ABSTRACT
Introduction:
Fracture of the femoral shaft is a common fracture encountered in orthopedic practice. In the 1939, Küntscher introduced the concept of intramedullary nailing for stabilization of long bone fractures. Intramedullary nailing has revolutionized the treatment of fractures.
Material and methods:
The study included 37 male patients and 13 female patients, averaged 39±20,5 years (range, 16 to 76 years).
Results and discussion:
There were 31 left femurs and 21 right femurs fractured. 46 fractures were the result of blunt trauma. Low energy trauma was the cause of fractures in six patients, of which five in elderly females. 49 fractures were closed. Healing time given in weeks was 19,36 ± 6,1. The overall healing rate was 93,6%. There were three (6,25%) major complications nonunion. There were one (2%) delayed union, one (2%) rotational malunion and no infection. The shortening of 1 cm were in two patients. Antercurvatum of 10 degrees was found in one patient. There was no statistically significant reduction of a motion in the hip and knee (p<0.05). There was statistically significant in the thigh (knee extensors) muscle weakness (p<0.001).
Conclusion:
Intramedullary nailing is the treatment of choice for femoral shaft fractures.
Keywords: fracture, femoris, unreamed, nails, union
1. INTRODUCTION
Fracture of the femoral shaft is a common fracture encountered in orthopedic practice, and it is often associated with other injuries. Since the femur is the longest and largest bone in the body and one of the most important supporting bone of the lower limb, the femur fracture will result in prolonged morbidity and significant disability regardless of adequate treatment (1).
In the 1939, Küntscher introduced the concept of intramedullary nailing for stabilization of long bone fractures (2). Intramedullary nailing has revolutionized the treatment of fractures. Antegrade femoral nailing (passing the intramedullary nail from proximal to distal) is the gold standard for surgical treatment of femoral shaft fractures. It has a high rate of union (99%) and a low rate of infection and malunion (<1%) (3, 4).
Femoral shaft fractures are most commonly the result of high energy trauma in the young adult population and may be associated with multiple system injuries. Early fixation by closed intramedullary nailing is the currently preferred method of treatment of fractures of the shaft of the femur in multiply injured patients (5).
The piriformis fossa and greater trochanter are viable starting points for antegrade nailing. Alternatively, retrograde nailing may be performed. Each option has relative advantages, disadvantages, and indications. Patient positioning can affect the relative ease of intramedullary nailing and the incidence of malalignment. The timing of femoral intramedullary nailing as well as the use of reaming must be tailored to each patient to avoid systemic complications. Associated co morbidities, the body habitus, and associated injuries should be considered when determining the starting point, optimal patient positioning for nailing, whether to use reduction aids as well as which to use, and any modifications of standard technique. This method yields high union rates and low complication rates when vigilance is maintained during preoperative planning, the surgical procedure, and the postoperative period. Regardless of the treatment method chosen, the following principles are agreed on: restoration of alignment, rotation, and length; preservation of the blood supply to aid union and prevent infection; and rehabilitation of the extremity and the patient (6).
2. AIM OF STUDY
To identify complications, time of healing and functional recovery in the treatment of femoral shaft fractures with unreamed intramedullary nails.
3. PATIENTS AND METHODS
The study was a retrospective-prospective and analyzed all the patients with fractures of the femoral shaft treated with unreamed IM nailing at the Clinic of Orthopedic and Traumatology, University Clinical Centre Tuzla from January 2000 to December 2009. Pathological fractures and nailing after corrective osteotomy, and those patients who continued treatment at other institutions because of a great migration in the post- war period, were also excluded from the study. The initial study population was 61 but 11 patients were excluded because of the above reasons. Four additional patients were referred to us from other institutions, of which two patients with plate fractures in the early postoperative period (after 8 weeks), and two with an external fixation (3 and 6 weeks), of which one patient with an external fixation at both femurs. Two patients had a bilateral femur fractures.
Closed unreamed antegrade intramedullary nails were placed in all of the patients with the exception of two patients with plate fractures. Nailing in the retrograde manner was performed in two patients, of which one for separated treatment of hip fractures, and other for pelvic fractures. The fracture table was used in all cases and nailing was performed in the antegrade manner using the piriformis entry point. All nails were statically locked. The supine position and general anesthesia were used in all of the patients. We used a free-hand technique in performing distal locking of intramedullary nails.
Radiographs were examined to assess the fracture type, post-reduction deformity and union. The minimum length of follow up was one year (range one year to five years). Control radiography were performed in the period 6-8 weeks. Union was defined as radiographic bridging at least 3 of 4 cortices on 2 orthogonal views and as lack of pain during weight bearing. Nonunion was defined by routine clinical and radiological criteria, and the need for a further surgical procedure. The absence of the radiologic features of fracture healing after nine months represents delayed union. Malalignment are defined as shortening or extending of the leg bigger than 1 cm, angulation of 10 degrees and more in any plane, and when the rotation is bigger than 15 degrees. Measurement of shortening or extending the leg is performed with the patient supine and the pelvis squared, a tape measure was used to measure the difference in the distance between the anterior superior iliac spine (ASIS) and medial malleolus. A block test was performed where the patient was asked to stand with a raise under the short leg until the leg length was corrected (using patient perception and assessment of ASIS heights). The block height was then measured using increments of 5 mm. Measurement of mobility in the hip and knee and the thigh (knee extensors) muscle weakness were conducted after clinical and bone consolidation, i.e. at the last check- up. The movements of the hip and knee were measured using a goniometer by comparing the injured and healthy leg. Hypotrophy of the thigh muscles was measured using a centimeter ruler by measuring the size 10 cm above the knee joint of injured and healthy leg.
Postoperative management with regard to weight-bearing and the range of motion of the extremity was individualized according to the fracture configuration and stability, the size of the implant, and associated injuries. The time to full weight-bearing was individualized for each patient and depended on the cortical contact of the major fragments, the presence of bridging callus as seen on radiographs, and the extent of other injuries.
There were nailing procedures with a Gross-Kempf (Howmedica), AO Universal Synthes, AO titanium Aesculap nail.
4. RESULTS
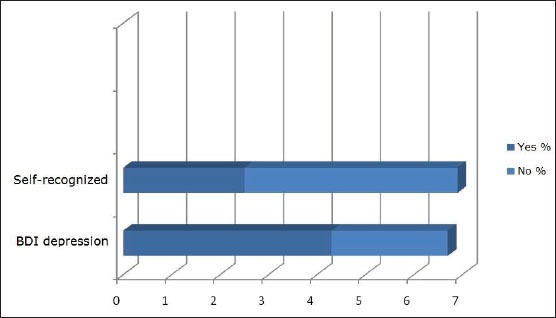
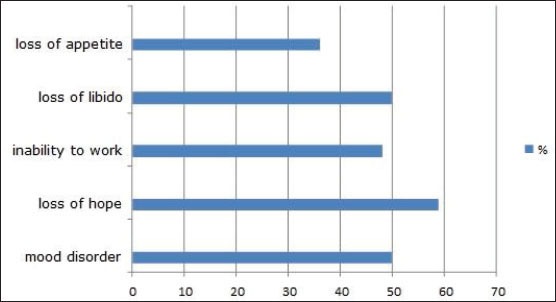
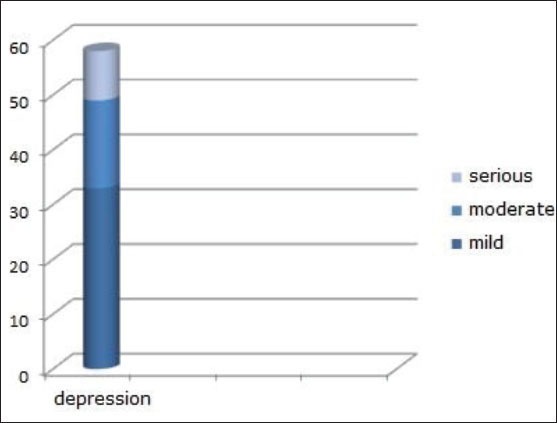
One death occurred one month after the date of injury and after intracerebral hemorrhage in 68-year-old woman. She sustained a fracture from a fall and had a history of diabetes mellitus, artery disease and BMI bigger than 30. There was the higher prevalence of male compared to female patients. The ratio between the genders male- female was 2.8:1. The study included 37 male patients and 13 female, averaged 39±20,5 years (range, 16 to 76 years). 31 left femurs and 21 right femurs were fractured. 46 fractures were the result of blunt trauma secondary to (in order of frequency) a motor-vehicle accident, a fall, a motorcycle accident, and a pedestrian-motor-vehicle accident. Low energy trauma was the cause of fractures in six patients, of which five in elderly females. 49 fractures were closed. Of the three open fractures, two were graded, according to the system of Gustilo and Anderson, as type I; one as type II. Orthopedic Trauma Association classification system, eight were classified as 32-A; 35 as 32-B; and nine as 32-C. Isolated fracture of the femur was in 24 patients. 21 of the patients had additional orthopedic injuries (average, two additional fractures or dislocations, or both; range, one to five). Of the total number of patients, 11 did not have combined injuries or co-existent disease. The average length of hospital stay was l5,5±7,6 days. In 12 patients the length of hospital stay was shorter than 10 days, and in 20 patients was shorter than 15 days. Eight patients were treated on the same day after suffering the injury and half of the patients were treated in the next four days. Four patients waited for surgery longer than 10 days, of whom two patients had combined craniocerebral injuries. The longest waiting time for surgery was 14 days.
Healing time given in weeks was 19,36 ± 6,1 weeks. The overall healing rate was 93,6%. There were three (6,25%) major complications nonunion. Two late aseptic nonunion with nail breakage was successfully treated with exchange one nailing and one dynamic hip screw. One nail breakage presented 25 months and other nine months later after minor trauma (Figure 1).
Figure 1.
Aseptic nonunion with nail breakage.
One late aseptic nonunion was successfully treated with reamed nailing (Figure 2, 3). The nonunion healed within six months. The proximal locking screws directed diagonally (less prominent) was removed in two patients, while distal in one patient. There were one (2%) delayed union, one (2%) rotational malunion and no infection. The shortening of 1 cm was in two patients, and an extension of 0.7 cm in one patient. One patient had antecurvatum of 10 degrees, one of 7 degrees and valgus of 5 degrees. One patient had pudendal nerve palsy, which recovered in the further course of treatment.
Figure 2.
Nonunion after the first surgical treatment.
Figure 3.
union after the exchange with reamed nailing.
Heterotopic ossification about the hip after intramedullary nailing was found in two patients, of whom one patient ha a cerebral contusion. An IM nail was removed in one patient, after healing due to disorders caused by proximal nail prominence up to 1cm. The size of the thigh was measured: four patients had a smaller size in comparison with a healthy side 0.5 cm, seven of 1cm, three of 1.5 cm, and 2cm. Fisher's exact test was used to establish statistically significant difference in the thigh (knee extensors) muscle between the test and control group. It was found a statistically significant difference (p<0.0001). After the treatment was completed, six patients could not perform their normal activities prior to the injury. Three patients were not capable to perform physically demanding labor they were capable of prior to the injury, including other jobs. Pain related to changes in the weather and discomfort occurred in 16 patients, of which on the place of insertion in seven patients and around the knee area in five patients. The Fisher's exact test was used to establish statistically significant difference of parameters of intermittent pain presence. It was found a statistically significant difference (p<0.0001).
We compared mobility of injured hip with a healthy side excluding the patients with bilateral fractures and those with fractures of the hip and pelvis.
A Chi- square test and Fisher's exact test was used to show statistically significant difference between the parameters of the test group and control group (Table 1). No statistically significant limitation was found in the range of motion: abduction, adduction, external and internal rotation in the test group compared to the control group (p<0.05).
Table 1.
Distribution of patients according to the degree of hip mobility.
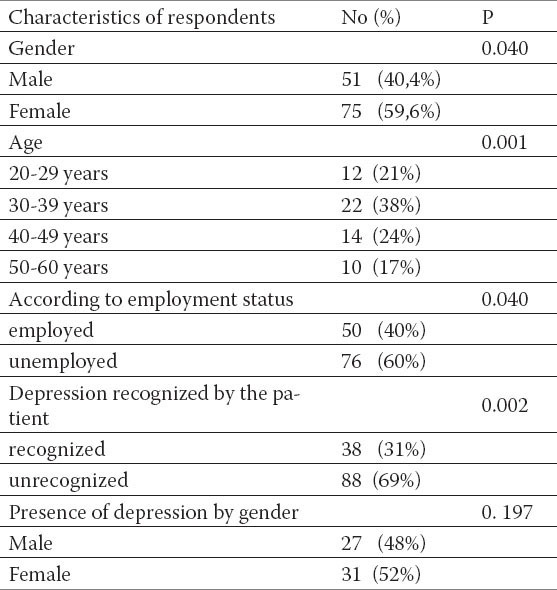
A Chi- square test i Fisher's test was used to show statistically significant difference between the parameters of the test group and control group (Table 2). No statistically significant difference was found in limitation of the range of motions: flexion and extension in the knee joint (chi2=2.32, P=0.024).
Table 2.
Distribution of patients according to the degree of knee joint mobility.
5. DISCUSSION
Suitable instruments, trained assistants, and optimal hospital conditions are necessary for successful insertion of intramedullary nails. The surgeon must be familiar both with open and closed nail surgical techniques, and regardless of experience with the closed nailing method, some fractures must be treated by open nailing method. If surgery is to be postponed for several days, it makes more difficult for the surgeon to restore limb length. The patient must be able to tolerate a major surgical procedure (1). Surgical procedures from this study performed a group of surgeons who did not have adequate training and optimal hospital conditions for this, in the world earlier applied demanding technique, but quite new for us.
A femoral shaft fracture usually occurs as a result of high-energy trauma of motor vehicle accidents, automobile-pedestrian accidents, gunshot injuries, falls from a height and may be associated with multiple system injuries (3). This study has also proved that traffic accidents are the most common cause of femoral shaft fractures occurring more frequently in younger male adults. Low energy traumatic fractures tend to occur more often in the elderly female population. The optimal time for intramedullary nailing of closed and open fractures has been an area of controversy; however, current data support early (within 24 hours) nailing for most femoral fractures. They recommend early static locked nailing, with little or no reaming, of open and closed femoral fractures as soon as possible (1, 6). This study included within 24 hours eight surgically treated patients. Time for surgery has affected the overall results of the treatment.
The primary advantage of nonreamed nailing is better preservation of the blood supply to the cortex, whereas the major advantage of reamed nailing is a more rigid construction, stronger implants, and earlier fracture union (9, 10). The overall healing rate was 93,6%. Healing time given in weeks was 19,36 ± 6,1 weeks. There were: three nonunions (6,25%), two nail breakage (4,2%), one delayed union (2%) one rotational malunion (2%) and no infection. Novotarski at al. were treated with early external fixation followed by planned conversion to intramedullary nail fixation. This two-stage stabilization protocol fifty-six (97 percent) healed within six months. Moed and Watson 1995 reported no infection or hardware failure in 22 femoral fractures treated with unreamed retrograde nailing. There were three nonunions (13.6%) and one rotational malunion (4.5%). Knee range of motion was normal in all patients except in one who had a concomitant knee dislocation. Union of the fracture occurred at an average of fifteen weeks. The operative time for the nailing averaged seventy-five minutes (range, thirty-five to 105 minutes). There were no infections, and no nail or screw failed (8). The operative time for the nailing in our study was 175 minutes.
Treatment goals include allowing early mobilization of the patient, restoration and maintenance of normal length and alignment, the ability to consistently achieve union, and to maintain a normal, functional range of motion in the hip and knee. The sum of hip and knee range of motion and flexion should total at least 160° to allow the patient comfortable stair climbing (11). In this study, there were no patients with the sum of hip and knee range of motion and flexion less than 160°. Weather related pain and discomfort of smaller intensity was found in 16 patients, of which seven at the site of insertion and five at the knee area. The Fisher's exact test was used to establish whether differences of parameters measuring occasional pain presence were statistically significant. It was found statistically significant difference (p<0.05). Knee pain was the most common and most severe source of patient discomfort 12 months after isolated femur fractures, and demonstrated moderate to good correlation with general and joint-specific functional outcome measures (12).
In this study, we found no statistically significant difference in a range of motion of the hip and knee operated side compared to a healthy side (chi2=2.32, P=0.13). It was found statistically significant difference in the thigh (knee extensors) muscle weakness (p<0.0001). In the study Helmy et al. from 2008 it was not found significant difference of a motion in the hip and knee operated side compared to a healthy side. Isokinetic muscular strength testing by the dynamometer showed significant difference between the hip abductors and extensors. Separation of the fibers of m. gluteus medius at the piriformis fossa entry and possible trauma of the tendon piriformis, obturator externus and internus is most likely a cause of consequent muscular weakness. There was no difference between the knee extensors. It was not found statistically significant difference in a motion between operated and healthy leg.
6. CONCLUSION
Our review of the initial 52 cases performed at our institution has shown it to be a successful experience. The overall healing rate was 93,6%. Although closed methods reduced the risk of infection and problems with severely comminuted fractures. Intramedullary nailing results in a short hospital stay, return of motion in all joints and relatively short total disability time. We also think that interlocking intramedullary nailing is the treatment of choice for femoral shaft fractures.
Footnotes
CONFLICT OF INTEREST: NONE DECLARED
REFERENCES
- 1.Whittle AP. Fracture of the lower extremity. In: Canale ST, Beaty JH, editors. Campbell's operative orthopaedics. 11th ed. Philadelphia: Mosby Elsevier publishers; 2008. pp. 3190–3217. [Google Scholar]
- 2.Küntscher G. Die Marknagelung von Knochenbrüchen. Arc Klin Chir. 1940;200:435–455. [Google Scholar]
- 3.Winquist RA, Hansen ST, Jr, Clawson DK. Closed intramedullary nailing of femoral fractures. A report of five hundred and twenty cases. J Bone Joint Surg Am. 1984;66:529–539. [PubMed] [Google Scholar]
- 4.Wolinsky PR, McCarty E, Shyr Y, Johnson K. Reamed intramedullary nailing of the femur: 551 cases. J Trauma. 1999;46:392–399. doi: 10.1097/00005373-199903000-00007. [DOI] [PubMed] [Google Scholar]
- 5.Riska EB, von Bonsdorff H, Hakkinen S, Jaroma H, Kiviluoto O, Paavilainen T. Primary operative fixation of long bone fractures in patients with multiple injuries. J. Trauma. 1977;17:111–121. doi: 10.1097/00005373-197702000-00005. [DOI] [PubMed] [Google Scholar]
- 6.Ricci WM, Gallagher B, Haidukewych GJ. Intramedullary nailing of femoral shaft fractures: Current concepts. J Am Acad Orthop Surg. 2009;17:296–305. doi: 10.5435/00124635-200905000-00004. [DOI] [PubMed] [Google Scholar]
- 7.Nowotarski PJ, Turen CH, Brumback RJ, Scarboro JM. Conversion of external fixation to intramedullary nailing for fractures of the shaft of the femur in multiply injured patients. J Bone Joint Surg. 2000;82-A:781–788. [PubMed] [Google Scholar]
- 8.Moed BR, Watson JT. Retrograde intramedullary nailing, without reaming, of fractures of the femoral shaft in multiply injured patients. J Bone Joint Surg Am. 1995;77(10):1520–1527. doi: 10.2106/00004623-199510000-00006. [DOI] [PubMed] [Google Scholar]
- 9.Chapman MW. The effect of reamed and nonreamed intramedullary nailing on fracture healing. Clin Orthop Relat Res. 1998 Oct;:230–238. doi: 10.1097/00003086-199810001-00023. [DOI] [PubMed] [Google Scholar]
- 10.Brumback RJ, Virkus WW. Intramedullary nailing of the femur: reamed versus nonreamed. J Am Acad Orthop Surg. 2000;8(2):83–90. doi: 10.5435/00124635-200003000-00002. [DOI] [PubMed] [Google Scholar]
- 11.Brumback RJ, Handal JA, Poka A, et al. Radiograph analysis of the Brooker-Wills interlocking nail in the treatment of comminuted femoral fractures. J Orthop Trauma. 1987;1:120–129. doi: 10.1097/00005131-198702010-00002. [DOI] [PubMed] [Google Scholar]
- 12.David WS, Mark ML, Tanya CS, Jeannette L, Andrea D, Christina T. Functional outcome and persistent disability after isolated fracture of the femur. Can J Surg. 2008;51(5):366–370. [PMC free article] [PubMed] [Google Scholar]
- 13.Helmy N, Jando TJ, Lu T, Chan H, O’Brien JP. Muscle Function and Functional Outcome Following Standard Antegrade Reamed Intramedullary Nailing of Isolated Femoral Shaft Fractures. J Orthop Trauma. 2008;22:10–15. doi: 10.1097/BOT.0b013e31815f5357. [DOI] [PubMed] [Google Scholar]


