Abstract
Lipoteichoic acid from Staphylococcus aureus was a potent inducer of procoagulant activity in isolated mononuclear cells but not in whole blood. In contrast, staphylococcal peptidoglycan showed equal levels of potency in isolated mononuclear cells and whole blood, suggesting that peptidoglycan is an important inducer of procoagulant activity in severe sepsis involving gram-positive bacteria.
Staphylococcus aureus is the most common bacterium in sepsis and endocarditis involving gram-positive bacteria (5, 11). It can activate blood coagulation, leading to disseminated intravascular coagulation during sepsis, and it causes formation of endocardial vegetations during endocarditis (2, 9, 10). Tissue factor (TF), a single-chain protein, is the main physiological initiator of blood coagulation (22). In blood circulation, only monocytes and endothelial cells can be stimulated to express TF. Lipopolysaccharide (LPS), a cell wall component of gram-negative bacteria, is a potent inducer of TF in both monocytes and endothelial cells (15). Gram-positive bacteria have two main cell wall components, peptidoglycan (PG) and lipoteichoic acid (LTA), and both can induce expression of proinflammatory cytokines (8, 12, 16, 24). Recently, it was shown that staphylococcal PG, but not commercially obtained LTA, induces TF expression in monocytes (13). Lately, a novel method for the isolation of LTA has been developed in which the d-alanine substitutions of the polyglycerophosphate backbone are preserved (17). Since the purification procedure is crucial for retaining the biological activity of LTA (17), the question was raised of whether LTA isolated by the novel method behaves differently from commercial LTA (cLTA) in the induction of procoagulant activity (PCA) and TF expression.
Peripheral blood mononuclear cells (PBMC) isolated over Ficoll-Paque (Pharmacia Biotech, Uppsala, Sweden) as described previously (12) were diluted in RPMI 1640 (Gibco, Life Technologies, Paisley, Scotland). The cells (final concentration, 2 × 106 cells/ml) were stimulated with cLTA (Sigma, St. Louis, Mo.), LTA (18), or PG (12), all derived from S. aureus. In brief, the isolation procedure for highly purified LTA was as follows. A defrosted aliquot of bacteria was mixed with an equal volume of n-butanol (Merck, Darmstadt, Germany), and the mixture was stirred for 30 min at room temperature. After centrifugation (13,000 × g) for 20 min, the aqueous phase was lyophilized, resuspended with chromatography start buffer (15% n-propanol in 0.1 M ammonium acetate, pH 4.7), and centrifuged (45,000 × g) for 15 min. The supernatant was subjected to hydrophobic interaction chromatography on octyl-Sepharose. The purity of LTA was >99% according to results of nuclear magnetic resonance and mass spectrometry analysis. Incubations were performed on a rotator at 37°C for 4 h. LPS from Escherichia coli O111:B4 (Sigma) served as a positive control. Subsequently, 100 μl of the cell incubation mixture was mixed with 200 μl of human plasma (obtained from healthy volunteers) that 1 min earlier had been recalcified with 30 mM CaCl2 at a ratio of 1:1. Clotting time was determined in duplicate by using a coagulometer (Amelung, Lemgo, Germany).
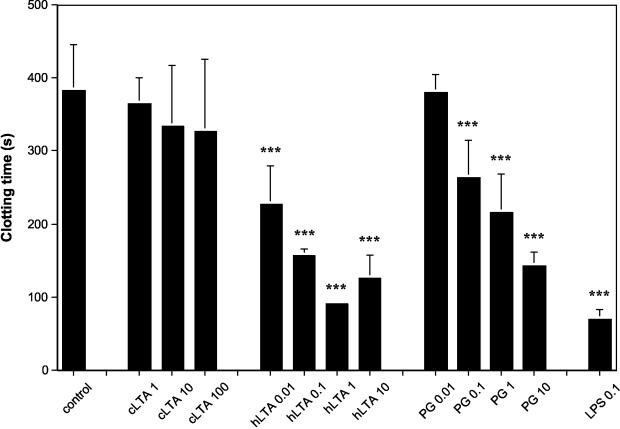
LTA, but not cLTA, induced PCA in PBMC in a concentration-dependent fashion (Fig. 1). LTA was about 10-fold more potent than PG on a weight basis in inducing significant PCA. However, LPS was an even stronger inducer of PCA than LTA. Analysis of time kinetics revealed that LTA induced PCA in a pattern similar to that previously shown for LPS and PG (13). Thus, stimulation by LTA resulted in a rapid process with increased PCA after 1 h, and a maximum PCA was reached after 4 h (data not shown).
FIG. 1.
Highly purified LTA from S. aureus induces PCA in PBMC. PBMC were incubated in medium alone or stimulated with various concentrations (given in micrograms per milliliter) of cLTA, highly purified LTA (hLTA), PG, or LPS for 4 h. Clotting time was determined for recalcified human plasma incubated with the cells. Values are means ± standard deviations (n = 3). Statistical analysis was performed by means of an analysis of variance (ANOVA). The overall P value was <0.0001. In addition, P values for differences between the mean for each stimulus and the mean for the control were calculated using the standard deviation from the ANOVA model and compared to the time distribution. No adjustments for multiple tests have been used. The level of statistical significance was set at P of <0.005 (***).
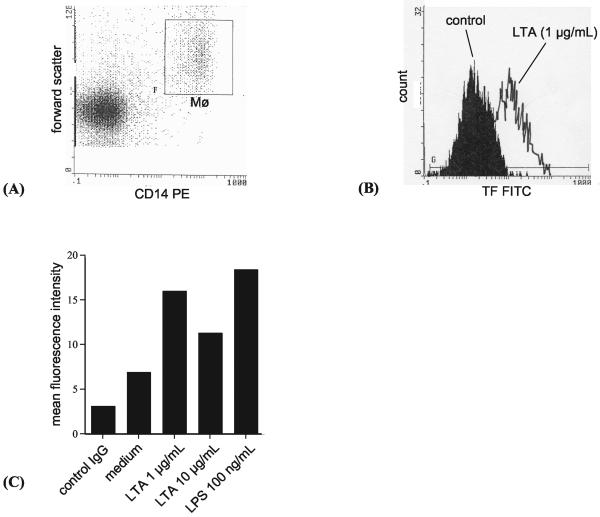
TF activity and TF antigen expression do not always correlate because encryption of the TF molecule and changes in the properties of the cell membrane can induce PCA (21). To investigate whether TF was responsible for the PCA induced by LTA, goat anti-human TF immunoglobulin G (IgG; 55 μg/ml; gift from Marianne Kjalke, Novo Nordisk, Copenhagen, Denmark) or control IgG (goat IgG against β2-microglobulin raised in our own laboratory) was added to PBMC after 4 h of incubation with LTA and incubated for another 30 min. Subsequently, clotting time was determined. IgG directed against TF effectively inhibited the increased PCA of LTA-stimulated cells, showing that the increased PCA was dependent on TF activity (Table 1). Further, TF expression on the cell surface was detected by flow cytometry by using fluorescein isothiocyanate (FITC)-conjugated monoclonal antibodies against TF (American Diagnostica, Greenwich, Conn). Monocytes stimulated with LTA revealed an increase in mean fluorescence compared with controls incubated in medium alone, demonstrating upregulation of TF on the cell surface (Fig. 2). At LTA concentrations of ≥10 μg/ml, upregulation of TF on the cell surface and PCA showed a tendency to decrease compared to those at concentrations of 1 μg/ml (Fig. 1 and 2). This paradox with regard to dose response effects from LTA has been shown by others and may be explained by micelle formation that renders LTA less active at higher concentrations (3, 6).
TABLE 1.
LTA-induced PCA in human PBMC in the presence or absence of anti-TF IgG or IL-1 Ra
| Stimulus | Clotting time (s)a |
|---|---|
| Medium alone | 384 ± 55 |
| Medium + anti-TF IgG | 361 ± 110 |
| Medium + control IgG | 323 ± 63 |
| Medium + IL-1 Ra | 395 ± 55 |
| IL-1β (500 pg/ml) | 206 ± 18 |
| IL-1β and IL-1 Ra | 400 ± 35*** |
| LTA (1 μg/ml) | 127 ± 28 |
| LTA + anti-TF IgG | 382 ± 54*** |
| LTA + control IgG | 118 ± 43 |
| LTA (0.1 μg/ml) | 212 ± 57 |
| LTA + IL-1 Ra | 204 ± 53 |
Clotting time was determined with a coagulometer. Values represent results from three independent experiments (means ± standard deviations). Statistical analysis was performed by means of ANOVA. No significant differences in clotting times were found in comparisons of the mean for medium alone and the means for controls containing antibodies or IL-1 Ra (overall P value, 0.73). IL-1β in the presence of IL-1 Ra induced a significant increase in clotting time compared with IL-1β alone. LTA (1 μg/ml) in the presence of anti-TF IgG significantly prolonged clotting time compared with LTA alone (overall P value, 0.0046). LTA (0.1 μg/ml) in the presence of IL-1 Ra induced no significant change in clotting time compared with LTA alone (P = 0.053). The level of statistical significance as indicated in the table was set at P of <0.005 (***).
FIG. 2.
LTA induces expression of TF on the surfaces of monocytes as detected by flow cytometry. (A) Monocytes (Mφ) were gated using their characteristics in forward scatter and expression of CD14. PE, phycoerythrin. (B) Histogram showing mean fluorescence intensities of monocytes after labeling with FITC-conjugated antibody against TF. Cells incubated in the presence of highly purified LTA (1 μg/ml) showed increased expression of TF, demonstrated by a shift to the right, compared with cells incubated in medium alone. (C) Comparison of levels of TF expression on the surfaces of monocytes after incubation in medium alone and labeling with FITC-conjugated control IgG or after incubation in medium alone, in the presence of highly purified LTA at the indicated concentrations, or in the presence of LPS for 4 h and labeling with FITC-conjugated TF IgG. The results from one representative of four experiments are shown.
The inflammatory response and coagulation are linked during host defense (1, 7, 19). LTA induces interleukin-1β (IL-1β) expression in monocytes (8), and it was recently observed that superantigens from S. aureus can induce PCA in PBMC via endogenously produced IL-1β (14). Therefore, LTA was incubated with PBMC in the presence or absence of recombinant IL-1 receptor antagonist (IL-1 Ra; 100 ng/ml; R&D, Abingdon, England), a naturally occurring antagonist of IL-1. IL-1 Ra effectively inhibited the PCA induced by recombinant IL-1β (500 pg/ml; R&D) while no effect of IL-1 Ra was observed in LTA-stimulated cells (Table 1). Therefore, it is unlikely that LTA induces PCA via release of endogenously produced IL-1β. Other cytokines of possible importance, for example, tumor necrosis factor alpha (TNF-α), could theoretically be produced during stimulation of cells. However, IL-1β is considered to be the key cytokine in the activation of TF expression (4, 20).
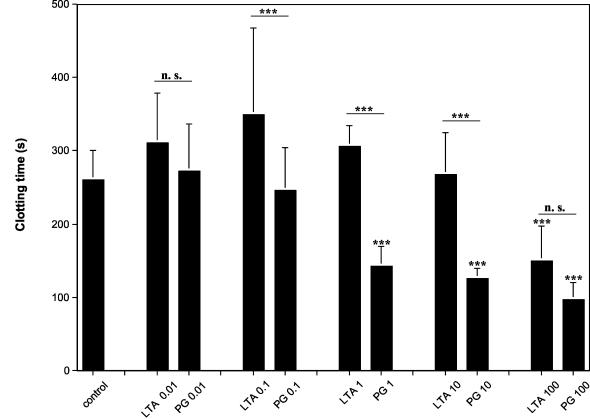
To study a more in vivo-like situation, LTA or PG was incubated in undiluted or diluted (40% blood in RPMI 1640) blood at 37°C for 4 h. Subsequently, 300 μl of blood was recalcified with 40 μl of CaCl2 (100 mM) and clotting time was determined. LTA was a weak inducer of PCA in whole blood compared with LTA incubated with PBMC. The threshold dose of LTA required to induce PCA was around 100 μg/ml, compared with 0.01 μg/ml in PBMC incubations (Fig. 1 and 3). Therefore, it seems likely that a neutralizing factor is present in whole blood, making LTA less active. Ellingsen et al. showed that LTA is a poor inducer of TNF-α release in whole blood but that diluting the blood lowers the threshold dose of LTA needed to induce TNF-α (8). This finding suggests the presence of such a factor. However, neither dilution of the blood (40% blood in RPMI 1640) nor prolonged incubation time changed the LTA-induced PCA in our hands. In a study of LTA-induced TNF-α release from monocytes, it was recently demonstrated that chylomicron-associated LPS-binding protein mediates the detoxification of LTA (23). This mechanism may represent such a neutralizing factor. The focus for coming studies will be to determine whether the neutralizing factor is also present in a local extravascular infection in which LTA could play a proinflammatory role by inducing TF in monocytes (7). An interesting finding in the present study is that our observations of PG-induced PCA in whole blood are identical to earlier observations of PG-induced PCA in PBMC, showing that PG is not affected by neutralizing factors in whole blood (13). This suggests that PG is a more important virulence factor than LTA with regard to TF induction in monocytes, at least during systemic S. aureus infection.
FIG. 3.
PG is a stronger inducer of PCA in whole blood than LTA. Undiluted human whole blood was incubated with LTA or PG at the indicated concentrations (given in micrograms per milliliter) for 4 h. Subsequently, the blood was recalcified and the clotting time was determined. Values are means ± standard deviations (n = 3). Statistical analysis was performed by means of ANOVA. The overall P value was <0.0001, and P values for differences between the mean for each stimulus and the mean for the control were calculated using the standard deviation from the ANOVA model and compared to the time distribution. No adjustments for multiple tests have been used. In addition, means with the same concentrations of LTA and PG on a weight basis were compared (indicated by a line). The level of statistical significance was set at P of <0.005 (***). n.s., not significant.
Editor: A. D. O'Brien
REFERENCES
- 1.Bernard, G., J. L. Vincent, P. F. Laterre, S. LaRosa, J. F. Dhainaut, A. Lopez-Rodriguez, J. Steingrub, G. Garber, J. Helterbrand, J. W. Ely, and C. Fischer. 2001. Efficacy and safety of recombinant human activated protein C for severe disease. N. Engl. J. Med. 344:699-709. [DOI] [PubMed] [Google Scholar]
- 2.Bick, R., and L. A. Kunkel. 1992. Disseminated intravascular coagulation syndromes. Int. J. Hematol. 55:1-26. [PubMed] [Google Scholar]
- 3.Blease, K., Y. Chen, P. G. Hellewell, and A. Burke-Gaffney. 1999. Lipoteichoic acid inhibits lipopolysaccharide-induced adhesion molecule expression and IL-8 release in human lung microvascular endothelial cells. J. Immunol. 163:6139-6147. [PubMed] [Google Scholar]
- 4.Boermeester, M. A., P. A. M. van Leeuwen, S. M. Coyle, G. Wolbink, E. Hack, and S. Lowry. 1995. Interleukin-1 receptor blockade in patients with sepsis syndrome: evidence that interleukin-1 contributes to the release of interleukin-6, elastase and phospholipase A2, and to the activation of the complement, coagulation, and fibrinolytic systems. Arch. Surg. 130:739-748. [DOI] [PubMed] [Google Scholar]
- 5.Cohen, J., and E. Abraham. 1999. Microbiological findings and correlation with serum tumor necrosis factor-α in patients with severe sepsis and septic shock. J. Infect. Dis. 180:116-121. [DOI] [PubMed] [Google Scholar]
- 6.Courtney, H. S., W. A. Simpson, and E. H. Beachey. 1986. Relationship of critical micelle concentrations of bacterial lipoteichoic acids to biological activities. Infect. Immun. 51:414-418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cunningham, M. A., P. Romas, P. Hutchinson, S. R. Holdsworth, and P. G. Tipping. 1999. Tissue factor and factor VIIa receptor/ligand interactions induce proinflammatory effects in macrophages. Blood 94:3413-3420. [PubMed] [Google Scholar]
- 8.Ellingsen, E., S. Morath, T. Flo, A. Schromm, T. Hartung, C. Thiemermann, T. Espevik, D. Golenbock, S. Foster, R. Solberg, A. Aasen, and J. Wang. 2002. Induction of cytokine production in human T cells and monocytes by highly purified lipoteichoic acid: involvement of Toll-like receptors and CD14. Med. Sci. Monit. 8:BR149-BR156. [PubMed] [Google Scholar]
- 9.Gando, S., S. Nanzaki, S. Sasaki, and O. Kemmotsu. 1998. Significant correlations between tissue factor and thrombin markers in trauma and septic patients with disseminated intravascular coagulation. Thromb. Haemostasis 79:1111-1115. [PubMed] [Google Scholar]
- 10.Hardaway, R., and C. H. Williams. 1996. Disseminated intravascular coagulation: an update. Compr. Ther. 22:737-743. [PubMed] [Google Scholar]
- 11.Lowy, F. D. 1998. Staphylococcus aureus infections. N. Engl. J. Med. 339:520-532. [DOI] [PubMed] [Google Scholar]
- 12.Mattsson, E., L. Verhage, J. Rollof, A. Fleer, J. Verhoef, and H. van Dijk. 1993. Peptidoglycan and teichoic acid from Staphylococcus epidermidis stimulate human monocytes to release tumour necrosis factor-alpha, interleukin-1 beta and interleukin-6. FEMS Immunol. Med. Microbiol. 7:281-287. [DOI] [PubMed] [Google Scholar]
- 13.Mattsson, E., H. Herwald, L. Björck, and A. Egesten. 2002. Peptidoglycan from Staphylococcus aureus induces tissue factor expression and procoagulant activity in human monocytes. Infect. Immun. 70:3033-3039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mattsson, E., H. Herwald, and A. Egesten. 2003. Superantigens from Staphylococcus aureus induce procoagulant activity and monocyte tissue factor expression in whole blood and mononuclear cells via interleukin-1β. J. Thromb. Haemostasis 1:2569-2576. [DOI] [PubMed] [Google Scholar]
- 15.Meszaros, K., S. Aberle, R. Dedrick, R. Machovich, A. Horwitz, C. Birr, G. Theofan, and J. Parent. 1994. Monocyte tissue factor induction by lipopolysaccharide (LPS): dependence on LPS-binding protein and CD14, and inhibition by a recombinant fragment of bactericidal/permeability-increasing protein. Blood 83:2516-2525. [PubMed] [Google Scholar]
- 16.Middelveld, R. J., and K. Alving. 2000. Synergistic septicemic action of the Gram-positive bacterial cell wall components peptidoglycan and lipoteichoic acid in the pig in vivo. Shock 13:297-306. [DOI] [PubMed] [Google Scholar]
- 17.Morath, S., A. Geyer, and T. Hartung. 2001. Structure-function relationship of cytokine induction by lipoteichoic acid from Staphylococcus aureus. J. Exp. Med. 193:393-397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Morath, S., A. Geyer, I. Spreitzer, C. Hermann, and T. Hartung. 2002. Structural decomposition and heterogeneity of commercial lipoteichoic acid preparations. Infect. Immun. 70:938-944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Opal, S. M., J. Palardy, N. Parejo, and A. Ceasey. 2001. The activity of tissue factor pathway inhibitor in experimental models of superantigen-induced shock and polymicrobial intra-abdominal sepsis. Crit. Care Med. 29:13-17. [DOI] [PubMed] [Google Scholar]
- 20.Van der Poll, T., M. Levi, S. J. H. van Deventer, H. Ten Cate, B. L. Haagmans, B. Biemond, H. Buller, E. Hack, and J. Ten Cate. 1994. Differential effects of anti-tumor necrosis factor monoclonal antibodies on systemic inflammatory responses in experimental endotoxemia in chimpanzees. Blood 83:446-451. [PubMed] [Google Scholar]
- 21.Rao, L. V. M., and U. R. Pendurthi. 1998. Tissue factor on cells. Blood Coagul. Fibrinolysis 9:S27-S35. [PubMed] [Google Scholar]
- 22.Rapaport, S. I., and L. V. M. Rao. 1995. The tissue factor pathway: how it has become a “prima ballerina.” Thromb. Haemostasis 74:7-17. [PubMed] [Google Scholar]
- 23.Vreugdenhil, A., C. H. Rousseau, T. Hartung, J. W. Greve, C. Van't Veer, and W. A. Buurman. 2003. Lipopolysaccharide (LPS)-binding protein mediates LPS detoxification by chylomicrons. J. Immunol. 170:1399-1405. [DOI] [PubMed] [Google Scholar]
- 24.Wang, J. E., P. Jörgensen, M. Almlöf, C. Thiemermann, S. J. Foster, O. Aasen, and R. Solberg. 2000. Peptidoglycan and lipoteichoic acid from Staphylococcus aureus induce tumor necrosis factor alpha, interleukin-6 (IL-6), and IL-10 production in both T cells and monocytes in a human whole blood model. Infect. Immun. 68:3965-3970. [DOI] [PMC free article] [PubMed] [Google Scholar]