Abstract
Early screening for psychological distress has been suggested to improve patient management for individuals experiencing low back pain. This study compared two approaches to psychological screening (i.e., multidimensional and unidimensional) so that preliminary recommendations on which approach may be appropriate for use in clinical settings other than primary care could be provided. Specifically, this study investigated STarT Back Screening Tool (SBT): 1) discriminant validity by evaluating its relationship with unidimensional psychological measures and 2) construct validity by evaluating how SBT risk categories compared to empirically derived subgroups using unidimensional psychological and disability measures. Patients (n = 146) receiving physical therapy for LBP were administered the SBT and a battery of unidimensional psychological measures at initial evaluation. Clinical measures consisted of pain intensity and self-reported disability. Several SBT risk dependent relationships (i.e., SBT low < medium < high risk) were identified for unidimensional psychological measure scores with depressive symptom scores associated with the strongest influence on SBT risk categorization. Empirically derived subgroups indicated that there was no evidence of distinctive patterns amongst psychological or disability measures other than high or low profiles, therefore two groups may provide a more clear representation of the level of pain associated psychological distress, maladaptive coping and disability in this setting, as compared to three groups which have been suggested when using the SBT in primary care settings.
Keywords: psychological screening, psychological subgrouping, STarT Back Screening Tool, low back pain, physical therapy
Introduction
Early risk factor screening for poor clinical outcomes has been identified as a potential method to improve the efficiency and effectiveness of care.9, 27, 50 Findings from recent reviews10, 47 indicate consistent relationships between elevated levels of psychological factors measured during initial assessment and poor future clinical outcomes. Therefore, routine and early identification of psychological risk factors (i.e. screening) has been suggested as method to improve patient management strategies with the ultimate goal being the prevention of future LBP-associated activity limitations.9, 38, 43 Despite these suggestions, potential problems exist when attempting to translate research findings from one clinical setting to another. For example, differences in psychological profiles have been reported for patients seeking care for LBP in primary care settings when compared to secondary care settings.46 Moreover, decision-making dilemmas may be more common for secondary care setting providers that are commonly referred patients from primary care physicians as previous studies have suggested that primary care physicians may not adequately screen for psychological distress.32, 36 Therefore, there is the potential that some patients referred to physical therapy may be more appropriate for referral to mental health providers which may have negative implications in regard to initial management strategies and subsequent patient outcomes that are provided by secondary care providers (e.g., physical therapists). As a result, measures or tools that were developed and intended to be used in primary care settings by physicians or physical therapists providing care in primary care settings require additional testing prior to being implemented in secondary care settings (e.g., outpatient physical therapy).
Two methods of screening for psychological factors include the use of unidimensional or multidimensional self-report questionnaires. Unidimensional measures consist of several items with each item representing the same psychological construct, whereas multidimensional measures commonly consist of several items with each item representing a different psychological construct and may also consist of items representing other domains (e.g., physical impairment). There are strengths and limitations to using multidimensional measures to screen for psychological factors.27, 47, 63, 64 For example, multidimensional measures can provide information related to general psychological distress and require less time to administer in comparison to using several unidimensional measures that provide more detailed information about specific psychological factors. Alternatively, multidimensional measures may not provide as robust estimates of construct reliability in comparison to unidimensional measures consisting of multiple items related to the same construct.
The STarT Back Tool (SBT) is an example of a multidimensional screening measure consisting of 9-items related to physical and psychological factors. Based on SBT overall and psychosocial subscale scoring, individuals are categorized as either SBT low, medium, or high risk for persistent disabling LBP in primary care settings.25 SBT low and medium risk categories are primarily distinguished by SBT overall scoring, whereas SBT medium and high risk categories are primarily distinguished by SBT psychosocial scale scoring. Relevant to the purpose of this current study, is the methodology used during the development phase to generate SBT categorization cutoff scores. Specifically, receiver operating characteristic (ROC) curves and areas under the curve (AUC) analyses were used to test overall and psychosocial scale scores against dichotomized reference standard (e.g., disability) scores.25 While findings from previous studies1, 63 support the clinical utility of the SBT when compared to unidimensional psychological measures, there is a need for more direct comparisons between multidimensional and unidimensional screening approaches to provide more definitive clinical recommendations. For example, the identification of patient subgroups has been implicated as a high priority for future LBP-related research16, 22, 50 with particular concern for the influence that psychological factors have on LBP outcomes being emphasized,43, 49, 60 however there is no clear direction for clinicians as to the most appropriate methods to screen for psychological distress and to identify psychological subgroups.36 In addition, patients receiving initial consultation for LBP may be associated with different psychosocial profiles based on the type of clinical setting,46 therefore additional data is needed to evaluate the SBT's validity and determine its applicability in other health care settings.
The purpose of this study was to compare multidimensional and unidimensional approaches to screening for pain-associated psychological distress, maladaptive coping, and disability. First, we assessed SBT discriminant validity by evaluating relationships between SBT risk categories with full-length psychological measures and a self-report LBP related disability measure. Second, we investigated SBT construct validity by evaluating how SBT categories compare to empirically derived subgroups using cluster analysis from unidimensional psychological and LBP related disability questionnaires. Then we compared the SBT categories and empirically derived subgroups to each other, and with clinical measures of pain intensity and self-report disability. The overall goal of conducting these analyses was to provide preliminary future research suggestions for assessment of these psychological constructs in clinical settings other than primary care (e.g., outpatient physical therapy) because the SBT was specifically designed to support first contact care decision making.17
Material and Methods
Data for this cross-sectional study were obtained from a larger observational, prospective cohort study that assessed the predictive validity of the SBT in comparison to unidimensional psychological measures for 6-month clinical outcomes.1 Data were collected between December 14, 2009 and February 5, 2012 from four outpatient physical therapy clinics of Brooks Rehabilitation located in Jacksonville, Florida and two outpatient physical therapy clinics of Shands Rehabilitation located in Gainesville, Florida.
Participants
Consecutive patients seeking treatment for LBP at 6 participating outpatient physical therapy clinics were screened for study eligibility by a physical therapist. All patients were referred for physical therapy by a physician therefore this setting was considered secondary care. Potential study participants met both of the following criteria before being enrolled into this study: 1) adults between the ages of 18 and 65 years seeking physical therapy for LBP (defined as having symptoms at T12 or lower, including radiating pain into the buttocks and lower extremity) and 2) the ability to read and speak the English language. We included patients with a full range of LBP based on self-reported current symptom duration (i.e., acute [less than or equal to 14 days], subacute [15 to 90 days], and chronic [greater than or equal to 91 days]). These broad inclusion criteria were to allow for a cohort that was applicable to clinical practice. Potential study participants were ineligible to participate in this study if any of the following criteria were met: 1) the presence of systemic involvement related to metastatic or visceral disease; 2) recent spinal fracture; 3) osteoporosis; or 4) pregnancy. Physical therapists provided all patients that met study eligibility criteria with a brief explanation of the study and a study advertisement with primary investigator contact information. Clinicians emphasized to patients that participating in this study would not dictate the treatment they received for their LBP and if they elected not to participate they would receive the same treatment. This study was approved by the University of Florida's Institutional Review Board and informed consent was obtained from each study participant.
Demographic and Historical Variables
Study participants were asked to complete a standardized self-report questionnaire consisting of demographic items related to age, sex, race, and employment status. Additionally, information involving LBP clinical characteristics (i.e., prior surgery, symptom duration, symptom onset, symptom location, work-related LBP) was obtained.
STarT Back Screening Tool (SBT)
The SBT is a 9-item multidimensional screening measure used to identify subgroups of patients with LBP in primary care settings based on the presence of modifiable prognostic factors which may be useful in matching patients with targeted interventions.24, 25 The SBT contains items related to physical and psychosocial factors that have been identified as strong independent predictors for persistent disabling LBP. SBT overall scores (ranging from 0 to 9) are determined by summing all positive responses and SBT psychosocial subscale scores (ranging from 0 to 5) are determined by summing items related to bothersomeness, fear, catastrophizing, anxiety, and depression. Based on patient responses, the SBT categorizes patients as ‘high-risk’ (psychosocial subscale scores ≥4) in which high levels of psychosocial prognostic factors are present with or without physical factors present, ‘medium-risk’ (overall score >3; psychosocial subscale score <4) in which physical and psychosocial factors are present, but not a high level of psychosocial factors, or ‘low-risk’ (overall score 0-3) in which few prognostic factors are present.25 Acceptable test-retest reliability and internal consistency has been reported for SBT overall and psychosocial scale scores.25 SBT overall scores have demonstrated acceptable to outstanding discriminant validity for physical reference standards (e.g., disability and referred leg pain), while SBT psychosocial subscale continuous scores best discriminated psychosocial reference standards (e.g., catastrophizing, fear, and depression) in primary care settings.25 The SBT has demonstrated good concurrent validity in comparison to a similar screening instrument.26
Psychological Measures
Our selection of unidimensional psychological measures was primarily based on SBT psychosocial scale items and constructs related to maladaptive coping strategies and psychological distress in response to pain. Psychological measures were collected at baseline and are described in more detail below.
Maladaptive Coping
Fear-Avoidance Beliefs Questionnaire (FABQ-PA, FABQ-W)
Fear-avoidance beliefs specific to LBP were assessed with the FABQ.61 The FABQ consists of a 4-item FABQ physical activity scale (FABQ-PA, potentially ranging from 0 to 24) and a 7-item FABQ work scale (FABQ-W, potentially ranging from 0 to 42), with higher scores indicating higher levels of fear-avoidance beliefs for both FABQ scales. Both FABQ scales have been found to have acceptable reliability31, 55, 61 and demonstrated internal consistency.55, 57, 58, 61 The FABQ-W has demonstrated predictive validity for disability and work loss in patients with LBP.18, 19, 21, 61
Tampa Scale of Kinesiophobia (TSK-11)
The TSK-11 was used to assess the degree of fear of movement and injury or re-injury in individuals with LBP.65 The TSK-11 is an 11-item questionnaire with a potential range of 11 to 44, with higher scores indicating greater fear of movement and injury or re-injury due to pain. The TSK-11 has been found to have good test-retest reliability and internal consistency.65 Predictive and concurrent validity have also been reported for the TSK-11.65
Pain Catastrophizing Scale (PCS)
The PCS was used to assess the degree of catastrophic cognitions due to painful experiences.56 Pain catastrophizing has been broadly defined as an exaggerated negative orientation towards actual or anticipated pain experiences.56 The PCS is a 13-item questionnaire with a potential range of 0 to 52, with higher scores indicating higher levels of pain catastrophizing. Previous studies have supported the PCS as a reliable and valid measure.11, 12, 48, 56
Psychological Distress
Patient Health Questionnaire (PHQ-9)
The PHQ-9 was used to assess the degree to which depressive symptoms have on patients with LBP. The PHQ-9 is a 9-item questionnaire with a potential range of 0 to 27, with higher scores indicating elevated depressive symptoms. The PHQ-9 has demonstrated various types of validity in different healthcare settings29, 40 and has been used in studies involving patients with LBP.13
State-Trait Anxiety Inventory
The trait portion of the STAI (STAI-T) was used to assess the degree that dispositional anxiety has on patients with LBP.54 The STAI-T is a 20-item questionnaire with a potential range of 20 to 80, with higher scores indicating elevated levels of anxiety. The STAI-T has been found to be reliable and valid.4, 35 We reported the trait portion of the STAI as this construct is considered to be relatively stable over time and this measure was only assessed at intake.
Clinical Measures
Clinical measures were collected at baseline and are described in more detail below.
Numerical Pain Rating Scale (NPRS)
Pain intensity was rated using a NPRS, ranging from “0” (no pain) to “10” (worst pain imaginable).7, 8, 33 Participants were asked to rate their current pain intensity, as well as their best and worst level of pain intensity over the past 24 hours. These three pain ratings were averaged and used as the NPRS variable in this study.34
Oswestry Disability Questionnaire (ODQ)
LBP-related disability was assessed with the ODQ, which has 10 items that assesses how LBP affects common daily activities.20, 30 The ODQ has a range of 0% “no disability due to LBP” to 100% “completely disabled due to LBP”, with higher scores indicating higher LBP related disability. The ODQ has been found to have high levels of test-retest reliability, internal consistency, validity, and responsiveness.15, 20, 52
Roland-Morris Disability Questionnaire (RMDQ)
LBP-related disability was also assessed with the RMDQ, which has 24 items that assesses the functional status over the past 24 hours in patients with LBP.53 The RMDQ has a range of 0 “no disability due to LBP” to 24 “maximum disability due to LBP”, with higher scores indicating higher LBP related disability. The RMDQ has been found to have high levels of test-retest reliability, internal consistency, validity, and responsiveness.52, 53
Data Analysis
All data analyses were performed using SPSS, Version 20.0. Intake descriptive statistics were calculated for demographic variables, psychological and clinical measures. Raw scores for each full-length specific psychological measure and the RMDQ were transformed to z-scores to provide standardized scores for subsequent cluster analysis techniques; however raw scores are reported for descriptive purposes because they are more clinically interpretable.
SBT discriminant validity
We assessed SBT discriminant validity by evaluating relationships between SBT categories and differences in full-length psychological measure and RMDQ scores. First, relationships between full-length psychological measure and RMDQ scores by SBT categorization were evaluated using one-way analysis of variance (ANOVA) with Bonferroni post-hoc testing as appropriate. Next, discriminant function analysis (DFA) with cross-validated jackknifed classification was performed on the same sample as a follow-up to interpret: 1) how psychological measure and RMDQ scores differentiated SBT categorization and 2) the accuracy in SBT categorization using psychological measure and RMDQ scores. Briefly, DFA is a multivariate statistical procedure used to determine if a set of variables (i.e., psychological measure and RMDQ scores) can predict group membership (i.e., SBT categorization).59 Eigenvalues were reported as a measure of variance, indicating how well the discriminant function discriminated between SBT categories with higher eigenvalues indicating greater discrimination. Canonical correlations were reported as a measure of the relationship between SBT categorization and the discriminant function, with chi-square tests used to determine the significance of the relationship. A summary of classification results from the DFA was generated to evaluate for accuracy in SBT categorization. Jackknifed (i.e., one case at a time deleted) classification was used because it estimates the ability of predictors to separate groups which has been suggested to reduce bias in classification.59 Finally, two separate linear regression models were used to provide a test of linear effect across the three SBT categories with intake NPRS and ODQ scores serving as dependent variables.
SBT construct validity
We investigated SBT construct validity by evaluating how SBT categories compare to empirically derived subgroups and to determine which method is more strongly associated with clinical measures of pain intensity (NPRS) and self-report disability (ODQ) at intake. A cluster analysis using unidimensional psychological measure and RMDQ scores was used to generate empirically derived subgroups without considering SBT categorization. Specifically, an exploratory hierarchical agglomerative cluster analysis was performed using Ward's clustering method with squared Euclidean distances as the similarity measure to create homogeneous cluster profiles among unidimensional psychological measures and the RMDQ. Agglomeration coefficients were inspected and plotted to establish the most optimal cluster solution based on the percent change between adjacent cluster solutions45 and plot characteristics (i.e., elbow criterion).37 Then, to identify potential cluster group differences in demographic and clinical measure scores at intake, independent t-tests were used. Next, we compared the distribution of SBT categories by our empirically derived subgroups using chi-square analysis. Finally, SBT categories and cluster solutions were independently assessed for relationships with NPRS and ODQ clinical measures using one-way ANOVA and independent t-testing, respectively.
SBT cutoff scores associated with empirically derived psychological subgroups
Receiver operating characteristic (ROC) curve analysis was used to determine SBT overall scores that predicted empirically derived subgroup categorization. Area under the ROC curve (AUC) was interpreted as the probability of correctly identifying individuals categorized as “elevated pain-associated psychological distress, maladaptive coping and disability”. The range of AUC scores are from 0.5 (no better than chance identification) to 1.0 (perfect identification). Cutoff scores were then calculated for SBT overall scores (to match current SBT categories) for predicting empirically derived psychological subgroup categorization. Cutoff scores were determined by calculating sensitivity, specificity, and likelihood ratios for each potential SBT overall score.
Results
During this study period 275 patients were screened for eligibility criteria. Of these patients, 123 were excluded from study participation with the most common reason being that they were greater than 65 years of age (n = 47). The remaining 152 patients provided informed consent and were enrolled into the study. Of these patients, six were not able to complete the study due to personal reasons. Therefore, intake data was obtained from 146 patients. Patient demographic, clinical characteristics and psychological scores at intake by SBT categorization are displayed in Table 1. The SBT categorized 53 (36.3%) patients as low risk, 55 (37.7%) as medium risk and 38 (26.0%) as high risk. There were no differences in demographic or clinical characteristics amongst SBT subgroups (p > .05).
Table 1.
Descriptive statistics for study sample.
| Variable | Total Sample (n=146) | STarT Low Risk (n=53) | STarT Medium Risk (n=55) | STarT High Risk (n=38) | p-value |
|---|---|---|---|---|---|
| Demographic & Clinical | |||||
| Age (years) | 41.1 (13.5) | 38.8 (14.0) | 44.6 (12.8) | 40.3 (13.0) | .069 |
| Sex, n female (%) | 89 (61.0%) | 28 (52.8%) | 37 (67.3%) | 24 (63.2%) | .291 |
| Race (Caucasian / White) | 110 (75.9%) | 39 (75.0%) | 41 (74.5%) | 30 (78.9%) | .635 |
| (African American / Black) | 25 (17.2%) | 12 (23.1%) | 9 (16.4%) | 4 (10.5%) | |
| (Other) | 11 (6.9%) | 2 (1.9%) | 5 (9.1%) | 4 (10.5%) | |
| Employment (Employed) | 94 (65.7%) | 35 (67.3%) | 39 (72.2%) | 20 (54.0%) | .219 |
| (Unemployed) | 39 (27.3%) | 15 (28.9%) | 9 (16.7%) | 15 (40.5%) | |
| (Retired) | 10 (7.0%) | 2 (3.8%) | 6 (11.1%) | 2 (5.4%) | |
| Previous low back surgery (yes) | 26 (17.9%) | 8 (15.1%) | 11 (20.4%) | 7 (18.4%) | .773 |
| Symptom duration | |||||
| Acute (≤ 14 days) | 17 (11.8%) | 3 (5.8%) | 11 (20.8%) | 3 (7.9%) | .079 |
| Subacute (15-90 days) | 56 (39.2%) | 20 (38.5%) | 17 (32.1%) | 19 (50.0%) | |
| Chronic (≥ 91 days) | 70 (49.0%) | 29 (55.8%) | 25 (47.2%) | 16 (42.1%) | |
| Symptom location (LBP only) | 49 (33.6) | 25 (47.2%) | 15 (27.3%) | 9 (23.7%) | .059 |
| (LBP & buttock or thigh) | 72 (49.3%) | 23 (43.4%) | 30 (54.5%) | 19 (50.0%) | |
| (LBP & lower leg) | 25 (17.1%) | 5 (9.4%) | 10 (18.2%) | 10 (26.3%) | |
| Work related LBP (yes) | 19 (13.0%) | 8 (15.1%) | 7 (12.7%) | 4 (10.5%) | .813 |
| STarT Measures | |||||
| STarT overall score (range: 0-9) | 4.5 (2.5) | 1.8 (0.9) | 5.1 (1.1) | 7.4 (1.1) | <.001 |
| STarT psychosocial score (range: 0-5) | 2.3 (1.6) | 0.9 (0.8) | 2.3 (0.9) | 4.5 (0.5) | <.001 |
| Psychological Measures | |||||
| FABQ-PA (range: 0-24) | 14.5 (5.7) | 11.8 (5.5) | 14.6 (5.3) | 18.4 (4.4) | <.001 |
| FABQ-W (range: 0-42) | 12.5 (10.9) | 9.6 (9.6) | 13.7 (10.7) | 15.6 (12.6) | .023 |
| PCS (range: 0-52) | 16.8 (12.1) | 10.7 (9.6) | 17.1 (10.5) | 25.3 (13.0) | <.001 |
| TSK-11 (range: 11-44) | 25.1 (6.8) | 21.9 (6.4) | 25.2 (5.4) | 29.7 (6.9) | <.001 |
| PHQ-9 (range: 0-27) | 7.2 (6.1) | 3.7 (3.8) | 7.5 (5.5) | 12.4 (6.0) | <.001 |
| STAI-T (range: 20-80) | 36.1 (9.1) | 33.4 (7.6) | 36.2 (9.9) | 39.5 (9.4) | .008 |
| Clinical Outcome Measures | |||||
| NPRS (range: 0-10) | 5.3 (2.0) | 4.4 (1.9) | 5.6 (1.9) | 6.6 (1.5) | <.001 |
| ODQ (range: 0-100%) | 32.4 (16.7) | 19.9 (12.7) | 37.0 (14.1) | 43.5 (14.2) | <.001 |
| RMDQ (range: 0-24) | 11.2 (5.9) | 6.7 (4.5) | 12.1 (5.1) | 16.2 (4.1) | <.001 |
Abbreviations: FABQ-PA: Fear-Avoidance Beliefs Questionnaire (physical activity scale); FABQ-W: Fear-Avoidance Beliefs Questionnaire (work scale); PCS: Pain Catastrophizing Scale; TSK-11: Tampa Scale for Kinesiophobia (11-item version); PHQ-9: Patient Health Questionnaire (9-item version); STAI-T: State-Trait Anxiety Inventory (trait portion); NPRS: Numerical Pain Rating Scale; ODQ: Oswestry Disability Questionnaire; RMDQ: Roland Morris Disability Questionnaire.
SBT discriminant validity
Comparisons amongst all SBT risk subgroups indicated a SBT risk dependent relationship (i.e., SBT low < medium < high risk) with several psychological measures and the RMDQ. Specifically, patients categorized as SBT low risk had lower intake FABQ-PA, PCS, TSK-11, PHQ-9, and RMDQ scores compared to those categorized as being medium or high risk (p < .05). Comparisons amongst SBT low and high risk subgroups indicated that patients initially categorized as SBT low risk had lower intake FABQ-W and STAI-T scores compared to those categorized as high risk (p < .05).
DFA run with simultaneous entry method with one self-report disability (RMDQ: Wilks’ λ = .61, p < .001) and six psychological predictors (FABQ-PA: Wilks’ λ = .80, p < .001; FABQ-W: Wilks’ λ = .95, p = .032; PCS: Wilks’ λ = .78, p < .001; TSK-11: Wilks’ λ = .81, p < .001; PHQ-9: Wilks’ λ = .69, p < .001; STAI-T: Wilks’ λ = .94, p = .012;) suggested that each predictor contributed uniquely to SBT categorization and resulted in two discriminant functions which is expected with three SBT risk categories. The overall test of the two functions was significant (χ2 (14) = 102.84, Wilks’ λ = .47, p < .001) indicating that predictor scores were able to discriminate amongst the three SBT categories. The test for function 2 alone was not significant (χ2 (6) = 2.00, Wilks’ λ = .98, p = .919), however function 1 accounted for 51.8% (canonical R = .72) of the total relationship between predictors and SBT categories. The pooled within-groups correlations between discriminating variables and standardized canonical discriminant functions, as well as the standardized canonical discriminant function coefficients (analogous to multiple regression beta weights) are provided in Table 2. RMDQ and PHQ-9 scores demonstrated the strongest positive relationships with the discriminant function, whereas FABQ-PA and PCS scores demonstrated moderate positive relationships and TSK-11 scores demonstrated the weakest positive relationship. FABQ-W and STAI-T scores demonstrated weak negative relationships with the discriminant function. The overall accuracy for classification using the discriminant function was 59.4% using the cross-validated jackknifing technique. The percentages classified correctly were 78.8% for SBT low-risk, 37.7% for SBT medium-risk, and 63.2% for SBT high-risk. Based on sample distribution, the prior probabilities for chance assignment were 36.3% for SBT low-risk, 37.7% for SBT medium-risk, and 26.0% for SBT high-risk. Classification by the discriminant function exceeded chance classification for SBT low and high-risk categories, and was identical for SBT medium-risk when the cross-validated values were compared.
Table 2.
Coefficients of unidimensional psychological and disability measures of the discriminant function.
| Discriminant Function | ||||
|---|---|---|---|---|
| Unidimensional Psychological and Disability Measures | 1 | 2 | ||
| Standardized Coefficients* | Correlation Coefficients† | Standardized Coefficients* | Correlation Coefficients† | |
| FABQ-PA | 0.288 | 0.475 | 0.540 | 0.475 |
| FABQ-W | −0.290 | 0.213 | −0.302 | −0.262 |
| PCS | 0.284 | 0.509 | −0.031 | 0.138 |
| TSK-11 | 0.084 | 0.465 | 0.325 | 0.403 |
| PHQ-9 | 0.413 | 0.645 | 0.454 | 0.217 |
| STAI-T | −0.072 | 0.246 | −0.133 | 0.042 |
| RMDQ | 0.640 | 0.770 | −0.764 | −0.582 |
Abbreviations: FABQ-PA: Fear-Avoidance Beliefs Questionnaire (physical activity scale); FABQ-W: Fear-Avoidance Beliefs Questionnaire (work scale); PCS: Pain Catastrophizing Scale; TSK-11: Tampa Scale for Kinesiophobia (11-item version); PHQ-9: Patient Health Questionnaire (9-item version); STAI-T: State-Trait Anxiety Inventory (trait portion); RMDQ: Roland-Morris Disability Questionnaire.
Key:
indicates standardized canonical discriminant function coefficients
indicates pooled within-groups correlations between discriminating variables and standardized canonical discriminant functions.
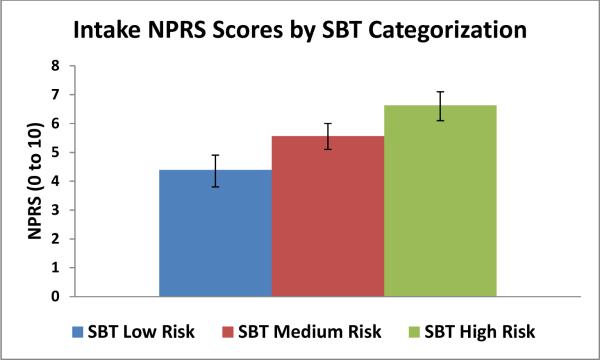
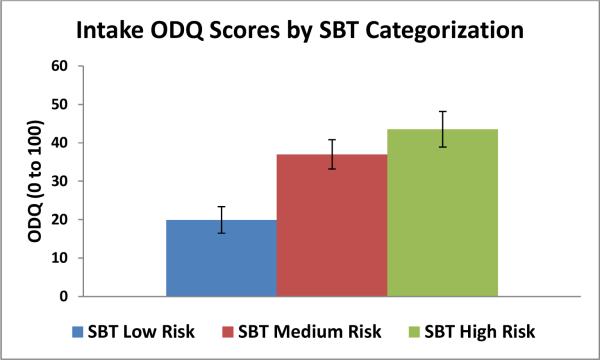
Results from two separate linear regression models indicated that SBT categorization accounted for 19.8% and 32.3% of the variance in intake NPRS (β = .44, p < .01) and ODQ (β = .57, p < .01) scores respectively. SBT risk categorization dependent relationships with intake NPRS and ODQ scores are provided in Figures 1a and 1b.
Figure 1.
a. Intake NPRS scores by SBT categorization.
Abbreviations: NPRS, Numerical Pain Rating Scale; SBT, STarT Back Tool. Error bars indicate 95% confidence intervals.
Figure 1b Intake ODQ scores by SBT categorization.
Abbreviations: ODQ, Oswestry Disability Questionnaire; SBT, STarT Back Tool. Error bars indicate 95% confidence intervals.
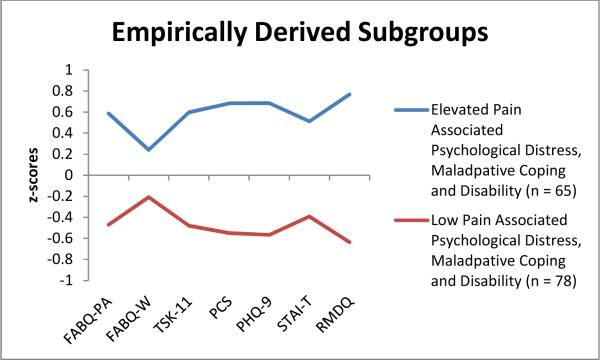
Empirically Derived Subgroups
Inspection of all predictor z-scores indicated that absolute values did not exceed 4.0 (range = −2.5 to 3.1), suggesting the data did not contain extreme outliers.44, 59 Inspection of agglomeration coefficients from a hierarchical agglomerative cluster analysis of 6 psychological measures and a single self-report disability measure revealed that the percent change was moderate (41.8%) between the 2 and 1-cluster solutions with relatively smaller changes in preceding steps, suggesting a 2-cluster solution is appropriate, which was further confirmed by visual inspection of plotted agglomeration coefficients.37, 45 The cluster profiles are shown in Figure 2. Cluster 1 was labeled “Low Pain-Associated Psychological Distress, Maladaptive Coping and Disability” (n = 78, 54.5%) and was comprised of individuals that were associated with lower psychological measure and RMDQ scores when compared to cluster 2 which was labeled “Elevated Pain-Associated Psychological Distress, Maladaptive Coping and Disability” (n = 65, 45.5%) and was comprised of individuals that were associated with higher psychological measure and RMDQ scores. There were no significant differences between the clusters in demographic or LBP clinical characteristic variables (p >.05). Descriptive statistics for psychological measure and RMDQ raw scores for each cluster are shown in Table 3 to make interpretation easier.
Figure 2.
Empirically derived psychological subgroups.
Abbreviations: FABQ-PA: Fear-Avoidance Beliefs Questionnaire (physical activity scale); FABQ-W: Fear-Avoidance Beliefs Questionnaire (work scale); TSK-11: Tampa Scale for Kinesiophobia (11-item version); PCS: Pain Catastrophizing Scale; PHQ-9: Patient Health Questionnaire (9-item version); STAI-T: State-Trait Anxiety Inventory (trait portion); RMDQ: Roland Morris Disability Questionnaire.
Table 3.
Psychological and clinical measure scores across empirically-based psychological subgroups.
| Low Pain-Associated Psychological Distress, Maladaptive Coping, and Disability Cluster (n = 78) | Elevated Pain-Associated Psychological Distress, Maladaptive Coping, and Disability Cluster (n = 65) | |||||
|---|---|---|---|---|---|---|
| m (sd) | m (sd) | p-value | Effect size | |||
| Psychological Measures | ||||||
| FABQ-PA | 11.9 (5.1) | 18.0 (4.4) | < .01 | 1.28 | ||
| FABQ-W | 10.4 (9.6) | 15.5 (11.9) | < .01 | 0.47 | ||
| PCS | 10.3 (8.6) | 25.2 (11.1) | < .01 | 1.50 | ||
| TSK-11 | 21.9 (5.8) | 29.3 (5.7) | < .01 | 1.29 | ||
| PHQ-9 | 4.0 (3.5) | 11.6 (5.9) | < .01 | 1.57 | ||
| STAI-T | 32.5 (6.8) | 40.7 (9.6) | < .01 | 0.99 | ||
| Clinical Measures | ||||||
| NPRS | 4.5 (1.9) | 6.4 (1.4) | < .01 | 1.14 | ||
| OSW | 23.3 (13.4) | 43.6 (13.3) | < .01 | 1.52 | ||
| RMDQ | 7.4 (4.6) | 15.8 (3.9) | < .01 | 1.97 | ||
Abbreviations: FABQ-PA: Fear-Avoidance Beliefs Questionnaire (physical activity scale); FABQ-W: Fear-Avoidance Beliefs Questionnaire (work scale); PCS: Pain Catastrophizing Scale; TSK-11: Tampa Scale for Kinesiophobia (11-item version); PHQ-9: Patient Health Questionnaire (9-item version); STAI-T: State-Trait Anxiety Inventory (trait portion); NPRS: Numerical Pain Rating Scale; ODQ: Oswestry Disability Questionnaire; RMDQ: Roland Morris Disability Questionnaire. All estimates reported as mean (m) and standard deviation (sd) unless otherwise indicated. Effect size estimate: Cohen's d.
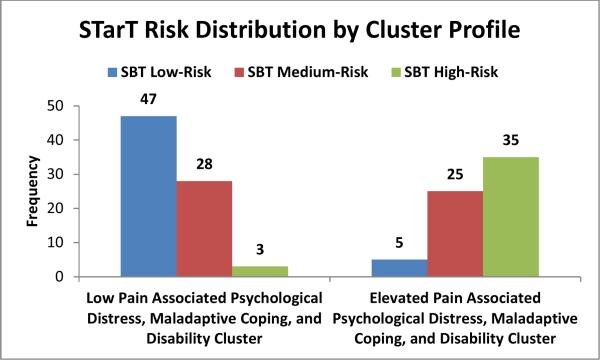
The distribution of cluster profiles by SBT categorization is provided in Figure 3. In the Low Pain-Associated Psychological Distress, Maladaptive Coping and Disability cluster, 60.3% of participants were categorized as SBT low risk compared to SBT medium and high risk (35.9% and 3.8% respectively) and in the Elevated Pain-Associated Psychological Distress, Maladaptive Coping and Disability cluster, 53.8% of participants were categorized as SBT high risk, compared to SBT medium and low risk (38.5% and 7.7% respectively) (χ2 = 60.36, p < .001). Inspection of standardized residuals indicated that the proportion of those categorized as SBT low risk was less than expected (std. residual = −3.8) and those categorized as SBT high risk was greater than expected (std. residual = 4.3) in the Elevated Pain-Associated Psychological Distress, Maladaptive Coping and Disability cluster.
Figure 3.
STarT category distribution by cluster profile.
Abbreviations: SBT: STarT Back Tool.
Using SBT categorization to evaluate for relationships amongst clinical measures, an SBT risk dependent relationship (i.e., SBT low < medium < high risk) was identified for NPRS scores (p < .01) (Cohen's d estimates: low vs. medium (0.63); low vs. high (1.29); medium vs. high (0.59)). Patients categorized as SBT low risk were associated with lower ODQ scores in comparison to those categorized as SBT medium (Cohen's d = 1.28) and high risk (Cohen's d = 1.75) (p < .01), however ODQ scores for SBT medium and high risk were similar (p > .05). Using our two empirically derived subgroups to evaluate for similar relationships indicated that patients allocated to the Low Pain-Associated Psychological Distress, Maladaptive Coping and Disability cluster were associated with lower NPRS (p < .01; Cohen's d = 1.14) and ODQ (p < .01; Cohen's d = 1.52) scores in comparison to those allocated to the Elevated Pain-Associated Psychological Distress, Maladaptive Coping and Disability cluster (Table 3).
SBT cut-off scores associated with empirically derived psychological subgroups
The AUC for SBT overall scoring was .907 (95% CI: .857 – .957). Upon visual inspection, the cutoff point nearest the upper-left hand corner of the ROC curve was 4.5 points for the SBT overall score (sensitivity = .892; specificity = .821; +LR = 4.98; −LR = 0.13) indicating that patients with SBT total scores ≥5 would have increased odds to be categorized as Elevated Pain-Associated Psychological Distress, Maladaptive Coping and Disability and those scoring ≤4 would be have decreased odds to be categorized as Elevated Pain-Associated Psychological Distress, Maladaptive Coping and Disability.
Discussion
The purpose of this study was to provide a direct comparison between the SBT with several psychological measures and a self-report LBP related disability measure. The overall intent of this study was to provide preliminary suggestions for measurement of key psychological constructs in settings other than primary care. The SBT has been successfully applied in primary care25 and chiropractic39 settings, therefore additional data are needed to evaluate the SBT's validity and determine the promising applicability of this screening measure in other health care settings because the SBT was specifically designed to support first contact care decision making.17 Our primary findings indicated that several SBT risk dependent relationships (i.e., SBT low < medium < high risk) exist for full-length unidimensional psychological measure scores and that with the exception of self-reported disability; depressive symptoms may have the strongest influence on risk categorization by the SBT. Our empirically derived subgroups indicated that there was no evidence of distinctive patterns amongst psychological or self-report disability measures other than high or low profiles in this setting, as compared to three groups which have been suggested when using the SBT in primary care settings. Therefore, the SBT has potential for use as a first line screening measure for identifying pain-associated psychological distress, maladaptive coping and disability in physical therapy settings, however future prospective studies are required to evaluate potential modification of SBT risk category cut off scores that may provide a more accurate representation of the subgroups in in this particular clinical setting.
The identification of SBT risk dependent relationships across several unidimensional psychological measure scores provide indications that administering the SBT can ably replace administering multiple unidimensional psychological measures at initial assessment as a first line screening measure for psychological distress. Previous studies conducted in physical therapy1 and primary care63 settings have indicated similar suggestions. This parsimonious measurement option may be advantageous for clinicians practicing in busy outpatient settings where time is becoming more limited and utilization of brief validated screening tools has been suggested as a method to improve clinical decision-making efficiency.26, 27, 47 However, clinicians using the SBT as a first line screening measure need to be aware of potential for misclassification because the SBT provides an indication of overall disability risk. The SBT does not provide detailed information about specific psychological factors; therefore, certain patients may require additional assessment for specific psychological factors. For example, our findings indicated that when only considering psychological measures, PHQ-9 scores were associated with the strongest positive relationship with SBT categorization potentially suggesting that further detailed assessment for depressive symptoms may be appropriate for those patients categorized as SBT high-risk. This additional information could then be implemented into clinical decision-making to determine if these patients are potential candidates for referral to mental health professionals.
We used cluster analysis to generate two empirical-based subgroups while the SBT categorizes patients into three subgroups. The SBT was developed to incorporate baseline prognostic information to distinguish patients categorized as SBT low risk from medium and high risk, however expected patient response to treatment is primarily used to distinguish SBT medium from high risk and would require analysis of prospective data.17 Therefore, we acknowledge that when comparing these two different subgrouping approaches our findings may have been a reflection of the cross-sectional design and analysis. Future prospective studies are necessary to determine if the 2 empirically derived subgroups identified in our cluster analysis provide predictive capabilities for clinical outcomes as well as the 3 SBT subgroups already described.1 Specifically, a prospective comparison of the 2 and 3 SBT subgroup options would be able to determine if incorporating only 2 subgroups is sensitive enough to distinguish outcome differences from SBT medium and high risk groups. This is an important issue to resolve in future studies because a 2 subgroup option may be more pragmatic for screening purposes, however if consolidation of risk subgroups limits how the SBT can be used to guide initial treatment decisions then the 2 subgroup option may not be acceptable for clinical adoption.
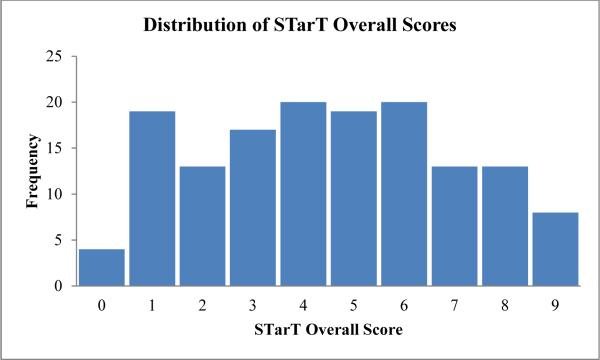
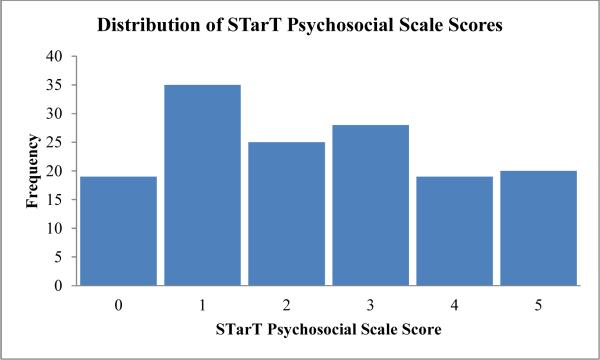
Despite the methodological differences in generating subgroups, visual inspection of the distribution of SBT scores generated from our sample did not reflect a trimodal distribution (Figures 4a-b), rather was more closely indicative of a bimodal distribution which parallel the number of our empirically derived subgroups. These findings are consistent with previous suggestions that current three SBT categorical designations may not represent underlying distributions of SBT scores for patients experiencing LBP in all clinical settings.51 Therefore, there is the potential that a modified risk stratification scoring system using the SBT may be more applicable in this clinical setting, however future studies are required prior to providing any preliminary recommendations. In our analyses the ROC generated SBT cutoff scores that can be used to categorize patients as Elevated Pain-Associated Psychological Distress, Maladaptive Coping and Disability were similar, compared to a SBT psychosocial scale score equal to or greater than 4 points for the same categorization in the primary care setting. Our empirically derived psychological subgroups were also associated with low and high levels for multiple clinical measure scores (i.e., NPRS and ODQ) each representing a unique clinical outcome domain (i.e., pain intensity and self-reported disability, respectively) which may have future research implications. Future longitudinal studies are required to determine if our 2-cluster solution provides an accurate prediction of pain and disability outcomes.
Figure 4.
a. Distribution of STarT overall scores.
b. Distribution of STarT psychosocial scale scores.
Related to our cluster analysis findings, the lack of specificity amongst psychological measures to generate patterns other than high or low pain-associated psychological distress and maladaptive coping potentially suggests that initial screening for specific psychological domains through the use of multiple measures may not be necessary for all patients. Rather, first line psychological risk factor screening with a single multidimensional measure may be used to identify patients requiring additional psychological assessment. There is preliminary evidence that the ability to identify greater than two psychological subgroups may be dependent upon the type of psychological distress assessed.2, 5, 6, 14, 62 For example, Beneciuk et al.2 identified three different subgroups by incorporating a measure of patient-specific pain related fear in addition to measures of general pain related fear and catastrophizing. Beneciuk et al.2 suggested that specific fear should then be accounted for separately with individuals experiencing LBP and that multidimensional measures (e.g., the STarT Back Tool) may not account for a potentially important patient subgroup because they do not include items associated with specific fears. Alternatively, there is support that the cumulative relationship amongst different elevated psychological factors may have an additive adverse effect on patient prognosis and clinical outcomes.3, 42, 64 For example, Bergbom et al.3 identified four subgroups with varying psychological profiles based on pain catastrophizing and depressive symptom scores where patients categorized as high risk were associated with the greatest levels of self-report disability and pain intensity when compared to other subgroups. Collectively, the above referenced studies provide insight to the ongoing debate regarding identification of the appropriate number of subgroups when screening for psychological distress and how that information can be used for prognostic purposes. Furthermore, the number of subgroups identified may not only be related to clinical setting, but may also be dependent upon the psychological measures that are administered. Future studies that incorporate consistent measures will help to resolve the issue of determining an appropriate number of psychological subgroups in clinical settings.
Findings from this cross-sectional study add to the literature involving the SBT as a screening measure for LBP-associated psychological distress, however does not provide information related to treatment. Results from a recent clinical trial in primary care settings indicated that initial treatment decisions based on SBT categorization on 3 levels (i.e., SBT low, medium, and high risk) were associated with greater improvements in clinical outcomes and cost savings when compared to usual care for patients with LBP.28 Specifically, future studies should evaluate the SBT to guide risk-stratified treatment in secondary care settings and determine if two categories is potentially more appropriate for decision making and providing effective treatment. Future studies should also consider investigating the SBT in work-related injury settings to determine how risk stratification may differ for those patient samples.
Several limitations should be considered when interpreting the results of this study. First, these results were based on cluster analysis, therefore we employed various “stopping rules” combined with practical judgment and theoretical foundations in determining our final number of clusters solutions.23 In our opinion, this subgrouping methodology should also be considered a strength of this study as our empirically derived subgroups reflected the underlying distribution of unidimensional psychological and disability measure scores and were not based on arbitrary cutoff scores. Future studies should consider establishing an a-priori optimal number of cluster solutions with an empirical basis, then determine if agglomeration coefficients and plot characteristics confirm or refute their hypothesis (e.g. confirmatory cluster analyses). Second, we acknowledge that our generated subgroups were based on the measures used in this study which were primarily aligned with the Fear-Avoidance Model of Musculoskeletal Pain41 and that including other potentially important psychological factors (e.g., self-efficacy) may have influenced our findings. Third, although we cannot confirm that patients in our study sample were or were not pre-screened by primary care physicians prior to being referred for physical therapy, patients in this study sample were associated with increased severity evidenced by higher mean pain intensity ratings (5.3 vs. 3.2 points) and self-reported disability scores (OSW scores: 16.2 points vs. Roland-Morris Disability Questionnaire scores: 6.7 points) when compared to primary care patients enrolled in the SBT development cohort.25 Finally, this study did not incorporate any predictive analyses with the empirically derived subgroups as that was beyond our purpose. Previous study findings1 suggest that the SBT may be valuable as a prognostic indicator for self-reported disability outcomes at 6-months when compared to unidimensional psychological measures thereby providing evidence for the SBT's predictive validity in physical therapy settings.
Conclusion
The SBT provides a viable option for use as an initial screening measure to identify elevated levels of pain-associated psychological distress and maladaptive coping as it adequately distinguishes among commonly used single construct, unidimensional measures. Our findings do provide suggestions for future research related to evaluation of a modified risk stratification scheme using different cutoff scores to identify low and high pain-associated psychologically distressed and maladaptive coping LBP patients referred for treatment in physical therapy and other secondary care settings.
Perspective.
This study suggests that the SBT can replace administering several unidimensional psychological measures as a first line screening measure for psychological distress. However clinicians need to be aware of potential for misclassification with SBT results when compared to unidimensional measures. This study also suggests a modified SBT risk stratification scheme based on empirically derived subgroups could potentially assist in identifying elevated levels of pain-associated psychological distress, maladaptive coping and disability in practice settings outside of primary care. Patients identified with elevated levels of pain-associated distress and maladaptive coping may be indicated for additional assessment using construct specific questionnaires.
Highlights.
We compared two screening approaches for identifying pain related distress.
STarT Back Tool (SBT) risk dependent relationships were identified.
Depressive symptoms were strongly related to SBT high risk categorization.
Clinicians need to be aware of misclassification when using the SBT.
Alternate subgroup methods could potentially improve screening outside primary care.
Acknowledgements
This study was conducted as part of JMB's doctoral dissertation, therefore he would like to acknowledge other dissertation committee members (i.e., Mark D. Bishop, PT, PhD; Julie M. Fritz, PT, PhD; Nabih R. Asal, PhD, FACE). We would also like to acknowledge the following clinicians and personnel from Brooks Rehabilitation in Jacksonville, Florida (M. Brian Hagist, Tim Shreve, Jason Kral, Matthew Stafford, Ryan Reed, Michael Spigel, Holly Morris, Flo Singletary, Amanda Osborne, Robert Rowe) and the University of Florida Orthopaedics and Sports Medicine Institute and Shands Rehabilitation Center at Magnolia Parke in Gainesville, Florida (Giorgio Zeppieri, Josh Barabas, Debi Jones, Derek Miles, Zack Sutton, Dalton Reed, Michael Hodges, Shannon Long, Tim Shay, Amy Borut, Yvette Silvey). Dr. Robinson's lab (Anne Nisenzon, Calia Torres and Laura Wandner) assisted with data collection and management.
This study was funded by a 2009 award from the Brooks Health System to the University of Florida Foundation. JMB was supported by a National Institutes of Health T32 Neuromuscular Plasticity Research Training Fellowship grant (T32 HD043730). This manuscript was written while JMB received support from the National Institutes of Health Rehabilitation Research Career Development Program (K12-HD055929).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosures
The authors declare no financial interest in the results of this research.
References
- 1.Beneciuk JM, Bishop MD, Fritz JM, Robinson ME, Asal NR, Nisenzon AN, George SZ. The STarT Back Screening Tool and Individual Psychological Measures: Evaluation of Prognostic Capabilities for Low Back Pain Clinical Outcomes in Outpatient Physical Therapy Settings. Phys Ther. 2013;93:321–333. doi: 10.2522/ptj.20120207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Beneciuk JM, Robinson ME, George SZ. Low back pain subgroups using fear-avoidance model measures: results of a cluster analysis. Clin J Pain. 2012;28:658–666. doi: 10.1097/AJP.0b013e31824306ed. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bergbom S, Boersma K, Overmeer T, Linton SJ. Relationship among pain catastrophizing, depressed mood, and outcomes across physical therapy treatments. Phys Ther. 2011;91:754–764. doi: 10.2522/ptj.20100136. [DOI] [PubMed] [Google Scholar]
- 4.Bieling PJ, Antony MM, Swinson RP. The State-Trait Anxiety Inventory, Trait version: structure and content re-examined. Behav Res Ther. 1998;36:777–788. doi: 10.1016/s0005-7967(98)00023-0. [DOI] [PubMed] [Google Scholar]
- 5.Boersma K, Linton SJ. Screening to identify patients at risk: profiles of psychological risk factors for early intervention. Clin J Pain. 2005;21:38–43. doi: 10.1097/00002508-200501000-00005. discussion 69-72. [DOI] [PubMed] [Google Scholar]
- 6.Boersma K, Linton SJ. Psychological processes underlying the development of a chronic pain problem: a prospective study of the relationship between profiles of psychological variables in the fear-avoidance model and disability. Clin J Pain. 2006;22:160–166. doi: 10.1097/01.ajp.0000159582.37750.39. [DOI] [PubMed] [Google Scholar]
- 7.Bolton JE. Accuracy of recall of usual pain intensity in back pain patients. Pain. 1999;83:533–539. doi: 10.1016/S0304-3959(99)00161-X. [DOI] [PubMed] [Google Scholar]
- 8.Childs JD, Piva SR, Fritz JM. Responsiveness of the numeric pain rating scale in patients with low back pain. Spine. 2005;30:1331–1334. doi: 10.1097/01.brs.0000164099.92112.29. [DOI] [PubMed] [Google Scholar]
- 9.Chou R, Qaseem A, Snow V, Casey D, Cross JT, Jr., Shekelle P, Owens DK. Clinical Efficacy Assessment Subcommittee of the American College of P, American College of P, American Pain Society Low Back Pain Guidelines P. Diagnosis and treatment of low back pain: a joint clinical practice guideline from the American College of Physicians and the American Pain Society. Ann Intern Med. 2007;147:478–491. doi: 10.7326/0003-4819-147-7-200710020-00006. [DOI] [PubMed] [Google Scholar]
- 10.Chou R, Shekelle P. Will this patient develop persistent disabling low back pain? JAMA. 2010;303:1295–1302. doi: 10.1001/jama.2010.344. [DOI] [PubMed] [Google Scholar]
- 11.Crombez G, Eccleston C, Baeyens F, Eelen P. When somatic information threatens, catastrophic thinking enhances attentional interference. Pain. 1998;75:187–198. doi: 10.1016/s0304-3959(97)00219-4. [DOI] [PubMed] [Google Scholar]
- 12.Crombez G, Vlaeyen JW, Heuts PH, Lysens R. Pain-related fear is more disabling than pain itself: evidence on the role of pain-related fear in chronic back pain disability. Pain. 1999;80:329–339. doi: 10.1016/s0304-3959(98)00229-2. [DOI] [PubMed] [Google Scholar]
- 13.Damush TM, Wu J, Bair MJ, Sutherland JM, Kroenke K. Self-management practices among primary care patients with musculoskeletal pain and depression. J Behav Med. 2008;31:301–307. doi: 10.1007/s10865-008-9156-5. [DOI] [PubMed] [Google Scholar]
- 14.Denison E, Asenlof P, Sandborgh M, Lindberg P. Musculoskeletal pain in primary health care: subgroups based on pain intensity, disability, self-efficacy, and fear-avoidance variables. The journal of pain : official journal of the American Pain Society. 2007;8:67–74. doi: 10.1016/j.jpain.2006.06.007. [DOI] [PubMed] [Google Scholar]
- 15.Fairbank JC, Pynsent PB. The Oswestry Disability Index. Spine (Phila Pa 1976) 2000;25:2940–2952. doi: 10.1097/00007632-200011150-00017. discussion 2952. [DOI] [PubMed] [Google Scholar]
- 16.Foster NE, Dziedzic KS, van der Windt DA, Fritz JM, Hay EM. Research priorities for non-pharmacological therapies for common musculoskeletal problems: nationally and internationally agreed recommendations. BMC Musculoskelet Disord. 2009;10:3. doi: 10.1186/1471-2474-10-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Foster NE, Hill JC, O'Sullivan P, Hancock M. Stratified models of care. Best practice & research. Clinical rheumatology. 2013;27:649–661. doi: 10.1016/j.berh.2013.10.005. [DOI] [PubMed] [Google Scholar]
- 18.Fritz JM, George SZ. Identifying psychosocial variables in patients with acute work- related low back pain: the importance of fear-avoidance beliefs. Phys Ther. 2002;82:973–983. [PubMed] [Google Scholar]
- 19.Fritz JM, George SZ, Delitto A. The role of fear-avoidance beliefs in acute low back pain: relationships with current and future disability and work status. Pain. 2001;94:7–15. doi: 10.1016/S0304-3959(01)00333-5. [DOI] [PubMed] [Google Scholar]
- 20.Fritz JM, Irrgang JJ. A comparison of a modified Oswestry Low Back Pain Disability Questionnaire and the Quebec Back Pain Disability Scale. Phys Ther. 2001;81:776–788. doi: 10.1093/ptj/81.2.776. [DOI] [PubMed] [Google Scholar]
- 21.George SZ, Fritz JM, Bialosky JE, Donald DA. The effect of a fear-avoidance-based physical therapy intervention for patients with acute low back pain: results of a randomized clinical trial. Spine (Phila Pa 1976) 2003;28:2551–2560. doi: 10.1097/01.BRS.0000096677.84605.A2. [DOI] [PubMed] [Google Scholar]
- 22.Goldstein MS, Scalzitti DA, Craik RL, Dunn SL, Irion JM, Irrgang J, Kolobe TH, McDonough CM, Shields RK. The revised research agenda for physical therapy. Phys Ther. 2011;91:165–174. doi: 10.2522/ptj.20100248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hair JE, Anderson RE, Tatham RL, Black WC. Cluster Analysis. In: Boyd J, editor. Multivariate Data Analysis. Prentice Hall; Upper Saddle River, NJ: 1998. pp. 469–515. [Google Scholar]
- 24.Hay EM, Dunn KM, Hill JC, Lewis M, Mason EE, Konstantinou K, Sowden G, Somerville S, Vohora K, Whitehurst D, Main CJ. A randomised clinical trial of subgrouping and targeted treatment for low back pain compared with best current care. The STarT Back Trial Study Protocol. BMC Musculoskelet Disord. 2008;9:58. doi: 10.1186/1471-2474-9-58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hill JC, Dunn KM, Lewis M, Mullis R, Main CJ, Foster NE, Hay EM. A primary care back pain screening tool: identifying patient subgroups for initial treatment. Arthritis Rheum. 2008;59:632–641. doi: 10.1002/art.23563. [DOI] [PubMed] [Google Scholar]
- 26.Hill JC, Dunn KM, Main CJ, Hay EM. Subgrouping low back pain: a comparison of the STarT Back Tool with the Orebro Musculoskeletal Pain Screening Questionnaire. Eur J Pain. 2010;14:83–89. doi: 10.1016/j.ejpain.2009.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hill JC, Fritz JM. Psychosocial influences on low back pain, disability, and response to treatment. Phys Ther. 2011;91:712–721. doi: 10.2522/ptj.20100280. [DOI] [PubMed] [Google Scholar]
- 28.Hill JC, Whitehurst DG, Lewis M, Bryan S, Dunn KM, Foster NE, Konstantinou K, Main CJ, Mason E, Somerville S, Sowden G, Vohora K, Hay EM. Comparison of stratified primary care management for low back pain with current best practice (STarT Back): a randomised controlled trial. Lancet. 2011;378:1560–1571. doi: 10.1016/S0140-6736(11)60937-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Huang FY, Chung H, Kroenke K, Delucchi KL, Spitzer RL. Using the Patient Health Questionnaire-9 to measure depression among racially and ethnically diverse primary care patients. J Gen Intern Med. 2006;21:547–552. doi: 10.1111/j.1525-1497.2006.00409.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hudson-Cook N, Tomes-Nicholson K, Breen A. A revised Oswestry disability questionnaire. In: Roland MO, Jenner JR, editors. Back Pain: New Approaches to Rehabilitation and Education. Manchester University Press; New York, NY: 1989. pp. 187–204. [Google Scholar]
- 31.Jacob T, Baras M, Zeev A, Epstein L. Low back pain: reliability of a set of pain measurement tools. Arch Phys Med Rehabil. 2001;82:735–742. doi: 10.1053/apmr.2001.22623. [DOI] [PubMed] [Google Scholar]
- 32.Jellema P, van der Windt DA, van der Horst HE, Blankenstein AH, Bouter LM, Stalman WA. Why is a treatment aimed at psychosocial factors not effective in patients with (sub)acute low back pain? Pain. 2005;118:350–359. doi: 10.1016/j.pain.2005.09.002. [DOI] [PubMed] [Google Scholar]
- 33.Jensen MP, Turner JA, Romano JM, Fisher LD. Comparative reliability and validity of chronic pain intensity measures. Pain. 1999;83:157–162. doi: 10.1016/s0304-3959(99)00101-3. [DOI] [PubMed] [Google Scholar]
- 34.Jensen MP, Turner LR, Turner JA, Romano JM. The use of multiple-item scales for pain intensity measurement in chronic pain patients. Pain. 1996;67:35–40. doi: 10.1016/0304-3959(96)03078-3. [DOI] [PubMed] [Google Scholar]
- 35.Kabacoff RI, Segal DL, Hersen M, Van Hasselt VB. Psychometric properties and diagnostic utility of the Beck Anxiety Inventory and the State-Trait Anxiety Inventory with older adult psychiatric outpatients. J Anxiety Disord. 1997;11:33–47. doi: 10.1016/s0887-6185(96)00033-3. [DOI] [PubMed] [Google Scholar]
- 36.Kent PM, Keating JL, Taylor NF. Primary care clinicians use variable methods to assess acute nonspecific low back pain and usually focus on impairments. Manual therapy. 2009;14:88–100. doi: 10.1016/j.math.2007.12.006. [DOI] [PubMed] [Google Scholar]
- 37.Ketchen DJ, Shook CL. The application of cluster analysis in strategic management research: an analysis and critique. Strategic Management Journal. 1996;17:441–458. [Google Scholar]
- 38.Koes BW, van Tulder MW, Thomas S. Diagnosis and treatment of low back pain. BMJ. 2006;332:1430–1434. doi: 10.1136/bmj.332.7555.1430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kongsted A, Johannesen E, Leboeuf-Yde C. Feasibility of the STarT back screening tool in chiropractic clinics: a cross-sectional study of patients with low back pain. Chiropr Man Therap. 2011;19:10. doi: 10.1186/2045-709X-19-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Leeuw M, Goossens ME, Linton SJ, Crombez G, Boersma K, Vlaeyen JW. The fear-avoidance model of musculoskeletal pain: current state of scientific evidence. J Behav Med. 2007;30:77–94. doi: 10.1007/s10865-006-9085-0. [DOI] [PubMed] [Google Scholar]
- 42.Linton SJ, Nicholas MK, MacDonald S, Boersma K, Bergbom S, Maher C, Refshauge K. The role of depression and catastrophizing in musculoskeletal pain. Eur J Pain. 2011;15:416–422. doi: 10.1016/j.ejpain.2010.08.009. [DOI] [PubMed] [Google Scholar]
- 43.Main CJ, George SZ. Psychologically informed practice for management of low back pain: future directions in practice and research. Phys Ther. 2011;91:820–824. doi: 10.2522/ptj.20110060. [DOI] [PubMed] [Google Scholar]
- 44.Meyers LW, Gamst G, Guarino AJ. Applied Multivariate Research: Design and Interpretation. Sage Publications; Thousand Oaks, CA: 2006. [Google Scholar]
- 45.Milligan GA, Cooper MC. An examination of procedures for determining the number of clusters in a data set. Psychometrika. 1985;50:159–179. [Google Scholar]
- 46.Morso L, Kent P, Albert HB, Manniche C. Is the psychosocial profile of people with low back pain seeking care in Danish primary care different from those in secondary care? Manual therapy. 2013;18:54–59. doi: 10.1016/j.math.2012.07.002. [DOI] [PubMed] [Google Scholar]
- 47.Nicholas MK, Linton SJ, Watson PJ, Main CJ. Decade of the Flags” Working G. Early identification and management of psychological risk factors (“yellow flags”) in patients with low back pain: a reappraisal. Phys Ther. 2011;91:737–753. doi: 10.2522/ptj.20100224. [DOI] [PubMed] [Google Scholar]
- 48.Osman A, Barrios FX, Gutierrez PM, Kopper BA, Merrifield T, Grittmann L. The Pain Catastrophizing Scale: further psychometric evaluation with adult samples. J Behav Med. 2000;23:351–365. doi: 10.1023/a:1005548801037. [DOI] [PubMed] [Google Scholar]
- 49.Pincus T, Smeets RJ, Simmonds MJ, Sullivan MJ. The fear avoidance model disentangled: improving the clinical utility of the fear avoidance model. Clin J Pain. 2010;26:739–746. doi: 10.1097/AJP.0b013e3181f15d45. [DOI] [PubMed] [Google Scholar]
- 50.Pransky G, Borkan JM, Young AE, Cherkin DC. Are we making progress?: the tenth international forum for primary care research on low back pain. Spine (Phila Pa 1976) 2011;36:1608–1614. doi: 10.1097/BRS.0b013e3181f6114e. [DOI] [PubMed] [Google Scholar]
- 51.Robinson ME, George SZ. Screening for problematic low back pain: STarT. Pain. 2012;153:2159–2160. doi: 10.1016/j.pain.2012.07.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Roland M, Fairbank J. The Roland-Morris Disability Questionnaire and the Oswestry Disability Questionnaire. Spine (Phila Pa 1976) 2000;25:3115–3124. doi: 10.1097/00007632-200012150-00006. [DOI] [PubMed] [Google Scholar]
- 53.Roland M, Morris R. A study of the natural history of back pain. Part I: development of a reliable and sensitive measure of disability in low-back pain. Spine (Phila Pa 1976) 1983;8:141–144. doi: 10.1097/00007632-198303000-00004. [DOI] [PubMed] [Google Scholar]
- 54.Spielberger CD, Gorsuch RL, Lushene RE, Vagg PR, Jacobs GA. Manual for the state and trait anxiety inventory (Form Y) Consulting Psychologists Press; Palo Alto, CA: 1983. [Google Scholar]
- 55.Staerkle R, Mannion AF, Elfering A, Junge A, Semmer NK, Jacobshagen N, Grob D, Dvorak J, Boos N. Longitudinal validation of the fear-avoidance beliefs questionnaire (FABQ) in a Swiss-German sample of low back pain patients. Eur Spine J. 2004;13:332–340. doi: 10.1007/s00586-003-0663-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Sullivan M, Bishop S, Pivik J. The Pain Catastrophizing Scale: development and validation. Psychological Assessment. 1995;7:524–532. [Google Scholar]
- 57.Swinkels-Meewisse IE, Roelofs J, Schouten EG, Verbeek AL, Oostendorp RA, Vlaeyen JW. Fear of movement/(re)injury predicting chronic disabling low back pain: a prospective inception cohort study. Spine (Phila Pa 1976) 2006;31:658–664. doi: 10.1097/01.brs.0000203709.65384.9d. [DOI] [PubMed] [Google Scholar]
- 58.Swinkels-Meewisse IE, Roelofs J, Verbeek AL, Oostendorp RA, Vlaeyen JW. Fear-avoidance beliefs, disability, and participation in workers and non-workers with acute low back pain. Clin J Pain. 2006;22:45–54. doi: 10.1097/01.ajp.0000148626.84874.93. [DOI] [PubMed] [Google Scholar]
- 59.Tabachnick BG, Fidell LS. Using Multivariate Statistics. 5th edition Pearson /Allyn and Bacon; Boston, MA: 2007. [Google Scholar]
- 60.van der Windt D, Hay E, Jellema P, Main C. Psychosocial interventions for low back pain in primary care: lessons learned from recent trials. Spine (Phila Pa 1976) 2008;33:81–89. doi: 10.1097/BRS.0b013e31815e39f9. [DOI] [PubMed] [Google Scholar]
- 61.Waddell G, Newton M, Henderson I, Somerville D, Main CJ. A Fear-Avoidance Beliefs Questionnaire (FABQ) and the role of fear-avoidance beliefs in chronic low back pain and disability. Pain. 1993;52:157–168. doi: 10.1016/0304-3959(93)90127-B. [DOI] [PubMed] [Google Scholar]
- 62.Westman AE, Boersma K, Leppert J, Linton SJ. Fear-avoidance beliefs, catastrophizing, and distress: a longitudinal subgroup analysis on patients with musculoskeletal pain. Clin J Pain. 2011;27:567–577. doi: 10.1097/AJP.0b013e318219ab6c. [DOI] [PubMed] [Google Scholar]
- 63.Wideman TH, Hill JC, Main CJ, Lewis M, Sullivan MJ, Hay EM. Comparing the responsiveness of a brief, multidimensional risk screening tool for back pain to its unidimensional reference standards: the whole is greater than the sum of its parts. Pain. 2012;153:2182–2191. doi: 10.1016/j.pain.2012.06.010. [DOI] [PubMed] [Google Scholar]
- 64.Wideman TH, Sullivan MJ. Development of a cumulative psychosocial factor index for problematic recovery following work-related musculoskeletal injuries. Phys Ther. 2012;92:58–68. doi: 10.2522/ptj.20110071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Woby SR, Roach NK, Urmston M, Watson PJ. Psychometric properties of the TSK-11: a shortened version of the Tampa Scale for Kinesiophobia. Pain. 2005;117:137–144. doi: 10.1016/j.pain.2005.05.029. [DOI] [PubMed] [Google Scholar]