patients about drug use and injection in addition to the built-in alarm system is also very important.
In deliver health care to chronic disease patient, considering social and human aspects and having systematic view is essential. Paying attention to all aspects such as: feedbacks, budget, motivation, hierarchy, and useful standards, individual's affordability, identification barriers and opportunity and so on are necessary. Also stakeholder's support to use of technology is very important.
5. CONLUSION
It is certain that application of existing technologies in the field of patient monitoring has significant benefits for communities. Select any one of these technologies in national level should be based on greater understanding of these tools, compare their advantages and disadvantages, and in accordance with the conditions, technical, human and financial resources in health care organizations, affordability of these facilities, strategic needs and challenges take place. It is obvious that proper application of each of these systems in the country is provided with identify and resolve technical and non-technical challenges that are playing a vital role in the successful implementation of these technologies; realize the benefits of these technologies. The successful implementation of mobile-based systems is constantly faced with challenges such as: increasing the accuracy of critical signals, interoperability between different systems, bandwidth limitations, quality of health services, battery life limited tools and so on.
Providing appropriate technical and information infrastructure such as adequate bandwidth, preparation of standard tools that provide maximum mobility and flexibility for users, decreasing obstacles which interrupt network communications, use suitable communication protocol, cost of purchasing and using, insurance coverage and supporting patients that uses remote monitoring devices, adoption of adaptable wireless technologies, data encryption while transferring, paying attention to legal and ethical aspects, user friendly, allowing the interaction between the system components, nomination and establishment of rules, guidelines and standards and proper policies regarding the use of these technologies particularly with respect to privacy and data security while sending critical patient signals are all important in the successful application of these systems across the country that should be considered.
Footnotes
CONFLICT OF INTEREST: NONE DECLARED
REFERENCES
- 1.Engelgau M, Rosenhouse S, El-Saharty S, Mahal A. The Economic Effect of Noncommunicable Diseases on Households and Nations: A Review of Existing Evidence. Journal of Health Communication: International Perspectives. 2011;16(2):75–81. doi: 10.1080/10810730.2011.601394. [DOI] [PubMed] [Google Scholar]
- 2.Mohammadzadeh M, Safdari R, Rahimi A. Multi-Agent System as a New Approach to Effective Chronic Heart Failure Management: Key Considerations. Healthc Inform Res. 2013 Sep;19(3):162–166. doi: 10.4258/hir.2013.19.3.162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zhang P, Zhang X, Brown J, Vistisen D, Sicree R, Shaw J, Nichols G. Global healthcare expenditure on diabetes for 2010 and 2030. Diabetes research and clinical practice. 2010;87(3):293–301. doi: 10.1016/j.diabres.2010.01.026. [DOI] [PubMed] [Google Scholar]
- 4.McAndrew LM, Napolitano MA, Pogach LM, Quigley KS, Shantz K, Vander Veur SS, Foster GD. The Impact of Self-monitoring of Blood Glucose on a Behavioral Weight Loss Intervention for Patients with Type 2 diabetes. The Diabetes Educator. 2013;39(3):397–405. doi: 10.1177/0145721712449434. [DOI] [PubMed] [Google Scholar]
- 5.Paré G, Moqadem K, Pineau G, St-Hilaire C. Clinical Effects of Home Tele monitoring in the Context of Diabetes, Asthma, Heart Failure and Hypertension: A Systematic Review. J Med Internet Res. 2010;12(2):e21. doi: 10.2196/jmir.1357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Barjis J, Kolfschoten G, Maritz J. A Sustainable and Affordable Support System for Rural Healthcare Delivery. Decision Support Systems. Available online 24 June 2013. In Press, Accepted Manuscript - Note to users. http://dx.doi.org/10.1016/j.dss.2013.06.005 .
- 7.Tan J. Medical Informatics: Concepts, Methodologies, Tools, and Applications. Securing Mobile Data Computing in Healthcare. 2009;1(Chapter 7.5):1930. [Google Scholar]
- 8.Skolnik NS. New York: Springer Humana Press; 2011. Electronic Medical Records A Practical Guide for Primary Care; p. 1. [Google Scholar]
- 9.Safdari R, Mohammadzadeh N. Tehran, Iran: Lecture in 2nd eHospital and Telemedicine Conference. Tehran University of Medical Sciences; 2011. Multi–agent systems and health information management. [Google Scholar]
- 10.Finn N, Bria W. London: Springer-Verlag; 2009. Digital Communication in Medical Practice; pp. 70–73. [Google Scholar]
- 11.Toledo FG, Triola A, Ruppert K, Siminerio LM. Telemedicine Consultations: An Alternative Model to Increase Access to Diabetes Specialist Care in Underserved Rural Communities. JMIR Res Protoc. 2012;1(2):e14. doi: 10.2196/resprot.2235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.McDaniel J. Amsterdam: IOS Press; 2009. Advances in information technology and communication in health; pp. 467–471. [Google Scholar]
- 13.Integrated mobile information- research. 2010. [Accessed 4 July 2013]. http://www.bth.se/research/imis/
- 14.Integrated mobile information. 2010. [Accessed 4 July 2013]. http://www.bth.se/research/imis/
- 15.Shaheen A, Ahmad khan W. Master Thesis. Computer Science. Sweden: Blekinge Institute of Technology; 2009. [Accessed 4 July 2013]. Intelligent Decision Support System in Diabetic eHealth Care From the perspective of Elders. http://www.bth.se/fou/cuppsats.nsf/all/89449be91369ee27c12575d60071c747/$file/Master_thesis_asma.pdf . [Google Scholar]
- 16.Zhang P. Blekinge Institute of Technology Licentiate Series. 5. Karlskrona: Blekinge Institute of Technology; 2005. [Open Document Accessed 4 July 2013]. Multi-agent Systems in Diabetic Health Care. ISBN: 91-7295-060-9. http://www.bth.se/fou/forskinfo.nsf/all/07625d65f3f89ee6c1256fef00220c36? [Google Scholar]
- 17.Bellazzi R, Carson ER, Cobelli C, Hernando E, Gomez EJ, Nabih-Kamel-Boulos M, Rendschmidt T, Roudsari V, et al. Vol. 4. Published in: Engineering in Medicine and Biology Society. Proceedings of the 23rd Annual International Conference of the IEEE; 2001. Merging Telemedicine With Knowledge Management: The M2DM Project; pp. 4117–4120. doi: 10.1109/IEMBS.2001.1019762. [Google Scholar]
- 18.Hernando ME, Garsia A, Javiar Perdices F, Torralba V, Gomez EJ, del Pozo F. Multi agent architecture for the provision of intelligent telemedicine services in diabetes management. [Accessed 4 July 2013]. http://cyber.felk.cvut.cz/EUNITE03-BIO/pdf/EHernando.pdf .
- 19.Jones V, Gay V, Leijdekkers P. Published in: Digital Society. ICDS ’ 10. Fourth International Conference on February; 2010. Body sensor networks for mobile health monitoring: experience in Europe and Australia. [Google Scholar]
- 20.Leijdekkers P, Gay V. 21st IEEE International Symposium on Computer-Based Medical Systems; 2008. A Self-Test to Detect a Heart Attack Using a Mobile Phone and Wearable Sensors; pp. 93–98. ISBN: 978-0-7695-3165-6. [Google Scholar]
- 21.Otto C, Milenkovic A, Sanders C, Jovanov E. System Architecture of a Wireless Body Area Sensor Network for Ubiquitous Health Monitoring. Journal of Mobile Multimedia. 2006;1(4):307–326. [Google Scholar]
- 22.Halteren Aart V, Bults R, Wac K, Konstantas D, Widya I, Dokovsky N, Koprinkov G, Jones V, Herzog R. Mobile Patient Monitoring: The MobiHealth System. The Journal on Information Technology in Healthcare. 2004;2(5):365–373. [PubMed] [Google Scholar]
- 23.MobiHealth–Shaping the Future of Healthcare. [Accessed 4 July 2013]. http://www.ltu.se/cms_fs/1.90345!/file/Mobihealth%20brochure.pdf .
- 24.Annicchiarico R, Cortés U, Urdiales C. Switzerland: Birkhäuser Verlag; 2008. Agent Technology and e-Health; pp. 141–148. [Google Scholar]
- 25.Isabelle B, Sachin V, Ashlesha J, Lakhmi J. Berlin: Springer-Verlag; 2010. Computational Intelligence in Healthcare 4; pp. 25–48. [Google Scholar]
- 26.Mohammadzadeh N, Safdari R. Artificial Intelligence Tools in Health Information Management. International Journal of Hospital Research. 2012;1(1):65–70. [Google Scholar]
- 27.Isern D, Sánchez D, Moreno A. Agents applied in health care: A review. International journal of medical informatics. 2010;79:145–166. doi: 10.1016/j.ijmedinf.2010.01.003. [DOI] [PubMed] [Google Scholar]
- 28.Safdari R, Mohammadzadeh N. Electronic Health Information Systems. Mirmah, Tehran. 2011:152–156. in Persian. [Google Scholar]
- 29.Cripps H, Standing C. The implementation of electronic health records: A case study of bush computing the Ngaanyatjarra Lands. International journal of medical informatics. 2011;80(12):841–848. doi: 10.1016/j.ijmedinf.2011.09.007. [DOI] [PubMed] [Google Scholar]
- 30.Cresswell K, Sheikh A. Organizational issues in the implementation and adoption of health information technology innovations: An interpretative review. International journal of medical informatics. 2013;82(5):e73–86. doi: 10.1016/j.ijmedinf.2012.10.007. [DOI] [PubMed] [Google Scholar]
- 31.Venkatesh V, Thong JY L, Xu X. Consumer Acceptance and Use of Information Technology: Extending the Unified Theory of Acceptance and Use of Technology. Forthcoming in MIS Quarterly. 2012;36(1):157–178. [Google Scholar]
- 32.Mohammadzadeh N, Safdari R, Rahimi A. Cancer Care Management through a Mobile Phone Health Approach: Key Considerations. Asian Pac J Cancer Prev. 2013;14(9):4961–4964. doi: 10.7314/apjcp.2013.14.9.4961. [DOI] [PubMed] [Google Scholar]
- 33.Blumenthal D. Stimulating the Adoption of Health Information Technology. N Engl J Med. 2009;360:1477–1479. doi: 10.1056/NEJMp0901592. [DOI] [PubMed] [Google Scholar]
- 34.Lucas H. Information and communications technology for future health systems in developing countries. Social Science & Medicine. 2008;66:2122–2132. doi: 10.1016/j.socscimed.2008.01.033. [DOI] [PubMed] [Google Scholar]
- 35.Lawler EK, Hedge A, Pavlovic-Veselinovic S. Cognitive ergonomics, socio-technical systems, and the impact of healthcare information technologies. International Journal of Industrial Ergonomics. 2011;41:336–344. [Google Scholar]
- 36.Viitanen J, Hyppönen H, Lääveri T, Vänskä J, Reponen J, Winblad I. National questionnaire study on clinical ICT systems proofs: Physicians suffer from poor usability. International journal of medical informatics. 2011;80(10):708–725. doi: 10.1016/j.ijmedinf.2011.06.010. [DOI] [PubMed] [Google Scholar]
- 37.Lluch M. Healthcare professionals’ organizational barriers to health information technologies-A literature review. International journal of medical informatics. 2011;80(12):849–862. doi: 10.1016/j.ijmedinf.2011.09.005. [DOI] [PubMed] [Google Scholar]
- 38.Nykänen P, Brender J, Talmon J, de Keizer N, Rigby M, Beuscart-Zephir M, Ammenwerth E. Guideline for good evaluation practice in health informatics (GEP-HI) International journal of medical informatics. 2011;80:815–827. doi: 10.1016/j.ijmedinf.2011.08.004. [DOI] [PubMed] [Google Scholar]
- 39.Aggarwal Neil K. Applying mobile technologies to mental health service delivery in South Asia. Asian Journal of Psychiatry. 2012;5:225–230. doi: 10.1016/j.ajp.2011.12.009. [DOI] [PubMed] [Google Scholar]
- 40.Patel M, Jianfeng Wang. Applications, challenges, and prospective in emerging body area networking technologies. Wireless Communications, IEEE. 2010;17(1):80–88. [Google Scholar]
- 41.Klingeberg T, Schilling M. Mobile wearable device for long term monitoring of vital signs. Computer methods and programs in biomedicine. 2012;106:89–96. doi: 10.1016/j.cmpb.2011.12.009. [DOI] [PubMed] [Google Scholar]
- 42.Chan M, Estève D, Fourniols J, Escriba C, Campo E. Smart wearable systems: Current status and future challenges. Artificial Intelligence in Medicine. 2012;56:137–156. doi: 10.1016/j.artmed.2012.09.003. doi: 10.1016/j.artmed.2012. [DOI] [PubMed] [Google Scholar]


