Abstract
Background
Clinically elevated anxiety is a common, impairing feature of autism spectrum disorders (ASD). A modular CBT program designed for preteens with ASD, Behavioral Interventions for Anxiety in Children with Autism (BIACA; Wood et al., 2009), was enhanced and modified to address the developmental needs of early adolescents with ASD and clinical anxiety.
Method
Thirty-three adolescents (11–15 years old) were randomly assigned to 16 sessions of CBT or an equivalent waitlist period. The CBT model emphasized exposure, challenging irrational beliefs, and behavioral supports provided by caregivers, as well as numerous ASD-specific treatment elements. Independent evaluators, parents, and adolescents rated symptom severity at baseline and post-treatment/post-waitlist.
Results
In intent-to-treat analyses, the CBT group outperformed the waitlist group on independent evaluators’ ratings of anxiety severity on the Pediatric Anxiety Rating Scale (PARS) and 79% of the CBT group met Clinical Global Impressions-Improvement scale criteria for positive treatment response at posttreatment, as compared to only 28.6% of the waitlist group. Group differences were not found for diagnostic remission or questionnaire measures of anxiety. However, parent-report data indicated that there was a positive treatment effect of CBT on autism symptom severity.
Conclusions
The CBT manual under investigation, enhanced for early adolescents with ASD, yielded meaningful treatment effects on the primary outcome measure (PARS), although additional developmental modifications to the manual are likely warranted. Future studies examining this protocol relative to an active control are needed.
Keywords: cognitive behavioral therapy, autism spectrum disorders, anxiety disorders, parent-training
Many youth with autism spectrum disorders (ASD) experience clinically elevated anxiety symptoms, a characteristic associated with disrupted functioning across multiple domains. Although considerable work has been done addressing the treatment needs of young children with ASD with varying clinical presentations (e.g., Dawson et al., 2010; Kasari, 2002), limited attention has been given to treatments for adolescents with ASD. There is an increasing base of research on cognitive behavioral therapy (CBT) for children with ASD and concurrent clinical anxiety (cf. Wood & Schwartzman, 2013), though again, relatively less research has focused on adolescents. Treatments for adolescents with ASD and concurrent anxiety disorders have at least two clear imperatives: they should be developmentally appropriate for adolescents; and they should address ASD-related barriers to youth uptake of anxiety treatment procedures (e.g., cognitive restructuring and exposure therapy).
A high proportion of youth with ASD meet criteria for a concurrent psychological disorder (e.g., anxiety or depressive disorders) or clinically elevated psychiatric symptoms (e.g., anxious or dysphoric symptoms) (e.g., de Bruin, Ferdinand, Meesters, de Nijs, & Verheij, 2007; Gadow, DeVincent, & Schneider, 2009; Kuusikko et al., 2008). For example, as compared to younger children with ASD and typically-developing youth, Kuusikko et al. (2008) found that social anxiety and behavioral avoidance are more pronounced among early adolescents with high-functioning ASD. Kuusikko and colleagues speculated that youth with high-functioning ASD might begin to observe and comprehend their own impaired social skills in early adolescence, thereby increasing the likelihood of self-consciousness in such situations, leading to behavioral withdrawal and other outward manifestations of anxiety. De Bruin and colleagues and other investigators using diagnostic interviews with youth with ASD have confirmed that rates of the primary anxiety disorders, not just social anxiety disorder, are elevated in youth with ASD.
Clinical anxiety is linked with significant functional impairment in youth with ASD. For example, higher levels of anxiety are associated with greater impairments in social responsiveness and social skills in youth with ASD (Bellini, 2004; Chang, Quan, & Wood, 2012; Green, Gilchrist, Burton, & Cox, 2000). This follows from the tendency of anxiety to promote social avoidance, which prevents opportunities for the development of relationships (Rinck et al., 2010). It is therefore possible that treatment of anxiety could positively impact functional impairment and even core ASD symptom severity (Drahota, Wood, Sze, & Van Dyke, 2011; Storch et al., 2013; Wood, Drahota, Sze, Har, et al., 2009).
Adolescents with ASD present a complex clinical picture. In addition to anxiety symptoms, adolescents with ASD are likely to present with more complex and severe diagnostic sequelae than same-age peers. Depression and anhedonia are frequently observed among adolescents with ASD (Ghaziuddin & Greden, 1998). Peer victimization is pronounced during adolescence for those with ASD (Shtayermman, 2007), which could be a factor associated with the high levels of anxiety and depression. High levels of conduct problems (Green et al., 2000) and hyperactivity (Attwood, 1998) have also been observed in samples of adolescents with ASD. The transition to adolescence is a sensitive developmental epoch for those with and without ASD, replete with significant changes in biological maturation and the evolution of one’s social network. As noted by McGovern and Sigman (2005), adolescence may be a time of both “continuity and change” for youth with ASD. Although research on adolescents with ASD is notably scant, overall continuity in the diagnosis of ASD between childhood and adolescence has been observed and even high-functioning adolescents with ASD still suffer significant impairments in domains such as social competence, peer approval, and anhedonia relative to non-affected peers (Eaves & Ho, 2008; Williamson, Craig, & Slinger, 2008). Interventions for anxiety in youth with ASD likely need to take into account these concurrent challenges in order to effect maximal impact on anxiety.
To date, there have been eight pilot studies using a randomized, controlled trial (RCT) design examining the efficacy of CBT protocols designed for treating anxiety in children and youth with ASD. Three of these trials were conducted using an individualized CBT manual developed for children with ASD (7 to 11 years old) entitled Behavioral Interventions for Anxiety in Children with Autism (BIACA; Wood, Drahota, Sze, Har, et al., 2009), which employs a modular treatment algorithm and includes significant caregiver involvement and training (Fujii et al., 2013; Storch et al., 2013; Wood, Drahota, Sze, Har, et al., 2009). BIACA is designed to the treat symptoms of separation anxiety disorder, generalized anxiety disorder, social anxiety disorder, and obsessive compulsive disorder in children with ASD. Each of these trials has demonstrated significant reductions in anxiety symptoms at post-treatment in comparison with a waitlist or treatment-as-usual comparison condition, with treatment response rates and anxiety disorder remission rates, as rated by an independent evaluator blind to treatment condition, at well over 50% across the three trials. Further, anxiety treatment gains in the CBT groups were accompanied by improved ratings of adaptive skills and reduced ASD symptom severity (Drahota et al., 2011; Storch et al., 2013; Wood, Drahota, Sze, Van Dyke, et al., 2009). The other five CBT protocols have been delivered in a group therapy format to children or adolescents (Chalfant, Rapee, & Carroll, 2006; Reaven, Blakeley-Smith, Culhane-Shelburne, & Hepburn, 2012; Sofronoff, Atwood, & Hinton, 2005; Sung et al., 2011; White et al., 2013), with three of five of the programs exhibiting statistically significant effects on at least some anxiety measures at post-treatment.
One area that remains unclear is whether an individually administered CBT protocol can address the anxiety symptoms in adolescents with ASD as it has addressed such symptoms in children with ASD under the age of 12 years. While several studies provide preliminary support for group CBT for adolescents with ASD, the linear format of group therapy limits matching intervention techniques to patient characteristics. Given the heterogeneity of phenotypes in adolescents with ASD, individual interventions (e.g., modular treatments) tailored to a patient’s specific characteristics are likely to be particularly efficacious (Mundy, Henderson, Inge, & Coman, 2007). However, as noted above, adolescents with ASD manifest particular forms of anxiety symptoms compared to preteen children with ASD (e.g., heightened social anxiety). Other aspects of adolescence (cognitive and physical development, increased stress from school workloads and social complexity, emerging sexuality) may impinge upon the typical treatment process that appears to be efficacious for preteens with ASD. Therefore, the individually administered CBT program, Behavioral Interventions for Anxiety in Children with Autism (BIACA; Wood, Drahota, Sze, Har, et al., 2009; Wood, Drahota, Sze, Van Dyke, et al., 2009), was adapted to address related adolescent-specific issues, incorporate teen-friendly language and handouts, and otherwise ensure developmental appropriateness. This protocol was tested with a cohort of early adolescents with ASD and clinical anxiety to evaluate efficacy for treating acute symptoms of separation anxiety disorder, generalized anxiety disorder, social anxiety disorder, and obsessive compulsive disorder. It was hypothesized that CBT would outperform a waitlist condition on independent evaluators’ ratings of symptom severity and treatment response. Secondary hypotheses were that CBT would outperform the waitlist control on child- and parent-rated anxiety and parent-reported autism symptom severity, given that other studies of BIACA with preteen children have found collateral effects on this domain (Storch et al., 2013; Wood, Drahota, Sze, Van Dyke, et al., 2009).
Method
Participants
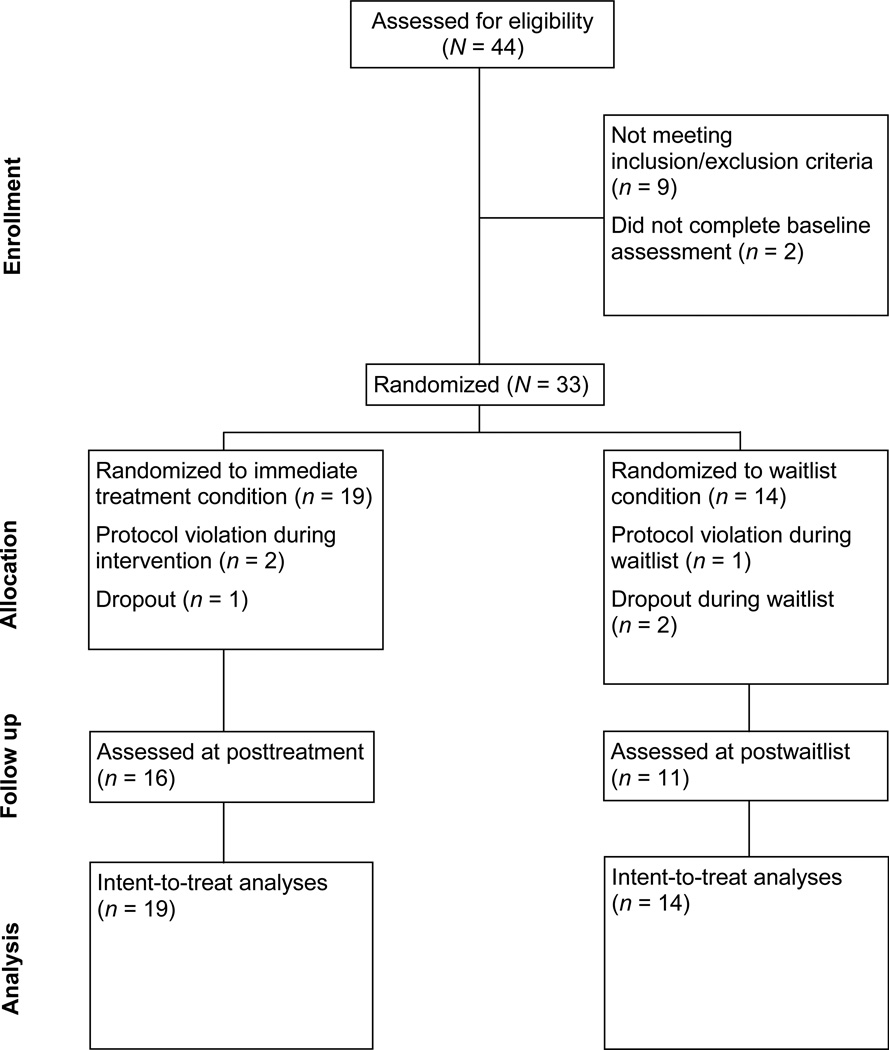
The sample included 33 adolescents, ranging in age from 11 to 15 years (M = 12.3 years, SD = 1.14) and their parents, recruited through two research sites: 17 at the University of South Florida (USF) Rothman Center for Neuropsychiatry (11 males, 6 females) and 16 at the University of California - Los Angeles (UCLA) Center for Autism Research and Treatment (12 males, 4 females). Sample size was determined via power analysis, where an ES of d=1.0 was assumed for group differences in anxiety reduction, based on past CBT trials (e.g., Storch et al., 2013; Wood, Drahota, Sze, Har, et al., 2009). Given this estimate, a sample size of N=33 would provide a power of .80. See Figure 1 for descriptive data on participant flow through the study. Youth met research criteria for ASD and at least one anxiety disorder with a clinical severity level above 3 (M = 5.76; SD = 0.79) as determined through interviews with both parents and youth. Youth were identified as 67% Non-Hispanic White, 9% Asian, 6% African American, 3% Latino and 15% Other/Mixed. Table 1 provides additional descriptive information by treatment group. There were no significant research site differences for demographic variables.
Figure 1.
Consort flow diagram.
Table 1.
Demographics, Diagnoses, and Medication Usage for Children in the Immediate Treatment (CBT) and Waitlist (WL) Conditions
|
CBT No. (%) n = 19 |
WL No. (%) n = 14 |
p | |
|---|---|---|---|
| Child sex (male) | 13 (68) | 10 (71) | 1.00 |
| Child age | 12.4 (SD = 1.3) | 12.2 (SD = .98) | 0.63 |
| Child ethnic background | |||
| Caucasian | 12 (63) | 10 (72) | 0.72 |
| Latino / Latina | 0 (0) | 1 (7) | 0.42 |
| Asian / Pacific Islander | 2 (11) | 1 (7) | 1.00 |
| African American | 1 (5) | 1 (7) | 1.00 |
| Multiracial / Other | 4 (21) | 1 (7) | 0.37 |
| Autism spectrum disorders | |||
| Autistic disorder | 12 (63) | 10 (72) | 0.72 |
| PDD-NOS | 1 (5) | 2 (14) | 0.56 |
| Asperger syndrome | 6 (32) | 2 (14) | 0.42 |
| Baseline anxiety disorders | |||
| SoP | 9 (47) | 5 (35) | 0.72 |
| SAD | 3 (16) | 4 (29) | 0.42 |
| OCD | 2 (11) | 1 (7) | 1.00 |
| GAD | 5 (26) | 4 (29) | 1.00 |
| Other comorbid diagnoses | |||
| ADHD | 14 (74) | 9 (64) | 0.71 |
| Dysthymia / MDD | 6 (32) | 1 (7) | 0.20 |
| ODD / CD | 4 (21) | 1 (7) | 0.37 |
| PTSD | 1 (5) | 0 (0) | 1.00 |
| Psychiatric medication use | |||
| Antidepressant | 8 (42) | 5 (36) | 0.74 |
| Atypical antipsychotic | 6 (32) | 3 (21) | 0.70 |
| Stimulant or atomoxetine | 3 (16) | 2 (14) | 1.00 |
Note. Comorbid diagnoses and psychiatric medication do not add up to 100% due to multiple diagnoses or medication.
SoP = social phobia; SAD = separation anxiety disorder; OCD = obsessive-compulsive disorder; GAD = generalized anxiety disorder; ADHD = attention deficit hyperactivity disorder; MDD = major depressive disorder; ODD = oppositional defiant disorder; CD = conduct disorder; PTSD = post-traumatic stress disorder.
Fisher’s exact tests were used for categorical outcomes, and independent t-tests were used for continuous outcomes
Autism diagnosis was confirmed through the use of the Autism Diagnostic Observation Schedule (ADOS; Lord, Rutter, DiLavore, & Risi, 2002) and the Autism Diagnostic Interview-Revised (ADI-R; Le Couteur, Lord, & Rutter, 2003). Additional inclusion criteria included being between 11–15 years of age and having a Full Scale IQ score of 85 or above on the Wechsler Intelligence Test for Children, 4th Edition (WISC-IV; Wechsler, 2003). Participants were excluded if youth: (1) were concurrently receiving cognitive behavioral therapy, social skills training with homework, or applied behavioral analysis (interventions could be discontinued prior to participation); (2) had initiated an antidepressant or antipsychotic within 12 or 6 weeks, respectively, prior to treatment (or, changed an established medication regimen within 8 weeks for an antidepressant or 4 weeks for an antipsychotic); (3) evidenced clinically significant suicidality within the past six months; or (4) met DSM-IV diagnostic criteria for bipolar, schizophrenia, schizoaffective disorders, or substance abuse (six months before treatment). However, youth receiving supportive psychotherapy (not CBT) in the community or school setting, or who had social skill groups or other group therapy that did not include homework assignments, or youth with stable psychiatric medication regimens were permitted to maintain this treatment during the study.
Procedures
Families interested in participating in the study initially contacted project coordinators at the UCLA and USF sites, respectively. Families who appeared to meet inclusion/exclusion criteria based on preliminary phone screens were invited for an in-person diagnostic assessment with trained clinicians. Written parental consent and child assent were reviewed and collected prior to initiation of assessments. Trained independent evaluators at each site, blind to group assignment, conducted anxiety and autism interviews with consented youth and at least one participating parent/legal guardian consisting of the Anxiety Disorders Interview Schedule for the DSM-IV-Child Version, Child and Parent Report Forms (ADIS-IV-C/P; Silverman & Albano, 1996) and the Pediatric Anxiety Rating Scale (PARS; RUPP, 2002) as well as the ADOS and ADI-R. If participants did not have documentation substantiating a Full Scale IQ score from an evaluation conducted within the past three years, the WISC-IV was conducted as well. Approximately one week after completing the screening assessments, consented participants completed additional study questionnaires. These assessment materials were given at baseline, post-treatment (after the final session), and at 1-month follow-up. Families were offered $15 for participating in the assessments at each timepoint.
All children who met inclusion/exclusion criteria were block randomized by a research coordinator at each site into either immediate treatment (CBT) or waitlist (WL) using a computer randomization program (the randomization sequence was concealed from investigators until interventions were assigned). Block randomization procedures stratified children based on age and gender; hence, when a child of a particular age and gender was randomized to one of the conditions, the next child with these same characteristics was automatically assigned to the other condition. Participants assigned to the WL condition waited 16 weeks before receiving the current treatment.
Clinicians and therapists were postdoctoral clinical psychology fellows or doctoral students in clinical or educational psychology programs, all with experience with and trained to work with youth with ASD. Clinicians received weekly individual clinical supervision, per participant, by the principal investigators and their doctoral level expert designees (with Ph.D.s in clinical psychology and expertise with the treatment protocol) at UCLA and USF. Additional supervision included as-needed cross-site conference calls with the principal investigators and therapists. The integrity and caliber of treatment was assessed independently at the University of Miami. Twenty sessions (10 sessions per site) were randomly selected for adherence rating using a checklist developed by Wood and colleagues (2009). After establishing accuracy with the second author, two coders otherwise uninvolved in the investigation rated all 20 tapes. Agreement between raters was excellent (κ = .89) as was adherence to the treatment protocol (75.4%).
Treatment Program
The BIACA manual was used for this investigation. Sixteen weekly sessions were offered to all families with sessions taking place at a university clinic or an associated autism community clinic that referred families to the study. Therapists worked with individual families, with each session lasting approximately 90 minutes (about 30 minutes separately with the youth and parent(s), and 30 minutes conjointly with the child and parents).
BIACA includes adaptations to traditional youth CBT protocols to optimize treatment effectiveness. Given the complexity of addressing youth anxiety in the context of ASD, sessions were provided in a modular format, adhering to a treatment algorithm (see Sze & Wood, 2007). Therapy modules were selected by the therapist and clinical supervisor on a session-by-session basis to appropriately address the clinical needs of the youth. Despite the added flexibility of the modular format, a minimum of three sessions were spent on basic coping skills and eight were spent on in vivo exposure to ensure an adequate and comparable dose of the core elements of CBT for anxiety across cases. Second, core CBT coping skills (e.g., behavioral activation, cognitive restructuring) and in vivo exposures were included in the treatment protocol. A youth-friendly acronym, the K.I.C.K. Plan, was utilized to help youth remember a sequence of steps to cope with anxious situations. Third, a series of modules focused on fundamental concerns of anxious adolescents who have autism addressed the following areas: poor social skills, adaptive skills deficits, circumscribed interests and stereotypies, poor attention and motivation, common comorbidities in ASD (e.g., disruptive behavior disorders), and school-based problems. The BIACA model emphasizes key skills for positive social behavior skills and developmentally appropriate get-togethers that can be used in real-world settings, such as offering others the first turn. Parent-training is provided through parent-only portions of each session in specific modules. With parents, a key emphasis was to encourage youth independence, increase communication skills, and create a toolbox of skills to diffuse problematic situations. Parent support of home-based exposures and use of reward systems was emphasized. Finally, one to two consultations are offered to teachers or other school personnel in support of the overall exposure-therapy goals that may take place on school grounds (e.g., participating in peer interactions during lunch) employing the same behavioral support strategies offered to parents.
Measures
Anxiety Disorders Interview Schedule for the DSM-IV-Child and Parent Versions (ADIS-IV-C/P; Silverman & Albano, 1996)
The ADIS-IV-C/P is a semi-structured diagnostic interview that assesses all DSM-IV anxiety disorders in children and adolescents ages 7–17 years. Interviews are conducted separately with the youth and the parent(s). Each diagnosis receives a clinical severity rating (CSR) on a 0–8 scale, with CSRs ≥ 4 indicating clinical levels of severity and impairment. Among youth with ASD, the ADIS-IV-C/P has demonstrated excellent parent-clinician agreement (Storch, Ehrenreich-May, et al., 2012) and convergent validity (Renno & Wood, 2013; Storch, Wood, et al., 2012). Agreement between primary diagnostician and a second independent reliability coder for primary anxiety disorder in the present sample was perfect (N=17; K=1.0). Positive diagnostic status at post-treatment/post-waitlist and follow-up was defined as a child still meeting criteria for their primary anxiety disorder diagnosis with an ADIS-C/P CSR score ≥ 4.
Clinical Global Impression–Improvement (CGI-Improvement; Guy, 1976)
The CGI-Improvement is a single-item, clinician-rated measure of overall diagnostic improvement and ranges from 1 (very much improved) to 7 (very much worse). Treatment responders were classified as those rated either a 1 (very much improved) or 2 (much improved). The CGI-Improvement scale was rated at post-treatment.
Multidimensional Adolescent Satisfaction Scale (MASS; Garland, Saltzman, & Aarons, 2000)
The MASS is a psychometrically sound 21-item instrument that assesses treatment satisfaction and perceived improvement in therapy. Items are rated on a 0–3 scale where anchors range from "strongly disagree/no, not at all" to "strongly agree/yes, a lot" in response to statements such as "has therapy helped your problems get better" and "overall, has therapy helped you". In the CBT group, parents (n=14) and youths (n=15) completed MASS forms at the post-treatment assessment, where average item responses were evaluated.
Multidimensional Anxiety Scale for Children—parent report (MASC-P; March, 1998)
The MASC-P is a standardized 39-item, 4-point Likert-type scale parent-report scale of anxiety symptoms within children. Each item is rated on a scale ranging from 0 (never true) to 3 (often true) with a higher score indicating a greater amount of anxiety. The MASC-P has previously been found to have robust psychometric properties, including in ASD samples (Renno & Wood, 2013). In the current sample, internal consistency for total MASC-P scores was good at all timepoints (α = .68–.84).
Pediatric Anxiety Rating Scale (PARS; RUPP, 2002)
The PARS is a 50-item, clinician-administered checklist of anxiety symptoms in children and adolescents. Interviews with the child/adolescent and parent(s) are conducted separately, asking each respondent to indicate if each symptom was present or absent (yes/no) during the previous week. Following these interviews, clinicians integrate child and parent information to collectively rate endorsed symptoms on seven dimensions of overall severity, using a 6-point scale (0 = none, 1–5 = minimal to extreme). The total score is calculated by summing the scores of five of these dimensions. Psychometric properties of the PARS Total Score in ASD samples are acceptable; the adolescents in this study were part of a larger study of the PARS in youth with ASD (Storch, Ehrenreich-May, et al., 2012) in which inter-rater reliability and test-retest reliability for the PARS Total Score were good (ICC = 0.86 and 0.83, respectively). The internal consistency of the PARS Total Score in the present study at each timepoint (α = .55–.74) was similar to that reported in the original measure development study of the PARS (RUPP, 2002).
Revised Child Anxiety and Depression Scale (RCADS; Chorpita, Yim, Moffitt, Umemoto, & Francis, 2000)
The RCADS is a 47-item, self-report measure of child/adolescent anxiety and depressive symptoms. The RCADS has previously demonstrated good internal consistency (average Cronbach’s α = .77; Chorpita et al., 2000), and has shown good validity in discriminating between anxiety and depression symptoms (Chorpita et al., 2000). In this sample, internal consistency was found to be excellent across all time points (α = .94–.96).
Service Assessment for Children and Adolescents (SACA; Horwitz et al., 2001)
The SACA is a standardized interview querying various mental health services obtained for the child (e.g., inpatient, outpatient, in-school, and family-based services). The SACA was administered at baseline and post-treatment.
Social Responsiveness Scale (SRS; Constantino, 2002)
The SRS is a standardized 65-item, 4-point Likert-type parent-report form assessing children’s autism-specific characteristics such as social communication deficits and repetitive behaviors. The SRS provides a total score and has demonstrated robust reliability and validity. Alphas for the current sample ranged from .75 to .85 across the three timepoints.
Analytic Plan
To evaluate between-group continuous outcomes, ANCOVAs were performed, where post-treatment scores were predicted by treatment condition while covarying for baseline scores. Comparison of response rates and post-treatment diagnostic status (i.e., categorical outcomes) were conducted by Fisher’s exact test, where post-treatment response/diagnostic status was contrasted with treatment group. CGI-Improvement scores reflecting “much improved” or “very much improved” were considered treatment responders, while all other cases were considered non-responders, following research precedent (e.g., Storch, Lewin, De Nadai, & Murphy, 2010). Missing data were addressed via multiple imputation using PROC MI and PROC MIANALYZE in SAS 9.3 using 100 imputations, where imputation models included all principal outcome ratings of anxiety and ASD functioning (i.e., the PARS, ADIS CSR, CGI-I, and SRS) as well as treatment group. Degrees of freedom for multiply imputed hypothesis-testing models were adjusted based on recommendations by Barnard and Rubin (1999), and all variables were within recommended ranges of ± 2 with regard to skewness and kurtosis (Cameron, 2004) prior to data imputation. Scores on the CGI-Improvement and diagnostic status at posttreatment/postwaitlist were imputed using the last observation carried forward (LOCF) method. Effect sizes were computed for both within- and between-group analyses to evaluate the size of treatment effects, where all effect sizes for continuous variables were converted first to Cohen’s d from imputed results using formulae provided by Cooper, Hedges, and Valentine (2009) and then converted to Hedges' g (Hedges & Olkin, 1985) to adjust for the study sample size, with effect sizes of .2, .5, and .8 representing small, medium, and large effects respectively (Cohen, 1988). Of note, some larger effects may be statistically nonsignificant while some relatively smaller effects may be significant, due to the effect sizes being point estimates while significance tests reflect uncertainty modeled during the imputation process. Among variables used for treatment outcome analyses, the proportion of missing data was relatively small (13%). To evaluate within-group changes from post-treatment to follow-up, paired t-tests and Fisher’s exact tests were used. Group differences in rates of service use were evaluated by Fisher's exact test.
Results
The intent-to-treat sample size was 33. There were 2 dropouts and 1 protocol violation during the waitlist, and 1 dropout and 2 protocol violations (beginning excluded treatments or changing medication dose) during CBT (see Figure 1). Recruitment began on 9/21/2010 and ended on 6/14/2011; post-treatment assessments were completed on 12/13/2011. Table 1 presents descriptive and diagnostic information for children in the two treatment conditions. Total child DSM-IV diagnoses including ASD, anxiety disorders, and additional comorbid diagnoses ranged from 3 to 8 diagnoses per participant, with an average of 5.55 (SD = 1.54).
Pretreatment Comparability
Pretreatment group differences were assessed with chi-square tests and t-tests. There were no statistically significant treatment group differences on demographic and youth diagnostic variables (results are presented in Table 1).
Treatment Outcome
Group means and standard deviations for study outcome variables are presented in Table 2. A significant difference was observed at post-treatment/post-waitlist for the PARS (p=.04, ES=0.74), with the CBT group showing lower anxiety scores after controlling for baseline relative to the WL group. With regard to CGI-Improvement criteria for positive treatment response, 79% (15/19) of those condition in the CBT condition experienced treatment response compared to 28.6% (4/14) of those in the WL at post-waitlist (p<.01, odds ratio=9.38). When considering positive diagnostic status at post-treatment, in the CBT condition, 6 of 19 (32%) participants did not meet criteria for their principal anxiety disorder diagnosis at post-treatment, in comparison to 3 of 14 (21%) of participants in the WL condition. However, this difference was not found to be statistically significant (p=.70, odds ratio=1.69), nor were group differences found for ADIS CSR changes for principal anxiety diagnoses (p=.25, ES=0.39)
Table 2.
Descriptive Statistics for Outcome Variables for Children in the Immediate Treatment (CBT) and Waitlist (WL) Conditions
| Measure | WL (n = 14) | CBT (n = 19) | ||||||
|---|---|---|---|---|---|---|---|---|
| Baseline M (SD) |
Post-treatment M (SD) |
dw | Baseline M (SD) |
Post-treatment M (SD) |
dw | db | ||
| PARS | 18.29 (2.09) | 14.04 (2.64) | 1.71 | 17.16 (2.39) | 11.62 (3.26) | 1.78 | 0.74 | |
| SRS | 113.25 (22.49) | 105.75 (11.89) | 1.52 | 108.41 19.08) | 82.56(16.34) | 6.01 | 1.17 | |
| ADIS-CSR | 5.50 (0.65) | 4.04 (1.88) | 0.36 | 5.68 (0.89) | 3.28 (2.10) | 0.64 | 0.39 | |
| MASC-P | 62.49 (14.48) | 58.44 (9.01) | 1.37 | 60.58 (16.01) | 50.21 (12.71) | 2.85 | 0.59 | |
| RCADS | 24.65 (17.31) | 18.31 (14.09) | 1.71 | 28.09 (20.27) | 19.58 (14.65) | 1.47 | 0.02 | |
Note. All statistics are based on the same multiple imputation models used for study analyses;
dw = Within-subjects d; db = Between-subjects d;
Abbreviations: PARS=Pediatric Anxiety Rating Scale; SRS=Social Responsiveness Scale; ADIS-CSR=Anxiety Disorders Interview Schedule Clinical Severity Rating; CBCL=Child Behavior Checklist; RCADS=Revised Child Anxiety and Depression Scale
Group differences were observed at post-treatment/post-waitlist for the SRS (p<.01, ES=1.17), reflecting significant improvement in ASD symptoms in the CBT group relative to the WL condition. However, group differences for parent-reported anxiety were only marginally statistically significant (using the MASC-P, p=.10, ES=0.59) and nonsignificant for youth-reported anxiety (using the RCADS; p=.93, ES=0.02). Both parents (M=2.49, SD=0.57) and youths (M=2.21, SD=0.46) in CBT reported satisfaction with treatment via the MASS.
Maintenance of treatment gains at 1-month follow-up
In the CBT condition, 13 adolescents who had been treatment responders (e.g., positive CGI response at posttreatment) returned for a 1-month follow-up assessment. At this time point, there was no significant change in clinician-rated anxiety between the post and 1-month assessment findings on the PARS (p=.79, ES=0.07), and 10 of the 13 participants maintained treatment responder status (a statistically non-significant decline; p=.22). Additionally, 8 of the 13 (62%) children showed remission of their principal diagnosis at follow-up (a significant improvement from post-treatment; p=.02). In this group of 13 youth, with regard to self-report measures, a significant reduction in anxiety from post-treatment to 1-month follow-up was reported by youths (using the RCADS; t(8)=2.86, p=.02, ES=0.95), with a marginal effect for parents (using the MASC-P; t(7)=2.10, p = .07, ES=.74). Additionally, no significant change in ASD symptoms was found at 1-month follow up (using the SRS; t(7)=0.77, p=.47, ES=0.27).
Service use
Since those youth who were removed or dropped out from the study did not complete post assessments, the services described represent treatment-completers. As assessed through the SACA, all youth randomized to the WL condition received some intervention services intended to target anxiety and/or ASD symptoms (e.g., social skill deficits) including social skills training (n=2; 18.2%), psychiatric medication management (n=7; 63.6%), or special education services (n=6; 54.5%). Seven participants (63.6%) received one service and 4 participants (36.4%) received two services. Over half of the adolescents in the WL condition (n=7; 63.6%) were taking psychiatric medications with 2 (18.2%) participants taking one medication and 5 (45.5%) youth taking two medications (see Table 1 for the proportion of randomized youth taking medication).
Similar to the WL arm, the majority of youth randomized to CBT (n=11; 68.8%) received services during the acute phase including medication management visits (n=7; 43.8%), counseling or therapy in school (n=3; 18.8%), special education services (n=5; 31.3%), religious counseling (n=1; 6.3%), case management (n=1; 6.3%), individual supportive psychotherapy (n=2; 12.5%), or was seen in the emergency room for emotional or behavioral problems (n=1; 6.3%). Regarding the number of services, 5 (31.3%) children received no services, 5 (31.3%) children received one service, and 6 (37.5%) youth received two or more services. Nine of 16 children (56.3%) were not taking any psychiatric medication while 2 children (12.5%) were taking one medication and 5 (31.3%) youth were taking two or more. With the exception of the emergency room visit, these services had been initiated prior to the onset of the study. Group differences were not detected in the rate of service use (p=.06).
Discussion
Early adolescents with clinical anxiety may benefit from developmentally appropriate, individually administered CBT with collateral parent and school support components. A notable characteristic of the participants in this study was their overall level of concurrent psychiatric symptomology as illustrated by meeting criteria for multiple (2 to 7) comorbid diagnoses over and above their ASD diagnosis. In spite of the overall level of clinical challenge posed by concurrent ASD-related difficulties and other emotional and behavioral symptoms, the targeted intervention under investigation was associated with greater improvement on the primary outcome measure in the study, the PARS anxiety total score, as rated by independent evaluators, when compared to the waitlist control group. Similarly, there were higher rates of positive treatment response for the CBT group than the waitlist group (79% vs. 28.6%, in intent-to-treat analyses), based on independent evaluator ratings on the CGI-I. Parent reports on the SRS also showed an advantage of CBT over waitlist for autism symptom severity reduction. However, group differences on ADIS anxiety diagnoses or parent and adolescent questionnaire measures of anxiety were not obtained.
Early adolescence is a challenging period for many youth with ASD. The transition to middle school often brings with it a reduced level of structure in the school setting, while simultaneously the onset of puberty introduces a new set of developmental challenges that have biological, emotional, and social aspects (e.g., adjusting to bodily changes; hormonally-mediated emotional changes; and increases in peer competition and interest in sexuality; Booth, Granger, Mazur, & Kivlighan, 2006; Susman et al., 1987; Tremblay, 1998). Navigating this period of development has proven difficult for many children with neurodevelopmental disorders and has been associated with setbacks in emotional and social adjustment when compared to the preadolescent period (Barkley, Anastopoulos, Guevremont, & Fletcher, 1991; Green et al., 2000; Pearson et al., 2006). Anxiety and mood disorders often manifest during this period for susceptible individuals, and traits of negative affectivity, inattention, and aggression can be magnified (Compas, Ey, & Grant, 1993; Kessler, Avenevoli, & Merikangas, 2001; Zahn-Waxler, Shirtcliff & Marceau, 2008). In the context of the multiple symptom domains that are prominent in many adolescents with ASD, strategically intervening with one or more of the sources of maladjustment may, in the best case, trigger some improvement in multiple domains (if the domains are interdependent and an intervention has a strong enough effect), or may, more modestly, only improve directly targeted symptoms to some degree.
The effects of the present intervention, with its relatively modest sample size, suggest an intermediate outcome wherein there may have been a reduction in manifest anxiety severity for many of the youth randomized to CBT, as evidenced by improvement in clinician-reported anxiety severity and positive treatment response, as well as some evidence of a broader effect of treatment in the domain of ASD symptom severity. This pattern of data suggests that observable aspects of anxiety that clinicians were able to rate decreased in the context of participation in CBT. The pattern of positive treatment response is comparable to the proportion reported in the original trial of the BIACA CBT intervention (Wood, Drahota, Sze, Har, et al., 2009), in which 78.5% of the children in CBT exhibited positive treatment response on the CGI in intent-to-treat analyses.
Notably, there was no treatment effect (when compared to the waitlist group) for youth or parent-reported anxiety symptoms on paper-and-pencil measures (although a trend was found for parent report data), or for remission of primary anxiety disorder diagnosis. Furthermore, independent evaluator ratings on the PARS were only modestly improved for the CBT group at posttreatment (M = 11.62; as a reference point, the development paper for the PARS [RUPP, 2002] suggested scores of 14 or higher represent high anxiety and that scores below 10 represent mild or little anxiety), although the between-groups ES was .74, near to the benchmark for a large effect. With a relatively small sample size of 33 youth randomly assigned to condition, there may have been limited statistical power to detect treatment effects with these measures, particularly if they are less sensitive to change in this population. Notably, in a recent consensus statement on recommended outcome measures for use in clinical trials for youth with ASD and anxiety disorders, primarily clinician- and parent-report measures, not youth-report measures, were recommended as the top echelon of measures (LeCavalier et al., 2013). The RCADS was not a highly recommended measure in this consensus statement. It is possible that youth anxiety symptom counts on the RCADS were not sufficiently improved by this CBT program to be detected in an RCT of this size. As noted above, the participating youths had a high level of comorbidity and overall symptomology, and while at the global level the youth may have experienced focal reduction in a few specific anxiety symptoms and associated impairment, which might be reflected in measures like the CGI-Improvement and the PARS total score, perhaps broader symptom count measures like the RCADS or diagnostic threshold measures like the ADIS-IV-C/P were insufficiently sensitive to these types of changes given the youths’ baseline degree of severity and impairment. It is also notable that the treatment appeared tolerable and acceptable for most families as illustrated by the relatively low dropout rate and positive treatment satisfaction data based on both youth and parent reports.
The finding of CBT-related improvement on the SRS, a measure of ASD symptom severity rated by parents, is consistent with the first trials of the BIACA intervention with children in which a similar treatment-related effect on the SRS was obtained (Storch et al., 2013; Wood, Drahota, Sze, Van Dyke, et al., 2009), as well as a more recent CBT intervention for adolescents with ASD and clinical anxiety (White et al., 2013). As noted above, if these changes actually represent attenuated ASD symptom severity, even to a modest degree, it suggests that the anxiety-focus of the CBT interventions may yield an indirect effect on an interdependent area of symptomatology, or that the augmented components of anxiety CBT utilized in the BIACA program, namely the treatment elements focused on social communication skills, exerted an effect on the ASD severity domain. There is increasing recognition in the field that anxiety and ASD symptom severity may be partially interdependent (e.g., Chang et al., 2012; Spiker et al., 2012; Wood & Gadow, 2010). For example, the social avoidance that social anxiety induces likely contributes to the challenges with social initiations, reciprocal communication, conversation maintenance, and friendship associated with ASD (Chang et al., 2012). However, the reciprocal is probably also true—some social anxiety, for example, is undoubtedly generated from social rejection engendered by ASD-related social differences and immaturity (Wood & Gadow, 2010). For this reason, the current intervention and related treatments have focused both on anxiety reduction as well as social skill acquisition. The effects of CBT on ASD symptom severity remain to be confirmed by measurement approaches other than parent report (e.g., school behavioral observations). However, this potentially promising pattern of findings suggests that a difficult area of symptomatology to modify—core ASD symptoms—may be responsive to outpatient CBT for at least some youth.
The modifications made to the BIACA manual for early adolescents with high functioning ASD appeared to be sufficient for achieving some clinical benefit in this sample of youth, though not necessarily for remission of all concurrent mood and anxiety disorders. Our experience with this iteration of the BIACA protocol with adolescents suggests that future treatment development for adolescents with ASD might beneficially include CBT modules that more comprehensively address (1) concurrent depression (e.g., with more than just cognitive restructuring techniques), (2) peer harassment issues and (3) teen-specific developmental issues (e.g., puberty and desire for romantic relationships). Although we did not track these issues systematically during treatment, we noted that in a few youths with concurrent depression, treatment engagement may have been affected by depression-related low positive affectivity and low energy and that the early use of evidence-based techniques for depression could be helpful. Peer harassment and bullying were not universally experienced by this cohort of youth but this was a clinical issue in some cases and exemplifies an objective stressor in need of a solution in order to relieve conditions that are threatening to youth and impair their mental health. A number of the participants experienced romantic interests without developmentally appropriate knowledge of how to conceptualize and address their feelings; equally, several youths experienced anxiety about bodily changes related to puberty. While these issues were addressed using adolescent-oriented adaptations of the extant cognitive restructuring and social skills modules from the original BIACA protocol, a more comprehensive approach to these issues incorporated in a CBT manual for this age-group and older teens is likely indicated.
In spite of the promising findings, this study has several limitations including its modest sample size and the lack of objective measures of anxiety that go beyond diagnostic interview or checklist measures. Another potential limitation in this study is the modest internal consistencies of some of the measures (e.g., PARS), although these are similar to published figures from the general clinical child and adolescent literature (e.g., RUPP, 2002).
In sum, this is the fourth RCT of the BIACA CBT manual for high-functioning youth with ASD and clinical anxiety to show clinical benefit of treatment in comparison to a waitlist or usual care control group (cf. Fujii et al., 2013; Storch et al. 2013; Wood, Drahota, Sze, Har, et al., 2009). The present trial suggests that the manual, with developmentally appropriate alterations of treatment content, can be beneficial for early adolescents, building off earlier treatment development work with preteens. In future studies, a credible active control group, such as an alternative form of psychotherapy, will be needed to determine the specificity of the effects of this intervention.
Supplementary Material
Highlights.
Clinically elevated anxiety is common among adolescents with high functioning autism spectrum disorders.
A CBT program designed for youth with ASD outperformed a 4-month waitlist condition in terms of independent evaluators’ ratings of symptom severity and treatment response.
The CBT program was also associated with relatively greater improvement in parent-rated autism symptom severity at posttreatment, in comparison with waitlist.
This is the first RCT of this CBT treatment manual with the early adolescent age-group, but the fourth RCT with children with ASD overall, to offer support for the CBT intervention under investigation, suggesting that a comparison to an active treatment condition is a logical next step in evaluating the intervention program.
Acknowledgements
This study was supported by a multisite grant awarded to Jeffrey J. Wood, Eric Storch, and Jill Ehrenreich from the National Institute of Child Health and Human Development (HD65270). We are very grateful to the participating families. We also acknowledge the contributions of Lindsay Brauer, P. Jane Mutch, Josh Nadeau, Amy Parks (University of South Florida), Michael Hernandez, Carly Schwartzman and Ilana Seager (University of Miami), and C. Enjey Lin and Kelly Decker (UCLA).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Attwood T. Asperger's syndrome: A guide for parents and professionals. Philadelphia: Jessica Kingsley; 1998. [Google Scholar]
- Barkley RA, Anastopoulos AD, Guevremont DC, Fletcher KE. Adolescents with ADHD: Patterns of behavioral adjustment, academic functioning, and treatment utilization. Journal of the American Academy of Child & Adolescent Psychiatry. 1991;30:752–761. doi: 10.1016/s0890-8567(10)80010-3. [DOI] [PubMed] [Google Scholar]
- Barnard J, Rubin DB. Small-sample degrees of freedom with multiple imputation. Biometrika. 1999;86:948–955. [Google Scholar]
- Bellini S. Social skill deficits and anxiety in high-functioning adolescents with autism spectrum disorder. Focus on Autism and Other Developmental Disabilities. 2004;19:78–86. [Google Scholar]
- Booth A, Granger DA, Mazur A, Kivlighan KT. Testosterone and social behavior. Social Forces. 2006;85:167–191. [Google Scholar]
- Cameron C. Kurtosis. In: Lewis-Beck MS, Bryman A, Liao TF, editors. The Sage encyclopedia of social science research methods. Thousand Oaks, CA: Sage; 2004. [Google Scholar]
- Chalfant A, Rapee R, Carroll L. Treating anxiety disorders in children with high-functioning autism spectrum disorders: A controlled trial. Journal of Autism and Developmental Disorders. 2006;33:283–298. doi: 10.1007/s10803-006-0318-4. [DOI] [PubMed] [Google Scholar]
- Chang Y, Quan J, Wood JJ. Effects of anxiety disorder severity on social functioning in children with autism spectrum disorders. Journal of Developmental and Physical Disabilities. 2012;24:235–245. [Google Scholar]
- Chorpita BF, Yim LM, Moffitt CE, Umemoto LA, Francis SE. Assessment of symptoms of DSM-IV anxiety and depression in children: A Revised Child Anxiety and Depression Scale. Behaviour Research and Therapy. 2000;38:835–855. doi: 10.1016/s0005-7967(99)00130-8. [DOI] [PubMed] [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. Hillsdale, NJ: Lawrence Erlbaum Associates; 1988. [Google Scholar]
- Compas BE, Ey S, Grant KE. Taxonomy, assessment, and diagnosis of depression during adolescence. Psychological Bulletin. 1993;114:323–344. doi: 10.1037/0033-2909.114.2.323. [DOI] [PubMed] [Google Scholar]
- Constantino JN. The Social Responsiveness Scale. Los Angeles: Western Psychological Services; 2002. [Google Scholar]
- Cooper H, Hedges LV, Valentine JC. The handbook of research synthesis and meta-analysis. 2nd ed. New York, NY US: Russell Sage Foundation; 2009. [Google Scholar]
- Dawson G, Rogers S, Munson J, Smith M, Winter J, Greenson J, Donaldson A, Varley J. Randomized, controlled trial of an intervention for toddlers with autism: The Early Start Denver Model. Pediatrics. 2010;125:e17–e23. doi: 10.1542/peds.2009-0958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Bruin EI, Ferdinand RF, Meesters S, de Nijs PFA, Verheij F. High rates of psychiatric co-morbidity in PDD-NOS. Journal for Autism and Developmental Disorders. 2007;37:877–886. doi: 10.1007/s10803-006-0215-x. [DOI] [PubMed] [Google Scholar]
- Drahota A, Wood JJ, Sze KM, Van Dyke M. Effects of cognitive behavioral therapy on daily living skills in children with high-functioning autism and concurrent anxiety disorders. Journal of Autism and Developmental Disorders. 2011;41:257–265. doi: 10.1007/s10803-010-1037-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eaves LC, Ho HH. Young adult outcome of autism spectrum disorders. Journal of autism and developmental disorders. 2008;38:739–747. doi: 10.1007/s10803-007-0441-x. [DOI] [PubMed] [Google Scholar]
- Fujii C, Renno P, McLeod BD, Lin CE, Decker K, Zielinski K, Wood JJ. Intensive cognitive behavioral therapy for anxiety disorders in school-aged children with autism: A preliminary comparison with treatment-as-usual. School Mental Health. 2013;5:25–37. [Google Scholar]
- Gadow KD, DeVincent CJ, Schneider J. Comparative study of children with ADHD only, autism spectrum disorder + ADHD, and chronic multiple tick disorder + ADHD. Journal of Attention Disorders. 2009;12:474–485. doi: 10.1177/1087054708320404. [DOI] [PubMed] [Google Scholar]
- Garland AF, Saltzman MD, Aarons GA. Adolescent satisfaction with mental health services: Development of a multidimensional scale. Evaluation and Program Planning. 2000;23:165–175. [Google Scholar]
- Ghaziuddin M, Greden J. Depression in children with autism/pervasive developmental disorders: A case-control family history study. Journal of Autism and Developmental Disorders. 1998;28:111–115. doi: 10.1023/a:1026036514719. doi:0162-3257/98/0400-0111. [DOI] [PubMed] [Google Scholar]
- Green J, Gilchrist A, Burton D, Cox A. Social and psychiatric functioning in adolescents with Asperger syndrome compared with conduct disorder. Journal of Autism and Developmental Disorders. 2000;30:279–293. doi: 10.1023/a:1005523232106. [DOI] [PubMed] [Google Scholar]
- Guy W. Revised. NIMH publication DHEW publNO (Adm) 76-338. Bethesda MD: National Institute of Mental Health; 1976. Early Clinical Drug Evaluation Unit (ECDEU) assessment manual for psychopharmacology; pp. 217–222. [Google Scholar]
- Hedges LV, Olkin I. Statistical methods for meta-analysis. New York, NY: Academic Press; 1985. [Google Scholar]
- Horwitz SM, Hoagwood K, Stiffman AR, Summerfeld T, Weisz JR, Costello EJ, Norquist G. Reliability of the services assessment for children and adolescents. Psychiatric Services. 2001;52:1088–1094. doi: 10.1176/appi.ps.52.8.1088. [DOI] [PubMed] [Google Scholar]
- Kasari C. Assessing change in early intervention programs for children with autism. Journal of Autism and Developmental Disorders. 2002;32:447–461. doi: 10.1023/a:1020546006971. doi:0162-3257/02/1000-0447/0. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Avenevoli S, Merikangas KR. Mood disorders in children and adolescents: An epidemiologic perspective. Biological Psychiatry. 2001;49:1002–1014. doi: 10.1016/s0006-3223(01)01129-5. [DOI] [PubMed] [Google Scholar]
- Kuusikko S, Pollock-Wurman R, Jussila K, Carter AS, Mattila M, Ebeling H, Pauls DL, Moilanen I. Social anxiety in high-functioning children and adolescents with autism and Asperger syndrome. Journal of Autism and Developmental Disorders. 2008;38:1697–1709. doi: 10.1007/s10803-008-0555-9. [DOI] [PubMed] [Google Scholar]
- Lecavalier L, Wood JJ, Halladay AK, Jones NE, Aman MG, Cook EH, Handen BL, King BH, Pearson DA, Hallett V, Sullivan KA, Grondhuis S, Bishop SL, Horrigan JP, Dawson G, Scahill L. Measuring anxiety as a treatment endpoint in youth with autism spectrum disorder. Journal of Autism and Developmental Disorders. 2013 doi: 10.1007/s10803-013-1974-9. Advance online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Le Couteur A, Lord C, Rutter M. The Autism Diagnostic Interview-Revised. Los Angeles: Western Psychological Services; 2003. [Google Scholar]
- Lord C, Rutter M, DiLavore PC, Risi S. Autism Diagnostic Observation Schedule. Los Angeles: Western Psychological Services; 2002. [Google Scholar]
- March JS. Multidimensional anxiety scale for children. North Tonawanda, NY: Multi-Health Systems; 1998. [Google Scholar]
- McGovern CW, Sigman M. Continuity and change from early childhood to adolescence in autism. Journal of Child Psychology and Psychiatry. 2005;46:401–408. doi: 10.1111/j.1469-7610.2004.00361.x. [DOI] [PubMed] [Google Scholar]
- Mundy PC, Henderson HA, Inge AP, Coman DC. The modifier model of autism and social development in higher functioning children. Research and Practice for Persons with Severe Disabilities. 2007;32:1–16. doi: 10.2511/rpsd.32.2.124. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2773555/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearson DA, Loveland KA, Lachar D, Lane DM, Reddoch SL, Mansour R, Cleveland LA. A comparison of behavioral and emotional functioning in children and adolescents with autistic disorder and PDD-NOS. Child Neuropsychology. 2006;12:321–333. doi: 10.1080/09297040600646847. [DOI] [PubMed] [Google Scholar]
- Reaven J, Blakeley-Smith A, Culhane-Shelburne K, Hepburn S. Group cognitive behavior therapy for children with high-functioning autism spectrum disorders and anxiety: A randomized trial. Journal of Child Psychology and Psychology. 2012;53:410–419. doi: 10.1111/j.1469-7610.2011.02486.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Renno P, Wood JJ. Discriminant and convergent validity of the anxiety construct in children with autism spectrum disorders. Journal of Autism and Developmental Disorders. 2013;43:2135–2146. doi: 10.1007/s10803-013-1767-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Research Units on Pediatric Psychopharmacology (RUPP) Autism Network. The Pediatric Anxiety Rating Scale (PARS): development and psychometric properties. Journal of the American Academy of Child and Adolescent Psychiatry. 2002;41:1061–1069. doi: 10.1097/00004583-200209000-00006. [DOI] [PubMed] [Google Scholar]
- Rinck M, Rortgen T, Lange W, Dotsch R, Wigboldus D, Becker E. Social anxiety predicts avoidance behaviour in virtual encounters. Cognition and Emotion. 2010;24:1269–1276. [Google Scholar]
- Shtayermman O. Peer victimization in adolescents and young adults diagnosed with Asperger's Syndrome: A link to depressive symptomatology, anxiety symptomatology and suicidal ideation. Issues in Comprehensive Pediatric Nursing. 2007;30:87–107. doi: 10.1080/01460860701525089. [DOI] [PubMed] [Google Scholar]
- Silverman WK, Albano AM. The Anxiety Disorders Interview Schedule for DSM-IV—Child and Parent Versions. San Antonio, TX: Graywind; 1996. [Google Scholar]
- Sofronoff K, Attwood T, Hinton S. A randomized controlled trial of a CBT intervention for anxiety in children with Asperger syndrome. Journal of Child Psychology and Psychiatry. 2005;46:1152–1160. doi: 10.1111/j.1469-7610.2005.00411.x. [DOI] [PubMed] [Google Scholar]
- Spiker MA, Lin CE, Van Dyke M, Wood JJ. Restricted interests and anxiety in children with autism. Autism. 2012;16:306–320. doi: 10.1177/1362361311401763. [DOI] [PubMed] [Google Scholar]
- Storch EA, Arnold EB, Lewin AB, Nadeau J, Jones AM, De Nadai AS, Mutch PJ, Selles RR, Ung D, Murphy TK. The effect of cognitive-behavioral therapy versus treatment as usual for anxiety in children with autism spectrum disorders: A randomized, controlled trial. Journal of the American Academy of Child & Adolescent Psychiatry. 2013;52:132–142. doi: 10.1016/j.jaac.2012.11.007. [DOI] [PubMed] [Google Scholar]
- Storch EA, Ehrenreich-May J, Wood JJ, Jones AM, De Nadai AS, Lewin AB, Arnold EB, Murphy TK. Multiple informant agreement on the anxiety disorders interview schedule in youth with autism spectrum disorders. Journal of Child and Adolescent Psychopharmacology. 2012;22:292–299. doi: 10.1089/cap.2011.0114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Storch EA, Lewin AB, De Nadai AS, Murphy TK. Defining treatment response and remission in obsessive-compulsive disorder: A signal detection analysis of the Children's Yale-Brown Obsessive-Compulsive Scale. Journal of the American Academy of Child and Adolescent Psychiatry. 2010;49:708–717. doi: 10.1016/j.jaac.2010.04.005. [DOI] [PubMed] [Google Scholar]
- Storch EA, Wood JJ, Ehrenreich-May J, Jones AM, Park JM, Lewin AB, Murphy TK. Convergent and discriminant validity and reliability of the pediatric anxiety rating scale in youth with autism spectrum disorders. Journal of Autism and Developmental Disorders. 2012;42:2374–2382. doi: 10.1007/s10803-012-1489-9. [DOI] [PubMed] [Google Scholar]
- Sung M, Ooi YP, Goh TJ, Pathy P, Fung DSS, Ang RP, Chua A, Lam CM. Effects of cognitive-behavioral therapy on anxiety in children with autism spectrum disorders: A randomized controlled trial. Child Psychiatry & Human Development. 2011;42:634–649. doi: 10.1007/s10578-011-0238-1. [DOI] [PubMed] [Google Scholar]
- Susman EJ, Inoff-Germain G, Nottelmann ED, Loriaux DL, Cutler GB, Jr, Chrousos GP. Hormones, emotional dispositions, and aggressive attributes in young adolescents. Child Development. 1987;58:1114–1134. http://www.jstor.org/stable/1130551. [PubMed] [Google Scholar]
- Sze KM, Wood JJ. Cognitive behavioral treatment of comorbid anxiety disorders and social difficulties in children with high-functioning autism: A case report. Journal of Contemporary Psychotherapy. 2007;37:133–143. [Google Scholar]
- Tremblay RE. Testosterone, physical aggression, dominance, and physical development in early adolescence. International Journal of Behavioral Development. 1998;22:753–777. [Google Scholar]
- Wechsler D. Wechsler Intelligence Scale for Children–Fourth Edition. San Antonio, TX: The Psychological Corporation; 2003. [Google Scholar]
- White SW, Ollendick T, Albano AM, Oswald D, Johnson C, Southam-Gerow MA, Kim I, Scahill L. Randomized controlled trial: Multimodal anxiety and social skill intervention for adolescents with autism spectrum disorder. Journal of Autism and Developmental Disorders. 2013;43:382–394. doi: 10.1007/s10803-012-1577-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williamson S, Craig J, Slinger R. Exploring the relationship between measures of self-esteem and psychological adjustment among adolescents with Asperger syndrome. Autism. 2008;12:391–402. doi: 10.1177/1362361308091652. [DOI] [PubMed] [Google Scholar]
- Wood JJ, Drahota A, Sze K, Har K, Chiu A, Langer DA. Cognitive behavioral therapy for anxiety in children with autism spectrum disorders: a randomized, controlled trial. Journal of Child Psychology & Psychiatry. 2009;50:224–234. doi: 10.1111/j.1469-7610.2008.01948.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wood JJ, Drahota A, Sze K, Van Dyke M, Decker K, Fujii C, Bahng C, Renno P, Hwang W, Spiker M. Brief report: Effects of cognitive behavioral therapy on parent-reported autism symptoms in school-age children with high-functioning autism. Journal of Autism and Developmental Disorders. 2009;39:1608–1612. doi: 10.1007/s10803-009-0791-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wood JJ, Gadow KD. Exploring the nature and function of anxiety in youth with autism spectrum disorders. Clinical Psychology: Research and Practice. 2010;17:281–292. [Google Scholar]
- Wood JJ, Schwartzman B. Cognitive behaviour therapies for youth with autism spectrum disorders. In: Graham P, Reynolds S, editors. Cognitive behaviour therapy for children and families: third edition. Cambridge: Cambridge University Press; 2013. [Google Scholar]
- Zahn-Waxler C, Shirtcliff EA, Marceau K. Disorders of childhood and adolescence: Gender and psychopathology. Annual Review of Clinical Psychology. 2008;4:275–303. doi: 10.1146/annurev.clinpsy.3.022806.091358. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.