Abstract
A fifty-year-old female non-smoker with no other specific medical history visited our institute. She complained of axial back pain with no other neurological deficit. Chest X-ray, chest computed tomography (CT) scan, CT-guided needle aspiration biopsy, whole-body positron emission tomography, spine CT and spine magnetic resonance image findings suggested NSCLC with epidermal growth factor receptor (EGFR) mutation, multiple brain metastases, and two isolated metastases to the T3 and L3 vertebral bodies. She underwent chemotherapy with gefitinib (Iressa™) for NSCLC and gamma knife surgery for multiple brain metastases. We performed a two-staged, total en bloc spondylectomy of the T3 and L3 vertebral bodies based on several good prognostic characteristics, such as the lack of metastases to the appendicular bone, good preoperative performance status, and being an excellent responder (Asian, never-smoker and adenocarcinoma histology) to EGFR inhibitors. Improved axial back pain after the surgery enabled her to walk with the aid of a thoracolumbosacral orthosis brace on the third postoperative day. Her Karnofsky performance status score (KPS) was 90 at the time of discharge and has been maintained to date 3 years after surgery. In selected NSCLC patients with good prognostic characteristics, we suggest that locally curative treatment such as total en bloc spondylectomy or radiosurgery should be emphasized to achieve longer term survival for the selected cases.
Keywords: Lung cancer, Spinal metastasis, Total en bloc spondylectomy
INTRODUCTION
Many patients with lung cancer are at advanced stages of the disease at the time of diagnosis. The prognosis of bone metastasis from lung cancer has been shown to be poor. Previous investigators have reported the mean length of survival for patients with stage IV lung cancer, including distant metastasis, to be approximately 6 months. The mean survival period for patients with lung cancer with bone metastasis has been reported to be 5 to 7.2 months8,13). Approximately 65% of patients with lung cancer develop bone metastases, and the spine is the most common bone metastasis site9). The poor prognosis of lung cancer with spine metastasis caused spine surgeons to adopt a palliative approach rather than more aggressive treatment, such as en bloc marginal resection. Deciding the best surgical plan for these patients is challenging, considering the aggressiveness of the disease. However, quality of life has been recently emphasized as an important issue even in patients with cancer at an advanced stage. Tomita et al.15) have insisted that spinal metastasis is not necessarily an end-stage condition. They concluded that first-time curative oncologic surgery is the most important treatment modality. The treatment of metastatic spine disease has evolved significantly with advanced interventional, surgical, and radiation techniques. In the present report, we describe the successful outcome after en bloc spondylectomies in a patient who had non-small cell lung cancer with two isolated metastases to vertebral bodies.
CASE REPORT
A fifty-year-old female non-smoker with no other specific medical history visited our institute for further evaluation and management of lung cancer diagnosed at another hospital. She complained of upper and lower axial back pain without any neuro-logical deficits. Chest X-ray and computed tomography (CT) revealed primary lung cancer (T2) in the right lower lobe with lymph node metastasis (N3) and lung-to-lung and bone metastasis (M1b). Whole-body positron emission tomography (PET) findings suggested lung cancer in the right lower lobe and bone metastases in the T3 and L3 vertebral bodies (Fig. 1). Multiple enhancing nodules in both temporal lobes and the left occipital lobe, which suggested brain metastases, were detected on brain magnetic resonance image (MRI). CT-guided percutaneous needle aspiration biopsy confirmed non-small cell lung cancer (NSCLC) with adenocarcinoma histology. A deletion was found in exon 19 of the epidermal growth factor receptor (EGFR) gene after an EGFR mutation sequencing test.
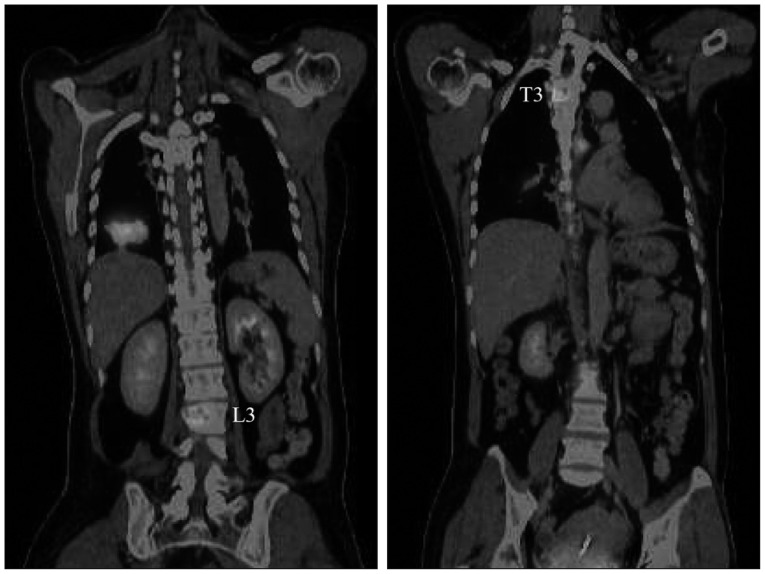
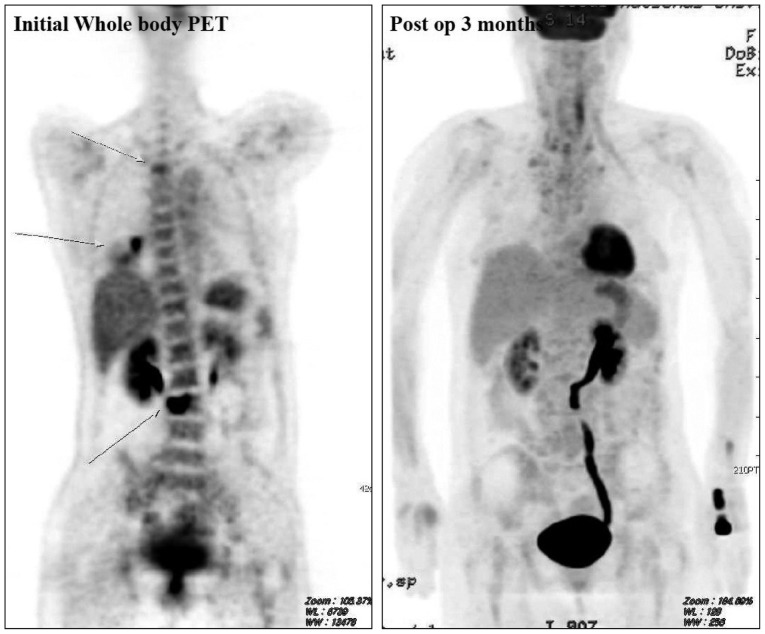
Fig. 1.
Preoperative whole-body positron emission tomography findings suggest lung cancer in the right lower lobe, and bone metastases in the T3 and L3 vertebral bodies.
She underwent chemotherapy with gefitinib (Iressa™) for NSCLC and underwent gamma knife surgery for multiple brain metastases. After 1 month, a slightly decreased size of multiple enhancing nodules in both temporal lobes and the left occipital lobe was found on post-gamma-knife-surgery brain MRI. After 3 months, the decreased size of NSCLC lesions in the right lower lobe on chest X-ray indicated a partial response to chemotherapy for lung cancer (Fig. 2). She complained of debilitating upper and lower axial back pain that was refractory to medical treatment. Bony metastases at the T3 and L3 vertebral bodies were noticeable on MRI, and osteolytic lesions were evident on spine CT. Pathologic compression fracture was noticed at the L3 vertebral body; however, no epidural and paravertebral extension was noted at the T3 and L3 levels (Fig. 3).
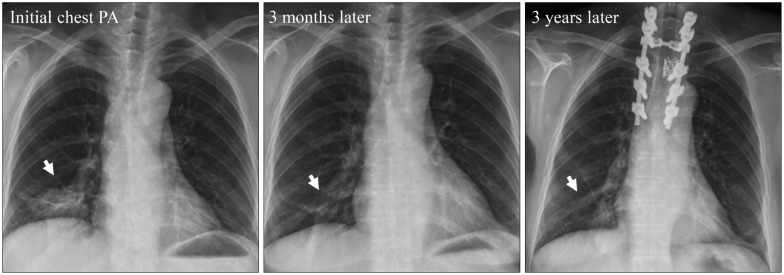
Fig. 2.
Plain radiographic findings by time course. An initial chest X-ray shows a nodular lesion in the right lower lobe. Partial response in a chest X-ray 3 months later and stable disease in a chest X-ray 3 years later were detected.
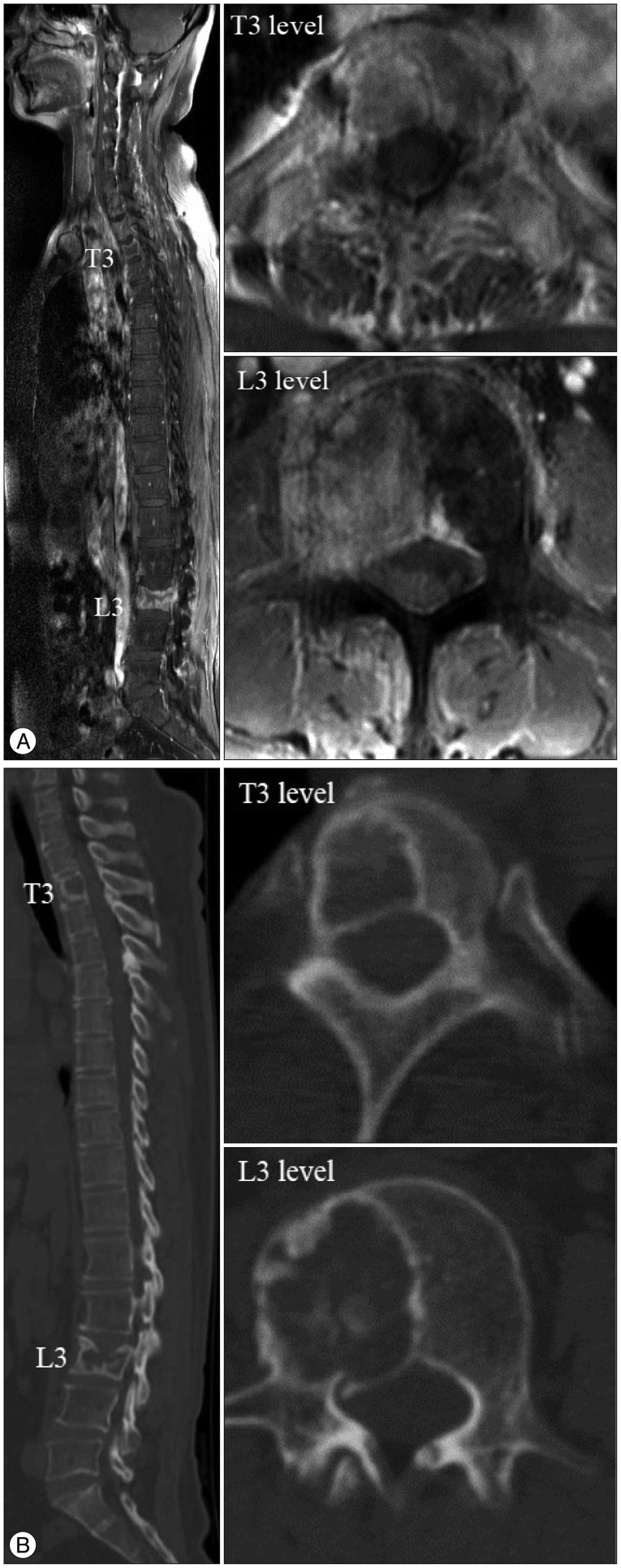
Fig. 3.
Preoperative spine MRI and CT. A : Sagittal T1-weighted image with gadolinium enhancement showing the whole spine. Bony metastases at the T3 and L3 vertebral bodies were remarkable, and pathologic compression fracture at the L3 vertebral body was identifiable. Axial T1-weighted images with gadolinium enhancement show bony metastasis at the T3 and L3 vertebral bodies without epidural and paravertebral extension. B : Sagittal CT scan of the whole spine. Osteolytic lesions are seen on axial CT.
Surgical treatment
We planned staged surgery for metastatic lesions at the T3 and L3 vertebral bodies considering the patient's general condition. After embolization of the tumor at the T3 vertebral body, she underwent total en bloc spondylectomy of the T3 vertebral body with posterior spinal instrumented fusion from the T1 to T6 vertebral bodies in accordance with previously reported surgical techniques4,15). Motor- and somatosensory-evoked potentials during the surgery showed no change compared with the baseline values. She was able to walk with a Minerva brace on the first postoperative day.
One week later, after embolization of the tumor at the L3 vertebral body, she underwent surgery for a metastatic tumor at the L3 vertebral body. The posterior element of L3 was removed as a single piece via a posterior approach, and posterior spinal instrumented fusion from L1 to L5 was performed. The anterior and middle column of L3 was subjected to en bloc extraction with protection of paravertebral structures via a left paramedian retroperitoneal approach (Fig. 4). She was able to walk with a brace on the third postoperative day. Her Karnofsky performance status (KPS) score was 90 at the time of discharge.
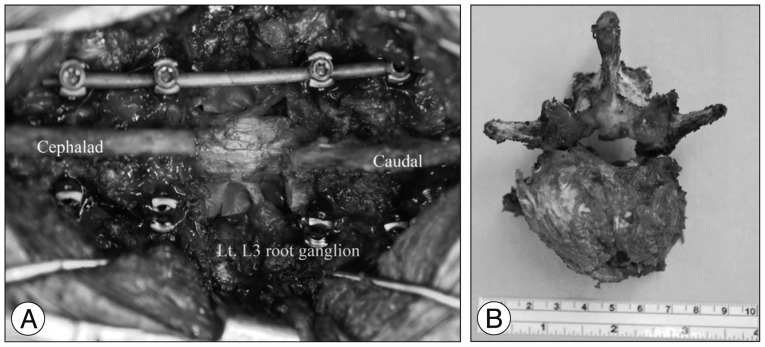
Fig. 4.
Intraoperative photograph at the L3 level. A : The thecal sac and L3 root ganglions were exposed after en bloc laminectomy. B : Resected specimen of the L3 vertebral body after total en bloc spondylectomy.
Postoperative course
Whole-body PET 3 months after surgery demonstrated no hypermetabolic lesion at the T3 and L3 vertebral bodies and right lower lobe of the lung (Fig. 5). Spine MRI with gadolinium enhancement at 27 months after surgery showed no evidence of recurrence at the T3 and L3 levels, and whole spine X-ray at 15 months after surgery revealed maintained spinal alignment (Fig. 6). She had no neurological deficits, no complications related to surgery and no respiratory complications at 3 years after surgery. Brain metastases were controlled with gamma knife surgery. Her KPS score has been maintained at 90 to date. Her chemotherapy response changed from a partial response to stable disease according to the chest X-ray findings at the last follow up, which was 3 years after the initial diagnosis (Fig. 2).
Fig. 5.
Whole-body positron emission tomography 3 months after surgery demonstrated no hypermetabolic lesion at the T3 and L3 vertebral bodies and the right lower lobe of the lung.
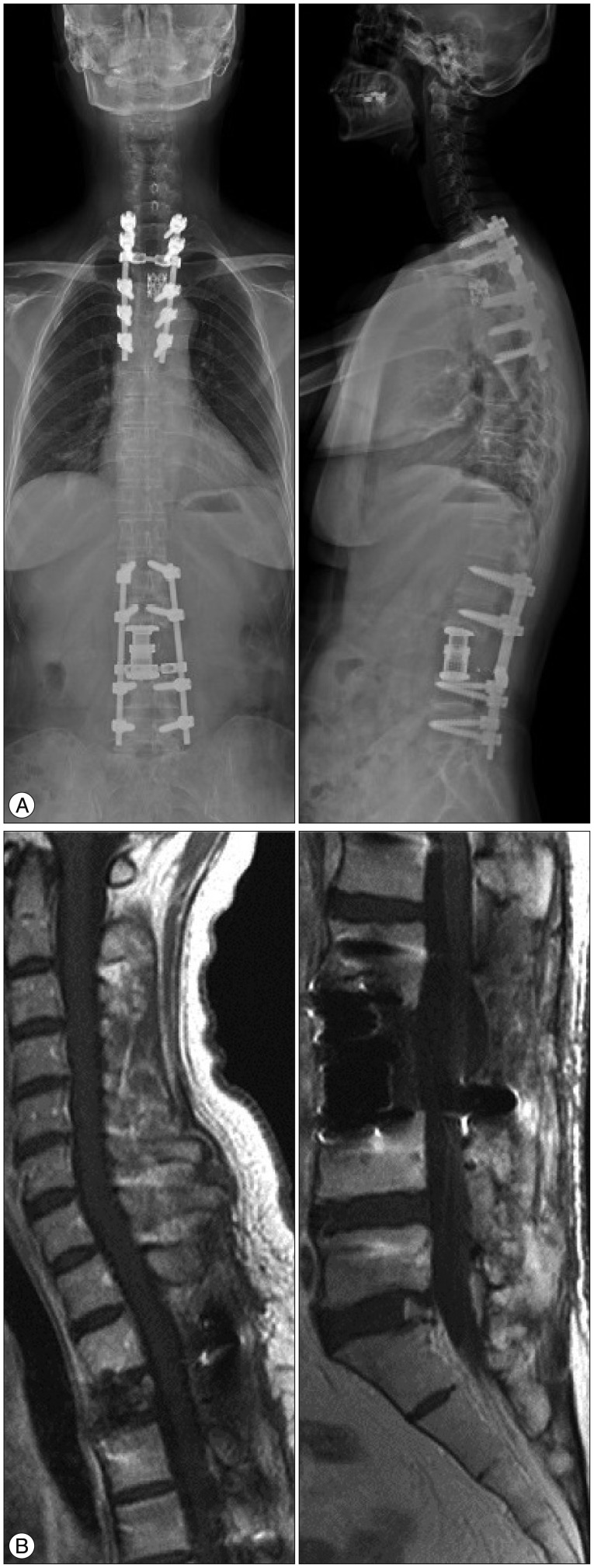
Fig. 6.
Postoperative X-ray at 15 months after surgery and follow-up spine MRI with gadolinium enhancement at 27 months after surgery. A : AP and lateral views of the whole spine revealed maintained spinal alignment. B : Sagittal T1-weighted image with gadolinium enhancement showing the T3 and L3 levels. No recurrence was evident.
DISCUSSION
We presented a patient with EGFR mutation-positive NSCLC metastasized to the spine. A favorable prognosis in patients with bone metastasis from lung cancer is more likely in women and patients with a performance status of 1 or less, adenocarcinoma histology, solitary bone metastasis, no metastases to the appendicular bone and no pathologic fractures, and who undergo systemic chemotherapy and EGFR inhibitor therapy13). Our patient underwent two staged, aggressive surgeries based on several good prognostic characteristics, such as no metastasis to the appendicular bone, good preoperative performance status, and criteria for being an excellent responder (Asian woman, never-smoker and adenocarcinoma histology) to EGFR inhibitors. Several articles have reported the effectiveness of EGFR inhibitors for the treatment of lung cancer, particularly lung cancer with adenocarcinoma histology2,3,7,10,13,16). EGFR inhibitors are new molecule-targeted agents for lung cancer that have been reported to be more effective in females and nonsmokers with lung cancer, particularly those who have lung cancer with adenocarcinoma histology. Our patient had a deletion in exon 19 of the EGFR gene, and EGFR mutations may predict the sensitivity to EGFR inhibitors. Gefitinib (Iressa™) is an EGFR tyrosine kinase inhibitor that provides a treatment option for patients with locally advanced or metastatic NSCLC, particularly those who harbor EGFR mutations2,11). Our patient showed a partial response 3 months after starting gefitinib therapy. This response was indicated as one of the positive prognostic factors.
Patients with spinal metastasis of lung cancer are often not candidates for surgical treatment because 1) survival is limited at the time of diagnosis, and 2) spinal metastasis is usually multiple at the time of detection. The first choice for treating spinal metastasis has been radiotherapy for pain control9). Recent radiotherapeutic or radiosurgical option was viable options to achieve local tumor control or pain palliation. Depending on the patients' condition, palliative radiotherapy or locally curative radiosurgery was available. In the past, the indication for the surgical management of spinal metastases was based on signs of neurological deficit, the presence of intractable pain, and spinal instability. To achieve local tumor control, the therapeutic strategies should include either locally curative surgical option, such as total en bloc spondylectomy and instrumentation or radiosurgery or locally ablative high dose radiotherapy with intensity modulation. Previous researchers have proposed the surgical classification of spinal tumors and surgical strategy for spinal metastases15). According to the surgical classification of spinal tumors, our patient belonged to multiple metastases (T3 and L3), but each level was isolated separately, and each was classified as pedicle extension without epidural or paraspinal extension. Moreover, the life expectancy of our patient was more than 2 years considering the partial response of the primary cancer, non-smoker status, female gender, and high KPS score. Our treatment aim was long-term local control of the metastasis at the spine. Consequently, we performed total en bloc spondylectomy of the T3 and L3 vertebral bodies.
Recent advances in modern spinal surgical techniques using advanced and reliable spinal instrumentation have made the removal of entire spinal segments feasible while maintaining stability of the vertebral column1,5,6,9,12,14,15). A recent study revealed that there is benefit from spinal surgery performed by metastatic spinal disease experts to control pain and maintain mobility, thus improving the quality of remaining life5). Our patient could walk with no neurological or respiratory complications and no local recurrence at the excised site more than 2 years after surgery. Brain metastases were decreased in size after gamma knife surgery and showed no recurrence or regrowth. The lung cancer response to chemotherapy was stable disease nearly 3 years after the diagnosis. She could perform routine daily life tasks by herself for 3 years although she was diagnosed with NSCLC with multiple metastases to the spine and brain.
We experienced a long term survivor who had NSCLC with multiple brain and spine metastases. Individual patient characteristics should be considered when determining whether marginal excisional surgery could be a good treatment option.
CONCLUSION
The local tumor control is the important treatment goal in selected NSCLC patients with good prognostic characteristics, such as female gender, adenocarcinoma histology, no metastasis to the appendicular bone, no visceral metastasis, high KPS score and an excellent response to EGFR inhibitors. Locally curative treatment of spinal metastases should be emphasized to achieve longer term survival for the selected cases.
References
- 1.Aoude AA, Amiot LP. Surgical treatment of a patient with lung cancer metastasized to the spine with EGFR mutation : a case report. Int J Surg Case Rep. 2012;3:510–512. doi: 10.1016/j.ijscr.2012.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Brown T, Boland A, Bagust A, Oyee J, Hockenhull J, Dundar Y, et al. Gefitinib for the first-line treatment of locally advanced or metastatic non-small cell lung cancer. Health Technol Assess. 2010;14(Suppl 2):71–79. doi: 10.3310/hta14suppl2/10. [DOI] [PubMed] [Google Scholar]
- 3.Herbst RS, Maddox AM, Rothenberg ML, Small EJ, Rubin EH, Baselga J, et al. Selective oral epidermal growth factor receptor tyrosine kinase inhibitor ZD1839 is generally well-tolerated and has activity in non-small-cell lung cancer and other solid tumors : results of a phase I trial. J Clin Oncol. 2002;20:3815–3825. doi: 10.1200/JCO.2002.03.038. [DOI] [PubMed] [Google Scholar]
- 4.Hsieh PC, Li KW, Sciubba DM, Suk I, Wolinsky JP, Gokaslan ZL. Posterior-only approach for total en bloc spondylectomy for malignant primary spinal neoplasms : anatomic considerations and operative nuances. Neurosurgery. 2009;65(6 Suppl):173–181. doi: 10.1227/01.NEU.0000345630.47344.17. discussion 181. [DOI] [PubMed] [Google Scholar]
- 5.Ibrahim A, Crockard A, Antonietti P, Boriani S, Bünger C, Gasbarrini A, et al. Does spinal surgery improve the quality of life for those with extradural (spinal) osseous metastases? An international multicenter prospective observational study of 223 patients. Invited submission from the Joint Section Meeting on Disorders of the Spine and Peripheral NervesNerves, March 2007. J Neurosurg Spine. 2008;8:271–278. doi: 10.3171/SPI/2008/8/3/271. [DOI] [PubMed] [Google Scholar]
- 6.Komagata M, Nishiyama M, Imakiire A, Kato H. Total spondylectomy for en bloc resection of lung cancer invading the chest wall and thoracic spine. Case report. J Neurosurg. 2004;100(4 Suppl Spine):353–357. doi: 10.3171/spi.2004.100.4.0353. [DOI] [PubMed] [Google Scholar]
- 7.Mitsudomi T, Kosaka T, Endoh H, Horio Y, Hida T, Mori S, et al. Mutations of the epidermal growth factor receptor gene predict prolonged survival after gefitinib treatment in patients with non-small-cell lung cancer with postoperative recurrence. J Clin Oncol. 2005;23:2513–2520. doi: 10.1200/JCO.2005.00.992. [DOI] [PubMed] [Google Scholar]
- 8.Mountain CF. Revisions in the International System for Staging Lung Cancer. Chest. 1997;111:1710–1717. doi: 10.1378/chest.111.6.1710. [DOI] [PubMed] [Google Scholar]
- 9.Murakami H, Kawahara N, Demura S, Kato S, Yoshioka K, Tomita K. Total en bloc spondylectomy for lung cancer metastasis to the spine. J Neurosurg Spine. 2010;13:414–417. doi: 10.3171/2010.4.SPINE09365. [DOI] [PubMed] [Google Scholar]
- 10.Paez JG, Jänne PA, Lee JC, Tracy S, Greulich H, Gabriel S, et al. EGFR mutations in lung cancer : correlation with clinical response to gefitinib therapy. Science. 2004;304:1497–1500. doi: 10.1126/science.1099314. [DOI] [PubMed] [Google Scholar]
- 11.Sanford M, Scott LJ. Gefitinib : a review of its use in the treatment of locally advanced/metastatic non-small cell lung cancer. Drugs. 2009;69:2303–2328. doi: 10.2165/10489100-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 12.Schirren J, Dönges T, Melzer M, Schönmayr R, Eberlein M, Bölükbas S. En bloc resection of non-small-cell lung cancer invading the spine. Eur J Cardiothorac Surg. 2011;40:647–654. doi: 10.1016/j.ejcts.2010.12.046. [DOI] [PubMed] [Google Scholar]
- 13.Sugiura H, Yamada K, Sugiura T, Hida T, Mitsudomi T. Predictors of survival in patients with bone metastasis of lung cancer. Clin Orthop Relat Res. 2008;466:729–736. doi: 10.1007/s11999-007-0051-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tomita K, Kawahara N, Kobayashi T, Yoshida A, Murakami H, Akamaru T. Surgical strategy for spinal metastases. Spine (Phila Pa 1976) 2001;26:298–306. doi: 10.1097/00007632-200102010-00016. [DOI] [PubMed] [Google Scholar]
- 15.Tomita K, Kawahara N, Murakami H, Demura S. Total en bloc spondylectomy for spinal tumors : improvement of the technique and its associated basic background. J Orthop Sci. 2006;11:3–12. doi: 10.1007/s00776-005-0964-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yokouchi H, Yamazaki K, Kinoshita I, Konishi J, Asahina H, Sukoh N, et al. Clinical benefit of readministration of gefitinib for initial gefitinib-responders with non-small cell lung cancer. BMC Cancer. 2007;7:51. doi: 10.1186/1471-2407-7-51. [DOI] [PMC free article] [PubMed] [Google Scholar]