ABSTRACT
Introduction:
Preoperative kidney tumor embolization is standard procedure for therapy in advanced kidney cancer. Preoperative embolization has a goal to reduce intraoperative bleeding and also to shorten the time of surgery.
Materials and methods:
We retrospectively observed 50 patients between 2000-2011, in which the preoperative embolization was performed. Mean age of patients was 64 years. All patients with preoperative embolization were compared with the group of 51 patients from Urology Sarajevo, who underwent nephrectomy without preoperative embolization.
Results:
Symptoms that are dominating among patients were haematuria and pain. Analysis of mean size of tumors based on CT evaluation showed statistically significance in between the biggest size of tumors in group from Hamburg (9.11±3cm) and the smallest size of tumors in Sarajevo group (4.94±1.6cm) p=0.0001. Reason for this is difference in selection of patients for treatment in Hamburg from Sarajevo.
Conclusion
Kidney as functional finishing organ is extremely suitable for transcatheter therapeutic procedures. The gold standard in the treatment of advanced and metastatic tumor is the nephrectomy. As preparation for nephrectomy in metastatic cancer total capillary embolization is performed. After embolization, surgery is shorter, procedure can be done 24-48 hours after embolization or delayed nephrectomy done 2-3 weeks after the intervention.
Keywords: kidney, preoperative tumor embolization
1. INTRODUCTION
Kidney cancer is the most common kidney tumor and the third one by the frequency in urology. Comparing to other malignancy, 2% of all tumors is the kidney cancer (1). In end stage kidney cancer therapy of choice is radically nephrectomy, which means and adrenalectomy with removing fat kidney capsule and proximal urethra.
Kidney tumor embolization is the standard procedure in therapy of kidney cancer, due to embolization whole kidney or its parts should be exclude from the function. First experimental embolization was performed by lang in 1971 (2). He used radioactive particles to induce tumor necrosis. On humans, first embolization was performed in 1973, by Almagard (3). From that time the technique has been changed a lot, also diagnostic procedures for detecting the tumors were fulfilled with CT and MRI. In the same time the new operative techniques were introduced laparoscopic nephrectomy, organoprotective resection and extracorporal Work-Bench procedures.
Preoperative tumor embolization is performed in patients with:
Advanced stage of tumor
Tumor rich in retroperitoneal collateralize
Infiltration of venous system
Tumor in close range of kidney hillus
Metastatic tumors and
Patients who are not treatable to become treatable.
Preoperative embolization has the goal to reduce intraoperative bleeding and to reduce the time of surgical procedure, by making preparation of tumor easier. This is particularly important for T3 and T4 tumors, with infiltration of renal vein and vena cava inferior.
2. MATERIALS AND METHODS
We retrospectively observed 50 patients between 2000-2011, in which the preoperative embolization was performed. The majority of patients were treated in Eilbek Clinic in Hamburg and few in Clinical Center Sarajevo. Mean age of patients was 64 years, range between 3 and 86 years. 19 patients were female and 31 patients were male. Patients that were enrolled on study were the patients with the tumor larger than 8cm on the upper pole of left kidney, and patients wit proven bilateral kidney tumor.
Patients that were excluded from study were the patients with tumor smaller than 8cm, if the tumor was good for surgical procedure. Embolised patient were compared with the group of 51 patients from Urology Clinic Sarajevo, which were performed surgical nephrectomy without embolization. This group has been concised from 19 female and 32 male. Mean age was 61 years, range between 32 and 80 years. The total number of patients was 101. Patients were diagnosed with CT or MRI, as outpatients and small amount of patients we diagnosed in our Institution (CT siemens Somatom duo and MRI Unit 1.5T Symphonie).
Conventional angiography was performed on Siemens Polystar, 2 frames/sec. Angiography was performed by Seldinger technique, with contrast agent Xenetix 300. Angiography was performed to determine the blood supply of tumors in attacked kidney; we performed first aortography followed by selective angiography of renal arteries. Once done selective angiography, we approached embolization. Embolization is done first on the capillary level. As embolization material at the capillary level in the course of the study we used alcohol or Ivalon 150-250 μ particles. Alcohol is the cheapest and most efficient means of embolization. The disadvantage is that alcohol is the only means of embolization during one embolization must be applied in a blocked blood vessel in order to prevent reflux. We used 96% alcohol. In some patients inhibit the supply vessel is impossible, and then we performed a combined embolization with alcohol and Ivalon or just Ivalon particle embolization. The advantage in using Ivalon that supply blood vessel may not be blocked. Upon completion of the capillary embolization, we performed control angiography, and if the tumor / kidney is embolised we performed the central embolization of supply vessel with metal spirals. In the course of the study, Tornado spirals (COOK) were used. After that is done aortography to confirm complete embolization and showed situation surrounding blood vessels that were not aimed by embolization.
Besides angiographies findings, we were processed operating protocols and protocols of anesthesia. To test the existence of the correlation between the groups for each parameter was used Pearson correlation test. In all tests of statistical significance was considered at p <0.05 or at the level of 95%. All data were analyzed using statistical software SPSS version 13.0 for Windows, while the resulting tables and graphs subsequently processed using Microsoft Word 2003.
3. RESULTS
Symptomatology that led the patient's physician is shown in Figure 1 and 2. A small number of patients reported the loss of body weight, 11 patients from the Hamburg group (H) and 7 patients in the Sarajevo group (S). Infiltration of the kidney hollow system has been registered with 5 (H) patients and in 7 (S) patients. Infiltration of veins, tumor thrombus was found in a total of 16 patients (10 H and 6 S) and the infiltration of adjacent organs was found in 15 patients (8 H 7 and S). AV-shunt was diagnosed in only one patient at Hamburg group. Analysis of the average size of the tumor based on CT findings showed a statistically significant difference in terms of the maximum average size of tumors in patients from Hamburg (9.11 ± 3 cm) and minimum size in patients in Sarajevo (4.94 ± 1.6 cm), p = 0.0001. The reason for this is in the selection of patients in Hamburg preoperative group compared to Sarajevo operative group. The presence of metastases in regional lymph nodes showed statistically significant differences between groups p = 0.030. It is evident that the invasion of local lymph nodes at least recorded in patients in Sarajevo (7.8%), and patients from Hamburg (22%). Distant metastases were found in 4 (H) and in 2 (S) patients.
Figure 1.
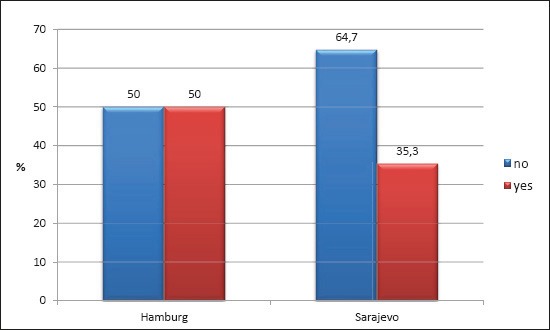
Number cases of Haematuria in our sample
Figure 2.
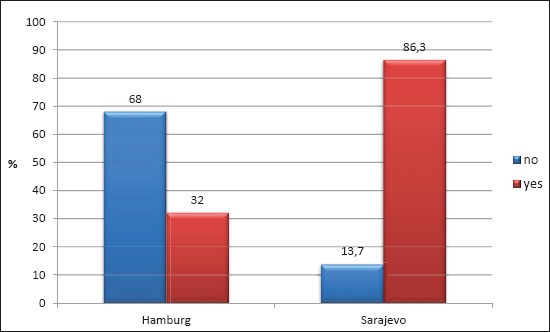
Presence of pain in our patients
Embolization was repeated in two patients. Patohistological classification is shown in Figure 3.
Figure 3.
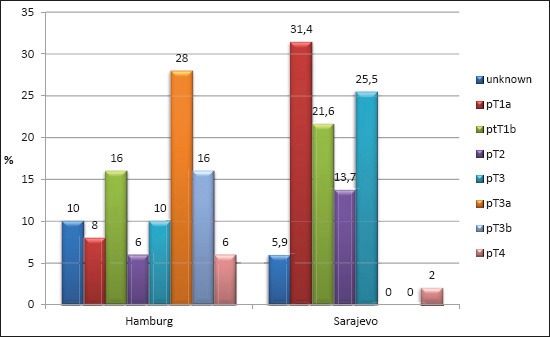
Pathohistological classifi cation
The most common t stage was pT3a with 28% (H) and pT1a (S), and the least represented pT4 and pT2 with 6% in the Hamburg group and pT4 in Sarajevo group with 2%.
Histological determination of tumor size confirms previous statement on CT tumor size that the same was higher in patients from Hamburg (8.2 ± 3.4 cm), compared to patients in Sarajevo (3.89 ± 1.5 cm). Analysis of variance also showed statistically significant differences p = 0.0001 in favor of more specific histopatological tumor size in patients from Hamburg.
The average length of surgery was very similar and it was 105.6 ± 23 minutes in patients from Hamburg, and 101.4 ± 38 minutes in patients in Sarajevo. Minimum duration of the procedure was recorded in Sarajevo on 45 minutes, which was recorded as well as the maximum duration of treatment of 195 minutes. There were no statistically significant differences. The Hamburg group's surgery was done on average 23 days after embolization. Blood transfusion during and after surgery are shown in Table 1. With statistical significance, the difference can be seen that the operations carried out in Sarajevo was used more units of blood during the same. Figure 4 presents the case of preoperative embolization, which was done in so called sandwich-technique alcohol mixed with lipiodol and Ivalon particle. Central occlusion was performed with Tornado spirals.
Table 1.
Blood transfusion intra-post op. χ2=5,492, p=0,040
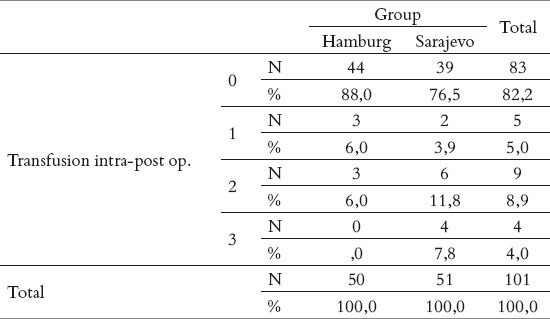
Figure 4.
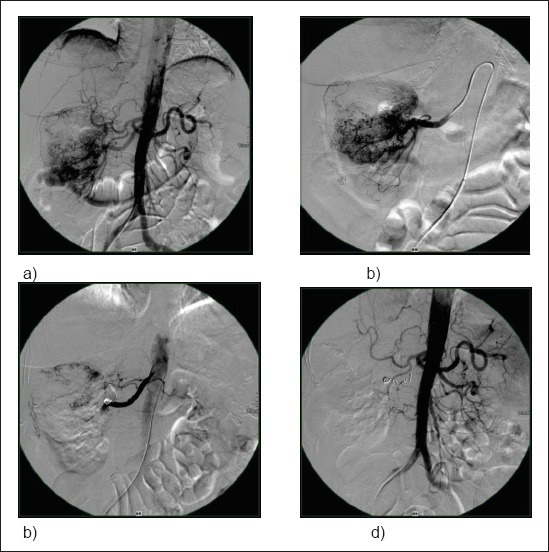
a), b) present angiographic findings of kidney tumor; c) and d) present angiographic findings after embolisation.
4. DISCUSSION
Treatment of choice for kidney cancer is surgical resection. In early stage of TU and with favorable localization is sufficient to perform enucleation or partially nephrectomy, and in advanced disease should be done radical nephrectomy (4).
By age, group of our patients who were preoperatively embolised, was very heterogeneous. We performed one embolization of Wilms tumor. Wilms tumor occurs at the age of 2-4 years. After 10 years of appearing less frequently (5, 6, 7). In addition to Wilms tumor in children is possible occurrence of renal cancer. Incidence of 3- 6% (8).
Reasons for blood loss during nephrectomy are: hypervascularisation of tumor, atypical blood vessels (9) and hilar lymph nodes that hamper visibility of blood vessels (10).
For decisive loss of blood atypical blood vessels are the main reason, which are often fulfilled with the blood. In violation of these vascular structures, Intraoperative bleeding is abundant because these vessels are less contractile. Another disadvantage is that these blood vessels are retroperitoneal positioned which makes preparation of large tumors very difficulty. With preoperative embolization, we have to occlude not only renal artery and capillary circulation, but must be able to occlude all atypical arteries to reduce blood loss to a minimum.
Craven study (11) showed minimal blood loss in delayed nephrectomy after embolization even with advanced stages of cancer with vascularized thrombus in the inferior vena cava. Delayed nephrectomy stimulates tumor regression as well as venous thrombosis, which significantly facilitates op procedure. In our group's average delay was 23 days. Some authors recommend a delay of less than 48 hours between embolization and surgery because postinfarctus syndromes do not develop fully (12). The same authors as Lanigian et al. (13) suggest that a longer interval between embolization and surgery lead to the development of collateral that hamper preparation. These data from the literature do not agree with our experience. In most of our patients, we performed delayed nephrectomy. In these patients, there was no collateral development in the periphery.
Our first embolization we performed only with the alcohol, in 96%. Alcohol is very potent and very cheap embolisaton material. If it is used in combination with distal balloon occlusion, the rate of complications such as migration is very low. Alcohol is very powerful embolization material, and destruction of capillary system is very powerful, better than any other embolization material. Destruction of capillary system lead to tumor necrosis. Tölle and Cramer (14) performed 20 embolisations with very low rate of the complications. Those authors claim that alcohol is very safe to use, and percent of recanalization is almost zero. We also performed majority of our embolisations with same techniques. The volume of alcohol that we used was determined for every patient individually. After balloon occlusion, angiography was performed. The volume of contrast material that was necessary for demarcation of whole kidney is the volume of alcohol that we used. Occlusion was performed 40 minutes after alcohol injection. In our study the rate of complication was zero. With lack of occlusion catheters we abandoned this technique. Some authors reported severe complications after alcohol embolization. Laarmann at all. (15) reported two cases of testicular damage, as reason of anatomical variation where art. testiculariswas the branch of renal artery. Same group of authors (16) performed alcohol embolization in 44 patients with no distal balloon occlusion. The volume of alcohol that was used was 14-22ml. Timmerman (17) performed capillary embolization in combination of alcohol and Etiblock.
Several publications confirmed severe complications after alcohol embolization, so the use of alcohol was diminished and Etiblock was introduced as main embolization material. Initial results with Etiblock determined vasospasm after its use, so results were incomplete embolization. After another embolization materials were introduced, such as Ivalon 150-250 microns. Ivalon embolization does not need use of occlusion balloons, and application is very simple over microcatheter. Ivalon also has very good X ray visibility. In our series we had two case of recanalization after Ivalon embolization, so embolization had to be repeated. After this we started with so called sandwich embolization technique alcohol and Ivalon particles 150-250 microns. Central embolization was performed with Tornado colils. We had no complication with these technique.
With preoperative embolization there is significant reduce of blood transfusion during surgery, comparing to patients with no embolization (20, 21). Volume of blood in group of embolised patients was around 250ml, and in group of non embolised patients was around 800ml.
Zielinski et al. (22) in their work compare rate of surveillance of five and ten years between group of 118 patients that were embolised and group of 116 patients with no embolization prior to surgery. The both groups had same demographics. Five and ten year's surveillance was statistically significant in first group 62%, and in the second group 35%.
Kauffmann (23) in his work showed reduction of blood loss during surgery in the group of patients preoperatively embolised. Vogel et al. (24) published the same results as Kauffmann with loss of blood of 600ml in patients that were preoperatively embolised. Embolization was performed with 2-6ml Histoacril mixed with 50 % Lipiodol. Danish group of authors with Christensen (26) published that they had smaller loss of blood during surgery in group of patients who were embolised prior to surgery, and the time of surgery was shorter, comparing with the group of patients with no embolization prior to surgery. Embolization was performed only with coils. The surgery was performed five days after embolization. Surveillance rate of embolised patients was better than in patients with no embolization.
Stösslein (27) at all. published that blood volume loss during surgery was in average 300ml. They had 92 patients. There were no significant shortening it time of surgery between two groups of patients. Surveillance rate was much higher in group of patient with embolization than in another group.
Latal at all (28) published that there were no statistically significance in surveillance rate between patients who were embolised prior to surgery comparing with patients who had only surgical nephrectomy.
5. CONCLUSION
Kidney cancer is the rare tumor considering other malignancies. Kidney as the organ is very suitable for all transcatheter procedures as for percutaneous procedures. The gold standard for treatment of kidney cancer in advanced stage is surgical procedure with nephrectomy, and for small tumor is enucleation of tumor. Full capillary embolization is method of choice to prepare surgical nephrectomy. The most potent embolization material is alcohol, but its is the most dangerous one. Because of that, alcohol should be administered over the occlusion or in small portions with conjunction of Lipiodol to be visible. The goal of this embolization is to make surgical procedure easier, thru less bleeding during the surgical procedure. On other goal is to make surgery less time consuming. The surgery can be made 24-48 h after the embolization, or it can be made as late nephrectomy after 2-3 weeks. Some percent of patients who were inoperable before the embolization, become operative after the procedure. It is a fact that the cost of treatment of those patients are bigger than with patients who are treated only with the surgery.
Footnotes
CONFLICT OF INTEREST: NONE DECLARED.
REFERENCES
- 1.Holzheimer S, Becker N. Heidelberg: Springer-Verlag 3, Auflage; 1998. Krebsatlas. [Google Scholar]
- 2.Lang EK. Superselective arterial catheterization as a vehicle for delivering radioactive infarct particles to tumors. Radiology. 1971;98:391–399. doi: 10.1148/98.2.391. [DOI] [PubMed] [Google Scholar]
- 3.Almgard LE, Fernstrom I, Haverling M, et al. Treatment of renal adenocarcinoma by embolic occlusion of the renal circulation. Br J Urol. 1973;45:474–479. doi: 10.1111/j.1464-410x.1973.tb06806.x. [DOI] [PubMed] [Google Scholar]
- 4.Hansmann HJ, Hallscheidt P, Aretz K, et al. Nierentumoremboisation. Radiologe. 1999;39:783–789. doi: 10.1007/s001170050576. [DOI] [PubMed] [Google Scholar]
- 5.Asanuma H, Nakai H, Takeda M, et al. Renal cell carcinoma in children: experience at a single institution in Japan. J Urol. 1999;162:1402–1405. [PubMed] [Google Scholar]
- 6.Freedman AL, Vates TS, Stewart T, et al. Renal cell carcinoma in children: the Detroit experience. J Urol. 1996;155:1708–1710. [PubMed] [Google Scholar]
- 7.Hawers W, Goeppel M, Rübben H. Nephroblastom. In: Rübben H, editor. (Hrsg) Uroonkologie. Vol. 5. Springer; 2001. pp. 568–587. [Google Scholar]
- 8.Ebert A, Gravou C, Stümpfl M, et al. Das Nierenzellkarzinom im Kindesalter. Urologe A. 2003;42:263–268. doi: 10.1007/s00120-002-0212-4. [DOI] [PubMed] [Google Scholar]
- 9.Giuliani L, Carmignani G, Belgrano E, et al. Usefulness of preopertive transcatheter embolisaton in kidney tumors. Urology. 1981;17:431–434. doi: 10.1016/0090-4295(81)90182-5. [DOI] [PubMed] [Google Scholar]
- 10.Singsaas MW, Choop RT, Mendez R. Preopertive renal embolization as adjunct to radical Nephrectomy. Urology. 1979;146:704–708. doi: 10.1016/0090-4295(79)90200-0. [DOI] [PubMed] [Google Scholar]
- 11.Craven WM, Redmond Pl, Kumpe DA, et al. Planned delayed nephrectomy after ethanol embolization of renal carcinoma. J Urol. 1991;146:704–708. doi: 10.1016/s0022-5347(17)37899-0. [DOI] [PubMed] [Google Scholar]
- 12.Kalman D, Varenhorst E. The role of arterial embolization in renal cell carcinoma. Scand J Urol Nephrol. 1999;33:162–170. doi: 10.1080/003655999750015934. [DOI] [PubMed] [Google Scholar]
- 13.Lanigan D, Jurrians E, Hammonds JC, et al. The current status of embolization in renal cell carcinoma - a survey of local and national practice. Clin Radiol. 1992;46:176–178. doi: 10.1016/s0009-9260(05)80440-4. [DOI] [PubMed] [Google Scholar]
- 14.Tölle E, Cramer BM. Klinische Erfahrungen mit der arteriellen Embolization von Nierentumoren mit Äthanol. Urologe A. 1983;22:208–212. [PubMed] [Google Scholar]
- 15.Laarmann S, Straube W, Timmermann J. Alkoholtoxische Gonadenschädigung durch Alkoholembolisation bei Nierenmalignomen. Urologe A. 1987;26:94–95. [PubMed] [Google Scholar]
- 16.Timmermann J, Schlake W, Straube W, et al. Der absolute Alkohol, ein steuerbares Embolisationsmaterial bei Nierentumoren. Urologe A. 1984;23:275–277. [PubMed] [Google Scholar]
- 17.Timmermann J, Straube W, Schlake W. Klinische Beobachtungen bei dem Gefäßverschluß des Nierentumors durch absoluten Alkohol. Urologe A. 1985;24:260–263. [PubMed] [Google Scholar]
- 18.Boeminghaus F, Greipel V, Schwartmann KP. Analyse der Langzeitergebnisse nach Nephrektomie wegen Hypernephrom anhand 442 Fällen. Urologie A. 1982;21:201–204. [PubMed] [Google Scholar]
- 19.Lanigan D, Jurriaans E, Hammond’s JC, et al. The current status of embolization in renal cell carcinoma-a survey of local and national practice. Clinical Radiology. 1992;46:176–178. doi: 10.1016/s0009-9260(05)80440-4. [DOI] [PubMed] [Google Scholar]
- 20.Bakal CW, Cynamon J, Lakritz PS, et al. Value of preoperative renal artery embolization in Reducing blood transfusion requirements during nephrectomy for renal cell carcinoma. J Vasc Interv Radiol. 1993;4:727–731. doi: 10.1016/s1051-0443(93)71958-2. [DOI] [PubMed] [Google Scholar]
- 21.Staehler G, Dhremer I, Pomer S. Tumorbefall der Vena cava beim Nierenzellkarzinom. Operationstechnik, Ergebnisse und Prognose. Urologe A. 1994;33:116–121. [PubMed] [Google Scholar]
- 22.Zielinski H, Szmigelski S, Petrovich Z. Comparison of preoperative embolization followed by radical nephrectomy with radical neprectomy alone for renal cell carcinoma. Am J Clin Oncol. 2000;23(1):6–12. doi: 10.1097/00000421-200002000-00002. [DOI] [PubMed] [Google Scholar]
- 23.Kauffmann GW, Richter GM. Palliative capillary embolization renal carcinoma. Ann Radiol. 1986;29:205–207. [PubMed] [Google Scholar]
- 24.Vogel J, Görich Jv, Ahlen H, et al. Ergebnisse nach Katheterembolization bei Nierenzellkarzinom. Akt Radiol. 1995;5:301–304. [PubMed] [Google Scholar]
- 25.Kauffmann GW, Richter GM, Rohrbach R, et al. Prolonged survival following palliative renal tumor embolization by capillary occlusion. Cardiovas Interv Radiol. 1989;12:22–28. doi: 10.1007/BF02577121. [DOI] [PubMed] [Google Scholar]
- 26.Christensen K, Dyreborg U, Andersen JF, et al. The value of transvascular embolization in the treatment of renal carcinoma. J Urol. 1985;133(2):191–193. doi: 10.1016/s0022-5347(17)48877-x. [DOI] [PubMed] [Google Scholar]
- 27.Stösslein F, Schwenke A, Münster W, et al. Verbesserung der Prognose des Nierenzellkarzinoms durch perkutane transvasale Embolization. Z Urol Nephrol. 1987;80:577–586. [PubMed] [Google Scholar]
- 28.Latal D, Kautzky W, Wanek R, et al. Einfluß der Nierenocclusion auf die Überlebensrate beim Nierenzellkarzinom: Eine retrospektive 10-Jahres-Studie. Z Urol Nephrol. 1990;83:27–31. [PubMed] [Google Scholar]
- 29.Karwowski A, Wojtowicz J. Long-term results of embolization in renal tumors. Radiol Diagn. 1987;28(4):533–535. [PubMed] [Google Scholar]
- 30.Schwartz MJ, Smith EB, Trost DW. Renal artery embolization: clnical indication and experience from over 100 cases. BJU. 2006;99:881–886. doi: 10.1111/j.1464-410X.2006.06653.x. [DOI] [PubMed] [Google Scholar]


