Abstract
Objectives
Self-reported hearing impairment is often used to gauge objective hearing loss in both clinical settings and research studies. The aim of this study was to examine whether demographic factors affect the accuracy of subjective, self-reported hearing in older adults.
Design
We examined 3,557 participants aged 50 and older in the National Health and Nutrition Examination Survey (NHANES) cycles 1999-2006 and 2009-10. We examined the relationship between objective and subjective hearing impairment using percent correct classification and misclassification bias in analyses stratified by gender, age group, race/ethnicity, and education.
Results
We found that younger participants tended to overestimate and older participants underestimate their hearing impairment. Older women, blacks, and Hispanics were less accurate in self-reporting than their respective younger age groups.
Conclusions
The association between subjective and objective hearing differs across gender, age, race/ ethnicity, and education and this observation should be considered by clinicians and researchers employing self-reported hearing.
Introduction
Hearing impairment is prevalent in nearly two-thirds of older adults and may contribute to poorer social, physical, and cognitive functioning (Lin et al. 2011; Lin 2012). Clinicians and researchers often utilize patient-reported assessments of hearing rather than objective audiometric assessments for convenience. Concordance of subjective assessments of hearing in comparison to audiometric assessments have been explored in multiple studies typically using measures of sensitivity, specificity, positive and negative predictive value, and these studies have produced varying results (Sindhusake et al. 2001; Valete-Rosalino and Rozenfeld 2005; Kiely et al. 2012). However, measures of sensitivity/ specificity and positive/ negative predictive value do not explicitly inform the clinician or investigator about the overall accuracy of subjective assessments of hearing and whether individuals may preferentially under or overestimate their hearing impairment. Moreover, possible differences in self-reported hearing loss by race/ethnicity have not been investigated in prior studies (Nondahl et al 1998).
In the present manuscript, we assess the performance of subjective assessments of hearing in relation to audiometric classification by calculating a measure of accuracy (total percent correct classification) and direction of misclassification (i.e. whether an individual over or underestimates their hearing impairment compared to audiometry). We investigate whether common demographic factors such as gender, age, race/ethnicity, and education affect the accuracy of self-reported hearing impairment and the direction of misclassification. Understanding the contribution of these factors to self-reported assessments of hearing will assist clinicians in interpreting subjective reports of hearing and researchers who are analyzing data on self-reported hearing status as a surrogate measure of objective audiometric hearing.
Materials and Methods
Study Population
We analyzed data from the 1999-2006 and 2009-2010 cycles of the National Health and Nutrition Examination Survey (NHANES), a nationally representative cross-sectional study of the non-institutionalized, civilian U.S. population. Our analytic cohort was comprised of 3,557 individuals who were 50 years or older and who had complete data on audiometric testing and self-reported subjective hearing.
Hearing Assessment
Objective hearing was defined according to the speech-frequency pure-tone average (PTA) of hearing thresholds at 0.5, 1, 2, and 4 kHz in the better-hearing ear in accordance with the World Health Organization definition (World Health Organization 2014). Hearing impairment was defined as PTA > 25 dB. Air-conduction thresholds were obtained by trained technicians in a sound-attenuating booth according to established NHANES protocols (Centers for Disease Control 2009). Subjective hearing loss was assessed with interviewer-administered questionnaires. Participants were asked to report their level of hearing without the use of hearing aids (for 1999-2004 cycles, respondents answered good, a little trouble, a lot of trouble, deaf; for 2005-06 and 2009-10 cycles, respondents answered excellent, good, a little trouble, moderate trouble, lot of trouble, deaf). We classified the presence of a subjective hearing impairment as any response other than excellent or good.
Statistical Analyses
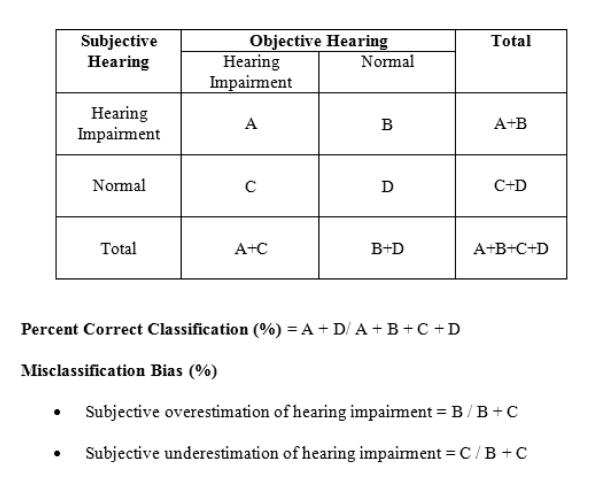
We examined the relationship between objective and subjective hearing impairment using percent correct classification and misclassification bias (Figure 1). Accuracy was the total number of correctly classified observations divided by the total number of observations. Using a 2×2 table, this was calculated by A+D/ A+B+C+D. Misclassification bias describes the percentage of misclassified answers that were overestimated and underestimated by subjective report. For example, subjective overestimation of hearing impairment would be defined by B (number of individuals incorrectly estimating themselves as having hearing impairment compared to audiometric assessment) divided by the total number of individuals who subjectively incorrectly estimated their hearing impairment compared to the audiometric assessment (B+C). Likewise, subjective underestimation of hearing impairment would be defined by C (number of individuals incorrectly estimating themselves as normal hearing compared to the audiometric assessment) divided by the total number of individuals who subjectively incorrectly estimated their hearing impairment compared to audiometric assessment (B+C).
Figure 1.
2×2 Table and calculations for percent correct classification and misclassification bias for subjective rating of hearing impairment (little trouble/ moderate trouble/ lot of trouble hearing/ deaf) compared to audiometric assessment of hearing impairment (speech frequency PTA > 25 dB in the better hearing ear).
Chi-square tests were used to compare accuracy and misclassification bias by gender, age group, race/ethnicity and education. The Mantel-Haenszel chi-square test was used to test age group trends in sub-analyses. We explored for effect modification in stratified analyses. Sampling weights were not included in analyses because the goal of this study was to investigate relationships between objective and subjective assessments of hearing and not to derive generalizable estimates of hearing impairment prevalence. Analyses were conducted with Stata (StataCorp, College Station, TX) and statistical significance was defined as two-sided p<0.05.
Results
Demographic characteristics of the cohort are presented in Table 1. Both genders are equally represented and nearly 60% of the cohort reported no trouble hearing. We analyzed rates of accuracy and misclassification according to demographic factors (Table 2). We observed that overall accuracy was significantly lower in older age groups (74.7% overall correct in age 50-59 vs. 67.8% correct in age 80+) and significantly higher in blacks compared to whites and Hispanics (76.6% correct in blacks vs. 70.5% correct in Hispanics vs. 71.3% correct in whites). Higher education was significantly associated with greater accuracy (75.5% correct in college or greater vs. 70.9% correct in < HS education).
Table 1. Demographic Characteristics of Adults Aged 50 and Older in the National Health and Nutrition Examination Survey Cycles 1999-2006 and 2009-2010.a.
Participants were included if they had objective and subjective hearing data. Percentages are column percentages.
| Characteristic | Cohort n=3557 |
|---|---|
|
| |
| Gender, n (%) | |
| Men | 1770 (49.8) |
| Women | 1787 (50.2) |
|
| |
| Age Groups, n (%) | |
| 50-59 | 862 (24.2) |
| 60-69 | 1026 (28.8) |
| 70-79 | 1029 (28.9) |
| 80+ | 640 (18.0) |
|
| |
| Race/ Ethnicity, n (%) | |
| Hispanic | 692 (19.5) |
| White | 2153 (60.5) |
| Black | 590 (16.6) |
| Other | 122 (3.43) |
|
| |
| Education, n (%) | |
| Less than HSb | 1242 (34.9) |
| HS | 832 (23.4) |
| Some college or AA degreec | 802 (22.5) |
| College grad or more | 677 (19.0) |
| Refused or unknown | 4 (0.11) |
|
| |
| Self-Reported Hearing, n (%) | |
| Excellent/ Goodd | 2111 (59.3) |
| A little trouble | 954 (26.8) |
| Moderate / a lot of trouble | 481 (13.5) |
| Deaf | 11 (0.31) |
Sampling weights were not used in these calculations.
HS – high school education
AA degree – Associate’s degree
Self-reported hearing was dichotomized in statistical analyses as excellent/good versus a little trouble/ moderate trouble/ lot of trouble/ deaf.
Table 2. Percent correct classification and misclassification bias of objective hearing loss compared to self-reported hearing loss.a.
These analyses are further stratified by gender, age group, race/ethnicity, and education. Objective hearing impairment was defined as at least speech PTA > 25 dB in the better-hearing ear and subjective hearing impairment was defined as a little trouble/ moderate trouble/ a lot of trouble hearing/ deaf.
| Percent Correct Classification (%) |
p-value | Misclassification Bias |
p-valueb | ||
|---|---|---|---|---|---|
| Overestimation (%) |
Underestimation (%) |
||||
|
| |||||
| Overall | 71.8 | --- | 45.0 | 55.0 | <.001 |
|
| |||||
| Gender | |||||
| Men | 71.5 | .63 | 44.4 | 55.6 | .68 |
| Women | 72.2 | 45.7 | 54.3 | ||
|
| |||||
| Age Groups | |||||
| 50-59 | 74.7 | .01 | 79.8 | 20.2 | <.001 |
| 60-69 | 73.6 | 62.7 | 37.3 | ||
| 70-79 | 70.2 | 30.3 | 69.7 | ||
| 80+ | 67.8 | 6.80 | 93.2 | ||
|
| |||||
| Race/ Ethnicity | |||||
| Hispanic | 70.5 | .02 | 46.1 | 53.9 | .54 |
| White | 71.3 | 43.7 | 56.3 | ||
| Black | 76.6 | 48.6 | 51.4 | ||
|
| |||||
| Education | |||||
| < HSc | 70.9 | .05 | 38.5 | 61.5 | <.001 |
| HS | 69.4 | 40.0 | 60.0 | ||
| Some college/AA degreed |
72.7 | 51.6 | 48.4 | ||
| College grad or more | 75.5 | 58.4 | 41.6 | ||
|
| |||||
| Sub-analyses | |||||
|
| |||||
| Men | |||||
| 50-59 | 72.0 | .93 | 76.7 | 23.3 | <.001 |
| 60-69 | 72.3 | 56.2 | 43.8 | ||
| 70-79 | 71.0 | 31.4 | 68.6 | ||
| 80+ | 70.3 | 7.37 | 92.6 | ||
|
| |||||
| Women | |||||
| 50-59 | 77.4 | .001 | 83.7 | 16.3 | <.001 |
| 60-69 | 74.8 | 69.4 | 30.6 | ||
| 70-79 | 69.3 | 29.2 | 70.8 | ||
| 80+ | 65.3 | 6.31 | 93.7 | ||
|
| |||||
| Hispanic | |||||
| 50-59 | 78.1 | .01 | 70.0 | 30.0 | <.001 |
| 60-69 | 71.3 | 53.9 | 46.1 | ||
| 70-79 | 62.6 | 30.9 | 69.1 | ||
| 80+ | 61.5 | 5.00 | 95.0 | ||
|
| |||||
| White | |||||
| 50-59 | 72.0 | .59 | 82.4 | 17.6 | <.001 |
| 60-69 | 72.3 | 70.7 | 29.3 | ||
| 70-79 | 71.9 | 27.7 | 72.3 | ||
| 80+ | 68.9 | 7.45 | 92.5 | ||
|
| |||||
| Black | |||||
| 50-59 | 80.5 | .002 | 76.7 | 23.3 | <.001 |
| 60-69 | 83.2 | 58.8 | 41.2 | ||
| 70-79 | 69.0 | 40.4 | 59.6 | ||
| 80+ | 66.0 | 5.88 | 94.1 | ||
Sampling weights were not used in these calculations.
Chi-squared tests for general association were used to compare percent correct classification by gender, age group, race/ethnicity, education, and sub-analyses. Chi-squared tests for general association were used to compare misclassification bias by gender, age group, race/ethnicity and education. The Mantel-Haenszel chi-square test was used to test age group trends in the sub-analyses.
HS – high school education
AA degree – Associate’s degree
For rates of misclassification, we found that younger participants were more likely to overestimate their hearing impairment while older participants tended to underestimate (79.8% overestimate in age 50-59 years vs. 93.2% underestimate in age 80+). This trend was consistent across gender and race/ethnicity. For education, we observed that those with less education underestimated while those with more education tended to overestimate (61.5% underestimate in < HS education vs. 58.4% overestimate in college or greater).
We next investigated whether the association of age and types of misclassification differed by gender and race/ethnicity. In analyses stratified by gender, we observed that accuracy rates were lower in older female age groups (77.4% correct in women age 50-59 vs. 65.3% correct in age 80+) but men had stable rates of accuracy across age groups (72.0% correct in men age 50-59 vs. 70.3% correct in age 80+). Both younger men and women tended to overestimate their hearing impairment, while older men and women underestimated their hearing impairment.
In analyses stratified by race/ethnicity, we observed that both older blacks and Hispanics had lower rates of accuracy (78.1% correct in Hispanics age 50-59 vs. 61.5% correct in age 80+; 80.5% correct in blacks age 50-59 vs. 66.0% correct in age 80+). However, this trend was not seen in whites (72.0% correct in whites age 50-59 vs. 68.9% correct in age 80+). Again, we found that among older age groups, underestimation of hearing impairment was higher across all ethnicities.
Discussion
Our results demonstrate that demographic factors such as gender, age, race/ethnicity, and education are associated with rates of accuracy and the direction of misclassification in subjective versus objective assessments of hearing impairment. Among older age groups, rates of overall accuracy decreased for women but not men and in blacks and Hispanics but not whites. In contrast, increasing rates of subjective underestimation of hearing impairment were associated with older age groups regardless of race/ethnicity or gender. The basis of these observed findings are likely to be multifactorial and could include differential perceptions of hearing loss in younger versus older adults (e.g. older adults may consider hearing impairment to be “normal” and do not report it) and also gender, education, and race/ethnicity differences in how hearing is perceived.
Differential item functioning (DIF) describes the measurement bias when groups with the same underlying ability (i.e. audiometric hearing thresholds) answer questions (i.e. self-reported hearing impairment) differently (Holland and Thayer 1988). Although this concept was historically used in the field of education to explore the DIF of exam questions, we extended this concept to the accuracy of self-reported hearing impairment. Our results found that demographic factors were clearly associated with differential rates of accuracy of self-reported hearing impairment and direction of misclassification.
Our results have relevance to both clinicians and researchers. Clinically, healthcare providers working with older adults should be cognizant of how these demographic factors affect the patient’s self-report of hearing impairment and have a lower threshold of referral for objective audiometric testing. Likewise, researchers who rely on self-reported hearing impairment should be aware that common demographic factors may differentially affect perceptions of hearing impairment and could substantially bias any observed analytic results. Clinical research often relies on self-reported hearing data based on the assumption that self-report is a reasonable surrogate measure of objective hearing. However, our observations call this supposition into question and demonstrate potential factors that may lead to bias.
A limitation of our current manuscript is that we used just one cutoff value (>25 dB speech-frequency average from 0.5-4 kHz in the better ear) to define objective hearing impairment. Different results may have been obtained if we used a different audiometric cutoff for defining objective hearing impairment (Swanepoel et al 2013). We chose to use this definition of objective hearing impairment a priori based on prior epidemiologic studies which demonstrated the clinical significance of this cutoff in the association of hearing with impaired cognitive and physical functioning (Lin et al 2011).
In summary, the relationship between subjective and objective hearing ability varies in accuracy across gender, age, race/ethnicity, and education. These findings should be considered by both clinicians and researchers using self-reported hearing assessments to inform clinical decisions and interpret research studies.
Acknowledgments
Conflicts of Interest and Source of Funding: Dr. Lin receives grants from the NIDCD/NIH (K23DC011279 Grant), Triological Society and American College of Surgeons Clinician Scientist Award, and Eleanor Schwartz Charitable Foundation. He also serves as a consultant for Cochlear Americas, board member for Pfizer and Autifony, receives an honorarium for teaching and speaking from Amplifon, and has a non-financial relationship consisting of volunteer teaching and speaking with Med-El. Dr. Genther receives a grant from the NIH T32 Institutional Training Grant (T32DC000027-24/DC/NIDCD NIH HHS/United States). Ms. Kamil’s coursework is supported by the Oticon Foundation. Funding for the NHANES hearing and disability data were generously provided by the NIDCD (including an interagency agreement with the National Institute for Occupational Safety and Health for training health technicians to perform audiometry), NIA, and NCHS.
References
- Centers for Disease Control [Retrieved 03/10, 2014];National health and nutrition examination survey (NHANES) audiometry procedures manual. 2009 from http://www.cdc.gov/nchs/data/nhanes/nhanes_09_10/audiometry_09.pdf.
- Holland PW, Thayer DT. Differential item performance and the mantel-haenszel procedure. In: Wainer H, Braun HI, editors. Test validity. Erlbaum; Hillsdale, New Jersey: 1988. pp. 129–145. [Google Scholar]
- Kiely KM, Gopinath B, Mitchell, et al. Evaluating a dichotomized measure of self-reported hearing loss against gold standard audiometry: Prevalence estimates and age bias in a pooled national data set. J Aging Health. 2012;24(3):439–458. doi: 10.1177/0898264311425088. [DOI] [PubMed] [Google Scholar]
- Lin FR. Hearing loss in older adults: Who’s listening? JAMA. 2012;307(11):1147–1148. doi: 10.1001/jama.2012.321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin FR, Thorpe R, Gordon-Salant S, et al. Hearing loss prevalence and risk factors among older adults in the united states. J Gerontol A Biol Sci Med Sci. 2011;66(5):582–590. doi: 10.1093/gerona/glr002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin FR, Metter EJ, O’Brien RJ, et al. Hearing loss and incident dementia. Arch Neurol. 2011;68:214–220. doi: 10.1001/archneurol.2010.362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nondahl DM, Cruickshanks KJ, Wiley TL, et al. Accuracy of self-reported hearing loss. Audiol. 1998;37(5):295–231. doi: 10.3109/00206099809072983. [DOI] [PubMed] [Google Scholar]
- Sindhusake D, Mitchell P, Smith W, et al. Validation of self-reported hearing loss. the blue mountains hearing study. Int J Epidemiol. 2001;30(6):1371–1378. doi: 10.1093/ije/30.6.1371. [DOI] [PubMed] [Google Scholar]
- Swanepoel, de W, Eikelboom RH, Hunter ML, et al. Self-reported hearing loss in baby boomers from the Busselton Healthy Ageing Study: audiometric correspondence and predictive value. J Am Acad Audiol. 2013;24(6):514–21. doi: 10.3766/jaaa.24.6.7. [DOI] [PubMed] [Google Scholar]
- Ventry IM, Weinstein BE. The hearing handicap inventory for the elderly: a new tool. Ear Hear. 1982;3(3):128–134. doi: 10.1097/00003446-198205000-00006. [DOI] [PubMed] [Google Scholar]
- Valete-Rosalino CM, Rozenfeld S. Auditory screening in the elderly: Comparison between self-report and audiometry. Braz J Otorhinolaryngol. 2005;71(2):193–200. doi: 10.1016/S1808-8694(15)31310-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. World health organization prevention of blindness and deafness (PBD) program [Retrieved, 2014];Prevention of deafness and hearing impaired grades of hearing impairment. from http://www.who.int/pbd/deafness/hearing_impairment_grades/en/index.html.