ABSTRACT
Purpose:
To evaluate safety and efficacy of day care cataract surgery in developing country.
Patients and Methods:
This prospective study included 200 patients planned for cataract surgery during October and November 2012 divided in to two groups, day care cataract surgery (DCCS) and inpatient cataract surgery (ICS), with same number of male and female patients right and left eyes. All patients had same operative conditions and postoperative follow up.
Results:
The average age of patients in this study was 68.4 ± 7.47 years. Visual acuity before cataract extraction was 0.1754 where 44.5% of patients had severe visual impairment and another 23% had complicated cataract. Posterior capsule rupture was noted in 4.5% of cases. The main risk factors in both groups were: higher age, female gender, left side, complicated cataract, higher dioptric power of IOL and ECCE. Regular control opthalmologic examinations 30, 90 and 180 days after the cataract extraction did not reveal signs bullous keratopathy, wound dehiscence, cystoid macular edema and endophtalmitis in any of patients. Postoperative visual acuity 180 days after the operation in DCCS was 0.920 ± 0.154 and 0.928 ± 0.144 in ICS. Visual acuity less than 0.5 was noted in 4.5% due to posterior eye segment changes. Patients in DCCS group had 30 control examinations more and 95 days of hospitalization less than ICS with 16.5% cost reduction.
Conclusion:
The concept of day care cataract surgery is equally safe and more cost effective than inpatient cataract surgery.
Keywords: day care surgery, Bosnia and Herzegovina
1. INTRODUCTION
Cataract presents the leading cause of blindness, taking 51% of estimated 39 million blind people throughout the world (1). Global population growth and increasing longevity will double the number of people with visual loss and blindness from cataract by the year 2020 (2). These figures suggest that it is necessary to increase the number of cataract operations, which should be easily accessible, with good quality and reasonable costs.
In order to overcome the problem of increasing demands for a larger number of cataract surgeries, concept of day care cataract surgery has been introduced (3). Several studies accessed outpatient day care cataract surgery, finding it equally safe and more cost effective than inpatient surgery (4, 5, 6). Rate of day care cataract surgery is as high as 100% in Denmark and as low as 0% in Austria (7). There is no data regarding day care cataract surgery from B&H. The purpose of this study is to evaluate safety and efficacy of day care cataract surgery in region with limited resources.
PATIENTS AND METHODS
This prospective study included 200 eyes from 200 patients scheduled for cataract surgery during October and November 2012. Patients were divided into two groups of 100 patients. Working group included patients in Public Health Care Institution Doboj–Jug operated as day care cataract surgery (DCCS). Control group included patients in Eye Clinic University Clinical Centre Tuzla, Bosnia and Herzegovina, operated as outpatient and inpatient cataract surgery (ICS).
Patients were operated by three experienced cataract surgeons with more than 2000 cataracts surgeries each. Patients were operated with phacoemulsification (PE) and large incision extracapsular cataract extraction with sutures (ECCE), depending on surgeons judgment. Operations were performed in local peribulbar anesthesia using 2% lidocaine (8), with antiseptic preparation based on povidone–iodine use, 10% on periocular area skin during dilation and 5% into conjunctival sac on the operating table and vancomycin (1.0 mg/0.1 mL) intracameral injection at the end of the procedure (9).
Patients in both groups underwent complete control opthalmologic examinations 1, 7, 30, 90 and 180 days after cataract surgery. Patients with pronounced corneal edema and inflammation had more often controls, with intensive therapy and usage of acetazolamide orally. Patients operated with ECCE had additional control examination two months after cataract extraction for sutures removal. Data were analyzed using the SPSS statistical package, version 20.0. The level of significance was established at α = 0.05.
3. RESULTS
Patients in this study were equally divided into two groups of 100 patients, with 50 male and female patients, with 25 right and left eyes equally distributed between the groups and genders (χ2 = 0.000, df = 1, p < 0.05). Average age of patients in DCCS group was 69.12 years (range (SD = ± 7.47, range 46–84) and 67.67 years (SD = ± 7.63, range 48–83) in ICS group (t = 1.424, df = 99, p = 0.158, p >0.05). There were no statistically significant differences in age of patients in relation to sex and side of the cataract surgery.
Visual acuity before the cataract extraction in DCCS group was 0.1492 (SD = ± 0.103, range light perception–0.4) and 0.2016 (SD = ± 0.129, range light perception–0.5) in ICS group with statistically significant difference between the groups (t = -2.917, df = 99, p = 0.004, p < 0.05). Intraocular pressure (IOP) before cataract extraction in DCCS group was 15.628 mm Hg (SD = ± 1.293, range 13.1–18.5) and 15.696 mm Hg in ICS group (SD = ± 1.273, range 14.3 – 18.5) (t = -0.353, df = 99, p = 0.725, p < 0.05). Forty eight percent of patients in DCCS group had dense cataracts (mature and corticonuclear cataract) that prevented posterior segment visualization, while 41% of patients in ICS group had poor posterior segment visualization due to cataract. Table 1. presents cataracts morphological analysis in both groups.
Table 1.
Cataract morphological analysis in both groups
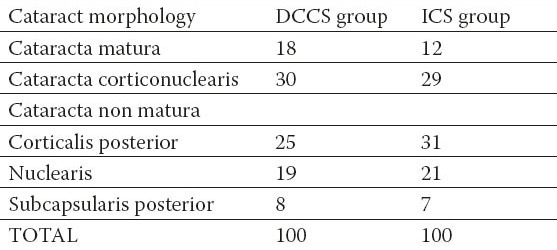
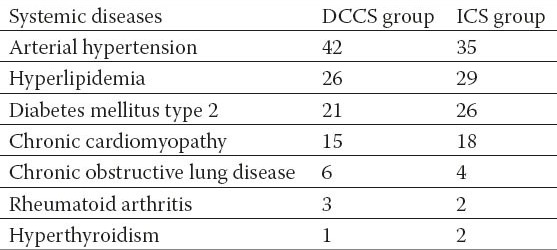
Twenty six percent of patients in DCCS group had complicated cataract, associated with other ocular diseases and 20% in ICS group (χ2 = 0.468, df = 1, p >0.05). Table 2. presents etiology of complicated cataracts included in this study. Most common systemic diseases associated with cataract in this study are presented in Table 3.
Table 2.
Etiology of complicated cataract
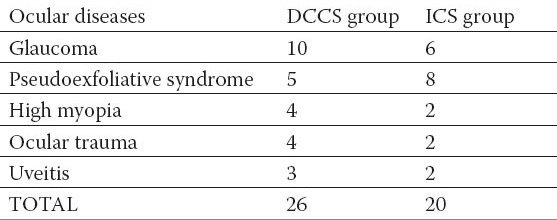
Table 3.
Common systemic diseases
In DCCS group 8% of patients were operated with ECCE and 10% in ICS group (χ2 = 0.244, df = 1, p = 0.621, p >0.05). Average dioptric power of implanted IOL in DCCS group was 22.37 D (SD = ± 2.15 D, range 12.0–27.0) and 21.89 D (SD = ± 2.58, range 12.0–28.0) in ICS group (t = 1.434, df = 99, p = 0.155, p >0.05). Intraoperative complications namely posterior capsule rupture (PCR) was noted in 5% of cases in DCCS and in 4% in ICS (χ2 = 0.116, df = 1, p = 0.733, p >0.05). Average age of patients with noted PCR in DCCS group was 75.6 years and 77.5 years in ICS group compared to 68.78 and 67.26 years in patients without complications (t = 2.711, df = 98, p = 0.008, p < 0.05). Four out of five patients (80%) in DCCS group with PCR were female gender and 2 out of four (50%) in ICS group. Four out of five (80%) patients in DCCS group had PCR while operating left eye and three out of four (75%) in ICS group. Three out of five (60%) patients in DCCS group and three out of four (75%) patients in ICS group had PCR in complicated cataract. Average dioptric power of implanted IOL in patients with PCR was 24.4 D in DCCS and 24.0 D in ICS compared to 22.3 D and 21.8 D in patients who did not have PCR (t = 2.201, df = 98, p = 0.030, p < 0.05). One out of eight (12.5%) patients in DCCS and one out of ten (10%) patients in ICS operated with ECCE had PCR. Corneal sutures after PE were used in 31 patient in DCCS group and 30 patients in ICS group (χ2 = 0.023, df = 1, p = 0.878, p >0.05). None of the patients in both groups had any of anesthesia related complications or surgical complications including iris prolapse, dropped nucleus or ocular hemorrhage.
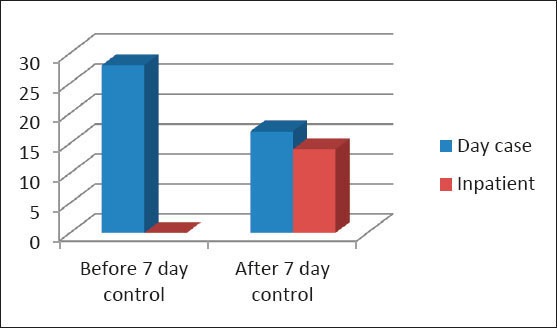
All patients in DCCS group were discharged day after cataract extraction, where 14 patients had pronounced corneal edema and had 2 additional control examinations 3 and 5 days postoperatively. Patients in ICS group were admitted in the hospital for preoperative preparation and some of them were operated the same day (25%) and other were operated day after. Patients with pronounced edema remained in hospital for more than 2 days and total length of hospitalization of all patients in control group was 195 days. Diagram 1. shows duration of hospitalization in ICS group of patients. Postoperative control ophthalmological examination 7 days after cataract surgery revealed that 25% of patients in DCCS and 18% of patients in ICS group did have persistent corneal edema (χ2 = 0.007, df = 1, p = 0.649, p >0.05). Corneal sutures were removed on control examination 7 days after cataract extraction in 14 patients in DCCS and 16 patients in ICS group, while remaining 17 sutures in DCCS and 14 sutures in ICS group were removed on additional control examination 14 days postoperatively (χ2 = 0.348, df = 1, p = 0.696, p >0.05). Diagram 2. presents number of additional control examinations in both groups. Regular control opthalmologic examinations 30, 90 and 180 days after the cataract extraction did not reveal signs of any serious postoperative complications in both groups such as bullous keratopathy, wound dehiscence or leakage, ocular hemorrhage, IOP rise, IOL decentration, cystoid macular edema and endophtalmitis. None of the patients required Nd YAg laser treatment due to posterior capsule opacification. Postoperative visual acuity 180 days the operation was 0.920 ± 0.154 in DCCS and 0.928 ± 0.144 in ICS (t = -0.364, df = 99, p = 0.716, p >0.05). Five patients in DCCS and four in ICS had visual acuity less than 0.5 due to posterior eye segment changes, which could not be detected preoperative due to dense cataracts. Diagram 3. shows preoperative and postoperative values of visual acuity in both groups.
Diagram 1.
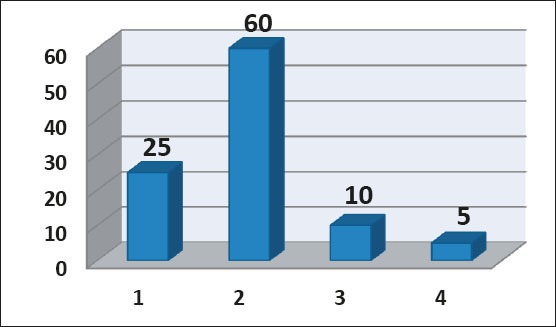
Duration of hospitalization in inpatient cataract surgery (ICS) group
Diagram 2.
Number of additional control examinations
Diagram 3.
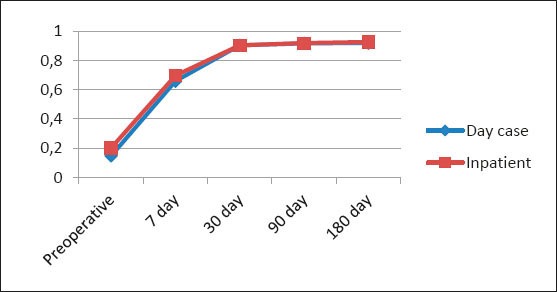
Visual acuity changes
Postoperative IOP 180 days after cataract surgery in DCCS was 15.546 mm Hg (SD ± 1.272) and in ICS 15.404 mm Hg (SD ± 1.110) (t = 0.843, df = 99, p = 0.401, p >0.05). Diagram 4. shows preoperative and postoperative values of IOP in both groups. Patients in DCCS group had 30 control examinations more and 95 days of hospitalization less than ICS patients. Average costs of the operative treatment and all postoperative control examination in DCCS group were 1150.4 KM and 1377.75 KM in ICS group. This means that patients operated as day care cataract surgery have at least 16.5% cost reduction compared to inpatient cataract surgery patients.
Diagram 4.
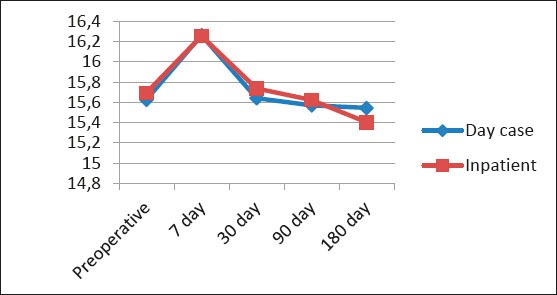
Intraocular pressure changes
4. DISCUSSION
Patients in both groups were operated in similar operative conditions, with same instruments, IOLs, same preoperative and postoperative regimen. All patients were divided into two groups, with same number of male and female patients, same number of right and left eyes and same average age. Average age of patients included in this study is 68.4 years and is higher than world average of 65 years and Eastern Mediterranean Region 60 years but lower than European average of 72 years. Average visual acuity (VA) before cataract surgery in this study was 0.1754 (DCCS 0.14892 and ICS 0.2016). Forty four point five percent of patients have severe visual impairment (VA lower than 0.1) consequent to advanced cataract and poor posterior segment visualization with an uncertain prognosis of postoperative visual outcome. In countries with low Human Development Index patients with severe visual impairment consist over 47% of all cataract patients while in developed countries it is only 1% (10, 11, 12). Therefore it can be concluded, that patients in B&H come to seek treatment of cataract when they feel significant visual loss, like in other developing countries (13).
Twenty three percent of patients in this study have complicated cataract, where glaucoma, pseudoexfoliative syndrome and high myopia are identified as leading ocular comorbidities. More than 70% of patients have one or more systemic disorders, where arterial hypertension, hyperlipidemia and diabetes mellitus are most common. In this study, 9% of all patients, namely older patients with signs of possible corneal dystrophy were operated using ECCE, similar to results of other authors (14, 15, 16). Four point five percent of patients included in this study (5% in DCCS and 4% in ICS) have reported PCR which is higher than previously reported 1.01 to 1.92 (14, 15). Higher rate of PCR in this study can be a result of difficult case mix included in this study, especially in DCCS, where many patients had one or more risk factors for PCR development, with reported higher PCR prevalence up to 32% (16). In this study higher age, higher IOL power associated with shallow anterior chamber, left side, female gender, ECCE are identified as risk factors for PCR development similar to previously published data (15). It important to note that 30.5% of patients had corneal suture as prevention of wound leakage and none of the patients had any other serious complications.
Control examination day after cataract extraction revealed corneal edema in 86.5% of patients (86% in DCCS and 85% in ICS) and 14% of patients in DCCS had 2 additional control examinations due to corneal edema. Dinakaran et al. found that 30% of patients can have corneal edema day after surgery that can need therapy modification and another 10% can have raised IOP that needs to be addressed (17). On the other side, it should be noted that in cases of uneventful phacoemulsification, telephone review can be safe, effective and acceptable first-day review method (19) and also postponed till two weeks postoperatively (20). Control examination 7 days after cataract surgery revealed that 25% of patients in DCCS and 18% of patients in ICS group still had corneal edema that needed topical treatment extension similar to results of previous research (20). Seventeen patients in DCCS and 14 in ICS group were removed on additional control examination 14 days postoperatively. Control examinations 30, 90 and 180 days after the cataract extraction did not reveal signs of postoperative complications such as bullous keratopathy, wound dehiscence, ocular hemorrhage, IOP rise, IOL decentration, cystoid macular edema, posterior capsule opacification and endophtalmitis similar to result of previous research (5). Postoperative VA 180 days after the operation was 0.924 (0.920 in DCCS and 0.928 in ICS). A total of nine patients (4.5%) (5 in DCCS and 4 in ICS) had VA worse than 0.5 due to posterior eye segment changes, but not related to PCR. Posterior segment causes of reduced postoperative VA included diabetic retinopathy, age related macular degeneration and optic nerve atrophy. In this study 89 patients had poor posterior segment visualization where 9 (9.9%) had poor postoperative VA similar to Jammal et al. (18) who found that 12.9% patients with dense cataracts and reduced posterior segment visualization have poor postoperative VA.
Costs of cataract surgery vary significantly from country to country, from 245 $ in developed to 1600 $ in developing countries (21, 22, 23). Average costs of cataract surgery in this study range from 810 $ in DCCS to 970 $ in ICS and these results put Bosnia and Herzegovina in group of middle developed countries (22). Day care surgery provides similar outcome measures, it is more economical and patient friendly option (4, 5, 21). Patients included in this study operated either as day care cataract surgery or inpatient cataract surgery had almost the same postoperative outcome measures, namely early and late postoperative surgical complications and VA. However, difference between groups is that patients in DCCS had 30 control examinations more and 95 days of hospitalization less than ICS patients. These adjustments resulted in 16.5% cost reduction in DCCS compared to ICS, similar to some other researches (5).
The rate of day care surgery differ significantly between European countries where Denmark has the highest (100%) and Austria the lowest (0%) rate of day care surgery (7). The rate is influenced by the acute-care beds density, but also by the density of practicing physicians and by the public expenditure on health (7). In this study in ICS group only 25% of patients were operated as day care cataract surgery. The important fact is that although it is easily accessible, all patients do not opt for day care surgery due to socio-economic reasons and feel more comfortable with the inpatient care (7, 22, 24). Also, surgeons should think of inpatients surgery in patients with complicated cataract and systemic illness (24, 24).
In the conclusion day care surgery is equally safe and more cost effective than inpatient cataract surgery. Certain patients will require inpatient care and both systems should coexist and be available at the same time.
Footnotes
CONFLICT OF INTEREST: NONE DECLARED
REFERENCES
- 1.Pascolini D, Mariotti SP. Global estimates of visual impairment 2010. Br J Ophthalmol. 2012;96(5):614–618. doi: 10.1136/bjophthalmol-2011-300539. [DOI] [PubMed] [Google Scholar]
- 2.Foster A, Gilbert C, Johnson G. Changing patterns in global blindness 1988 – 2008. Community Eye Health. 2008;21:37–39. [PMC free article] [PubMed] [Google Scholar]
- 3.Ingram RM, Banerjee D, Traynar MJ, Thompson RK. Day-case cataract surgery. Trans Ophthalmol Soc U K. 1980;100(Pt 1):205–209. [PubMed] [Google Scholar]
- 4.Fedorowicz Z, Lawrence D, Gutierrez P, van Zuuren EJ. Day care versus in-patient surgery for age-related cataract. Cochrane Database of Systematic Reviews. 2011;(Issue 7) doi: 10.1002/14651858.CD004242.pub4. Art. No.: CD004242. [DOI] [PubMed] [Google Scholar]
- 5.Castells X, Alonso J, Castilla M, Ribo C, Cots F, Anto J. Outcomes and costs of outpatient and inpatient cataract surgery: a randomised clinical trial. Journal of Clinical Epidemiology. 2001;54(1):23–29. doi: 10.1016/s0895-4356(00)00271-7. [DOI] [PubMed] [Google Scholar]
- 6.Galin MA, Boniuk V, Obstbaum SA, Barasch KR, Baras I. Hospitalization and cataract surgery. Annals of Ophthalmology. 1981;13(3):365–367. [PubMed] [Google Scholar]
- 7.Mojon-Azzi SM, Mojon DS. The rate of outpatient cataract surgery in ten European countries: an analysis using data from the SHARE survey. Graefes Arch Clin Exp Ophthalmol. 2007;245(7):1041–104. doi: 10.1007/s00417-007-0550-4. [DOI] [PubMed] [Google Scholar]
- 8.Malik A, Fletcher EC, Chong V, Dasan J. Local anesthesia for cataract surgery. J Cataract Refract Surg. 2010;36(1):133–152. doi: 10.1016/j.jcrs.2009.10.025. [DOI] [PubMed] [Google Scholar]
- 9.Behndig A, Cochener B, Güell JL, Kodjikian L, Mencucci R, Nuijts RM, Pleyer U, Rosen P, Szaflik JP, Tassignon MJ. Endophthalmitis prophylaxis in cataract surgery: overview of current practice patterns in 9 European countries. J Cataract Refract Surg. 2013;39(9):1421–1431. doi: 10.1016/j.jcrs.2013.06.014. [DOI] [PubMed] [Google Scholar]
- 10.Cakir H, Utine CA. Lift and crack technique for risky cataract cases. J Cataract Refract Surg. 2010;36(4):539–541. doi: 10.1016/j.jcrs.2009.11.011. [DOI] [PubMed] [Google Scholar]
- 11.Falabella P, Yogi MS, Teixeira A, Jopetibe F, Sartori J, Schor P. Retrochop technique for rock-hard cataracts. J Cataract Refract Surg. 2013;39(6):826–829. doi: 10.1016/j.jcrs.2013.03.015. [DOI] [PubMed] [Google Scholar]
- 12.Shah SP, Gilbert CE, Razavi H, Turner EL, Lindfield RJ International Eye Research Network. Preoperative visual acuity among cataract surgery patients and countries’ state of development: a global study. Bull World Health Organ. 2011;89(10):749–756. doi: 10.2471/BLT.10.080366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Khanna R, Pujari S, Sangwan V. Cataract surgery in developing countries. Curr Opin Ophthalmol. 2011;22(1):10–14. doi: 10.1097/ICU.0b013e3283414f50. [DOI] [PubMed] [Google Scholar]
- 14.Haripriya A, Chang DF, Reena M, Shekhar M. Complication rates of phacoemulsification and manual small-incision cataract surgery at Aravind Eye Hospital. J Cataract Refract Surg. 2012;38(8):1360–1369. doi: 10.1016/j.jcrs.2012.04.025. [DOI] [PubMed] [Google Scholar]
- 15.Narendran N, Jaycock P, Johnston RL, Taylor H, Adams M, Tole DM, Asaria RH, Galloway P, Sparrow JM. The Cataract National Dataset electronic multicentre audit of 55 567 operations: risk stratification for posterior capsule rupture and vitreous loss. Eye. 2009;23:31–37. doi: 10.1038/sj.eye.6703049. [DOI] [PubMed] [Google Scholar]
- 16.Osborne SA, Adams WE, Bunce CV, Fraser SG. Validation of two scoring systems for the prediction of posterior capsule rupture during phacoemulsification surgery. Br J Ophthalmol. 2006;90(3):333–336. doi: 10.1136/bjo.2005.080754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dinakaran S, Desai SP, Raj PS. Is the first post-operative day review necessary following uncomplicated phacoemulsification surgery? Eye (Lond) 2000;14(Pt 3A):364–366. doi: 10.1038/eye.2000.89. [DOI] [PubMed] [Google Scholar]
- 18.Jammal HM, Khader Y, Shawer R, Al Bdour M. Posterior segment causes of reduced visual acuity after phacoemulsification in eyes with cataract and obscured fundus view. Clin Ophthalmol. 2012;6:1843–1848. doi: 10.2147/OPTH.S38303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mandal K, Dodds SG, Hildreth A, Fraser SG, Steel DH. Comparative study of first-day postoperative cataract review methods. J Cataract Refract Surg. 2004;30(9):1966–1971. doi: 10.1016/j.jcrs.2004.01.037. [DOI] [PubMed] [Google Scholar]
- 20.Saeed A, Guerin M, Khan I, Keane P, Stack J, Hayes P, Tormey P, Mullhern M, Beatty S. Deferral of first review after uneventful phacoemulsification cataract surgery until 2 weeks: randomized controlled study. J Cataract Refract Surg. 2007;33(9):1591–1596. doi: 10.1016/j.jcrs.2007.05.022. [DOI] [PubMed] [Google Scholar]
- 21.Lansingh VC, Carter MJ, Martens M. Global cost-effectiveness of cataract surgery. Ophthalmology. 2007;114(9):1670–1678. doi: 10.1016/j.ophtha.2006.12.013. [DOI] [PubMed] [Google Scholar]
- 22.Fattore G, Torbica A. Cost and reimbursement of cataract surgery in Europe: a cross-country comparison. Health Econ. 2008;17(1 Suppl):S71–82. doi: 10.1002/hec.1324. [DOI] [PubMed] [Google Scholar]
- 23.Agarwal A, Kumar DA. Cost-effectiveness of cataract surgery. Curr Opin Ophthalmol. 2011;22(1):15–18. doi: 10.1097/ICU.0b013e3283414f64. [DOI] [PubMed] [Google Scholar]
- 24.Prakash G, Jhanji V, Sharma N, Titiyal JS. Day care vs inpatient cataract surgery: factors governing choices of patients and surgeons in the developing world. Eye (Lond) 2007;21(7):999. doi: 10.1038/sj.eye.6702790. [DOI] [PubMed] [Google Scholar]


