Abstract
Introduction
Clinical lumbar instability (CLI) is one of the subgroups of chronic non-specific low back pain. Thai rice farmers often have poor sustained postures during a rice planting process and start their farming at an early age. However, individual associated factors of CLI are not known and have rarely been diagnosed in low back pain. This study aimed to determine the prevalence and individual associated factors of CLI in Thai rice farmers.
Methods
A cross-sectional survey was conducted among 323 Thai rice farmers in a rural area of Khon Kaen province, Thailand. Face-to-face interviews were conducted using the 13-item Delphi criteria questionnaire, after which an objective examination was performed using aberrant movement sign, painful catch sign, and prone instability test to obtain information. Individual factors such as sex, body mass index, waist-hip ratio, smoking, and number of years of farming experience, were recorded during the face-to-face interview.
Results
The prevalence of CLI in Thai rice farmers calculated by the method described in this study was 13% (age 44±10 years). Number of years of farming experience was found to be significantly correlated with the prevalence of CLI (adjusted odds ratio =2.02, 95% confidence interval =1.03–3.98, P<0.05).
Conclusion
This study provides prevalence of CLI in Thai rice farmers. Those with long-term farming experience of at least 30 years have a greater risk of CLI.
Keywords: Delphi study, aberrant movement sign, painful catch sign, prone instability test
Introduction
Rice farming is a tradition in Thailand. Despite advances in agricultural technology, most Thai farmers still utilize the traditional way of farming their crop, requiring extensive labor for each process. This results in abnormal mechanical loading and accumulating repetitive strain to the lumbar spine is a consequence. Low back pain (LBP) is the most common musculoskeletal complaint among this sector of the work force. Stooping together with trunk twisting, a common working posture of Thai rice farmers, generates an extremely high load on the lumbar spine, leading to a micro-fracture of the vertebral end plate.1 After the healing process, the thick and dense scar tissue developed over the micro-fracture deters the nutrient delivery to the disc fibers. The disc fibers and surrounding structures then become weaker and later atrophic. Over a period of time, this cumulative trauma may cause disc protrusion and spine instability eventually.2 Many studies demonstrate the problems of pain, functional disability, quality of life, and economic burden of LBP.3–6 The 1 year prevalence of LBP for farmers in developed countries is 47% in Sweden, 37% in the US and Ireland, and 23% in Finland, however in developing countries, it is higher; 72% in South West Nigeria, 64% in the People’s Republic of China, and 60% in India.7 In Thailand, the 1 year prevalence of LBP in rice farmers amounts to 57%, and the lumbar spine is the most common region of body discomfort.6,8 Lumbar instability is one of the causes of nonspecific LBP9–11 and is divided into two subgroups, clinical lumbar instability (CLI) and radiological lumbar instability.12 None of the previous studies have yet addressed CLI in farmers.
Lumbar instability without any defects of the bony structure of the lumbar spine has been frequently mentioned as a biomechanically important subgroup associated with spinal dysfunction and risk of recurrence of LBP. Although traditional radiographic film is quantifiable, it concentrates on the end range of movements. Symptoms of CLI often occur either during movements or provocation tests, and are prominent in the middle range of movements. Diagnostic methods for detecting CLI are both subjective and objective descriptors.12,13 The popular subjective aspect is based on the Delphi checklist for CLI.13 Many clinical tests such as aberrant movement, prone instability, painful catch, and apprehension sign are recommended for detecting CLI.3,5,11,14 Up to date, however, the prevalence of CLI in rice farmers based on a combination of the subjective aspect of the Delphi checklist and physical examination has not been reported.
Risk factors of LBP have been studied thoroughly, but those of CLI have not been determined yet. Individual factors such as heredity, age, sex, body build, postural deformities, physical activity, marital and social factors are associated with LBP as well as physical factors (heavy physical strain, frequent lifting, and postural stress).4,15–17 We hypothesized that individual factors such as age, sex, smoking, and number of years of farming experience were associated with CLI. The purpose of this study therefore, was to determine the prevalence of CLI and the individual risk factors associated with CLI in rice farmers. Its aim to prove that early detection of CLI may help prevent deterioration in lumbar instability.
Material and methods
Study design
This study was a cross-sectional survey, conducted in Khon Kaen Province, Thailand. It was approved by the Ethics Committee for Human Research at Khon Kaen University (HE 562080) based on the Declaration of Helsinki.
Participants
Three hundred and twenty-three rice farmers, aged between 20–60 years, who had LBP at the time of our interview participated in the study. LBP was defined as persisting pain in the area between the twelfth rib and inferior gluteal fold with or without associated leg pain at least 24 hours prior to the interview.4 They were excluded if they had other spinal pathology such as fracture, tumor, and tuberculosis that might interfere with the study protocol and/or were pregnant.5
Diagnosis of CLI
At least seven out of 13 subjective examinations must be positive,13 and with at least two out of three giving a positive response, namely the painful catch sign, prone instability test, and aberrant movement sign, as defined as a criterion for CLI.3,5,11 The process of screening tests for CLI was as follows: 1) each volunteer farmer was interviewed using the subjective aspect of the Delphi checklist for CLI.12 To be diagnosed with CLI, an individual must score at least 7 out of 13 points. 2) A physical therapist with 9 years of clinical experience in musculoskeletal disorders assessed individual farmers using three tests: aberrant movement, painful catch, and prone instability test. These tests were specifically selected because they signified the spinal stabilizing subsystems based on Panjabi’s model.18
The aberrant movement represents functional motions (bending and return from bending) related to lumbar instability.19 For painful catch test, participants lifted both legs with knee extension and slowly placed their legs back down on the floor. The positive painful catch sign implies poor trunk muscle co-ordination and control which represents active stabilizing and/or neural control stabilizing subsystems deficit.20 Lastly, the positive prone instability test denotes an insufficient control of the passive stabilizing subsystem to manage an induced anterior shear force of the lumbar segment.21
To determine the inter-rater reliability of these tests, an expert examiner with over 20 years of clinical experience in musculoskeletal disorders repeated the tests in the first 20 subjects.
Statistical analysis
All data were presented as means and standard deviations. The passing independence variables (P-value less than 0.2) were included in the initial model of logistic regression. Pearson’s chi-squared test (χ2) was used to test the goodness-of-fit by determining the frequency and percentage for each of the back risk categories with each of the independent categorical variables; and to perform a test of independence measured by association between the variables P-value less than 0.2 was included into the initial model of logistic regression. The backward stepwise elimination procedure was used for data analysis. Significance was set at P-value less than 0.05.
Results
Prevalence of CLI
The demographic characteristics of the 323 rice farmers with LBP (140 males, 183 females) are presented in Table 1. Body mass index (BMI) was normal for an Asian population. Figure 1 demonstrates a percentage of 282 Thai rice farmers without CLI, and 41 Thai rice farmers with CLI, using our criterion. Three-hundred and twenty-three farmers with LBP who got a score of at least 7 out of 13 points, and with at least two out of three positive responses to the tests were detected in 41 farmers (13%). The inter-rater reliability was analyzed between two physical therapists and all tests presented good reliability: aberrant movement sign was κ=0.97, 95% confidence interval (CI) 0.52, 1.00, painful catch sign was κ=0.737, 95% CI 0.49, 1.00, and prone instability test was κ=0.737, 95% CI 0.49, 1.00.
Table 1.
The demographic characteristics of the 323 rice farmers
| Demographic characteristics | Mean | SD | Minimum | Maximum |
|---|---|---|---|---|
| Age (years) | 43.93 | 10.42 | 20 | 60 |
| Weight (kg) | 58.63 | 12.18 | 38 | 92 |
| Height (cm) | 158.48 | 5.79 | 140 | 192 |
| BMI (kg/m2) | 23.04 | 4.88 | 16.41 | 34.96 |
| Waist-hip ratio | 0.88 | 0.06 | 0.71 | 1.03 |
| Farming experience (years) | 24.29 | 12.38 | 1 | 58 |
Abbreviations: BMI, body mass index; SD, standard deviation.
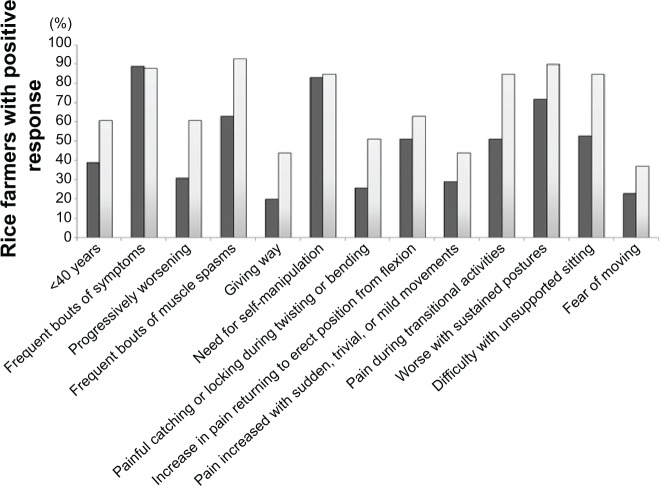
Figure 1.
Percentage of rice farmers with positive response to each question.
Notes: ■ Represents the rice farmers with LBP (n=282); □ represents the rice farmers with LBP who scored at least 7 out of 13 on subjective examination (n=41).
Abbreviation: LBP, low back pain.
The top three answers among the 282 Thai rice farmers found without CLI were: 1) frequent episodes of symptoms (89%); 2) need for self-manipulation (83%); and 3) worsening symptoms after sustained postures (72%), whereas the top three answers among the 41 rice farmers found with CLI were: 1) frequent episodes of muscle spasm (93%); 2) worsening symptoms with sustained postures (90%); and 3) frequent episodes of symptoms (88%). At least two of the positive responses to the objective examination in rice farmers found with CLI were: 19% – painful catch sign, 52% – prone instability test, and 49% – aberrant movement sign.
Risk factors associated with CLI
Table 2 shows the independent variables such as age, BMI, and farming experience (passing P-value less than 0.2) which were included in the initial model of logistic regression. Table 3 shows factors associated with CLI. Univariate and multiple regression analysis showed that the number of years of farming experience was significantly associated with CLI. Those who had labored longer showed an increase in CLI almost twice as high as those who had labored for a shorter period (adjusted odds ratio =2.02, 95% CI adjusted odds ratio =1.03–3.98, P=0.041). However, age and BMI were not associated with CLI. CLI in the younger group (15.98%) was similar to the older group (9.88%), and CLI in the overweight group (15.48%) was not significantly different from the non-overweight group (10.12%).
Table 2.
The independent variables of the rice farmers who had CLI and χ2 before inclusion in initial model
| Independent variables | Mean | SD | Total farmers
|
CLI
|
χ2 | P-value | ||
|---|---|---|---|---|---|---|---|---|
| n | % | n | % | |||||
| Sex | 0.07 | 0.795 | ||||||
| • Male | 140 | 43.34 | 17 | 12.14 | ||||
| • Female | 183 | 56.66 | 24 | 13.11 | ||||
| Age (years) | 44.20 | 9.51 | 2.62 | 0.105* | ||||
| • <45 years | 151 | 46.75 | 24 | 15.89 | ||||
| • ≥45 years | 172 | 53.25 | 17 | 9.88 | ||||
| BMI (kg/m2) | 23.21 | 3.45 | 2.09 | 0.148* | ||||
| • <23 kg/m2 | 168 | 52.01 | 17 | 10.12 | ||||
| • ≥23 kg/m2 | 155 | 49.99 | 24 | 15.48 | ||||
| Waist-hip ratio | 0.88 | 0.06 | 0.53 | 0.466 | ||||
| • M <0.9, F <0.8 | 119 | 36.84 | 13 | 10.92 | ||||
| • M ≥0.9, F ≥0.8 | 204 | 63.16 | 28 | 13.73 | ||||
| Smoking | 1.20 | 0.272 | ||||||
| • No | 221 | 68.42 | 25 | 11.31 | ||||
| • Yes | 102 | 31.58 | 16 | 15.69 | ||||
| Farming experience (years) | 24.29 | 12.38 | 4.72 | 0.030* | ||||
| • <30 years | 177 | 54.80 | 16 | 9.04 | ||||
| • ≥30 years | 146 | 45.20 | 25 | 17.12 | ||||
Note:
P-value <0.2.
Abbreviations: CLI, clinical lumbar instability; M, male; F, female; BMI, body mass index; SD, standard deviation.
Table 3.
Risk factors associated with clinical lumbar instability in rice farmers with chronic non-specific low back pain: univariate and multiple regression analysis (n=41)
| Characteristics | ORcrude
|
ORadj
|
||
|---|---|---|---|---|
| (95% CI) | P-value | (95% CI) | P-value | |
| Sex | ||||
| • M | 1 | |||
| • F | 1.09 (0.57 to 2.10) | 0.795 | ||
| Age (years) | ||||
| • <45 years | 1 | 1 | ||
| • ≥45 years | 0.58 (0.30 to 1.12) | 0.105 | 0.54 (0.27 to 1.06) | 0.073 |
| BMI | ||||
| • <23 kg/m2 | 1 | 1 | ||
| • ≥23 kg/m2 | 1.63 (0.84 to 3.13) | 0.148 | 1.76 (0.89 to 3.47) | 0.105 |
| Waist-hip ratio | ||||
| • M <0.9, F <0.8 | 1 | |||
| • M ≥0.9, F ≥0.8 | 1.30 (0.65 to 2.59) | 0.466 | ||
| Smoking | ||||
| • No | 1 | |||
| • Yes | 1.46 (0.75 to 2.85) | 0.272 | ||
| Farming experience (years) | ||||
| • <30 years | 1 | 1 | ||
| • ≥30 years | 2.08 (1.07 to 4.03) | 0.030 | 2.02 (1.03 to 3.98) | 0.041* |
Note:
P-value <0.05.
Abbreviations: BMI, body mass index; OR, odds ratio; ORadj, adjusted odds ratio; CI, confidence interval; M, male; F, female.
Discussion
This study investigated the prevalence of CLI and the individual risk factors associated with CLI in rice farmers with LBP. The prevalence of and individual risk factors associated with CLI in the general population in Thailand have not been reported yet. The new and important discoveries from this study showed that a prevalence of 13% of CLI among Thai rice farmers, and that farmers with over 30 years of experience are at a greater risk of CLI. It is, therefore, evident that the occurrence of CLI is significantly correlated to their years of experience.
Prevalence of CLI
The prevalence of CLI in chronic non-specific LBP was diagnosed utilizing a combination of subjective and objective examinations. The subjective examination was based on the Delphi checklist for CLI.13 The objective examinations were painful catch sign, prone instability test, and aberrant movement sign. Under subjective examination the prevalence of CLI with at least two out of three positive responses to tests, was 13%. As the current study is the first study to specifically assess CLI in rice farmers, our finding should not be compared to most previous studies, which investigated the prevalence of only nonspecific LBP among the same occupational group.6,8 Our findings are limited in similarity to those of Abbott et al22 who reported that prevalence of CLI in nonspecific LBP (n=138, age 23–60 years) was 12% by using only the objective examination as passive accessory intervertebral movement and passive physiological intervertebral movement. Traditional rice farming is characterized by extensive labor, repetitive flexion-extension, twisting trunk movement, and prolonged sustained stooped posture. These may induce frequent episodes of muscle spasms. Among agricultural workers in general, type of plants, farming methods, and the degree of mechanization affect the work load on the lumbar spine differently and the prevalence of lumbar biomechanical strain varies. When transplanting seedlings by hand to the fields, or harvesting crops, rice farmers flex and rotate their trunks repetitively and at a higher degree in comparison to other sector workers.
The positive responses of three objective tests illustrate an impairment of the active stabilizing subsystem, the passive stabilizing subsystem, and the neural control subsystem.18,23 Throughout the farming process, forward trunk-bending triggers an anterior tilting of the pelvis, causing accumulative stress on the passive stabilizing subsystem surrounding the lumbar spine. Likewise, paraspinal muscles play an important role in such posture. This may lead to imbalance of the active stabilizing subsystem. Aberrant movement sign presents 90% of specificity.19 This test does not isolate a particular spinal stabilizing subsystem. Our results were in good agreement with previous studies.11,19,20,24
Risk factors associated with CLI
Poor lifting technique such as forward-bend posture and asymmetric lifting is associated with LBP. An ongoing morphological change of the spine alters the biomechanical loading from back muscles, ligaments, and joints, and can yield back injuries.25,26 Granata and Marras reported that body mass, task asymmetry, and level of experience affected the magnitude and variability of spinal load during repeated lifting exertions.27 In aging workers, bending and lifting activities generate loads on the spine that exceed the failure load of vertebrae with low bone mineral density25 which is associated with spinal degeneration. The degenerative change does not only affect intervertebral discs, but also ligament and bone.
The present study revealed that the rice farmers with at least 30 years of farming experience had high risk of CLI. The possible reasons are their long-term cumulative loading and repetitive tissue injuries. Thai manual rice farming, which requires extensive labor in all processes and working hours per day, yields abnormal mechanical loading and accumulating repetitive strain to the lumbar spine. CLI is a progress pathogenesis of degenerative processes of the spine and is associated with repeated movement of bending, twisting, and lifting.15 Participants who have LBP without CLI may be in either early phase of spinal degeneration (dysfunction phase) or late phase (stabilizing phase). In this study, we found that CLI was more prevalent among younger subjects compared to older subjects. It is possible that the older group may be in the stabilizing phase.28
Regarding sex, some previous studies demonstrated that females are at greater risk of chronic LBP than males due to their anatomical structure and hormonal effects,29,30 Robinson et al however, showed the opposite result.31 Our study demonstrated that CLI was not associated with sex (Table 3). Previous studies showed that smoking was associated with LBP due to a reduction of oxygen supply to discs.32,33 This study did not find any association between CLI and smoking (Table 3). Future investigation is needed.
Ideally, any rice farmer who has worked for over 30 years should have their spine checked regularly. Better co-contraction of trunk muscles provides an excellent active stabilizing subsystem for the lumbar segment.14 Core stabilization exercise is therefore highly recommended to individuals with CLI to help improve pain intensity and trunk muscle activity.3,5 Proper assessment of muscle function on physical activities prior to exercise training is important for individuals to provide a better exercise prescription at home or at the community center.34,35
Limitation
There are some limitations to this study. Firstly, our study was performed only in Khon Kaen province. Secondly, it is possible that personal working habits of the rice farmers may influence our findings. Therefore, further study is needed to investigate more details of this issue. Lastly, as our study recruited the farmers by convenient sample, based on our informal survey, most rice farmers in this study prefer manual labor to machines. Careful consideration might be taken to apply the results to different landscape areas. Likewise, the prevalence of CLI probably differs among workers in other agricultural crops.
Conclusion
This study showed 13% CLI in LBP, and that CLI is associated with farming experience in the traditional way of rice farming. The diagnostic process of CLI is practical in the community because it is less time consuming and no test equipment is needed. Being able to detect CLI early helps prevent progression of lumbar instability.
Acknowledgments
The authors thank the participants of the study. This study was supported by grants from the Research Center in Back, Neck, Other Joint Pain and Human Performance (BNOJPH), Khon Kaen University, Thailand.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Nachemson A, Morris JM. In vivo measurements of intradiscal pressure. Discometry, a method for the determination of pressure in the lower lumbar discs. J Bone Joint Surg Am. 1964;46:1077–1092. [PubMed] [Google Scholar]
- 2.Marras WS. Occupational low back disorder causation and control. Ergonomics. 2000;43(7):880–902. doi: 10.1080/001401300409080. [DOI] [PubMed] [Google Scholar]
- 3.Areeudomwong P, Puntumetakul R, Jirarattanaphochai K, et al. Core Stabilization Exercise Improves Pain Intensity, Functional Disability and Trunk Muscle Activity of Patients with Clinical Lumbar Instability: a Pilot Randomized Controlled Study. J Phys Ther Sci. 2012;24(10):1007–1012. [Google Scholar]
- 4.Keawduangdee P, Puntumetakul R, Chatchawan U, Kaber D, Siritaratiwat W. Prevalence and associated risk factors of low-back pain in textile fishing net manufacturing. Human Factors and Ergonomics in Manufacturing and Service Industries. 2012;22(6):562–570. [Google Scholar]
- 5.Puntumetakul R, Areeudomwong P, Emasithi A, Yamauchi J. Effect of 10-week core stabilization exercise training and detraining on pain-related outcomes in patients with clinical lumbar instability. Patient Prefer Adherence. 2013;7:1189–1199. doi: 10.2147/PPA.S50436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Puntumetakul R, Siritaratiwat W, Boonprakob Y, Eungpinichpong W, Puntumetakul M. Prevalence of musculoskeletal disorders in farmers: Case study in Sila, Muang Khon Kaen, Khon Kaen province. J Med Tech Phys Ther. 2011;23(3):297–303. [Google Scholar]
- 7.Gupta G, Tarique Prevalence of Musculoskeletal Disorders in Farmers of Kanpur-Rural, India. Journal of Community Medicine and Health Education. 2013;3:249. [Google Scholar]
- 8.Taechasubamorn P, Nopkesorn T, Pannarunothai S. Prevalence of low back pain among rice farmers in a rural community in Thailand. Chotmaihet Thangphaet. 2011;94(5):616–621. [PubMed] [Google Scholar]
- 9.Fritz JM, Erhard RE, Hagen BF. Segmental instability of the lumbar spine. Phys Ther. 1998;78(8):889–896. doi: 10.1093/ptj/78.8.889. [DOI] [PubMed] [Google Scholar]
- 10.Panjabi MM. Clinical spinal instability and low back pain. J Electromyogr Kinesiol. 2003;13(4):371–379. doi: 10.1016/s1050-6411(03)00044-0. [DOI] [PubMed] [Google Scholar]
- 11.Beazell JR, Mullins M, Grindstaff TL. Lumbar instability: an evolving and challenging concept. J Man Manip Ther. 2010;18(1):9–14. doi: 10.1179/106698110X12595770849443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cook C, Brismée JM, Sizer PS., Jr Subjective and objective descriptors of clinical lumbar spine instability: a Delphi study. Man Ther. 2006;11(1):11–21. doi: 10.1016/j.math.2005.01.002. [DOI] [PubMed] [Google Scholar]
- 13.Kumar SP. Efficacy of segmental stabilization exercise for lumbar segmental instability in patients with mechanical low back pain: A randomized placebo controlled crossover study. N Am J Med Sci. 2011;3(10):456–461. doi: 10.4297/najms.2011.3456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Demoulin C, Distrée V, Tomasella M, Crielaard JM, Vanderthommen M. Lumbar functional instability: a critical appraisal of the literature. Ann Réadapt Médecine Phys. 2007;50(8):677–684. 669–676. doi: 10.1016/j.annrmp.2007.05.007. [DOI] [PubMed] [Google Scholar]
- 15.Manchikanti L. Epidemiology of low back pain. Pain Physician. 2000;3(2):167–192. [PubMed] [Google Scholar]
- 16.Barrero LH, Hsu YH, Terwedow H, Perry MJ, Dennerlein JT, Brain JD, Xu X. Prevalence and Physical Determinants of Low Back Pain in a Rural Chinese Population. Spine (Phila Pa 1976) 2006;31(23):2728–2734. doi: 10.1097/01.brs.0000244583.35982.ea. [DOI] [PubMed] [Google Scholar]
- 17.Rosecrance J, Rodgers G, Merlino L. Low back pain and musculoskeletal symptoms among Kansas farmers. Am J Ind Med. 2006;49(7):547–556. doi: 10.1002/ajim.20324. [DOI] [PubMed] [Google Scholar]
- 18.Panjabi MM. The stabilizing system of the spine. Part II. Neutral zone and instability hypothesis. J Spinal Disord. 1992;5(4):390–396. doi: 10.1097/00002517-199212000-00002. discussion 397. [DOI] [PubMed] [Google Scholar]
- 19.Fritz JM, Piva SR, Childs JD. Accuracy of the clinical examination to predict radiographic instability of the lumbar spine. Eur Spine J. 2005;14(8):743–750. doi: 10.1007/s00586-004-0803-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kasai Y, Morishita K, Kawakita E, Kondo T, Uchida A. A new evaluation method for lumbar spinal instability: passive lumbar extension test. Phys Ther. 2006;86(12):1661–1667. doi: 10.2522/ptj.20050281. [DOI] [PubMed] [Google Scholar]
- 21.Ravenna MM, Hoffman SL, Van Dillen LR. Low interrater reliability of examiners performing the prone instability test: a clinical test for lumbar shear instability. Arch Phys Med Rehabil. 2011;92(6):913–919. doi: 10.1016/j.apmr.2010.12.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Abbott JH, McCane B, Herbison P, Moginie G, Chapple C, Hogarty T. Lumbar segmental instability: a criterion-related validity study of manual therapy assessment. BMC Musculoskelet Disord. 2005;6:56. doi: 10.1186/1471-2474-6-56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.O’Sullivan PB. Lumbar segmental “instability”: clinical presentation and specific stabilizing exercise management. Man Ther. 2000;5(1):2–12. doi: 10.1054/math.1999.0213. [DOI] [PubMed] [Google Scholar]
- 24.Hicks GE, Fritz JM, Delitto A, Mishock J. Interrater reliability of clinical examination measures for identification of lumbar segmental instability. Arch Phys Med Rehabil. 2003;84(12):1858–1864. doi: 10.1016/s0003-9993(03)00365-4. [DOI] [PubMed] [Google Scholar]
- 25.Pope MH, Goh KL, Magnusson ML. Spine ergonomics. Annu Rev Biomed Eng. 2002;4:49–68. doi: 10.1146/annurev.bioeng.4.092101.122107. [DOI] [PubMed] [Google Scholar]
- 26.Vieira ER, Kumar S. Working postures: a literature review. J Occup Rehabil. 2004;14(2):143–159. doi: 10.1023/b:joor.0000018330.46029.05. [DOI] [PubMed] [Google Scholar]
- 27.Granata KP, Marras WS. Cost-benefit of muscle cocontraction in protecting against spinal instability. Spine (Phila Pa 1976) 2000;25(11):1398–1404. doi: 10.1097/00007632-200006010-00012. [DOI] [PubMed] [Google Scholar]
- 28.Kirkaldy-Willis WH, Wedge JH, Yong-Hing K, Reilly J. Pathology and pathogenesis of lumbar spondylosis and stenosis. Spine (Phila Pa 1976) 1978;3(4):319–328. doi: 10.1097/00007632-197812000-00004. [DOI] [PubMed] [Google Scholar]
- 29.Fillingim RB, Maixner W. Gender differences in the responses to noxious stimuli. Pain Forum. 1995;4(4):209–221. [Google Scholar]
- 30.Malmqvist S, Kjaermann I, Andersen K, Økland I, Brønnick K, Larsen JP. Prevalence of Low Back and Pelvic Pain During Pregnancy in a Norwegian Population. J Manipulative Physiol Ther. 2012;35(4):272–278. doi: 10.1016/j.jmpt.2012.04.004. [DOI] [PubMed] [Google Scholar]
- 31.Robinson ME, Dannecker EA, George SZ, Otis J, Atchison JW, Fillingim RB. Sex Differences in the Associations Among Psychological Factors and Pain Report: A Novel Psychophysical Study of Patients With Chronic Low Back Pain. J Pain. 2005;6(7):463–470. doi: 10.1016/j.jpain.2005.02.007. [DOI] [PubMed] [Google Scholar]
- 32.Shiri R, Karppinen J, Leino-Arjas P, Solovieva S, Viikari-Juntura E. The Association between Smoking and Low Back Pain: A Meta-analysis. Am J Med. 2010;123(1):87.e7–87.e35. doi: 10.1016/j.amjmed.2009.05.028. [DOI] [PubMed] [Google Scholar]
- 33.Zvolensky MJ, McMillan KA, Gonzalez A, Asmundson GJ. Chronic musculoskeletal pain and cigarette smoking among a representative sample of Canadian adolescents and adults. Addict Behav. 2010;35(11):1008–1012. doi: 10.1016/j.addbeh.2010.06.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Peungsuwan P, Sermcheep P, Harnmontree P, et al. The Effectiveness of Thai Exercise with Traditional Massage on the Pain, Walking Ability and QOL of Older People with Knee Osteoarthritis: A Randomized Controlled Trial in the Community. J Phys Ther Sci. 2014;26(1):139–144. doi: 10.1589/jpts.26.139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Yamauchi J, Nakayama S, Ishii N. Effects of bodyweight-based exercise training on muscle functions of leg multi-joint movement in elderly individuals. Geriatr Gerontol Int. 2009;9(3):262–269. doi: 10.1111/j.1447-0594.2009.00530.x. [DOI] [PubMed] [Google Scholar]