ABSTRACT
Aim:
The objective of the study was to examine whether cardiotocography can (CTG) predict asphyxia of the embryo, manifested as hypoxic-ischemic encephalopathy (HIE), and to what extent one can rely on CTG record.
Material and methods:
Retrospective research was carried out at the Clinic for Gynecology and Obstetrics UKC Tuzla and medical documentation from the history of mothers and newborns was used. The study group consisted of 68 pregnancies and newborns who developed HIE. The control group consisted of 40 pregnancies, which resulted in birth of healthy newborns – without signs of asphyxia. CTG records were analyzed, Apgar score, the ways of finishing delivery.
Results:
Pathological CTG records (bradycardia 100, tachycardia 180, silent type of curve, late decelerations) were found in 45 (66,17%) cases of the study group in comparison to 11 (27,5%) in the control group. In the study group Apgar score in 5th minute lower than 7 had 17,46% newborns and the highest incidence of the normally finished deliveries. We conclude that cardiotocography is one of the reliable methods of fetal monitoring in pregnancy and delivery, and that pathological CTG record very likely indicates the possible presence of perinatal asphyxia.
Conclusion:
Achieving a low degree of correlation between pathological intrapartum cardiotocography findings and long-term outcome of children can be achieved by rapid and adequate obstetric intervention and the relatively short duration of fetal acidosis, and optimal procedures during intensive care of newborns.
Keywords: cardiotocography, perinatal outcome
1. INTRODUCTION
Great progress in antepartal and partal diagnosis of fetal condition was made by the introduction of cardiotocography–simultaneous registration of fetal heartbeats (KCS) and contractions. Hon was the first to show characteristic decelerations of FHBs during fetal asphyxia, and other authors further elaborated cardiotocographic (CTG) records (1, 2, 3, 4).
In the current situation, almost all women are monitored cardiotocographically, which probably significantly increases the number of Caesarean sections for “fetal indications” (5).
FIGO guidelines for reading CTG records introduce in obstetrics unique terminology and interpretation ante and intrapartal cardiogram. These guidelines are descriptive in character, and allow assessment of CTG as normal, suspected and pathological (6).
Fetal asphyxia is a condition of disturbed gas exchange, leading to progressive hypoxemia and hypercapnia with significant metabolic acidosis (7). Asphyxic baby can die, recover, manifest hypoxic-ischemic encephalopathy (HIE), and later have neurodevelopmental disorders (5).
Advantage of cardiotocography as generally accepted, and certainly the most widely used non-invasive method of monitoring fetal comes out from the fact that for its implementation there are no contraindications and the CTG findings can be written that is documented. There is significant correlation between pathological CTG and the state of the newborn evaluated by Apgar score (8), the existence of acidosis (9), hypoxic-ischemic encephalopathy (10) and subsequent neuromotor development (11).
However, not rarely records are false positive or false negative results. False positive means that the record is pathological, and fresh undepressed child is born, without acidosis; false negative record means that with the normal CTG record asphyxic / depressed child with HIE is born and that will manifest later in neurodevelopmental disorders. The objective of the study was to examine can CTG predict fetal asphyxia, present as HIE, and to what extent one can rely on CTG records, that is when to intervene with operation.
2. PATIENTS AND METHODS
Retrospective research was carried out at the Gynaecological-obstetrics clinic UKC Tuzla. The study group consisted of 68 pregnancies, which resulted in deliveries of newborns, who were postnatally diagnosed with hypoxic ischaemic encephalopathy HIE (mild, moderate and severe). The control group consisted of 40 pregnancies with the birth of healthy babies–no signs of asphyxia.
Analyzed parameters were taken from the history of diseases of pregnant women and newborns. In the center of our professional interest was intrapartum fetal monitoring, which we implemented using cardiotocography. In this study we used CTG devices Philips Series 50 IP–2. While clinically interpreting cardiotocographic findings as usually we used the following elements (FIGO guidelines): fundamental frequency of heart (normal 120–160/min, mild tachycardia 160–180/min, severe tachycardia 180/min, bradycardia 120–100/min, severe bradycardia 100/min), type of variability (amplitudes) fundamental frequency (undulation 10–25/min, saltatory 25/min, narrowed undulation 5–10/min, silent 5/min), decelerations (early–the SEC and, late–SEC II and variable decelerations) and rapid frequency oscillations in one minute (normal findings 2–5; abnormal 2). We considered pathological findings the occurrence of late decelerations in 30% contraction, silent type CTG curve for 30 minutes, the occurrence of variable decelerations 80/min for at least 60 seconds, bradycardia 100/min for at least three minutes and tachycardia at 180/min for at least 30 minutes, as well as combinations of these records.
Postnatal assessment of the state of the newborn was done by neonatologist and HIE was diagnosed on the basis of the Apgar score in the first and fifth minute after birth, clinical features, neurological status, and ultrasound examination of the brain.
Statistical processing of data
Statistical processing of data was done by applicative software Statistical Package for Social Sciences for Windows, version 18.0 PASW-SPSS Inc., Chicago, IL, USA). Category variables will be shown as frequencies and percentages. Normality of distribution and homogenity of variance is checked by adequate tests. Testing of differences in the distribution of crossed qualitative variables (independent distribution) will be shown by chi square test. The results are then clearly presented in tables and charts. For statistical significance values ‘’ p’’ usual level of significance p <0.05’’ was chosen.
3. RESULTS
Data on cardiotocographic monitoring (often used intermittent CTG registration) are shown in the diagram No.1. In the study group from a total of 68 pregnancies abnormal CTG record was found in 45 (66.17%) cases and normal in 23 (33, 82%). In control group abnormal CTG record was present in 11 (27.5%) and normal in 29 (72.5%) cases. Statistical analysis found a significant difference (χ ² = 3.841, p <0.05).
Diagram 1.
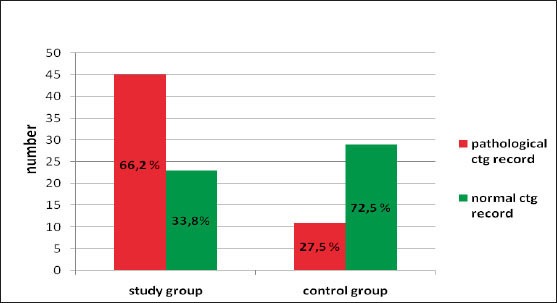
The frequency of certain variables pathological CTG records, the mode of finishing delivery and Apgar score in the 5th minute after birth.
Table 1.
Cardiotocographic findings in our sample examination
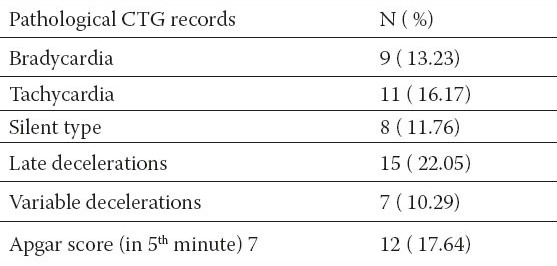
Diagram 2.
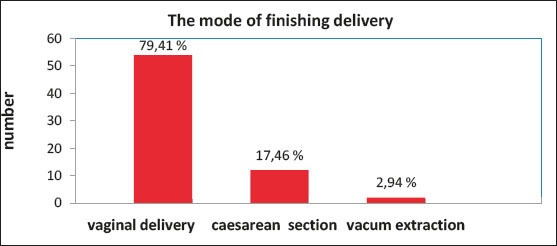
The mode of finishing delivery
In the study there were 11(27,5%) false positive and 23 (33,82%) false negative records.
Table 2.
Pathological CTG records as diagnostic test of intrauterine asphyxia
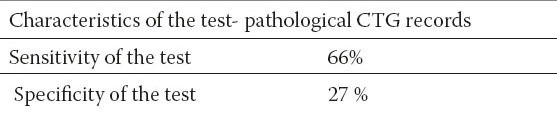
In Table 2. Sensitivity and specificity of the pathological CTG records as diagnostic test of intrauterine asphyxia is shown.
Sensitivity test: ability of method to show positive finding when the required lesion is present. Specificity test: ability of the procedure to show negative finding in cases when there is no required lesion. High sensitivity of the test means that the patients with pathological CTG records will very likely deliver asphyxic child.
Positive predictive value of cardiotocography was 80 %.
4. DISCUSSION
From the literature data it has been proven without doubt that there is a correlation of pathological CTG and conditions of the newborn evaluated by Apgar score and hypoxic–ischaemic encephalopathy (5). In our research of 68 newborns pathological CTG record was found in 45 (66,17 %) cases. Painter and associates found early neurological disorder (HIE) in 2 to 12 children with normal CTG record, 10 to 16 with suspicious record and 16 to 22 with pathological CTG record (12). Nelson and associates in 78 children with HIE retrospectively in 21 child (27%) found narrowed variability of the curve and/or late decelerations; in the control group those records were in 9,3 % women (11). Spencer and associates analyzed retrospectively CTG record of mothers of 38 children with late cerebral paralysis and compared it with 36 of the control group. Late decelerations were in 5,3% women in labor, variability in 10,5%, and in the control group 5,7% women in labor (13). Škrablin and associates compared CTG record of 69 women in labor whose child manifested HIE; they found prepathological CTG record in 32 and pathological record in 17 women in labor, total 49 or 71,0% (10).
Of the elements that make cardiotocographic record abnormal in 68 pregnancies, we found the most common late decelerations–DIP II in 15 (22.05%) cases, followed by tachycardia in 11 (16.17%), bradycardia in 9 (13.23%), silent type CTG curve in 8 (11.76%), variable decelerations in 7 (10.29%) cases.
Our results are in agreement with the results of Petrovic and associates who in their work by examining the presence of asphyxia (with CTG and pH monitoring) in 880 births, found that late decelerations are most often associated with fetal acidosis, as well as bradycardia and tachycardia (14). The same authors state that in the cases of variable decelerations normal pH of fetal blood (14) was found. Experience, moreover, confirms that 20-30% CTG records cannot be reliably interpreted, and there is a possibility of confusion in the interpretation of CTG records, when in cases of fetal death, maternal heart rate can be misinterpreted as fetal.
The occurrence of HIE is of particular importance, because among those children, children with neurodevelopmental disorders are recruited (12). Correlation of pathological CTG records and HIE are found in the studies of other authors. So Palsdottir of 127 investigated cases finds abnormal CTG record in 79% of cases of HIE in newborns (15). In cases of the narrow variability it was 38.9% (13) up to 64% of children with neonatal HIE, and 14% with neurodevelopmental disorders (8). Late decelerations in 32% (8) and 47.2% (13) prior to neonatal HIE, and in 23% (12) and 26% (11) neurodevelopmental disorders.
FIGO recommendations form the basis for guidelines for the application of electronic fetal monitoring, which in 2001 announced the pouring “Royal College of Obstetricians and Gynecology–RCOG,” and these recommendations are fully accepted by the German Society of Gynaecologists and Obstetricians “Deutsche Gesellschaft fur Gynakologie und Geburtshilfe–DGGG”. Recent data speak in favor of significant reduction in perinatal mortality and significantly better recognition of acidosis during labor monitored by CTG (16).
Neonatal encephalopathy and later cerebral paralysis is 3,9 times more frequent at intrapartal late decelerations, and 2,7 times more frequent at intrapartal finding of decreased variability (11). Pathological CTG form – evaluated according to FIGO guidelines, is also statistically more frequent at neonatal encephalopathy (13). Additionally, auscultatory monitoring of labor is not only more demanding for the staff but also the documentation is worse, and certainly it is not safe for early discovery of loss of oscillations, lack of acceleration, shallow decelerations and tachycardia (17)
Clinical evaluation of the vitality of the newborn at birth based on the Apgar score in the first and fifth minute of life today is not considered as important as before. However, the connection was found between low Apgar score and pathological CTG as a predictor of perinatal asphyxia, and also with later long-term prognosis (18). Weakest correlation of CTG changes is with Apgar score, Apgar score less than 7 was found in only 12 (17.64%) newborns (who developed HIE). Linkage of low Apgar score in the fifth minute, pathological CTG and the existence of HIE is also stated by other authors (18, 19, 20).
Late deceleration and loss of variability are highly predictive patterns of CTG record, and to a lesser extent variable deceleration. When mother is found reduced variability (5/min) with late decelerations or prolonged decelerations, in up to 80% of cases there is fetal asphyxia (5). Unfortunately, records are false positive or false negative quite often.
Pathological record, and delivered undepressed child (false positive) we had in 11(27,5%) cases; while normal CTG record and delivered asphyxic / depressed child (false negative) we had in 23(33,82%) cases and among them statistically significant differences were found. Pathological CTG record, that is false negative record, that is sick children with normal CTG records in literature there is 7% to 84% (11, 21). Škrablin and associates in their study found 17,5% false positive and 29% false negative CTG records in 69 newborns with HIE and 80 without HIE (10). Spencer and associates in 36 newborns with HIE found that CTG record before birth was pathological in 86% women in labor, but in 52,8% children with HIE CTG records was false negative, it was not pathological (13). According to research of Painter and associates there were 31,6% false positive records when HIE did not develop, and 16,7% cases of false negative (12).
In case of pathological CTG record and HIE newborns we had operation to finish delivery in 14 cases (12-17,64% Caesarean Sections 2 – 2,94% vacuum extractions). Petrović in 880 cases of diagnosed fetal asphyxia by CTG record and pH monitoring finds linear correlation between the ways to finish delivery and pH finding of fetal scalp (14). It is questionable whether the highest percentage of normal vaginally finished deliveries can be considered a good result, or should we intervene faster at timely detected asphyxia (with cardiotocography and complementary method such as pH monitoring) by operating, all with an aim to have a smaller percentage of births of children with HIE.
Cardiotocograpfy is an important method of the monitoring of fetus in pregnancy and during labor. According to our research pathological CTG record with sensitivity of 66% indicates ability to predetermine perinatal asphyxia.
Bradycardia below 100/min., tachycardia 180/min., silent type curve, and late decelerations are very predictive forms of CTG records. When such parameters of pathological CTG records are found, in up to 80% cases there is fetal asphyxia.
5. CONCLUSION
Cardiotocography is one of the reliable methods of monitoring of fetus in pregnancy and during childbirth. Pathological CTG record with high probability indicates possibility of existence of perinatal asphyxia. Unfortunately, cardiotocography has also large number of false positive findings. Therefore, records from pregnancy, suspicion of fetal hypoxia / asphyxia should be confirmed by ultrasound Doppler examination; in birth suspicious (positive ones) records should be checked by pH monitoring.
Achieving low level of correlation between pathological intrapartal cardyotocographic findings and long-term outcome of children can be achieved by quick and adequate obstetric intervention and relatively short duration of fetal acidosis, and optimal procedures during intensive treatment of newborns.
Footnotes
CONFLICT OF INTEREST: NONE DECLARED
REFERENCES
- 1.Hammacher K. Neue Methoda zur selektiven Refistrierung der fetalen Herzschlagenfrequenz. Geburtshilfe Frauenhk. 1962;22:1542–1543. [Google Scholar]
- 2.Hammacher K. The clinical significance of cardiotokography. In: Huntingford PJ, Huter K, Saling E, editors. Perinatal Medicine. I European Congress. Stuttgart: G.Thieme; 1969. pp. 80–92. [Google Scholar]
- 3.Saling E. Stuttgart: G. Thieme; 1966. Das Kind im Bereich der Geburtshilfe. [Google Scholar]
- 4.Fischer W. Lehrbuh und Atlas. Stuttgart: G. Thieme; 1973. Kardiotokographie. [Google Scholar]
- 5.Dražančić A. Kardiotokografija - njeni dosezi i pretkazljivost. Gynaecol Perinatol. 2006;15(2):71–87. [Google Scholar]
- 6.Harni V, Gudelj M, Šemnički N. Kardiotokografija: od otkrića kucaja čedinjeg srca do FIGO smjernica. Gynaecol Perinatol. 2006;15(1):19–29. [Google Scholar]
- 7.Low JA. Intrapartum fetal asphyxia: Definition, diagnosis and classification. Am J Obstet Gynecol. 1999;176(5):957–959. doi: 10.1016/s0002-9378(97)70385-5. [DOI] [PubMed] [Google Scholar]
- 8.Wilken HP, Hackel B, Wilken H. Klinishe Erfahrungen mit dem antepartalen CTg - Auswertererfahren nach fisher, Hammacher, Hodr und Kubli. Zentralbl Gynekol. 1980;102:909–914. [PubMed] [Google Scholar]
- 9.Ivanišević M. Kardiotokografija i pH-metrija kod fetalne asfiksije i acidoze. XVII Perinatalni dani. Gynaecol Perinatol. 1999;(Suppl.1):61–64. [Google Scholar]
- 10.Škrablin S, Dražančić A, Letica-Protega N, Tadić V. Trudnoća i porod u novorođenčadi s encefalopatijom u ranom neonatal-nom razdoblju. LiječVjesn. 1992;114:10–15. [PubMed] [Google Scholar]
- 11.Nelson KB, Dambrosia JM, Tiny TY, Grehter JK. Uncertain value of electrinc fetal monitoring in predicting cerebral palsy. N Engl J Med. 1996;334:613–618. doi: 10.1056/NEJM199603073341001. [DOI] [PubMed] [Google Scholar]
- 12.Painter MJ, Scott M, Hirsch MPO, Donoghue P, Depp R. Fetal heart rate patterns during labor: neurologic and cognitive developement at six to nine years of age. Am J Obstet Gynecol. 1988;159:854–858. doi: 10.1016/s0002-9378(88)80153-4. [DOI] [PubMed] [Google Scholar]
- 13.Spencer JA, Badawi N, Burton P, et al. The intrapartum CTG prior to neonatal encephalopathy at term: A case control study. Br J Obstet Gynecol. 1997;104:25–27. doi: 10.1111/j.1471-0528.1997.tb10643.x. [DOI] [PubMed] [Google Scholar]
- 14.Petrović O, Sindik N, Marić M, Mahulja–Stamenković V. Kardiotokografija i pH metrija u prognozi perinatalnog ishoda. Gynaecol Perinatol. 2010;19(2):73–78. [Google Scholar]
- 15.Palsdottir K, Dabjartsson A, Thorkelsson T, Hardardottir H. Birth asphyxia and hypoxic ischaemic encephalopathy, incidence and obstetric risk factors. Laeknabladid. 2007;93(9):595–601. [PubMed] [Google Scholar]
- 16.Vintzileous AM, Nochimson DJ, Antsaklis A, et al. Comparasion of intrapartum electronic fetal heart rate monitoring versus intermittent auscultation in detecting fetal acidemia at birth. Am j Obstet Gynecol. 1995;173:1021–1024. doi: 10.1016/0002-9378(95)91320-3. [DOI] [PubMed] [Google Scholar]
- 17.Goeschen K. Derzeitiger Stand der intraparatlen Uberwachung des Kondes. Gynaecologe. 1997;30:525–533. [Google Scholar]
- 18.Futrakul S, Praisuwanna P, Thaitumyanon P. Risk factors for hypoxic – ischaemic encepalopathy in asphyxiated newborn infants. J Med Assoc Thai. 2006;89(3):322–328. [PubMed] [Google Scholar]
- 19.Blix E. The admission CTG: is there any evidence for still using the test? Acta Obstet Gynecol Scand. 2013;30:1111–1121. doi: 10.1111/aogs.12091. [DOI] [PubMed] [Google Scholar]
- 20.Salustiano EM, Campos JA, Ibidi SM, Ruano R, Zugaib M. Low Aogar scor at 5 minutes in a low risk population: maternal and obsterical factors and postnatal outcome. Rev Assoc Med Bras. 2012;58(5):587–593. [PubMed] [Google Scholar]
- 21.Sameshima H, Ikemone T, Ikeda T, Kamitomo M, Ibara S. Unselected low risk pregnancies and the effect of continous intrapartum fetal heart rate monitoring on umbilical blood gases and crebral palsy. Am J Obstet Gynecol. 2004;190:118–123. doi: 10.1016/j.ajog.2003.07.014. [DOI] [PubMed] [Google Scholar]


