Appropriate and timely treatment of pain are very important, particularly in the emergency department, where pain continues to be undertreated. One of the ways in which the undertreatment of pain can be mitigated is the use of defined quality benchmarks. This systematic review of the literature was performed to identify such quality indicators. The resulting 20 quality indicators may be used to improve pain assessment and management protocols in the emergency department setting.
Keywords: Emergency department, Pain assessment and management, Quality indicators, Systematic review
Abstract
BACKGROUND:
Evidence indicates that pain is undertreated in the emergency department (ED). The first step in improving the pain experience for ED patients is to accurately and systematically assess the actual care being provided. Identifying gaps in the assessment and treatment of pain and improving patient outcomes requires relevant, evidence-based performance measures.
OBJECTIVE:
To systematically review the literature and identify quality indicators specific to the assessment and management of pain in the ED.
METHODS:
Four major bibliographical databases were searched from January 1980 to December 2010, and relevant journals and conference proceedings were manually searched. Original research that described the development or collection of data on one or more quality indicators relevant to the assessment or management of pain in the ED was included.
RESULTS:
The search identified 18,078 citations. Twenty-three articles were included: 15 observational (cohort) studies; three before-after studies; three audits; one quality indicator development study; and one survey. Methodological quality was moderate, with weaknesses in the reporting of study design and methodology. Twenty unique indicators were identified, with the majority (16 of 20) measuring care processes. Overall, 91% (21 of 23) of the studies reported indicators for the assessment or management of presenting pain, as opposed to procedural pain. Three of the studies included children; however, none of the indicators were developed specifically for a pediatric population.
CONCLUSION:
Gaps in the existing literature include a lack of measures reflecting procedural pain, patient outcomes and the pediatric population. Future efforts should focus on developing indicators specific to these key areas.
Abstract
HISTORIQUE :
D’après les données probantes, la douleur n’est pas assez traitée en salle d’urgence (SU). La première étape pour atténuer l’expérience de la douleur chez les patients en SU consiste à évaluer les soins administrés de façon précise et systématique. Pour déterminer les lacunes dans l’évaluation et le traitement de la douleur et améliorer le résultat des patients, il faut des mesures de rendement pertinentes et fondées sur des faits probants.
OBJECTIF :
Faire l’analyse systématique des publications et déterminer les indicateurs de qualité propres à l’évaluation et à la prise en charge de la douleur en SU.
MÉTHODOLOGIE :
Les chercheurs ont interrogé quatre grandes bases de données bibliographiques entre janvier 1980 et décembre 2010 et fouillé manuellement les revues et délibérations de congrès ou colloques pertinents. Ils ont inclus les recherches originales qui décrivaient la mise sur pied ou la collecte de données sur au moins un indicateur de qualité propre à l’évaluation ou à la prise en charge de la douleur en SU.
RÉSULTATS :
La recherche a permis d’extraire 18 078 citations. Vingttrois articles ont été retenus : 15 études d’observation (cohortes), trois études avant-après, trois vérifications, une étude d’élaboration d’indicateurs de qualité et une enquête. La méthodologie était de qualité modérée, comportant des faiblesses dans la déclaration de la conception et de la méthodologie. Vingt indicateurs uniques ont été relevés, la majorité (16 sur 20) mesurant les processus de soins. Dans l’ensemble, 91 % des études (21 sur 23) rendaient compte d’indicateurs pour l’évaluation ou la prise en charge de la douleur à la présentation, en opposition à la douleur causée par une intervention. Trois études incluaient les enfants. Cependant, aucun indicateur n’a été élaboré expressément pour la population pédiatrique.
CONCLUSION :
Le peu de mesures reflétant la douleur liée à l’intervention, les résultats des patients et la population pédiatrique font partie des lacunes des publications actuelles. Les futurs efforts devraient porter sur l’élaboration d’indicateurs axés sur ces secteurs clés.
Pain is the most common reason for seeking health care in the Western world (1–3). Multiple national and international bodies, including the WHO, have focused on the importance of pain management (4–6). Research has shown that inadequate pain treatment can have detrimental effects; it can result in extended length of hospitalization, slower healing, altered pain processing, depression, anxiety, and substantial social and economic costs to society (5,7,8). Although pain is a common reason for visiting the emergency department (ED), evidence consistently indicates that pain is undertreated in the ED (9–15).
Policy makers, researchers and health care providers use quality indicators, or performance measures, to measure and improve the quality of care provided to patients. Previous research and experience has shown that quality indicators and performance measurement improve health care outcomes (16,17). The first step in improving the treatment of pain for ED patients is to accurately and systematically assess the actual care being provided. Identifying gaps in the assessment and treatment of pain and improving patient outcomes requires relevant, evidence-based performance measures. Quality indicators have previously been developed and applied to a number of clinical conditions and health care settings, including the ED management of asthma, acute myocardial infarction and pneumonia (18–22). The objective of the present study was to systematically review the literature and identify quality indicators for the assessment and management of pain in the ED setting. To create health care system improvements in the ED that meet the needs of patients with presenting (eg, illness or injury-related) and procedural (eg, medical test or other procedure-related) pain, an accurate summary of existing performance measures is required.
METHODS
Literature search and selection
The search strategy was developed by a medical research librarian (AM), in consultation with the research team and preidentified content experts. A commonly accepted definition of quality indicators that has been employed in previous research was used: “explicitly defined and measurable items referring to the structures (staff, equipment, and facilities), processes (prescribing, investigations, interactions between professionals and patients) or outcomes (such as mortality, morbidity or patient satisfaction) of care” (23–25). A systematic literature search of journals published between January 1980 and December 2010 was conducted using the following bibliographic databases: Medline, Cochrane Library, EMBASE and CINAHL. Search terms included those corresponding to quality indicators and quality improvement combined with terms describing the assessment and treatment of pain in the ED (Appendix 1). Due to resource constraints, only English-language publications were considered.
All titles and abstracts generated by the search were independently screened by two of three authors (AS, SA and CF) and any articles team members believed were likely to provide potential indicators were included for full-text review. Using predefined eligibility criteria, the full text of screened articles were independently assessed for inclusion by two authors (AS, CF). Original research that described the development or collection of data for one or more quality indicators relevant to the assessment or management of pain in the ED setting was included. Studies that were conducted outside of the ED, including the prehospital setting, inpatient setting or operating room were excluded, as were studies conducted in the ED that described the epidemiology, assessment or management of pain but did not measure the quality of care using quality indicators or a related term such as performance measure, audit filter, indicator, care indicator, benchmark, clinical path expected outcome or quality measure. To identify additional studies, reference lists of included articles and review papers were screened, and relevant journals and proceedings of key scientific meetings were hand searched (Appendix 2). Consensus was required for final exclusion of screened articles and disagreements were resolved through involvement of a third author (SA). Before implementation, ethics approval for this study was obtained from the University of Calgary’s Conjoint Health Research Ethics Board (Calgary, Alberta).
Data extraction
Data were abstracted from each study by one of two authors (AS, CF) using a standardized, piloted form, with accuracy of extraction verified by the second author (AS, CF). Abstracted data included: study methodology (design, setting, population), indicator definition and indicator measurement properties (reliability, validity, data source) and the degree to which the quality indicator was judged to be operational (described explicitly and in sufficient detail to be potentially implemented by a reader) (26).
Assessment of methodological quality
Methodological quality was rated using the Newcastle-Ottawa Quality Assessment Scale (NOS) (27) for observational studies and a modified version of the NOS for before-after studies (28). To the authors’ knowledge, there is no validated tool to measure the methodological quality of indicator development studies. The indicator development process used in included studies was compared with the steps recommended by the Agency for Healthcare Research and Quality for quality indicator measure development, implementation, maintenance and retirement (29) (Appendix 3).
Analysis
The results of the present review are primarily described in a qualitative manner, with the use of counts and proportions where relevant. The primary outcome was the count of existing quality indicators for the assessment and treatment of pain in the ED, including the type of indicator (structure [such as staff, equipment, and facilities], process [prescribing, investigations, interactions between professionals and patients] or outcome [such as mortality, morbidity or patient satisfaction]) (25) and the aspect of pain measured (assessment or management). Secondary outcomes included the indicator data source, the proportion of indicators that are operational, the results of indicator measurement, and the type of pain, either presenting (eg, musculoskeletal injury, abdominal pain, sickle cell crisis) or procedural (eg, fracture reduction, intravenous insertion, lumbar puncture).
RESULTS
Study selection
The search identified 18,078 citations (Figure 1). Review of titles and abstracts resulted in the retrieval of 168 full-text articles. No additional articles were identified through the manual search of references, journals or conference proceedings. Twenty-three articles met the inclusion and exclusion criteria for the present review (Appendix 4).
Figure 1).
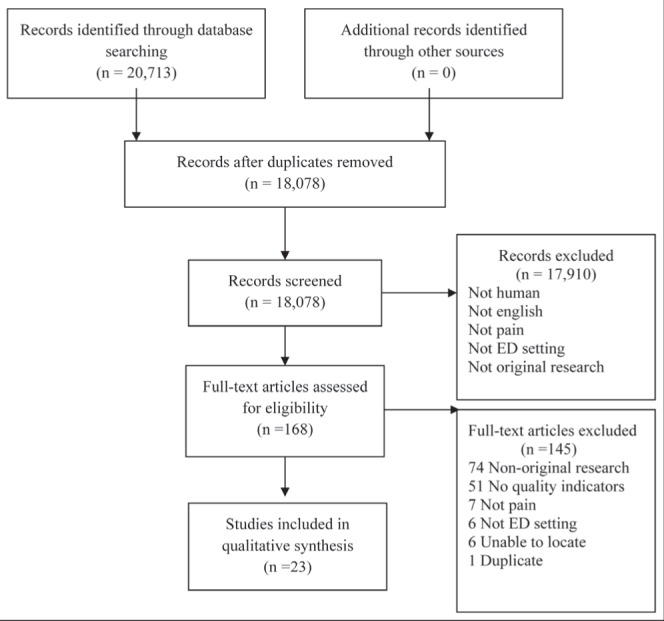
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) diagram. ED Emergency department
Study characteristics
The studies included in the review are described in Table 1; 15 of the studies were observational (cohort) studies, three were before-after studies, three were audits, one was a quality indicator development study and one was a survey. The number of patients enrolled in each of the studies ranged from 18 (30) to 156,729 (31), with a median of 302 patients. The majority of participants were adults. One study was performed in a pediatric ED (32), while three studies focused on pain in the elderly (33–35). The majority (n=10) of studies were performed in EDs in the United States, four in Australia, five in the United Kingdom, one in France and one in Canada; one study focused on indicator development, and was not health care facility-based.
TABLE 1.
Summary of included studies
| Study | Study design | Setting (annual visits) | n | Age, years | Objective | |||
|---|---|---|---|---|---|---|---|---|
| Arendts and Fry (69), 2006 | Retrospective cohort | ED, trauma centre, Australia (46,000) | 857 | Median 47 (range 0–101) | To determine: the proportion of patients that require parenteral opiate analgesia for pain in an ED and who receive the opiate in <60 min; and whether any factors are predictive for the first dose of analgesia being delayed beyond 60 min | |||
| Chu and Brown (44), 2009 | Analytic observational | ED, tertiary referral hospital, Australia (70,000) | 72 | Median 47 (IQR 35–56) | To provide exploratory data seeking an association between access block and time to parenteral opioid analgesia in patients presenting to the ED with renal colic | |||
| Eder et al (41), 2003 | Retrospective | ED, United States (NR) | 261 | Mean ± SE 40±15, median 40 | To evaluate ED documentation of patient pain in light of the Joint Commission of Accreditation of Healthcare Organization’s emphasis on pain assessment and management | |||
| Forero et al (45), 2008 | Retrospective cohort | ED, referral hospital, Australia (>40,000) | 13,449 | 23% 0–14, 41% 15–44, 26% 45–75, 9% ≥76 | To explore the association of morphine use with factors influencing time to initial analgesia | |||
| Goodacre and Roden (39), 1996 | Audit | ED, United Kingdom (NR) | 200 | NR | To evaluate a protocol for intervention used to improve on shortcomings in the use of analgesia in an accident and ED | |||
| Grant et al (42), 2006 | Retrospective analysis of patient records | ED, United Kingdom (NR) | 473 | NR (<18 excluded) | To evaluate the effectiveness of analgesia delivery, in the ED setting, to patients presenting with acute pain, with regard to guidelines from the British Association of Accident and Emergency Medicine | |||
| Guru and Dubinski (49), 2000 | Prospective cohort | ED, Canada (NR) | 71 | Mean ± SE 35.5±15.7 | To assess how well pain was evaluated and treated in accordance with recommended guidelines in the Canadian Association of Emergency Physicians consensus document | |||
| Hawkes et al (32), 2008 | Before-after | ED, third level trauma, Ireland (50,000, 10,000 pediatric) | 240 | Before, median 8 (IQR 4–12); after, 10 (IQR 4–13) | To describe the provision of analgesia for pediatric patients in a large Irish ED and to analyse and modify the protocol in this hospital with a view to improving the quality of care provided for children | |||
| Hwang et al (43), 2008 | Retrospective observational | ED, urban, academic tertiary care ED, United States (NR) | 1068 | Mean ± SD 47±19 | To evaluate the association of three ED crowding factors with the quality of general ED pain care | |||
| Hwang et al (33), 2006 | Retrospective cohort | ED, tertiary care teaching facility, United States (70,000) | 158 | Mean 83 (range 52–101) | To evaluate the effect of ED crowding on the assessment and treatment of pain in older adults | |||
| Jackson (34), 2010 | Before-after (educational intervention) | ED, United States (NR) | 302 | Mean 83 (range 65–99) | To explore the results of a staff educational intervention with evaluation of medical record documentation before and after implementation | |||
| Kuan et al (50), 2009) | Before-after (educational intervention) | ED, tertiary referral centre, Ireland (40,000) | 151 | Audit 1; median 38 (range 15–90) audit 2, 37 (16–83) audit 3, 38 (15–82) | To evaluate the impact of a brief educational intervention on prompt recognition and treatment of pain in the ED | |||
| Mitchell et al (46), 2009 | Observational retrospective | ED, metropolitan teaching hospital, Australia (32,000) | 436 | Median 57 | To determine whether overcrowding negatively impacts on the timeliness of pain management, an indicator of ED quality of care | |||
| Odesina et al (30), 2010 | Retrospective medical record review | ED, suburban university health care centre, United States (29,200) | 18 | Mean ± SE 29.9±5.61 | To examine the current sickle cell disease pain management practice patterns, explore evidence-based sickle cell disease pain management clinical guidelines, and develop and implement an adapted ED sickle cell pain management clinical pathway | |||
| Pines et al (54), 2008 | Retrospective | ED, urban tertiary care, United States (55,000) | 13,758 | Mean ± SD 39±16 | To study the impact of ED crowding on both treatment and delays in treatment in a broad cohort of ED patients who presented at triage with a complaint of severe pain | |||
| Pines and Hollander (48), 2010 | Retrospective cohort | ED, United States, multicentre, academic tertiary care (57,000), community hospital (35,000) | 5616 | Mean ± SD 44±17 | To study the association between ED crowding and the use of, and delays in, analgesia in patients with back pain in two EDs | |||
| Pletcher et al (31), 2008 | Analysis of national database | ED, United States, multicentre (NR) | 156,729 | Reported by race: white, mean ± SE 39.0±22; black, 34.3±19; Hispanic, 31.9±20; Asian/other, 36.7±21 |
To determine whether opioid prescribing in EDs has increased, whether non-Hispanic white patients are more likely to receive an opioid than other racial/ethnic groups, and whether differential prescribing according to race/ethnicity has diminished since 2000 | |||
| Ritsema et al (40), 2007 | Retrospective cohort | ED, multicentre, United States (NR) | 2064 | 1998–2000, mean ± SE 33±1.2, 2001–2003, 35±1.2 | To compare the quality of ED pain management before and afterimplementation of the Joint Commission on the Accreditation of Healthcare organizations standards in 2001 | |||
| Ricard-Hibon et al (36), 2004 | Survey | ED and prehospital EMS, France, multicentre (23% <15,000; 44% 15,000–30,000; 33% >30,000) | 363 responses | NR | To evaluate the existence of a quality control program for acute pain management in the ED and in the prehospital EMS, and the needs in training and support to implement these procedures. | |||
| Shah and Lendrum (37), 2004 | Audit | ED, United Kingdom (NR) | 25 | NR | To compare the practice in the Chesterfield Royal hospital ED with the standards set by The British Association of Accident and Emergency Medicine, and critically evaluate the results. | |||
| Tanabe et al (47), 2007 | Retrospective cohort | ED, United States, academic medical centres, multicentre (NR) | 159 | Mean ± SE 32±10 | To characterize the initial management of patients with sickle cell disease and an acute pain episode, to compare these practices with the American Pain Society Guideline for the Management of Acute and Chronic Pain in Sickle-Cell Disease in the ED, and to identify factors associated with a delay in receiving an initial analgesic. | |||
| Terrell et al (35), 2009 | Task force (quality N/A indicator development) | N/A | ≥65 | To develop ED-specific quality indicators for older patients | ||||
| Vega-Stromberg et al (38), 2002 | Audit | Acute care, United States, multicentre (NR) | NR | NR | To describe an interdisciplinary model for process improvement within an integrated health care system. | |||
ED Emergency department; EMS Emergency medical services; IQR Interquartile range; NR Not recorded; SE Standard error; N/A Not applicable
Overall, there were weaknesses in the reporting of study design and methodology, which made assessment of methodological quality challenging for the present review. Methodological quality was moderate (Appendix 3). The NOS was applied to studies described by the study authors or classified by data extractors as observational studies. Application of the NOS identified weaknesses in comparability of study groups and outcome ascertainment, particularly in the description of subjects lost to follow-up. For the studies identified by authors or data extractors as before-after studies, there were weaknesses identified in the selection of the pre- and postintervention sample as well as in outcome reporting and pre- and postintervention comparability with respect to the timeframe of data collection. The quality indicator development study demonstrated weaknesses in the assessment of candidate indicators. A quality assessment could not be completed for four studies due to study design, namely survey (36) and audit (37–39) methodology.
Primary outcome
Table 2 provides a summary of the quality indicators, the number of studies reporting each indicator and the results of data collected on the indicators. The most commonly measured indicators reflected the documentation and timeliness of pain assessment and reassessment, and the receipt and timeliness of analgesia. Table 3 provides details on the quality indicators extracted from each of the individual studies, including the type of indicator, data source, results of indicator measurement, extent to which indicator as reported is operational and type of pain. There were a total of 20 indicators measured, with considerable overlap in the indicators reported across studies. Eighty percent (16 of 20) of the indicators measured care processes, 15% (three of 20) measured structure and 5% (one of 20) measured patient outcome. For the purposes of categorizing indicator type, indicators measuring pain assessment were considered process indicators. Sixty percent (12 of 20) of the indicators reflected pain management and 40% (eight of 20) reflected pain assessment.
TABLE 2.
Summary of quality indicators and results of measurement
| Quality indicators | Type of indicator | Studies reporting indicator, n | Results of indicator measurement, including range of results when similar indicators were measured in multiple studies |
|---|---|---|---|
| Pain assessment | |||
| Patients with any documented pain assessment | Process | 5 | 57% to 94% |
| Patients with documented pain assessment using validated pain score | Process | 1 | 23% |
| Patients with physician-documented pain assessment | Process | 1 | 85% to 86% |
| Timeliness of pain assessment | Process | 2 | Mean 40 min to 174 min (from arrival/triage) |
| Patients with documented pain reassessment after treatment | Process | 4 | 32% to 50% |
| Timely reassessment of pain relief after treatment | Process | 4 | 0% to 55.3% of patients, mean 113 min |
| Pain assessment documented before discharge from ED | Process | 2 | 56% (of sites) |
| Patients with pain rated 0/10 at discharge | Process | 1 | 8% |
| Pain management | |||
| Patients administered any analgesia | Process | 9 | 6% to 79% |
| Patients with analgesia offered at triage | Process | 3 | 18% to 83% |
| Timely access to any analgesia | Process | 12 | Mean or median >60 min in 6 of 9 studies, % of patients with delay ≥1 h 14% to 81% (from arrival/triage) |
| Timely access to parenteral opioid analgesia | Process | 2 | Median 0.8 h to mean 67.5 min from arrival/triage |
| Elderly patients treated with meperidine | Process | 2 | 32.8% |
| Patients receiving appropriate analgesic dose | Process | 1 | 92% |
| Patients receiving analgesic by appropriate route | Process | 1 | 55% |
| Provision of bowel regimen with opioid analgesia prescription | Process | 1 | NR |
| Sites with training specifically for pain management for physicians | Structure | 1 | 56% of sites |
| Sites with training specifically for pain management for nurses | Structure | 1 | 68% of sites |
| Sites with pain therapeutics protocols | Structure | 1 | 69% of sites |
| Patients satisfied with pain management | Outcome | 1 | 34% to 39% |
ED Emergency department; NR Not reported
TABLE 3.
Detailed summary of results of data collection on quality indicators
| Study | Quality indicator | Type* | Data source | n† | Result | Operational‡ | Type of pain§ |
|---|---|---|---|---|---|---|---|
| Arendts and Fry (69), 2006 | Delay to analgesia (% of patients with time from arrival to analgesia ≥60 min) | Process | Administrative database | 857 | 47% | Yes | Presenting, all types |
| Chu and Brown (44), 2009 | Time to parenteral opioid analgesia (time of arrival to parenteral opioid) | Process | Chart review | 69 | Median 0.80 h (IQR 0.37 h to 1.37 h) | Yes | Presenting, renal colic |
| Time to parenteral opioid analgesia (% ≤1 h) | Process | Chart review | 69 | 60.9% | Yes | Presenting, renal colic | |
| Eder et al (41), 2003 | % patients with initial pain assessments | Process | Chart review | 261 | 94% | Yes | Presenting, all types |
| % of patients with initial pain assessments measured using pain scale | Process | Chart review | 261 | 23% | Yes | Presenting, all types | |
| % of patients with documented pain assessment subsequent to therapy | Process | Chart review | 261 | 39% | Yes | Presenting, all types | |
| % of patients with documented pain assessment subsequent to therapy measured using pain scale | Process | Chart review | 261 | 19% | Yes | Presenting, all types | |
| Forero et al (45), 2008 | Time to analgesia (time from triage to administration of morphine) | Process | Chart review | 1097 | Median 79 min, 95% CI 71–85 | Yes | Presenting, all types |
| Goodacre and Roden (39), 1996 | Percent of fracture clinic referrals with no analgesia offered in ED | Process | Chart review | 200 | Initial audit 91% repeat audit 69% | No | Presenting, MSK, fracture |
| % of orthopedic admissions with no analge-sia offered in ED | Process | Chart review | 200 | Initial audit 39% repeat audit 22% | No | Presenting, MSK, fracture | |
| Grant et al (42), 2006 | % of patients in severe pain (score 7 to 10/10) who receive appropriate analgesia within 20 min of arrival or triage (whichever is earlier) | Process | Administrative database | 213 | 24% | Yes | Presenting, all types |
| % of patients in moderate pain (score 4 to 6/10) offered analgesia at triage | Process | Administrative database | 105 | 18% | Yes | Presenting, all types | |
| % of patients who have documented re-evaluation of analgesia requirements | Process | Administrative database | NR | 32% | Yes | Presenting, all types | |
| Guru and Dubinsky (49), 2000 | % patients offered analgesia for mild pain (score 0 to 3/10) | Process | Survey | 71 | 6% | Yes | Presenting, all types |
| % analgesia offered for moderate pain (score 4 to 6/10) | Process | Survey | 71 | 18% | Yes | Presenting, all types | |
| % analgesia offered for severe pain (score 7 to 10/10) | Process | Survey | 71 | 68% | Yes | Presenting, all types | |
| % rating no pain (score 0/10) on discharge | Process | Survey | 71 | 8% | Yes | Presenting, all types | |
| Hawkes et al (32), 2008 | Time from triage to analgesia major fracture (long bone, rib, clavicle) | Process | Chart review | 36 | Pre median 54 min (IQR 25 to 90); Post median 7 min (IQR 4 to 12); P=0.0004 | Yes | Presenting, major fracture |
| % receiving analgesia major fracture (long bone, rib, clavicle) | Process | Chart review | 36 | Pre 55.6%; post 61.1% P=0.735 | Yes | Presenting, major fracture | |
| Time from triage to analgesia other diagnoses | Process | Chart review | 183 | Pre median 14 min (IQR 4 to 45); Post median 6 min (IQR 6 to 61) P=0.794 | Yes | Presenting, all types | |
| % receiving analgesia other diagnoses | Process | Chart review | 183 | Pre 34.7%; post 39.8% | Yes | Presenting, all types | |
| Hwang et al (33), 2006 | % of patients with documentation of pain assessment | Process | Chart review | 158 | 72.8% | Yes | Presenting, hip fracture |
| Time to pain assessment by a physician (from triage) | Process | Chart review | 128 | Mean 40 min (range 0 min to 600 min) | Yes | Presenting, hip fracture | |
| % of patients with documentation of administration of pain medication | Process | Chart review | 128 | 64.1% | Yes | Presenting, hip fracture | |
| Time to pain treatment (from triage) | Process | Chart review | 128 | Mean 141 min range (10 min to 525 min) | Yes | Presenting, hip fracture | |
| % of patients receiving opioid who were treated with meperidine | Process | Chart review | 73 | 32.8% | Yes | Presenting, hip fracture | |
| Hwang et al (43), 2008 | % of patients with physician documented pain assessment | Process | Chart review | 1068 | Census low: 86%, Census high: 85% | Yes | Presenting, all types |
| % of patients with any documented pain assessment | Process | Chart review | 1068 | Census low: 90% Census high: 90% | Yes | Presenting, all types | |
| % of patients with follow-up pain assessment | Process | Chart review | 961 | Census low: 50%, Census high: 47% | Yes | Presenting, all types | |
| % of patients who received analgesic medication | Process | Chart review | 642 | Census low: 65%, Census high:55% | Yes | Presenting, all types | |
| Time to first clinician pain assessment | Process | Chart review | 899 | Census low: mean 106 min, Census high: mean 174 min | Yes | Presenting, all types | |
| Time to first analgesic medication ordering | Process | Chart review | 604 | Census low: mean 104 min, Census high: mean 136 min | Yes | Presenting, all types | |
| Time to first analgesic medication administration | Process | Chart review | 590 | Census low: mean 125 min, Census high: mean167 min | Yes | Presenting, all types | |
| Jackson (34), 2010 | Time to first pain treatment after assessment (% <60 min) | Process | Chart review | 220 | Pre 41.8%; post 50% | Yes | Presenting, hip fracture |
| Time to reassessment documentation after treatment (% <60 min) | Process | Chart review | 149 | Pre 30.9%; post 55.3% | Yes | Presenting, hip fracture | |
| Kuan et al (50), 2009) | % of patients with analgesia offered at triage | Process | Chart review | 151 | 43% | Yes | Presenting, all types |
| % of patients with analgesia offered at triage for severe pain (≤20 min of arrival or at triage for severe pain [score 7 to 10/10]) | Process | Chart review | 24 | 83% | Yes | Presenting, all types | |
| % of patients with timely reassessment of pain relief (within ≤30 min for 90% of patients with severe pain [score 7 to 10/10]) | Process | Chart review | 19 | 0% | Yes | Presenting, all types | |
| % of patients with timely treatment of pain (≤60 min of arrival for >75% of patients with moderate pain [score 4 to 6/10]) | Process | Chart review | 64 | 14% | Yes | Presenting, all types | |
| Mitchell et al (46),2009 | Time to analgesia (from ED arrival) | Process | Chart review | 232 | Median 53 mins (IQR 30.5 to 114.5) | Yes | Presenting, fracture, renal/biliary colic |
| Odesina et al (30), 2010 | Time from registration to receiving first opioid | Process | Chart review | 44 | Mean ± SD 67.5±48.1 min | Yes | Presenting, sickle cell disease |
| Time to reassessment for pain relief after first opioid administration | Process | Chart review | 44 | Mean ± SD 113±118.4 min | Yes | Presenting, all types | |
| Pines and Hollander (54), 2008 | % of patients with severe pain (score 9 to 10/10) with no analgesia in the ED | Process | Administrative database | 13,758 | 51% | Yes | Presenting, all types |
| % of patients with severe pain (score 9 to 10/10) with delay >1 h in time to analgesia from triage | Process | Administrative database | 6746 | 59% | Yes | Presenting, all types | |
| % of patients with severe pain (score 9 to 10/10) with delay >1 h in time to analgesia from placement in room | Process | Administrative database | 1319 | 20% | Yes | Presenting, all types | |
| Pines et al (48), 2010 | % of patients with administration of any analgesia | Process | Administrative database | 5616 | 79% | Yes | Presenting, back pain |
| Time from triage to first analgesia | Process | Administrative database | 4425 | Median 130 min (IQR 73 to 217) | Yes | Presenting, back pain | |
| % of patients with delay of ≥1 h from triage to analgesia | Process | Administrative database | 4425 | 81% | Yes | Presenting, back pain | |
| Time from room placement to analgesia | Process | Administrative database | 4425 | Median 86 min (IQR 51 to 135) | Yes | Presenting, back pain | |
| % of patients with delay of ≥1 h from room placement to analgesia | Process | Administrative database | 4425 | 67% | Yes | Presenting, back pain | |
| Pletcher et al (31), 2008 | % of patients receiving opioid analgesic prescription for pain-related visits | Process | Administrative database | 156,729 | 29% (95% CI 28% to 30%) | Yes | Presenting, all types |
| Ricard-Hibon et al (36), 2004 | % of sites with training specifically for pain management for physicians | Process | Survey | 356 | 56% | No | Presenting, all types |
| % of sites with training specifically for pain management for nurses | Process | Survey | 356 | 68% | No | Presenting, all types | |
| % of sites with pain therapeutics protocols | Process | Survey | 356 | 69% | No | Presenting, all types | |
| % of sites where pain intensity was evaluated ‘systematically or often’ at the beginning of patient management | Process | Survey | 356 | 64% | No | Presenting, all types | |
| % of sites where pain intensity was evaluated ‘systematically or often’ at the end of patient management | Process | Survey | 356 | 56% | No | Presenting, all types | |
| Ritsema et al (40), 2007 | Proportion of patients whose pain was assessed | Process | Administrative database | 2064 | 1998 to 2000 57%, 2001 to 2003 74%(P<0.01) | Yes | Presenting, long bone fracture |
| Proportion of patients receiving analgesia | Process | Administrative database | 2064 | Any analgesia 1998 to 2000 68% 2001 to 2003 76% | Yes | 1, long bone fracture | |
| Shah and Lendrum (37), 2004 | % of patients with moderate pain (score 4 to 6/10) with analgesia offered at triage | Process | Chart review | 13 | 24% | Yes | Presenting, MSK, abdominal pain |
| % of patients severe pain (score 7 to 10/10) who receive appropriate analgesia within 20 min of arrival or triage (whichever is earlier) | Process | Chart review | 12 | 42% | Yes | Presenting, MSK, abdominal pain | |
| % of patients with moderate pain (score 4 to 6/10) with documented re-evaluation and action within 60 min of receiving first dose of analgesic | Process | Chart review | 13 | 0% | Yes | Presenting, MSK, abdominal pain | |
| % of patients with severe pain (score 7 to 10/10) with documented re-evaluation and action within 30 min of receiving first dose of analgesic | Process | Chart review | 13 | 0% | Yes | Presenting, MSK, abdominal pain | |
| Tanabe et al (47), 2007 | Time from triage to analgesia | Process | Chart review | 529 | Median 90 min (IQR 54–149) | Yes | Presenting, sickle cell disease |
| % of patients who received morphine or hydromorphine as initial analgesic | Process | Chart review | 529 | 87% | Yes | Presenting, sickle cell disease | |
| % of patients who received recommended dose of analgesic | Process | Chart review | 529 | 92% | Yes | Presenting, sickle | |
| cell disease | |||||||
| %of patients who received analgesic by either intravenous or subcutaneous route | Process | Chart review | 529 | 55% | Yes | Presenting, sickle cell disease | |
| Terrell et al (35), 2009 | If an older person remains in the ED for >6 h, then a second pain assessment should be documented within 1 h of arrival to the ED | Process | Chart review | N/A | N/A | No | Presenting, all types |
| If an older person received pain treatment while in the ED, then a pain assessment should be documented before discharge home from the ED | Process | Chart review | N/A | N/A | No | Not specified | |
| If an older person presents to the ED and has moderate to severe pain (score ≥4/10) then pain treatment should be initiated | Process | Chart review | N/A | N/A | No | Presenting, all types | |
| If an older person receives analgesic medication while in the ED, then meperidine should be avoided | Process | Chart review | N/A | N/A | No | Not specified | |
| If an older person receives an opioid analgesia prescription on discharge fromthe ED, then a bowel regimen should also be provided | Process | Chart review | N/A | N/A | No | Not specified | |
| Vega-Stromberg et al (38), 2002 | Patient reports of satisfaction with pain management (% excellent rating) | Outcome | Survey | NR | 34% quarter A, 39% quarter B | No | Not specified |
Type of indicator: Process, Structure, Outcome;
Number of subjects;
Operational: described explicitly and in sufficient detail to be potentially implemented by a reader;
Type of pain: presenting or procedural pain, condition/illness. IQR Interquartile range, MSK Muskuloskeletal; N/A Not applicable, NR Not recorded
Secondary outcomes
Within the included studies, data for the specific indicators were abstracted from chart review (14 of 23), administrative databases (six of 23) and surveys (three of 23). Ninety-one percent of the studies (21 of 23) reported indicators reflecting presenting pain complaints. Some of the included studies evaluated the quality of pain assessment and management for patients with all types of presenting pain (10 of 23), while others focused on specific conditions including back pain, fractures, sickle cell disease, hip fracture and renal/biliary colic (11 of 23). The remaining studies did not specify presenting or procedural pain (two of 23). For 19 of 23 of the studies, our study team rated the indicators as operational (Table 3).
Data collected on the indicators in the individual studies are summarized in Tables 2 and 3. The proportion of patients with documentation of pain assessment ranged from 57% (40) to 94% (41) with 23% of assessments in the latter study measured using a validated pain scale. The proportion of patients with pain reassessment ranged from 32% (42) to 50% (43). For the studies that provided data on indicators reflecting time to analgesia (from arrival or triage), the mean or median was >60 min in six of the nine studies (30,32,33,43–48). The receipt and timing of analgesia varied according to pain severity and type of presenting pain. For example, in one study (49) the proportion of patients offered analgesia ranged from 6% for mild pain (score one to three of 10) to 68% for severe pain (score seven to 10 of 10). With respect to timing of analgesia, the proportion of patients in severe pain (score seven to 10 of 10) who received analgesia within 20 min of arrival or triage ranged from 24% (42) to 83% (50). In another study, 59% of patients with severe pain had a delay >1 h in the time to first analgesic, when measured from triage presentation (48). With respect to specific types of presenting pain, the time to analgesia included a mean of 141 min (from triage) for hip fracture (33), a median of 48 min (from arrival) for renal colic (44) and a median of 90 min (from triage) for sickle cell pain crisis (47). One study measured patient satisfaction, with 34% to 39% of patients reporting ‘excellent’ satisfaction with pain management (38).
DISCUSSION
The increasing awareness of the prevalence and impact of untreated pain in the ED setting, and the growing body of evidence on this topic, precludes a comprehensive summary and review of all studies describing the epidemiology, assessment and management of pain in the ED. As such, we chose to focus on studies that provided quality indicators for the assessment and management of pain in the ED. Our approach enabled us to provide data on performance using existing indicators and to identify important gaps in measurement and quality improvement that are relevant to clinicians, administrators and researchers. Our comprehensive review has identified a total of 20 indicators. While previous work has focused on reviewing existing quality indicators for trauma care (26,51), pediatric emergency medicine (52) and palliative care (53), to the best of our knowledge, this is the first publication to systematically review quality indicators specific to the assessment and management of pain in the ED.
Clinical implications
The clinical implications of the present review are directly relevant to nurses, physicians and administrators alike. Although a significant proportion of patients in the studies reviewed had documentation of pain assessment, few patients were assessed using a validated pain scale. An even smaller proportion of patients had documentation of pain reassessment. Given the negative implications of delays in pain treatment, these findings highlight the importance of encouraging the use of a validated pain scale, and conducting and documenting pain reassessments. It is imperative that pain not only be measured with a valid, objective tool, but also be frequently reassessed to optimize pain management. Our results further suggest that there are delays in the receipt of analgesia, even for patients in severe pain (48) or with clinical conditions known to be associated with significant pain (47). A number of the included studies identified an association between ED crowding and delays in pain management (33,43,45,48,54). An awareness of the impact of crowding on pain management may help to further focus the attention of individual caregivers and hospital administrators on the importance of adequate and timely pain management.
Research implications
A key finding of the present review is that 91% of the identified indicators were specific to presenting pain only. The importance of procedural pain management and the harmful effects of such pain, when left untreated, have long been recognized (8,55–59). Poor management of procedural pain has been documented in multiple care settings including hospitalized children (60), children and adults in acute and critical care settings (61), and adults in the ED (13,62). The relative lack of indicators for procedural pain highlights a significant gap in measurement and a potential missed opportunity for quality improvement.
Previous research has documented variation in pain management based on patient demographic characteristics including race, age and sex (63–68). Results from one of the studies included in the present review indicate that although opioid prescribing in the United States for patients with a pain-related ED visit increased after national quality improvement efforts in the 1990s, differences according to race and ethnicity have not diminished (31). With respect to sex, one of the included studies demonstrated a longer time to analgesia for female patients with acute pain compared with men (47). Other identified factors associated with delays in analgesia that deserve further exploration included language barriers (46) and insurance status (Medicaid) (40). Delays in analgesia were also more likely among children (69) and elderly patients (40,69), suggesting that those at the extremes of the age spectrum are suboptimally assessed and treated for acute pain. Although many of the reviewed studies included or focused on elderly patients, few of the studies included children and none of the indicators were specific to the pediatric population. Given the particular vulnerability of neonates, infants and children to both the short- and long-term consequences of untreated pain (8,55–57), the lack of pediatric-specific pain indicators for the ED represents another important gap in the existing quality measurement and improvement literature.
A final gap identified in the present review was the lack of measures reflecting patient-focused outcomes. Previous work involving performance measurement has highlighted the importance of outcome indicators or, at a minimum, evidence of a link between the process of care and patient outcome (70,71). There was only one outcome indicator identified in the present review (patient satisfaction) (38). Research on the link between pain management and patient satisfaction has generated conflicting results (72–74) and the utility of isolated measurement of patient satisfaction with pain management as a quality improvement tool has been questioned (14). Other potentially relevant and complementary outcomes that warrant further exploration include achievement of pain reduction to the level desired by the patient, quality of life measures, absence from work/school due to pain and pain-related health care visits/admissions. Were these measures to be considered alongside patient satisfaction, we may then have a more comprehensive understanding of patient-level outcomes.
Although many studies have suggested that oligoanalgesia in the ED is both a common and long-standing problem (10–14,75,76), a recent commentary has questioned whether this is true, citing the retrospective nature of the majority of these studies (77). Retrospective data cannot account for patient preference, pain perception and appropriate medical justifications for avoiding analgesia. Furthermore, chart abstraction has variable reliability, and documentation (or lack thereof) does not necessarily reflect analgesia administration (77). Most of the studies included in the present review are subject to the same criticisms. Despite this recent controversy, it is clear that awareness and documentation of pain and its management are, at best, suboptimal. Given that modification of clinical behaviour begins with recognition of the problem, improvements in documentation of patient care and objective measures of quality of care will likely result in better patient outcomes. In addition to further prospective research on pain management, the development of patient-centred outcome indicators and work linking process measures to these patient outcomes would help to clarify the degree to which our current analgesia practices impact the patient.
Strengths and limitations
The strengths of the present review include its comprehensive search strategy, clearly defined eligibility criteria and standardized data extraction. The main weakness of the present review was the variability in study design of included articles, and weaknesses in their description of methodology, outcome assessment and reporting. This made it difficult to compare performance on the indicators among studies. Furthermore, there is no validated quality assessment tool for before-after studies or quality indicator development studies. We mitigated this limitation by using a version of the NOS adapted for before-after studies and rated the quality indicator development study against the indicator development and assessment process, as outlined by the Agency for Healthcare Research and Quality. Additionally, much of the data on the quality indicators is based on chart review and administrative databases. The reliability and accuracy of these data sources for measures of true analgesia provision has, as previously discussed, been raised (77). Finally, our search did not include any literature after December 2010; however, given the large number of screened articles identified, resource limitations prevent further updating of the search.
CONCLUSION
The present review provides a summary of existing quality indicators for pain assessment and management in the ED setting. From a clinical perspective, the results highlight the importance of pain assessment and reassessment using a validated pain score and the potential for delays in analgesia administration, particularly at times when the ED is busy. We also identified gaps in existing performance measures, including a lack of measures for procedural pain and those specific to the pediatric population. Finally, the present review highlights the need for further work linking process measures to patient outcomes. These results can serve as the foundation for future work aimed at generating a complete list of quality indicators that will comprehensively measure the assessment and management of pain in the ED setting and establish a link between measurement of the indicators and patient outcomes.
Acknowledgments
The authors thank Andrea Milne, who conducted the literature search.
APPENDIX 1: MEDLINE* SEARCH STRATEGY
MeSH and key words for quality indicators:
1. exp Quality Indicators, Health Care/
2. exp “Quality of Health Care”/
3. exp Quality Assurance, Health Care/
4. exp Clinical Competence/
5. exp Guideline Adherence/
6. exp “Outcome and Process Assessment (Health Care)”/
7. exp Peer Review, Health Care/
8. exp Program Evaluation/
9. exp Practice Guideline/
10. exp Practice Guideline as Topic/
11. exp Patient Care Management/
12. exp Benchmarking/
13. exp “Outcome Assessment (Health Care)”/
14. exp “Process Assessment (Health Care)”/
15. (adherence adj3 guideline*).tw
16. quality performance measure.tw
17. (performance adj3 guideline*).tw
18. (program adj 3 evaluat*).tw
19. (performance adj3 evaluat*).tw
20. (quality adj3 assess*).tw
21. (quality adj3 improv*).tw
22. OR/1–23
MeSH and keywords for emergency care:
23. exp Emergency Medicine/
24. exp Emergency Medical Services/
25. exp Emergency Service, Hospital/
26. exp Emergencies/
27. exp Ambulatory Care/
28. exp Critical Care/
29. exp Trauma Centers/
30. exp Emergency Nursing/
31. exp Emergency Treatment/
32. emergency department*.tw
33. (emergency adj3 admission*).tw
34. (emergency adj3 admit*)
35. emergency room*.tw
36. emergency ward*.tw
37. acute care.tw
38. (ED or ER).tw
39. (EDs or ERs).tw
40. (emergenc$ adj5 (department$ or ward$ or unit$ or room$ or hospital$ or care or patient$ or physician$ or doctor$ or treatment$)).tw
41. emergency unit*.tw
42. emergency care.tw
43. (trauma adj (centres or centers)).tw
44. (emergency or emergencies).jn
45. OR/23–44
46. 22 (quality indicator terms) AND 45 (emergency terms)
MeSH and key words terms for pain:
47. exp Pain/
48. exp Neuralgia/
49. exp Nociceptors/
50. pain.tw
51. exp Pain Measurement/
52. exp Pain threshold/
53. (pain adj2 management).tw
54. (pain adj 2 assessment).tw
55. (pain adj (scale or score)).tw
56. exp Analgesia/
57. exp Anesthesia/
58. exp “Anesthesia and Analgesia”/
59. analgesi$/tw
60. an?esthes$.tw
61. OR/50–60
62. 46 (quality indicator and emergency terms) AND 61 (pain terms)
63. Limit year to “1980-Current”
The search strategy was translated as appropriate for the other databases
APPENDIX 2. Journals and conference proceedings
| Journals | Conference proceedings |
|---|---|
| Academic Emergency Medicine | American Academy of Pediatrics |
| Annals of Emergency Medicine | American College of Emergency Physicians |
| BMJ Quality and Safety | |
| Canadian Journal of Emergency Medicine | Canadian Association of Emergency Physicians |
| Canadian Medical Association Journal | |
| The Journal of Emergency Medicine | Pediatric Academic Societies |
| Journal of the American Medical Association | Society for Academic Emergency Medicine |
| New England Journal of Medicine Pediatrics |
APPENDIX 3: SUMMARY OF METHODOLOGICAL QUALITY ASSESSMENT:
TABLE 1.
Observational studies (Newcastle Ottawa Scale)†
| Article | Selection‡ | Comparability§ | Outcome¶ |
|---|---|---|---|
| Arendts and Fry (69), 2006 | **** | ** | ** |
| Chu and Brown (44), 2009 | **** | * | * |
| Eder et al (41), 2003 | *** | * | * |
| Forero et al (45), 2008 | **** | ** | ** |
| Grant et al (42), 2006 | *** | ** | |
| Guru and Dubinsky (49), 2000 | *** | * | |
| Hwang et al (43), 2008 | **** | ** | ** |
| Hwang et al (33), 2006 | **** | ** | * |
| Mitchell et al (46), 2009 | **** | ** | * |
| Odesina et al (30), 2010 | *** | * | |
| Pines and Hollander (54), 2008 | **** | ** | ** |
| Pines et al (48), 2010 | **** | ** | ** |
| Pletcher et al (31), 2008 | **** | * | ** |
| Ritsema et al (40), 2007 | **** | * | ** |
| Tanabe et al (47), 2007 | **** | ** | * |
| Maximum | **** | ** | *** |
Not completed for four studies due to study design (one survey [Ricard-Hibon 2004 (56)] and three audits [Goodacre 1996 (25), Shah 2004 (62), Vega-Stromberg 2002 (76)]).
Maximum of four stars for: representativeness of the exposed cohort; selection of the nonexposed cohort; ascertainment of exposure; and demonstration that outcome of interest was not present at start of study;
Maximum of two stars for: comparability of cohorts on the basis of the design or analysis;
Maximum of three stars for: assessment of outcome; was follow-up long enough for outcome to occur; and adequacy of follow-up of cohorts
APPENDIX 3: TABLE 2.
Before-after studies (adapted from Newcastle Ottawa Scale)
| Pre- and post intervention | |||||
|---|---|---|---|---|---|
| Article | Selection† | Comparability‡ | Outcome§ | Intervention¶ | periods†† |
| Hawkes et al (32), 2008 | * | ** | |||
| Jackson (34), 2010 | ** | ||||
| Kuan et al (50), 2009) | * | * | *** | ** | |
| Maximum | *** | * | ***** | ** | ** |
Maximum of three stars for: representativeness of the postintervention group; representativeness of the preintervention group; pre-post intervention groups drawn from the same source.
Maximum of one star for: comparability of the pre- and postintervention groups on the basis of design or analysis.
Maximum of five stars for: validity of outcome assessment; reliability/accuracy of outcome assessment; method of outcome assessment the same for pre-and postintervention groups.
Maximum of two stars for: reporting point in time that intervention occurs; clearly describing intervention.
Maximum of two stars for: pre and postintervention data collected during similar time frame
APPENDIX 3: TABLE 3.
Quality assessment of included indicator development study†
| Article | Identification of candidate indicators‡ | Assessment of candidate indicators§ |
|---|---|---|
| Terrell et al (35), 2009 | ** | * |
| Maximum | *** | ******* |
Based on the Agency for Healthcare Research and Quality (AHRQ) Document on Quality Indicator Measure Development, Implementation, Maintenance, and Retirement;
Maximum of three stars for: literature review to identify candidate indicators; development of conceptual model; expert engagement.
Maximum of seven stars for: initial specifications; literature review on evidence base for candidate indicators; panel review using modified Delphi or Nominal Group process; risk adjustment; empirical analysis; finalization of specifications; summary of evidence for each recommended indicator
APPENDIX 4: INCLUSION CRITERIA FOR FULL TEXT REVIEW
Objective: To identify existing quality indicators for the assessment and management of pain in the ED and acute care setting.
Definitions
Quality of care is defined by the Institute of Medicine (IOM) as the “degree to which health services for individual’s increases the likelihood of desired health outcomes and are consistent with current professional knowledge”.
Quality indicators are explicitly defined and measurable items referring to the structures (staff, equipment, and facilities), processes (prescribing, investigations, interactions between professionals and patients) or outcomes (such as mortality, morbidity or patient satisfaction) of care.
Alternate terms for quality indicators: performance measure, audit filter, indicator, care indicator, benchmark, clinical path expected outcome, quality measure.
Screening Questions
-
Is the article in English?
Yes: go to question 2
No: Exclude and mark as 1-Not English
-
Is the complete article available?
Yes: go to question 3
No: Exclude and mark as 2-Abstract only (we will find full references for these)
-
Are the subjects of the article human?
Yes: go to question 4
No: Exclude and mark as 3-Not Human
-
Is this article a Duplicate?
Yes: Exclude and mark as 4-Duplicate and link to duplicate article by highlighting both in same color
No: go to question 5
-
Is the article original research?
Yes: go to question 6
No: Exclude and mark as 5-Not original research
Examples of original research include:
Systematic Reviews and Meta-analysis
Experimental studies (randomized controlled trials, cluster randomized controlled trials, nonrandomized trials)
Observational studies (cohort study, case-control study, case report, case-series, ecological study, survey, audit, time-series analysis)
Consensus methodologies (systematic methods to combine expert opinion and medical evidence including consensus development conference, Guideline Based, Nominal Group Technique, Delphi (or modified Delphi) Technique, Rand/UCLA appropriateness method)
Examples of non-original research include: letters to the editor, commentaries, nonsystematic reviews, book chapters, guideline, news items
-
Does the article include the development or collection of data on one or more quality indicators?
Yes: Go to question 7
No: Exclude and mark as 6-No Quality Indicators
-
Does the article contain quality indicators relevant to the assessment or treatment of pain?
Yes: Go to question 8
No: Exclude and mark as 7-Not Pain
-
Does the article contain quality indicators relevant to the assessment or management of pain in the ED setting?
Yes: Go to question 9
No: Exclude and mark as 8-Not ED setting
-
Is there another reason for exclusion?
Yes: Exclude and mark as 9 with explanation for reason
No: Include
Footnotes
DISCLOSURES: All authors listed have contributed substantially to the manuscript. This project was supported by an Alberta Innovates Health Solutions (AIHS) Knowledge Transfer/Innovation Research Grant secured by Drs A Stang and S Ali. Dr L Hartling holds a New Investigator Salary Award from the Canadian Institutes of Health Research (CIHR). The funding source (AIHS) had no involvement in data collection, analysis or interpretation. None of the authors were paid to write this article. The corresponding author (Dr A Stang) had full access to all the data and had final responsibility for the decision to submit for publication. All authors have no financial relationships with any organizations that might have an interest in the submitted work. All authors have no other relationships or activities that could appear to have influenced the submitted work. This work has not been submitted or accepted for previous publication.
DISCLOSURES: All authors have no financial relationships with any organizations that may have an interest in the submitted work. All authors have no other relationships or activities that could appear to have influenced the submitted work.
REFERENCES
- 1.Cordell WH, Keene KK, Giles BK, Jones JB, Jones JH, Brizendine EJ. The high prevalence of pain in emergency medical care. Am J Emerg Med. 2002;20:165–9. doi: 10.1053/ajem.2002.32643. [DOI] [PubMed] [Google Scholar]
- 2.Johnston CC, Gagnon AJ, Pepler CJ, Bourgault P. Pain in the emergency department with one-week follow-up of pain resolution. Pain Res Manag. 2005;10:67–70. doi: 10.1155/2005/781916. [DOI] [PubMed] [Google Scholar]
- 3.Tanabe P, Buschmann M. A prospective study of ED pain management practices and the patient’s perspective. J Emerg Nurs. 1999;25:171–7. doi: 10.1016/s0099-1767(99)70200-x. [DOI] [PubMed] [Google Scholar]
- 4.The assessment and management of acute pain in infants, children, and adolescents. Pediatrics. 2001;108:793–7. doi: 10.1542/peds.108.3.793. [DOI] [PubMed] [Google Scholar]
- 5.Brennan F, Carr DB, Cousins M. Pain management: A fundamental human right. Anesth Analg. 2007;105:205–21. doi: 10.1213/01.ane.0000268145.52345.55. [DOI] [PubMed] [Google Scholar]
- 6.Gordon DB, Dahl JL, Miaskowski C, et al. American pain society recommendations for improving the quality of acute and cancer pain management: American Pain Society Quality of Care Task Force. Arch Intern Med. 2005;165:1574–80. doi: 10.1001/archinte.165.14.1574. [DOI] [PubMed] [Google Scholar]
- 7.Anand KJ. Pain, plasticity, and premature birth: A prescription for permanent suffering? Nat Med. 2000;6:971–3. doi: 10.1038/79658. [DOI] [PubMed] [Google Scholar]
- 8.Weisman SJ, Bernstein B, Schechter NL. Consequences of inadequate analgesia during painful procedures in children. Arch Pediatr Adolesc Med. 1998;152:147–9. doi: 10.1001/archpedi.152.2.147. [DOI] [PubMed] [Google Scholar]
- 9.Brown JC, Klein EJ, Lewis CW, Johnston BD, Cummings P. Emergency department analgesia for fracture pain. Ann Emerg Med. 2003;42:197–205. doi: 10.1067/mem.2003.275. [DOI] [PubMed] [Google Scholar]
- 10.Ducharme J. Acute pain and pain control: State of the art. Ann Emerg Med. 2000;35:592–603. doi: 10.1016/s0196-0644(00)70033-3. [DOI] [PubMed] [Google Scholar]
- 11.Ngai B, Ducharme J. Documented use of analgesics in the emergency department and upon release of patients with extremity fractures. Acad Emerg Med. 1997;4:1176–8. doi: 10.1111/j.1553-2712.1997.tb03708.x. [DOI] [PubMed] [Google Scholar]
- 12.Petrack EM, Christopher NC, Kriwinsky J. Pain management in the emergency department: patterns of analgesic utilization. Pediatrics. 1997;99:711–4. doi: 10.1542/peds.99.5.711. [DOI] [PubMed] [Google Scholar]
- 13.Singer AJ, Richman PB, Kowalska A, Thode HC., Jr Comparison of patient and practitioner assessments of pain from commonly performed emergency department procedures. Ann Emerg Med. 1999;33:652–8. [PubMed] [Google Scholar]
- 14.Todd KH, Ducharme J, Choiniere M, et al. Pain in the emergency department: Results of the pain and emergency medicine initiative (PEMI) multicenter study. J Pain. 2007;8:460–6. doi: 10.1016/j.jpain.2006.12.005. [DOI] [PubMed] [Google Scholar]
- 15.Johnston CC, Gagnon AJ, Fullerton L, Common C, Ladores M, Forlini S. One-week survey of pain intensity on admission to and discharge from the emergency department: A pilot study. J Emerg Med. 1997;16:6. doi: 10.1016/s0736-4679(98)00012-2. [DOI] [PubMed] [Google Scholar]
- 16.Lee TH. Eulogy for a quality measure. N Engl J Med. 2007;357:1175–7. doi: 10.1056/NEJMp078102. [DOI] [PubMed] [Google Scholar]
- 17.Bradley EH, Holmboe ES, Mattera JA, Roumanis SA, Radford MJ, Krumholz HM. A qualitative study of increasing beta-blocker use after myocardial infarction: Why do some hospitals succeed? JAMA. 2001;285:2604–11. doi: 10.1001/jama.285.20.2604. [DOI] [PubMed] [Google Scholar]
- 18.Graff L, Stevens C, Spaite D, Foody J. Measuring and improving quality in emergency medicine. Acad Emerg Med. 2002;9:1091–107. doi: 10.1111/j.1553-2712.2002.tb01563.x. [DOI] [PubMed] [Google Scholar]
- 19.Lindsay P, Schull M, Bronskill S, Anderson G. The development of indicators to measure the quality of clinical care in emergency departments following a modified-delphi approach. Acad Emerg Med. 2002;9:1131–9. doi: 10.1111/j.1553-2712.2002.tb01567.x. [DOI] [PubMed] [Google Scholar]
- 20.Mourad SM, Hermens RP, Nelen WL, Braat DD, Grol RP, Kremer JA. Guideline-based development of quality indicators for subfertility care. Hum Reprod. 2007;22:2665–72. doi: 10.1093/humrep/dem215. [DOI] [PubMed] [Google Scholar]
- 21.McGory ML, Shekelle PG, Ko CY. Development of quality indicators for patients undergoing colorectal cancer surgery. J Natl Cancer Inst. 2006;98:1623–33. doi: 10.1093/jnci/djj438. [DOI] [PubMed] [Google Scholar]
- 22.Guru V, Anderson GM, Fremes SE, O’Connor GT, Grover FL, Tu JV. The identification and development of Canadian coronary artery bypass graft surgery quality indicators. J Thorac Cardiovasc Surg. 2005;130:1257. doi: 10.1016/j.jtcvs.2005.07.041. [DOI] [PubMed] [Google Scholar]
- 23.Campbell SM, Braspenning J, Hutchinson A, Marshall MN. Research methods used in developing and applying quality indicators in primary care. BMJ. 2003;326:816–9. doi: 10.1136/bmj.326.7393.816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Campbell SM, Cantrill JA, Roberts D. Prescribing indicators for UK general practice: Delphi consultation study. BMJ. 2000;321:425–8. doi: 10.1136/bmj.321.7258.425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Donabedian A. The quality of care. How can it be assessed? JAMA. 1988;260:1743–8. doi: 10.1001/jama.260.12.1743. [DOI] [PubMed] [Google Scholar]
- 26.Stelfox HT, Bobranska-Artiuch B, Nathens A, Straus SE. A systematic review of quality indicators for evaluating pediatric trauma care. Crit Care Med. 2010;38:1187–96. doi: 10.1097/CCM.0b013e3181d455fe. [DOI] [PubMed] [Google Scholar]
- 27.Wells GA, Shea B, O’Connell D, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Ottawa: Ottawa Health Research Institute; < wwwohrica/programs/clinical_epidemiology/oxford.asp> (Accessed December 11, 2013) [Google Scholar]
- 28.Bond KO, Blitz S, Friesen C, et al. Interventions to reduce overcrowding in emergency departments. Technology Report 67.4. Ottawa: Canadian Agency for Drugs and Technologies in Health; 2006. [Google Scholar]
- 29.Quality Indicator Measure Development, Implementation, Measurement and Retirement 2011. Agency for Healthcare Research and Quality; Rockville, MD: < http://qualityindicators.ahrq.gov/Downloads/Resources/Publications/2011/QI%20Measure%20Development%20Implementation%20Maintenance%20Retirement%20Full%205-3-11.pdf> (Accessed September 9, 2013) [Google Scholar]
- 30.Odesina V, Bellini S, Delaney C, et al. Evidence-based sickle cell pain management in the emergency department. Adv Emerg Nurs J. 2010;18:102–11. [Google Scholar]
- 31.Pletcher MJ, Kertesz SG, Kohn MA, Gonzales R. Trends in opioid prescribing by race/ethnicity for patients seeking care in US emergency departments. JAMA. 2008;299:70–8. doi: 10.1001/jama.2007.64. [DOI] [PubMed] [Google Scholar]
- 32.Hawkes C, Kelleher G, Hourihane J. Paediatric analgesia in an emergency department. Ir Med J. 2008;101:106–9. [PubMed] [Google Scholar]
- 33.Hwang U, Richardson LD, Sonuyi TO, Morrison RS. The effect of emergency department crowding on the management of pain in older adults with hip fracture. J Am Geriatr Soc. 2006;54:270–5. doi: 10.1111/j.1532-5415.2005.00587.x. [DOI] [PubMed] [Google Scholar]
- 34.Jackson SE. The efficacy of an educational intervention on documentation of pain management for the elderly patient with a hip fracture in the emergency department. J Emerg Nurs. 2010;36:10–5. doi: 10.1016/j.jen.2008.08.022. [DOI] [PubMed] [Google Scholar]
- 35.Terrell KM, Hustey FM, Hwang U, Gerson LW, Wenger NS, Miller DK. Quality indicators for geriatric emergency care. Acad Emerg Med. 2009;16:441–9. doi: 10.1111/j.1553-2712.2009.00382.x. [DOI] [PubMed] [Google Scholar]
- 36.Ricard-Hibon A, Ducasse JL, Ravaud P, et al. Quality control programme for acute pain management in emergency medicine: A national survey. Eur J Emerg Med. 2004;11:198–203. doi: 10.1097/01.mej.0000136698.56966.f0. [DOI] [PubMed] [Google Scholar]
- 37.Shah K, Lendrum K. Pain management in an accident and emergency department: How good are we? J Orthopaed Med. 2004:26. [Google Scholar]
- 38.Vega-Stromberg T, Holmes SB, Gorski LA, Johnson BP. Road to excellence in pain management: Research, outcomes and direction (ROAD) J Nurs Care Qual. 2002;17:15–26. doi: 10.1097/00001786-200210000-00003. [DOI] [PubMed] [Google Scholar]
- 39.Goodacre SW, Roden RK. A protocol to improve analgesia use in the accident and emergency department. J Accid Emerg Med. 1996;13:177–9. doi: 10.1136/emj.13.3.177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ritsema TS, Kelen GD, Pronovost PJ, Pham JC. The national trend in quality of emergency department pain management for long bone fractures. Acad Emerg Med. 2007;14:163–9. doi: 10.1197/j.aem.2006.08.015. [DOI] [PubMed] [Google Scholar]
- 41.Eder SC, Sloan EP, Todd K. Documentation of ED patient pain by nurses and physicians. Am J Emerg Med. 2003;21:253–7. doi: 10.1016/s0735-6757(03)00041-x. [DOI] [PubMed] [Google Scholar]
- 42.Grant PS. Analgesia delivery in the ED. Am J Emerg Med. 2006;24:806–9. doi: 10.1016/j.ajem.2006.05.004. [DOI] [PubMed] [Google Scholar]
- 43.Hwang U, Richardson L, Livote E, Harris B, Spencer N, Morrison RS. Emergency department crowding and decreased quality of pain care. Acad Emerg Med. 2008;15:1248–55. doi: 10.1111/j.1553-2712.2008.00267.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Chu K, Brown A. Association between access block and time to parenteral opioid analgesia in renal colic: A pilot study. Emerg Med Australas. 2009;21:38–42. doi: 10.1111/j.1742-6723.2008.01146.x. [DOI] [PubMed] [Google Scholar]
- 45.Forero R, Mohsin M, McCarthy S, et al. Prevalence of morphine use and time to initial analgesia in an Australian emergency department. Emerg Med Australas. 2008;20:136–43. doi: 10.1111/j.1742-6723.2008.01068.x. [DOI] [PubMed] [Google Scholar]
- 46.Mitchell R, Kelly AM, Kerr D. Does emergency department workload adversely influence timely analgesia? Emerg Med Australas. 2009;21:52–8. doi: 10.1111/j.1742-6723.2008.01145.x. [DOI] [PubMed] [Google Scholar]
- 47.Tanabe P, Myers R, Zosel A, et al. Emergency department management of acute pain episodes in sickle cell disease. Acad Emerg Med. 2007;14:419–25. doi: 10.1197/j.aem.2006.11.033. [DOI] [PubMed] [Google Scholar]
- 48.Pines JM, Shofer FS, Isserman JA, Abbuhl SB, Mills AM. The effect of emergency department crowding on analgesia in patients with back pain in two hospitals. Acad Emerg Med. 2010;17:276–83. doi: 10.1111/j.1553-2712.2009.00676.x. [DOI] [PubMed] [Google Scholar]
- 49.Guru V, Dubinsky I. The patient vs. caregiver perception of acute pain in the emergency department. J Emerg Med. 2000;18:7–12. doi: 10.1016/s0736-4679(99)00153-5. [DOI] [PubMed] [Google Scholar]
- 50.Kuan SC, Collins NC, Ryan JM, Callanan I. Treating pain in the emergency department. Eur J Emerg Med. 2009;17:52–5. doi: 10.1097/MEJ.0b013e32832dbe3c. [DOI] [PubMed] [Google Scholar]
- 51.Stelfox HT, Bobranska-Artiuch B, Nathens A, Straus SE. Quality indicators for evaluating trauma care: A scoping review. Arch Surg. 2010;145:286–95. doi: 10.1001/archsurg.2009.289. [DOI] [PubMed] [Google Scholar]
- 52.Alessandrini E, Varadarajan K, Alpern ER, et al. Emergency department quality: An analysis of existing pediatric measures. Acad Emerg Med. 2011;18:519–26. doi: 10.1111/j.1553-2712.2011.01057.x. [DOI] [PubMed] [Google Scholar]
- 53.Pasman HR, Brandt HE, Deliens L, Francke AL. Quality indicators for palliative care: A systematic review. J Pain Symptom Manage. 2009;38:145–56. doi: 10.1016/j.jpainsymman.2008.07.008. [DOI] [PubMed] [Google Scholar]
- 54.Pines JM, Hollander JE. Emergency department crowding is associated with poor care for patients with severe pain. Ann Emerg Med. 2008;51:1–5. doi: 10.1016/j.annemergmed.2007.07.008. [DOI] [PubMed] [Google Scholar]
- 55.Czarnecki ML, Turner HN, Collins PM, Doellman D, Wrona S, Reynolds J. Procedural pain management: A position statement with clinical practice recommendations. Pain Manag Nurs. 2011;12:95–111. doi: 10.1016/j.pmn.2011.02.003. [DOI] [PubMed] [Google Scholar]
- 56.Taddio A, Katz J, Ilersich AL, Koren G. Effect of neonatal circumcision on pain response during subsequent routine vaccination. Lancet. 1997;349:599–603. doi: 10.1016/S0140-6736(96)10316-0. [DOI] [PubMed] [Google Scholar]
- 57.Taddio A, Shah V, Gilbert-MacLeod C, Katz J. Conditioning and hyperalgesia in newborns exposed to repeated heel lances. JAMA. 2002;288:857–61. doi: 10.1001/jama.288.7.857. [DOI] [PubMed] [Google Scholar]
- 58.Bach S, Noreng MF, Tjellden NU. Phantom limb pain in amputees during the first 12 months following limb amputation, after preoperative lumbar epidural blockade. Pain. 1988;33:297–301. doi: 10.1016/0304-3959(88)90288-6. [DOI] [PubMed] [Google Scholar]
- 59.Gordon SM, Dionne RA, Brahim J, Jabir F, Dubner R. Blockade of peripheral neuronal barrage reduces postoperative pain. Pain. 1997;70:209–15. doi: 10.1016/s0304-3959(96)03315-5. [DOI] [PubMed] [Google Scholar]
- 60.Stevens BJ, Abbott LK, Yamada J, et al. Epidemiology and management of painful procedures in children in Canadian hospitals. CMAJ. 2011;183:E403–10. doi: 10.1503/cmaj.101341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Puntillo KA, White C, Morris AB, et al. Patients’ perceptions and responses to procedural pain: Results from Thunder Project II. Am J Crit Care. 2001;10:238–51. [PubMed] [Google Scholar]
- 62.Tcherny-Lessenot S, Karwowski-Soulie F, Lamarche-Vadel A, Ginsburg C, Brunet F, Vidal-Trecan G. Management and relief of pain in an emergency department from the adult patients’ perspective. J Pain Symptom Manage. 2003;25:539–46. doi: 10.1016/s0885-3924(03)00147-7. [DOI] [PubMed] [Google Scholar]
- 63.Chen EH, Shofer FS, Dean AJ, et al. Gender disparity in analgesic treatment of emergency department patients with acute abdominal pain. Acad Emerg Med. 2008;15:414–8. doi: 10.1111/j.1553-2712.2008.00100.x. [DOI] [PubMed] [Google Scholar]
- 64.Heins A, Grammas M, Heins JK, Costello MW, Huang K, Mishra S. Determinants of variation in analgesic and opioid prescribing practice in an emergency department. J Opioid Manag. 2006;2:335–40. doi: 10.5055/jom.2006.0049. [DOI] [PubMed] [Google Scholar]
- 65.Platts-Mills TF, Esserman DA, Brown DL, Bortsov AV, Sloane PD, McLean SA. Older US emergency department patients are less likely to receive pain medication than younger patients: Results from a national survey. Ann Emerg Med. 2011;60:199–206. doi: 10.1016/j.annemergmed.2011.09.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Safdar B, Heins A, Homel P, Miner J, Neighbor M, DeSandre P, Todd KH. Impact of physician and patient gender on pain management in the emergency department – a multicenter study. Pain Med. 2009;10:364–72. doi: 10.1111/j.1526-4637.2008.00524.x. [DOI] [PubMed] [Google Scholar]
- 67.Todd KH, Deaton C, D’Adamo AP, Goe L. Ethnicity and analgesic practice. Ann Emerg Med. 2000;35:11–6. doi: 10.1016/s0196-0644(00)70099-0. [DOI] [PubMed] [Google Scholar]
- 68.Selbst SM, Clark S. Analgesic use in the emergency department. Ann Emerg Med. 1990;19:4. doi: 10.1016/s0196-0644(05)82565-x. [DOI] [PubMed] [Google Scholar]
- 69.Arendts G, Fry M. Factors associated with delay to opiate analgesia in emergency departments. J Pain. 2006;7:682–6. doi: 10.1016/j.jpain.2006.03.003. [DOI] [PubMed] [Google Scholar]
- 70.Rubin HR, Pronovost P, Diette GB. The advantages and disadvantages of process-based measures of health care quality. Int J Qual Health Care. 2001;13:469–74. doi: 10.1093/intqhc/13.6.469. [DOI] [PubMed] [Google Scholar]
- 71.Clancy CM, Dougherty D, Walker E. The importance of outcomes research in pediatric emergency medicine. Ambul Pediatr. 2002;2(4 Suppl):293–300. doi: 10.1367/1539-4409(2002)002<0293:tioori>2.0.co;2. [DOI] [PubMed] [Google Scholar]
- 72.Downey LV, Zun LS. Pain management in the emergency department and its relationship to patient satisfaction. J Emerg Trauma Shock. 2010;3:326–30. doi: 10.4103/0974-2700.70749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Stahmer SA, Shofer FS, Marino A, Shepherd S, Abbuhl S. Do quantitative changes in pain intensity correlate with pain relief and satisfaction? Acad Emerg Med. 1998;5:851–7. doi: 10.1111/j.1553-2712.1998.tb02811.x. [DOI] [PubMed] [Google Scholar]
- 74.Kelly AM. Patient satisfaction with pain management does not correlate with initial or discharge VAS pain score, verbal pain rating at discharge, or change in VAS score in the Emergency Department. J Emerg Med. 2000;19:113–6. doi: 10.1016/s0736-4679(00)00219-5. [DOI] [PubMed] [Google Scholar]
- 75.Drendel AL, Brousseau DC, Gorelick MH. Pain assessment for pediatric patients in the emergency department. Pediatrics. 2006;117:1511–8. doi: 10.1542/peds.2005-2046. [DOI] [PubMed] [Google Scholar]
- 76.Rupp T, Delaney KA. Inadequate analgesia in emergency medicine. Ann Emerg Med. 2004;43:494–503. doi: 10.1016/j.annemergmed.2003.11.019. [DOI] [PubMed] [Google Scholar]
- 77.Green SM. There is oligo-evidence for oligoanalgesia. Ann Emerg Med. 2012;60:212–4. doi: 10.1016/j.annemergmed.2012.06.006. [DOI] [PubMed] [Google Scholar]


