Abstract
Per-oral endoscopic myotomy (POEM) represents a natural orifice endoscopic surgery (NOTES) approach to laparoscopy Heller myotomy (LHM). POEM is arguably the most successful clinical application of NOTES. The growth of POEM from a single center in 2008 to approximately 60 centers worldwide in 2014 with several thousand procedures having been performed attests to the success of POEM. Initial efficacy, safety and acid reflux data suggest at least equivalence of POEM to LHM, the previous gold standard for achalasia therapy. Adjunctive techniques used in the West include impedance planimetry for real-time intraprocedural luminal assessment and endoscopic suturing for challenging mucosal defect closures during POEM. The impact of POEM extends beyond the realm of esophageal motility disorders as it is rapidly popularizing endoscopic submucosal dissection in the West and spawning offshoots that use the submucosal tunnel technique for a host of new indications ranging from resection of tumors to pyloromyotomy for gastroparesis.
Keywords: Per oral endoscopic myotomy, Achalasia, Natural orifice transluminal endoscopic surgery, Submucosal tunnel endoscopic resection, Submucosal tunnel endoscopy, Endoscopic suturing, Endoscopic myotomy, Endoscopic submucosal dissection, EndoFLIP
Core tip: Per-oral endoscopic myotomy (POEM) is a novel endosurgical therapy for achalasia. POEM developed as an offshoot of early natural orifice endoscopic surgery (NOTES) approach investigation, but, now, is arguably the most successful clinical application of NOTES. The clinical results of POEM therapy in terms of dysphagia relief and safety have been excellent. The impact of POEM is extending far beyond the narrow domain of esophageal motility disorders. As the first successful clinical application of submucosal endoscopy it is now spawning many other NOTES interventions utilizing a submucosal tunnel approach including submucosal tunnel endoscopic resection of submucosal and mucosal lesions and per oral pyloromyotomy for gastroparesis.
INTRODUCTION
Achalasia is a rarely encountered motor disorder of the esophagus, which is usually of unclear etiology. Most patients have dysphagia to solids and liquids and others may have chest pain, regurgitation, and coughing. Barium esophageal contrast study usually shows a dilated esophagus tapering to a “bird’s beak” with delayed contrast passage into the stomach, but diagnosis is confirmed by esophageal manometry showing infrequent or no relaxation of the lower esophageal sphincter (LES) and a variety of abnormalities in the esophageal body. Medical therapy is ineffective in achalasia and treatment is centered on ablation of the LES. Large-diameter balloon pneumatic dilation (PD) and laparoscopic Heller myotomy (LHM) are the current mainstays in achalasia therapy with botulinum toxin injection (BTI) reserved for the frail elderly. A recent pivotal article noted equivalent results between PD and LHM with Dor’s fundoplication at 43 mo post-therapy as noted by LES pressure measurements and dysphagia scores[1]. LHM is still considered the best therapy for achalasia because of its durable response and the possibility of perforation with PD[2]. A systematic review and meta-analysis noted LHM to yield superior and more durable results than PD and BTI[3]. End stage achalasia with a hugely dilated esophagus may necessitate partial esophagectomy (recently performed via laparoscopy)[4].
HISTORICAL BACKGROUND
Ortega described a case series of 17 achalasia patients in 1981 described a direct trans-mucosal lower esophageal sphincter myotomy and good clinical, radiologic and manometric results; there were no confirmatory work perhaps related to complications such as perforation and mediastinitis[5]. Natural orifice transluminal endoscopic surgery (NOTES) came to the fore in 2004 and there has been a push to design endoscopic less traumatic alternatives to traditional transcutaneous surgical interventions. Thus the concept of a submucosal tunnel closed by a mucosal flap with access to the mediastinum or the peritoneum was formulated[6]. Interventions on the esophageal muscularis could be performed at a distance from a mucosal entry point, which is then closed at the procedure termination. The concept was implicated in 2007 to perform a LES myotomy in a porcine survival model[7]. In 2008, Inoue used the technique of submucosal tunneling to perform the first human endoscopic LES myotomy for achalasia and coined the term POEM for per oral endoscopic myotomy[8]. Our group performed the first human POEM outside Japan in 2009[9]. There is a rapidly increasing international experience with over fifty centers now performing POEM. An international survey (IPOEMS) was performed describing the global POEM experience through July 2012[10].
INDICATIONS AND CONTRAINDICATIONS
Patients considered for POEM therapy must have a high-quality (preferably high resolution) esophageal manometry to define their specific motor abnormality as this will dictate both their eligibility for POEM and specifics of the procedure. POEM is performed predominantly for achalasia, but this technique has also been successfully applied in diffuse esophageal spasm, nutcracker and jackhammer esophagus[11,12]. The international survey (IPOEMS) revealed that 28% of the 841 reported POEMs performed by the 16 reporting centers, were performed for hypertensive esophageal motor disorders disorders including DES, hypertensive LES, nutcracker and jackhammer esophagus[10]. The consensus from IPOEMS and other studies is that POEM has significant efficacy in nutcracker esophagus, hypertensive LES, DES and type III (spastic) achalasia[10-13]. POEM seems to be more helpful in diminishing dysphagia than the chest pain associated with these disorders[13]. POEM may be ideally suited in the treatment of patients with hypertensive esophageal motor disorders other than achalasia because in those disorders often a longer myotomy is required than can be achieved via the laparoscopic approach.
Experienced POEM operators can also now successfully treat patients with prior Heller myotomy and previous endoscopic intervention including botulinum injection and pneumatic dilation[14,15]. Forty-three percent of subjects in the IPOEMS database had prior intervention (BTI, PD, LHM)[10]. The consensus was that that the cases were more technically challenging, but there was similar good efficacy with few adverse events as the total subjects group. Subsequent smaller reported studies are consistent with these findings[14,15].
POEM has been performed throughout the age spectrum[10,16]. Most experienced operators will consider POEM in the gamut of achalasia subtypes, achalasia with “sigmoid” esophagus and medically fragile patients. POEM has been performed in post-gastric bypass patients with achalasia[17]. POEM contraindications by consensus include severe pulmonary disease, esophageal irradiation, esophageal malignancy, bleeding disorders including coagulopathy and recent esophageal surgery or endoscopic intervention including endoscopic mucosal resection and endoscopic submucosal dissection (ESD)[10].
POEM TECHNIQUE
POEM was developed from a technique devised to access the mediastinum in NOTES[6]. POEM features the creation of a submucosal tunnel enabling the LES myotomy to be performed away from the mucosal entry site. The procedure requires equipment employed in ESD with capability for dissection, cutting, coagulation and infusion of volume-expanders within the submucosal space. POEM is performed with general anesthesia with the patient usually in the supine position. Carbon dioxide is used for insufflation utilizing a high-definition forward-viewing gastroscope with accessory water jet for irrigation with an attached clear cap. The esophageal submucosal space is expanded with injection of an indigo carmine-saline mixture[18]. The submucosal tunnel is typically initiated 10-15 cm above the gastroesophageal junction (GEJ). The submucosal space is entered by the gastroscope after a small electrosurgical cut and subsequently a submucosal tunnel is dissected using ESD technique for creation of a conduit to the GEJ and the lower esophageal sphincter. The submucosal tunnel is extended into the gastric cardia 2-3 cm distal to the GEJ. Delineation of the GEJ while in the tunnel is done in a variety of ways including monitoring endoscope insertion length, visually noting changes in tunnel diameter and vascularity, tactile feedback and even transillumination viewed by a second endoscope[19]. Then the myotomy is performed starting 2-3 centimeters distal to the mucosal entry point. The final critical step is closure of the tunnel at the mucosal entry point. Figure 1 demonstrates the critical steps in the POEM technique. We have presented a detailed explanation of the technique in video format elsewhere (VJGIEN, 2013)[20]. Patients typically have a post-procedural contrast study to exclude complications such as perforations and may be discharged the following day if clinically well including ingestion of clear liquids. Antibiotics are given during the POEM and continued for several days after discharge.
Figure 1.
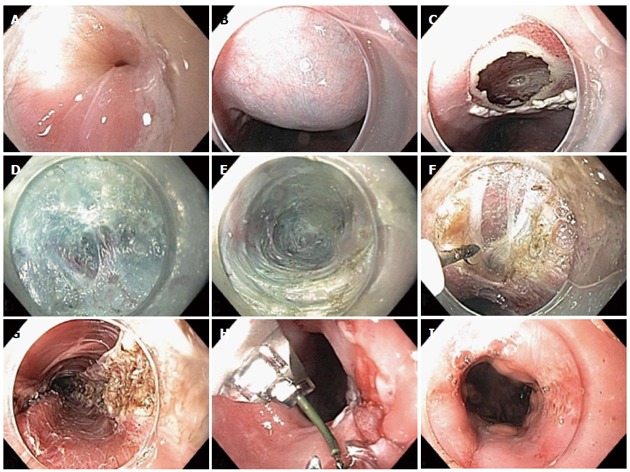
Per-oral endoscopic myotomy technique. A: Prior to per-oral endoscopic myotomy (POEM), there is evidence of a tightly puckered lower esophageal sphincter (LES); B: Submucosal injection is performed with saline stained with indigo carmine; C: Mucosotomy is performed along the right anterior wall of the esophagus; D: Submucosal dissection is performed with hybrid knife; E: Submucosal tunnel is extended into the gastric cardia; F: Myotomy is intiated 2 cm below site of mucosotomy; G: Final full thickness myotomy is seen as endoscope is withdrawn from the submucosal tunnel; H: Mucosotomy is closed with an endoscopic suturing device; I: After POEM, the LES appears patulous.
TECHNIQUE VARIATIONS
Individual POEM operators have generally evolved in their techniques. The Shanghai group has converted to carbon dioxide after frequent serious complications with room air, and this group touts the hybrid (inject/cautery) ESD knife for faster dissection during POEM[21,22]. Inoue prefers the triangular tip knife and initially performed more modest length circular muscle myotomies[16]. Our group initially employed balloon dilation in tunnel creation (lack of ESD knives in the US before 2011), but now electrocautery dissection is exclusively used and we are more comfortable with extended length circular and longitudinal full-thickness muscle dissection[9,23]. Most centers employ clips for closure of the mucosal defect at the tunnel initiation. We have used an endoscopic suture device (OverStitch™ Endoscopic Suturing System; Apollo Endosurgery Austin, Texas) (Figure 2) for our recent cases and this is also invaluable for inadvertent mucosal tunnel perforation[24]. Figure 3 demonstrates a mucosal flap injury at the GEJ closed effectively with the endoscopic suturing device without concern for delayed leak in the patient. In our series when we compared the last 25 consecutive mucosotomy closures using endoclips and endoscopic suturing, there was no statistically significant difference in mean closure time (clips 8.8 min vs suture 10.1 min, P = 0.1), complications or mean cost (clips $915.84 vs suturing $818, P = 0.2) (unpublished data) Closure has also been described with an over-the-scope clip and fibrin glue[25,26].
Figure 2.

OverStitch endoscopic suturing system (Courtesy of Apollo Endosurgery, Austin Texas).
Figure 3.
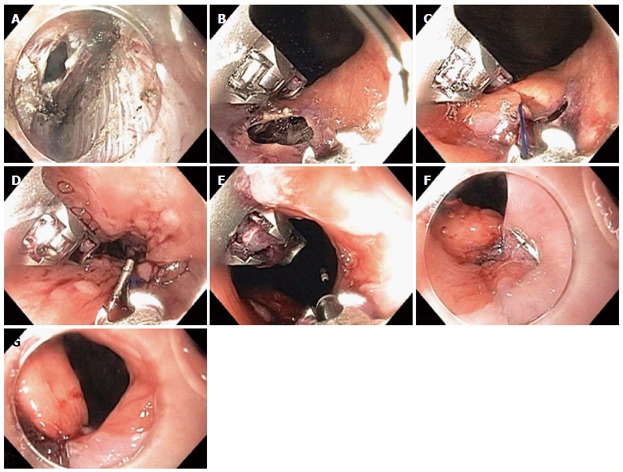
Closure of gastroesophageal junction mucosal perforation with endoscopic suturing device. A: Inadvertent mucosal perforation at the gastroesophageal junction (GEJ) seen within the submucosal tunnel; B: Inadvertent mucosal perforation at the GEJ seen endoluminally; C: Endoscopic suture-initial “bite”; D: Suture closure; E: Cinch T-tag is deployed; F: Endoscopic suturing achieved secure closure of the perforation; G: Patulous lower esophageal sphincter.
There are POEM controversies regarding the orientation and extent of LES dissection. The human LES has several components that include a weaker clasp (circular) fiber part on the lesser curvature of the stomach centered at 2 o’clock (using the convention of 12 o’clock being the most anterior point) and a sling (oblique) fiber part on the left posterior lateral wall of the LES at 7 o’clock and draping over the anterior and posterior walls at 5 and 11 o’clock respectively[27]. These sling fibers are a significant barrier to reflux. Laparoscopic Heller Myotomy is often performed anteriorly at 11-12 o’clock and thus partially transects the sling fibers at 11 o’clock and thus GERD is common after LHM. Currently, most POEM operators reportedly perform myotomy at 2 o’clock, which may theoretically minimize post-procedure reflux, but be less efficacious as LES disruption is the main goal in achalasia surgery. We and others (Shanghai group) that employ a predominant 5 o’clock position for the myotomy may have less dysphagia because of sling fiber resection but could theoretically have more GERD. We believe most post-POEM patients with GERD will do well with medical therapy. A lesser controversy with a similar theme is whether to dissect the weaker longitudinal muscle component of the LES along with the LES circular muscle. Additional resection of this longitudinal muscle may promote post-POEM reflux, but a study on this issue found no difference between POEM patients who had the additional resection and those that did not in terms of dysphagia relief and GERD[28].
ENDOFLIP
The adequacy of the POEM can be grossly assessed by visualization and passage of the gastroscope. Our group and other assess the esophagogastric junction distensibility quantitatively with the EndoFLIP system intraoperatively to confirm that an adequate myotomy has been performed[29]. The endoluminal functional lumen imaging probe (EndoFLIP®)(Crospon Ltd., Galway, Ireland) device is a balloon-tipped catheter that measures shape and compliance of the GEJ using impedance planimetry. It determines minimal luminal diameter and cross-sectional area (CSA) at the level of the LES. Real time quantitative assessment of GEJ distensibility can be calculated by dividing CSA by the balloon pressure that is also recorded by the device. This may assist in confirming that adequate myotomy has been achieved and possibly predict degree of dysphagia relief. A recent study by Rohof and colleagues demonstrated that GEJ distensibility more closely correlated with symptomatic recurrence after interventions for achalasia than manometry[30]. In our series, there was a patient who required additional LES dissection in another plane based on this data[23]. Using EndoFLIP intraoperative assessment in 43 POEMs at a 30 mL balloon inflation, there was a mean 3.5 fold increase in GEJ distensibility[31]. Figure 4 demonstrates nearly a two fold increase in Dmin diameter as well as three fold increase in cross-sectional area after myotomy. In a small but provocative study, intraoperative Endoflip measurements suggested that LHM requires more of a proximal esophageal myotomy to reduce GEJ distensibility than POEM[32].
Figure 4.
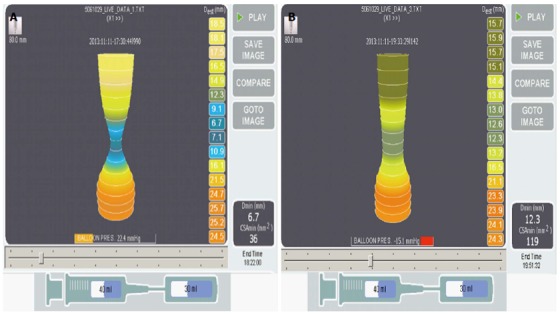
EndoFLIP Images before and after per-oral endoscopic myotomy. Seventy-seven years old man with achalasia for 4 years, prior Botox × 1, esophageal diameter of 5 cm, non-sigmoid, underwent per-oral endoscopic myotomy (POEM), 8 cm posterior myotomy. A: EndoFLIP performed immediately prior to POEM; B: immediately after POEM at 30 mL balloon volume shows an excellent response with increase of the minimal diameter at the gastroesophageal junction (GEJ) (Dmin) from 6.7 to 12.3 cm and increase in cross-sectional diameter at the GEJ (cross-sectional area) from 36 to 119 mm2.
EFFICACY AND SAFETY
The global results of POEM have been superb with dysphagia efficacy (using Eckardt score) in > 90% of subjects and no reported mortality in > 1000 patients[10,13,31,33-40] (Table 1). More limited data from these studies and smaller ones suggest significant diminution of LES pressure after POEM. Only a small number of studies have reported efficacy based on objective assessment of esophageal emptying by timed barium esophagram. However, their results confirm the high efficacy of the procedure (Table 1). We have performed > 130 cases with similar efficacy and safety.
Table 1.
Overview of peroral endoscopic myotomy efficacy and gastro-esophageal reflux disease data
| Location primary investigator | Patients (n) | Mean age (yr) | Eckardt score (pre/post) | LES pressure (pre/post) (mmHg) | Follow-up (mo) | Timed barium esophagram | Efficacy | Objective GERD evidence n (%) |
| Costamagna et al[34], Rome, Italy | 11 | 41 (23-68) | 7.1/1.1 | 45.1/16.9 | 3 | 100% | ||
| Swanstrom et al[13], Portland, Oregon | 18 | 59 (22-88) | 6/0 | 45/16.8 | 6 | Median emptying at 5 min 15/16: 80%-100% emptying 1/16 less than 80% emptying | 94% | Esophagitis (Grade 1 Savory-Miller classification) |
| 4/14 (28) | ||||||||
| +pH study | ||||||||
| 6/13 (46) | ||||||||
| Chiu et al[35], Hong Kong, China | 16 | 47 (22-87) | 5.5/0 | 43.6/29.8 | 3 | 100% | +pH study 3/15 (20) | |
| Hungness et al[36], Chicago, Illinois | 18 | 38 (22-69) | 7/1 | 19/9 | 63 | Median height | 89% | Esophagitis |
| 1 min 7 cm (0-15 cm) | Los Angeles (LA) class | |||||||
| 2 min 5 (0-13 cm) | A 2/15 (13.3) | |||||||
| 5 min 0 (0-9 cm) (P < 0.001) | B 2/15 (13.3) | |||||||
| C 1/15 (6.7) | ||||||||
| Minami et al[37], Nagasaki, Japan | 28 | 52 (19-84) | 6.7/0.7 | 71.2/21 | 163 | 100% | Esophagitis (11/28) 39.3% | |
| LA class | ||||||||
| M 2/28 | ||||||||
| A 7/28 | ||||||||
| B 1/28 | ||||||||
| C 1/28 | ||||||||
| Von Renteln et al[38], European MCT | 70 | 45 | 6.9/1 | 27.6/8.9 | 12 | 82% | Esophagitis (42) | |
| LA class | ||||||||
| A 29.2% | ||||||||
| B 12.3% | ||||||||
| Stavropoulos et al[31], Mineola, New York1 | 100 | 52 (17-93) | 7.8/0.2 | 44.2/17.6 | 13.32 | Mean emptying at 5 min | 98% | Esophagitis |
| 31/42: 100% emptying | 17/53 (32) | |||||||
| 41/42: > 50% emptying | +pH study | |||||||
| 17/52 (33) | ||||||||
| Onimaru et al[39], Yokohama, Japan1 | 300 | 45 (3-87) | 6.13/1.33 | 27.3/13.4 | 12 | 98% | ||
| Verlaan et al[40], Amsterdam, Netherlands | 10 | 43 | 8/1 | 20.5/6.8 | 3 | Median height | 100% | Esophagitis (60%) |
| 1 min 3.2 cm (IQR 0.5-6.5) (P = 0.005) | LA class | |||||||
| 2 min 2.7 cm (IQR 0.4-5.2) (P = 0.005) | A 3/10 (30) | |||||||
| 5 min 2.3 cm (IQR 0-3.2) (P = 0.005) | B 3/10 (30) |
Abstract;
Mean;
Median, remainder are minimum follow-up. GERD: Gastroesophageal reflux disease; LES: Lower esophageal sphincter; IQR: Interquartile range.
GERD as defined by symptoms and available pH and endoscopy data is the most prevalent adverse event after POEM, though prevalence varied widely[10,13,23,31,35-38,40]. In the European multicenter POEM study, esophagitis was in noted in 42% of subjects though was usually mild[38]. A small study suggested almost 40% of POEM subjects had abnormal acid exposure on pH testing, but this was similar to LHM subjects[41]. Insufflation related complications are less common with CO2 insufflation[42]. Damage to overlying esophageal mucosa seems to be the common technical concern for the POEM operator. Modest rents can usually be remedied with clips or endoscopic suturing[24]. Bleeding in the tunnel is unusual but may require reentry for hemostasis[26].
Comparison to laparoscopic Heller myotomy
There is a lack of long-term efficacy of POEM generally and in relation to LHM or PD. There are no randomized controlled trials comparing POEM to LHM. One prospective series compared 18 POEM and 21 LHM subjects and noted no difference in operative time, myotomy length, relief of dysphagia or complications (each group had one perforation), but the POEM subjects had less postoperative pain and quicker return to work[43]. However, another group comparing 34 POEM to 64 LHM subjects found the POEM group to have less operative time, lower postoperative Eckardt scores, lower LES pressures, less length of stay and less dysphagia at six month follow-up[41]. A third series comparing 70 POEM and 110 LHM subjects found lower Eckardt and LES scores in the POEM group with no significant difference in erosive esophagitis[44]. More such comparative studies with longer follow-up are expected.
FUTURE PERSPECTIVES
There is current intense investigation in comparing POEM and LHM for achalasia, but long term data for POEM is lacking[13,41]. The available comparison bodes well for POEM with relative shorter operative times and hospital stays, lower cost and greater patient satisfaction[36]. Diminishing efficacy of POEM with time is a concern, but more studies are needed[38]. There is controversy regarding POEM operator background and training as well as credentialing. The apparent success of POEM has fueled some of this debate. Most POEM operators in the US and the world are surgeons[10]. Yet our group and others feature gastroenterologists with an impressive track record[23]. The Inoue group feels that extensive animal model practice in paramount for POEM success[45]. Two American “learning curve” studies were small and yielded somewhat conflicting results[46,47].
POEM OFFSHOOTS: OTHER RAPIDLY GROWING APPLICATIONS OF THE SUBMUCOSAL TUNNEL
POEM was derived from earlier NOTES experiments[5], but currently POEM is more clinically advanced and more widely adopted than any other NOTES procedure. NOSCAR has recently completed a comprehensive “White Paper” on POEM as a demonstration of this procedure’s prominence[48]. More currently relevant is that the success of POEM has spurred interest and development in ESD; especially in the US[49]. Arguably POEM has contributed more to ESD adoption in the US in the past few years than over 10 years of presentations and publications by Japanese and other Asian endoscopists. However, the impact of POEM extends even further. POEM offers a controlled standardized setting for gastroenterologists to familiarize themselves with previously taboo spaces such as the mediastinum and peritoneum and become adept in fundamentals of NOTES such as managing insufflation (capnoperitoneum, capnomediastinum) and achieving secure closure of full thickness breeches of the GI lumen. Thus, the success of POEM has inspired other NOTES offshoots such as submucosal tunneling endoscopic resection (STER) to achieve full-thickness en bloc resection of muscularis based subepithelial tumors (Figure 5). Guidelines recommend resection of many of these tumors when they are larger than 2-3 cm, particularly if they are suspected to be gastrointestinal stromal tumors or if they are causing symptoms, increasing in size on surveillance or have high risk features on biopsy, endoscopic ultrasound (EUS) or computed tomography. Surgery can be difficult requiring resection of large portions of an organ such as partial gastrectomy or esophagectomy even for small tumors, especially those located in the esophagus, GE junction, pylorus or other challenging locations. For low risk lesions ≤ 2 cm, often endoscopic/endosonographic life-long surveillance is pursued. This overall approach generates a large burden of surgery and endoscopy for subepithelial tumors (SETs) less than 5 cm, the majority of which represent low risk lesions. STER may allow minimally invasive resection of submucosal tumors less than 3-4 cm and is especially appropriate for tumors in challenging locations for the surgeon including the GE junction, esophagus and gastric cardia. It offers a less invasive approach to resection for tumors requiring resection. For small tumors that were destined for surveillance it offers definitive histologic diagnosis (which not infrequently eludes standard endoscopic sampling such as EUS-guided fine needle aspiration). Furthermore, by achieving en bloc resection of these small low risk tumors it allows definitive histologic confirmation (including mitotic rate) of their benign nature and eliminates the need for life-long surveillance. It is not surprising that the initial reports of this technique originated at the two most prominent Asian POEM centers. Inoue et al[50] from Yokohama, and Li et al[51] from Shanghai reported their respective initial successes utilizing submucosal tunneling to safely and effectively achieve endoscopic resection of muscularis propria based submucosal tumors in a small series of patients. The Shanghai group subsequently reported their series of 290 patients with follow-up for 4 years showing no residual tumor, local tumor recurrence or distant metastasis[52]. Our group performed the first STER in the US in September 2012. Our small series of patients also supports that STER is a safe and feasible method for removing muscularis propria based SETs[53] (Table 2).
Figure 5.
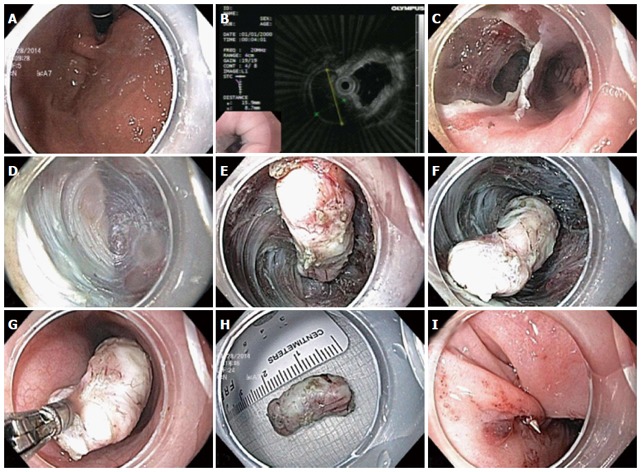
Submucosal tunneling endoscopic resection technique. A: Gastroesophageal junction lesion seen on retroflexion during endoscopy; B: Endoscopic ultrasound probe demonstrates hypoechoic muscularis propria based lesion; C: Creation of submucosal tunnel parallel to esophageal lumen; D: Endoscopic submucosal dissection (ESD) with submucosal tunnel; E-F: Freeing of submucosal lesion via ESD; G: Removal of submucosal lesion from tunnel with biopsy forceps; H: 2.5 cm leiomyoma; I: Endoscopic sutured closure of mucosal entrance to tunnel.
Table 2.
Characteristics of United States single center submucosal tunneling endoscopic resection series n (%)
| Characteristics | Value |
| STER cases (n) | 7 |
| Time period | 9/2013-4/2014 |
| Mean age (yr) | 52 (47-62) |
| Gender | 3 males: 4 females |
| ASA classification | |
| II | 6 (86) |
| III | 1 (14) |
| Location of lesion | 4 GE junction; 2 esophagus; 1 gastric cardia |
| General anesthesia | 100% |
| Procedure time (min) | 53 (23-80) |
| Closure technique | 2 clips (29); 5 endoscopic suture (71) |
| Histopathology | 6 leiomyoma (86); 1 GIST (2/50 hpf) (14) |
| Mean size (cm) | 1.5 (1-2.7) |
| En bloc resection | 100% |
| Length of hospital stay (d) | 2.3 (1-4) |
| Follow-up | 100% no recurrence |
| Complications | 1 mucosotomy required clipping |
| 1 stricture at submucosal tunnel site responded to balloon dilation at 4 wk |
GE: Gastroesophageal; STER: Submucosal tunneling endoscopic resection; ASA: American Society of Anesthesiologists.
The principle of the submucosal tunnel technique has been adapted to perform wide resections of mucosal lesions (early cancers) in the esophagus. In a series of five patients, en bloc resection of superficial esophageal cancer was achieved in all without evidence of recurrence or complications including dysphagia at follow-up between 3-13 mo[54]. In a larger series of 25 superficial esophageal cancers, 92% en bloc resection was achieved with two patients having intramucosal carcinoma recurrence requiring further treatment at mean follow-up 22 mo[55].
There is a report from a small series employing submucosal tunnel endoscopy under conscious sedation to safely and effectively explore the peritoneal and thoracic cavities through transgastric peritoneoscopy[56].
Lastly, peroral pyloromyotomy (POP) using a tunneled approach very similar to that used to cut the lower esophageal sphincter in POEM, has been proposed as a potential therapy for gastroparesis[57]. Studies are in progress at a number of centers. If POP proves effective for even a subset of gastroparesis patients, it may have a large impact on the therapy of this challenging disease.
CONCLUSION
In conclusion, POEM has the potential to be the preferred modality for achalasia and related esophageal motor disorders when personnel and logistics allow. Many questions remain regarding POEM, but its future is bright. The impact of POEM is extending far beyond the narrow domain of esophageal motility disorders. As the first successful clinical application of submucosal endoscopy it is now spawning many other NOTES interventions utilizing a submucosal tunnel approach.
Footnotes
P- Reviewer: Aytac E, Scheidbach H S- Editor: Gou SX L- Editor: A E- Editor: Liu XM
References
- 1.Boeckxstaens GE, Annese V, des Varannes SB, Chaussade S, Costantini M, Cuttitta A, Elizalde JI, Fumagalli U, Gaudric M, Rohof WO, et al. Pneumatic dilation versus laparoscopic Heller’s myotomy for idiopathic achalasia. N Engl J Med. 2011;364:1807–1816. doi: 10.1056/NEJMoa1010502. [DOI] [PubMed] [Google Scholar]
- 2.Weber CE, Davis CS, Kramer HJ, Gibbs JT, Robles L, Fisichella PM. Medium and long-term outcomes after pneumatic dilation or laparoscopic Heller myotomy for achalasia: a meta-analysis. Surg Laparosc Endosc Percutan Tech. 2012;22:289–296. doi: 10.1097/SLE.0b013e31825a2478. [DOI] [PubMed] [Google Scholar]
- 3.Campos GM, Vittinghoff E, Rabl C, Takata M, Gadenstätter M, Lin F, Ciovica R. Endoscopic and surgical treatments for achalasia: a systematic review and meta-analysis. Ann Surg. 2009;249:45–57. doi: 10.1097/SLA.0b013e31818e43ab. [DOI] [PubMed] [Google Scholar]
- 4.Agarwal AK, Javed A. Laparoscopic esophagogastroplasty: a minimally invasive alternative to esophagectomy in the surgical management of megaesophagus with axis deviation. Surg Endosc. 2013;27:2238–2242. doi: 10.1007/s00464-012-2751-0. [DOI] [PubMed] [Google Scholar]
- 5.Ortega JA, Madureri V, Perez L. Endoscopic myotomy in the treatment of achalasia. Gastrointest Endosc. 1980;26:8–10. doi: 10.1016/s0016-5107(80)73249-2. [DOI] [PubMed] [Google Scholar]
- 6.Sumiyama K, Tajiri H, Gostout CJ. Submucosal endoscopy with mucosal flap safety valve (SEMF) technique: a safe access method into the peritoneal cavity and mediastinum. Minim Invasive Ther Allied Technol. 2008;17:365–369. doi: 10.1080/13645700802528512. [DOI] [PubMed] [Google Scholar]
- 7.Pasricha PJ, Hawari R, Ahmed I, Chen J, Cotton PB, Hawes RH, Kalloo AN, Kantsevoy SV, Gostout CJ. Submucosal endoscopic esophageal myotomy: a novel experimental approach for the treatment of achalasia. Endoscopy. 2007;39:761–764. doi: 10.1055/s-2007-966764. [DOI] [PubMed] [Google Scholar]
- 8.Inoue H, Minami H, Satodate H, Kudo SE. First Clinical Experience of Submucosal Endoscopic esophageal myotomy for esophageal achalasia with no skin incision. Gastrointest Endosc. 2009;69:AB122. [Google Scholar]
- 9.Stavropoulos SN, Harris MD, Hida S, Brathwaite C, Demetriou C, Grendell J. Endoscopic submucosal myotomy for the treatment of achalasia (with video) Gastrointest Endosc. 2010;72:1309–1311. doi: 10.1016/j.gie.2010.04.016. [DOI] [PubMed] [Google Scholar]
- 10.Stavropoulos SN, Modayil RJ, Friedel D, Savides T. The International Per Oral Endoscopic Myotomy Survey (IPOEMS): a snapshot of the global POEM experience. Surg Endosc. 2013;27:3322–3338. doi: 10.1007/s00464-013-2913-8. [DOI] [PubMed] [Google Scholar]
- 11.Minami H, Isomoto H, Yamaguchi N, Ohnita K, Takeshima F, Inoue H, Nakao K. Peroral endoscopic myotomy (POEM) for diffuse esophageal spasm. Endoscopy. 2014;46 Suppl 1 UCTN:E79–E81. doi: 10.1055/s-0032-1309922. [DOI] [PubMed] [Google Scholar]
- 12.Kandulski A, Fuchs KH, Weigt J, Malfertheiner P. Jackhammer esophagus: high-resolution manometry and therapeutic approach using peroral endoscopic myotomy (POEM) Dis Esophagus. 2014:Epub ahead of print. doi: 10.1111/dote.12182. [DOI] [PubMed] [Google Scholar]
- 13.Swanstrom LL, Kurian A, Dunst CM, Sharata A, Bhayani N, Rieder E. Long-term outcomes of an endoscopic myotomy for achalasia: the POEM procedure. Ann Surg. 2012;256:659–667. doi: 10.1097/SLA.0b013e31826b5212. [DOI] [PubMed] [Google Scholar]
- 14.Zhou PH, Li QL, Yao LQ, Xu MD, Chen WF, Cai MY, Hu JW, Li L, Zhang YQ, Zhong YS, et al. Peroral endoscopic remyotomy for failed Heller myotomy: a prospective single-center study. Endoscopy. 2013;45:161–166. doi: 10.1055/s-0032-1326203. [DOI] [PubMed] [Google Scholar]
- 15.Sharata A, Kurian AA, Dunst CM, Bhayani NH, Reavis KM, Swanström LL. Peroral endoscopic myotomy (POEM) is safe and effective in the setting of prior endoscopic intervention. J Gastrointest Surg. 2013;17:1188–1192. doi: 10.1007/s11605-013-2193-6. [DOI] [PubMed] [Google Scholar]
- 16.Familiari P, Marchese M, Gigante G, Boskoski I, Tringali A, Perri V, Costamagna G. Peroral endoscopic myotomy for the treatment of achalasia in children. J Pediatr Gastroenterol Nutr. 2013;57:794–797. doi: 10.1097/MPG.0b013e3182a803f7. [DOI] [PubMed] [Google Scholar]
- 17.Yang D, Draganov PV. Peroral endoscopic myotomy (POEM) for achalasia after Roux-en-Y gastric bypass. Endoscopy. 2014;46 Suppl 1 UCTN:E11–E12. doi: 10.1055/s-0033-1359140. [DOI] [PubMed] [Google Scholar]
- 18.Inoue H, Tianle KM, Ikeda H, Hosoya T, Onimaru M, Yoshida A, Minami H, Kudo SE. Peroral endoscopic myotomy for esophageal achalasia: technique, indication, and outcomes. Thorac Surg Clin. 2011;21:519–525. doi: 10.1016/j.thorsurg.2011.08.005. [DOI] [PubMed] [Google Scholar]
- 19.Baldaque-Silva F, Marques M, Vilas-Boas F, Maia JD, Sá F, Macedo G. New transillumination auxiliary technique for peroral endoscopic myotomy. Gastrointest Endosc. 2014;79:544–545. doi: 10.1016/j.gie.2013.10.023. [DOI] [PubMed] [Google Scholar]
- 20.Stavropoulos SN, Iqbal S, Modayil R, Dejesus D. Per oral endoscopic myotomy, equipment and technique: A step-by-step explanation. VJGIEN. 2013;1:96–100. [Google Scholar]
- 21.Ren Z, Zhong Y, Zhou P, Xu M, Cai M, Li L, Shi Q, Yao L. Perioperative management and treatment for complications during and after peroral endoscopic myotomy (POEM) for esophageal achalasia (EA) (data from 119 cases) Surg Endosc. 2012;26:3267–3272. doi: 10.1007/s00464-012-2336-y. [DOI] [PubMed] [Google Scholar]
- 22.Cai MY, Zhou PH, Yao LQ, Xu MD, Zhong YS, Li QL, Chen WF, Hu JW, Cui Z, Zhu BQ. Peroral endoscopic myotomy for idiopathic achalasia: randomized comparison of water-jet assisted versus conventional dissection technique. Surg Endosc. 2014;28:1158–1165. doi: 10.1007/s00464-013-3300-1. [DOI] [PubMed] [Google Scholar]
- 23.Friedel D, Modayil R, Iqbal S, Grendell JH, Stavropoulos SN. Per-oral endoscopic myotomy for achalasia: An American perspective. World J Gastrointest Endosc. 2013;5:420–427. doi: 10.4253/wjge.v5.i9.420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Modayil R, Friedel D, Stavropoulos SN. Endoscopic suture repair of a large mucosal perforation during peroral endoscopic myotomy for treatment of achalasia. Gastrointest Endosc. 2014;80:1169–1170. doi: 10.1016/j.gie.2014.03.035. [DOI] [PubMed] [Google Scholar]
- 25.Saxena P, Chavez YH, Kord Valeshabad A, Kalloo AN, Khashab MA. An alternative method for mucosal flap closure during peroral endoscopic myotomy using an over-the-scope clipping device. Endoscopy. 2013;45:579–581. doi: 10.1055/s-0032-1326398. [DOI] [PubMed] [Google Scholar]
- 26.Li H, Linghu E, Wang X. Fibrin sealant for closure of mucosal penetration at the cardia during peroral endoscopic myotomy (POEM) Endoscopy. 2012;44 Suppl 2 UCTN:E215–E216. doi: 10.1055/s-0032-1309358. [DOI] [PubMed] [Google Scholar]
- 27.Stein HJ, Liebermann-Meffert D, DeMeester TR, Siewert JR. Three-dimensional pressure image and muscular structure of the human lower esophageal sphincter. Surgery. 1995;117:692–698. doi: 10.1016/s0039-6060(95)80014-x. [DOI] [PubMed] [Google Scholar]
- 28.Li QL, Chen WF, Zhou PH, Yao LQ, Xu MD, Hu JW, Cai MY, Zhang YQ, Qin WZ, Ren Z. Peroral endoscopic myotomy for the treatment of achalasia: a clinical comparative study of endoscopic full-thickness and circular muscle myotomy. J Am Coll Surg. 2013;217:442–451. doi: 10.1016/j.jamcollsurg.2013.04.033. [DOI] [PubMed] [Google Scholar]
- 29.Rieder E, Swanström LL, Perretta S, Lenglinger J, Riegler M, Dunst CM. Intraoperative assessment of esophagogastric junction distensibility during per oral endoscopic myotomy (POEM) for esophageal motility disorders. Surg Endosc. 2013;27:400–405. doi: 10.1007/s00464-012-2484-0. [DOI] [PubMed] [Google Scholar]
- 30.Rohof WO, Hirsch DP, Kessing BF, Boeckxstaens GE. Efficacy of treatment for patients with achalasia depends on the distensibility of the esophagogastric junction. Gastroenterology. 2012;143:328–335. doi: 10.1053/j.gastro.2012.04.048. [DOI] [PubMed] [Google Scholar]
- 31.Stavropoulos SN, Modayil R, Brathwaite CE, Halwan B, Taylor SI, Coppola T, Long D, Friedel D, Grendell JH. Per Oral Endoscopic Myotomy (POEM) for Achalasia: Large Single-Center 4-Year Series by a Gastroenterologist With Emphasis on Objective Assessment of Emptying, GERD, LES Distensibility and Post-Procedural Pain. Gastrointest Endosc. 2014;79:AB365. [Google Scholar]
- 32.Teitelbaum EN, Soper NJ, Pandolfino JE, Kahrilas PJ, Boris L, Nicodème F, Lin Z, Hungness ES. An extended proximal esophageal myotomy is necessary to normalize EGJ distensibility during Heller myotomy for achalasia, but not POEM. Surg Endosc. 2014;28:2840–2847. doi: 10.1007/s00464-014-3563-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Zhou PH, Cai MY, Yao LQ, Zhong YS, Ren Z, Xu MD, Chen WF, Qin XY. [Peroral endoscopic myotomy for esophageal achalasia: report of 42 cases] Zhonghua Weichang Waike Zazhi. 2011;14:705–708. [PubMed] [Google Scholar]
- 34.Costamagna G, Marchese M, Familiari P, Tringali A, Inoue H, Perri V. Peroral endoscopic myotomy (POEM) for oesophageal achalasia: preliminary results in humans. Dig Liver Dis. 2012;44:827–832. doi: 10.1016/j.dld.2012.04.003. [DOI] [PubMed] [Google Scholar]
- 35.Chiu PW, Wu JC, Teoh AY, Chan Y, Wong SK, Liu SY, Yung MY, Lam CC, Sung JJ, Chan FK, et al. Peroral endoscopic myotomy for treatment of achalasia: from bench to bedside (with video) Gastrointest Endosc. 2013;77:29–38. doi: 10.1016/j.gie.2012.08.018. [DOI] [PubMed] [Google Scholar]
- 36.Hungness ES, Teitelbaum EN, Santos BF, Arafat FO, Pandolfino JE, Kahrilas PJ, Soper NJ. Comparison of perioperative outcomes between peroral esophageal myotomy (POEM) and laparoscopic Heller myotomy. J Gastrointest Surg. 2013;17:228–235. doi: 10.1007/s11605-012-2030-3. [DOI] [PubMed] [Google Scholar]
- 37.Minami H, Isomoto H, Yamaguchi N, Matsushima K, Akazawa Y, Ohnita K, Takeshima F, Inoue H, Nakao K. Peroral endoscopic myotomy for esophageal achalasia: clinical impact of 28 cases. Dig Endosc. 2014;26:43–51. doi: 10.1111/den.12086. [DOI] [PubMed] [Google Scholar]
- 38.Von Renteln D, Fuchs KH, Fockens P, Bauerfeind P, Vassiliou MC, Werner YB, Fried G, Breithaupt W, Heinrich H, Bredenoord AJ, et al. Peroral endoscopic myotomy for the treatment of achalasia: an international prospective multicenter study. Gastroenterology. 2013;145:309–11.e1-e3. doi: 10.1053/j.gastro.2013.04.057. [DOI] [PubMed] [Google Scholar]
- 39.Onimaru M, Inoue H, Ikeda H, Yoshida A, Santi EG, Sato H, Ito H, Maselli R, Kudo SE. Peroral endoscopic myotomy is a viable option for failed surgical esophagocardiomyotomy instead of redo surgical Heller myotomy: a single center prospective study. J Am Coll Surg. 2013;217:598–605. doi: 10.1016/j.jamcollsurg.2013.05.025. [DOI] [PubMed] [Google Scholar]
- 40.Verlaan T, Rohof WO, Bredenoord AJ, Eberl S, Rösch T, Fockens P. Effect of peroral endoscopic myotomy on esophagogastric junction physiology in patients with achalasia. Gastrointest Endosc. 2013;78:39–44. doi: 10.1016/j.gie.2013.01.006. [DOI] [PubMed] [Google Scholar]
- 41.Bhayani NH, Kurian AA, Dunst CM, Sharata AM, Rieder E, Swanstrom LL. A comparative study on comprehensive, objective outcomes of laparoscopic Heller myotomy with per-oral endoscopic myotomy (POEM) for achalasia. Ann Surg. 2014;259:1098–1103. doi: 10.1097/SLA.0000000000000268. [DOI] [PubMed] [Google Scholar]
- 42.Li QL, Zhou PH, Yao LQ, Xu MD, Chen WF, Hu JW, Cai MY, Zhang YQ, Zhong YS, Qin WZ, et al. Early diagnosis and management of delayed bleeding in the submucosal tunnel after peroral endoscopic myotomy for achalasia (with video) Gastrointest Endosc. 2013;78:370–374. doi: 10.1016/j.gie.2013.04.172. [DOI] [PubMed] [Google Scholar]
- 43.Ujiki MB, Yetasook AK, Zapf M, Linn JG, Carbray JM, Denham W. Peroral endoscopic myotomy: A short-term comparison with the standard laparoscopic approach. Surgery. 2013;154:893–897; discussion 897-900. doi: 10.1016/j.surg.2013.04.042. [DOI] [PubMed] [Google Scholar]
- 44.Von Renteln D, Fuchs KH, Fockens P, Bauerfeind P, Vassiliou M, Werner Y, Gockel I, Fried G, Breithaupt W, Heinrich H, et al. Endoscopic versus Surgical Myotomy for Idiopathic Achalasia: Results of a Prospective Multicenter Study and Comparison with Laparoscopic Surgery. Gastrointest Endosc. 2013;77:AB122. [Google Scholar]
- 45.Eleftheriadis N, Inoue H, Ikeda H, Onimaru M, Yoshida A, Hosoya T, Maselli R, Kudo SE. Training in peroral endoscopic myotomy (POEM) for esophageal achalasia. Ther Clin Risk Manag. 2012;8:329–342. doi: 10.2147/TCRM.S32666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kurian AA, Dunst CM, Sharata A, Bhayani NH, Reavis KM, Swanström LL. Peroral endoscopic esophageal myotomy: defining the learning curve. Gastrointest Endosc. 2013;77:719–725. doi: 10.1016/j.gie.2012.12.006. [DOI] [PubMed] [Google Scholar]
- 47.Teitelbaum EN, Soper NJ, Arafat FO, Santos BF, Kahrilas PJ, Pandolfino JE, Hungness ES. Analysis of a learning curve and predictors of intraoperative difficulty for peroral esophageal myotomy (POEM) J Gastrointest Surg. 2014;18:92–98; discussion 98-99. doi: 10.1007/s11605-013-2332-0. [DOI] [PubMed] [Google Scholar]
- 48.Stavropoulos SN, Desilets DJ, Fuchs KH, Gostout CJ, Haber G, Inoue H, Kochman ML, Modayil R, Savides T, Scott DJ, et al. Per-oral endoscopic myotomy white paper summary. Gastrointest Endosc. 2014;80:1–15. doi: 10.1016/j.gie.2014.04.014. [DOI] [PubMed] [Google Scholar]
- 49.Inoue H, Santi EG, Onimaru M, Kudo SE. Submucosal endoscopy: from ESD to POEM and beyond. Gastrointest Endosc Clin N Am. 2014;24:257–264. doi: 10.1016/j.giec.2013.12.003. [DOI] [PubMed] [Google Scholar]
- 50.Inoue H, Ikeda H, Hosoya T, Onimaru M, Yoshida A, Eleftheriadis N, Maselli R, Kudo S. Submucosal endoscopic tumor resection for subepithelial tumors in the esophagus and cardia. Endoscopy. 2012;44:225–230. doi: 10.1055/s-0031-1291659. [DOI] [PubMed] [Google Scholar]
- 51.Li QL, Yao LQ, Zhou PH, Xu MD, Chen SY, Zhong YS, Zhang YQ, Chen WF, Ma LL, Qin WZ. Submucosal tumors of the esophagogastric junction originating from the muscularis propria layer: a large study of endoscopic submucosal dissection (with video) Gastrointest Endosc. 2012;75:1153–1158. doi: 10.1016/j.gie.2012.01.037. [DOI] [PubMed] [Google Scholar]
- 52.Wang XY, Xu MD, Yao LQ, Zhou PH, Pleskow D, Li QL, Zhang YQ, Chen WF, Zhong YS. Submucosal tunneling endoscopic resection for submucosal tumors of the esophagogastric junction originating from the muscularis propria layer: a feasibility study (with videos) Surg Endosc. 2014;28:1971–1977. doi: 10.1007/s00464-014-3420-2. [DOI] [PubMed] [Google Scholar]
- 53.Stavropoulos SN, Modayil R, Mehta C, Ghevariya V. Per Oral Full Thickness Endoscopic Resection of Muscularis Based Subepithelial Tumors. First cases at a US center. Gastrointest Endosc. 2013;77:AB116. [Google Scholar]
- 54.Linghu E, Feng X, Wang X, Meng J, Du H, Wang H. Endoscopic submucosal tunnel dissection for large esophageal neoplastic lesions. Endoscopy. 2013;45:60–62. doi: 10.1055/s-0032-1325965. [DOI] [PubMed] [Google Scholar]
- 55.Arantes V, Albuquerque W, Freitas Dias CA, Demas Alvares Cabral MM, Yamamoto H. Standardized endoscopic submucosal tunnel dissection for management of early esophageal tumors (with video) Gastrointest Endosc. 2013;78:946–952. doi: 10.1016/j.gie.2013.05.031. [DOI] [PubMed] [Google Scholar]
- 56.Lee SH, Kim SJ, Lee TH, Chung IK, Park SH, Kim EO, Lee HJ, Cho HD. Human applications of submucosal endoscopy under conscious sedation for pure natural orifice transluminal endoscopic surgery. Surg Endosc. 2013;27:3016–3020. doi: 10.1007/s00464-013-2844-4. [DOI] [PubMed] [Google Scholar]
- 57.Khashab MA, Stein E, Clarke JO, Saxena P, Kumbhari V, Chander Roland B, Kalloo AN, Stavropoulos S, Pasricha P, Inoue H. Gastric peroral endoscopic myotomy for refractory gastroparesis: first human endoscopic pyloromyotomy (with video) Gastrointest Endosc. 2013;78:764–768. doi: 10.1016/j.gie.2013.07.019. [DOI] [PubMed] [Google Scholar]


