Abstract
Myeloid cells, including granulocytes, monocytes, macrophages and dendritic cells, are crucial players in innate immunity and inflammation. These cells constitutively or inducibly express a number of receptors of the TNF receptor and Toll-like receptor (TLR) families, whose signals are transduced by TRAF molecules. In vitro studies showed that TRAF3 is required for TLR-induced type I interferon production, but the in vivo function of TRAF3 in myeloid cells remains unknown. Here we report the generation and characterization of myeloid cell-specific TRAF3-deficient (M-TRAF3−/−) mice, which allowed us to gain insights into the in vivo functions of TRAF3 in myeloid cells. We found that TRAF3 ablation did not affect the maturation or homeostasis of myeloid cells in young adult mice, even though TRAF3-deficient macrophages and neutrophils exhibited constitutive NF-κB2 activation. However, in response to injections with LPS (a bacterial mimic) or polyI:C (a viral mimic), M-TRAF3−/− mice exhibited an altered profile of cytokine production. M-TRAF3−/− mice immunized with T cell-independent (TI) and -dependent (TD) antigens displayed elevated TI IgG3 as well as TD IgG2b responses. Interestingly, 15–22 month old M-TRAF3−/− mice spontaneously developed chronic inflammation or tumors, often affecting multiple organs. Taken together, our findings indicate that TRAF3 expressed in myeloid cells regulates immune responses in myeloid cells and acts to inhibit inflammation and tumor development in mice.
Introduction
Tumor necrosis factor receptor-associated factor 3 (TRAF3), a member of the TRAF family of cytoplasmic adaptor proteins, is employed in signaling by a variety of immune receptors, including the tumor necrosis factor receptor (TNF-R) superfamily, Toll-like receptors (TLRs), NOD-like receptors (NLRs), and RIG-I-like receptors (RLRs) (1, 2). TRAF3 binds directly to almost all members of the TNF-R superfamily that do not contain death domains, including CD40, BAFF-R, TACI, BCMA, LT-βR, CD27, CD30, RANK, HVEM, EDAR, XEDAR, 4-1BB (CD137), OX-40 (CD134), and GITR (TNFRSF18). TRAF3 is also indirectly recruited to the signaling complexes of pattern recognition receptors (PRRs) of the innate immune system through interactions with additional adaptor proteins, including MyD88 and TRIF for TLR signaling, RIP2 for NLR signaling, and MAVS for RLR signaling (3–5). The shared usage of TRAF3 by such a variety of immune receptors is indicative of its broad functional roles in the immune system.
Mice made genetically deficient in TRAF3 (TRAF3−/−) die within 10 days of birth with severe progressive runting, illustrating crucial developmental functions of TRAF3 (6). To circumvent experimental limitations imposed by the early mortality of TRAF3−/− mice and to explore the in vivo functions of TRAF3 in various cell types of adult mice, we recently employed a conditional gene targeting strategy to generate conditional TRAF3-deficient (TRAF3flox/flox) mice. This makes it possible to delete the Traf3 gene in specific cell types or tissues (7). Characterization of conditional TRAF3-deficient mouse models revealed that TRAF3 is critically involved in regulating multiple receptor signaling pathways in different immune cell types. We previously reported that specific ablation of TRAF3 in B lymphocytes results in marked peripheral B cell hyperplasia, due to remarkably prolonged survival of mature B cells independent of the B cell survival factor BAFF, leading to the development of splenic marginal zone lymphomas (MZL) or B1 lymphomas by 18 months of age (7, 8). These findings indicated that a major homeostatic function of TRAF3 in peripheral B cells is the promotion of spontaneous apoptosis, a conclusion subsequently corroborated by Gardam and colleagues (9). In contrast, specific deletion of TRAF3 from the T cell lineage leads to defective IgG1 responses to a T cell-dependent (TD) antigen (Ag) and impaired T cell-mediated immunity to infection with Listeria monocytogenes due to compromised T cell receptor (TCR)/CD28 signaling in both CD4 and CD8 T cells (10). Additionally, recent evidence from other groups demonstrated that TRAF3 regulates the effector function of Treg cells (11) and that TRAF3 is required for the development of iNKT cells (12). Thus, TRAF3 plays distinct and pivotal roles in regulating the development and function of different subsets of immune cells.
Myeloid cells, including granulocytes, monocytes, macrophages and dendritic cells (DCs), are crucial determinants of innate immunity and inflammation, and also play essential roles in antigen presentation as well as the effector phase of adaptive immunity. These cells constitutively or inducibly express a number of receptors of the TNF-R, TLR, NLR, and RLR families, whose signals are regulated by TRAF3 (1, 2). Although in vitro evidence indicates that TRAF3 is required for TLR-induced type I interferon (IFN) production (13, 14) and for CD40-induced IL-12 production in macrophages (15), the in vivo functions of TRAF3 in myeloid cells remain unclear. In the present study, we generated TRAF3flox/floxLysM+/Cre myeloid cell-specific TRAF3-deficient mice (M-TRAF3−/−) to evaluate the functions of TRAF3 in innate immunity and inflammation mediated by myeloid cells. Cre expression driven by the lysozyme M promoter mediates deletion of TRAF3 from neutrophils, eosinophils, basophils, monocytes, macrophages, and monocyte-derived DCs but not plasmacytoid DCs (pDC) (16, 17). We report here that deletion of TRAF3 in myeloid cells resulted in altered systemic responses to injections with LPS (an agonist of TLR4) or polyI:C (an agonist of TLR3), as well as TI and TD antigens. Furthermore, we found that M-TRAF3−/− mice spontaneously developed inflammation, infection, and tumors between 15 and 22 months of age. Taken together, our findings demonstrate obligatory and indispensable roles for myeloid cell TRAF3 in inhibiting inflammation and tumor development.
Materials and methods
Generation of M-TRAF3−/ − mice
TRAF3flox/flox mice were generated as previously described (7). The TRAF3flox/flox line was backcrossed with C57BL/6J (B6) mice (Jackson Laboratory) for >9 generations to generate TRAF3flox/flox mice on the B6 genetic background. These mice were subsequently bred with B6 mice transgenic for LysM-driven Cre expression (Jackson Laboratory, stock number: 4781). TRAF3+/floxLysM+/Cre mice were backcrossed with TRAF3flox/flox B6 mice to generate TRAF3flox/floxLysM+/Cre (M-TRAF3−/−) mice. Mouse tails were screened by genomic PCR using primer sets (FC3 + BT6) (7), (Lys-Com + Lys-WT), and (Lys-Com + Lys-Cre) (16) as described. Deletion of exons 1 and 2 of the TRAF3 gene in peritoneal macrophages was detected by genomic PCR using primers U7 and BT6 as previously described (7). All experimental mice for this study were subsequently produced by breeding of TRAF3flox/flox mice with TRAF3flox/floxLysM+/Cre mice, and TRAF3flox/flox littermates (LMC) were used as controls for all experiments. All mice were kept in specific pathogen-free conditions in the Animal Facility at Rutgers University, and were used in accordance with NIH guidelines and under an animal protocol (Protocol # 08-048) approved by the Animal Care and Use Committee of Rutgers University.
Antibodies and reagents
Polyclonal rabbit Abs to TRAF1 (N19), TRAF3 (H122), TRAF6 (H274), and RelB were from Santa Cruz Biotechnology (Santa Cruz, CA). Polyclonal rabbit Ab to TRAF2 was from Medical and Biological Laboratories (Nagoya, Japan). Fluorescein isothiocyanate (FITC), phycoerythrin (PE), or Cy5 labeled Abs against mouse CD3, CD4, CD8, CD45R (B220), CD19, IgM, CD11b, Ly6C, Ly6G, CD115, F4/80, Siglec-F, CD68, CD11c, NK1.1, CD49b, CD21, CD23, CD5, CD44, CD62L, CD69, CD80, and MHC class II were purchased from eBioscience (San Diego, CA). Anti-mouse IL-6, IL-12, and TNF-α ELISA Ab pairs were also purchased from eBioscience. Anti-mouse IL-1β and IL-10 ELISA Ab pairs were also purchased from R&D (Minneapolis, MN). Polyclonal rabbit Abs against total or phosphorylated IRF3, p38, ERK, JNK, IκBα, Akt, and NF-κB2 were from Cell Signaling Technology (Beverly, MA). Anti-actin Ab was from Chemicon (Temecula, CA). HRP-labeled secondary Abs were from Jackson ImmunoResearch Laboratories, Inc. (West Grove, PA). Alkaline phosphatase (AP)-conjugated polyclonal goat Abs specific for mouse Ig isotypes were from Southern Biotechnology Associates (Birmingham, AL). Neutrophil purification kits were from Miltenyi Biotec Inc. (Auburn, CA). Tissue culture supplements including stock solutions of sodium pyruvate, L-glutamine, non-essential amino acids, and HEPES (pH 7.55) were from Invitrogen (Carlsbad, CA). DNA oligonucleotide primers were obtained from Integrated DNA Technologies (Coralville, IA). AP substrates were purchased from Sigma-Aldrich Corp. (St. Louis, MO).
Flow cytometry
Single cell suspensions were made from the spleen, bone marrow (BM), and peritoneal lavage. Immunofluorescence staining and FACS analyses were performed as previously described (7, 8). Erythrocytes from spleen were depleted with ACK lysis buffer. Cells (1×106) were blocked with rat serum and FcR blocking Ab (2.4G2), and incubated with various Abs conjugated to FITC, PE, PerCP, or Cy5 for multiple color fluorescence surface staining. Analyses of cell surface markers included antibodies to CD3, CD4, CD8, CD45R (B220), CD19, IgM, CD11b, Ly6C, Ly6G, CD115, F4/80, Siglec-F, CD68, CD11c, CD317, NK1.1, CD49b, CD21, CD23, CD5, CD44, CD62L, CD69, CD80, and MHC class II. Listmode data were acquired on a FACSCalibur (Becton Dickinson, Mountain View, CA) using Cell Quest software. The results were analyzed using FlowJo software (TreeStar, San Carlos, CA). FSC/SSC gating was used to identify live cells.
Culture of BM-derived macrophages (BMDMs) and peritoneal exudate macrophages (PEMs)
Bone marrow cells were harvested from 7–10 week old littermate control (LMC) or M-TRAF3−/− mice. BMDMs were prepared by culturing BM cells in complete RPMI-1640 medium (Invitrogen) supplemented with 20% conditioned medium from L929 cells overexpressing M-CSF for 7 days as described (18–20). For preparation of PEMs, 7–10 week old LMC or M-TRAF3−/− mice were injected intraperitoneally (i.p.) with 3 ml of 4% thioglycollate (Becton Dickinson), and cells were harvested by peritoneal lavage on day 4 post injection as described (18). The cells were washed, macrophages were allowed to adhere to the tissue culture plates for two hours, and non-adherent cells were removed.
Preparation of thioglycollate-elicited peritoneal neutrophils
7–10 week old LMC or M-TRAF3−/− mice were injected i.p. with 3 ml of 4% thioglycollate (BD), and cells were harvested by peritoneal lavage at 18 h post injection. Neutrophils were purified from peritoneal cells using anti-Ly-6G-Biotin and anti-Biotin magnetic beads following the manufacturer’s protocol (Miltenyi). Purified neutrophils were resuspended in RPMI-1640 medium containing 5% FCS, and aliquoted for stimulation.
TLR4 signaling
Before stimulation with LPS, BMDMs or PEMs were cultured in 2.5% FCS medium for 2 hours. BMDMs, PEMs or neutrophils were stimulated with 100 ng/ml LPS. Total protein lysates were prepared at different time points as previously described (21) for measurements of early signaling events by immunoblot analysis. Total cellular RNA was extracted at different time points for measurement of cytokine transcript levels by quantitative real time PCR (RT-qPCR) using Taqman assay. Culture supernatants were collected at different time points for measurements of cytokine protein levels by ELISA.
Taqman assays of Ifnb, Ifna4, Il12a, Il6, and Tnfa transcripts
Total cellular RNA was extracted using TRIzol reagent (Invitrogen, Carlsbad, CA) according to the manufacturer’s protocol. cDNA was prepared from RNA using the High Capacity cDNA Reverse Transcription Kit (Applied Biosystems, Foster City, CA). Quantitative real-time PCR (qPCR) was performed using TaqMan Gene Assay kit (Applied Biosystems) as described (22). TaqMan primers and probes (FAM-labeled) specific for individual mouse cytokines were used in the PCR reaction to detect Ifnb, Ifna4, Il12a, Il6, or Tnfa mRNA. Each reaction also included primers and a probe (VIC-labeled) specific for mouse Actb (b-actin) mRNA, which served as an endogenous control. Reactions were performed on a 7500 Fast Real-Time PCR System (Applied Biosystems). Relative mRNA expression levels of cytokines were analyzed using Sequencing Detection Software (Applied Biosystems) and the comparative Ct (ΔΔCt) method following the manufacturer’s procedures.
For each cytokine assay, the calibrator sample was the one with lowest detectable RNA level (highest Ct value). Duplicate PCR reactions were performed for each biological sample.
Cytokine ELISA
Concentrations of IL-6, IL-12, and TNFα in culture supernatants or mouse sera were determined by quantitative ELISA using cytokine-specific coating Abs and biotinylated detection Abs (eBioscience) as previously described (10, 22). Mouse serum levels of IL-10 and IL-1β were analyzed by ELISA using cytokine-specific coating Abs and biotinylated detection Abs (R&D) as previously described (10, 22). Levels of IFN-β in mouse sera were measured using the VeriKine-HS™ Mouse Interferon Beta Serum ELISA Kit (PBL Assay Science, Piscataway, NJ) following the manufacturer’s protocol.
In vivo responses to challenges with LPS or polyI:C
Age- and gender- matched 8–12 week old LMC and M-TRAF3−/− mice were injected i.p. with LPS (E. coli 0127:B8, Sigma; 300 μg LPS/20g body weight) or polyI:C (InvivoGen, 200 μg polyI:C/20g body weight). Sera were collected at 2 h and 6 h post injection, and cytokine levels in sera were analyzed by ELISA as described above.
Immunoblot analysis
Total protein lysates were prepared as described (21). Proteins were separated by SDS-PAGE and immunoblotted with antibodies to phosphorylated (P-) or total IRF3, p38, ERK, JNK, Akt, IκBα, NF-κB2, RelB, TRAF3 and actin. Immunoblot analysis was performed using antibodies as previously described (8, 21). Images of immunoblots were acquired using a low-light imaging system (LAS-4000 mini, FUJIFILM Medical Systems USA, Inc., Stamford, CT) (8, 21).
Immunizations and Ig ELISAs
Basal serum levels of various Ig isotypes in naïve 8–12 week old LMC and M-TRAF3−/− mice were analyzed by ELISA as previously described (7). For TI antibody responses, age- and gender- matched 8–12 week old LMC and M-TRAF3−/− mice were immunized i.p. with 50 μg of trinitrophenyl (TNP)-Ficoll (Biosource Technologies, Vacaville, CA), and sera were collected on day 7 after immunization. For TD antibody responses, age- and gender- matched 8–12 week old LMC and M-TRAF3−/− mice were injected i.p. with 100 μg of TNP-KLH (Biosource Technologies) in an equal volume of Imject Alum (Thermo scientific, Rockford, IL), and sera were collected on day 7 after immunization. Serum TNP-specific Ig isotypes were measured by ELISA as previously described (7). Plates were read on a Versamax plate reader (Molecular Devices, Sunnyvale, CA) and results analyzed by using SoftMax Pro 4.0 software as described (7).
Mouse disease monitoring and histology
Mice were monitored daily for signs of illness including weight loss, labored breathing, hunched posture, and paralysis or spontaneous tumor formation indicated by enlarged lymph nodes or abdomen (8). Necropsy and hematoxylin-eosin staining of formalin-fixed paraffin embedded tissues were performed to assess the presence of phenotypic abnormalities as described (7, 8, 23–28). Bright field micrographs of stained sections were taken using a microscope (Olympus BX-51, Olympus America Inc., Center Valley, PA).
Mouse cytokine protein array analyses
Sera were collected from 15–22 month old LMC and diseased M-TRAF3−/− mice. Serum levels of cytokines and chemokines were measured using a Mouse Cytokine Array Panel A kit (R&D, Minneapolis, MN) following the manufacturer’s instructions. Images of the blots were acquired, and quantitative analyses of cytokine or chemokine spots were performed using a low-light imaging system (LAS-4000 mini, FUJIFILM Medical Systems USA, Inc., Stamford, CT) (8, 21).
Statistics
Statistical analyses were performed using Prism software (GraphPad, La Jolla, CA). Survival curves were generated using the Kaplan-Meier method, and were compared using a log-rank (Mantel-Cox) test to determine whether differences are significant. For direct comparison of cytokine or Ig isotype levels between LMC and M-TRAF3−/− mice, statistical significance was determined with the unpaired t test for two-tailed data. P values less than 0.05 are considered significant, and P values less than 0.001 are considered highly significant.
Results
Validation of M-TRAF3−/− mice
Previous in vitro studies indicated that TRAF3 regulates type I IFN and pro-inflammatory cytokine production in myeloid cells (13, 14). However, the in vivo functions of TRAF3 in myeloid cells had not been determined. To address this issue, we generated myeloid cell-specific TRAF3-deficient mice by crossing TRAF3flox/flox mice with mice that express Cre under the control of endogenous lysozyme M regulatory elements (LysM-Cre mice), which allows the specific deletion of floxed genes in myeloid cells (16). Progeny were born at expected Mendelian frequencies with no developmental abnormalities noted, and matured and bred normally.
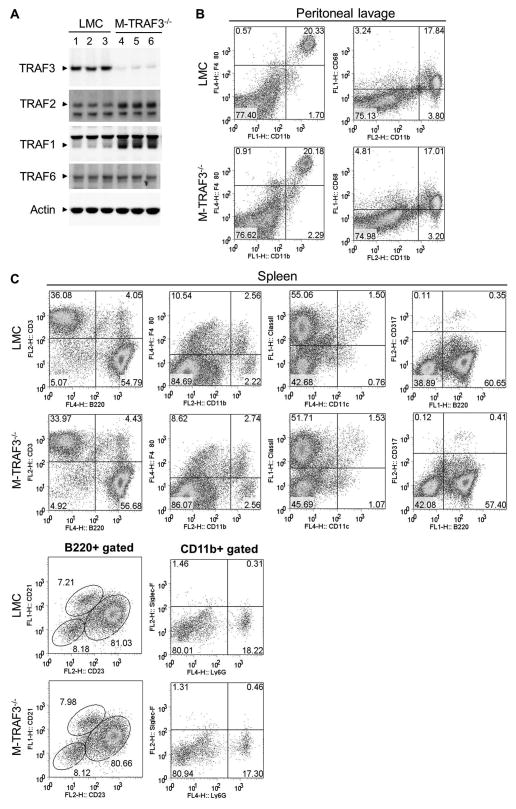
LysM-driven Cre expression has been shown to induce specific and highly efficient deletion of loxP-flanked gene segments in mature neutrophils and macrophages with a higher deletion efficiency in neutrophils (16, 17, 29). In contrast, LysM-Cre-mediated deletion does not occur in T cells, B cells, NK cells, and pDCs, despite the presence of LysM activity in a small population of the hematopoietic stem cells (30). Consistent with previous studies, we verified highly efficient deletion of the Traf3 gene and a corresponding loss of TRAF3 protein (80~90% reduction) in peritoneal macrophages and BMDMs prepared from M-TRAF3−/− mice as determined by genomic PCR and Western blot analysis (Fig. 1A and data not shown). No deletion of Traf3 was observed in splenic T and B cells of M-TRAF3−/− mice (data not shown). Interestingly, we found that TRAF1 and TRAF2 protein levels were modestly increased in TRAF3-deficient macrophages (Fig. 1A). In contrast, TRAF6 protein levels were unchanged. We previously had observed modestly increased TRAF1 and TRAF2 protein levels in TRAF3−/− B cells and T cells (7, 10). These findings raise the possibility that increased TRAF1 and TRAF2 may partially compensate for the loss of TRAF3 in these cell types. Together, these data validated TRAF3flox/floxLysM+/Cre mice as myeloid cell-specific TRAF3-deficient (M-TRAF3−/−) mice.
Figure 1. Normal lymphocyte and myeloid cell populations in young adult M-TRAF3−/− mice.
TRAF3flox/flox littermate control (LMC) and M-TRAF3−/− mice analyzed were 8 to 12 weeks old. (A) Verification of TRAF3 deletion in BMDMs by Western blot analysis. Total cellular proteins were prepared from BMDMs derived from 3 pairs of LMC and M-TRAF3−/− mice. Proteins were immunoblotted for TRAF3, followed by TRAF2, TRAF1, TRAF6 and actin. (B) Representative FACS profiles of peritoneal lavage prepared from LMC and M-TRAF3−/− mice. Cells were stained with fluorochrome-conjugated antibodies specific for CD11b, F4/80, and CD68, and then analyzed by a FACSCalibur. Peritoneal macrophages are identified as CD11b+F4/80+CD68+. (C) Representative FACS profiles of splenocytes prepared from LMC and M-TRAF3−/− mice. Cells were stained with fluorochrome-conjugated antibodies specific for B220, CD3, CD11b, F4/80, CD11c, MHC ClassII, CD21, CD23, Ly6G, Siglec-F, and CD317 (PDCA-1), and then analyzed by a FACSCalibur. FACS profiles were scatter-gated on live cells. Gated cell populations include: B cells, B220+CD3−; T cells, CD3+B220−; red pulp macrophages, CD11b+F4/80+; cDCs, CD11c+MHC ClassII+; follicular (FO) B cells, B220+CD21IntCD23+; marginal zone (MZ) B cells, B220+CD21+CD23Int; neutrophils, CD11b+Ly6G+Siglec-F-; pDCs, B220+CD317 (PDCA-1)+. Similar results were observed in 4 additional experiments.
Young adult M-TRAF3−/− mice have normal populations of lymphoid and myeloid cells
We previously reported that TRAF3 regulates mature B cell homeostasis in secondary lymphoid organs (7). To investigate whether TRAF3 is involved in the maturation and homeostasis of myeloid cells, we first examined the size and cell numbers of lymphoid organs of 8–12 week old M-TRAF3−/− and TRAF3-sufficient littermate control mice (TRAF3flox/flox, LMC). We found that M-TRAF3−/− mice had normal sized spleens, lymph nodes, and thymi, and also had normal numbers of cells in the BM and peritoneum (Supplementary Table I and data not shown). We next used flow cytometry to characterize lymphocyte and myeloid cell populations in the BM, spleen, and peritoneum. Our data demonstrated that M-TRAF3−/− and LMC mice had similar proportions and numbers of splenic follicular and marginal zone B cell subsets and CD4 and CD8 T cells. This was also true for comparisons of granulocytes, monocytes and macrophages in the BM, spleen, and peritoneal lavage (Fig. 1B, 1C, and Supplementary Table I). Interestingly, TRAF3−/− and LMC CD11b+F4/80+ macrophages in the spleen and peritoneal cavity also expressed comparable levels of MHC class II, CD80 and CD86, suggesting that macrophages were not activated as a result of TRAF3 deficiency in mice of this age (data not shown). In addition, following i.p. injection of thioglycollate, the numbers of neutrophils (analyzed at 2, 4, 6, 12 or 18 h post injection) and macrophages (analyzed at day 3 or day 4 post injection) recruited to the peritoneal cavity were also comparable between M-TRAF3−/− and LMC mice (data not shown). Collectively, our findings indicate that specific ablation of TRAF3 in myeloid cells did not affect maturation, homeostasis or migration of macrophages and neutrophils and, as expected, had no effects on T and B cells.
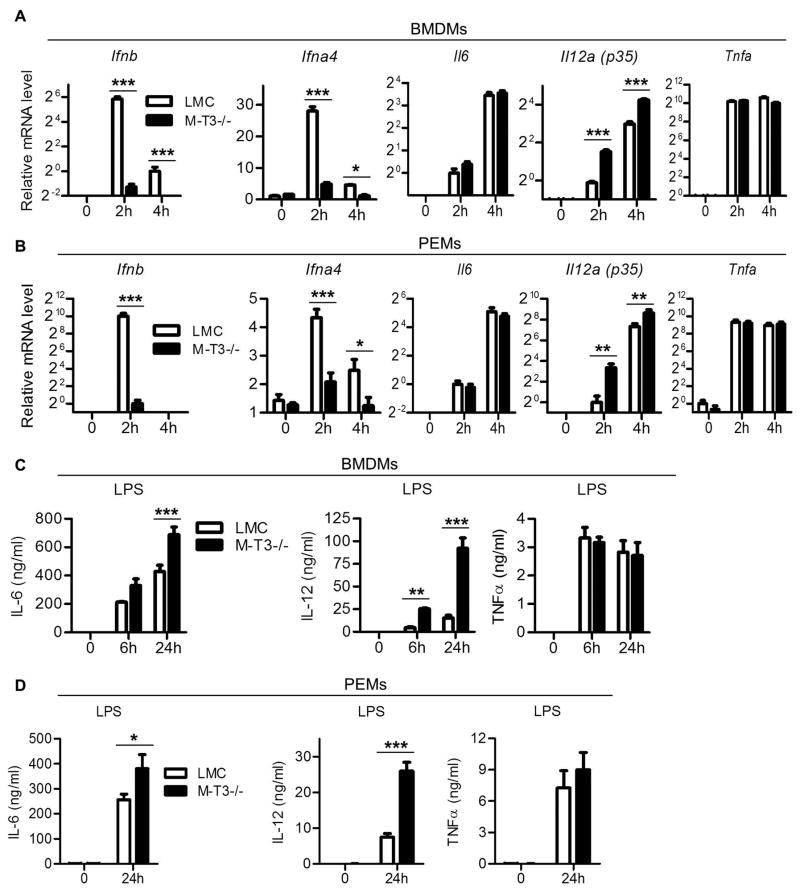
Altered cytokine production in TRAF3−/− BMDMs and PEMs in response to LPS stimulation
It was shown previously that LPS-induced type I IFN production is abolished but IL-12 production is enhanced in BMDMs derived from chimeric mice reconstituted with TRAF3−/− fetal liver cells (13, 14). We therefore analyzed LPS-induced cytokine production in BMDMs and PEMs derived from M-TRAF3−/− mice by RT-qPCR and ELISA. Consistent with published studies, we found that LPS-induced expression of Ifnb and Ifna4 was almost abolished in BMDMs and PEMs derived from M-TRAF3−/− mice (Fig. 2A and 2B). Interestingly, production of IL-12 was enhanced by TRAF3 deficiency at both the transcript and protein levels (Fig. 2A–2D). In addition, although transcription of Il6 was not changed (Fig. 2A and 2B), secretion of IL-6 was significantly increased in TRAF3−/− BMDMs and PEMs (Fig. 2C and 2D). In contrast, LPS-induced production of TNF-α in either cell population was not affected by TRAF3 deletion (Fig. 2A–2D). Taken together, our results showed that in response to LPS stimulation, TRAF3-deficient macrophages exhibited alterations in expression of some cytokines but not others. These studies validated M-TRAF3−/− mice as a suitable model to explore the in vivo functions of myeloid cell TRAF3.
Figure 2. Impaired type I IFN but enhanced IL-6 and IL-12 production in TRAF3−/− macrophages in response to LPS stimulation.
(A and B) LPS-induced mRNA expression of cytokines in macrophages. BMDMs (A) or PEMs (B) derived from M-TRAF3−/− and LMC mice (7–10 week-old) were cultured in the absence or presence of 100 ng/ml of LPS for 2 or 4 hours. RNA was extracted, and real-time PCR was performed using TaqMan primers and probes specific for Ifnb, Ifna4, Il6, Il12a (p35), and Tnfa. Each reaction also included the probe (VIC-labeled) and primers for b-actin mRNA, which served as an endogenous control. Relative mRNA expression levels of each cytokine were analyzed using the Sequence Detection Software (Applied Biosystems) and the comparative Ct method. Graphs depict the results of three independent experiments with duplicate reactions in each experiment (mean ± S.D.). (C and D) LPS-induced secretion of cytokines in macrophages. BMDMs (C) or PEMs (D) derived from M-TRAF3−/− and LMC mice (7–10 week-old) were cultured in the absence or presence of 100 ng/ml of LPS for indicated time periods. The levels of IL-6, IL-12 and TNFα in culture supernatants were analyzed by ELISA. Graphs depict the results of three independent experiments with duplicate samples in each experiment (mean ± S.D.). *, significantly different between LMC and M-TRAF3−/− (t test, p < 0.05); **, very significantly different between LMC and M-TRAF3−/− (t test, p < 0.01); ***, highly significantly different between LMC and M-TRAF3−/− (t test, p < 0.001).
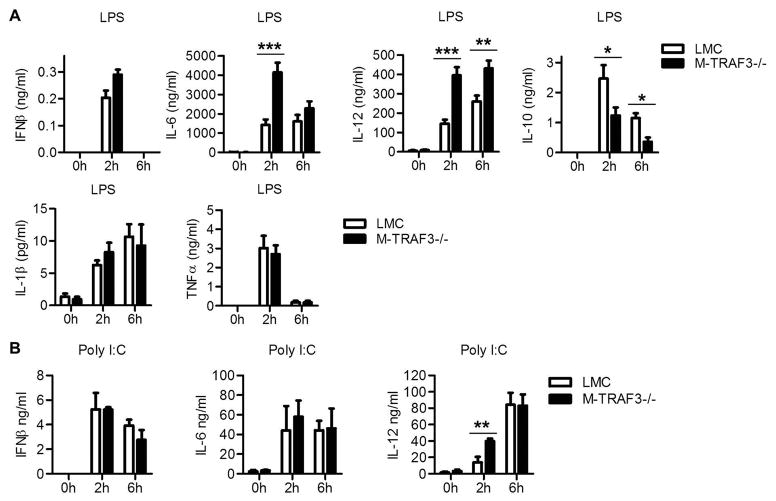
Enhanced pro-inflammatory responses in M-TRAF3−/− mice challenged with LPS or PolyI:C
Myeloid cells provide the first line of defense against bacterial and viral infections by producing type I IFN and pro-inflammatory cytokines. In light of our in vitro evidence for TRAF3 regulation of cytokine production in BMDMs and PEMs, we investigated the in vivo responses of M-TRAF3−/− mice inoculated with LPS or PolyI:C, which mimic aspects of bacterial and viral infections, respectively. We measured serum levels of IFN-β as well as pro-inflammatory and anti-inflammatory cytokines at different times after injection. Our results demonstrated that in response to LPS, serum levels of the pro-inflammatory cytokines TNFα and IL-1β were comparable in M-TRAF3−/− and LMC mice (Fig. 3A). In contrast to the reduced in vitro inducibility of Ifnb observed in LPS-simulated BMDMs and PEMs of M-TRAF3−/− mice, serum levels of IFN-β were not decreased in M-TRAF3−/− mice inoculated with LPS or polyI:C (Fig. 3A). The normal in vivo production of IFN-β may reflect the lack of TRAF3 deletion in pDCs, which are the most potent producers of type I IFN following TLR ligation. Interestingly, levels of the pro-inflammatory cytokines IL-6 and IL-12 in sera of M-TRAF3−/− mice were elevated at 2 h, and IL-12 levels were also increased at 6 h post LPS injection (Fig. 3A). Similarly, serum levels of IL-12 were also significantly elevated in M-TRAF3−/− mice at 2 h post injection with polyI:C (Fig. 3B). In contrast, serum levels of the anti-inflammatory cytokine IL-10 were markedly decreased in M-TRAF3−/− mice compared to LMC mice at 2 and 6 h post LPS injection (Fig. 3A). These results suggest that TRAF3 inactivation in myeloid cells alters cytokine production profiles to favor pro-inflammatory responses following in vivo challenges with LPS or polyI:C.
Figure 3. In vivo cytokine production in response to injection with LPS or polyI:C.
Gender and age-matched M-TRAF3−/− and LMC mice (8–12 week-old) were i.p. injected with LPS (300 μg LPS/20g body weight, n=9 for each group, A) or polyI:C (200 μg polyI:C/20g body weight, n=4 for each group, B), and sera were collected at 2 and 6 h post-injection. Serum levels of IFN-β, IL-6, IL-12, IL-10, IL-1β, and TNFα were measured by ELISA. *, significantly different between LMC and M-TRAF3−/− (t test, p < 0.05); **, very significantly different between LMC and M-TRAF3−/− (t test, p < 0.01); ***, highly significantly different between LMC and M-TRAF3−/− (t test, p < 0.001).
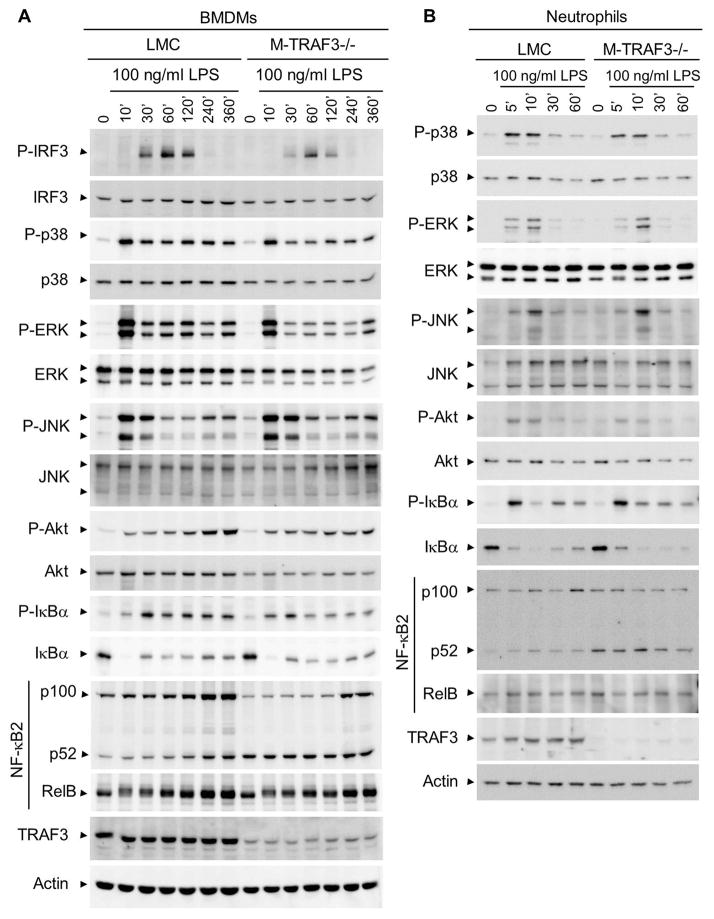
Proximal signaling events downstream of LPS/TLR4 engagement in TRAF3-deficient BMDMs and neutrophils
To understand how TRAF3 deficiency affects LPS-induced cytokine production in myeloid cells, we investigated proximal signaling events following TLR4 engagement by LPS in TRAF3-deficient BMDMs and neutrophils. Purified thioglycollate-elicited neutrophils and BMDMs were stimulated with LPS, and total cellular proteins were prepared from both cell types at different time points. Phosphorylation of proximal signaling components of TLR4 including IRF3, p38, ERK, JNK, Akt, and IκBα were examined by immunoblot analyses. We found that LPS-induced phosphorylation of IRF3, the key transcription factor driving type I IFN expression, was markedly reduced in TRAF3−/− BMDMs (Fig. 4A). We did not detect any induction of IRF3 phosphorylation by LPS in LMC or TRAF3−/− neutrophils (data not shown). We found that LPS-induced phosphorylation of p38, ERK, JNK, and Akt was normal in TRAF3−/− BMDMs and neutrophils (Fig. 4A and 4B). Similarly, activation of the classical NF-κB1 pathway was not affected by TRAF3 deletion in either cell type as measured by phosphorylation and degradation of IκBα after stimulation with LPS (Fig. 4A and 4B). We previously found that TRAF3 deficiency resulted in constitutive NF-κB2 activation in B cells, leading to prolonged B cell survival (7, 8). We therefore compared NF-κB2 processing in TRAF3−/− and LMC BMDMs and neutrophils. Interestingly, in the absence of stimulation, TRAF3-deficient cells exhibited constitutive processing of NF-κB2 from the inactive precursor p100 to the active p52, which was as robust as that observed in LMC cells after stimulation with LPS (Fig. 4A and 4B). However, in contrast to TRAF3-deficient B cells, constitutive NF-κB2 processing did not result in prolonged survival or decreased apoptosis in TRAF3−/− BMDMs or neutrophils (data not shown). Collectively, our findings indicate that TRAF3 deficiency leads to constitutive activation of NF-κB2 in both BMDMs and neutrophils, and specifically impairs LPS-induced activation of IRF3 in BMDMs, thereby modulating their cytokine production.
Figure 4. Altered signaling events in TRAF3−/− BMDMs and neutrophils in response to LPS stimulation.
BMDMs (A) or thioglycollate elicited peritoneal neutrophils (B) prepared from M-TRAF3−/− and LMC mice (8–12 week-old) were stimulated with 100 ng/ml of LPS for indicated time periods. Total protein lysates were prepared, and signaling events of TLR4 were analyzed by immunoblot analysis. Proteins were immunoblotted for phosphorylated (P-) or total IRF-3, p38, ERK, JNK, Akt, IκBα, followed by NF-κB2 (p100 and p52), RelB, TRAF3 and actin. Results shown are representative of 3 independent experiments.
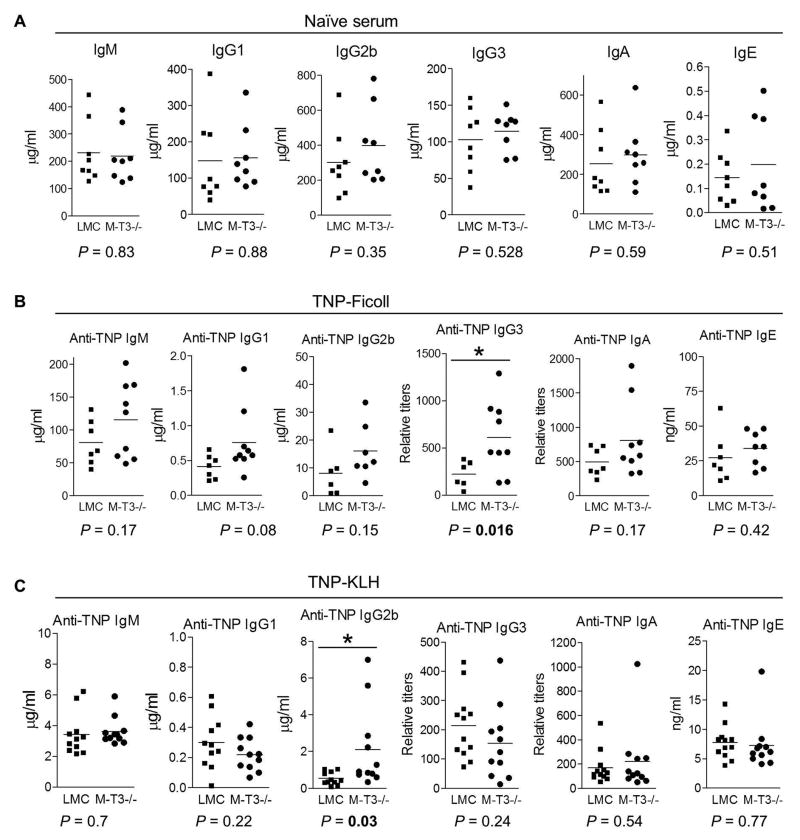
Enhanced TI and TD IgG responses in M-TRAF3−/− mice
In addition to serving as primary players in innate immunity and inflammation, myeloid cells also play important roles in antigen presentation to activate adaptive immunity. We therefore measured basal Ig isotype levels in sera from 8–12 week old M-TRAF3−/− and LMC mice, and found that the levels of IgM, IgG1, IgG2b, IgG3, IgA and IgE were similar in both cohorts (Fig. 5A). Following immunization with the TI Ag, TNP-Ficoll, M-TRAF3−/− mice tended to have slightly higher levels of all TNP-specific isotypes than LMC mice although only IgG3 differences were significant (Fig. 5B). In contrast, following immunization with the TD Ag, TNP-KLH, only TNP-specific IgG2b levels were significantly increased in sera of M-TRAF3−/− as compared to LMC mice (Fig. 5C). Collectively, these results indicate that while baseline levels of serum immunoglobulins were similar in M-TRAF3−/− and LMC mice, the responses to TI and TD antigens were altered in M-TRAF3−/− mice.
Figure 5. Altered antibody responses in M-TRAF3−/− mice.
LMC and M-TRAF3−/− mice analyzed were 8 to 12 weeks old. (A) Basal serum titers of Ig isotypes. Sera from naïve LMC and M-TRAF3−/− mice (n=8 for each group) were tested for IgM, IgG1, IgG2b, IgG3, IgA, and IgE levels by ELISA. (B) TI antibody responses. LMC and M-TRAF3−/− mice (n=9 for each group) were immunized with the TI Ag TNP-Ficoll, and sera were collected on day 7 after immunization. Serum titers of anti-TNP IgM, IgG1, IgG2b, IgG3, IgA, and IgE were analyzed by ELISA. (C) TD antibody responses. LMC and M-TRAF3−/− mice (n=12 for each group) were immunized with the TD Ag TNP-KLH in Alum. Sera were collected on day 7 after immunization. Serum titers of anti-TNP IgM, IgG1, IgG2b, IgG3, IgA, and IgE were measured by ELISA. Multiple serial dilutions of each serum sample were tested to ensure that the readout is within the linear range of the assay. *, significantly different from LMC (t-test, P < 0.05).
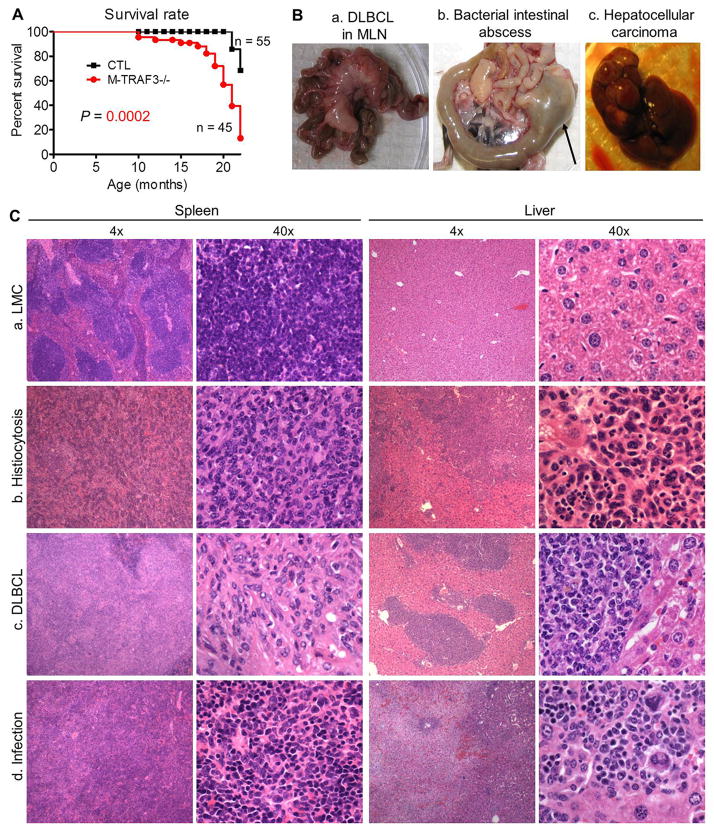
Spontaneous inflammation, infection, and tumor development in aging M-TRAF3−/− mice
In light of understandings that elevated pro-inflammatory cytokines contribute to inflammatory diseases, we hypothesized that M-TRAF3−/− mice should be predisposed to inflammation. We thus monitored the health of aging M-TRAF3−/− and LMC mice. We first noticed that beginning around 10 months of age, mortality of M-TRAF3−/− mice was greatly accelerated over that of LMC (Fig. 6A). Histopathological studies were performed on 22 M-TRAF3−/− mice of 15–22 months old. We found that 15 out of the 22 (68.2%) mice displayed inflammation, infection, or tumors involving multiple organs, features that were not observed in age-matched LMC mice (Table I and Fig. 6B). Twelve mice developed tumors, including two cases of histiocytic sarcomas (histiocytic neoplasms, tumors of a type of tissue-resident macrophages), one hepatocellular adenoma, and nine B cell lymphomas (Table I). Lymphomas observed in M-TRAF3−/− mice were diffuse large B cell lymphomas (DLBCLs) or follicular lymphomas (FLs). Six M-TRAF3−/− mice displayed inflammation involving multiple organs, including the liver, gastrointestinal tract (GI tract), lung, kidney, pancreas, and heart (Table I). Three M-TRAF3−/− mice had infections in the intestine/colon, liver, and lung (Table I). Notably, seven M-TRAF3−/− mice had internal hemorrhages and two had blistering (Table I). Interestingly, individual M-TRAF3−/− mice often had more than one type of pathology. Examples include B cell lymphoma and lung inflammation, pancreatitis and hepatocellular adenoma, bacterial infection and hemorrhagic liver. Together, our findings indicate that specific ablation of TRAF3 in myeloid cells contributed to spontaneous development of different types of tumors, inflammation, and infection.
Figure 6. Gross and histopathological features of M-TRAF3−/− mice with spontaneous tumor, inflammation or infection.
(A) Accelerated mortality of M-TRAF3−/− mice. Survival curves of LMC and M-TRAF3−/− mice were generated using the Kaplan-Meier method. P<0.001 as determined by the Mantel-Cox log-rank test. (B) Representative images of affected organs in diseased M-TRAF3−/− mice. a, Massively enlarged mesenteric lymph node (MLN) in a mouse with DLBCL (mouse ID: 237-2). b, GI tract and MLN of a mouse with bacterial infection and inflammation (mouse ID: 228-5). Arrow indicates the large bacterial intestinal abscess. c, Liver of a mouse with hepatocellular adenoma (mouse ID: 237-4). (C) Representative micrographs of the spleen and liver of diseased M-TRAF3−/− mice. Sections of the spleen and liver were stained with hematoxylin and eosin, and representative micrographs of LMC and M-TRAF3−/− mice are shown for comparison. a, Normal tissues from a LMC mouse. b, Mouse (ID: 237-5) with extensive histiocytosis and increased erythroid activity in the spleen and areas of pure histiocytosis in the liver. c, Mouse (ID: 233-5) with DLBCL showing marked enlargement of the splenic white pulp by tumor cells and large perivascular infiltrates with tumor cells in the liver. d, Mouse (ID: 274-12) with infection showing inflammation and necrotic areas in the liver and marked red pulp hyperplasia of myeloid and erythroid elements in the spleen.
Table I.
Summary of histological observations of M-TRAF3−/− mice at the age of 15–22 months
| Mice examined (n=22) | Number | Organs involved |
|---|---|---|
| Tumor | ||
| Histiocytic sarcoma | 2 | Spleen, liver |
| Hepatocellular adenoma | 1 | Liver |
| B cell lymphoma (DLBCL or FL) | 9 | Spleen, CLN, MLN, liver |
| Inflammation | 6 | Liver, GI tract, lung, kidney, pancreas, heart |
| Infection | 3 | GI tract, liver, lung |
| Unknown | ||
| hemorrhage | 7 | |
| blister | 2 | |
| Normal | 7 | |
Histologic diagnoses were made based on established criteria (23–28). Mice with DLBCL and FL were diagnosed histologically using criteria outlined in a consensus nomenclature of mouse lymphoid neoplasms (23). Malignancies of histiocytes (histiocytic sarcoma) were diagnosed histologically as described (24). Inflammation was diagnosed histologically using criteria of myeloid cell/lymphocyte infiltration in tissues as described (25). Cases diagnosed with inflammatory conditions exhibited expansions of immature myeloid cells, monocytes and granulocytes in tissues outside the bone marrow and often in spleen or liver. Infections were diagnosed with evidence for bacterial or parasitic infection in different tissues, including visualization of bacteria and entamoeba as described (26–28).
Individual mice could have more than one type of pathology. Examples include B cell lymphoma and lung inflammation, pancreatitis and hepatocellular adenoma, bacterial infection and hemorrhagic liver.
Histopathologic features of M-TRAF3−/− mice with spontaneous inflammation, infection or tumor development
Histologically, affected spleens of M-TRAF3−/− mice with spontaneous inflammation, infection or tumor development were most often characterized by a near complete loss of normal architecture (Fig. 6C). In mice with histiocytic sarcomas, tumor cells were identified as the major cell type in the spleen, and nodal areas of pure histiocytosis were also observed in the liver (Fig. 6C). In the mouse with hepatocellular adenoma, the liver was massively occupied by liver cancer cells in association with large cytoplasmic vacuoles (Supplementary Fig. 1). In mice with DLBCL, lymphoma cells were responsible for marked expansion of the splenic white pulp and infiltration of the liver (Fig. 6C). In mice with inflammation, the majority of splenic lymphocytes were replaced with myeloid cells, and granulocyte infiltration was observed in multiple organs, including the liver, intestine, lung, and pancreas (Supplementary Fig. 2 and data not shown). In addition, glomerular damage was observed in the kidneys of mice with inflammation (Supplementary Fig. 2). In mice with infection and inflammation, the splenic architecture was also disrupted by myeloid cells, and the liver contained clustered inflammatory cells, including histiocytes and necrotic areas (Fig. 6C). We observed two cases of bacterial abscesses (Fig. 6B), in which bacteria were clearly identified in micrographs (Supplementary Fig. 3a and 3b). Interestingly, we also detected one case of infection by Entamoeba muris, a strain of commensal protozoan parasite, in cecum (Supplementary Fig. 3c). Taken together, the splenic red pup and white pulp were disrupted in mice with histiocytic sarcoma, DLBCL, inflammation, or infection, and other affected organs also exhibited infiltration with tumor or myeloid cells.
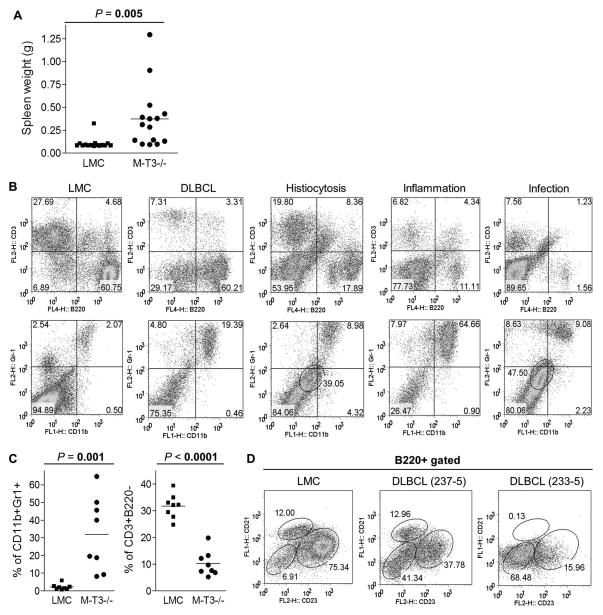
Flow cytometry reveals drastically altered lymphocyte and myeloid cell populations in M-TRAF3−/− mice with spontaneous inflammation, infection or tumors
To detect potential alterations of lymphocyte and myeloid cell populations underlying the above disease conditions, we performed immunophenotypic analyses using flow cytometry. In sharp contrast to the normal spleen size observed in young 8–12 week old M-TRAF3−/− mice or old LMC mice, diseased M-TRAF3−/− mice had greatly enlarged spleens as evidenced by significantly increased spleen weights (Fig. 7A). Similarly, the splenic cell populations in M-TRAF3−/− mice with spontaneous inflammation, infection or tumor development were altered with increased populations of B220−CD3−CD11b+/lowGr-1+/low myeloid cells (Fig. 7B). Consistent with the histological diagnoses, the frequencies of normal B and T cells observed in LMC mice were often diminished in diseased M-TRAF3−/− mice. In mice with histiocytic sarcomas, splenic lymphocytes were mainly replaced by histiocytic tumor cells (B220−CD3−CD11blowGr-1low) (Fig. 7B). In mice with inflammation, most lymphocytes were replaced with a major population of Gr-1+CD11b+ myeloid cells in the spleen (Fig. 7B). In mice with infections, splenic lymphocytes were also replaced with CD11b+Gr-1+ myeloid cells or B220−CD3− CD11blowGr-1low histiocytes (Fig. 7B). In summary, common features of altered cell populations observed in spleens of different individual M-TRAF3−/− mice with spontaneous inflammation, infection or tumor development include increased percentages of CD11b+Gr-1+ myeloid cells and decreased percentages of CD3+B220− T lymphocytes (Fig. 7C). In mice with DLBCL, splenic B lymphoma cells were B220+CD21−CD23− (Fig. 7D). These results suggest that TRAF3 deficiency in myeloid cells promotes inflammation but also greatly compromises the ability of mice to resist infections or control development of hematopoietic and solid tumors.
Figure 7. Abnormal lymphocyte and myeloid cell populations in the spleen of diseased M-TRAF3−/− mice.
(A) Enlarged spleens of M-TRAF3−/− mice (age: 15–22 month-old). The graph depicts spleen weights of age-matched LMC and M-TRAF3−/− mice (n=15 for each group of mice). (B) Representative FACS profiles of splenocytes of age-matched LMC and diseased M-TRAF3−/− mice. Splenocytes were stained with fluorochrome-conjugated B220, CD3, CD11b, Gr-1, CD21 and CD23 Abs, and then analyzed by a FACSCalibur. FACS profiles were scatter-gated on live cells. Gated cell populations include: B cells, B220+CD3−; T cells, CD3+B220−; myeloid cells, CD11b+Gr-1+; a distinct population of histiocytes (gated with a circle in the 3rd and 5th panel): CD11blowGr-1low. M-TRAF3−/− mice shown include: 237-2, DLBCL; 237-5, histiocytosis; 237-1, inflammation; 274-12, infection and inflammation. FACS profiles shown are representative of 2 cases of DLBCL, 2 cases of histiocytosis, 2 cases of inflammation, and 2 cases of infection, respectively. (C) Increased percentage of CD11b+Gr-1+ myeloid cells and decreased percentage of CD3+B220− T cells in diseased M-TRAF3−/− mice. The graphs depict the percentages of CD11b+Gr-1+ myeloid cells or CD3+B220− T cells of age-matched LMC and diseased M-TRAF3−/− mice (n=8 for each group of mice) analyzed by FACS. P values (t-test) between LMC and M-TRAF3−/− mice are shown. (D) Representative FACS profiles of B220+ splenic B cells of M-TRAF3−/− mice with DLBCL. Follicular (FO) B cells are identified as B220+CD21IntCD23+, and marginal zone (MZ) B cells are identified as B220+CD21+CD23Int. The small population (6.91%) of B220+CD21−CD23− observed in LMC are immature and activated B cells, and the major population (41.34% in mouse ID 237-5 and 68.48% in mouse ID 233-5) of B220+CD21−CD23− observed in M-TRAF3−/− mice are predominantly DLBCL cells.
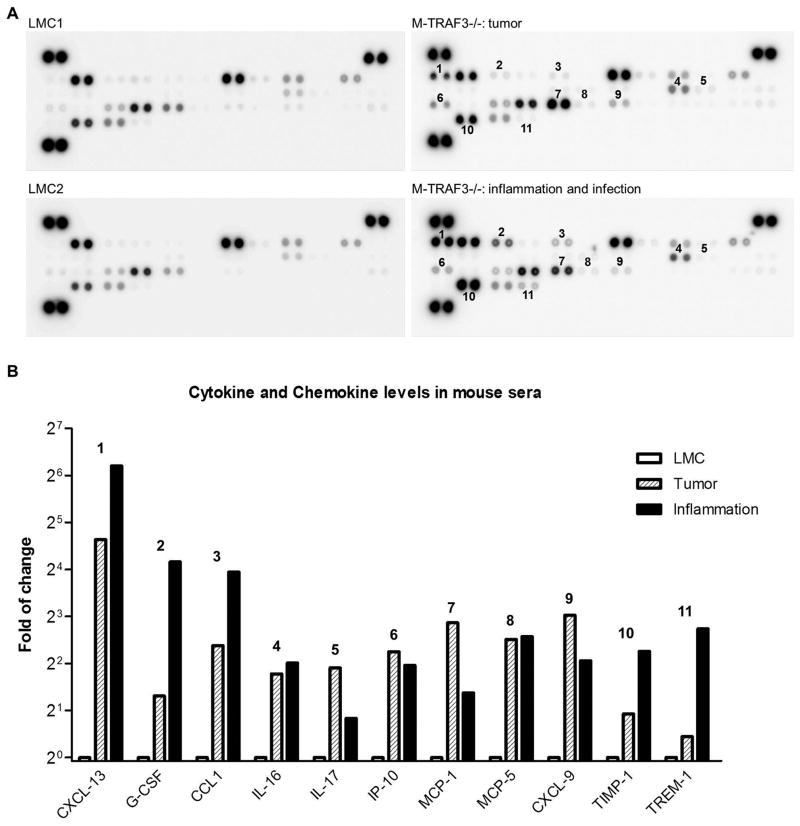
Aberrant production of cytokines and chemokines in diseased M-TRAF3−/− mice
To gain deeper understandings of diseased M-TRAF3−/− mice, we measured the serum levels of 40 cytokines and chemokines using a Mouse Cytokine Array assay kit. Our results demonstrated that M-TRAF3−/− mice with spontaneous tumor development or inflammation/infection exhibited strikingly elevated serum levels of a number of chemokines and cytokines, including CXCL-13, G-CSF, CCL1, IL-16, IL-17, IP-10, MCP-1, MCP-5, CXCL9, TIMP-1, and TREM-1 (Fig. 8). Among these, G-CSF stimulates the bone marrow to produce granulocytes and release them into the blood stream, and also promotes the survival, proliferation, differentiation, and function of neutrophil precursors and mature neutrophils (31, 32). IL-17 is potent in inducing and mediating pro-inflammatory responses (33). Four chemokines, including CCL1, MCP-1 (CCL2), MCP-5 (CCL12), and IP-10 (CXCL10), all act as chemoattractants to recruit monocytes/macrophages, dendritic cells, and lymphocytes to the sites of inflammation (34–40). Interestingly, TREM-1, a triggering receptor expressed on myeloid cells, plays a role in promoting inflammatory responses mediated by monocytes/macrophages and neutrophils (41, 42). These cytokines and chemokines are also implicated in the pathogenesis of various inflammatory diseases and tumor development (26–37), consistent with the phenotypes observed in our M-TRAF3−/− mice. Thus, aberrantly elevated serum levels of these cytokines and chemokines suggest that dysregulation of myeloid cells actively contributes to the pathogenesis of spontaneous inflammation, infection and tumor development observed in aging M-TRAF3−/− mice.
Figure 8. Aberrant serum cytokine and chemokine levels of diseased M-TRAF3−/− mice.
(A) Cytokine and chemokine protein array blots of age-matched LMC and diseased M-TRAF3−/− mice. Cytokines and chemokines in mouse sera were detected using the Mouse Cytokine Array Assay kit (R&D) following the manufacturer’s protocol. In each blot, combined sera of three mice (70 μl serum of each mouse) were used for the cytokine array assay. Sera of M-TRAF3−/− mice with tumor examined include 237-5 (histiocytosis), 228-7 (DLBCL), and 274-11 (FL). Sera of M-TRAF3−/− mice with inflammation and infection examined include 228-5, 237-1, and 274-12. (B) Quantification of cytokine and chemokine levels of diseased M-TRAF3−/− mice measured by the cytokine protein array analyses. Each cytokine or chemokine spots on the blots in (A) were quantitated using a low-light imaging system, and the results presented graphically. The amount of each cytokine or chemokine in diseased M-TRAF3−/− mice (tumor or inflammation) was relative to the mean of the intensity of corresponding LMC1 and LMC2 spots. Each cytokine or chemokine has duplicate detection spots. The graph depicts the fold change (M-TRAF3−/−/LMC) of each cytokine or chemokine (mean). Bold numeric labels indicate the spots that are strikingly different between M-TRAF3−/− mice with tumor or inflammation/infection and LMC in (A) and the corresponding cytokine/chemokine quantitation data in (B).
Discussion
In the present study, we generated and characterized M-TRAF3−/− mice to investigate the in vivo functions of TRAF3 in myeloid cells, central players in innate immunity and inflammation. Our results showed that 8–12 week old M-TRAF3−/− mice had normal lymphocyte and myeloid cell populations in various hematopoietic compartments, demonstrating that LysM-Cre-mediated TRAF3 ablation neither affects the development nor alters the homeostasis of myeloid cells in young adult mice. However, in response to challenge with LPS (a bacterial mimic) or polyI:C (a viral mimic), M-TRAF3−/− mice exhibited an altered profile of cytokine production. Following immunization, M-TRAF3−/− mice displayed elevated T-independent IgG3 as well as T-dependent IgG2b responses. Interestingly, 15–22 month old M-TRAF3−/− mice spontaneously developed chronic inflammation or tumors with some cases showing two pathologic conditions affecting multiple organs. Together, our findings indicate that myeloid cell TRAF3 regulates immune responses and is required for inhibiting inflammation and tumor development in mice.
It has been shown that TRAF3 regulates the homeostasis of multiple cell types through different mechanisms. Specific deletion of TRAF3 from B cells leads to vastly prolonged survival of mature B cells due to constitutive activation of the NIK-NF-κB2 pathway (7, 9). Although ablation of TRAF3 from T cells does not affect the homeostasis of CD4 or CD8 T cells (9, 10), the frequency and number of regulatory T cells (Treg) are increased in T-TRAF3−/− mice and Treg-specific TRAF3−/− mice (10, 11). TRAF3 promotes IL-15-mediated survival and proliferation in invariant natural killer T cells (12). TRAF3 also regulates the development of medullary thymic epithelial cells by affecting the LTβR-NF-κB2 and CD40-NF-κB2 pathways (43). In osteoclast precursor cells, TRAF3 inhibits osteoclast formation by suppressing RANK-NF-κB2 signaling (44). In the present study, we also observed constitutive NF-κB2 activation in TRAF3-deficient macrophages and neutrophils. Interestingly, although the homeostasis of macrophages and neutrophils was normal in young adult M-TRAF3−/− mice, we detected malignant histiocytosis and frequent expansion of CD11b+Gr-1+ myeloid cells in aged M-TRAF3−/− mice. It would thus be interesting to investigate whether and how TRAF3 regulates the survival and/or proliferation of histiocytes and CD11b+Gr-1+ myeloid cells. We speculate that TRAF3 deficiency may gradually lead to prolonged survival or increased proliferation of CD11b+Gr-1+ myeloid cells, causing chronic inflammation in M-TRAF3−/− mice. However, increasing evidence indicates that both inflammation and tumors stimulate the expansion of CD11b+Gr-1+ myeloid-derived suppressor cells (MDSCs) (45–48). Therefore, it remains possible that the increased population of CD11b+Gr-1+ cells observed in our study consists mostly of expanded MDSCs as a consequence of spontaneous inflammation and tumor development.
The importance of TRAF3 in innate immunity is highlighted by the evidence that a variety of viral and bacterial proteins target TRAF3 for inactivation. These include Lb(pro) of foot-and-mouth disease virus, X protein (HBx) of hepatitis B virus, UL36 of herpes simplex virus 1 (HSV-1), YopJ of the Gram- bacterium Yersinia pestis, Tat protein of HIV-1, Gn protein of NY-1 hantavirus, and M protein of severe acute respiratory syndrome coronavirus (1). All these pathogen proteins target TRAF3 and thus inhibit IRF3 phosphorylation and type I IFN production (1). Consistent with these findings, TRAF3 mediates type I IFN production and viral resistance in BMDMs, DCs, and TLR2-reprogrammed macrophages (13, 14, 49–51). In the present study, we verified previous observations that LPS-induced IRF3 phosphorylation and type I IFN production are impaired in TRAF3−/− BMDMs, and extended these findings to PEMs. Paradoxically, in vivo IFN-β production was not affected in young adult M-TRAF3−/− mice injected with LPS or polyI:C, which is likely due to compensation by TRAF3-sufficient plasmacytoid DCs, the most potent producers of type I IFN. Regardless of this, innate immunity is evidently altered by TRAF3 deletion in myeloid cells, as demonstrated by the spontaneous development of inflammation and infection in M-TRAF3−/− mice older than 15 months. Bacterial or entamoeba infections observed in aged M-TRAF −/− mice are most likely caused by opportunistic strains of commensal microbiota (termed “pathobionts”) (52–54), which may trigger TRAF3-dependent signaling pathways via TLRs or NLRs in macrophages, neutrophils and DCs. For example, lipopeptidophosphoglycan of entamoeba has been shown to induce signaling through TLR2 and TLR4, while DNA of entamoeba triggers signaling via TLR9 in macrophages (55). Similarly, muramyl dipeptide and meso-diaminopimelic acid of commensal bacteria stimulate signaling through NOD1 and NOD2, respectively (56, 57). Defective type I IFN production in TRAF3−/− myeloid cells in response to TLR or NLR signaling may occasionally allow colonization of commensal bacteria or entamoeba following opportunistic penetration of protective mucosal and epithelial barriers in the gut. Thus, TRAF3 appears to be required for the proper control of commensal microbiota-triggered innate immune responses and inflammation in myeloid cells.
Myeloid cells not only mediate innate immunity and inflammation, but also act as antigen-presenting cells in adaptive immunity. Here we found that a TI Ag stimulated increased IgG3 response while a TD Ag induced increased IgG2b response in M-TRAF3−/− mice, which may result from elevated levels of pro-inflammatory cytokines in myeloid cells. It has been previously shown that IL-12 enhances TI IgG3 responses (58). IL-6 selectively promotes IgG2b production in germinal center (GC) B cells, and TD IgG2b responses are selectively impaired in IL-6−/− mice (59, 60). Additionally, IL-6 induces the differentiation, expansion, and maintenance of T follicular helper (TFH) cells by inducing Bcl6 expression (61–63). Decreased TFH cell number has been shown to correlate with decreased TD IgG2b response (64). Therefore, elevated levels of IL-12 and IL-6 likely mediate increased TI IgG3 and TD IgG2b responses, respectively. We previously reported that specific deletion of TRAF3 in B cells leads to hypergammaglobulinemia, increased IgM and IgG responses after immunization with a TI Ag, but normal IgG1 responses to a TD Ag (7). In contrast, specific deletion of TRAF3 in T cells causes defective IgG1 responses to a TD Ag due to impaired CD4 helper T cell activation (10). Interestingly, specific ablation of TRAF3 in Treg cells results in moderately enhanced IgG2b responses to a TI Ag and markedly increased IgG1 and IgG2b responses to a TD Ag, due to decreased induction of follicular regulatory CD4 T cells (TFR) after immunization (11). Therefore, TRAF3 deficiency in different immune cell types modulates antibody responses in distinct manners.
One particularly interesting finding of our study is spontaneous tumor development in older M-TRAF3−/− mice. Notably, malignant transformation was not only detected in TRAF3-deficient histiocytes, a type of tissue-resident macrophages, but was also observed in other cell types that are TRAF3-sufficient, including B cells and hepatocytes. In contrast, tumor development is limited to TRAF3-deficient B cells but is not observed in other TRAF3-sufficient cell types in B-TRAF3−/− mice (8). This suggests that TRAF3 signaling pathways in myeloid cells may contribute to tumor surveillance. In this regard, B cells are especially susceptible to genetic alterations due to the unique features of B cell formation and development, which includes V(D)J recombination, somatic hypermutation (SHM) and class switch recombination (CSR) of Ig genes. All of these processes produce double strand DNA breaks (DSBs), which increase the risk of genomic instability in B cells (65–67). Indeed, unlike MZLs and B1 lymphomas observed in B-TRAF3−/− mice that do not involve SHM or CSR (8), the DLBCLs and FLs identified in M-TRAF3−/− mice originate from germinal center (GC) or post-GC B cells, which are undergoing or have gone through GC related events, including SHM and CSR. B cells that have acquired oncogenic alterations during GC passage may escape the compromised tumor surveillance and develop into malignant lymphomas in M-TRAF3−/− mice. Alternatively, the chronic inflammatory environment of M-TRAF3−/− mice, a strong risk factor for cancer, may induce mutations that facilitate malignant transformation of TRAF3-sufficient cells (e.g., hepatocytes and B cells), stimulate tumor growth, and promote angiogenesis to accelerate tumor progression, invasion, and metastasis (68–71). Consistent with this notion, we did detect strikingly elevated levels of 11 cytokines and chemokines in M-TRAF3−/− mice with tumors. Furthermore, chronic inflammation may induce the generation and expansion of CD11b+Gr-1+ MDSCs, which in turn suppress the anti-tumor immune responses mounted by natural killer (NK) cells and CD8 cytotoxic T cells (45–48). MDSCs can also recruit and activate Treg cells to further inhibit anti-tumor responses (45–48). Taken together, the above evidence suggests that TRAF3 is a tumor suppressor gene not only in B cells but also in myeloid cells.
Considering that TRAF3 is employed in signaling by many immune receptors (1, 2), it will be especially interesting to further decode the signaling pathways that lead to spontaneous inflammation and tumor development in M-TRAF3−/− mice. In the absence of infection with pathogens, TLRs and NLRs can be activated by commensal micro-organisms or danger-associated molecular patterns (DAMPs) derived from injured body cells or necrotic cancer cells (56, 57, 72–74). TRAF3 regulates signaling of TLRs through direct interaction with two key adaptor proteins MyD88 and TRIF. Similarly, TRAF3 participates in NOD1 and NOD2 signaling via direct binding to the adaptor protein RIP2 (1, 2). Defective type I IFN production in TRAF3−/− myeloid cells in response to TLR-MyD88, TLR-TRIF, or NOD1-RIP2 signaling may result in compromised tumor surveillance or anti-tumor immunity (1, 2, 73, 75). Meanwhile, enhanced production of pro-inflammatory cytokines in TRAF3−/− myeloid cells mediated by TLR-MyD88 or NOD1/2-RIP2 signaling may exacerbate inflammation (1, 2, 75, 76). Of particular interest, TRAF3 also directly interacts with NLRP12, which inhibits NF-κB2 activation and inflammation (77). Additionally, TRAF3 is a negative regulator of LT-βR signaling (1), which inhibits inflammatory responses by inducing cross-tolerance to TLR4 and TLR9 activation in macrophages (78). Relevant to our mouse model, myeloid cell-specific deletion of MyD88 rescues the spontaneous colitis observed in IL-10−/− mice (79), and TLR4−/−, NOD1−/−, NOD2−/−, RIP2−/−, or NLRP12−/− mice are all more susceptible to colitis and colorectal cancer development when subjected to AOM-DSS treatment (75, 77, 80). Thus, breeding of M-TRAF3−/− mice with conditional knockout mice of MyD88, TRIF, RIP2, or NF-κB2 will help to delineate the involvement of specific signaling pathways in the disease pathogenesis.
Findings obtained from different TRAF3-deficient mouse models generated in multiple laboratories strongly indicate that aberrant functions of TRAF3 may contribute to the pathogenesis of a variety of diseases, and have sparked interest in investigating Traf3 genetic alterations in human patients. Published reports have mainly focused on Traf3 mutations in B cell malignancies. Indeed, somatic biallelic deletions and inactivating mutations of Traf3 have been documented in a variety of human B cell neoplasms, including multiple myeloma, MZL, B cell chronic lymphocytic leukemia, mantle cell lymphoma, Waldenström’s macroglobulinemia and Hodgkin lymphoma (81–87). To date, only one case of a heterozygous Traf3 autosomal dominant mutation has been reported in a young adult with a history of herpes simplex virus-1 encephalitis in childhood, due to impaired TLR3-induced type I IFN production (88). Interestingly, expression of TRAF3 is significantly decreased in peripheral blood mononuclear cells of patients chronically infected with hepatitis B virus as compared to healthy controls (89). In the present study, we demonstrated that TRAF3 deletion leads to spontaneous inflammation and tumor development in mice. Future studies thus need to be directed at systematically determining the existence and frequency of somatic deletions, mutations, single nucleotide polymorphisms, or decreased expression of Traf3 in myeloid cells in human patients with chronic inflammation and tumors, including hepatitis, inflammatory bowel diseases, pneumonia, histiocytic sarcoma, DLBCL, and hepatocellular adenoma.
Supplementary Material
Acknowledgments
We would like to express our gratitude to Dr. Jerrold M. Ward (National Institute of Allergy and Infectious Diseases, NIH) for identifying bacterial and entamoeba infection of aged M-TRAF3−/− mice and for critical review of this manuscript. We also thank Jocelyn Gerges, Sukhdeep Grewal, Shanique Edwards, and Punit Arora for technical assistance of this study.
Abbreviations used in this paper
- BMDMs
bone marrow-derived macrophages
- CLN
cervical lymph nodes
- Cre
Cre recombinase
- CSR
class switch recombination
- DCs
dendritic cells
- DLBCL
diffuse large B-cell lymphoma
- DSBs
double strand DNA breaks
- ERK
extracellular signal-regulated kinase
- FACS
fluorescence-activated cell sorting
- FL
follicular lymphoma
- G-CSF
granulocyte colony stimulating factor
- GI tract
gastrointestinal tract
- IFN
interferon
- IP-10
IFNγ-induced protein 10
- IRF3
interferon regulatory factor 3
- JNK
c-Jun N-terminal kinase
- LMC
littermate control
- LN
lymph node
- LPS
lipopolysaccharides
- LysM
lysozyme M
- MCP
monocyte chemotactic protein
- MDSCs
myeloid derived suppressor cells
- MLN
mesenteric lymph nodes
- M-TRAF3−/−
myeloid cell-specific TRAF3-deficient
- MZL
splenic marginal zone lymphoma
- NF-κB
nuclear factor κ light chain enhancer of activated B cells
- NLRs
NOD-like receptors
- RT-qPCR
real time quantitative polymerase chain reaction
- pDCs
plasmacytoid dendritic cells
- PEMs
peritoneal exudate macrophages
- RLRs
RIG-I-like receptors
- SHM
somatic hypermutation
- TCR
T cell receptor
- TD
T cell-dependent
- TI
T cell-independent
- TLRs
Toll-like receptors
- TNF-R
tumor necrosis factor-receptor
- TRAF3
TNF-R associated factor 3
- TNP-KLH
trinitrophenol-keyhole limpet hemocyanin
- Treg
regulatory T cells
Footnotes
This study was supported by the Cancer Institute of New Jersey through Grant Number P30CA072720 from the National Cancer Institute (P. Xie), a Faculty Research Grant (P. Xie), and the Arthur Herrmann Endowed Cancer Research Fund (P. Xie), and in part by the Intramural Research Program of the NIH, National Institute of Allergy and Infectious Diseases (H. Morse III).
Competing interests statement
The authors declare that they have no competing financial interests.
References
- 1.Xie P. TRAF molecules in cell signaling and in human diseases. J Mol Signal. 2013;8:7. doi: 10.1186/1750-2187-8-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hacker H, Tseng PH, Karin M. Expanding TRAF function: TRAF3 as a tri-faced immune regulator. Nat Rev Immunol. 2011;11:457–468. doi: 10.1038/nri2998. [DOI] [PubMed] [Google Scholar]
- 3.Kawai T, Akira S. The role of pattern-recognition receptors in innate immunity: update on Toll-like receptors. Nat Immunol. 2010;11:373–384. doi: 10.1038/ni.1863. [DOI] [PubMed] [Google Scholar]
- 4.Saleh M. The machinery of Nod-like receptors: refining the paths to immunity and cell death. Immunol Rev. 2011;243:235–246. doi: 10.1111/j.1600-065X.2011.01045.x. [DOI] [PubMed] [Google Scholar]
- 5.Yu M, Levine SJ. Toll-like receptor, RIG-I-like receptors and the NLRP3 inflammasome: key modulators of innate immune responses to double-stranded RNA viruses. Cytokine Growth Factor Rev. 2011;22:63–72. doi: 10.1016/j.cytogfr.2011.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Xu Y, Cheng G, Baltimore D. Targeted disruption of TRAF3 leads to postnatal lethality and defective T-dependent immune responses. Immunity. 1996;5:407–415. doi: 10.1016/s1074-7613(00)80497-5. [DOI] [PubMed] [Google Scholar]
- 7.Xie P, Stunz LL, Larison KD, Yang B, Bishop GA. Tumor necrosis factor receptor-associated factor 3 is a critical regulator of B cell homeostasis in secondary lymphoid organs. Immunity. 2007;27:253–267. doi: 10.1016/j.immuni.2007.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Moore CR, Liu Y, Shao CS, Covey LR, Morse HC, 3rd, Xie P. Specific deletion of TRAF3 in B lymphocytes leads to B lymphoma development in mice. Leukemia. 2012;26:1122–1127. doi: 10.1038/leu.2011.309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gardam S, Sierro F, Basten A, Mackay F, Brink R. TRAF2 and TRAF3 signal adapters act cooperatively to control the maturation and survival signals delivered to B cells by the BAFF receptor. Immunity. 2008;28:391–401. doi: 10.1016/j.immuni.2008.01.009. [DOI] [PubMed] [Google Scholar]
- 10.Xie P, Kraus ZJ, Stunz LL, Liu Y, Bishop GA. TNF Receptor-Associated Factor 3 Is Required for T Cell-Mediated Immunity and TCR/CD28 Signaling. J Immunol. 2011;186:143–155. doi: 10.4049/jimmunol.1000290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chang JH, Hu H, Jin J, Puebla-Osorio N, Xiao Y, Gilbert BE, Brink R, Ullrich SE, Sun SC. TRAF3 regulates the effector function of regulatory T cells and humoral immune responses. J Exp Med. 2014;211:137–151. doi: 10.1084/jem.20131019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yi Z, Stunz LL, Bishop GA. TNF receptor associated factor 3 plays a key role in development and function of invariant natural killer T cells. J Exp Med. 2013;210:1079–1086. doi: 10.1084/jem.20122135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hacker H, Redecke V, Blagoev B, Kratchmarova I, Hsu LC, Wang GG, Kamps MP, Raz E, Wagner H, Hacker G, et al. Specificity in Toll-like receptor signalling through distinct effector functions of TRAF3 and TRAF6. Nature. 2006;439:204–207. doi: 10.1038/nature04369. [DOI] [PubMed] [Google Scholar]
- 14.Oganesyan G, Saha SK, Guo B, He JQ, Shahangian A, Zarnegar B, Perry A, Cheng G. Critical role of TRAF3 in the Toll-like receptor-dependent and -independent antiviral response. Nature. 2006;439:208–211. doi: 10.1038/nature04374. [DOI] [PubMed] [Google Scholar]
- 15.Rub A, Dey R, Jadhav M, Kamat R, Chakkaramakkil S, Majumdar S, Mukhopadhyaya R, Saha B. Cholesterol depletion associated with Leishmania major infection alters macrophage CD40 signalosome composition and effector function. Nat Immunol. 2009;10:273–280. doi: 10.1038/ni.1705. [DOI] [PubMed] [Google Scholar]
- 16.Clausen BE, Burkhardt C, Reith W, Renkawitz R, Forster I. Conditional gene targeting in macrophages and granulocytes using LysMcre mice. Transgenic Res. 1999;8:265–277. doi: 10.1023/a:1008942828960. [DOI] [PubMed] [Google Scholar]
- 17.Clemens RA, Lenox LE, Kambayashi T, Bezman N, Maltzman JS, Nichols KE, Koretzky GA. Loss of SLP-76 expression within myeloid cells confers resistance to neutrophil-mediated tissue damage while maintaining effective bacterial killing. J Immunol. 2007;178:4606–4614. doi: 10.4049/jimmunol.178.7.4606. [DOI] [PubMed] [Google Scholar]
- 18.Zhang X, Goncalves R, Mosser DM. The isolation and characterization of murine macrophages. Curr Protoc Immunol. 2008;Chapter 14(Unit 14):11. doi: 10.1002/0471142735.im1401s83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Weischenfeldt J, Porse B. Bone Marrow-Derived Macrophages (BMM): Isolation and Applications. CSH Protoc. 2008;2008 doi: 10.1101/pdb.prot5080. pdb prot5080. [DOI] [PubMed] [Google Scholar]
- 20.Manzanero S. Generation of mouse bone marrow-derived macrophages. Methods Mol Biol. 2012;844:177–181. doi: 10.1007/978-1-61779-527-5_12. [DOI] [PubMed] [Google Scholar]
- 21.Edwards SK, Moore CR, Liu Y, Grewal S, Covey LR, Xie P. N-benzyladriamycin-14-valerate (AD 198) exhibits potent anti-tumor activity on TRAF3-deficient mouse B lymphoma and human multiple myeloma. BMC Cancer. 2013;13:481. doi: 10.1186/1471-2407-13-481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Xie P, Poovassery J, Stunz LL, Smith SM, Schultz ML, Carlin LE, Bishop GA. Enhanced Toll-like receptor (TLR) responses of TNFR-associated factor 3 (TRAF3)-deficient B lymphocytes. J Leukoc Biol. 2011;90:1149–1157. doi: 10.1189/jlb.0111044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Morse HC, 3rd, Anver MR, Fredrickson TN, Haines DC, Harris AW, Harris NL, Jaffe ES, Kogan SC, MacLennan IC, Pattengale PK, et al. Bethesda proposals for classification of lymphoid neoplasms in mice. Blood. 2002;100:246–258. doi: 10.1182/blood.v100.1.246. [DOI] [PubMed] [Google Scholar]
- 24.Hao X, Fredrickson TN, Chattopadhyay SK, Han W, Qi CF, Wang Z, Ward JM, Hartley JW, Morse HC., 3rd The histopathologic and molecular basis for the diagnosis of histiocytic sarcoma and histiocyte-associated lymphoma of mice. Vet Pathol. 2010;47:434–445. doi: 10.1177/0300985810363705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.King CG, Kobayashi T, Cejas PJ, Kim T, Yoon K, Kim GK, Chiffoleau E, Hickman SP, Walsh PT, Turka LA, et al. TRAF6 is a T cell-intrinsic negative regulator required for the maintenance of immune homeostasis. Nat Med. 2006;12:1088–1092. doi: 10.1038/nm1449. [DOI] [PubMed] [Google Scholar]
- 26.Fredrickson TN, Hartley JW, Morse HC., 3rd Citrobacter-induced colitis in mice with murine acquired immunodeficiency syndrome. Vet Pathol. 2010;47:312–317. doi: 10.1177/0300985809358605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lin TM. Colonization and encystation of Entamoeba muris in the rat and the mouse. J Parasitol. 1971;57:375–382. [PubMed] [Google Scholar]
- 28.Cobo ER, He C, Hirata K, Hwang G, Tran U, Eckmann L, Gallo RL, Reed SL. Entamoeba histolytica induces intestinal cathelicidins but is resistant to cathelicidin-mediated killing. Infect Immun. 2012;80:143–149. doi: 10.1128/IAI.05029-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Dzhagalov I, St John A, He YW. The antiapoptotic protein Mcl-1 is essential for the survival of neutrophils but not macrophages. Blood. 2007;109:1620–1626. doi: 10.1182/blood-2006-03-013771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Yang Y, Liu B, Dai J, Srivastava PK, Zammit DJ, Lefrancois L, Li Z. Heat shock protein gp96 is a master chaperone for toll-like receptors and is important in the innate function of macrophages. Immunity. 2007;26:215–226. doi: 10.1016/j.immuni.2006.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Beekman R, Touw IP. G-CSF and its receptor in myeloid malignancy. Blood. 2010;115:5131–5136. doi: 10.1182/blood-2010-01-234120. [DOI] [PubMed] [Google Scholar]
- 32.Greenbaum AM, Link DC. Mechanisms of G-CSF-mediated hematopoietic stem and progenitor mobilization. Leukemia. 2011;25:211–217. doi: 10.1038/leu.2010.248. [DOI] [PubMed] [Google Scholar]
- 33.Gaffen SL. Recent advances in the IL-17 cytokine family. Curr Opin Immunol. 2011;23:613–619. doi: 10.1016/j.coi.2011.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Das S, Sarrou E, Podgrabinska S, Cassella M, Mungamuri SK, Feirt N, Gordon R, Nagi CS, Wang Y, Entenberg D, et al. Tumor cell entry into the lymph node is controlled by CCL1 chemokine expressed by lymph node lymphatic sinuses. J Exp Med. 2013;210:1509–1528. doi: 10.1084/jem.20111627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kyriakides TR, Foster MJ, Keeney GE, Tsai A, Giachelli CM, Clark-Lewis I, Rollins BJ, Bornstein P. The CC chemokine ligand, CCL2/MCP1, participates in macrophage fusion and foreign body giant cell formation. Am J Pathol. 2004;165:2157–2166. doi: 10.1016/S0002-9440(10)63265-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Conti I, Rollins BJ. CCL2 (monocyte chemoattractant protein-1) and cancer. Semin Cancer Biol. 2004;14:149–154. doi: 10.1016/j.semcancer.2003.10.009. [DOI] [PubMed] [Google Scholar]
- 37.Sarafi MN, Garcia-Zepeda EA, MacLean JA, Charo IF, Luster AD. Murine monocyte chemoattractant protein (MCP)-5: a novel CC chemokine that is a structural and functional homologue of human MCP-1. J Exp Med. 1997;185:99–109. doi: 10.1084/jem.185.1.99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Charo IF, Peters W. Chemokine receptor 2 (CCR2) in atherosclerosis, infectious diseases, and regulation of T-cell polarization. Microcirculation. 2003;10:259–264. doi: 10.1038/sj.mn.7800191. [DOI] [PubMed] [Google Scholar]
- 39.Liu M, Guo S, Hibbert JM, Jain V, Singh N, Wilson NO, Stiles JK. CXCL10/IP-10 in infectious diseases pathogenesis and potential therapeutic implications. Cytokine Growth Factor Rev. 2011;22:121–130. doi: 10.1016/j.cytogfr.2011.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Liu M, Guo S, Stiles JK. The emerging role of CXCL10 in cancer (Review) Oncol Lett. 2011;2:583–589. doi: 10.3892/ol.2011.300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sharif O, Knapp S. From expression to signaling: roles of TREM-1 and TREM-2 in innate immunity and bacterial infection. Immunobiology. 2008;213:701–713. doi: 10.1016/j.imbio.2008.07.008. [DOI] [PubMed] [Google Scholar]
- 42.Arts RJ, Joosten LA, van der Meer JW, Netea MG. TREM-1: intracellular signaling pathways and interaction with pattern recognition receptors. J Leukoc Biol. 2013;93:209–215. doi: 10.1189/jlb.0312145. [DOI] [PubMed] [Google Scholar]
- 43.Jenkinson SR, Williams JA, Jeon H, Zhang J, Nitta T, Ohigashi I, Kruhlak M, Zuklys S, Sharrow S, Adams A, et al. TRAF3 enforces the requirement for T cell cross-talk in thymic medullary epithelial development. Proc Natl Acad Sci U S A. 2013;110:21107–21112. doi: 10.1073/pnas.1314859111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Xiu Y, Xu H, Zhao C, Li J, Morita Y, Yao Z, Xing L, Boyce BF. Chloroquine reduces osteoclastogenesis in murine osteoporosis by preventing TRAF3 degradation. J Clin Invest. 2014;124:297–310. doi: 10.1172/JCI66947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Baniyash M, Sade-Feldman M, Kanterman J. Chronic inflammation and cancer: suppressing the suppressors. Cancer Immunol Immunother. 2014;63:11–20. doi: 10.1007/s00262-013-1468-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Wesolowski R, Markowitz J, Carson WE., 3rd Myeloid derived suppressor cells - a new therapeutic target in the treatment of cancer. J Immunother Cancer. 2013;1:10. doi: 10.1186/2051-1426-1-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Brandau S, Moses K, Lang S. The kinship of neutrophils and granulocytic myeloid-derived suppressor cells in cancer: cousins, siblings or twins? Semin Cancer Biol. 2013;23:171–182. doi: 10.1016/j.semcancer.2013.02.007. [DOI] [PubMed] [Google Scholar]
- 48.Ostrand-Rosenberg S, Sinha P. Myeloid-derived suppressor cells: linking inflammation and cancer. J Immunol. 2009;182:4499–4506. doi: 10.4049/jimmunol.0802740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Saha SK, Pietras EM, He JQ, Kang JR, Liu SY, Oganesyan G, Shahangian A, Zarnegar B, Shiba TL, Wang Y, et al. Regulation of antiviral responses by a direct and specific interaction between TRAF3 and Cardif. Embo J. 2006;25:3257–3263. doi: 10.1038/sj.emboj.7601220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Watanabe T, Asano N, Fichtner-Feigl S, Gorelick PL, Tsuji Y, Matsumoto Y, Chiba T, Fuss IJ, Kitani A, Strober W. NOD1 contributes to mouse host defense against Helicobacter pylori via induction of type I IFN and activation of the ISGF3 signaling pathway. J Clin Invest. 2010;120:1645–1662. doi: 10.1172/JCI39481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Perkins DJ, Polumuri SK, Pennini ME, Lai W, Xie P, Vogel SN. Reprogramming of Murine Macrophages through TLR2 Confers Viral Resistance via TRAF3-Mediated, Enhanced Interferon Production. PLoS Pathog. 2013;9:e1003479. doi: 10.1371/journal.ppat.1003479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Izcue A, Coombes JL, Powrie F. Regulatory lymphocytes and intestinal inflammation. Annu Rev Immunol. 2009;27:313–338. doi: 10.1146/annurev.immunol.021908.132657. [DOI] [PubMed] [Google Scholar]
- 53.Chow J, Tang H, Mazmanian SK. Pathobionts of the gastrointestinal microbiota and inflammatory disease. Curr Opin Immunol. 2011;23:473–480. doi: 10.1016/j.coi.2011.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Kamada N, Chen GY, Inohara N, Nunez G. Control of pathogens and pathobionts by the gut microbiota. Nat Immunol. 2013;14:685–690. doi: 10.1038/ni.2608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Ivory CP, Prystajecky M, Jobin C, Chadee K. Toll-like receptor 9-dependent macrophage activation by Entamoeba histolytica DNA. Infect Immun. 2008;76:289–297. doi: 10.1128/IAI.01217-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Philpott DJ, Sorbara MT, Robertson SJ, Croitoru K, Girardin SE. NOD proteins: regulators of inflammation in health and disease. Nat Rev Immunol. 2014;14:9–23. doi: 10.1038/nri3565. [DOI] [PubMed] [Google Scholar]
- 57.Biswas A, Kobayashi KS. Regulation of intestinal microbiota by the NLR protein family. Int Immunol. 2013;25:207–214. doi: 10.1093/intimm/dxs116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Buchanan RM, Arulanandam BP, Metzger DW. IL-12 enhances antibody responses to T-independent polysaccharide vaccines in the absence of T and NK cells. J Immunol. 1998;161:5525–5533. [PubMed] [Google Scholar]
- 59.Kopf M, Herren S, Wiles MV, Pepys MB, Kosco-Vilbois MH. Interleukin 6 influences germinal center development and antibody production via a contribution of C3 complement component. J Exp Med. 1998;188:1895–1906. doi: 10.1084/jem.188.10.1895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Poudrier J, Graber P, Herren S, Gretener D, Elson G, Berney C, Gauchat JF, Kosco-Vilbois MH. A soluble form of IL-13 receptor alpha 1 promotes IgG2a and IgG2b production by murine germinal center B cells. J Immunol. 1999;163:1153–1161. [PubMed] [Google Scholar]
- 61.Choi YS, Eto D, Yang JA, Lao C, Crotty S. Cutting edge: STAT1 is required for IL-6-mediated Bcl6 induction for early follicular helper cell differentiation. J Immunol. 2013;190:3049–3053. doi: 10.4049/jimmunol.1203032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Sweet RA, Lee SK, Vinuesa CG. Developing connections amongst key cytokines and dysregulated germinal centers in autoimmunity. Curr Opin Immunol. 2012;24:658–664. doi: 10.1016/j.coi.2012.10.003. [DOI] [PubMed] [Google Scholar]
- 63.Chakarov S, Fazilleau N. Monocyte-derived dendritic cells promote T follicular helper cell differentiation. EMBO Mol Med. 2014;6:590–603. doi: 10.1002/emmm.201403841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Pratama A, Vinuesa CG. Control of TFH cell numbers: why and how? Immunol Cell Biol. 2014;92:40–48. doi: 10.1038/icb.2013.69. [DOI] [PubMed] [Google Scholar]
- 65.Shaffer AL, Rosenwald A, Staudt LM. Lymphoid malignancies: the dark side of B-cell differentiation. Nat Rev Immunol. 2002;2:920–932. doi: 10.1038/nri953. [DOI] [PubMed] [Google Scholar]
- 66.Kuppers R, Dalla-Favera R. Mechanisms of chromosomal translocations in B cell lymphomas. Oncogene. 2001;20:5580–5594. doi: 10.1038/sj.onc.1204640. [DOI] [PubMed] [Google Scholar]
- 67.Peled JU, Kuang FL, Iglesias-Ussel MD, Roa S, Kalis SL, Goodman MF, Scharff MD. The biochemistry of somatic hypermutation. Annu Rev Immunol. 2008;26:481–511. doi: 10.1146/annurev.immunol.26.021607.090236. [DOI] [PubMed] [Google Scholar]
- 68.Karin M, Lawrence T, Nizet V. Innate immunity gone awry: linking microbial infections to chronic inflammation and cancer. Cell. 2006;124:823–835. doi: 10.1016/j.cell.2006.02.016. [DOI] [PubMed] [Google Scholar]
- 69.Mechtcheriakova D, Svoboda M, Meshcheryakova A, Jensen-Jarolim E. Activation-induced cytidine deaminase (AID) linking immunity, chronic inflammation, and cancer. Cancer Immunol Immunother. 2012;61:1591–1598. doi: 10.1007/s00262-012-1255-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Hasselbalch HC. Chronic inflammation as a promotor of mutagenesis in essential thrombocythemia, polycythemia vera and myelofibrosis. A human inflammation model for cancer development? Leuk Res. 2013;37:214–220. doi: 10.1016/j.leukres.2012.10.020. [DOI] [PubMed] [Google Scholar]
- 71.Kamp DW, Shacter E, Weitzman SA. Chronic inflammation and cancer: the role of the mitochondria. Oncology (Williston Park) 2011;25:400–410. 413. [PubMed] [Google Scholar]
- 72.Rakoff-Nahoum S, Paglino J, Eslami-Varzaneh F, Edberg S, Medzhitov R. Recognition of commensal microflora by toll-like receptors is required for intestinal homeostasis. Cell. 2004;118:229–241. doi: 10.1016/j.cell.2004.07.002. [DOI] [PubMed] [Google Scholar]
- 73.Pradere JP, Dapito DH, Schwabe RF. The Yin and Yang of Toll-like receptors in cancer. Oncogene. 2014;33:3485–3495. doi: 10.1038/onc.2013.302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Sato Y, Goto Y, Narita N, Hoon DS. Cancer Cells Expressing Toll-like Receptors and the Tumor Microenvironment. Cancer Microenviron. 2009;2(Suppl 1):205–214. doi: 10.1007/s12307-009-0022-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Saxena M, Yeretssian G. NOD-Like Receptors: Master Regulators of Inflammation and Cancer. Front Immunol. 2014;5:327. doi: 10.3389/fimmu.2014.00327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Wang JQ, Jeelall YS, Ferguson LL, Horikawa K. Toll-Like Receptors and Cancer: MYD88 Mutation and Inflammation. Front Immunol. 2014;5:367. doi: 10.3389/fimmu.2014.00367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Allen IC, Wilson JE, Schneider M, Lich JD, Roberts RA, Arthur JC, Woodford RM, Davis BK, Uronis JM, Herfarth HH, et al. NLRP12 suppresses colon inflammation and tumorigenesis through the negative regulation of noncanonical NF-kappaB signaling. Immunity. 2012;36:742–754. doi: 10.1016/j.immuni.2012.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Wimmer N, Huber B, Barabas N, Rohrl J, Pfeffer K, Hehlgans T. Lymphotoxin beta receptor activation on macrophages induces cross-tolerance to TLR4 and TLR9 ligands. J Immunol. 2012;188:3426–3433. doi: 10.4049/jimmunol.1103324. [DOI] [PubMed] [Google Scholar]
- 79.Hoshi N, Schenten D, Nish SA, Walther Z, Gagliani N, Flavell RA, Reizis B, Shen Z, Fox JG, Iwasaki A, et al. MyD88 signalling in colonic mononuclear phagocytes drives colitis in IL-10-deficient mice. Nat Commun. 2012;3:1120. doi: 10.1038/ncomms2113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Fukata M, Chen A, Vamadevan AS, Cohen J, Breglio K, Krishnareddy S, Hsu D, Xu R, Harpaz N, Dannenberg AJ, et al. Toll-like receptor-4 promotes the development of colitis-associated colorectal tumors. Gastroenterology. 2007;133:1869–1881. doi: 10.1053/j.gastro.2007.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Keats JJ, Fonseca R, Chesi M, Schop R, Baker A, Chng WJ, Van Wier S, Tiedemann R, Shi CX, Sebag M, et al. Promiscuous mutations activate the noncanonical NF-kappaB pathway in multiple myeloma. Cancer Cell. 2007;12:131–144. doi: 10.1016/j.ccr.2007.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Annunziata CM, Davis RE, Demchenko Y, Bellamy W, Gabrea A, Zhan F, Lenz G, Hanamura I, Wright G, Xiao W, et al. Frequent engagement of the classical and alternative NF-kappaB pathways by diverse genetic abnormalities in multiple myeloma. Cancer Cell. 2007;12:115–130. doi: 10.1016/j.ccr.2007.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Demchenko YN, Glebov OK, Zingone A, Keats JJ, Bergsagel PL, Kuehl WM. Classical and/or alternative NF-kappaB pathway activation in multiple myeloma. Blood. 2010;115:3541–3552. doi: 10.1182/blood-2009-09-243535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Nagel I, Bug S, Tonnies H, Ammerpohl O, Richter J, Vater I, Callet-Bauchu E, Calasanz MJ, Martinez-Climent JA, Bastard C, et al. Biallelic inactivation of TRAF3 in a subset of B-cell lymphomas with interstitial del(14)(q24.1q32.33) Leukemia. 2009;23:2153–2155. doi: 10.1038/leu.2009.149. [DOI] [PubMed] [Google Scholar]
- 85.Rossi D, Deaglio S, Dominguez-Sola D, Rasi S, Vaisitti T, Agostinelli C, Spina V, Bruscaggin A, Monti S, Cerri M, et al. Alteration of BIRC3 and multiple other NF-{kappa}B pathway genes in splenic marginal zone lymphoma. Blood. 2011;118:4930–4934. doi: 10.1182/blood-2011-06-359166. [DOI] [PubMed] [Google Scholar]
- 86.Braggio E, Keats JJ, Leleu X, Van Wier S, Jimenez-Zepeda VH, Valdez R, Schop RF, Price-Troska T, Henderson K, Sacco A, et al. Identification of copy number abnormalities and inactivating mutations in two negative regulators of nuclear factor-kappaB signaling pathways in Waldenstrom’s macroglobulinemia. Cancer Res. 2009;69:3579–3588. doi: 10.1158/0008-5472.CAN-08-3701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Otto C, Giefing M, Massow A, Vater I, Gesk S, Schlesner M, Richter J, Klapper W, Hansmann ML, Siebert R, et al. Genetic lesions of the TRAF3 and MAP3K14 genes in classical Hodgkin lymphoma. Br J Haematol. 2012;157:702–708. doi: 10.1111/j.1365-2141.2012.09113.x. [DOI] [PubMed] [Google Scholar]
- 88.de Diego Perez R, Sancho-Shimizu V, Lorenzo L, Puel A, Plancoulaine S, Picard C, Herman M, Cardon A, Durandy A, Bustamante J, et al. Human TRAF3 adaptor molecule deficiency leads to impaired Toll-like receptor 3 response and susceptibility to herpes simplex encephalitis. Immunity. 2010;33:400–411. doi: 10.1016/j.immuni.2010.08.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Momeni M, Zainodini N, Bidaki R, Hassanshahi G, Daneshvar H, Khaleghinia M, Ebrahim M, Karimi-Googheri M, Askari A, Arababadi MK, et al. Decreased expression of toll like receptor signaling molecules in chronic HBV infected patients. Hum Immunol. 2014;75:15–19. doi: 10.1016/j.humimm.2013.09.015. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.