Abstract
Background
There are substantial disparities in breast and cervical cancer screening that stem from lack of health insurance. Although the Affordable Care Act (ACA) expands insurance coverage to many Americans, there are differences in availability of Medicaid coverage across states.
Purpose
To understand the potential impact of Medicaid expansions on disparities in preventive care for low-income women by assessing pre-ACA breast and cervical cancer screening across states currently expanding and not expanding Medicaid to low-income adults.
Methods
Data from the 2012 Behavioral Risk Factor Surveillance System (analyzed in 2014) were used to consider differences in demographics among women for whom screening is recommended, including income and race/ethnicity, across expansion and non-expansion states. Self-reported screening was compared by state expansion status overall, for the uninsured, and for low-income women. Logistic regressions were estimated to assess differences in self-reported screening across expansion and non-expansion states controlling for demographics.
Results
Women in states that are not expanding Medicaid had significantly lower odds of receiving recommended mammograms (OR=0.87, 95% CI=0.79, 0.95) or Pap tests (OR=0.87, 95% CI=0.79, 0.95). The difference was larger among the uninsured (OR=0.72, 95% CI=0.56, 0.91 for mammography; OR=0.78, 95% CI=0.65, 0.94 for Pap tests).
Conclusions
As women in non-expansion states remain uninsured while others gain coverage, existing disparities in cancer screening by race and socioeconomic status are likely to widen. Health risks and associated costs to underserved populations must be taken into account in ongoing debates over expansion.
Introduction
Evidence suggests that women with health insurance are more than twice as likely to receive breast and cervical cancer screening1–7 and are likely to be diagnosed at earlier stages.8 Treatment of early-stage disease detected through population-wide screening can reduce morbidity and mortality.9,10 Although mortality rates have fallen over recent decades, these benefits are not distributed equally across the population.11 There are substantial disparities in breast and cervical cancer diagnosis and outcomes in the U.S. by race/ethnicity, SES, and insurance.1,12,13 The Affordable Care Act (ACA) aims to increase health insurance coverage through various pathways. In particular, in approximately half of states, non-elderly adults with incomes below 138% of the federal poverty level (FPL) are now eligible for Medicaid regardless of family structure or disability status. Nonetheless, almost half of states have not chosen to expand Medicaid.
This paper considers variation in self-reported screening across states currently expanding Medicaid and those not expanding to draw implications for the effects of coverage changes on disparities and to understand where additional effort may be needed to increase screening among underserved populations. An understanding of the role of Medicaid expansions in addressing or perpetuating differences in health care across groups is needed to narrow existing disparities.
Methods
The 2012 Behavioral Risk Factor Surveillance System (BRFSS) provided data on self-reported screening and individual demographics.14 Information on state Medicaid expansion decisions as of February 2014 came from the Centers for Medicare and Medicaid Services.15 Based on U.S. Preventive Services Task Force guidelines,16,17 receipt of mammograms among women with non-missing data aged 52–64 years and Pap tests among women aged 24–64 years who have not undergone a hysterectomy were examined. Outcomes of interest were guideline-consistent screening, specifically mammogram or Pap test within the past 2 or 3 years, respectively.
The independent variable of interest was an indicator of residence in a non-Medicaid expansion state. Models controlled for age, race/ethnicity, income, employment, marital status, education, and insurance status. The BRFSS asks whether individuals have insurance but not type of coverage. Therefore, the insurance variable is an indicator of any coverage. Income as a percentage of FPL was constructed by assigning individuals the median household income in the reported category and applying Census Bureau poverty guidelines by household size. For example, in 2012 poverty thresholds were $11,945 for a single person and $23,364 for a family of four.18
Demographic characteristics were compared across expansion and non-expansion states. Unadjusted rates of self-reported screening were calculated by insurance and income group, comparing women with incomes less than 138% FPL (eligible for Medicaid in expansion states), between 138% and 400% FPL (eligible for subsidies through healthcare marketplaces), and more than 400% FPL.
Multiple logistic regression models estimated self-reported screening outcomes as a function of state Medicaid expansion status, controlling for insurance, income, and the set of other demographic covariates. Models were estimated for each outcome variable for all women in the sample, uninsured women, and women below 138% FPL. ORs for differences in outcomes between expansion and non-expansion states were calculated for all models. All analyses employed survey weights accounting for complex sampling design. Statistical analyses were conducted in 2014 using Stata, version 11 (StataCorp LP, College Station TX).
Results
Table 1 presents demographic characteristics and outcomes for the mammogram and Pap test samples by state Medicaid expansion status. Women in states that have not expanded Medicaid were significantly more likely to be black or white (as opposed to Asian or other race) and have income less than 138% FPL.
Table 1.
Descriptive statistics for mammogram and Pap test samples by 2014 state Medicaid expansion status
| Mammogram Sample | Pap test Sample | |||
|---|---|---|---|---|
| Characteristic | Expansion States (N=28752) | Non-expansion States (N=27732) | Expansion States (N=45603) | Non-expansion States (N=39264) |
| Mean age (years) | 57.6± (.048) | 57.7± (.049) | 45.7±(.113) | 45.6±(.110) |
| Age group (%) | ||||
| 24–34 years | 18.5 | 18.3 | ||
| 35–49 years | 40.6 | 41.8 | ||
| 50–54 yearsa. | 27.9 | 26.8 | 16.5 | 15.9 |
| 55–59 years | 36.6 | 36.7 | 12.8 | 12.7 |
| 60–64 years | 35.4 | 36.5 | 11.6 | 11.3 |
| Race (%) | ||||
| White | 80.4 | 81.2** | 76.9 | 78.7** |
| Black | 8.9 | 14.8** | 9.2 | 15.0** |
| Asian | 6.4 | 1.1** | 8.5 | 2.3** |
| Other race | 4.3 | 2.8** | 5.4 | 4.0** |
| Hispanic ethnicity (%) | 8.9 | 6.1** | 15.4 | 9.8** |
| Income (%) | ||||
| <138% of FPL | 16.9 | 20.1** | 24.1 | 24.4 |
| 138–100% of FPL | 41.6 | 41.5** | 48.3 | 49.8** |
| >400% of FPL | 41.5 | 38.4** | 27.7 | 25.8** |
| Education | ||||
| Less than high school | 8.3 | 9.8** | 9.9 | 8.7** |
| High school | 26.4 | 31.0** | 22.0 | 25.3** |
| Some college | 33.7 | 32.9** | 31.3 | 31.8** |
| College or more | 31.6 | 26.3 | 36.9 | 34.2** |
| Employed (%) | 59.9 | 54.2* | 66.2 | 64.2** |
| Insured (%) | 89.0 | 85.7** | 86.4 | 82.1 |
| Mammogram in past 2 years (%) | 80.4 | 77.0** | ||
| Pap test in past 3 years (%) | 86.9 | 84.8** | ||
Note: cells represent weighted mean (standard error) or weighted percentage of sample. All analyses employ survey weights accounting for the BRFSS complex sampling design.
p<0.01
p<0.05 in test of difference by state Medicaid expansion status. Results with significant p-values indicated in bold.
The age range for the mammogram sample is 52 to 64 years; the youngest age in each sample is the number of years of the recommended screening interval past the recommended age for initiation of routine screening.
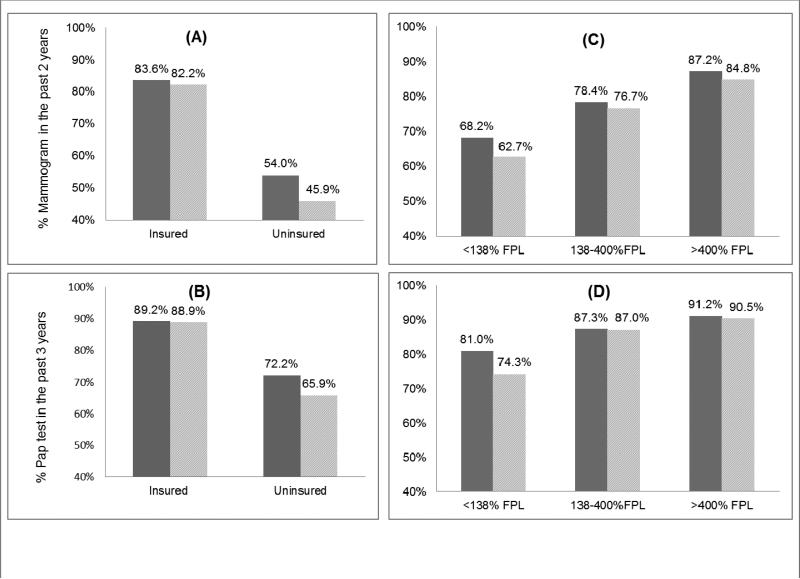
Figure 1 presents unadjusted rates of screening by state expansion status across insurance and income groups. Insured women were far more likely to receive screening than uninsured women. Further, uninsured women in non-expansion states were 15.1% (95% CI=5.5%, 24.7%) less likely to receive a mammogram (Figure A) and 8.7% (95% CI=3.5%, 13.8%) less likely to receive a Pap test (Figure B) than uninsured women in expansion states. Among women with income less than 138% FPL, those in non-expansion states were 8.1% (95% CI=1.6%, 14.6%) less likely to receive a mammogram (Figure C) and 8.3% (95% CI=4.9%, 11.8%) less likely to receive a Pap test (Figure D) than low-income women in expansion states.
Figure 1.
Unadjusted screening rates by state Medicaid expansion status, insurance, and income
Table 2 presents logistic regression results, which further support the descriptive results. Columns 1 and 2 present results for the full sample and show that, controlling for a rich set of demographic characteristics, women in non-expansion states have significantly lower odds of being screened at baseline. Columns 3 and 4 restrict the sample to uninsured women, and show that in non-expansion states, uninsured women have lower odds of receiving a mammogram (OR= 0.72, 95% CI=0.56, 0.91) or a Pap test (OR=0.78, 95% CI=0.648, 0.939). Columns 5 and 6 restrict the sample to less than 138% FPL and show that in non-expansion states, odds of mammography are lower (OR=0.85, 95% CI=0.69, 1.05) albeit not statistically significant, and odds of receiving a Pap test are significantly lower (OR=0.79, 95% CI=0.66, 0.95).
Table 2.
Logistic regressions of screening outcome measures on state Medicaid expansion status
| Full sample | Uninsured sample | Low-income sample | ||||
|---|---|---|---|---|---|---|
| Mammogram in past two years | Pap test in past three years | Mammogram in past two years | Pap test in past three years | Mammogram in past two years | Pap test in past three years | |
| N | 56,484 | 84,867 | 6,488 | 11,149 | 9,757 | 17,237 |
| Non-expansion state | 0.870** (0.794 - 0.953) | 0.871** (0.794 - 0.954) | 0.715** (0.562 - 0.909) | 0.780** (0.648 - 0.939) | 0.853 (0.691 - 1.054) | 0.789* (0.658 - 0.945) |
| Expansion state | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Insured | 3.939** (3.475 - 4.466) | 3.038** (2.683 - 3.440) | 3.453** (2.797 - 4.263) | 2.425** (2.010 - 2.927) | ||
| Uninsured | 1.00 | 1.00 | 1.00 | 1.00 | ||
| >400%ofFPL | 1.845** (1.576 - 2.159) | 1.835** (1.569 - 2.146) | 2.197** (1.496 - 3.228) | 2.096** (1.457 - 3.016) | ||
| 138-400% of FPL | 1.277** (1.111 - 1.469) | 1.332** (1.162 - 1.527) | 1.065 (0.824 - 1.376) | 1.076 (0.866 - 1.335) | ||
| Income < 138% FPL | 1.00 | 1.00 | 1.00 | 1.00 | ||
| Age 60–64 years | 1.216** (1.076 - 1.374) | 0.545** (0.459 - 0.648) | 1.321 (0.990 - 1.762) | 0.660** (0.482 - 0.902) | 1.084 (0.832 - 1.413) | 0.570** (0.425 - 0.766) |
| Age 55–59 years | 1.082 (0.961 - 1.219) | 0.558** (0.468 - 0.666) | 0.887 (0.661 - 1.191) | 0.476** (0.346 - 0.654) | 0.974 (0.751 - 1.264) | 0.510** (0.385 - 0.676) |
| Age 50-54 years| | 1.00 | 0.650** (0.547 - 0.772) | 1.00 | 0.487** (0.354 - 0.669) | 1.00 | 0.581** (0.442 - 0.763) |
| Age 35–49 years | 0.822* (0.696 - 0.970) | 0.771 (0.578 - 1.028) | 0.729* (0.561 - 0.947) | |||
| Age 24–34 years† | 1.00 | 1.00 | 1.00 | |||
| Black | 2.131** (1.783 - 2.547) | 1.859** (1.541 - 2.241) | 2.291** (1.584 - 3.312) | 2.311** (1.709 - 3.125) | 1.786** (1.369 - 2.330) | 1.848** (1.406 - 2.429) |
| Asian | 1.282 (0.830 - 1.980) | 0.540** (0.386 - 0.756) | 0.968 (0.342 - 2.741) | 1.302 (0.650 - 2.608) | 0.752 (0.302 - 1.869) | 0.753 (0.346 - 1.641) |
| Other Race | 0.830 (0.661 - 1.043) | 0.830 (0.668 - 1.031) | 0.966 (0.647 - 1.442) | 0.729 (0.489 - 1.087) | 1.196 (0.861 - 1.662) | 0.815 (0.585 - 1.135) |
| White | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Hispanic | 1.609** (1.248 - 2.075) | 2.283** (1.841 - 2.831) | 1.544 (0.997 - 2.390) | 2.362** (1.698 - 3.286) | 1.478* (1.002 - 2.180) | 2.562** (1.911 - 3.436) |
| Non-Hispanic | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Married | 1.359** (1.229 - 1.501) | 1.471** (1.332 - 1.626) | 1.297* (1.018 - 1.651) | 1.321** (1.097 - 1.591) | 1.434** (1.144 - 1.798) | 1.324** (1.101 - 1.593) |
| Unmarried | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| College or more | 1.473** (1.191 - 1.821) | 2.091** (1.654 - 2.644) | 0.931 (0.633 - 1.368) | 1.174 (0.840 - 1.639) | 1.047 (0.736 - 1.491) | 1.562** (1.129 - 2.162) |
| Some college | 1.339** (1.089 - 1.646) | 1.454** (1.162 - 1.820) | 1.066 (0.730 - 1.557) | 0.983 (0.715 - 1.351) | 1.196 (0.885 - 1.614) | 1.214 (0.911 - 1.619) |
| High School | 1.210 (0.988 - 1.480) | 1.289* (1.040 - 1.598) | 1.031 (0.723 - 1.469) | 0.944 (0.700 - 1.272) | 0.975 (0.739 - 1.286) | 1.207 (0.932 - 1.564) |
| Less than high school | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Employed | 1.086 (0.982 - 1.201) | 1.014 (0.911 - 1.129) | 1.130 (0.899 - 1.421) | 0.968 (0.795 - 1.177) | 1.024 (0.800 - 1.309) | 0.949 (0.783 - 1.151) |
| Not employed | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
Note: Cells represent odds ratios with 95% CI in parentheses. All analyses employ survey weights account for complex sampling design of the Behavioral Risk Factor Surveillance System.
FPL = Federal poverty level.
Boldface indicates statistical significance
p<0.05
p<0.01
The gaps in screening between expansion and non-expansion states are larger for uninsured women than for the general population. Predicted probabilities of screening based on the results in Columns 3 and 4 suggest that, conditional on a rich set of demographic covariates, uninsured women in non-expansion states are 7.9 and 4.9 percentage points less likely to receive recommended mammograms or Pap tests, respectively, than women in expansion states.
Discussion
Low-income and uninsured women are less likely to receive potentially lifesaving recommended cancer screening services. Although the CDC funds screening and diagnostic services for uninsured and underinsured women through the Breast and Cervical Cancer Early Detection Program, evidence suggests limited success reaching the targeted population.19 Differences across states in Medicaid coverage under the ACA may lead to a widening of racial and income disparities in cancer between states that expand and those that do not.
This study faces some limitations. Although measures of women's cancer screening in the BRFSS have been validated,20,21 there is evidence of over-reporting of screening, particularly among minorities.22,23 If anything, this may bias the present estimates of state differences downward. Response rates also vary across states and are low for some. Nonetheless, average response rates are similar across expansion (45%) and non-expansion states (47%); the analysis employs survey weights constructed to reduce non-response bias, and this is among the best data for tracking cancer screening at the state level.
Low-income women in non-expansion states have the lowest baseline breast and cervical cancer screening rates. As women in non-expansion states, who are more likely to be low-income and African American, remain uninsured while those in other states gain coverage, existing disparities by race and SES are likely to widen. Despite existing public cancer screening programs, uninsured women are still screened at significantly lower rates than women with insurance. States that do not expand their Medicaid programs are likely to perpetuate national disparities in cancer screening. The health risks and associated costs to underserved populations who do not receive preventive care must be taken into account in ongoing debates over expansion.
Acknowledgments
This research was supported by a grant from the NIH (No. R01CA178980, co-funded by the National Cancer Institute and the Office of Behavioral and Social Sciences Research, Principal Investigator, Lindsay M. Sabik). The funders had no role in study design; collection, analysis, and interpretation of data; writing; or the decision to submit for publication.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
No financial disclosures were reported by the authors of this paper.
The authors have no conflicts of interest to disclose.
References
- 1.Jones BA, Patterson EA, Calvocoressi L. Mammography screening in African American women: evaulating the research. Cancer. 2003;97(S1):258–72. doi: 10.1002/cncr.11022. [DOI] [PubMed] [Google Scholar]
- 2.Rodríguez MA, Ward LM, Pérez-Stable EJ. Breast and cervical cancer screening: impact of health insurance status, ethnicity, and nativity of Latinas. Ann Fam Med. 2005;3(3):235–41. doi: 10.1370/afm.291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Selvin E, Brett KM. Breast and cervical cancer screening: sociodemographic predictors among White, Black, and Hispanic women. Am J Public Health. 2003;93(4):618–23. doi: 10.2105/ajph.93.4.618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shi L, Lebrun LA, Zhu J, Tsai J. J Health Care Poor Underserved. 2011;Cancer screening among racial/ethnic and insurance groups in the United States: a comparison of disparities in 2000 and 2008.22(3):945–61. doi: 10.1353/hpu.2011.0079. [DOI] [PubMed] [Google Scholar]
- 5.Busch SH, Duchovny N. Family coverage expansions: impact on insurance coverage and health care utilization of parents. J Health Econ. 2005;24(5):876–90. doi: 10.1016/j.jhealeco.2005.03.007. [DOI] [PubMed] [Google Scholar]
- 6.Finkelstein A, Taubman S, Wright B, Bernstein M, Gruber J, Newhouse JP, et al. The Oregon health insurance experiment: evidence from the first year. Q J Econ. 2012;127(3):1057–106. doi: 10.1093/qje/qjs020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wherry LR. Medicaid family planning expansions and related preventive care. Am J Public Health. 2013;103(9):1577–82. doi: 10.2105/AJPH.2013.301266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Roetzheim RG, Pal N, Tennant C, et al. Effects of health insurance and race on early detection of cancer. J Natl Cancer Inst. 1999;91(16):1409–15. doi: 10.1093/jnci/91.16.1409. [DOI] [PubMed] [Google Scholar]
- 9.Hartmann KE, Hall SA, Nanda K, Boggess JF, Zolnoun D. Screening for Cervical Cancer. Agency for Healthcare Research and Quality; Rockville, MD: 2002. [PubMed] [Google Scholar]
- 10.Nelson HD, Tyne K, Naik A, Bougatsos C, Chan BK, Humphrey L. Screening for breast cancer: an update for the U.S. Preventive Services Task Force. Ann J Intern Med. 2009;151(10):727–W.242. doi: 10.1059/0003-4819-151-10-200911170-00009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.CDC Cancer screening - United States, 2010. MMWR Morb Mortal Wkly Rep. 2012;61(3):41–5. [PubMed] [Google Scholar]
- 12.Peek MF, Han JH. Disparities in screening mammography: current status, interventions, and implications. J Gen Intern Med. 2004;19(2):184–94. doi: 10.1111/j.1525-1497.2004.30254.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ross J, Bradley E, Busch S. Use of health care services by lower-income and higher-income uninsured adults. JAMA. 2006;295(17):2027–36. doi: 10.1001/jama.295.17.2027. [DOI] [PubMed] [Google Scholar]
- 14.Centers for Disease Control and Prevention Behavioral Risk Factor Surveillance System: Overview: BRFSS 2012. 2013 www.cdc.gov/brfss/annual_data/2012/pdf/Overview_2012.pdf.
- 15.Centers for Medicare and Medicaid Services State Medicaid and CHIP Income Eligibility Standards. 2014 www.medicaid.gov/AffordableCareAct/Medicaid-Moving-Forward-2014/Downloads/Medicaid-and-CHIP-Eligibility-Levels-Table.pdf.
- 16.U.S. Preventive Services Task Force Screening for Cervical Cancer. 2012 www.uspreventiveservicestaskforce.org/uspstf/uspscerv.htm.
- 17.U.S. Preventive Services Task Force Screening for Breast Cancer. 2009 www.uspreventiveservicestaskforce.org/uspstf/uspsbrca.htm.
- 18.U.S. Census Bureau Poverty Thresholds. 2014 www.census.gov/hhes/www/poverty/data/threshld/
- 19.Tangka FKL, O'Hara B, Gardner J, et al. Meeting the cervical cancer screening needs of underserved women: the National Breast and Cervical Cancer Early Detection Program, 2004-2006. Cancer Causes Control2010. 21(7):1081–90. doi: 10.1007/s10552-010-9536-3. [DOI] [PubMed] [Google Scholar]
- 20.Caplan LS, McQueen DV, Qualters JR, Leff M, Garrett C, Calonge N. Validity of Women’s Self-Reports of Cancer Screening Test Utilization in a Managed Care Population. Cancer Epidemiol Biomarkers Prev. 2003;12(11):1182–7. [PubMed] [Google Scholar]
- 21.Zapka JG, Bigelow C, Hurley T, et al. Mammography Use among Sociodemographically Diverse Women: The Accuracy of Self-Report. Am J Public Health. 1996;86(7):1016–21. doi: 10.2105/ajph.86.7.1016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Fiscella K, Holt K, Meldrum S, Franks P. Disparities in preventive procedures: comparisons of self-report and Medicare claims data. BMC Health Serv Res. 2006;6(1):122–29. doi: 10.1186/1472-6963-6-122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Njai R, Siegel PZ, Miller JW, Liao Y. Misclassification of survey responses and black-white disparity in mammography use, behavioral risk factor surveillance system, 1995-2006. Prev Chronic Dis. 2011;8(3):A59. [PMC free article] [PubMed] [Google Scholar]