Abstract
Background: Despite mortality rates that exceed those of most cancers, hospice remains underutilized in patients with end-stage renal disease (ESRD) on dialysis and nearly half of all dialysis patients die in the hospital.
Objective: To review the impact of advance care planning on withdrawal from dialysis, use of hospice, and location of death.
Design: Retrospective review.
Setting: A rural outpatient dialysis unit.
Participants: Former dialysis patients who died over a 5-year period.
Exposure: Advance care planning, the use of physician orders for life-sustaining therapy program (POLST).
Main Outcome and Measure: Use of hospice among patients withdrawing from dialysis, location of death.
Results: Advance care planning was associated with a low incidence of in-hospital death and among those who withdrew, a high use of hospice.
Conclusions and Relevance: Comprehensive and systematic advance care planning among patients with ESRD on dialysis promotes greater hospice utilization and may facilitate the chance that death will occur out of hospital.
Introduction
Mortality rates for end-stage renal disease (ESRD) patients on long-term hemodialysis exceed those of most cancers, and nearly half (44%) of all dialysis patient deaths occur in hospital.1 Although planned withdrawal from dialysis precedes death for many dialysis patients,2 less than half of those who withdraw (42%) use hospice3 and its use in the dialysis population overall (22%) is less than in patients dying of other terminal chronic illnesses such as cancer (25%) and heart failure (39%).2 Chronic failure to thrive (CFTT) constitutes the largest group of patients who withdraw from dialysis exceeding by 50% those who withdraw after an acute medical complication.2 We reviewed the use of advance care planning and its impact on withdrawal, location of death, and use of hospice among patients from a rural West Virginia dialysis unit under the care of providers with a keen interest in life transitions and end-of-life care.
Methods
Dialysis and medical records for patients dying between January 1, 2008 and December 31, 2012 were reviewed. All patients were under the outpatient care of a single nephrologist and dedicated nurse practitioner who had rounded at this unit for 9 and 7 years, respectively. Patients were seen weekly except in circumstances of hospitalization, patient travel, or rarely, provider scheduling conflicts. The dialysis unit is 62 miles distant to hospital dialysis availability and 94 miles from the closest tertiary care center. In addition to dialysis protocol-required signed statements elucidating resuscitation wishes should a cardiopulmonary arrest occur in the dialysis facility, all patients were queried on admission about prior completion of an advance directive and in addition, presented with a Physician Orders for Scope of Treatment (POST) form (which does not include dialysis but is similar to Physician Orders for Life-Sustaining Treatment [POLST] form in other states; www.polst.org).4 Medical records were reviewed for patient demographics, clinical characteristics, comorbid conditions, events prompting contemplation of withdrawal, and circumstances surrounding each patient's death.
Patients considered highly likely to die in the coming 6 months (for whom we answered the surprise question (“Would I be surprised if this patient died in the next 6 months?5 in the negative) were approached about withdrawal if they or their family had not approached us first. At the time of this review, estimates of survival were made by the Hemodialysis Mortality Predictor, an integrated prognostic model validated in hemodialysis patients that includes the surprise question.6,7 Patients who had been approached or who had approached us about withdrawal were categorically assigned a “no” to the surprise question; for patients who had not been approached were ascribed an affirmative answer. In addition to inclusion of the mortality predictor estimates that have an accuracy of 85% (C statistic=0.85), all patients had at least three additional triggers considered to be adequate criteria for assigning them to the CFFT group and prompting a withdrawal discussion.
A private office or conference room was the preferred site for advance care planning discussions, although when not possible, discussions took place chairside in the unit or in the hospital. Family members, including the medical power of attorney, were asked to participate. Advance directives and the POST were updated by the nurse practitioner in discussion with the physician when a change in medical status occurred. Discussions often included the nursing supervisor and the unit clerk, who has intimate involvement with families, their transportation, and is a conduit for communication when problems arise at home. Discussions were postponed or deferred if the sole reason for requesting withdrawal was untreated or unsuccessfully treated depression or a medical issue that was under treatment with the potential for improvement. Final decisions to withdraw were reaffirmed in conversations and discussed with designated family members or other caregivers. The POST form was updated to be consistent with the plan for withdrawal. The patient's preferred site of death was determined and discussed. Hospice was recommended for all patients and for those who chose to forgo the hospice benefit, a plan for attending to medical needs was established including clarification of caregivers. Patients' wishes for palliative sedation of refractory symptoms were discussed and clarified and the patient was apprised of the possibility that uremic symptoms might require additional medication.
Comparisons of demographic and clinical characteristics were performed using Fisher's exact test. Equality of means for all continuous variables was tested using the unequal variance t test.
Results
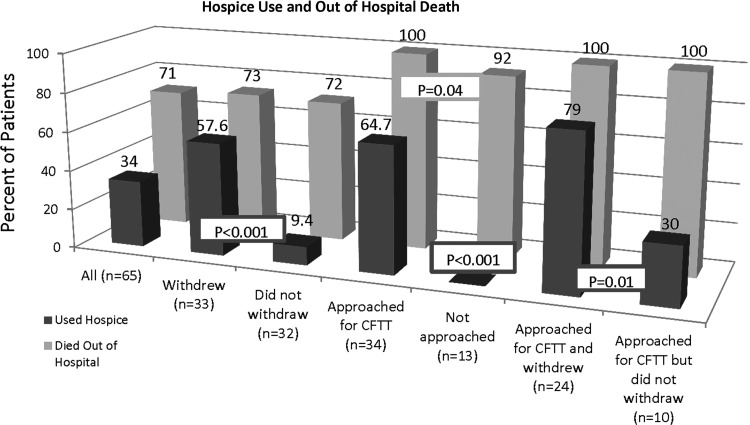
Sixty-five deaths occurred during the 5-year review period of which 46 (71%) occurred out of hospital and 33 (51%) followed withdrawal from dialysis. Demographic and clinical characteristics are presented in Table 1. All patients had completed the POST form. Hospice was engaged more frequently in patients who withdrew (57.6%) compared to those who did not withdraw (9.4%; p<0.001). The use of hospice and location of death are presented in Figure 1. Withdrawal discussions took place with 52 patients (80%), the majority of these (24 or 65%) for reasons related to chronic conditions or deteriorating status (CFTT); 18 patients (35%) were approached because of an acute event or during a hospitalization. No patient in the latter group engaged hospice and all patients died in hospital; among those patients in the CFTT group, 64.7% engaged hospice and no patient died in hospital, the majority (82.4%) dying at home. Four patients entered nursing homes and two a hospice house, none of whom died in the hospital. Among the CFTT group, patients who withdrew used hospice significantly more often than patients who did not (79.2% versus 30%; p=0.01). The majority of patients actively voiced their wish to die at home. Several were ambivalent but chose home when the time came. One patient preferred to die in the inpatient hospice facility and four others died in a nursing home as per their wish or because of lack of home support.
Table 1.
Clinical, Demographic, and Survival Characteristics of Patients Contemplating and Withdrawing from Dialysis
| Did not withdraw (n=32) | Withdrew (n=33) | p Value | Not approached (n=13) | Approached b/o CFTT (n=34) | p Value | Approached b/o CFTT but did not withdraw (n=10) | Approached b/o CFTT and withdrew (n=24) | p Value | |
|---|---|---|---|---|---|---|---|---|---|
| Years on dialysis | 2.8 (2.97) | 3 (3.5) | 0.81 | 3.4 (3.93) | 2.3 (2.51) | 0.35 | 2.5 (2.42) | 2.2 (2.59) | 0.7 |
| Age at start of dialysis | 61.1 (16.39) | 65.7 (10.34) | 0.18 | 56 (18.94) | 66 (13.29) | 0.1 | 64.8 (18.09) | 66.4 (11.16) | 0.8 |
| Age at death | 63.9 (15.86) | 68.7 (9.95) | 0.15 | 59.4 (18.15) | 68.2 (13.17) | 0.13 | 67.4 (18.07) | 68.6 (10.97) | 0.85 |
| Change in albumin over previous 3 months | 0.2 (0.39) | 0.2 (0.53) | 0.58 | 0.2 (0.42) | 0.3 (0.53) | 0.33 | 0.4 (0.39) | 0.3 (0.59) | 0.67 |
| Charlson Comorbidity Index | 9.5 (2.99) | 10 (2.8) | 0.49 | 8.6 (3.55) | 9.9 (2.89) | 0.22 | 9.2 (2.53) | 10.3 (3.03) | 0.31 |
| Mortality predictor (XBETA) | −121.2 (117.14) | −38.9 (80.19) | 0.002 | −204.3 (91.81) | −28.2 (84.89) | 0.001 | −58.4 (107.16) | −15.7 (72.72) | 0.27 |
| Probability of survival at 6 months | 77.9 (17.37) | 64.8 (20.09) | 0.01 | 90.2 (9.93) | 61.9 (19.04) | 0.001 | 68.0 (15.48) | 59.4 (200.09) | 0.19 |
| Probability of survival at 12 months | 57.9 (28.55) | 39.1 (24.12) | 0.01 | 78.7 (18.63) | 34.8 (22.68) | 0 | 40.9 (23.82) | 32.2 (22.20) | 0.34 |
CFTT, chronic failure to thrive as reflected by loss of function due to amputation, diagnosis of a nonrenal terminal illness, increasing frequency of hospitalizations, admission to nursing home for long-term care, loss of personal drive to continue dialysis, severe depression refractory to treatment, loss of mental or emotional capacity to understand changes in medical status or requirements of dialysis, or acceleration of one or more comorbid conditions refractory to treatment.
FIG. 1.
Use of hospice and location of death.
Compared to those who were not approached, patients who requested or were approached about considering withdrawal for CFTT had higher mortality predictor scores (−204.3±91.81 versus −28.2±87.89; p<0.001) and lower predicted estimates for survival at 6 months (90.2±9.93 versus 61.9±19.04; p<0.001; Table 1).5,6 Among those who withdrew for reasons related to CFTT (24 or 73%), all (including those who requested discussion of withdrawal of their own volition) were judged to have more than 1, and on average, 4 factors prompting consideration of withdrawal (Table 2). Discussions were postponed because of the need to treat a medical or psychosocial condition in a majority of patients and in some, more than once. Twelve of those approached engaged in only 1 discussion; 4 of these patients withdrew; multiple conversations took place with 22 of the patients and/or their families. Except for the use of hospice, which was greater in those who withdrew (Fig. 1), no clinical or demographic differences were found among patients who were approached or approached us about withdrawal for CFFT, irrespective of whether or not they withdrew.
Table 2.
Criteria for Chronic Failure to Thrive and Triggers Prompting Contemplation of Withdrawal
| Criteria or trigger: | Number | Percent of CFTT group |
|---|---|---|
| Physician answer of “No, I would not be surprised” to the surprise question | 24 | 71% |
| Accelerating comorbid illnesses | 22 | 65% |
| Poor prognosis based on patient-specific estimate of prognosis | 18 | 53% |
| Increased frequency of hospitalizations | 16 | 47% |
| Loss of personal drive to continue or severe, unrelenting depression | 14 | 41% |
| Failure to thrive | 14 | 41% |
| Diagnosis of non-renal terminal illnesses | 11 | 32% |
| Loss of function including admission to a nursing home (4) | 11 | 32% |
Chronic failure to thrive (CFTT) defined as loss of function due to amputation, diagnosis of a nonrenal terminal illness, and other parameters suggestive of CFTT, including increasing frequency of hospitalizations, admission to nursing home for long-term care, loss of personal drive to continue dialysis, severe depression refractory to treatment, loss of mental or emotional capacity to understand changes in medical status or requirements of dialysis, or acceleration of one or more comorbid conditions refractory to treatment.
Patients who were approached or whose family approached us because of events reflecting CFTT more often were considered cognitively impaired, lacked decision making capacity, carried the diagnosis of dementia or were otherwise mentally compromised and unable to grasp the requirements of dialysis (50 versus 7.7%; p=0.01) than those who were not approached or did not request withdrawal. Among those with CFTT, more of the withdrawal group were considered cognitively impaired compared to the nonwithdrawal group, although the difference did not reach statistical significance (63 versus 20%; p=0.06; Table 3). The decision to withdraw was made jointly by patient and family in 11 cases (46%) and by the family alone in 9 (36%; Table 3). All but 2 of the 9 patients in the latter group were considered cognitively impaired; these 2 patients expressed interest in withdrawing but would not acquiesce to family wishes that they continue dialysis. Nine patients made the decision without or in opposition to family wishes (4 withdrew and 5 did not).
Table 3.
Decision Making Among Patients with Chronic Failure to Thrive and Cognitive Impairment
| Number | Cognitive impairment | Multiple conversations | Family involved or made the decision | |
|---|---|---|---|---|
| Patients approached about or requesting withdrawal because of chronic failure to thrive | 34 | 17a (50%) | 22 (65%) | 25 (74%) |
| Withdrew | 24 | 15 (63%) | 19 (79%) | 20 (83%) |
| Did not withdraw | 10 | 2 (20%) | 3 (30%) | 5 (50%) |
Decision made by both the patient and family in 4 cases and solely by the family in 11 cases; two patients with decision making capacity despite mild cognitive impairment refused further treatment.
Discussion
Withdrawal from dialysis occurred prior to death in half of all patients dying during a 5-year period, with the majority of patients withdrawing because of accelerating comorbid illnesses or conditions reflective of CFTT. No patient withdrawing for reasons of CFTT died in hospital and nearly all who withdrew utilized hospice. Hospice use was significantly greater in patients who withdrew and in those who were approached but did not withdraw compared to those who did not withdraw or were not approached. Death occurred at home for all but six patients who died in nursing homes or a hospice house. The stigma of hospice as an imminent harbinger of death remains prevalent in this rural population, thus the high use of hospice reflects a strong advocacy for its benefits. Communication between inpatient and outpatient nephrology teams is purposeful to assure that POST form wishes are clearly addressed with each hospitalization.
Limitations of this study include that it is a single center review. Second, a reluctance of many rural patients to travel the necessary distance for tertiary care clearly contributes to the low prevalence of in hospital death and all patients who died in hospital did so after an acute event prompted hospitalization. The distance factor notwithstanding, advance care planning is begun early in our unit and while we refer many patients to hospice, we do not rely on hospice enrollment to initiate a palliative approach. Patients and families who are adverse to withdrawal, hospice, or both may fear a hospital death and still wish to die peacefully at home and efforts to accommodate this wish are made priority. A third limitation is the retrospective use of a mortality predictor tool that includes the surprise question and thus could potentially introduce bias. Real-time assignment of a negative answer to the surprise question was the impetus for withdrawal conversations and patients were approached specifically because neither the nurse practitioner nor the physician would have been surprised if the patient had died in the subsequent 6 months. Thus, while it is true that the predictor estimates were calculated after the outcomes were known, the data used to make the calculation (including a negative answer previously ascribed to the surprise question) was that which was known at the time a withdrawal discussion was contemplated. A positive correlation of the Charlson Comorbidity Index between and across all groups and subgroups supports the mortality predictor results and perhaps mitigates the limitation posed by the retrospective use of this tool.
Advance care planning and withdrawal from dialysis was associated with a high use of hospice. Along with the low incidence of in-hospital death, this contrasts with national reports that among patients withdrawing from dialysis, hospice is underutilized3 and nearly half of all patients die in hospital.1 Comorbid illnesses and clinical deterioration may be subtle and not immediately life-threatening but both emotionally and physically debilitating for patients and their families.8 Our outcomes complement other reports of the power of a systematic and comprehensive approach to advance care planning prior to the end of life for dialysis patients with CFTT.9 Advance care planning, completion of POST, and guided withdrawal processes allow deliberate determinations about the end of life, are associated with greater hospice utilization, and may facilitate the chance for an out-of-hospital death.
Acknowledgments
We thank Alvin Moss, MD, for his editorial insight as well as Jeanine Zurbuch, RN, and Linda Coleman for their technical assistance.
Author Disclosure Statement
Dr. Schmidt is a Joint Venture Partner in a dialysis company. Ms. Weaner has no disclosures.
Dr. Long is partially supported by the National Institute of General Medical Sciences of the National Institutes of Health under Award Number U54GM104942. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
References
- 1.Wong SPY, Kreuter W, O'Hare AM: Treatment intensity at the end of life in older adults receiving long-term dialysis. Arch Intern Med 2012;172:661–662 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.United States Renal Data System: USRDS 2008 Annual Data Report: Atlas of Chronic Kidney Disease and End-Stage Renal Disease in the United States. Bethesda, MD, National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases, 2011 [Google Scholar]
- 3.Murray AM, Arko C, Chen S-C, Gilbertson DT, Moss AH: Use of hospice in the United States dialysis population. Clin J Am Soc Nephrol 2006;1:1248–1255 [DOI] [PubMed] [Google Scholar]
- 4.Citko J, Moss AH, Carley M, Tolle SW: The National POLST Paradigm Initiative, 2nd ed. Fast Facts and Concepts. September2010;178. www.eperc.mcw.edu/fastfact/ff_178.htm (Last accessed June24, 2014)
- 5.Moss AH, Ganjoo J, Sharma S, Gansor J, Senft S, Weaner B, Dalton C, MacKay K, Pellegrino B, Anantharaman P, Schmidt R: Utility of the “surprise” question to identify dialysis patients with high mortality. Clin J Am Soc Nephrol 2008;3:1379–1384 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cohen LM, Ruthazer R, Moss AH, Germain MJ: Predicting six-month mortality in patients maintained with hemodialysis. Clin J Am Soc Nephrol 2010;5:72–79 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fadem S, Fadem J: Hemodialysis mortality predictor. http://touchcalc.com/calculators/sq (Last accessed May15, 2013)
- 8.Schmidt R, Moss A: Dying on dialysis: The case for a dignified withdrawal. Clin J Am Soc Nephrol 2014;9:174–180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hammes BJ, Rooney BL, Gundrum JD, Hickman SE, Hager N: The POLST program: A retrospective review of the demographics of use and outcomes in one community where advance directives are prevalent. J Palliat Med 2012;15:77–85 [DOI] [PubMed] [Google Scholar]