Abstract
Kawasaki disease, predominantly a disease of childhood, includes such symptoms as acute vasculitis, mucosal inflammation, rash, cervical adenopathy, and edema. Its most severe forms are associated with coronary artery aneurysms. We report a rare case of this disease in an asymptomatic adult and review its epidemiology, etiology, diagnosis, treatment, and prognosis.
Key words: Coronary artery aneurysm, coronary artery bypass grafting, Kawasaki disease, mucocutaneous lymph node syndrome
Kawasaki disease, or mucocutaneous lymph node syndrome, occurs predominantly in children and rarely in adults.1 Symptoms include acute vasculitis, mucosal inflammation, rash, cervical adenopathy, hand and foot swelling, and late fingertip desquamation.2 In the most severe cases, aneurysms develop in one or more coronary arteries.3 We report a rare case of Kawasaki disease associated with multiple coronary artery aneurysms in an asymptomatic adult and review the epidemiology, etiology, differential diagnosis, treatment, and prognosis.
Case Report
A 36-year-old white man with dyslipidemia presented at our institution for routine annual examination, including treadmill testing and technetium-99m sestamibi single-photon emission computed tomography (TMT-MIBI). The patient had experienced no chest pain, shortness of breath, paroxysmal nocturnal dyspnea, or orthopnea. Medical history included pneumonia and scarlet fever complicated by severe mucositis and conjunctivitis at 4 years of age. Family history included myocardial infarction in the patient's father at 50 years of age. The patient was not taking medications and had no history of tobacco or recreational drug use. On physical examination, the blood pressure was 128/76 mmHg, and the heart rate was 68 beats/min. Pulmonary and cardiovascular examination revealed nothing unusual. Resting electrocardiography showed sinus rhythm and early repolarization but no other abnormality (Fig. 1).
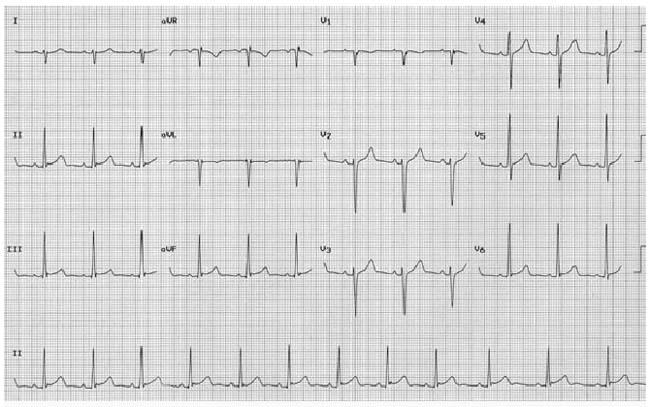
Fig. 1 Electrocardiogram shows normal sinus rhythm and early repolarization.
The patient underwent exercise stress testing on a continuous graded treadmill for 7 minutes. He reported no exercise-induced symptoms during testing and achieved 93% of the maximum predicted heart rate and an adequate blood pressure response. At peak exercise, the exercise electrocardiogram was abnormal. Perfusion imaging of the heart showed a large area of severe stress-induced ischemia encompassing the anterior, anterolateral, inferoapical, and apical walls and a mild decrease in left ventricular ejection fraction (Fig. 2).
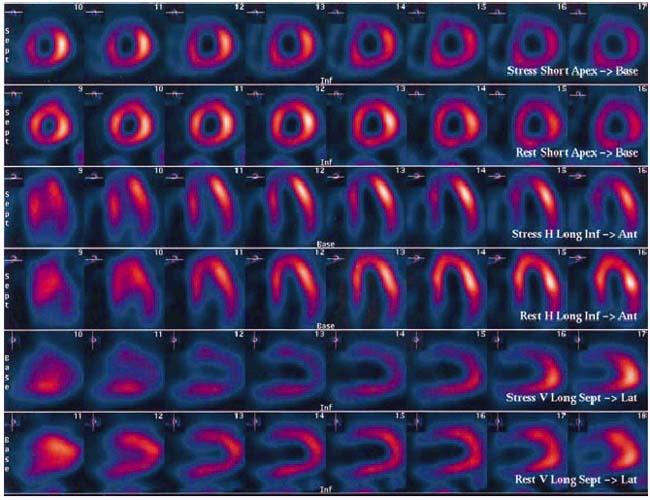
Fig. 2 Results of treadmill testing and technetium-99m sestamibi single-photon emission computed tomography (TMT-MIBI).
Coronary angiography revealed a heavily calcified and aneurysmal left main coronary artery and proximal left anterior descending coronary artery (LAD), 90% stenosis of the proximal LAD with atresia in the middle to distal segments, neovascularization in the area supplied by the LAD, and stenotic but nonobstructive aneurysms in the proximal and middle segments of the right coronary artery (Fig. 3).
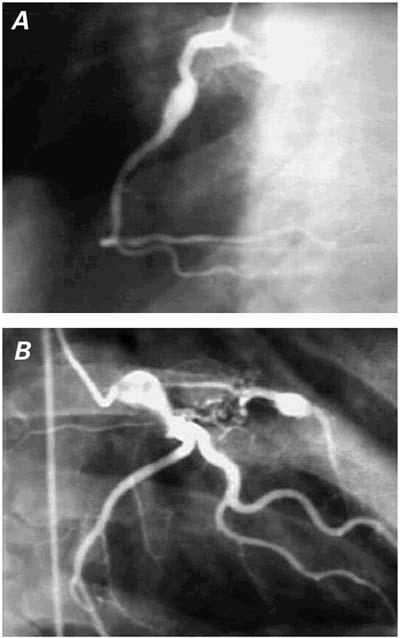
Fig. 3 Coronary angiograms show A) abnormal right coronary artery and B) abnormal left main and left anterior descending coronary arteries.
A diagnosis of Kawasaki disease was made on the basis of these findings. The patient subsequently underwent coronary artery bypass grafting in which the left internal mammary artery was grafted onto the LAD. No surgical complications occurred, and anticoagulant therapy was begun postoperatively with the intention of continuing it indefinitely. The preoperative catheterization findings were confirmed at surgery. The patient was examined 6 months postoperatively and was completely asymptomatic.
Discussion
Epidemiology
Kawasaki disease occurs worldwide. In many areas, it is more common than rheumatic fever and viral myocarditis. Kawasaki disease is the leading cause of acquired heart disease in children in North America and Japan, where its annual incidence is rising.4,5 Major epidemics have occurred in both Japan and the United States. The recurrence rate is very low (<2%–3%). Secondary cases are rare and usually occur in siblings.6
Kawasaki disease is most commonly found in the Asian population.7,8 In Japan, the incidence is 10 times greater than it is in Western countries.9 The mean annual incidence is 90 to 112 per 100,000 people in Japan,10,11 compared with 3.6 to 3.7 per 100,000 people in Britain and Australia.12,13 In the United States, 2,000 cases of Kawasaki disease are reported annually, with a mean annual incidence of 6 to 9 per 100,000 children less than 5 years old and a peak incidence in children from 1 to 2 years old.14 Interestingly, the overall incidence in Hawaii, where a large proportion of the population is of Asian ancestry, is lower than the incidence in Japan.15 This suggests that both genetic susceptibility and environmental factors may play a role in Kawasaki disease. Previous epidemiologic studies have identified possible environmental factors, including carpet cleaning, residence near a large body of water, and residence in temperate climates. One study16 found that the incidence of Kawasaki disease in San Diego correlated inversely with average monthly temperature and positively with average monthly precipitation.
Etiology and Pathophysiology
Although an infectious origin for Kawasaki disease is suspected, no pathogen has been identified. Kawasaki disease has two phases: an acute phase lasting 1 to 2 weeks, followed by a chronic (“convalescent”) phase.17 Untreated disease usually resolves spontaneously after several weeks. The major pathologic feature of Kawasaki disease is acute systemic vasculitis. Coronary artery lesions usually develop early in the acute phase; rarely do they develop more than 4 weeks after disease onset. These early lesions are marked by endothelial cell edema, proliferation, necrosis, and adhesion of polymorphonuclear leukocytes to endothelium. These events are accompanied by marked immune activation, characterized by increasing levels of circulating cytokines and CD4 and CD8 cells, polyclonal hypergammaglobulinemia, and circulating IgG and IgM immunocomplexes.18
Clinical and Laboratory Findings
Classic symptoms of Kawasaki disease include fever, rash, oral mucositis, conjunctivitis, lymphadenopathy, and skin desquamation. At least 5 of these—or 4 if accompanied by coronary artery aneurysm—are required for diagnosis. Common laboratory findings include leukocytosis, thrombocytosis, elevated erythrocyte sedimentation rate, C-reactive protein positivity, and slightly elevated serum transaminase. Antinuclear antibody and rheumatoid factor are usually absent.
Cardiac Findings
Myocardial Involvement
Generally, myocarditis occurs to some degree during the acute phase of Kawasaki disease but typically resolves completely and does not predict coronary artery involvement.19 Clinical findings include an S3 or S4 gallop on physical examination, nonspecific ST-T changes or low voltage on the electrocardiogram, small pericardial effusions and depressed left ventricular systolic function on the echocardiogram, and cardiomegaly on the chest radiograph. Long-term impairment of left ventricular systolic function seldom occurs in the absence of coronary artery disease. The aortic and mitral valves are rarely involved; if they are, the involvement is usually clinically benign and regresses spontaneously. Persistent valvular disease generally coexists with coronary artery disease.20
Coronary Artery Aneurysms
Coronary artery sequelae, usually aneurysms, occur in 20% to 25% of cases. Factors in aneurysmal formation include maximum body temperature, prolonged fever, prolonged erythrocyte sedimentation rate elevation, markedly elevated white blood cell count, anemia, and time (<1 year) since disease onset. However, none of these can absolutely predict aneurysmal development.21
In Kawasaki disease, aneurysms occur predominantly in the proximal segments and at bifurcations of the coronary arteries and often involve multiple vessels. They are seen in 90% of fatal cases. Distal aneurysms are uniformly accompanied by more proximal aneurysms. Aneurysms may also form in other arteries, most often the renal, iliac, or axillary.22
Coronary artery aneurysms are classified as localized or giant (>8 mm in diameter) and are usually diagnosed by 2-dimensional echocardiography. Half to two thirds resolve spontaneously.23 In about 50% of cases, complete, spontaneous resolution is seen on echocardiography or angiography within 1 year after onset.24 Resolution is directly proportional to the extent of dilatation and occurs by myointimal proliferation or thrombus organization.
Prognosis
Patients with Kawasaki disease-related aneurysms generally remain asymptomatic. They display normal findings on electrocardiograms and stress tests and are at low risk of subsequent myocardial infarction or sudden death. Sometimes, aneurysms persist and become occlusive, thereby increasing the risk of myocardial infarction or sudden death. Myocardial infarction can occur early or late after the acute phase; therefore, patients should be counseled to avoid atherosclerotic risk factors, and the progress of these patients should be followed into adulthood.25
The most important predictor of myocardial infarction and other chronic sequelae is aneurysmal size.26 Giant coronary artery aneurysms have a poor prognosis. They do not regress and usually result in ischemic heart disease. Affected arterial segments eventually calcify, thrombose, or become stenotic. In 1 long-term study of coronary artery aneurysms in 1,215 patients who had Kawasaki disease, giant coronary artery aneurysms developed in 64 (5%).27 Analysis of this subgroup revealed regression without complications in 3 (5%), occlusion or stenosis in 30 (47%), and myocardial infarction in 15 (23%).
Coronary artery lesions are dynamic in the late acute and early convalescent phases. The longer the aneurysms or stenotic lesions persist, the less likely they are to resolve.28 Lesions in the right and left coronary arteries appear to progress differently.29 Massive thrombosis of the aneurysm is seen predominantly in the right coronary artery, usually within 1 year after disease onset. Progressive localized stenosis at the aneurysm inlet or outlet is seen predominantly in the left coronary artery, again usually within 1 year.
It is unclear whether resolution of coronary artery aneurysms represents true healing, permanent “filling in” by either intimal proliferation or thrombus organization, or arterial wall contraction after scar formation. Kurisu and colleagues30 showed that angiographically normal arterial segments at previously aneurysmal sites are less distensible. Researchers using intravascular ultrasound31 and coronary angiography32 have shown that, in patients whose aneurysms regress, coronary arteries become stiffer and can exhibit chronic morphologic and functional abnormalities.
Vascular damage incurred during the acute phase of Kawasaki disease can lead to vascular abnormalities years later.33 It is unknown whether survivors who have angiographically normal coronary arteries after resolution of aneurysms are at increased risk for premature coronary artery atherosclerosis. Using a Doppler guidewire, Hamaoka's group34 found abnormalities in flow dynamics and decreased flow reserve in intermediate and large coronary artery aneurysms, even those of mild-to-moderate severity. Although some of the chronic coronary artery aneurysms in patients with Kawasaki disease are associated with stenosis and abnormal perfusion and ventricular function in adjacent myocardium, Hijazi and associates,35 using TMT-MIBI, found that most such aneurysms are associated with normal perfusion and function.
Morbidity and Mortality
The overall mortality rate of Kawasaki disease in children is less than 1%.36 This low rate is due to the advantages of critical care facilities, early surgical intervention, improved management of complications, and early use of antithrombotic therapy. A nonfatal myocardial infarction increases the risk of subsequent myocardial infarction and death unless intervention, usually revascularization, takes place. Most deaths now occur during the convalescent phase, generally secondary to complications of ischemic heart disease.
Treatment
The goal in treating Kawasaki disease is to control acute inflammation and to prevent serious cardiovascular complications, such as coronary artery disease.37
Intravenous Gammaglobulin
Until recently, the standard treatment for acute-phase Kawasaki disease was a 4-day regimen of intravenous (IV) gammaglobulin (400 mg/kg daily), supplemented with aspirin (100 mg/kg daily through day 14 and 3–5 mg/kg daily thereafter).38 Now, the standard treatment is a single infusion of IV gammaglobulin (2 g/kg) followed by low-dose aspirin therapy. The newer regimen is apparently more effective because it safely accelerates the resolution of systemic inflammation.39 Concerns about the use of routine IV gammaglobulin include the cost, the risk of transfusion-related complications, and the need to delay scheduled live-virus vaccinations for at least 6 months.40 Since up to 80% of IV gammaglobulin recipients may never have coronary artery aneurysms, identifying those patients with Kawasaki disease who are at highest risk for coronary artery disease is fundamental.
Revascularization
Coronary revascularization is recommended for patients with giant or multiple coronary artery aneurysms or significant stenosis. Overall mortality is low for such operations, and graft target sites are easily accessible, since most coronary artery lesions occur in proximal segments with little distal involvement.39,41 In situ arterial grafts are preferred, because they have excellent potential for growth with the patient.
Screening Echocardiography
Screening echocardiography is used to determine the nature and extent of coronary artery lesions and to establish a management plan.42 Echocardiography has a sensitivity and specificity of 90% to 95% in detecting proximal coronary artery aneurysms.43 If an aneurysm is found, serial echocardiography is warranted. Coronary angiography is considered essential only when coronary artery aneurysms are discovered.
Summary
Kawasaki disease usually resolves spontaneously but may lead to serious complications, including coronary artery disease, if left untreated. Treatment includes early control of acute inflammation and monitoring for aneurysmal complications. As in the present rare case of Kawasaki disease in an adult, coronary revascularization, followed by monitoring for complications and initiation of appropriate therapy, is recommended for patients with giant or multiple coronary artery aneurysms and stenotic or occlusive lesions.
Footnotes
Address for reprints: Benjamin W. Eidem, MD, Texas Children's Hospital, MC 2-2280, 6621 Fannin, West Tower, 20th Floor, Houston, TX 77030
E-mail: bweidem@texaschildrenshospital.org
References
- 1.Naoe S, Takahashi K, Masuda H, Tanaka N. Kawasaki disease. With particular emphasis on arterial lesions. Acta Pathol Jpn 1991;41:785–97. [DOI] [PubMed]
- 2.Gersony WM. Diagnosis and management of Kawasaki disease. JAMA 1991;265:2699–703. [PubMed]
- 3.Bradway MW, Drezner AD. Popliteal aneurysm presenting as acute thrombosis and ischemia in a middle-aged man with a history of Kawasaki disease. J Vasc Surg 1997;26: 884–7. [DOI] [PubMed]
- 4.Rowley SH, Shulman ST. The search for the etiology of Kawasaki disease. Pediatr Infect Dis J 1987;6:506–8. [DOI] [PubMed]
- 5.Rauch AM. Kawasaki syndrome: issues in etiology and treatment. Adv Pediatr Infect Dis 1989;4:163–82. [PubMed]
- 6.Yanagawa H, Nakamura Y, Yashiro M, Fujita Y, Nagai M, Kawasaki T, et al. A nationwide incidence survey of Kawasaki disease in 1985–1986 in Japan. J Infect Dis 1988;158: 1296–301. [DOI] [PubMed]
- 7.Taubert KA. Epidemiology of Kawasaki disease in the United States and worldwide. Prog Pediatr Cardiol 1997;6:181–5.
- 8.Rowley AH, Shulman ST. Kawasaki syndrome. Pediatr Clin North Am 1999;46:313–29. [DOI] [PubMed]
- 9.Mason W, Schneider T, Takahashi M. The epidemiology and etiology of Kawasaki disease. Cardiol Young 1991;1: 196–205.
- 10.Yanagawa H, Nakamura Y, Yashiro M, Oki I, Hirata S, Zhang T, Kawasaki T. Incidence survey of Kawasaki disease in 1997 and 1998 in Japan. Pediatrics 2001;107:E33. [DOI] [PubMed]
- 11.Yanagawa H, Nakamura Y, Yashiro M, Ojima T, Tanihara S, Oki I, Zhang T. Results of the nationwide epidemiologic survey of Kawasaki disease in 1995 and 1996 in Japan. Pediatrics 1998;102:E65. [DOI] [PubMed]
- 12.Royle JA, Williams K, Elliott E, Sholler G, Nolan T, Allen R, Isaacs D. Kawasaki disease in Australia, 1993–95. Arch Dis Child 1998;78:33–9. [DOI] [PMC free article] [PubMed]
- 13.Dhillon R, Newton L, Rudd PT, Hall SM. Management of Kawasaki disease in the British Isles. Arch Dis Child 1993; 69:631–8. [DOI] [PMC free article] [PubMed]
- 14.Dajani AS, Taubert KA, Gerber MA, Shulman ST, Ferrieri P, Freed M, et al. Diagnosis and therapy of Kawasaki disease in children. Circulation 1993;87:1776–80. [DOI] [PubMed]
- 15.Holman RC, Shahriari A, Effler PV, Belay ED, Schonberger LB. Kawasaki syndrome hospitalizations among children in Hawaii and Connecticut. Arch Pediatr Adolesc Med 2000;154:804–8. [DOI] [PubMed]
- 16.Bronstein DE, Dille AN, Austin JP, Williams CM, Palinkas LA, Burns JC. Relationship of climate, ethnicity and socioeconomic status to Kawasaki disease in San Diego County, 1994 through 1998. Pediatr Infect Dis J 2000;19:1087–91. [DOI] [PubMed]
- 17.Laupland KB, Dele Davies H. Epidemiology, etiology, and management of Kawasaki disease: state of the art. Pediatr Cardiol 1999;20:177–83. [DOI] [PubMed]
- 18.Butler DF, Hough DR, Friedman SJ, Davis HE. Adult Kawasaki syndrome. Arch Dermatol 1987;123:1356–61. [PubMed]
- 19.Hiraishi S, Yashiro K, Oguchi K, Kusano S, Ishii K, Nakazawa K. Clinical course of cardiovascular involvement in the mucocutaneous lymph node syndrome. Relation between clinical signs of carditis and development of coronary arterial aneurysm. Am J Cardiol 1981;47:323–30. [DOI] [PubMed]
- 20.Akagi T, Kato H, Inoue O, Sato N, Imamura K. Valvular heart disease in Kawasaki syndrome: incidence and natural history. Am Heart J 1990;120:366–72. [DOI] [PubMed]
- 21.Gidding SS. Risk factors for coronary aneurysms in Kawasaki disease. In: Program and Abstracts of the Third International Kawasaki Disease Symposium; 1988 Nov 29; Tokyo, Japan. p. 229–32.
- 22.Kato H, Inoue O, Akagi T. Kawasaki disease: cardiac problems and management. Pediatr Rev 1988;9:209–17. [DOI] [PubMed]
- 23.Sundel RP, Newburger JW. Kawasaki disease and its cardiac sequelae. Hosp Pract (Off Ed) 1993;28:51–4, 57–60, 64–6. [DOI] [PubMed]
- 24.Kato H, Ichinose E, Yoshioka F, Takechi T, Matsunaga S, Suzuki K, Rikitake N. Fate of coronary aneurysms in Kawasaki disease: serial coronary angiography and long-term follow-up study. Am J Cardiol 1982;49:1758–66. [DOI] [PubMed]
- 25.Iemura M, Ishii M, Sugimura T, Akagi T, Kato H. Long term consequences of regressed coronary aneurysms after Kawasaki disease: vascular wall morphology and function. Heart 2000;83:307–11. [DOI] [PMC free article] [PubMed]
- 26.Suzuki A, Kamiya T. Visualization of coronary artery lesions in Kawasaki disease by angiography. Cardiol Young 1991;1:225–33.
- 27.Inoue O, Akagi T, Kato H. Fate of giant coronary artery aneurysms in Kawasaki disease: long-term follow-up study [abstract]. Circulation 1989;80(Suppl II):II262.
- 28.Suzuki A, Kamiya T, Ono Y, Kohata T, Kimura K, Takamiya M. Follow-up study of coronary artery lesions due to Kawasaki disease by serial selective arteriography in 200 patients. Heart Vessels 1987;3:159–65. [DOI] [PubMed]
- 29.Suzuki A, Kamiya T, Yasuo O, Kuroe K. Extended long term follow-up study of coronary arterial lesions in Kawasaki disease. J Am Coll Cardiol 1991;17(2):33A.
- 30.Kurisu Y, Azumi T, Sugahara T, Igarashi Y, Takamiya M, Kozuka T. Variation in coronary arterial dimension (distensible abnormality) after disappearing aneurysm in Kawasaki disease. Am Heart J 1987;114:532–8. [DOI] [PubMed]
- 31.Suzuki A, Yamagishi M, Kimura K, Sugiyama H, Arakaki Y, Kamiya T, Miyatake K. Functional behavior and morphology of the coronary artery wall in patients with Kawasaki disease assessed by intravascular ultrasound. J Am Coll Cardiol 1996;27:291–6. [DOI] [PubMed]
- 32.Sugimura T, Kato H, Inoue O, Takagi J, Fukuda T, Sato N. Vasodilatory response of the coronary arteries after Kawasaki disease: evaluation by intracoronary injection of isosorbide dinitrate. J Pediatr 1992;121(5 Pt 1):684–8. [DOI] [PubMed]
- 33.Dhillon R, Clarkson P, Donald AE, Powe AJ, Nash M, Novelli V, et al. Endothelial dysfunction late after Kawasaki disease. Circulation 1996;94:2103–6. [DOI] [PubMed]
- 34.Hamaoka K, Onouchi Z, Kamiya Y, Sakata K. Evaluation of coronary flow velocity dynamics and flow reserve in patients with Kawasaki disease by means of a Doppler guide wire. J Am Coll Cardiol 1998;31:833–40. [DOI] [PubMed]
- 35.Hijazi ZM, Udelson JE, Snapper H, Rhodes J, Marx GR, Schwartz SL, Fulton DR. Physiologic significance of chronic coronary aneurysms in patients with Kawasaki disease. J Am Coll Cardiol 1994;24:1633–8. [DOI] [PubMed]
- 36.Yanagawa H, Nakamura Y, Yashiro M, Ojima T, Koyanagi H, Kawasaki T. Update of the epidemiology of Kawasaki disease in Japan—from the results of 1993–94 nationwide survey. J Epidemiol 1996;6:148–57. [DOI] [PubMed]
- 37.Pahl E, Neches WH, Ettedgui JA. Controversies in the medical management of Kawasaki disease. Cardiol Young 1991;1:234–9.
- 38.Newburger JW, Takahashi M, Beiser AS, Burns JC, Bastian J, Chung KJ, et al. A single intravenous infusion of gamma globulin as compared with four infusions in the treatment of acute Kawasaki syndrome. N Engl J Med 1991;324:1633–9. [DOI] [PubMed]
- 39.Kitamura S, Kameda Y, Seki T, Kawachi K, Endo M, Takeuchi Y, et al. Long-term outcome of myocardial revascularization in patients with Kawasaki coronary artery disease. A multicenter cooperative study. J Thorac Cardiovasc Surg 1994;107:663–74. [PubMed]
- 40.Ferusho K, Kamiya T, Nakano H, Kiyosawa N, Shinomiya K, Hayashidera T, et al. High-dose intravenous gammaglobulin for Kawasaki disease. Lancet 1984;2(8411):1055–8. [DOI] [PubMed]
- 41.Kitamura S. Surgical management of cardiovascular lesions in Kawasaki disease. Cardiol Young 1991;1:240–53.
- 42.Capannari TE, Daniels SR, Meyer RA, Schwartz DC, Kaplan S. Sensitivity, specificity and predictive value of two-dimensional echocardiography in detecting coronary artery aneurysms in patients with Kawasaki disease. J Am Coll Cardiol 1986;7:355–60. [DOI] [PubMed]
- 43.Ettedgui J, Neches WH, Pahl E. The role of cross-sectional ECHO in Kawasaki disease. Cardiol Young 1991;1:221–4.


