ABSTRACT
The aim:
of this study was to compare two methods of polypropylene mesh fixation for inguinal hernia repair according to Lichtenstein using fibrin glue and suture fixation.
Material and Methods:
The study included 60 patients with unilateral inguinal hernia, divided into two groups of 30 patients – Suture fixation and fibrin glue fixation.
All patients were analyzed according to:
age, gender, body mass index (BMI), indication for surgery–the type, localization and size of the hernia, preoperative level of pain and the type of surgery. Overall postoperative complications and the patient’s ability to return to regular activities were followed for 3 months.
Results and discussion:
Statistically significant difference in the duration of surgery, pain intensity and complications (p<0.05) were verified between method A, the group of patients whose inguinal hernia was repaired using polypropylene mesh–fibrin glue and method B, where inguinal hernia was repaired with polypropylene mesh using suture fixation. Given the clinical research, this systematic review of existing results on the comparative effectiveness, will help in making important medical decisions about options for surgical treatment of inguinal hernia.
Conclusions:
The results of this study may impact decision making process for recommendations of methods of treatment by professional associations, making appropriate decisions on hospital procurement of materials, as well as coverage of health funds and insurance.
Keywords: inguinal hernia, fixation, fibrin glue, polypropylene mesh
1. INTRODUCTION
Inguinal hernia is the protrusion of abdominal organs into the inguinal canal through the natural or acquired defect of the abdominal wall. It is the most common surgical ailments faced by primary care physicians. Hernia operations are one of the earliest forms of surgery. Operation of inguinal hernia represent the most frequent surgical intervention in the domain of general surgery with about twenty million procedures performed a year worldwide. Frequency of inguinal hernia in men is 25%, and in women 2%. In men, indirect inguinal hernias are two times more common than direct inguinal hernias. Risk of inguinal hernia increases with age and annual incidence in persons older than 75 years is about 50%. On average about two thirds of inguinal hernias are indirect and one third is direct (1). About 10% of all inguinal hernias are bilateral (2). Application of prosthetic mesh in inguinal hernia repair results in reduced incidence of relapse, and fibrin glue used as mesh fixative, has contributed to comfortable postoperative period with mild controlled pain and rapid return to daily activities. The method is simple and it can be performed by all surgeons, even by those who have no special interest in hernia surgery. The aim of this study was to compare two methods of fixation of polypropylene mesh for inguinal hernia repair according to Lichtenstein, using fibrin glue fixation and suture fixation.
2. MATERIAL AND METHODS
Prospective and retrospective analysis of 60 patients, who underwent inguinal hernia surgery, were performed at the Department of Surgery, University Clinical Center in Tuzla. Patients were divided into two groups. The experimental group consisted of 30 patients who underwent surgery using the modified method by Lichtenstein–polypropylene mesh fixation with fibrin glue. The control group consisted of 30 patients who underwent surgery using a conventional method by Lichtenstein–suture polypropylene mesh fixation. Both groups were proportionally represented by patients with unilateral, direct (M1, M2) and indirect (L1, L2), inguinal hernia, age 18 to 80 years with physical status ASA 1 and ASA2. From the study were excluded: persons with recurrent, bilateral and hernia type L3 and M3, persons with body mass index above 35kg/m2, those with prolonged use of analgetics, steroids, and anticoagulant drugs, persons addicted to alcohol or drugs, persons suffering from cirrhosis of the liver, with immunodeficiency syndrome, and severe damage to physical or mental health that could affect the investigation. All patients were analyzed according to the following information: age, gender, body mass index (BMI), type, location and size of the hernia, preoperative level of pain (presurgical pain level), surgical techniques, intrasurgical complications, duration of surgery, postsurgical pain level, postsurgical complication (ecchymosis, hematoma, seroma, wound infection, pain), reintervention, postsurgical hospital stay, postsurgical quality of life and postsurgical functional activities. Groin hernias are classified by EHS classification (3). All patients were classified according to the standard anesthetic protocol ASA (American Society of Anesthesiologists) and had surgery under general anesthesia. Polypropylene mesh (Prolene, Ethicon Germany, weight 100g/m2, 164x96 micron pore size, dimensions 15x8cm), is placed on the back wall of the inguinal canal, and the fixation of the mesh is done with individual slowly resorbable suture (poliglactin 910–Vicryl 2.0) and fibrin glue (Tissucol Kit, Baxter, USA), (Figure 1).
Figure 1.

Polypropylene mesh fixation with fibrin glue (Tissucol)
Overall postoperative complications and the patient’s ability to return to regular activities were followed for 3 months. Postoperative patients examination was made after 7 days, 1 month, and 3 months. Pain level was evaluated by visual analogue scale (VAS), graded from 0-10, before surgery, first day after surgery, seventh day after surgery, 1 month and 3 months after surgery.
In statistical data analysis methods of descriptive and inferential statistics were used. The SPSS statistical software for Windows (SPSS, Inc., Chicago, IL) was used for data analysis. Data are expressed as the median value and range or the mean ± standard deviation appropriate. Data from groups were compared with Student t-test. A p-value less than 0.05 was considered as significant in all of the tests.
3. RESULTS
The study included 56 male (93.3%) and 4 female (6.7%) patients, evenly distributed in groups. The average age was 51.3 years (range 19-72 years). Group A had an average age of 52.3 years and group B of 50.3 years. Table 1 is showing presurgical characteristics of patients.
Table 1.
Preoperative characteristics of patients
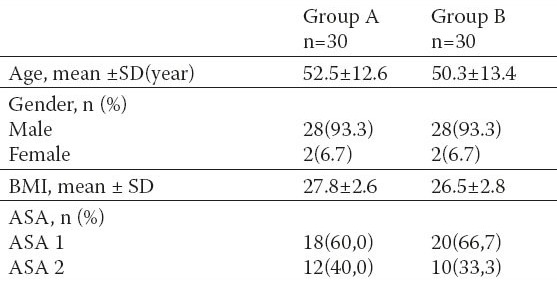
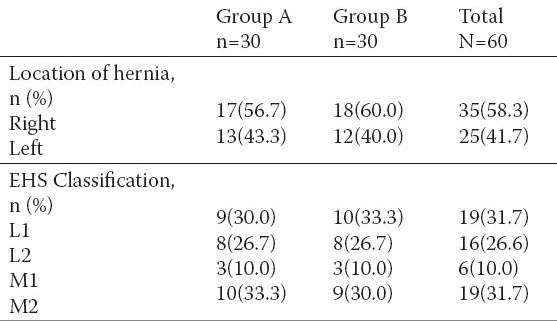
In 35 (58.3%) patients right-sided hernias were found (group A-17, Group B-18), and in 25 (41.7%) patients left-sided hernias were found (group A-13, Group B-12). Intraoperative hernia presentation was: L1-19 (31.7%), L2-16 (26.6%), M1-6 (10%), M2-19 (31.7%). Both groups had similar ratio of different types of hernia. Group A had, L1-9, L2-8, M1-3, M2-10. Group B had, L1-10, L2 -8, M1-3, M2-9 (Table 2).
Table 2.
Preoperative and intraoperative characteristics of inguinal hernias
Study results and statistical analysis of data showed significant differences in the duration of surgery between methods A–fibrin glue, and B–suture fixation (p = 3.121 E-09). The results showed that the duration of surgery by method A was shorter by 5,667 min as compared to method B4.
The intensity of pain evaluated by visual analogue scale (VAS) was measured on 5 occasions: before surgery, first day after surgery, seventh day after surgery, 1 month and 3 months after surgery. Significantly lower pain level was noted in group A after the first and seventh postoperative day, as well as a month after the surgery. Mean values of VAS the first day after surgery was 3.53 vs. 4.70, seventh day after surgery 2.23 vs. 3.16, a month after surgery 0.80 vs.1.56. These values show significant differences between group A and group B.
There was a statistically significant difference in pain intensity between samples first day after surgery (p = 2.281 E-06). Specifically, calculated t-test value (-5.256) is outside of the range which indicates that the null hypothesis (2.00) for bidirectional test values of arithmetic means in observed populations cannot be accepted.
In addition to the risk of 5%, working hypothesis stating that there is a statistically significant difference in pain intensity between group A and group B seventh day after surgery (p = 4.7314 E-06) is accepted. Measured t-test value (-5.06) is outside of the range which indicates that the null hypothesis (2.00) for bidirectional test values of arithmetic means in observed populations cannot be accepted.
Based on the obtained results it can be concluded that there is a significant differences in the severity of pain between the two groups seven day after surgery. In addition, based on the obtained results it can be concluded that there is a statistically significant difference in pain intensity between the groups investigated a month after surgery (p = 7.0051 E-06). Measured t-test value (-6.19) is outside of the range which indicates that the null hypothesis (2.00) for bidirectional test values of arithmetic means in observed populations cannot be accepted.
There was no statistically significant difference in pain intensity between the two groups three months after surgery (p = 0.4468). Measured t-test value (-0.7658) is outside of the range which indicates that the null hypothesis (2.00) for bidirectional test values of arithmetic means in observed populations cannot be accepted (Figure 2).
Figure 2.
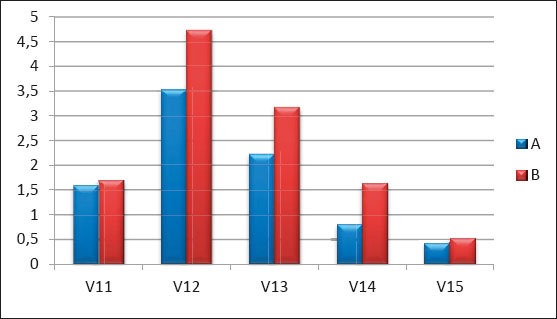
Results obtained by comparing the arithmetic mean of the intensity of pain before surgery (V11), first day after surgery (V12), seventh day after surgery (V13), one month after surgery (V14) and 3 months after surgery (V15).
Paresthesia in the area of the surgical wound or scar was significantly lower in group A. Peresthesia in the same area was followed for seven days, one month and three months after surgery. The ratio between group A and B was as follows: the seventh day after surgery 13.3 vs. 26%, one month after surgery 6.6 vs. 20%, 3 months after surgery 3.3 vs. 13.3% (p = 0.035) (Figure 3).
Figure 3.
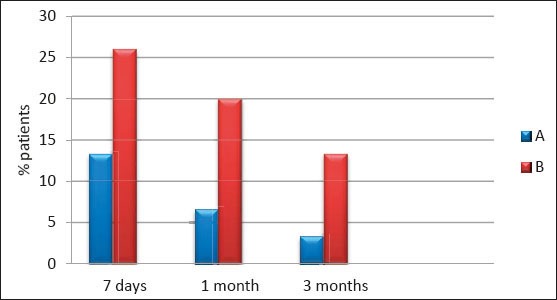
Comparative diagram of paresthesia in studied groups
During the early postsurgical phase 17 complications were observed, two in group A (ecchymosis 1, seroma 1), and 15 in group B (ecchymosis 6, seroma 9). Results showed that 28/30 (93.3%) patients from the group A and 15/30 (50.0%) patients from the group B had no complications. Therefore, group A had significantly less postsurgical complications than group B. The results obtained by statistical processing of the total number of complications between the two groups, with a calculated p value = 0.024, indicates a statistically significant difference in the number of complications (Table 3).
Table 3.
Comparative analysis of the total number of complications in studied groups
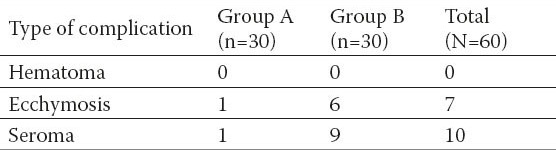
The results confirmed (with the risk of 0.05) a working hypothesis, according to which there is a statistically significant difference in complications–ecchymosis (p = 0.048) between the surgery method A and method B.
The results also confirmed (with the risk of 0.05) the second working hypothesis, according to which there is a statistically significant difference in the proportion of complications–seroma (p = 0.033) between the surgery method A and method B.
The results showed that there were no complications such as hematoma and recurrence, and that there is no statistically significant difference in the proportion of these complications between surgery method A and method B (4).
4. DISCUSSION
The method chosen for surgical treatment of inguinal hernia has to meet certain criteria. Successful surgical treatment of inguinal hernia implies a low rate of recurrence, permanent relief of pain and discomfort caused by a hernia, as well as a low incidence of postoperative complications. For last fifteen years inguinal hernia surgery by Lichtenstein is the first and most widely used open tension-free method. Systematic review on the use of fibrin glue in abdominal wall repair showed to be more beneficiary for fixation of polypropylene mesh with fibrin glue than mechanical–suture fixation. The literature analyzed was from: MEDLINE, EMBASE, and the Cochrane Library Plus databases. Articles found showed randomized clinical trials, non randomized comparative studies and case series that included minimum of 10 patients. In these studies fibrin glue has proven to be biocompatible with the surrounding tissue. In patients treated with fibrin glue, there was a lower prevalence of acute and chronic postoperative pain, and hemorrhagic complications (5).
Our results largely agree with published studies that compared the fixation of the mesh with fibrin glue and suture technique in open inguinal hernia repair by Lichtenstein (6). Data obtained during our research, showed that the use of fibrin glue for fixation of polypropylene mesh in inguinal hernia repair achieved excellent results, with significantly fewer side effects as compared to the conventional method of suture fixation. The results confirmed that the seroma type of complications are significantly less present in fibrin glue fixation methods, while the ecchymosis type of complications are insignificant when using suture techniques. Mean surgical time was reduced by 10% in the group where the fixation was performed using fibrin glue. Patients in this group had less local hemorrhagic complications (hematoma, ecchymosis, seroma) than the patients from the suture group. In the early postoperative period, patients from the fibrin glue group had lower pain intensity and paresthesia (numbness) in the groin. The differences in the results after 7 days and 1 month proved to be significant, however, after 3 months they were not significant. Paresthesia was more prominent in the suture group even after 3 months, in that way showing a significant difference (4).
A prospective, multicenter study was designed to compare fibrin glue with conventional suture tissue fixation in inguinal hernia repair by Lichtenstein. Five hundred and twenty patients were analyzed in whom mesh fixation was performed using fibrin glue (349 patients) or suture (171 patients). Average pain intensity by VAS in the preoperative phase was 2.9, with no significant difference between the groups. Surgery parameters were similar between the treated groups, with the exception of the average duration of the surgery. The surgery was shorter in patients where fibrin glue was used (55.6 vs. 61.2min, p <0.001). Patients in fibrin group also rarely experienced early local “hemorrhagic” complications (hematoma, ecchymosis …) as compared to suture group. After a one-month assessment, patients from the fibrin group reported significantly less pain, paresthesia, and discomfort, as compared to patients from suture group. There was a lower incidence of hematoma (1.7 vs. 8.2%) and ecchymosis (8.6 vs. 15.2%) in patients treated with fibrin glue, as compared to patients in the suture group (both p = 0.001). The average VAS value for pain intensity was significantly lower in the group treated with fibrin glue (2.5 vs. 3.2; p <0.001) (7). One randomized study compared the suture technique, cyanoacrylate glue and fibrin glue as a means of fixation of polypropylene mesh. Morbidity in suture group was 38.98%, in the fibrin glue group was 9.62%, and in cyanoacrylate glue group 10.71% (Suture group vs. Fibrin glue, p <0.001; suture group vs. cyanoacrylate glue, p <0.001) (8).
5. CONCLUSIONS
The presented results show that the mesh fixation with fibrin glue in open, tension-free repair by Lichtenstein is simple, safe and effective. This method of fixation show distinct advantages over staple fixation, with slight possibility of chronic pain, and complications from the wound recurrence. Mesh fixation with fibrin glue is simple procedure that is related to the reduction of postoperative inguinal pain. Fixation with glue causes less nerve injuries, the pubic periosteum injuries, or injuries to blood vessels than conventional methods that are associated with iatrogenic tissue trauma and neuropathic pain.
During polypropylene mesh fixation with fibrin glue minimal retraction is required. Greater retraction, as in suture methods, leads to increased tissue contusion and short-term pain. Therefore, consistent with our results, a small contusion of soft tissues associated with minimal postoperative pain is what makes this method more advanced. Therefore, fibrin glue can be considered as the first option in the fixation of polypropylene mesh in open inguinal hernia repair.
Footnotes
CONFLICT OF INTEREST: NONE DECLARED
REFERENCES
- 1.Nicks BA, Askew K. Hernias eMedicine Web site. 2010. Jan, p. 25. Available at: http://emedicine.medscape.com/article/775630-overview .
- 2.Schneider E. Inguinal hernia: excerpt from the 5-minute Pediatric Consult. WD Web site. Available: http://www.wrongdiagnosis.com/i/inguinal_hernia/book-diseases-20a.htm.2011 .
- 3.Miserez M. The European hernia society groin hernia classification: simple and easy to remember. Hernia. 2007;11(2):113–116. doi: 10.1007/s10029-007-0198-3. [DOI] [PubMed] [Google Scholar]
- 4.Odobašić A. Uloga načina fiksacije polipropilenske mreže u otvorenoj reparaciji preponskih kila. Magistarski rad. 2012 [Google Scholar]
- 5.Morales-Conde S, Barranco A, Socas M, et al. Systematic review of the use of fibrin sealant in abdominal-wall repair surgery. Hernia. 2011;15(4):361–369. doi: 10.1007/s10029-011-0809-x. [DOI] [PubMed] [Google Scholar]
- 6.Campanelli G, Champault G, Pascual MH, Hidalgo M, et al. Randomized, controlled, blinded trial of Tissucol/Tisseel for mesh fixation in patients undergoing Lichtenstein technique for primary inguinal hernia repair: rationale and study design of the TIMELI trial. Hernia. 2008;12:159–165. doi: 10.1007/s10029-007-0315-3. [DOI] [PubMed] [Google Scholar]
- 7.Negro P, Basile F, Brescia A. Open tension-free Lichtenstein repair of inguinal hernia: use of fibrin glue versus for mesh fixation. Hernia. 2011;15:7–14. doi: 10.1007/s10029-010-0706-8. [DOI] [PubMed] [Google Scholar]
- 8.Testini M, Lissidini G, Poli E. A single-surgeon randomized trial comparing sutures, N-butyl-2-cyanoacrylate and human fibrin glue for mesh fixation during primary inguinal hernia repair. Can J Surg. 2010;53(3):155–160. [PMC free article] [PubMed] [Google Scholar]


