Asthma is a chronic respiratory disease affecting nearly 9.6% of United States children.1 Asthma disproportionately burdens children from poor and minority backgrounds.2 Children with asthma have high rates of school absenteeism.3 With children spending nearly half of their day at school, appropriate school asthma management can help optimize care for students with asthma.
Successful school asthma management involves individual case identification and provision of medications to students when needed.4 New York City (NYC) schools require caregiver submission of a Medication Administration Form (MAF; a physician-completed order form that must be renewed every school year) to confirm asthma diagnoses and allow school nurses to administer medication for asthma exacerbations.5 Without an MAF, due to systems-based regulations, the nurse cannot administer medication, even if a student is having an asthma attack.
Many NYC schools struggle with individual asthma case identification6 and have difficulty obtaining MAFs for students, making acute asthma management challenging. Therefore, the objectives of this study were to 1) compare asthma prevalence in four NYC schools based on caregiver and school report; and 2) identify asthma morbidity factors associated with MAF submission.
We conducted a cross-sectional survey of caregivers of children attending 2nd-4th grades in four Bronx, New York (NY) elementary schools as the first step in preparation for a school-based intervention study. The NYC Department of Education and the university's Institutional Review Board (IRB) approved this study. We developed a 6-item self-administered English-Spanish asthma survey based on prior surveys7,8 and NYC DOE guidelines for MAF.5 The survey was field-tested with 10 caregivers of children with and without asthma at routine office visits to ensure questions were clear and easy to comprehend. The survey is available in an online supplement. Surveys and return envelopes were sent home with students during the fall of 2012. Caregivers were instructed to return completed surveys to the classroom teachers in the sealed envelopes. We then collected envelopes from the teachers. Children received a small gift (e.g. stickers, tattoos) for reminding caregivers to return the surveys. Schools were asked to report the number of students with asthma in the same grades. Schools use several Board of Education forms, such as health examination forms and MAFs sent to all students, to identify asthma cases.
We performed descriptive statistics for all variables. Differences in proportions were tested by Chi-square. A two-sided α<0.05 was considered statistically significant. We used SPSS V20.0 software (Statistical Product and Service Solutions 20.0, SPSS Inc., Chicago, IL).
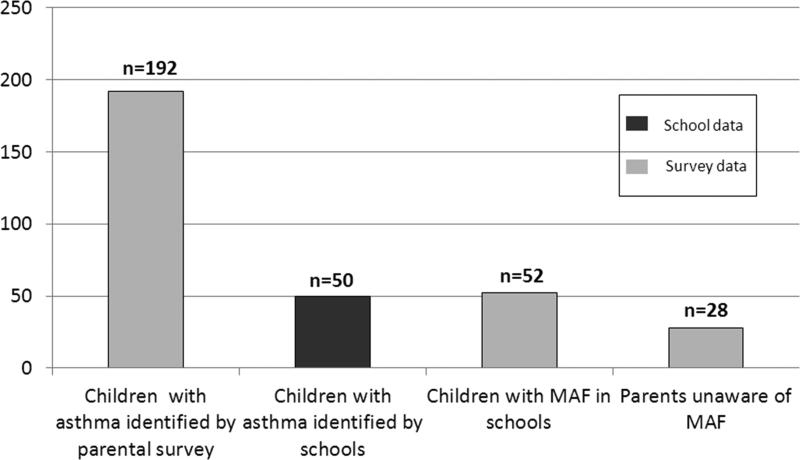
The survey was distributed to 1,270 students and 769 (61%) were returned. Overall, 192 (25%) children had physician-diagnosed asthma. Of these, 150 (80%) were prescribed asthma medication and 106 (55%) had ≥1 urgent asthma visits in the past year. Half (51%) of caregivers reported that their child had symptoms with exercise and 18 (9%) listed asthma as a condition limiting their child's sports participation. Only 52 (27%) had an MAF at school, and 28 (15%) of caregivers were unaware the MAF existed. (Figure 1) Children were more likely to have an MAF on file at school if they were prescribed asthma medication (32.6% vs 10.5%, p=.007) or had ≥1 urgent asthma visit in the past 12 months (38.7% vs 14.1%, p<.001). Schools identified only 50 students with asthma in the same grades using their usual screening methods.
Figure 1.
Survey Results on Asthma Identification and Medication Administration Forms in NYC schools.
These results show a high prevalence of asthma in this population of inner-city elementary school-age children. According to caregiver report, 1/4 of children had physician-diagnosed asthma. This is consistent with an earlier study that reported a 20% asthma prevalence in several Bronx elementary schools.9 Similarly, the 2009 Child Community Health Survey reported a 16.7% (95% CI (14.4 - 19.4)) asthma prevalence in Bronx children 6-12 years of age.10
Our survey identified many more cases of asthma compared to the prevalence reported by schools. This suggests that methods used by schools to identify children substantially underestimate asthma cases. Further, while children with a medication prescription and those with more urgent visits in the past year were more likely to have an MAF submitted, overall less than 1/3 of caregivers submitted MAF and, even among those with urgent visits, MAFs were frequently unavailable. This makes prompt and appropriate school management of acute asthma challenging and may contribute to avoidable visits to the physician's office or emergency department. Future research should focus on the reasons for low MAF submission by caregivers and the impact system-based regulations may have on students’ school asthma management.
Our study had some limitations. The study was conducted in NYC elementary schools. Thus, the conclusions may not be generalizable to other schools in different communities. Our response rate, while comparable to other urban school-based asthma prevalence studies,4 was only 61%. While subject self-selection might have biased estimates of asthma prevalence, an earlier school-based study in the Bronx found similar prevalence rates.9 Differences in the definition of asthma used, methods to identify cases and timing of data collection may have accounted for some discrepancy between asthma cases identified by our survey and those identified by schools. Further, due to privacy rules, we were unable to link individual survey and school data; thus, we do not know if students identified by the school were the same students whose caregivers reported having MAF on file at the school. However these limitations are unlikely to account for the large discrepancy in asthma prevalence found.
In conclusion, our study is the first to compare asthma prevalence as reported by caregiver with school report, and to assess factors associated with MAF submission in NYC public schools. We found that a short, take-home, self-administered caregiver survey identified 74% more cases of asthma than schools, and that MAFs are markedly lacking. Instituting a streamlined method of school asthma case identification and communicating to caregivers the importance of MAF may improve school asthma management. Further, this process may serve as the first step toward establishing interventions to improve outcomes of inner-city children with asthma.
ACKNOWLEDGMENTS
This study was presented in part at the 2014 Pediatric Academic Societies Meeting on May 4, 2014. The authors thank research assistants Florinda Islamovic, Yudilyn Jaramillo and Maria Ivanna Avalos for help with data collection. The authors thank the study participants, the school administrators and teachers who took part in the study.
Financial Support: This study was supported by 5K23HD065742 (Reznik: PI) from the National Institutes of Health (NIH) Eunice Kennedy Shriver National Institute of Child Health & Human Development and Department of Pediatrics, the Stony-Wold Herbert Foundation, Monaghan Medical Corporation, and Department of Pediatrics/Children's Hospital at Montefiore. We would like to acknowledge the support of the Bronx CREED funded by the National Institutes of Health National Center for Minority Health & Health Disparities, Grant No P60 MD000514 for Spanish translation services of informed consent materials.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Clinical Trial Registration: clinicaltrials.gov Identifier: NCT01873755
Contributor Information
Marina Reznik, Pediatrics, Albert Einstein College of Medicine, Children's Hospital at Montefiore, Bronx, NY, United States.
Laurie J. Bauman, Pediatrics, Albert Einstein College of Medicine, Children's Hospital at Montefiore, Bronx, NY, United States.
Sande Okelo, Division of Pediatric Pulmonology, Department of Pediatrics, David Geffen School of Medicine at UCLA, Mattel Children's Hospital UCLA, United States.
Jill S. Halterman, Pediatrics, University of Rochester School of Medicine and Dentistry, Rochester, NY, United States..
REFERENCES
- 1.Akinbami LJ, Moorman JE, Liu X. Asthma prevalence, health care use, and mortality: United States, 2005-2009. National health statistics reports. 2011:1–14. [PubMed] [Google Scholar]
- 2.Smith LA, Hatcher-Ross JL, Wertheimer R, Kahn RS. Rethinking race/ethnicity, income, and childhood asthma: racial/ethnic disparities concentrated among the very poor. Public Health Rep. 2005;120:109–16. doi: 10.1177/003335490512000203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Moonie SA, Sterling DA, Figgs L, Castro M. Asthma status and severity affects missed school days. J Sch Health. 2006;76:18–24. doi: 10.1111/j.1746-1561.2006.00062.x. [DOI] [PubMed] [Google Scholar]
- 4.Vargas PA, Magee JS, Bushmiaer M, et al. School-based asthma case finding: the Arkansas experience. J Sch Health. 2006;76:223–6. doi: 10.1111/j.1746-1561.2006.00101.x. [DOI] [PubMed] [Google Scholar]
- 5.Barbot O, Platt R, Marchese C. Using preprinted rescue medication order forms and health information technology to monitor and improve the quality of care for students with asthma in New York City public schools. J Sch Health. 2006;76:329–32. doi: 10.1111/j.1746-1561.2006.00122.x. [DOI] [PubMed] [Google Scholar]
- 6.Snow RE, Larkin M, Kimball S, Iheagwara K, Ozuah PO. Evaluation of asthma management policies in New York City public schools. J Asthma. 2005;42:51–3. doi: 10.1081/jas-200044776. [DOI] [PubMed] [Google Scholar]
- 7.Jones CA, Morphew T, Clement LT, et al. A school-based case identification process for identifying inner city children with asthma: the Breathmobile program. Chest. 2004;125:924–34. doi: 10.1378/chest.125.3.924. [DOI] [PubMed] [Google Scholar]
- 8.Bonner S, Matte T, Rubin M, et al. Validating an asthma case detection instrument in a Head Start sample. J Sch Health. 2006;76:471–8. doi: 10.1111/j.1746-1561.2006.00144.x. [DOI] [PubMed] [Google Scholar]
- 9.Webber MP, Hoxie AM, Odlum M, Oruwariye T, Lo Y, Appel D. Impact of asthma intervention in two elementary school-based health centers in the Bronx, New York City. Pediatr Pulmonol. 2005;40:487–93. doi: 10.1002/ppul.20307. [DOI] [PubMed] [Google Scholar]
- 10.The New York City Department of Health and Mental Hygiene [June 25, 2014];Child Community Health Survey. 2009 Available at https://a816-healthpsi.nyc.gov/SASStoredProcess/guest?_PROGRAM=%2FEpiQuery%2Fchild%2Fchildindex.