Abstract
College is a time of increased risk for problematic alcohol use and depressed mood. The comorbidity of these conditions is well documented, but is less well understood, with few interventions designed to prevent or reduce the related consequences. The current study evaluated a web-based personalized intervention for students (N=311) who reported an AUDIT score of 8 or more, a BDI-II score of 14 or more, and reported drinking four (women) or five (men) or more drinks on at least one occasion in the past month. Method: Invited participants were randomly selected from all enrolled undergraduates at a large, public, Pacific Northwestern university. Participants completed a screening and baseline assessment, and those who met study eligibility criteria were randomized to one of four conditions (alcohol only, depressed mood only, integrated, and referral-only control). Follow-up occurred one-month post-intervention. Results: While no main effects for the interventions were found, there were moderation effects, such that students in the alcohol only and integrated conditions who had lower levels of depressed mood or alcohol-related problems at baseline showed greater reductions in alcohol-related problems at follow-up compared to students in the control condition. Implications for interventions are discussed.
Keywords: depressed mood, alcohol use, college students
1. Introduction
Emerging evidence on the comorbidity of alcohol use, related problems and depressed mood in college students points to the need for development of effective prevention and intervention approaches for this high-risk population. Numerous studies have found a relationship between greater alcohol use and/or related problems and depression or depressed mood symptoms in both community and college samples (Berger & Adesso, 1991; Camatta & Nagoshi, 1995; Colder, 2001; Flynn, 2000; Geisner, Larimer, & Neighbors, 2004; Wills, Sandy, Shinar, & Yaeger, 1999). Research has shown college student drinkers have a 50% increase in risk of mood or anxiety disorder compared to non-drinkers (Dawson, Grant, Stinson, & Chou, 2005). Further, students with alcohol dependence are more than twice as likely as non-drinkers to have a mood disorder. Similarly, college students with depressed mood have been shown to be more likely than non-depressed peers to use alcohol and other drugs and report more related consequences (Geisner et al., 2004; Ross, 2004; Weitzman, 2004). Approximately 82% of students with “poor mental health/depression” report drinking alcohol, 50% report heavy episodic or binge drinking, and these students report increased likelihood of drinking to get drunk compared to those without depression (Gilvarry, 2000; Weitzman, 2004).
Both alcohol misuse and depressed mood are common in college populations, and the comorbidity of these disorders is related to increased risk of negative consequences and decreased likelihood of maturing out of alcohol use problems in the future (Christensen, Griffiths, & Jorm, 2004; Perkins, 1999). Though there is great debate as to causality (i.e. does depression lead to more drinking or more drinking lead to more depression?), the nature of the relationship is complicated and it is likely that the relationship between mood and drinking is actually bidirectional. For example, Hussong and colleagues (Hussong, Hicks, Levy, & Curran, 2001) found sadness and hostility predicted subsequent drinking behavior, and drinking was associated with relief from sadness and hostility. However, drinking was also related to increased sadness and hostility dependent upon timeframe and social context, illustrating the complex nature of these relationships (Hussong et al., 2001). Unfortunately, students experiencing these difficulties are often not identified, and when they are, they often receive no services. Thus, an additional challenge involves connecting people who could benefit from clinical services with appropriate care earlier, to prevent development of a more significant problem in the future. It remains an empirical question that has been largely unaddressed in the field as to whether treating alcohol first, depression first, or both at the same time is most efficacious.
1.1. Brief Interventions for Comorbid Alcohol Use and Depressed Mood
Many preventions and brief interventions exist to help college student drinking (see Cronce & Larimer, 2011; Larimer & Cronce, 2002, 2007, for reviews) with web-based, personalized normative preventions/interventions showing both cost and outcome effectiveness. For depressed mood, fewer preventions and brief interventions are available for college students, though several on-line options have been tested and found to be effective for depression/stress (Bergström et al., 2003; Christensen et al., 2004; Clarke et al., 2002; Proudfoot et al., 2004; Zetterqvist, Maanmies, Ström, & Andersson, 2003). However, despite the documented comorbidity between depression and alcohol problems (Grant & Harford, 1995; Kessler et al., 1997; Substance Abuse and Mental Health Services Administration [SAMHSA], 2008), relatively few prevention or brief intervention studies could be found for those who are both heavy drinkers and have depressed mood. Specifically, Geisner and colleagues (Geisner, Neighbors, Lee, & Larimer, 2007) found normative feedback significantly reduced normative perceptions about peer alcohol use as well as personal alcohol use and problems in college students screened for depressed mood. A study examining comorbid depressed mood and alcohol use in an adult community sample found computerized and in-person versions of an intervention to be equally efficacious in reducing both mood symptoms and alcohol use at 12 month follow up (Kay-Lambkin, Baker, Lewin, & Carr, 2009). Taken together, these studies suggest it may be beneficial to utilize web-based interventions with comorbid populations.
1.2. Web-based Approaches as Part of a Stepped-Care Model
Web-based approaches are attractive due to cost-effectiveness, ability to personalize information, and the widespread accessibility of the internet (McCabe, Diez, Boyd, Nelson, & Weitzman, 2006). Furthermore, younger people not only wish to access health information through forums using technology, they are actually critical of more traditional delivery methods (Chambers, Connor, & McElhinney, 2005). Stigma, cost, and other barriers could prevent those who may need services from seeking them (Harris & Edlund, 2005; Ross, 2004; SAMHSA, 2008). Providing individuals with personalized information about their symptoms in private (via the web) could enable them to prevent escalation of symptoms and problems and facilitate future treatment seeking if needed (Geisner, Neighbors, & Larimer, 2006; Patel, Branch, Mottur-Pilson, & Pinard, 2004; Sirey, Bruce, & Alexopoulos, 2005).
It has been suggested that a stepped care approach could be appropriately utilized with dually diagnosed individuals (Parikh, 2008). Brief alcohol-based feedback interventions have shown efficacy across a variety of drinkers ranging from light, non-problem drinkers to heavy problematic drinkers (for reviews see Larimer and Cronce, 2007; 2011; Murphy et al., 2012). However, less is known regarding the level to which students with comorbid depressed mood and alcohol use will benefit from these types of interventions (Merrill, Reid, Carey, Carey, 2014; Murphy et al., 2012). Previous studies have shown similar brief interventions are particularly effective for those with milder disturbances (Murphy et al., 2012), and have been used within a step care model for other comorbid conditions (e.g., alcohol use and smoking [Cunningham, Selby, & van Mierlo, 2006], depression and anxiety [Christensen et al., 2004]). One consideration when utilizing a brief feedback intervention with individuals experiencing depressed mood is that individuals with more severe symptoms may have less motivation to engage in the intervention (Merrill et al., 2014). Individuals experiencing more severe symptoms may require more intensive in-person interventions. Brief feedback interventions were designed to be used as an early intervention/prevention rather than a treatment of more severe disorders. Therefore, if brief interventions show efficacy in individuals with mild symptoms, they could prevent escalation to more severe disorders and reduce the future needs for long term care by identifying and intervening with people earlier. Thus, for college students already experiencing symptoms of both mood and alcohol problems, such an approach has the potential to be part of an effective and efficient model for delivering interventions targeted to people along the continuum of depression and alcohol use (Geisner et al., 2006, 2007; Marks, 2002). The proposed study evaluates a web based intervention for college students with comorbid mood and alcohol problems.
1.3. The Present Study
The current study is the first to evaluate a brief, personalized, web-based intervention for college students experiencing both elevated alcohol use and depressed mood. The first goal of the study was to extend previous work by evaluating the efficacy of an internet based adaptation of a mailed, brief intervention targeting comorbid depressed mood and alcohol use (Geisner et al., 2006, 2007). Further, previous work examined one intervention condition (combined mood and alcohol feedback) compared to control. In order to extend this work, the present study compared three intervention conditions (i.e., mood only, alcohol only, and integrated) to a control group in order to identify the type and amount of content needed to reduce alcohol use and problems among college students endorsing comorbid depressed mood and risky alcohol use. Based on previous work showing the benefits of brief alcohol (Larimer & Cronce, 2002, 2007) and mood interventions (e.g. Geisner et al., 2006), we hypothesized individuals in the mood only and alcohol only intervention conditions would report significantly less alcohol use and fewer consequences compared to controls. Additionally, considering the integrated condition addressed both mood and alcohol use, we hypothesized individuals in this condition would report significantly less alcohol use and fewer alcohol-related consequences compared to individuals in the other conditions.
A secondary focus of the study examined moderating variables for intervention effects, as similar brief interventions have been shown to be effective at reducing alcohol use and have been able to identify which students benefitted most from the intervention (Neighbors, Lee, Lewis, Fossos, & Walter, 2009; Neighbors, Lewis, Bergstrom, & Larimer, 2006). Based on research showing individuals with milder comorbid symptoms tend to benefit more from brief interventions (Christensen et al., 2004; Clarke et al., 2002), we expected individuals with milder depression symptoms and a history of experiencing fewer alcohol related problems would have a more optimal drinking response to the intervention compared to those with more severe symptoms and alcohol problems.
2. Methods
2.1 Sample Characteristics
The sample consisted of 311 students (62.4% female) from a large, public university in the Pacific Northwestern United States. The mean age at baseline was 20.14 (SD=1.34) years. With respect to racial background, 59.7% of the sample identified as white or Caucasian, 19.4% identified as Asian or Pacific Islander, 1.2% identified as black or African American, 8.4% identified as multiracial, less than 1% identified as Native American, and the remaining proportion of the sample identified as being of some other racial background. Separate from race, 7.8% of the sample reported being of Hispanic/Latino ethnicity.
Associations between baseline characteristics and the mood and drinking outcomes were assessed. At baseline, there were significant gender differences in levels of depression (t = 2.73, p < .01; mean for females = 23.51 [SD = 7.94]; mean for males = 22.57 [SD = 7.25]), and typical weekly drinking (t = 2.28, p < .05; mean for females = 15.91 [SD = 8.95]; mean for males = 17.15 [SD = 10.16]). Racial background was coded dichotomously so that 0 = non-white/Caucasian and 1 = white/Caucasian. At baseline, consequences were significantly higher among non-whites (t = 2.68, p < .05; mean for non-white/Caucasian = 22.51 [SD = 17.11]; mean for white/Caucasian = 18.15 [SD = 12.92]). Thus gender and racial background were included as control variables in the following analyses. There were no differences in depression (F = .10, p = .96), typical weekly drinking (F = .57, p = .64), or consequences (F = .23, p = .88), by intervention condition at baseline. Table 1 shows the means for the three outcome variables by intervention condition at baseline.
Table 1.
Means (and SD) for Outcome Variables at Baseline, by Intervention Condition.
| Condition | |||||
|---|---|---|---|---|---|
|
| |||||
| Integrated | Alcohol Only | Mood Only | Control | F (3,307) | |
| Depression | 22.81 (8.31) | 23.49 (7.47) | 23.14 (7.79) | 23.35 (7.44) | 0.10 |
| Typical weekly drinks | 18.39 (11.69) | 16.27 (9.16) | 16.90 (9.57) | 17.12 (10.23) | 0.57 |
| Alcohol-related consequences | 19.92 (15.89) | 18.67 (13.78) | 19.59 (14.46) | 20.60 (14.78) | 0.23 |
Note. Means and F-values correspond to one-way ANOVA with no covariates.
2.2 Procedures
Participant flow through the study is presented in Figure 1. The purpose of this study was to examine the efficacy of web-based personalized feedback at reducing depressed mood and alcohol use in college students. Outcome analyses focused on participants' mood, alcohol use, and related consequences reported at the one-month follow-up assessment. All study procedures were approved by the university IRB. There were no adverse events reported.
Fig. 1.
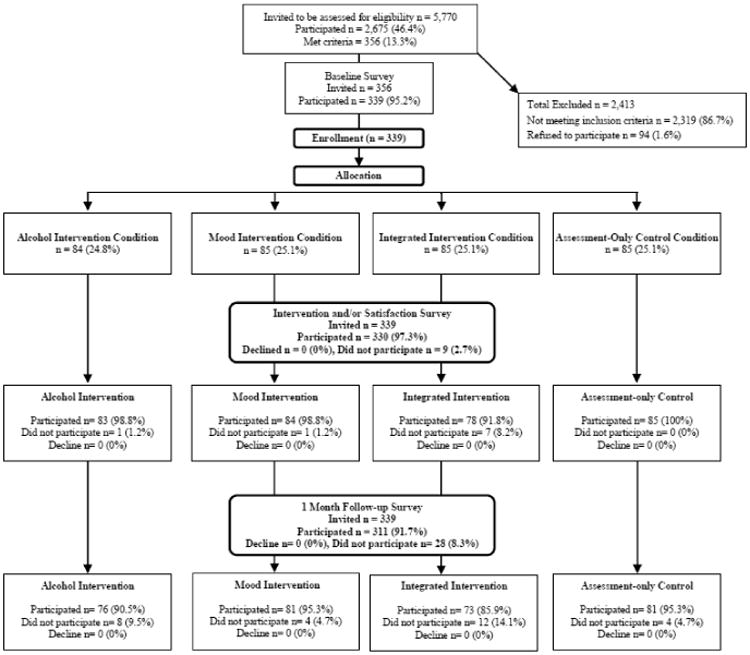
Participant Flow.
A randomly selected list of 5,770 enrolled undergraduates age 18 to 24 was obtained from the university registrar office. Participants were recruited across four academic quarters between fall 2011 and winter of 2013. Interested students logged on to the study website, viewed an online consent form and were asked to complete a brief 15 minute screening survey about their mood and alcohol use, perceptions of depression among other students, and demographic information. Participants met criteria if they reported consuming 4+/5+ drinks (women/men) on at least one occasion in the past month, a problem drinking score of 8 or greater on the Alcohol Use Disorders Identification Test (AUDIT; Saunders, Aasland, Babor, & de la Fuente, 1993), and a depressed mood score of 14 or greater on the Beck Depression Inventory-II (BDI-II; Beck, Steer, & Brown, 1996). These cut-off scores on self-administered tests were used in order to select a population for intervention that has been shown to be at-risk for both alcohol use disorders and depression. Generally, a cutoff score of 8 on the AUDIT has been suggested for detecting at-risk drinking in adult populations (Saunders et al., 1993). A recent study found that at a score of 8 on the AUDIT showed the best sensitivity and specificity in detecting at-risk drinking in a sample of college students (DeMartini and Carey, 2012). According to Beck et al. (Beck, Steer, & Brown, 1996), scores of 14 or greater indicate mild to severe depression (for scores 29 or greater). Those who consented and met screening criteria for the longitudinal trial were invited for further participation. A total of 2,675 students (46.4%) participated in the initial survey and 356 (13.3%) met eligibility criteria.
Immediately following the screening survey, eligible participants were routed to a 40-45 minute baseline survey, which asked further questions about alcohol use and mood, including drinking patterns, alcohol-related consequences, perceptions of other students' drinking, and coping. Of those eligible, 95.2% participated in the baseline assessment and were invited to the remainder of the study.
Upon completing baseline, participants were randomly assigned to one of four conditions: 1) Alcohol only intervention, 2) Depressed mood only intervention, 3) Integrated intervention, and 4) Assessment only control. The web-based interventions were presented immediately following the baseline survey and individual procedures are described below. Participants in the first three conditions were routed to view personalized online feedback materials after completing baseline. Participants in the Control condition were routed to view treatment resource information for depression and substance use, but did not view any personalized feedback or intervention materials. All participants were invited to a short satisfaction questionnaire after viewing these materials. Of those eligible, 97% participated in both the baseline and satisfaction assessments, and 91.7% participated in a follow-up assessment one month after the intervention. Participants received up to five email reminders for each survey, a postcard reminder, a phone call reminder, and were paid $10 for completing screening and $25 for completing each of baseline and the one-month follow-up assessment. Participants in the first three conditions received weekly email invitations to log in and review their feedback for a period of five weeks. There was variability between conditions in completion rates at follow-up, which ranged from 85.9% to 95.3%, χ2(df = 3) = 6.86, p=.08. Figure 1 includes specific follow-up rates by condition. Upon completion of the study, participants in the Control condition were emailed a link to view the online integrated feedback materials.
2.3 Interventions
Custom programming was used to link feedback to the screening and baseline surveys in order to allow each participant's intervention material to be customized with their responses. Personalized feedback included responses regarding alcohol use and related consequences, protective behavioral strategies, normative perceptions, and/or depression symptoms and coping strategies.
2.3.1 Alcohol only intervention
The alcohol intervention was theoretically based on a tailored social norms approaches and was composed of a personalized feedback component and suggested protective behaviors (i.e. tips/strategies for reducing problematic alcohol use) as well as brief psycho-education regarding the potential relationship between alcohol and depressed mood, without directly targeting mood symptoms. Personalized feedback utilized text and graphic formatting to provide an overview of participant's own reported drinking frequency and quantity, and enabled them to compare their own drinking to their perceived drinking norms for college students, as well as to the actual average rate of drinking reported among college students. Participants were presented with their own drinking percentile relative to other students. Protective strategies the participant was already using when drinking were summarized, and additional strategies were listed, along with encouragement for the participant to consider utilizing new strategies not already endorsed. The intervention finished by providing participants with a referral list of treatment resources.
2.3.2 Depressed mood only intervention
This intervention was designed based on aspects of the alcohol personalized interventions including social norms skills/protective strategies, and customized information about one's own behaviors (i.e. depressed mood), and consisted of personalized feedback and coping strategies based on literature on treatment for depression. The intervention began with a statement about the prevalence of depressed mood in order to provide context, normalize and empathize with the participant's experience. Personalized feedback utilized text and graphic formatting to provide an overview of participant's own reported depression symptoms, without directly targeting drinking behavior. Participants were reinforced for positive coping strategies they were using, and were encouraged to utilize a list of strategies shown to be effective in the treatment of depressed mood. The intervention finished by providing participants with a referral list of treatment resources.
2.3.3 Integrated intervention
This intervention was designed to target both alcohol use and depressed mood, and consisted of a combination of the same material presented in both the Alcohol only and Depressed mood only interventions. In addition, more in-depth psycho-education was provided regarding the potential relationship between alcohol and depression, with a focus on pointing out any specific depressed symptoms reported by the participants that may be exacerbated by alcohol use.
2.4 Intervention Fidelity
Intervention fidelity was assessed as follows. Participants were asked to indicate whether they read the intervention materials (“Did you view the mood feedback and tips on the previous pages?” [For the Depressed Mood only and Integrated conditions], and “Did you view the alcohol feedback and tips on the previous pages?” [For the Alcohol only and Integrated conditions]). For those in the mood only or integrated conditions, 89.0% reported reading the mood-related intervention materials. For those in the alcohol only or integrated conditions, 90.6% reported reading the alcohol-related intervention materials. Intent-to-treat analyses were conducted, so participants were included in the analyses regardless of whether they indicated that they read the intervention materials.
2.5 Measures
2.5.1 Depression symptoms
The Beck Depression Inventory-II (BDI-II; Beck et al, 1996) was used to assess depression symptoms occurring during the past two weeks up to and including the study day. This widely used self-report measure of depression includes 21 multiple-choice items (each ranging from 0–3), summed to create a single composite score, with higher scores indicating more symptoms of depression (scores 0-13 indicate minimal depression; 14-19 mild depression; 20-28 moderate depression; 29-66 indicate severe depression). Cronbach's α was .83 at baseline and .92 at follow-up.
2.5.2 Typical weekly drinking
The Daily Drinking Questionnaire (DDQ; Collins, Parks, & Marlatt, 1985; Dimeff, Baer, Kivlahan, & Marlatt, 1999) was used to assess the number of standard drinks participants consumed in a typical week. Participants were asked to provide responses for each of the 7 days. A definition of a standard drink was provided prior to the questions. At baseline, the instructions asked participants to think about their drinking over the past three months; whereas instructions at one-month follow-up asked only about the past one month in order to avoid participants reporting about drinking which took place prior to the intervention.
2.5.3 Alcohol consequences
The Rutgers Alcohol Problem Index (RAPI; White & Labouvie, 1989) includes 25 multiple-choice items assessing alcohol-related consequences occurring from 0 (Never) to 4 (more than 10 times). At baseline, the instructions asked participants to report consequences occurring over the past three months; whereas, instructions at one-month follow-up asked only about the past one month in order to avoid participants reporting consequences which took place prior to the intervention. Cronbach's α was .93 at baseline and .95 at follow-up.
2.6 Data Management
Missing data (less than 5% for all variables) were confirmed to be missing at random (MAR; Rubin, 1976). Missing data were imputed using EM methods (expectation-maximization; Schafer & Graham, 2002). Data points greater than 3.29 standard deviations from the mean (less than 5% for all variables) were recoded to 3.29 standard deviations from the mean (Tabachnick & Fidell, 2012) prior to further analysis.
2.7 Analysis Plan
Generalized linear models were used 1) to estimate the main effects of intervention condition on depression, typical weekly drinking, and alcohol-related consequences, and 2) to assess whether baseline severity (assessed with respect to depression, typical weekly drinking, and alcohol-related consequences) moderated the effect of intervention condition on the three outcomes listed above. For the main effects analyses, gender, racial background, and baseline levels of the outcome variable were included as covariates in the models, and a p-value of less than .05 for the F-value associated with the intervention condition was considered evidence of a significant effect. For the moderation analyses, an intervention condition × baseline severity term was included in the model, and the same criteria were used to determine whether effects were significant. In cases where significant interactions were detected, predicted values of the outcome variable at below average (1 SD below the mean), average (mean) and above average (1 SD above the mean) levels of the moderator were plotted according to the suggestions of Jaccard, Wan, & Turrisi (1990). Tukey's HSD test was used to determine whether predicted values of outcomes were significantly different from each other.
3. Results
3.1 Main Effects
Table 2 shows the means for the three outcome variables by intervention condition at one-month follow-up, when no covariates were included in the model. There were no significant differences. After controlling for gender, racial background, and baseline levels of the outcome variables, there were no main effects of intervention condition on depression (F=.81, p=78), typical weekly drinking (F=1.51, p=.54), or consequences (F=1.51, p=.28).
Table 2.
Means (and Standard Deviations) for Drinking and Mood-Related Outcomes at One-Month Follow-up, by Treatment Condition.
| Condition | |||||
|---|---|---|---|---|---|
|
| |||||
| Integrated | Alcohol Only | Mood Only | Control | F (3,307) | |
| Depression | 21.31 (11.53) | 21.31 (12.15) | 20.77 (10.71) | 22.35 (10.02) | 0.36 |
| Typical weekly drinks | 14.41 (11.15) | 14.16 (10.90) | 12.39 (10.58) | 14.35 (10.09) | 0.72 |
| Alcohol-related consequences | 13.40 (14.40) | 11.71 (13.09) | 13.29 (13.38) | 15.90 (13.57) | 1.28 |
Note: Means and F-values correspond to one-way ANOVA with no covariates.
3.2 Moderated Effects
3.2.1 Baseline depression
Moderation analyses revealed baseline depression scores moderated the effect of intervention condition on alcohol-related consequences at follow-up, after controlling for gender, racial background, and baseline consequences (F=1.57, p=.01). Figure 2 shows the predicted values of consequences for each of the four intervention conditions at three levels of baseline depression (below average, average, and above average, relative to the rest of the sample). Tukey's post-hoc HSD test revealed that at below average levels of baseline depression, the predicted number of reported alcohol-related consequences at follow-up was significantly lower in the alcohol only (9.32 consequences) and integrated (10.16 consequences) conditions than in the control condition (16.51 consequences). The mood only condition (11.11 consequences) was not significantly different from the other conditions. At average and above average levels of baseline depression (again relative to the rest of the sample), the predicted number of reported alcohol-related consequences was not significantly different between conditions.
Fig. 2.
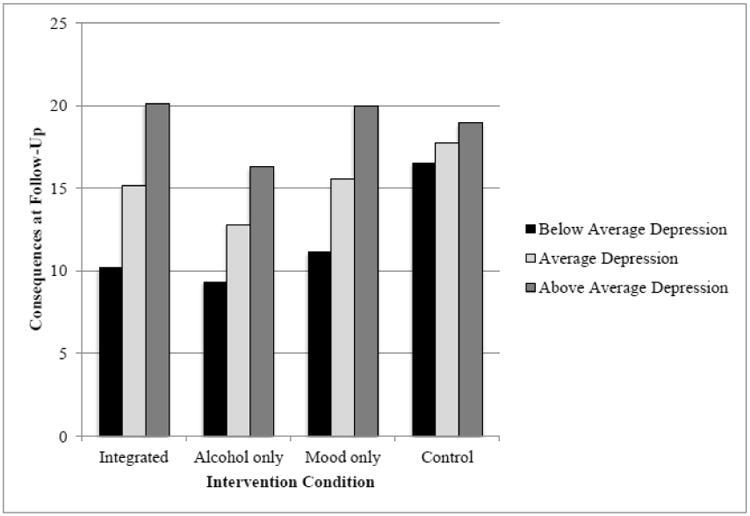
Predicted Values of Consequences at Follow-Up for Baseline Depression by Intervention Condition Interaction.
3.2.2 Baseline consequences
Similarly, baseline alcohol-related consequences score moderated the effect of intervention condition on alcohol-related consequences at follow-up after controlling for gender and racial background (F=1.49, p=.01). Figure 3 shows the predicted value of alcohol-related consequences for each of the four intervention conditions at three levels of baseline consequences (below average, average, and above average relative to the rest of the sample). The pattern of predicted values was consistent with previous analyses, such that at below average levels of baseline consequences, the predicted value of consequences at follow-up was lower in the alcohol only condition (3.07 consequences) than in the control condition (5.97 consequences). At above average levels of baseline consequences, the number of reported consequences at follow-up was lower in the mood only (23.81 consequences), alcohol only (23.29 consequences), and integrated (23.93 consequences) conditions relative to the control condition (26.37 consequences). Tukey's post-hoc HSD test did not indicate these differences were statistically significant.
Fig. 3.
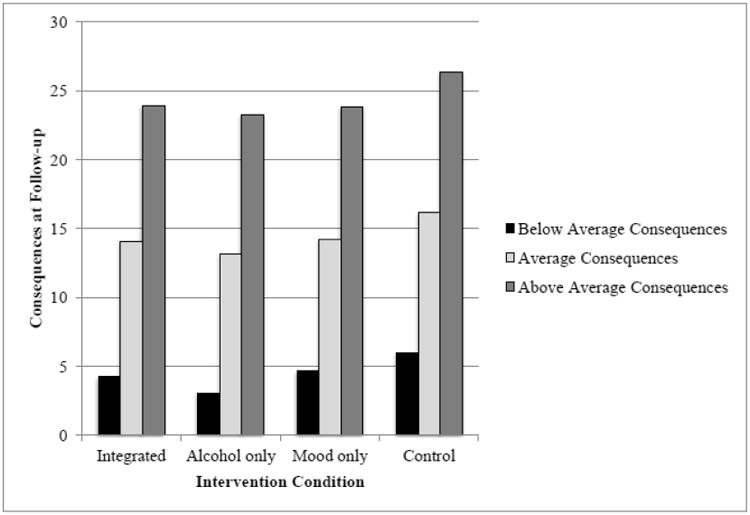
Predicted Values of Consequences at Follow-Up for Baseline Consequences by Intervention Condition Interaction.
4. Discussion
The current study evaluated the efficacy of a brief, personalized, web-based intervention for college students experiencing both risky alcohol use and depressed mood. Contrary to our primary hypothesis, no main effects were observed on alcohol or mood outcome variables for any of the three intervention conditions (i.e., mood only, alcohol only, and integrated) compared to control. Previous work has shown the benefits of printed or web-based brief alcohol (e.g., Kypri et al. 2004; Murphy et al., 2004; Neighbors et al., 2006) and mood interventions (e.g. Geisner et al., 2006) as well as combined treatment (Baker et al., 2014; Riper et al., 2014). However additional alcohol studies utilizing a similar type of intervention approach had less than optimal or mixed findings (Brown et al., 2011; Lysaught et al., 2003; Merrill, 2014). Specifically, some studies observed significant reductions in drinking but not negative consequences (e.g., Larimer et al., 2007; Walters et al, 2007), and others found no significant differences on any alcohol outcomes (e.g., Neal & Carey, 2004). It is unclear what factors contribute to these mixed findings across studies.
One potential reason for this finding in the current study is the complicated relationship between alcohol and depressive symptoms in college students. Research is inconclusive about the cause and effect pattern between depressed mood and alcohol consumption and related problems. Studies have shown individuals who report higher rates of depressive symptoms also report increased alcohol-related consequences compared to non-depressed students; however, no differences in alcohol consumption rates are typically observed (Geisner et al., 2004; Gilvarry, 2000; Ross, 2004; Weitzman, 2004). A second reason for our findings is that college students often drink for multiple motives, some drink to cope and alleviate negative affect, while others drink for social reasons (Cooper, Frone, M.R., Russell, M. & Mudar, 1995; Kuntsche, Knibbe, Gmel, & Engels, 2005). The alcohol intervention used in this study is based on a social norms approach, and thus it is possible that such interventions do not work as well for those who drink for coping reasons (and are thus likely to be more depressed). Similarly, online interventions may just not work well for those with more severe depression symptoms due to problems sustaining attention or other issues (Merrill et al., 2014).
Another reason for our findings could be due to variability within our sample in terms of severity of depressive symptoms and high risk drinking behaviors. Therefore, we examined these potential moderating variables to identify if certain students benefited from the intervention. Findings from the moderation analyses indicated students who had milder depression symptoms at baseline and were in the alcohol only and integrated intervention conditions reported fewer alcohol related consequences at follow-up compared to controls. In addition, students who reported fewer alcohol-related consequences at baseline and were randomized to the alcohol only intervention reported fewer alcohol-related consequences at follow-up. These findings were mostly consistent with our hypotheses positing individuals who reported milder depression symptoms and/or fewer alcohol-related problems would have a more optimal response to the intervention compared to those with more severe symptoms and/or alcohol problems. We initially expected that individuals in the integrated condition would have the most optimal response; however, students in the alcohol only condition also saw significant reductions in alcohol-related consequences. This is consistent with findings of a recent meta-analysis which did not show integrated treatment to be superior to single-focus treatment when looking at alcohol and depression (Riper et al., 2014). Our findings suggests that students with milder depressive symptoms and less problematic drinking patterns may benefit from an alcohol only intervention and is consistent with previous studies showing individuals with milder symptoms tend to benefit more from brief interventions (Christensen et al., 2004; Clarke, et al., 2002; Merrill et al., 2014).
4.1 Clinical Implications
Students experiencing comorbid depressive symptoms and risky alcohol use are in need of intervention efforts. Unfortunately, it is difficult to identify these individuals and they often do not seek or receive services (Eisenberg, Golberstein, & Gollust, 2007). Findings from the current study suggest a brief screen can easily detect individuals who report both depressive symptoms and alcohol use. Further, individuals experiencing milder depressive symptoms and/or alcohol problems may benefit from a brief, web-based alcohol feedback intervention. While it is uncertain whether treating alcohol first, depression first, or both at the same time is most efficacious, reducing the amount of alcohol problems students experience is beneficial. Further, using a brief screen can identify students with more severe depressive symptoms and alcohol problems. While a brief intervention may not be optimal for these students, they can be connected to more appropriate clinical services. These students may benefit from more intensive in-person intervention efforts aimed at alleviating distress and reducing alcohol consumption and consequences. This is consistent with other studies that have found that people with more severe depression may benefit more from a provider-led treatment (Penberthy, Hook, Hettema, Farrell-Carnahan, Ingersoll, 2013).
4.2 Limitations & Future Directions
While careful controls were in place throughout the study, certain limitations remain. First, data were collected at one university and generalizability to other types of institutions and students in other geographical locations is limited. Second, participants' level of engagement with the feedback was difficult to assess due to the web-based platform used to deliver the intervention. Additional research examining the possible benefits of making feedback interventions more interactive rather than having students simply read personalized feedback would be useful. This study highlights that certain interventions (i.e. alcohol only, mood only, etc.) may work for certain subpopulations and not others (i.e. those with lower/no depression). One of the benefits of web-based interventions is their flexibility and adaptability which means that we have the potential to truly personalize interventions based on a variety of individual difference variables. Thus students with different levels of depression could get completely different interventions. Finally, while a computer-based delivery method has the potential to capitalize on the efficiency and cost effectiveness of using the Internet to deliver prevention and intervention materials, students with more severe symptoms may need more intensive in-person treatment. Additional research is needed to evaluate in-person interventions as well as develop and test a stepped-care approach to treat students with high risk alcohol use and comorbid depression.
4.3 Conclusion
Results from the current study found a brief, web-based feedback intervention was efficacious in reducing alcohol problems for college students endorsing mild depressive symptoms and alcohol consequences. Using a brief screen is a cost effective way to identify at-risk students with comorbid mood and alcohol problems and offering an immediate web-based feedback intervention provides early intervention for individuals not seeking treatment. Additional research is needed to test potential interventions for students with more severe depressive symptoms and drinking patterns.
Highlights.
Evaluated a web-based intervention for college student alcohol use and depressed mood
No main effects for the interventions were found
Intervention effective for those with less depression and/or alcohol use at baseline
Acknowledgments
This research was supported by a grant from the National Institute on Alcohol Abuse and Alcoholism (NIAAA; R21AA019993) awarded to Irene Markman Geisner. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIAAA or the National Institutes of Health.
Role of Funding Sources: Funding for this study was provided by NIAAA Grant R21AA019993. NIAAA had no role in the study design, collection, analysis or interpretation of the data, writing the manuscript, or the decision to submit the paper for publication.
Footnotes
Contributors: Author I. M Geisner designed the study, wrote the protocol, and wrote the first draft of the manuscript. Author L. Varvil-Weld, K. Mallett, and R. Turrisi conducted the statistical analyses. Author A. Mittmann wrote the methods section. Author K. Mallett wrote the discussion section, and all authors contributed to and have approved the final manuscript.
Conflict of Interest: All authors declare that they have no conflicts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Irene M. Geisner, Email: geisner@u.washington.edu.
Lindsey Varvil-Weld, Email: lvweld@psu.edu.
Angela J. Mittmann, Email: mittmann@u.washington.edu.
Kimberly Mallett, Email: kmallett@psu.edu.
Rob Turrisi, Email: rjt13@psu.edu.
References
- Baker AL, Kavanagh DJ, Kay-Lambkin FJ, Hunt SA, Lewin TJ, Carr VJ, McElduff P. Randomized controlled trial of MICBT for co-existing alcohol misuse and depression: Outcomes to 36-months. Journal of Substance Abuse Treatment. 2014;46(3):281–290. doi: 10.1016/j.jsat.2013.10.001. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA, Brown GK. Manual for the Beck Depression Inventory–II. San Antonio, TX: Psychological Corp; 1996. [Google Scholar]
- Berger BD, Adesso VJ. Gender differences in using alcohol to cope with depression. Addictive Behaviors. 1991;16:315–327. doi: 10.1016/0306-4603(91)90024-C. [DOI] [PubMed] [Google Scholar]
- Bergstrom J, Hollandare F, Carlbring P, Kaldo-Sandstrom V, Ekselius L, Andersson G. Treatment of depression via the Internet: A randomized trial of a self-help programme. Journal of Telemedicine and Telecare. 2003;9(Suppl2):85–91. doi: 10.1258/135763303322596381. [DOI] [Google Scholar]
- Brown RA, Ramsey SE, Kahler CW, Palm KM, Monti PM, Abrams D, et al. Miller IW. A randomized controlled trial of cognitive-behavioral treatment for depression versus relaxation training for alcohol-dependent individuals with elevated depressive symptoms. Journal Of Studies On Alcohol And Drugs. 2011;72(2):286–296. doi: 10.15288/jsad.2011.72.286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Camatta CD, Nagoshi CT. Stress, depression, irrational beliefs, and alcohol use and problems in a college student sample. Alcoholism: Clinical and Experimental Research. 1995;19:142–146. doi: 10.1111/j.1530-0277.1995.tb01482.x. [DOI] [PubMed] [Google Scholar]
- Chambers M, Connor SL, McElhinney S. Substance use and young people: The potential of technology. Journal of Psychiatric and Mental Health Nursing. 2005;12:179–186. doi: 10.1111/j.1365-2850.2004.00815.x. [DOI] [PubMed] [Google Scholar]
- Christensen H, Griffiths KM, Jorm AF. Delivering interventions for depression by using the Internet: Randomized controlled trial. British Medical Journal. 2004;328:265–269. doi: 10.1136/bmj.37945.566632.EE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clarke G, Reid E, Eubanks D, O'Connor E, DeBar LL, Kelleher C, et al. Nunley S. Overcoming depression on the internet (ODIN): A randomized controlled trial of an internet depression skills intervention program. Journal of Medical Internet Research. 2002;4:e14. doi: 10.2196/jmir.4.3.e14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colder CR. Life stress, physiological and subjective indexes of negative emotionality, and coping reasons for drinking: Is there evidence for a self-medication model of alcohol use? Psychology of Addictive Behaviors. 2001;15:237–245. doi: 10.1037/0893-164X.15.3.237. [DOI] [PubMed] [Google Scholar]
- Collins RL, Parks GA, Marlatt GA. Social determinants of alcohol consumption: the effects of social interaction and model status on the self-administration of alcohol. Journal of Consulting and Clinical Psychology. 1985;53:189–200. doi: 10.1037/0022-006X.53.2.189. [DOI] [PubMed] [Google Scholar]
- Cooper M, Frone MR, Russell M, Mudar P. Drinking to regulate positive and negative emotions: A motivational model of alcohol use. Journal of Personality & Social Psychology. 1995;69:990–1005. doi: 10.1037//0022-3514.69.5.990. [DOI] [PubMed] [Google Scholar]
- Cronce JM, Larimer ME. Individual-focused approaches to the prevention of college student drinking. Alcohol Research & Health. 2011;34:210–221. [PMC free article] [PubMed] [Google Scholar]
- Cunningham JA, Selby P, van Mierlo T. Integrated online services for smokers and drinkers? Use of the Check Your Drinking assessment screener by participants of the Stop Smoking Center. Nicotine & Tobacco Research. 2006;8(Suppl1):S21–S25. doi: 10.1080/14622200601039865. [DOI] [PubMed] [Google Scholar]
- Dawson DA, Grant BF, Stinson FS, Chou PS. Psychopathology associated with drinking and alcohol use disorders in the college and general adult populations. Drug and Alcohol Dependence. 2005;77:139–150. doi: 10.1016/j.drugalcdep.2004.07.012. [DOI] [PubMed] [Google Scholar]
- DeMartini KS, Carey KB. Optimizing the use of the AUDIT for alcohol screening in college students. Psychological Assessment. 2012;24:954–963. doi: 10.1037/a0028519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dimeff LA, Baer JS, Kivlahan DR, Marlatt G. Brief Alcohol Screening and Intervention for College Students (BASICS): A harm reduction approach. New York, NY US: Guilford Press; 1999. [Google Scholar]
- Eisenberg D, Golberstein E, Gollust SE. Help-seeking and access to mental health care in a university student population. Medical Care. 2007;7:594–601. doi: 10.1097/MLR.0b013e31803bb4c1. [DOI] [PubMed] [Google Scholar]
- Flynn HA. Comparison of cross-sectional and daily reports in studying the relationship between depression and use of alcohol in response to stress in college students. Alcoholism: Clinical and Experimental Research. 2000;24:48–52. doi: 10.1111/j.1530-0277.2000.tb04552. [DOI] [PubMed] [Google Scholar]
- Geisner IM, Larimer ME, Neighbors C. The relationship between alcohol use, related problems, and psychological distress: Gender as a moderator in a college sample. Addictive Behaviors. 2004;29:843–848. doi: 10.1016/j.addbeh.2004.02.024. [DOI] [PubMed] [Google Scholar]
- Geisner IM, Neighbors C, Larimer ME. A randomized clinical trial of a brief, mailed intervention for symptoms of depression. Journal of Consulting and Clinical Psychology. 2006;74:393–399. doi: 10.1037/0022-006X.74.2.393. [DOI] [PubMed] [Google Scholar]
- Geisner IM, Neighbors C, Lee CM, Larimer ME. Evaluating personal alcohol feedback as a selective prevention for college students with depressed mood. Addictive Behaviors. 2007;32:2776–2787. doi: 10.1016/j.addbeh.2007.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilvarry E. Substance abuse in young people. Journal of Child Psychology and Psychiatry. 2000;41:55–80. doi: 10.1017/S0021963099004965. [DOI] [PubMed] [Google Scholar]
- Grant BF, Harford TC. Comorbidity between DSM-IV alcohol use disorders and major depression: results of a national survey. Drug and Alcohol Dependence. 1995;39:197–206. doi: 10.1016/0376-8716(95)01160-4. [DOI] [PubMed] [Google Scholar]
- Harris KM, Edlund MJ. Use of mental health care and substance abuse treatment among adults with co-occurring disorders. Psychiatric Services. 2005;56:954–959. doi: 10.1176/appi.ps.56.8.954. [DOI] [PubMed] [Google Scholar]
- Hussong AM, Hicks RE, Levy SA, Curran PJ. Specifying the relations between affect and heavy alcohol use among young adults. Journal of Abnormal Psychology. 2001;110:449–461. doi: 10.1037/0021-843X.110.3.449. [DOI] [PubMed] [Google Scholar]
- Jaccard J, Wan CK, Turrisi R. The detection and interpretation of interaction effects between continuous variables in multiple regression. Multivariate Behavioral Research. 1990;25:467–478. doi: 10.1207/s15327906mbr2504_4. [DOI] [PubMed] [Google Scholar]
- Kay-Lambkin FJ, Baker AL, Lewin TJ, Carr VJ. Computer-based psychological treatment for comorbid depression and problematic alcohol and/or cannabis use: a randomized controlled trial of clinical efficacy. Addiction. 2009;104:378–388. doi: 10.1111/j.1360-0443.2008.02444. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Crum RM, Warner LA, Nelson CB, Schulenberg J, Anthony JC. Lifetime co-occurrence of DSM-III-R alcohol abuse and dependence with other psychiatric disorders in the National Comorbidity Survey. Archives of General Psychiatry. 1997;54:313–321. doi: 10.1001/archpsyc.1997.01830160031005. [DOI] [PubMed] [Google Scholar]
- Kuntsche E, Knibbe R, Gmel G, Engels R. Why do young people drink? A review of drinking motives. Clinical Psychology Review. 2005;25:841–61. doi: 10.1016/j.cpr.2005.06.002. [DOI] [PubMed] [Google Scholar]
- Kypri K, Saunders JB, Williams SM, McGee RO, Langley JD, Cashell-Smith ML, Gallagher SJ. Web-based screening and brief intervention for hazardous drinking: A double-blind randomized controlled trial. Addiction. 2004;99(11):1410–1417. doi: 10.1111/j.1360-0443.2004.00847.x. [DOI] [PubMed] [Google Scholar]
- Larimer ME, Cronce JM. Identification, prevention and treatment: A review of individual-focused strategies to reduce problematic alcohol consumption by college students. Journal of Studies on Alcohol, Supplement. 2002;14:148–163. doi: 10.15288/jsas.2002.s14.148. [DOI] [PubMed] [Google Scholar]
- Larimer ME, Cronce JM. Identification, prevention, and treatment revisited: individual-focused college drinking prevention strategies 1999-2006. Addictive Behaviors. 2007;32:2439–2468. doi: 10.1016/j.addbeh.2007.05.006. [DOI] [PubMed] [Google Scholar]
- Larimer ME, Lee CM, Kilmer JR, Fabiano PM, Stark CB, Geisner IM, et al. Neighbors C. Personalized mailed feedback for college drinking prevention: A randomized clinical trial. Journal Of Consulting And Clinical Psychology. 2007;75(2):285–293. doi: 10.1037/0022-006X.75.2.285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lysaught E, Wodarski JS, Parris H. A comparison of an assessment/information-based group versus an assessment-only group: An investigation of drinking reduction with young adults. Journal of Human Behavior in the Social Environment. 2003;8(4):23–43. doi: 10.1300/J137v08n04_02. [DOI] [Google Scholar]
- Marks IM. The maturing of therapy: Some brief psychotherapies help anxiety/depressive disorders but mechanisms of action are unclear. British Journal of Psychiatry. 2002;180:200–204. doi: 10.1192/bjp.180.3.200. [DOI] [PubMed] [Google Scholar]
- McCabe SE, Diez A, Boyd CJ, Nelson TF, Weitzman ER. Comparing web and mail responses in a mixed mode survey in college alcohol use research. Addictive Behaviors. 2006;31:1619–1627. doi: 10.1016/j.addbeh.2005.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merrill JE, Reid AE, Carey MP, Carey KB. Gender and depression moderate response to brief motivational intervention for alcohol misuse among college students. Journal of Consulting and Clinical Psychology. 2014 doi: 10.1037/a0037039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy JG, Dennhardt AA, Skidmore JR, Borsari B, Barnett NP, Colby SM, Martens MP. A randomized controlled trial of a behavioral economic supplement to brief motivational interventions for college drinking. Journal of Consulting and Clinical Psychology. 2012;80(5):876–886. doi: 10.1037/a0028763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neal DJ, Carey KB. Developing discrepancy within self-regulation theory: Use of personalized normative feedback and personal strivings with heavy-drinking college students. Addictive Behaviors. 2004;29(2):281–297. doi: 10.1016/j.addbeh.2003.08.004. [DOI] [PubMed] [Google Scholar]
- Neighbors C, Lee CM, Lewis MA, Fossos N, Walter T. Internet-based personalized feedback to reduce 21st-birthday drinking: A randomized controlled trial of an event-specific prevention intervention. Journal of Consulting and Clinical Psychology. 2009;77:51–63. doi: 10.1037/a0014386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neighbors C, Lewis MA, Bergstrom RL, Larimer ME. Being controlled by normative influences: Self-determination as a moderator of a normative feedback alcohol intervention. Health Psychology. 2006;25:571–579. doi: 10.1037/0278-6133.25.5.571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parikh SV. Screening and treating mental disorders in addiction treatment settings: A stepped care model. International Journal of Mental Health and Addiction. 2008;6:137–140. doi: 10.1007/s11469-007-9095-3. [DOI] [Google Scholar]
- Patel VL, Branch T, Mottur-Pilson C, Pinard G. Public awareness about depression: The effectiveness of a patient guideline. International Journal of Psychiatry in Medicine. 2004;34:1–20. doi: 10.2190/yn2k-thq1-33va-hqmq. [DOI] [PubMed] [Google Scholar]
- Penberthy JK, Hook JN, Hettema J, Farrell-Carnahan L, Ingersoll K. Depressive symptoms moderate treatment response to brief intervention for prevention of alcohol exposed pregnancy. Journal of Substance Abuse Treatment. 2013;45:335–42. doi: 10.1016/j.jsat.2013.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perkins HW. Stress-motivated drinking in collegiate and post collegiate young adulthood: Life course and gender patterns. Journal of Studies on Alcohol. 1999;60:219–227. doi: 10.15288/jsa.1999.60.219. [DOI] [PubMed] [Google Scholar]
- Proudfoot J, Ryden C, Everitt B, Shapiro DA, Goldberg D, Mann A, et al. Gray JA. Clinical efficacy of computerized cognitive-behavioural therapy for anxiety and depression in primary care: Randomized controlled trial. British Journal of Psychiatry. 2004;185:46–54. doi: 10.1192/bjp.185.1.46. [DOI] [PubMed] [Google Scholar]
- Riper H, Andersson G, Hunter SB, de Wit J, Berking M, Cuijpers T. Treatment of comorbid alcohol use disorders and depression with cognitive-behavioural therapy and motivational interviewing: A meta-analysis. Addiction. 2014;109:394–406. doi: 10.1111/add.12441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ross V. Depression, anxiety, and alcohol or other drug use among college students. 2004 Retrieved from Education Development Center, Inc website: www.edc.org.
- Rubin DB. Inference and missing data. Biometrika. 1976;63(3):581–592. doi: 10.1093/biomet/63.3.581. [DOI] [Google Scholar]
- Saunders JB, Aasland OG, Babor TF, de la Fuente JR. Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption: II. Addiction. 1993;88:791–804. doi: 10.1111/j.1360-0443.1993.tb02093.x. [DOI] [PubMed] [Google Scholar]
- Schafer JL, Graham JW. Missing data: Our view of the state of the art. Psychological Methods. 2002;7:147–177. doi: 10.1037/1082-989X.7.2.147. [DOI] [PubMed] [Google Scholar]
- Sirey J, Bruce ML, Alexopoulos GS. The treatment initiation program: An intervention to improve depression outcomes in older adults. American Journal of Psychiatry. 2005;162:184–186. doi: 10.1176/appi.ajp.162.1.184. [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration (SAMHSA), U.S. Department of Health and Human Services. Results from the 2007 National Survey on Drug Use and Health: National Findings. Office of Applied Statistics; Rockville, MD: 2008. (Report No. NSDUH Series H-34). DHHS Publication No. SMA 08-4343. [Google Scholar]
- Tabachnick BG, Fidell LS. Using multivariate statistics. 5th. New York, NY: Pearson; 2012. [Google Scholar]
- Walters ST, Vader AM, Harris T. A controlled trial of Web-based feedback for heavy drinking college students. Prevention Science. 2007;8(1):83–88. doi: 10.1007/s11121-006-0059-9. [DOI] [PubMed] [Google Scholar]
- Weitzman E. Poor mental health, depression, and associations with alcohol consumption, harm, and abuse in a national sample of young adults in college. Journal of Nervous and Mental Disease. 2004;192:269–277. doi: 10.1097/01.nmd.0000120885.17362.94. [DOI] [PubMed] [Google Scholar]
- White HR, Labouvie EW. Toward the assessment of adolescent problem drinking. Journal of Studies on Alcohol. 1989;50:30–37. doi: 10.15288/jsa.1989.50.30. [DOI] [PubMed] [Google Scholar]
- Wills TA, Sandy JM, Shinar O, Yaeger A. Contributions of positive and negative affect to adolescent substance use: Test of a bidimensional model in a longitudinal study. Psychology of Addictive Behaviors. 1999;13:327–338. doi: 10.1037/0893-164X.13.4.327. [DOI] [Google Scholar]
- Zetterqvist K, Maanmies J, Ström L, Andersson G. Randomized controlled trial of Internet-based stress management. Cognitive Behaviour Therapy. 2003;32:151–160. doi: 10.1080/16506070302316. [DOI] [PubMed] [Google Scholar]


